Abstract
Objective
To examine the impact of neighbourhood marginalization on avoidable mortality (AM) from preventable and treatable causes of death.
Methods
All premature deaths between 1993 and 2014 (N = 691,453) in Ontario, Canada, were assigned to quintiles of neighbourhood marginalization using the four dimensions of the Ontario Marginalization Index: dependency, ethnic concentration, material deprivation, and residential instability. We conducted two multivariate logistic regressions to examine the association between neighbourhood marginalization, first with AM compared with non-AM as the outcome, and second with AM from preventable causes compared with treatable causes as the outcome. All models were adjusted for decedent age, sex, urban/rural location, and level of comorbidity.
Results
A total of 463,015 deaths were classified as AM and 228,438 deaths were classified as non-AM. Persons living in the most materially deprived (OR, 1.24; 95% CI, 1.22 to 1.27) and residentially unstable neighbourhoods (OR, 1.13; 95% CI, 1.11 to 1.15) had greater odds of AM, particularly from preventable causes. Those living in the most dependent (OR, 0.91; 95% CI, 0.89 to 0.93) and ethnically concentrated neighbourhoods (OR, 0.93; 95% CI, 0.91 to 0.93) had lower odds of AM, although when AM occurred, it was more likely to arise from treatable causes.
Conclusion
Different marginalization dimensions have unique associations with AM. By identifying how different aspects of neighbourhood marginalization influence AM, these results may have important implications for future public health efforts to reduce inequities in avoidable deaths.
Electronic supplementary material
The online version of this article (10.17269/s41997-019-00270-9) contains supplementary material, which is available to authorized users.
Keywords: Marginalization, Dependency, Ethnic concentration, Material deprivation, Residential instability, Avoidable mortality
Résumé
Objectif
Examiner les incidences de la marginalisation du quartier sur la mortalité évitable due aux causes de décès évitables et traitables.
Méthode
Tous les décès prématurés survenus entre 1993 et 2014 (n = 691 453) en Ontario, au Canada, ont été associés à un quintile de marginalisation du quartier à l’aide des quatre dimensions de l’indice de marginalisation ontarien : la dépendance, la concentration ethnique, la défavorisation matérielle et l’instabilité résidentielle. Nous avons effectué deux régressions logistiques multivariées pour examiner l’association entre la marginalisation du quartier, la première axée sur la mortalité évitable (MÉ) comparée à la mortalité inévitable, et la seconde axée sur la MÉ de causes évitables comparée à la MÉ de causes traitables. Tous les modèles ont été ajustés en fonction de l’âge, du sexe, du milieu de vie (urbain ou rural) et des niveaux de comorbidité de la personne décédée.
Résultats
En tout, 463 015 décès ont été catégorisés comme étant évitables, et 228 438 décès comme étant inévitables. Les résidents des quartiers les plus défavorisés sur le plan matériel (RC : 1,24, IC de 95 % : 1,22 à 1,27) et les plus instables sur le plan résidentiel (RC : 1,13, IC de 95 % : 1,11 à 1,15) présentaient une probabilité accrue de MÉ, particulièrement de causes évitables. Chez les résidents des quartiers présentant la plus grande dépendance (RC : 0,91, IC de 95 % : 0,89 à 0,93) et la plus grande concentration ethnique (RC : 0,93, IC de 95 % : 0,91 à 0,93), la probabilité de MÉ était plus faible, mais quand elle survenait, elle était plus susceptible de découler de causes traitables.
Conclusion
Différentes dimensions de la marginalisation présentent des associations uniques avec la MÉ. En indiquant comment différents aspects de la marginalisation du quartier influencent la MÉ, ces résultats peuvent avoir des conséquences importantes pour les futures démarches de santé publique visant à réduire les inégalités devant la mortalité évitable.
Mots-clés: Marginalisation sociale, Dépendance, Concentration ethnique, Défavorisation matérielle, Instabilité résidentielle, Mortalité évitable
Introduction
Avoidable mortality (AM) is a population health indicator that has been used to assess health system functioning and to identify areas for targeted health system intervention (Nolte and McKee 2004; James et al. 2006; James et al. 2007). AM is defined as deaths considered preventable or treatable given existing medical and public health interventions (Canadian Institute for Health Information 2012). AM from preventable causes includes deaths that could be averted through public health and policy interventions as well as primary prevention, for example those aimed at curbing tobacco use or increasing vaccination uptake (Canadian Institute for Health Information 2012). AM from treatable causes encompasses deaths that could be averted or delayed by secondary and tertiary prevention efforts as well as medical treatment, such as timely detection and effective treatment of colorectal and breast cancer (Canadian Institute for Health Information 2012).
Marginalized populations are at greater risk of adverse health outcomes, including mortality (Commission on Social Determinants of Health 2008; Mikkonen and Raphael 2010). Several studies have demonstrated the association between individual social factors and AM. For example, First Nations adults in Canada have more than twice the AM when compared with non-First Nations adults; immigrants and those with higher income have lower rates of AM (Khan et al. 2017; Omariba 2015; Park et al. 2015). Higher AM rates have been identified in men than in women and in urban than in rural areas (James et al. 2006; Sundmacher 2013).
Socio-economic inequities tend to be greater for AM from preventable causes than from treatable causes (James et al. 2006; James et al. 2007). Previous studies examining the association between marginalization and AM are limited by non-validated definitions of AM, older data, one-dimensional indicators of marginalization, and lack of adjustment for other factors known to be associated with mortality (James et al. 2006; James et al. 2007). To our knowledge, no study has addressed these gaps by using summary measures of marginalization in a population-based cohort.
As the determinants of health intersect in complex ways, there have been efforts to develop meaningful multi-dimension indicators of marginalization that can be used to more accurately estimate their impact on health outcomes (Hankivsky and Christoffersen 2008). The Ontario Marginalization (ON-Marg) index is a theoretically grounded and validated index developed to identify multiple dimensions of marginalization in the province of Ontario at the neighbourhood level (Matheson and van Ingen 2006; Matheson et al. 2012). The ON-Marg Index links individual postal code data to Canadian census tract data to assign every individual a level of marginalization based on the neighbourhood they live in (Matheson and van Ingen 2006; Matheson et al. 2012). The ON-Marg Index applies four dimensions of marginalization: dependency (population workforce eligibility), ethnic concentration (recent immigration and visible minorities), material deprivation (income, education, single-parent families), and residential instability (home security, ownership, and occupancy) (Matheson and van Ingen 2006; Matheson et al. 2012). The ON-Marg Index has been used to assess avoidable health outcomes for subsets of the population, including glycemic control among persons with diabetes (Inman et al. 2016), cardiac arrests (Buick et al. 2016), and motorized vehicle collisions (Silverman et al. 2013).
The objective of our study was to examine the relative impact of the four dimensions of neighbourhood marginalization on AM for the entire population of Ontario, Canada’s most populous province with universal funding of physician services.
Methods
Study design
We conducted a retrospective population-based study to identify all decedents in Ontario between January 1, 1993 and December 31, 2014.
