Abstract
The diagnosis of rare genetic diseases is one of the most difficult areas in medicine. Whole-exome sequencing (WES) technology makes it easier to diagnose these diseases. In addition, next-generation phenotyping can help to diagnose computer-based algorithms. Detailed dysmorphologic findings of 25 patients diagnosed by WES in our center were described. The success of this technology in diagnosing rare genetic diseases was investigated by scanning the photographs of 25 patients with Face2Gene application. The application listed possible preliminary diagnoses (30 disease suggestion). Of these, 12 (48%) cases were correctly matched. The most common disease group in the patients was neurological disease (96%). The most common mode of inheritance in the patients was autosomal recessive. The rate of consanguineous marriages was determined in 80% of the patients. Ten patients had microcephaly and 7 patients had corpus callosum anomaly. In our study, we found that the success of Face2Gene was lower than described in the literature. We think that the probable cause of this condition is that the cases are very rare, and there is not enough data about these diseases in the application. Therefore, it is recommended that applications should be used more frequently by pediatricians and clinical geneticists. The diagnosis of rare diseases still is quite difficult. Nowadays, WES is a successful method. However, applications such as Face2Gene help to make a clinical prediagnosis and create a larger database.
Keywords: Artificial intelligence, Deep learning, Whole-exome sequencing
Diseases with genetic etiology affect most of the population during their lifetimes. Syndromic cases have symptoms that significantly reduce the quality of life of patients, and they affect about 8% of the population [Baird et al., 1988]. Genetic diagnosis is important in syndromic cases because, following a diagnosis, there are special prevention and screening programs available for primary and secondary symptoms.
Many of these syndromic cases have facial phenotypes and some characteristic facial features that provide a clue for the diagnosis of genetic diseases. Approximately 30-40% of the genetic diseases show craniofacial alteration (as in Down syndrome, Fragile X, etc.) [Ferry et al., 2014].
Dysmorphology provides identification of before- or after-birth nonnormative forms that enables classification of various congenital malformations. This term provides a comparable description of all body characteristics (stature, feet, hands, neck) and face (such as shape of head, nose length, position of ears, thickness of vermillion, etc.) of the individuals of the same age group and ethnicity. A genetic etiology should be suspected if a child has a dysmorphic appearance with one of these features: (a) congenital anomalies, (b) growth retardation, (c) developmental delay and intellectual disability or developmental regression, (d) undeveloped secondary sexual characteristics, or (e) ambiguous genitalia [Featherstone et al., 2005; Smigiel and Demkow, 2016].
In the last 3 decades, with the advancement of technology, various databases have been created to determine the dysmorphic facial findings of patients (London Dysmorphology Database, Pictures Of Standard Syndromes and Undiagnosed Malformations Database, etc.) [Guest et al., 1999; Strømme, 1999]. These databases allow the comparison between the facial gestalt of patients and normal facial features, but these findings are affected by external factors such as available lighting conditions, posture of patients, etc. [Hammond, 2007]. In recent years, DeepGestalt program has been developed using computer technology and deep learning algorithms that measure similarities to hundreds of genetic syndromes based on unconstrained 2D images [Gurovich et al., 2018]. In a previous study, DeepGestalt achieved 91% top-10 correctness in identifying the syndrome on 502 different patient photos [Gurovich et al., 2019]. The Face2Gene (FDNA Inc, Boston, USA) application is a novel framework based on DeepGestalt, and it is one of the next-generation phenotyping (NGP) technologies used to determine the phenotype in thousands of diseases and correlate this phenotype with the genotype. In addition to DeepGestalt, which is an analysis based on a frontal facial photo of the patient, Face2Gene also offers an analysis based on the clinical findings of the patient (feature match). In this study, we considered both types of analysis and included them.
With the development of technology, other methods have been developed for the diagnosis of genetic diseases using molecular genetic tests. One of these methods is whole-exome sequencing (WES). This technique allows sequencing of the whole protein-coding region of genes in a genome (known as the exome) [Ng et al., 2009]. Exomes are about 2% of the whole genome, and mutations in these regions cause approximately 80% of mendelian diseases [Botstein and Risch, 2003; Yang et al., 2014]. In previous meta-analysis studies, the reported success rate of WES for molecular diagnosis was 24-68% (approximately 31%) [Clark et al., 2018]. This method has become a good alternative for the molecular diagnosis of rare genetic diseases that have prevalence below 1/2,000 [Ng et al., 2010].
Dysmorphic facial features are important to determine the causative variants of rare genetic diseases in WES. Therefore, when determining that pathogenic variants are causative of a disease or not, phenotypic features of patients are compared with similar previously reported cases using WES. For this reason, any type of clue (face gestalt, any prenatal findings, biochemical results, etc.) is increasingly important. In this study, we aimed to investigate the importance of determining dysmorphic facial features in rare genetic diseases with definitive molecular diagnosis using the WES method. We also evaluated the success of NGP technologies in this disease group.
Materials and Methods
The aim of this study was to determine the dysmorphic facial features of rare diseases diagnosed using WES and the power of NGP technology. This is a retrospective study. Therefore, the hospital registry system and patient files were reevaluated. The criteria for inclusion in the study are as follows: (1) patients were admitted to the Department of Medical Genetics at Afyonkarahisar University of Health Sciences between 2012-2019, (2) all patients had had sequencing results, (3) all patients had at least 1 front face image in the their files to evaluate the facial features, and (4) all patients had signed a consent form. Patients without adequate photographs to assess facial features were excluded from the study.
We selected 25 patients (9 females and 16 males) younger than 16 years of age who met all inclusion criteria. The photos and relevant clinical features were uploaded to Face2Gene, and the resulting analysis was assessed and correlated to the molecular diagnosis. We also checked how the correct diagnosis is ranked by both types of analysis, DeepGestalt and feature match. In addition, the research application of Face2Gene was used to understand whether the tool differentiated the group of patients from control groups [Pantel et al., 2018].
We used the hospital registry system to evaluate if the selected patients had anamnesis information, biochemical test results, MR images, echocardiographic results, and genetic reports. The parameters questioned in the anamnesis information were prenatal (oligohydroamnios, polyhydroamniosis, fetal akinesia, any abnormal ultrasound image), natal (delivery type, birth weight, gestation week at birth), postnatal stories (story of neonatal intensive care, hypoxic ischemic birth history, hypotonia, sucking difficulty), pedigree, presence of individuals with similar symptoms in the family, if consanguineous marriage (when yes, which degree), delay in intellectual/motor development stages, surgery history, and seizures.
Human Malformation Terminology (The Elements of Morphology) was used to determine the presence of any dysmorphic finding. This terminology was created by a group of clinicians working in the field of dysmorphology to standardize the definition of human morphology in which a reliable comparison of phenotypic findings among patients is provided [Allanson et al., 2009]. This terminology consists of 6 articles. These are standard terminology for the head and face; the periorbital region; the ear; the nose and philtrum; the lips, mouth, and oral region as well as the hands and feet.
WES analysis of the patients was performed by the contracted institutions or the universities we worked with in this study, and the test results were examined extensively. If the same gene was found to cause 2 or more diseases, differential diagnosis was made by detailed physical examination. Dysmorphic findings had a very important role at this stage. MR images and echocardiography findings were also used.
WES analysis findings of patients, anamnesis information, pedigree analysis, and clinical findings were collected. Dysmorphic facial features were evaluated in detail. Since dysmorphic facial features are a diagnostic clue to medical genetic doctors, we aimed to present dysmorphic facial findings of patients diagnosed as rare genetic diseases in our clinic. In this study, we evaluated the power of Face2Gene, a new NGP technology that makes recommendations for possible genetic disease using face gestalt information. Therefore, when choosing which test to perform in the diagnosis of rare genetic disease, we also evaluated the necessity of the recommendations of this next-generation approach.
Results
The disease-causing mutations of all patients and their demographics are presented in Table 1. According to the mutation points, physical examination findings, laboratory and imaging tests, results were reevaluated and a definitive diagnosis was determined. Except for 1 patient, all of the diagnosed diseases were of autosomal recessive inheritance. In terms of consanguinity, consanguineous marriages were found in 80% (12 of them were first-degree cousins, 6 of them were second-degree, and 2 of them were third-degree cousins). No consanguinity was defined for parents of the other 5 patients, but they were from the same village (except for the parents of P25).
Table 1.