Data sources
We used the health administrative databases at ICES (formerly the Institute for Clinical Evaluative Sciences). These de-identified databases are linked at the individual level using encrypted health card numbers as unique identifiers and are made available through a data-sharing agreement with the Ontario Ministry of Health and Long-Term Care. Databases included the following: The Office of the Registrar General – Deaths (ORG-D) to identify decedents and obtain primary cause of death data, coded using the 9th and 10th editions of the International Classification of Diseases (ICD-9 and ICD-10); the Ontario Health Insurance Plan (OHIP) database; the Registered Persons Database (RPDB) to link decedents with demographic information, including age, sex, and postal code; and the Ontario Marginalization (ON-Marg) index calculated using the Canadian Census 2001 and 2006. Data on comorbidities were obtained from a variety of administrative databases, including hospitalizations from the Discharge Abstract Database (DAD) and emergency department visits from the National Ambulatory Care Reporting System (NACRS) database. We used validated ICES macros to identify the presence of multi-morbidities (Gruneir et al. 2016; Lane et al. 2015; Mondor et al. 2016; Mondor et al. 2017; Pefoyo et al. 2015; Petrosyan et al. 2017; Thavorn et al. 2017).
Study population
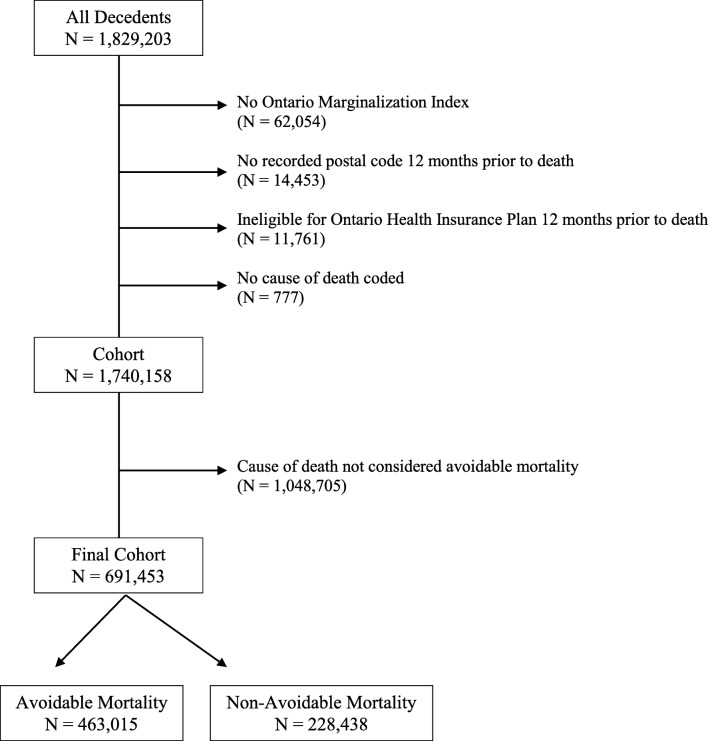
We captured all decedents in Ontario using the ORG-D. We excluded those with no ON-Marg Index, no recorded postal code 12 months prior to death, ineligible for OHIP coverage 12 months prior to death, and no cause of death coded. Reasons individuals may not have an ON-Marg Index include having a new postal code not available in the years for which the index was created (2001 or 2006), a postal code error in the database, and missing data in the dissemination area or census tract files due to small cell size data suppression. We then excluded all deaths not considered premature (i.e., occurring at age 75 or greater). Records with missing data in at least one of our independent covariates were excluded from the logistic regression analysis.
ON-Marg Index
Our primary exposure of interest was neighbourhood-level marginalization, measured using the ON-Marg Index (Matheson and van Ingen 2006). The ON-Marg Index is a validated tool that links individual postal code data to census tract-level data to assign inequalities in health and social well-being within Ontario at the neighbourhood level. The ON-Marg Index includes four dimensions of marginalization: dependency, ethnic concentration, material deprivation, and residential instability. Each ON-Marg dimension is a summary measure of multiple constructs of marginalization (Appendix 1). Decedents in our cohort were linked to the ON-Marg Index using 2001 census data (for deaths until December 31, 2003) and 2006 census data (for deaths after January 1, 2004). For each census year and each marginalization dimension, postal codes were scored, ranked, and categorized into quintiles, with quintile 1 (Q1) considered the least marginalized and quintile 5 (Q5) the most marginalized. The ON-Marg Index dimensions can be considered separately or combined into a total marginalization score; however, if one or more dimensions are in the opposite direction of effect, the ON-Marg Index user guide does not recommend combining the dimensions (Matheson and van Ingen 2006). ON-Marg Index dimensions cannot be stratified into their constructs.
Independent variables
Independent variables included decedent age, sex, urban vs. rural location (du Plessis et al. 2001), and level of comorbidity. These independent variables were chosen given their previous associations with AM and are adjusted for in our analyses as we expect they may vary by quintile of marginalization. We used previously established methods to ascertain the presence of 18 chronic conditions, including the following: acute myocardial infarction, cardiac arrhythmia, asthma, cancer, congestive heart failure, chronic obstructive pulmonary disease, chronic coronary syndrome, dementia, diabetes, hypertension, inflammatory bowel disease, mood disorders, other mental health disorders, osteoarthritis, osteoporosis, renal failure, rheumatoid arthritis, and stroke. We categorized comorbidities into the following levels: low (0 to 3 chronic conditions), medium (4 to 5 chronic conditions), high (6 chronic conditions), and very high (greater than 7 chronic conditions).
Dependent variables
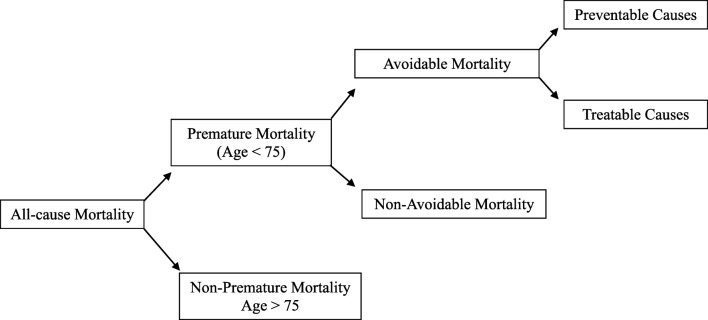
Figure 1 shows the CIHI classifications of mortality. Our primary outcome was AM, defined by CIHI as premature deaths occurring before 75 years of age with a preventable or treatable cause of death. CIHI defined AM and included various preventable and treatable causes of death based on a standard set of ICD-9 and ICD-10 codes (Appendix 2) (Canadian Institute for Health Information 2012). All premature deaths not classified as AM were classified as non-AM.
Fig. 1.
Classifications of mortality (Canadian Institute for Health Information 2012)
Analyses
We used frequencies and proportions to report characteristics of the study population. We then calculated annual age–sex-standardized mortality rates per 100,000 population for overall AM, preventable AM, and treatable AM to examine trends over time. We used two multivariable logistic regression models to assess the relationship between all of the ON-Marg Index dimensions and AM, controlling for potential confounders. First, among decedents with premature mortality, we estimated odds ratios (ORs) of AM by quintile of the ON-Marg Index dimensions with non-AM as the reference category. Second, among decedents with AM, we estimated ORs for AM from preventable causes by quintile of the ON-Marg Index dimension with AM from treatable causes as the reference category. We adjusted these models for age (reference, age 0–17), sex (reference, female sex), rural location (reference, urban location), and levels of comorbidities (reference low comorbidity). In order to determine if the association between marginalization and AM changed over time, for each regression model, we conducted a sensitivity analysis to include time dummy variables.