Positive exome cases with pathogenic variants and secondary findings
| Case ID | Genes | OMIM | Mode of inheritance | Consanguineous marriage | Other affected individuals | Mutations | Zygosity | Genetic diagnosis |
|---|---|---|---|---|---|---|---|---|
| P1 | COL6A2 | 120240 | Autosomal recessive | Same village | No | c.2584C>T (p.Arg862Trp) (p.R862W) | Homozygous | Betdlem myopatdy 1 |
| P2 | COG5 | 613612 | Autosomal recessive | First-degree cousin marriage | 1 male sibling | hg19:chr7:107002545A>G; c.1052T>C; p.Leu351Pro | Homozygous | Congenital disorder of glycosylation, type IIi |
| P3 | SPG11 | 604360 | Autosomal recessive | First-degree cousin marriage | No | hg19:44925739; c.1699C>T; p.Gln567* | Homozygous | Spastic paraplegia 11, autosomal recessive |
| P4 | POMT1 | 607423 | Autosomal recessive | Second-degree cousin marriage | No | c.598G>C (p.Ala200Pro) (p.A200P) | Homozygous | Muscular dystrophydystroglycanopatdy (congenital with mental retardation), type B, 1 |
| P5 | LARP7 | 612026 | Autosomal recessive | First-degree cousin marriage | 1 female sibling (case 6) | NM_015454.1_c.802_1142 + 267del (p.Lys278*/c.832A>T) | Homozygous | Alazami syndrome |
| P6 | LARP7 | 612026 | Autosomal recessive | First-degree cousin marriage | 1 male sibling (case 5) | NM_015454.1_c.802_1142 + 267del (p.Lys278*/c.832A>T) | Homozygous | Alazami syndrome |
| P7 | THOC6 | 615403 | Autosomal recessive | First-degree cousin marriage | 1 male sibling (case 8) | Exon11: c.709delG; p.G237fs; chr16:3077179_AG>A | Homozygous | Beaulieu-Boycott-Innes syndrome |
| P8 | THOC6 | 615403 | Autosomal recessive | First-degree cousin marriage | 1 male sibling (case 7) | Exon11: c.709delG; p.G237fs; chr16:3077179_AG>A | Homozygous | Beaulieu-Boycott-Innes syndrome |
| P9 | NAGLU | 609701 | Autosomal recessive | First-degree cousin marriage | No | c.1694G>A (p.Arg565Gln) (p.R565Q) | Homozygous | Mucopolysaccharidosis type IIIB (Sanfilippo B) |
| P10 | KLHL7 | 611119 | Autosomal recessive | Third-degree cousin marriage | 1 male sibling (case 11) | Exon 8: c.C1051T; p.R351X | Homozygous | Crisponi/CISS1-like phenotype associated with early-onset retinitis pigmentosa |
| P11 | KLHL7 | 611119 | Autosomal recessive | Third-degree cousin marriage | 1 male sibling (case 10) | Exon 8: c.C1051T; p.R351X | Homozygous | Crisponi/CISS1-like phenotype associated with early-onset retinitis pigmentosa |
| P12 | VLDLR | 192977 | Autosomal recessive | Second-degree cousin marriage | 1 male sibling (case 13) | NM_001018056.1:c.1459G>T; p.Asp487Tyr | Homozygous | Cerebellar hypoplasia and mental retardation with or without quadrupedal locomotion 1 |
| P13 | VLDLR | 192977 | Autosomal recessive | Second-degree cousin marriage | 1 male sibling (case 12) | NM_001018056.1:c.1459G>; p.Asp487Tyr/ | Homozygous | Cerebellar hypoplasia and mental retardation with or without quadrupedal locomotion 1 |
| P14 | TBCD | 604649 | Autosomal recessive | Same village | No | c.230A>G (p.His77Arg) (p.H77R) | Homozygous | Encephalopathy, progressive, early-onset, with brain atrophy and thin corpus callosum |
| P15 | COG6 | 606977 | Autosomal recessive | First-degree cousin marriage | 1 female cousin | Exon8: c.G697A; p.Glu233Lys | Homozygous | Congenital disorder of glycosylation, type IIl |
| P16 | COG6 | 606977 | Autosomal recessive | First-degree cousin marriage | 1 female cousin | Exon8: c.G697A; p.Glu233Lys | Homozygous | Congenital disorder of glycosylation, type IIl |
| P17 | LAMA1 | 615960 | Autosomal recessive | Same village | 1 male sibling (case 18) | c.8192C>A (p.S2731*) (p.Ser2731Ter) | Homozygous | Poretti-Boltshauser Syndrome; PTBHS |
| P18 | LAMA1 | 615960 | Autosomal recessive | Same village | 1 male sibling (case 17) | c.8192C>A (p.S2731*) (p.Ser2731Ter) | Homozygous | Poretti-Boltshauser Syndrome; PTBHS |
| P19 | LARP7 | 612026 | Autosomal recessive | Second-degree cousin marriage | 2 male cousins | NM_001267039.1(LARP7):c.441del | Homozygous | Alazami syndrome |
| P20 | TPP1 | 607998 | Autosomal recessive | Second-degree cousin marriage | No | hg19:chr11:6639009T>C; c.230-2A>G;p.? | Homozygous | Ceroid Lipofuscinosis, Neuronal, 2; CLN2 |
| P21 | MASP1 | 600521 | Autosomal recessive | First-degree cousin marriage | No | hg19:chr3:186954244G>A; c.1415C>T; p.Thr472Ile hg19:chr3:186980508C>A; c.238G>T; p.Val80Leu |
Compound heterozygous | 3MC syndrome 1 |
| P22 | GPT2 | 138210 | Autosomal recessive | Second-degree cousin marriage | No | hg19:chr16:46960903G>A; c.1435G>A; p.Val479Met | Homozygous | Intellectual disability, autosomal recessive 49 |
| P23 | OCLN | 602876 | Autosomal recessive | First-degree cousin marriage | 1 male sibling (case 24) | hg19:chr5:68830667G>A; c.1037 + 1G>A | Homozygous | Pseudo-TORCH syndrome 1 |
| P24 | OCLN | 602876 | Autosomal recessive | First-degree cousin marriage | 1 male sibling (case 23) | hg19:chr5:68830667G>A; c.1037 + 1G>A | Homozygous | Pseudo-TORCH syndrome 1 |
| P25 | ACSL4 | 300157 | X-linked dominant | Same village | Mother | hg19:chrX:108926022G>T; c.455C>A; p.Thr152Asn | Hemizygous | Intellectual disability, X-linked 63 |
The symptoms and dysmorphic facial features in our patients are summarized in Table 2. Almost all of the patients were evaluated as neurological diseases (only 1 patient had a storage disorder). All other patients had neuromotor growth retardation and different degrees of learning disability. Ten patients (40%) had microcephaly. Two patients had muscle weakness, and 3 patients had persistent hypotonia. Only 1 patient had inadequacy in cerebellar tests. Twenty-two of the 25 patients had an MRI. When MRI findings were examined, 4 patients had normal findings, and 18 patients had abnormal findings. The most common findings were corpus callosum anomalies (7/18). Other anomalies were periventricular hyperintensity (4/18), dilated ventricles (4/18), and cortical atrophy (3/18), respectively.
Table 2.