As the data structure and coding practice in the ORG-D were modified in 2013, leading to a change in how primary cause of death was attributed to different disease groups, for each regression model we conducted a sensitivity analysis excluding data from 2013 and 2014. We present results as ORs along with 95% confidence intervals (CI). All statistical tests were two-tailed and we used p < 0.05 to determine statistical significance. All analyses were performed using SAS Software (version 9.4.3.0).
Results
There were 1,829,203 deaths in Ontario between 1993 and 2014. After exclusions (n = 89,045) and removal of non-premature deaths (n = 1,048,705), our final cohort included 691,453 decedents with a premature death (Fig. 2). In addition, there were 5014 records with missing data in at least one of our independent covariates excluded from the logistic regression analysis.
Fig. 2.
Flow diagram of excluded decedents and final cohort
Table 1 illustrates the characteristics of our cohort by type of mortality. Of the premature deaths, 463,015 (67.0%) were AM and 228,438 (33.0%) were non-AM. Of the avoidable deaths, 294,799 (63.7%) were attributable to preventable causes while 168,216 (36.3%) were attributable to treatable causes. Compared with women, men were nearly twice as likely to have AM from preventable causes (65.9% men vs. 34.1% women), but this difference was attenuated for AM from treatable causes (52.8% men vs. 47.2% women).
Table 1.
Characteristics of decedent cohort by type of mortality
| Variable | Deaths from all causes | Deaths from premature causes | |||
|---|---|---|---|---|---|
| Avoidable mortality (AM) | Non-avoidable mortality | ||||
| Overall AM | AM from preventable causes | AM from treatable causes | |||
| Total population | N = 1,740,158 | N = 463,015 | N = 294,799 | N = 168,216 | N = 228,438 |
| Age (years) | |||||
| Mean age ± SD | 75.1 ± 15.5 | 60.5 ± 12.5 | 60.0 ± 12.9 | 61.5 ± 11.7 | 59.2 ± 14.4 |
| 0-17 | 8689 (0.5%) | 4060 (0.9%) | 2563 (0.9%) | 1497 (0.9%) | 4629 (2.0%) |
| 18-44 | 72,399 (4.2%) | 44,874 (9.7%) | 32,486 (11.0%) | 12,388 (7.4%) | 27,525 (12.0%) |
| 45-54 | 181,943 (10.5%) | 124,343 (26.9%) | 78,604 (26.7%) | 45,739 (27.2%) | 57,600 (25.2%) |
| 55-64 | 96,981 (5.6%) | 66,302 (14.3%) | 42,741 (14.5%) | 23,561 (14.0%) | 30,679 (13.4%) |
| 65-74 | 331,073 (19.0%) | 223,239 (48.2%) | 138,323 (46.9%) | 84,916 (50.5%) | 107,834 (47.2%) |
| 75-84 | 526,801 (30.3%) | n/a | n/a | n/a | n/a |
| 85+ | 521,904 (30.0%) | n/a | n/a | n/a | n/a |
| Missing | 368 (0.0%) | 197 (0.0%) | 82 (0.0%) | 115 (0.1%) | 171 (0.1%) |
| Sex | |||||
| F | 862,432 (49.6%) | 179,918 (38.9%) | 100,503 (34.1%) | 79,415 (47.2%) | 94,661 (41.4%) |
| M | 877,718 (50.4%) | 283,096 (61.1%) | 194,295 (65.9%) | 88,801 (52.8%) | 133,774 (58.6%) |
| Urban vs. Rural | |||||
| Urban | 1,469,787 (84.5%) | 388,824 (84.0%) | 246,877 (83.7%) | 141,947 (84.4%) | 191,822 (84.0%) |
| Rural | 268,544 (15.4%) | 73,654 (15.9%) | 47,579 (16.1%) | 26,075 (15.5%) | 36,337 (15.9%) |
| Missing | 1827 (0.1%) | 537 (0.1%) | 343 (0.1%) | 194 (0.1%) | 279 (0.1%) |
| Total Comorbidities | |||||
| Mean ± SD | 4.1 ± 2.2 | 3.4 ± 2.2 | 3.3 ± 2.2 | 3.5 ± 2.2 | 3.2 ± 2.1 |
| Low (0-3) | 739,361 (42.5%) | 264,966 (57.2%) | 172,042 (58.4%) | 92,924 (55.2%) | 138,711 (60.7%) |
| Medium (4-5) | 531,402 (30.5%) | 118,141 (25.5%) | 75,079 (25.5%) | 43,062 (25.6%) | 57,759 (25.3%) |
| High (6) | 195,296 (11.2% | 35,127 (7.6%) | 21,453 (7.3%) | 13,674 (8.1%) | 15,093 (6.6%) |
| Very high (≥7) | 274,099 (15.8%) | 44,781 (9.7%) | 26,225 (8.9%) | 18,556 (11.0%) | 16,875 (7.4%) |
Table 2 presents population totals by the ON-Marg Index dimension for each type of mortality. There were clear gradients for AM from preventable and treatable causes, with increasing mortality as marginalization increased for the dependency, material deprivation, and residential instability dimensions. A reverse trend was observed for ethnic concentration. For most dimensions, the difference between Q1 and Q5 was greater for AM from preventable causes compared with that for AM from treatable cause: ethnic concentration (4.9% vs. 4.0%), material deprivation (13.4% vs. 11.0%), and residential instability (16.7% vs. 14.2%). For the dependency dimension, however, the difference between Q1 and Q5 was greater for AM from treatable causes (12.8% vs. 11.5%).
Table 2.
ON-Marg Index dimensions among decedent cohort by mortality category
| Variable | Deaths from all causes | Deaths from premature causes | |||
|---|---|---|---|---|---|
| Avoidable mortality (AM) | Non-avoidable mortality | ||||
| Overall AM | AM from preventable causes | AM from treatable causes | |||
| Dependency | |||||
| Q1 (lowest) | 188,268 (10.8%) | 69,290 (15.0%) | 44,735 (15.2%) | 24,555 (14.6%) | 34,055 (14.9%) |
| Q2 | 249,876 (14.4%) | 79,796 (17.2%) | 50,896 (17.3%) | 28,900 (17.2%) | 39,786 (17.4%) |
| Q3 | 307,749 (17.7%) | 90,404 (19.5%) | 57,708 (19.6%) | 32,696 (19.4%) | 44,837 (19.6%) |
| Q4 | 371,525 (21.4%) | 98,700 (21.3%) | 62,798 (21.3%) | 35,902 (21.3%) | 48,695 (21.3%) |
| Q5 (highest) | 622,740 (35.8%) | 124,825 (27.0%) | 78,662 (26.7%) | 46,163 (27.4%) | 61,065 (26.7%) |
| Q5 - Q1 difference | 434,472 (25.0%) | 55,535 (12.0%) | 33,927 (11.5%) | 21,608 (12.8%) | 27,010 (11.8%) |
| Ethnic Concentration | |||||
| Q1 (lowest) | 434,680 (25.0%) | 107,053 (23.1%) | 68,315 (23.2%) | 38,738 (23.0%) | 52,874 (23.1%) |
| Q2 | 378,034 (21.7%) | 99,064 (21.4%) | 63,345 (21.5%) | 35,719 (21.2%) | 48,981 (21.4%) |
| Q3 | 336,768 (19.4%) | 88,081 (19.0%) | 56,468 (19.2%) | 31,613 (18.8%) | 43,751 19.2%) |
| Q4 | 304,237 (17.5%) | 83,087 (17.9%) | 52,888 (17.9%) | 30,199 (18.0%) | 41,026 (18.0%) |
| Q5 (highest) | 286,439 (16.5%) | 85,730 (18.5%) | 53,783 (18.2%) | 31,947 (19.0%) | 41,806 (18.3%) |
| Q5 - Q1 difference | –148,241 (–8.5%) | –21,323 (–4.6%) | –14,532 (–4.9%) | –6791 (–4.0%) | –11,068 (–4.8%) |
| Material Deprivation | |||||
| Q1 (lowest) | 286,314 (16.5%) | 66,375 (14.3%) | 41,391 (14.0%) | 24,984 (14.9%) | 37,569 (16.4%) |
| Q2 | 314,989 (18.1%) | 78,558 (17.0%) | 49,298 (16.7%) | 29,260 (17.4%) | 41,924 (18.4%) |
| Q3 | 346,717 (19.9%) | 90,987 (19.7%) | 57,512 (19.5%) | 33,475 (19.9%) | 45,346 (19.9%) |
| Q4 | 378,817 (21.8%) | 102,760 (22.2%) | 65,722 (22.3%) | 37,038 (22.0%) | 48,869(21.4%) |
| Q5 (highest) | 413,321 (23.8%) | 124,335 (26.9%) | 80,876 (27.4%) | 43,459 (25.8%) | 54,730 (24.0%) |
| Q5 - Q1 difference | 127,007 (7.3%) | 57,960 (12.5%) | 39,485 (13.4%) | 18,475 (11.0%) | 17,161 (7.5%) |
| Residential Instability | |||||
| Q1 (lowest) | 181,822 (10.4%) | 56,402 (12.2%) | 34,861 (11.8%) | 21,541 (12.8%) | 30,965 (13.6%) |
| Q2 | 278,505 (16.0%) | 81,037 (17.5%) | 50,962 (17.3%) | 30,075 (17.9%) | 42,713 (18.7%) |
| Q3 | 341,471 (19.6%) | 91,530 (19.8%) | 57,854 (19.6%) | 33,676 (20.0%) | 46,372 (20.3%) |
| Q4 | 406,869 (23.4%) | 104,712 (22.6%) | 67,164 (22.8%) | 37,548 (22.3%) | 50,335 (22.0%) |
| Q5 (highest) | 531,491 (30.5%) | 129,334 (27.9%) | 83,958 (28.5%) | 45,376 (27.0%) | 58,053 (25.4%) |
| Q5 - Q1 difference | 181,822 (10.4%) | 72,932 (15.8%) | 49,097 (16.7%) | 23,835 (14.2%) | 27,088 (11.9%) |
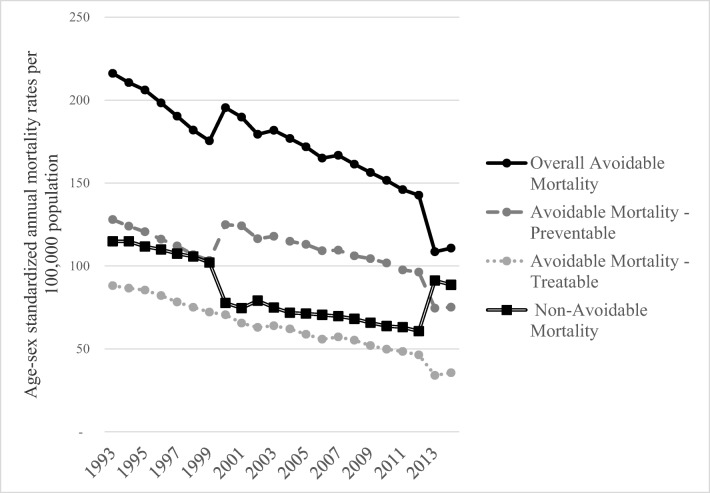
Figure 3 presents annual age–sex-standardized mortality rates per 100,000 population between 1993 and 2014 by overall AM, preventable AM, treatable AM, and non-AM. Overall AM rates were almost halved (48.6%) from 1993 to 2014 (216 vs. 111 per 100,000 population). Compared with treatable AM, preventable AM contributed the greater proportion of all avoidable deaths, increasing from a ratio of approximately 1.5:1 in 1993 (128 vs. 75 deaths per 100,000 population) to approximately 2:1 in 2014 (88 vs. 36 deaths per 100,000 population). Appendices 3 and 4 include sensitivity analyses with time dummy variables showing a significant reduction in AM over time and the persistence of an association between marginalization and AM over time. In comparison, the adjusted odds ratios between the models without time dummy variables and those with time dummy variables were similar.
Fig. 3.
Age-sex standardized annual mortality rates per 100,000 population, 1993-2014
Table 3 shows the ORs and 95% CI of AM compared with those of non-AM among decedents with premature mortality living in each of the ON-Marg Index dimension quintiles (reference Q1), after adjustment for age, sex, urban vs. rural location, and level of comorbidity. Each dimension was statistically significantly associated with AM. Decedents living in the most (Q5) materially deprived (OR, 1.24; 95% CI, 1.22–1.27) and residentially unstable neighbourhoods (OR, 1.13; 95% CI, 1.11–1.15) had significantly greater AM than those living in the least marginalized neighbourhoods (Q1). Decedents living in the most (Q5) dependent (OR, 0.91; 95% CI, 0.89–0.93) and ethnically concentrated neighbourhoods (OR, 0.93; 95% CI, 0.91–0.94) had significantly lower AM than those living in the Q1 reference category. In our sensitivity analysis excluding data from 2013 and 2014, we found no statistically significant differences compared with the main model, thus did not exclude these years from this logistic regression analysis (data not shown).
Table 3.