Summary of clinical and dysmorphic findings of patients
| Case ID | Presenting symptoms | Dysmorphic facial findings | MRI findings |
|---|---|---|---|
| P1 | Decreased fetal movements at intrauterine period, resistant epilepsy, neuromotor developmental delay, severe learning disability, microcephaly, upper and lower limb muscle weakness, pes equinusvarus, spasticity, contracture lower extremities, increased deep tendon reflexes, proximal muscle atrophy, strabismus | Brachycephaly, flat occiput, square face, narrow forehead, sloping forehead, malar flatting, pointed chin, deeply set eyes, thick eyebrows, almond-shaped palpebral fissure, telecanthus, prominent inferior crus of antihelix, prominent antihelix stem, prominent superior crus of antihelix, underdeveloped crus helix, large lobe, bifid tragus, low insertion of columella, enlarged nares, wide nasal bridge, depressed nasal bridge, wide nasal ridge, midline sinus of philtrum, thin upper lip vermilion, thick lower lip vermilion | Hydrocephalus, thin corpus callosum |
| P2 | Neuromotor developmental delay, mild learning disability, dysmetria and dysdiadochokinesia, seizure, imbalance to especially right side, generalized hypertrichosis, dysmorphic facial features | Square face, broad forehead, premaxillary underdevelopment, broad jaw, full cheeks, broad and horizontal eyebrow, long palpebral fissure, synophrys, telecanthus, long ear, underdeveloped crus helix, underdeveloped tragus, broad columella, wide nasal bridge, broad philtrum, smooth philtrum, prominent nasolabial fold, thick low and upper lip vermilion | Diffuse cerebellar atrophy |
| P3 | Walking disability, moderate learning disability, decrease of muscular power at extremities, bilateral 5th trigger finger, foot spasticity, increase of deep tendon reflex, pes cavus | Hypertelorism, horizontal eyebrow, downslanted palpebral fissure, telecanthus, prominent antitragus, expanded terminal portion of crus helix, macrotia, broad columella, low insetion of columella, enlarged nares, wide nasal bridge, wide nasal ridge, broad nasal tip, thin upper lip vermilion, diastema in anterior incisor teeth | Periventricular hyperintensity |
| P4 | Global developmental delay, severe learning disability, skeletal muscle weakness, increased creatinine level, macroglossia, joint contractures, spinal scoliosis, hypertrichosis | Brachycephaly, flat occiput, triangular face, narrow forehead, prominent cheekbone, prominent nasolabial fold, broad chin, long palpebral fissure, prominent antihelix stem, prominent antitragus, expanded terminal portion of crus helix, wide nasal base, wide nasal bridge, broad nasal tip, deep philtrum, everted lower lip vermilion, thin lower lip vermilion, downturned corners of mouth, wide mouth | Normal |
| P5 | Neuromotor developmental delay, severe learning disability, microcephaly, autistic behaviors, pulmonary stenosis, epiphyseal changes in the proximal phalanges, strabismus, tortuous at retinal blood vessels, hyperkeratosis, diabetes mellitus type 2, short stature, pes planus | Brachycephaly, coarse face, malar prominence, midface prominence, prominent nasolabial fold, broad chin, hypertelorism, deep-set eyes, broad eyebrow, infraorbital crease, angulated antihelix, underdeveloped antihelix crus superior, prominent antitragus, long ear, low-set ears, protruding ears, anterior crease lobes, large lobes, macrotia, broad columella, large nose, wide nasal base, depressed nasal bridge, wide nasal bridge, wide nasal ridge, broad nasal tip, long nose, prominent nose, short philtrum, tented philtrum, wide mouth, macrostomia, large tongue | Arnold Chiari malformation type 1 |
| P6 | Neuromotor developmental delay, severe learning disability, seizure, microcephaly, autistic behaviors, pulmonary stenosis, hyperkeratosis | Brachycephaly, short face, square face, full cheeks, malar prominence, midface prominence, premaxillary prominence, broad chin, short chin, hypertelorism, laterally extended eyebrow, deep-set eyes, infraorbital fold, telecanthus, long ears, protruding ears, large lobe, broad columella, large nose, wide nasal base, depressed nasal bridge, wide nasal bridge, wide nasal ridge, broad nasal tip, long nose, short philtrum, tented philtrum, wide mouth, thick lower lip vermilion, macrostomia | Corpus callosum agenesis, distinct vascular structures, venous angioma |