Logistic regression analysis of avoidable mortality (vs. non-avoidable mortality)
| Crude Odds Ratio (95% Confidence Interval) |
P value | Adjusted Odds Ratio (95% Confidence Interval) | P value | ||
|---|---|---|---|---|---|
| Age | 0-17 | 1.00 | – | 1.00 | – |
| 18-44 | 1.86 (1.78 – 1.94) | <0.001 | 1.81 (1.73 – 1.90) | <0.01 | |
| 45-54 | 2.46 (2.36 – 2.58) | <0.001 | 2.39 (2.29 – 2.50) | <0.01 | |
| 55-64 | 2.46 (2.36 – 2.57) | <0.001 | 2.34 (2.24 – 2.45) | <0.01 | |
| 65-74 | 2.36 (2.26 – 2.46) | <0.001 | 2.20 (2.11 – 2.30) | <0.01 | |
| Sex | Female | 1.00 | – | 1.00 | – |
| Male | 1.11 (1.10 – 1.13) | <0.001 | 1.12 (1.11 – 1.13) | <0.01 | |
| Urban vs. Rural | Urban | 1.00 | – | 1.00 | – |
| Rural | 1.00 (0.99 – 1.01) | 0.93 | 1.00 (0.99 – 1.02) | 0.7048 | |
|
Level of Comorbidities |
0-3 | 1.00 | – | 1.00 | – |
| 4-5 | 1.07 (1.06 – 1.08) | <0.001 | 1.03 (1.02 – 1.05) | 0.07 | |
| 6 | 1.22 (1.19 – 1.24) | <0.001 | 1.17 (1.15 – 1.20) | <0.001 | |
| ≥7 | 1.39 (1.36 – 1.42) | <0.001 | 1.34 (1.31 – 1.36) | <0.001 | |
| Dependency | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 0.99 (0.97 – 1.00) | 0.11 | 0.97 (0.96 – 0.99) | 0.00 | |
| Q3 | 0.99 (0.97 – 1.01) | 0.30 | 0.96 (0.94 – 0.97) | <0.001 | |
| Q4 | 1.00 (0.98 – 1.01) | 0.66 | 0.94 (0.92 – 0.96) | <0.001 | |
| Q5 (high) | 1.01 (0.99 – 1.02) | 0.57 | 0.91 (0.89 – 0.93) | <0.001 | |
| Ethnic Concentration | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.00 (0.98 – 1.01) | 0.89 | 0.99 (0.97 – 1.00) | 0.09 | |
| Q3 | 0.99 (0.98 – 1.01) | 0.47 | 0.97 (0.95 – 0.98) | <0.001 | |
| Q4 | 1.00 (0.99 – 1.02) | 0.97 | 0.95 (0.93 – 0.97) | <0.001 | |
| Q5 (high) | 1.01 (1.00 – 1.03) | 0.11 | 0.93 (0.91 – 0.94) | <0.001 | |
| Material Deprivation | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.06 (1.04 – 1.08) | <0.001 | 1.06 (1.04 – 1.08) | <0.001 | |
| Q3 | 1.14 (1.12 – 1.16) | <0.001 | 1.13 (1.11 – 1.14) | <0.001 | |
| Q4 | 1.19 (1.17 – 1.21) | <0.001 | 1.17 (1.15 – 1.19) | <0.001 | |
| Q5 (high) | 1.29 (1.27 – 1.31) | <0.001 | 1.24 (1.22 – 1.27) | <0.001 | |
| Residential Instability | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.04 ( 1.02 – 1.06) | <0.001 | 1.02 (1.100 – 1.04) | 0.07 | |
| Q3 | 1.08 (1.07 – 1.10) | <0.001 | 1.04 (1.02 – 1.06) | <0.001 | |
| Q4 | 1.14 (1.12 – 1.16) | <0.001 | 1.06 (1.04 – 1.08) | <0.001 | |
| Q5 (high) | 1.22 (1.20 – 1.24) | <0.001 | 1.13 (1.11 – 1.15) | <0.001 |
Table 4 shows the ORs and 95% CI of AM from preventable causes compared with those from treatable causes for each ON-Marg Index dimension quintile among all decedents with AM, after adjustment for age, sex, urban vs. rural location, and level of comorbidity. Decedents living in the most (Q5) materially deprived (OR, 1.10; 95% CI, 1.08–1.12) and residentially unstable neighbourhoods (OR, 1.17; 95% CI, 1.15–1.20) had significantly greater AM from preventable causes compared with that from treatable causes than those living in the least (Q1) marginalized neighbourhoods. Decedents living in the most (Q5) dependent (OR, 0.90; 95% CI, 0.88–0.92) and ethnically concentrated neighbourhoods (OR, 0.87; 95% CI, 0.85–0.89) had significantly lower AM from preventable causes compared with that from treatable causes than those living in the Q1 reference category. In our sensitivity analysis excluding data from 2013 and 2014, we again found no statistically significant differences compared to the main model, thus did not exclude these years from this logistic regression analysis (data not shown).
Table 4.
Logistic regression analysis of avoidable mortality from preventable causes (versus AM from treatable causes)
| Crude Odds Ratio (95% Confidence Interval) |
P value | Adjusted Odds Ratio (95% Confidence Interval) | P value | ||
|---|---|---|---|---|---|
| Age | 0-17 | 1.00 | – | 1.00 | – |
| 18-44 | 1.53 (1.43 – 1.64) | <0.001 | 1.49 (1.39 – 1.59) | <0.001 | |
| 45-54 | 1.06 (0.99 – 1.13) | 0.08 | 1.05 (0.98 – 1.12) | 0.14 | |
| 55-64 | 1.00 (0.94 – 1.07) | 0.91 | 1.00 (0.94 – 1.07) | 0.96 | |
| 65-74 | 0.95 (0.89 – 1.02) | 0.13 | 0.98 (0.91 – 1.04) | 0.46 | |
| Sex | Female | 1.00 | – | 1.00 | – |
| Male | 1.73 (1.71 – 1.75) | <0.001 | 1.72 (1.69 – 1.74) | <0.001 | |
| Urban vs. Rural | Urban | 1.00 | – | 1.00 | – |
| Rural | 1.05 ( 1.03 – 1.07) | <0.001 | 1.05 (1.03 – 1.06) | <0.001 | |
|
Level of Comorbidities |
0 - 3 | 1.00 | – | 1.00 | – |
| 4-5 | 0.94 (0.93 – 0.96) | <0.001 | 1.01 (1.00 – 1.03) | 0.12 | |
| 6 | 0.85 (0.83 – 0.87) | <0.001 | 0.92 (0.90 – 0.94) | <0.001 | |
| ≥7 | 0.76 (0.75 – 0.78) | <0.001 | 0.83 (0.82 – 0.85) | <0.001 | |
| Dependency | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 0.97 (0.95 – 0.99) | 0.00 | 0.97 (0.95 – 0.99) | 0.01 | |
| Q3 | 0.97 (0.95 – 0.99) | 0.00 | 0.96 (0.94 – 0.98) | <0.001 | |
| Q4 | 0.96 (0.94 – 0.98) | <0.001 | 0.94 (0.92 – 0.96) | <0.001 | |
| Q5 (high) | 0.94 (0.92 – 0.95) | <0.001 | 0.90 (0.88 – 0.92) | <0.001 | |
| Ethnic Concentration | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.01 (0.99 – 1.02) | 0.54 | 0.99 (0.97 – 1.01) | 0.21 | |
| Q3 | 1.01 (0.99 – 1.03) | 0.18 | 0.98 (0.96 – 1.00) | 0.03 | |
| Q4 | 0.99 (0.98 – 1.01) | 0.47 | 0.94 (0.92 – 0.96) | <0.001 | |
| Q5 (high) | 0.95 (0.94 – 0.97) | <0.001 | 0.87 (0.85 – 0.89) | <0.001 | |
| Material Deprivation | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.02 (1.00 – 1.04) | 0.12 | 1.01 (0.99 – 1.04) | 0.23 | |
| Q3 | 1.04 (1.02 – 1.06) | 0.00 | 1.03 (1.01 – 1.05) | 0.01 | |
| Q4 | 1.07 (1.05 – 1.09) | <0.001 | 1.05 (1.03 – 1.08) | <0.001 | |
| Q5 (high) | 1.12 (1.10 – 1.15) | <0.001 | 1.10 (1.08 – 1.12) | <0.001 | |
| Residential Instability | Q1 (low) | 1.00 | – | 1.00 | – |
| Q2 | 1.05 (1.02 – 1.07) | <0.001 | 1.05 (1.02 – 1.07) | 0.00 | |
| Q3 | 1.06 (1.04 – 1.09) | <0.001 | 1.07 (1.04 – 1.09) | <0.001 | |
| Q4 | 1.11 (1.08 – 1.13) | <0.001 | 1.11 (1.08 – 1.13) | <0.001 | |
| Q5 (high) | 1.14 (1.12 – 1.17) | <0.001 | 1.17 (1.15 – 1.20) | <0.001 |
Discussion
In this study, we used four dimensions of neighbourhood marginalization to examine their relationship with AM overall and by preventable and treatable causes of death. Among all premature deaths (under the age of 75 years) occurring in Ontario between 1993 and 2014, we found that decedents from neighbourhoods with greater material deprivation and residential instability had greater AM while decedents from neighbourhoods with greater dependency and ethnic concentration had lower AM. We further found that among AM, those living in neighbourhoods with greater material deprivation and residential instability were more likely to die from preventable causes, whereas those living in areas of greater dependency and ethnic concentration were more likely to have died from treatable causes. These findings provide insight into the specific drivers of previously identified differences in AM from both preventable and treatable causes. As such, our findings can contribute to future research into public health and medical interventions to reduce health inequities and improve AM outcomes at the neighbourhood level.
Of the four ON-Marg Index dimensions, material deprivation had the greatest association with AM, in particular for deaths due to preventable causes, identifying a key marginalization target area for future public health and policy interventions. There were 57,960 more avoidable deaths in the most materially deprived neighbourhoods compared with those in the least materially deprived neighbourhoods. Previous research has found an association between increasing material deprivation and higher AM from specific preventable causes, such as infectious and parasitic diseases, diabetes, and ischemic heart disease (Benach et al. 2003; Saint-Jacques et al. 2014; Santana et al. 2015). Previous research has also identified an association between certain material deprivation constructs and AM, such as lower income quintiles having higher AM (Khan et al. 2017). This is the first study, however, to use a summary measure of neighbourhood poverty to examine its association with all causes of AM. Material deprivation not only incorporates income and education but also captures neighbourhood vulnerability through factors such as the proportions of single-parent families, those requiring government transfer payments, the unemployed, and those living in poor housing conditions (Matheson and van Ingen 2006). Further exploration of these constructs and their association with avoidable health outcomes may delineate future targets for public health and policy interventions (Farmanara et al. 2018; Gilbert et al. 2017; Muldoon et al. 2013).
Residential instability was positively associated with AM, largely due to preventable causes. In total, there were 72,932 more avoidable deaths in the most residentially unstable neighbourhoods compared with those in the least unstable neighbourhoods. This dimension encompasses factors of neighbourhood quality and social support, including the proportions of those living alone, moving frequently, and home overcrowding (Matheson and van Ingen 2006). Studies have identified positive health outcomes for those with housing stability; for example, as homeless individuals became stably housed, there was a decreased use of emergency department services and subsequent hospitalizations (Kerman et al. 2018; Lim et al. 2018). Few studies, however, have connected the residential instability dimension with specific avoidable health outcomes, such as ischemic heart disease, homicides, and high alcohol consumption (Chaix et al. 2007; Lachaud et al. 2017; Matheson et al. 2014). In order to inform future public health efforts to reduce inequities in avoidable health outcomes, emerging research is exploring the constructs of residential instability in more detail. For example, neighbourhoods with strong social supports may lead to improved AM outcomes, such as survival from acute myocardial infarction (Chaix et al. 2008).
Neighbourhoods with a greater concentration of visible minorities and immigrants offered a modest protective effect against AM. We noted 21,323 fewer avoidable deaths in the most ethnically diverse neighbourhoods compared with those in the least ethnically diverse neighbourhood.
Visible minorities in Canada are more likely to access general practitioner services, the cornerstone for provision of preventive care, which may contribute to less avoidable deaths in these populations (Hutchison et al. 2011; Quan et al. 2006). In addition, the healthy immigrant phenomenon, where new immigrants to Canada tend to be healthier than the average Canadian population, is likely contributory to our results (Ali et al. 2004; McDonald and Kennedy 2004). For example, immigrants have lower rates of ischemic heart disease, smoking-related diseases, and cancers which represent the greatest proportion of avoidable deaths from preventable causes (James et al. 2006; Omariba 2015). We also found that a greater proportion of the avoidable deaths that do occur in more ethnically diverse neighbourhoods are from treatable causes of death than from preventable causes. This finding may be explained by higher rates of certain treatable causes of death in immigrant populations, such as tuberculosis and malaria (Pottie et al. 2011). Further, visible minorities are less likely to access tertiary care services in hospital compared with other Canadians and may therefore have less access to medical interventions prior to a treatable cause of death (Quan et al. 2006). In our study, ethnic concentration was not an indicator of marginalization for avoidable health outcomes. One reason for this may be its simplicity in only measuring the proportions of immigrants and visible minorities in a neighbourhood. Future studies examining avoidable health outcomes may consider the use of other constructs of diversity, such as ethnic origin, country of origin, or community cohesion (O’Campo et al. 2015).
Dependency is a measure of a neighbourhood’s workforce eligibility to support those who do not have income from employment, namely children, seniors, and the unemployed (Matheson and van Ingen 2006). In our crude analysis, we noted 55,535 more avoidable deaths in the most dependent neighbourhoods compared with those in the least dependent neighbourhoods. In our regression analysis, however, we found that neighbourhoods with greater dependency were associated with lower AM. Our findings were not expected given previous research examining certain constructs of dependency. For example, higher unemployment has been shown to be associated with higher mortality (Clemens et al. 2015). The most likely explanation of our findings is the use of the summary measure of dependency where it is assumed that all of its constructs have the same direction of effect. This assumption may have been problematic given the dependency constructs are based on age (proportion of the population aged 65 and older, dependency ratio, and proportion of the population not participating in the labour force aged 15 and over) as was our main mortality outcome of interest (AM only considers deaths under the age of 75). Previous research has identified different mortality patterns in those aged 14 years and younger compared with those 65 years and older (Shumanty 2018). As such, our results may not reflect a true protective association between dependency and AM. Future studies using age-based health outcomes may consider first examining each dependency construct individually to determine the direction of effect before using a summary dimension measure.