| P7 | Global developmental delay, severe learning disability, autistic behaviors, microcephaly, early closure of anterior fontanelle, lack of eye contact, criptorchidism, left equinovarus foot deformity | Brachycephaly, long face, underdeveloped supraorbital ridges, underdevelopment cheekbone, malar flattening, underdeveloped nasolabial fold, premaxillary, prominence, narrow jaw, pointed chin, hypertelorism, almond-shaped palpebral fissure, telecanthus, prominent antihelix stem, underdeveloped crus superior antihelix, long ears, small lobe, broad columella, anteverted nares, wide nasal base, prominent nasal bridge, wide nasal bridge, wide nasal ridge, broad nasal tip, bulbouse nose, smooth philtrum, absent Cupid's bow, everted lower lip vermilion, thick lower lip vermilion | Normal |
| P8 | Neuromotor developmental delay, severe learning disability, autistic behaviors, microcephaly, seizure, lack of eye contact, criptorchidism | Brachycephaly, flat occiput, full checks, premaxillary prominence, pointed chin, hypertelorism, almond-shaped palpebral fissure, upslanted palpebral fissure, telecanthus, prominent antihelix stem, prominent antihelix inferior crus, prominent antihelix superior crus, angulated antihelix, everted antitragus, protruding ear, crus helix connected to antihelix, small lobe, long ears, low-hanging columella, wide nasal base, depressed nasal bridge, wide nasal ridge, bulbouse nose, short philtrum, everted upper lip vermilion, thick upper lip vermilion | Hydrocephalus |
| P9 | Speech disability, developmental delay, hepatomegaly, mild learning disability, ptosis left eye, otitis media with effusion | Square face, malar flatting, underdeveloped nasolabial fold, broad jaw, broad chin, epicanthus, hypertelorism, downslanted palpebral fissure, telecanthus, prominent anithelix stem, serpenginous antihelix stem, everted antitragus, low-set ear, protruding ear, prominent crus helix, uplifted lobe, short columella, anteverted nares, wide nasal bridge, thick lower lip vermilion | Thin corpus callosum, mucosal thickening at the paranasal sinuses, hyperintense cells in left mastoid cells |
| P10 | Neuromotor developmental delay, inability to walk, inability to talk, spasticity, microcephaly, severe learning disability, fetal akinesia, intrauterine growth restriction, perinatal asphyxia, Y-shaped syndactyly, hypospadias, scoliosis, intestinal obstruction | Narrow forehead, cheekbone underdevelopment, full cheeks, malar flatting, underdeveloped nasolabial fold, tall chin, hypertelorism, thick eyebrows, long eyelashes, prominent eyelashes, upslanted palpebral fissure, telecanthus, underdeveloped antitragus, low-set ears, expanded terminal portion of crus helix, underfolded helix, attached lobe, underdeveloped tragus, underdeveloped ala nasi, short columella, anteverted nares, depressed nasal bridge, wide nasal bridge, wide nasal ridge, depressed nasal tip, broad philtrum, deep philtrum, exaggerated Cupid's bow, thick lower lip vermilion | Periventricular hyperintensity, thin corpus callosum, dilated third and lateral ventricles |
| P11 | Neuromotor developmental delay, inability to walk, inability to talk, spasticity, microcephaly, severe learning disability, fetal akinesia, perinatal asphyxia, Y-shaped syndactyly, hypospadias, scoliosis, intestinal obstruction, abnormal EEG | Frontal balding, narrow forehead, prominent forehead, underdeveloped supraorbital ridges, full cheeks, malar flatting, prominent nasolabial fold, premaxillary prominence, pointed chin, hypertelorism, thick eyebrow, long eyelashes, infra-orbital crease, telecanthus, antihelical shelf, underdeveloped antitragus, cupped ear, low-set ears, protruding ears, expanded terminal portion of crus helix, prominent crus helix, underfolded helix, small lobes, broad columella, low-hanging columella, wide nasal base, nasal bridge depressed, wide nasal bridge, convex nasal ridge, wide nasal ridge, broad nasal tip, midline sinus of philtrum, smooth philtrum, thick lower lip vermilion, thin upper lip vermilion | Dilated lateral ventricles, plagiocephaly |
| P12 | Neuromotor developmental delay, moderate learning disability, delayed psychosocial development, macrocephaly, chronic constipation, strabismus | High anterior hairline, long face, narrow forehead, narrow jaw, pointed chin, tall chin, hypertelorism, sparse eyebrow, long palpebral fissure, telecanthus, prominent inferior crus of antihelix, prominent antihelix stem, prominent superior crus of antihelix, everted antitragus, expanded terminal portion of crus helix, prominent crus helix, low insertion of columella, prominent nasal bridge, broad nasal tip, bulbouse nose, long nose, short philtrum, smooth philtrum, wide mouth, microdontia | Dilated at 4th ventricles, vermis and bilateral cerebellar hemisphere hypoplasia, pachygyria |