Our study used robust, population-level databases that captured all deaths in a population with universal coverage for medically necessary health services. We used standardized definitions of AM developed through a rigorous process by CIHI. This is the first study to measure several dimensions of marginalization and their association with AM. As with any study using administrative data, however, important limitations remain. First, as the ON-Marg Index is based on 2001 and 2006 census data, it is possible that its accuracy is greater proximal to these years than at the extremes of our study period (Matheson and van Ingen 2006; Matheson et al. 2012). Second, we used the ON-Marg Index to assign decedents a summary level of neighbourhood marginalization that, while validated, may not always reflect individual level marginalization. Third, we excluded individuals with no ON-Marg Index, reasons for which include having a new postal code that was not available in the years for which the index was created (prior to 2006). This would exclude individuals who lived in new housing developments in Ontario from 2006 to 2014 which may reflect a more affluent cohort leading to a possible over-estimation of marginalization in our study. Fourth, classifications of cause of death varied during 2013 and 2014; however, our sensitivity analyses assured us these changes did not significantly impact our overall findings. Fifth, this study uses four dimensions of marginalization without the ability to stratify into each of their constructs in order to quantify their association with AM, identifying an important area for future research. In addition, AM encompasses a comprehensive list of preventable and treatable causes of death, and future studies may focus on the relationship between marginalization and specific avoidable conditions in order to provide targeted and actionable interventions. Finally, with the understanding that marginalization is not experienced in isolation, future research could consider how marginalization dimensions intersect to affect health outcomes (Durbin et al. 2015).
Conclusion
Neighbourhoods with high material deprivation and residential instability have higher AM while more ethnically dense neighbourhoods have lower AM. Age-based marginalization dimensions such as dependency might not be suitable to examine age-based health outcomes such as AM.
Our results suggest that neighbourhoods with high material deprivation and residential instability may be of most interest to public health practitioners and researchers given their association with preventable AM. In order to provide targeted public health and policy interventions, future research should examine which constructs of material deprivation and residential instability are most greatly associated with avoidable health outcomes, and may consider stratification by specific preventable conditions.
Electronic supplementary material
(DOCX 33 kb)
Funding information
This study is financially supported by the Bruyère Research Institute through the Big Data Research Program. This study was also supported by the Institute for Clinical Evaluative Sciences, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC).
Compliance with ethical standards
Competing interest
The authors declare that they have no conflict of interest.
Ethics approval
ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects conducted under section 45, by definition, do not require review by a Research Ethics Board. This project was conducted under section 45, and approved by ICES’ Privacy and Compliance Office.
Data
Parts of this material are based on data and/or information compiled and provided by Canadian Institute for Health Information (CIHI). Parts of this report are based on Ontario Registrar General (ORG) information on deaths, the original source of which is Service Ontario. We attest that we have obtained appropriate permissions and paid any required fees for use of copyright protected materials.
Data sharing
The data set from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors upon request, understanding that the programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Disclaimer
The funder of the study had no role in the study design; data collection, analysis, or interpretation; or writing of the report. The opinions, results, and conclusions reported in this paper are those of the authors and are independent and do not necessarily reflect those of the funding sources, CIHI, and ORG or Ministry of Government Services. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ali JS, McDermott S, Gravel RG. Recent research on immigrant health from Statistics Canada’s population surveys. Canadian Journal of Public Health. 2004;95(3):I9–I13. doi: 10.1007/BF03403659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benach J, Yasui Y, Borrell C, Pasarin MI, Martinez JM, Daponte A. The public health burden of material deprivation: excess mortality in leading causes of death in spain. Preventive Medicine. 2003;36(3):300–308. doi: 10.1016/s0091-7435(02)00014-2. [DOI] [PubMed] [Google Scholar]
- Buick JE, Ray JG, Kiss A, Morrison LJ. The association between neighborhood effects and out-of-hospital cardiac arrest outcomes. Resuscitation. 2016;103:14–19. doi: 10.1016/j.resuscitation.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. (2012). Health Indicators. https://secure.cihi.ca/free_products/health_indicators_2012_en.pdf
- Chaix B, Rosvall M, Merlo J. Neighborhood socioeconomic deprivation and residential instability: effects on incidence of ischemic heart disease and survival after myocardial infarction. Epidemiology. 2007;18(1):104–111. doi: 10.1097/01.ede.0000249573.22856.9a. [DOI] [PubMed] [Google Scholar]
- Chaix B, Lindstrom M, Rosvall M, Merlo J. Neighbourhood social interactions and risk of acute myocardial infarction. Journal of Epidemiology and Community Health. 2008;62(1):62–68. doi: 10.1136/jech.2006.056960. [DOI] [PubMed] [Google Scholar]
- Clemens T, Popham F, Boyle P. What is the effect of unemployment on all-cause mortality? A cohort study using propensity score matching. European Journal of Public Health. 2015;25(1):115–121. doi: 10.1093/eurpub/cku136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. World Health Organization http://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=FF6A6FCFEC2F60C251C7C3B674535A72?sequence=1. [DOI] [PubMed]
- du Plessis, V., Beshiri, R., Bollman, R.D., & Clemenson, H. (2001). Definitions of rural, rural and small town Canada analysis bulletin Vol. 3, No. 3. Statistics Canada, Catalogue. no. 21-006-XIE.
- Durbin A, Moineddin R, Lin E, Steele LS, Glazier RH. Examining the relationship between neighbourhood deprivation and mental health service use of immigrants in Ontario, Canada: a cross-sectional study. BMJ Open. 2015;5(3):e006690-2014-006690. doi: 10.1136/bmjopen-2014-006690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmanara N, Sherrard L, Dube E, Gilbert NL. Determinants of non-vaccination against seasonal influenza in Canadian adults: findings from the 2015-2016 influenza immunization coverage survey. Canadian Journal of Public Health. 2018;109(3):369–378. doi: 10.17269/s41997-018-0018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert NL, Gilmour H, Wilson SE, Cantin L. Determinants of non-vaccination and incomplete vaccination in Canadian toddlers. Human Vaccines & Immunotherapeutics. 2017;13(6):1–7. doi: 10.1080/21645515.2016.1277847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruneir A, Bronskill SE, Maxwell CJ, Bai YQ, Kone AJ, Thavorn K, et al. The association between multimorbidity and hospitalization is modified by individual demographics and physician continuity of care: a retrospective cohort study. BMC Health Services Research. 2016;16:154. doi: 10.1186/s12913-016-1415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankivsky O, Christoffersen A. Intersectionality and the determinants of health: a Canadian perspective. Critical Public Health. 2008;18:271–283. [Google Scholar]
- Hutchison B, Levesque JF, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. The Milbank Quarterly. 2011;89(2):256–288. doi: 10.1111/j.1468-0009.2011.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inman M, Daneman D, Curtis J, Sochett E, Clarke A, Dunger DB, et al. Social determinants of health are associated with modifiable risk factors for cardiovascular disease and vascular function in pediatric type 1 diabetes. The Journal of Pediatrics. 2016;177:167–172. doi: 10.1016/j.jpeds.2016.06.049. [DOI] [PubMed] [Google Scholar]
- James PD, Manuel DG, Mao Y. Avoidable mortality across Canada from 1975 to 1999. BMC Public Health. 2006;6:137. doi: 10.1186/1471-2458-6-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James PD, Wilkins R, Detsky AS, Tugwell P, Manuel DG. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. Journal of Epidemiology and Community Health. 2007;61(4):287–296. doi: 10.1136/jech.2006.047092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerman N, Sylvestre J, Aubry T, Distasio J. The effects of housing stability on service use among homeless adults with mental illness in a randomized controlled trial of housing first. BMC Health Services Research. 2018;20; 18(1):190. doi: 10.1186/s12913-018-3028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan AM, Urquia M, Kornas K, Henry D, Cheng SY, Bornbaum C, Rosella LC. Socioeconomic gradients in all-cause, premature and avoidable mortality among immigrants and long-term residents using linked death records in Ontario, Canada. Journal of Epidemiology and Community Health. 2017;71(7):625–632. doi: 10.1136/jech-2016-208525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachaud J, Donnelly PD, Henry D, Kornas K, Calzavara A, Bornbaum C, Rosella L. A population-based study of homicide deaths in Ontario, Canada using linked death records. International Journal for Equity in Health. 2017;16(1):133-017-0632-9. doi: 10.1186/s12939-017-0632-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane NE, Maxwell CJ, Gruneir A, Bronskill SE, Wodchis WP. Absence of a socioeconomic gradient in older adults’ survival with multiple chronic conditions. Ebiomedicine. 2015;2(12):2094–2100. doi: 10.1016/j.ebiom.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S, Singh TP, Hall G, Walters S, Gould LH. Impact of a New York City Supportive Housing Program on Housing Stability and Preventable Health Care among Homeless Families. Health Services Research. 2018;53(5):3437–3454. doi: 10.1111/1475-6773.12849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson, F., & van Ingen, T. (2006). Ontario Marginalization Index: User guide Versuib, 1 http://www.torontohealthprofiles.ca/ont/onmarg/userguide_data/ON-Marg_user_guide_1.0_FINAL_MAY2012.pdf.
- Matheson FI, Dunn JR, Smith KL, Moineddin R, Glazier RH. Development of the Canadian Marginalization Index: a new tool for the study of inequality. Canadian Journal of Public Health. 2012;103(8 Suppl 2):S12–S16. doi: 10.1007/BF03403823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Creatore MI, Gozdyra P, Park AL, Ray JG. A population-based study of premature mortality in relation to neighbourhood density of alcohol sales and cheque cashing outlets in Toronto, Canada. BMJ Open. 2014;4(12):e006032-2014-006032. doi: 10.1136/bmjopen-2014-006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald JT, Kennedy S. Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Social Science & Medicine. 2004;59(8):1613–1627. doi: 10.1016/j.socscimed.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Mikkonen J, Raphael D. Social determinants of health: the Canadian facts. 2010. [Google Scholar]
- Mondor L, Maxwell CJ, Bronskill SE, Gruneir A, Wodchis WP. The relative impact of chronic conditions and multimorbidity on health-related quality of life in Ontario long-stay home care clients. Quality of Life Research. 2016;25(10):2619–2632. doi: 10.1007/s11136-016-1281-y. [DOI] [PubMed] [Google Scholar]
- Mondor L, Maxwell CJ, Hogan DB, Bronskill SE, Gruneir A, Lane NE, Wodchis WP. Multimorbidity and healthcare utilization among home care clients with dementia in Ontario, Canada: a retrospective analysis of a population-based cohort. PLoS Medicine. 2017;14(3):e1002249. doi: 10.1371/journal.pmed.1002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muldoon KA, Duff PK, Fielden S, Anema A. Food insufficiency is associated with psychiatric morbidity in a nationally representative study of mental illness among food insecure Canadians. Social Psychiatry and Psychiatric Epidemiology. 2013;48(5):795–803. doi: 10.1007/s00127-012-0597-3. [DOI] [PubMed] [Google Scholar]
- Nolte, E, &. McKee, M. (2004). Does health care save lives? Avoidable mortality revisited. The Nuffield Trust, p. 139. http://researchonline.lshtm.ac.uk/id/eprint/15535
- O’Campo P, Wheaton B, Nisenbaum R, Glazier RH, Dunn JR, Chambers C. The neighbourhood effects on health and well-being (NEHW) study. Health & Place. 2015;31:65–74. doi: 10.1016/j.healthplace.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Omariba DW. Immigration, ethnicity, and avoidable mortality in Canada, 1991-2006. Ethnicity & Health. 2015;20(4):409–436. doi: 10.1080/13557858.2014.995155. [DOI] [PubMed] [Google Scholar]
- Park J, Tjepkema M, Goedhuis N, Pennock J. Avoidable mortality among First Nations adults in Canada: A cohort analysis. Health Reports. 2015;26(8):10–16. [PubMed] [Google Scholar]
- Pefoyo AJ, Bronskill SE, Gruneir A, Calzavara A, Thavorn K, Petrosyan Y, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:415. doi: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosyan Y, Bai YQ, Kone Pefoyo AJ, Gruneir A, Thavorn K, Maxwell CJ, et al. The relationship between diabetes care quality and diabetes-related hospitalizations and the modifying role of comorbidity. Canadian Journal of Diabetes. 2017;41(1):17–25. doi: 10.1016/j.jcjd.2016.06.006. [DOI] [PubMed] [Google Scholar]
- Pottie K, Greenaway C, Feightner J, Welch V, Swinkels H, Rashid M, et al. Canadian Collaboration for Immigrant and Refugee Health: evidence-based clinical guidelines for immigrants and refugees. Canadian Medical Association Journal. 2011;183(12):E824–E925. doi: 10.1503/cmaj.090313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan H, Fong A, De Coster C, Wang J, Musto R, Noseworthy TW, Ghali WA. Variation in health services utilization among ethnic populations. Canadian Medical Association Journal. 2006;174(6):787–791. doi: 10.1503/cmaj.050674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint-Jacques N, Dewar R, Cui Y, Parker L, Dummer TJ. Premature mortality due to social and material deprivation in Nova Scotia, Canada. International Journal for Equity in Health. 2014;13(1):94. doi: 10.1186/s12939-014-0094-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santana P, Costa C, Mari-Dell’Olmo M, Gotsens M, Borrell C. Mortality, material deprivation and urbanization: exploring the social patterns of a metropolitan area. International Journal for Equity in Health. 2015;14:55. doi: 10.1186/s12939-015-0182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumanty, R. (2018). Report on the demographic situation in Canada - mortality: overview, 2014 to 2016. Statistics Canada — Catalogue no. 91-209-X, 1–12.
- Silverman JD, Hutchison MG, Cusimano MD. Association between neighbourhood marginalization and pedestrian and cyclist collisions in Toronto intersections. Canadian Journal of Public Health. 2013;104(5):e405–e409. doi: 10.17269/cjph.104.4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundmacher L. Trends and levels of avoidable mortality among districts: “healthy” benchmarking in Germany. Health Policy. 2013;109(3):281–289. doi: 10.1016/j.healthpol.2012.07.003. [DOI] [PubMed] [Google Scholar]
- Thavorn K, Maxwell CJ, Gruneir A, Bronskill SE, Bai Y, Pefoyo K, et al. Effect of socio-demographic factors on the association between multimorbidity and healthcare costs: A population-based, retrospective cohort study. BMJ Open. 2017;7(10):e017264-2017-017264. doi: 10.1136/bmjopen-2017-017264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 33 kb)