| P13 | Neuromotor developmental delay, severe learning disability, delayed psychosocial development, chronic constipation, strabismus | Prominent forehead, full cheeks, premaxillary prominence, short chin, deeply set eye, laterally extended eyebrow, sparse eyebrow, long eyelashes, proptosis, telecanthus, prominent inferior crus of antihelix, prominent antihelix stem, prominent antitragus, low-set ears, expanded terminal portion of crus helix, prominent crus helix, localized underdeveloped helix, bifid tragus, broad columella, depressed nasal bridge, wide nasal bridge, broad nasal tip, bulbouse nasal tip, broad philtrum | Periventricular hyperintensity, vermis and bilateral cerebellar hemisphere hypoplasia, pachygyria |
| P14 | Neuromotor developmental delay, severe learning disability, spastic tetraplegia, arthrogryposis, walking disability, speech disability, seizure | Brachycephaly, flat occiput, flat face, prominent glabella, malar flatting, pointed chin, epicanthus inversus, hypertelorism, deeply set eye, sparse eyebrow, prominent eyelashes, serpenginous antihelix stem, underdeveloped antitragus, cupped ears, low-set ears, expanded terminal portion of crus helix, prominent crus helix, overfolded helix, forward facing lobe, underdeveloped tragus, low-hanging columella, depressed nasal bridge, nasal bridge narrow, midline sinus philtrum, smooth philtrum, U-shaped upper lip vermilion | Bifrontotemporal atrophy, dilated bilateral ventricles and 3rd ventricular, periventricular hyperintensity, thin corpus callosum |
| P15 | Mental motor retardation, seizure, patent ductus arteriosus, cryptorchidism, hypothyroidism | Flat occiput, round face, midface prominence, broad chin, long chin, epicanthus, deep-set eyes, infraorbital crease, long palpebral fissure, synophrys, telecanthus, prominent antihelix stem, prominent antitragus, low-set ears, expanded terminal portion of crus helix, broad columella, wide nasal base, depressed nasal bridge, wide nasal bridge, wide nasal ridge, concave nasal ridge, broad nasal tip, long nose, broad philtrum, short philtrum, smooth philtrum, absent Cupid's bow, U-shaped upper lip vermilion | – |
| P16 | Mental motor retardation, intrauterine growth restriction, perinatal asphyxia, seizure, patent ductus arteriosus, bilateral iris coloboma, hypothyroidism, horizontal nystagmus | Flat occiput, midface prominent, broad chin, bilateral blepharophimosis, synophrys, telecanthus, prominent antihelix stem, prominent antitragus, low-set ears, expanded terminal portion of crus helix, small lobe, wide nasal base, depressed nasal bridge, wide nasal bridge, wide nasal ridge, broad nasal tip, long nose, broad philtrum, short philtrum, smooth philtrum, absent Cupid's bow, thick lower lip vermilion, U-shaped upper lip vermilion | – |
| P17 | Motor development delay, intrauterine growth restriction, cerebellar ataxia, mild learning disability | Flat face, midface prominence, underdeveloped nasolabial fold, pointed chin, telecanthus, prominent antihelix stem, low-set ears, unfolded helix, short columella, wide nasal base, wide nasal ridge, smooth philtrum, thin lower lip vermilion, thin upper lip vermilion | Multiple cysts in millimetric dimensions at both cerebellar hemispheres, irregularities in the cerebellum cortex, cerebellar vermis hypoplasia and enlarged at 4th ventricle |
| P18 | Motor development delay, intrauterine growth restriction, mirocephaly, encephalocele, spasticity at lower and upper extremities, blindness, cerebellar ataxia, mild learning disability, seen lateral ventricles and 3rd ventricular collapsed at CT | Brachycephaly, flat occiput, flat face, underdeveloped nasolabial fold, upslanted palpebral fissures, telecanthus, low-set ears, protruding ears, thick ala nasi, narrow nasal bridge, narrow nasal ridge, narrow nasal tip, smooth philitrum, exaggerated Cupid's bow | – |
| P19 | Motor development delay, small for gestational age, spasticity, severe learning disability, epiphyseal changes, short stature | Dolichocephaly, frontal balding, narrow forehead, underdeveloped supraorbital ridge, full cheeks, malar prominence, premaxillary prominence, pointed chin, entropion, hypertelorism, sparse eyebrows, almond-shaped palpebral fissures, telecanthus, angulated antihelix, prominent antihelix stem, low-set ears, expanded terminal portion crus helix, anterior crease lobe, thick ala nasi, wide nasal base, depressed nasal bridge, wide nasal ridge, broad nasal tip, deep philtrum, exaggerated Cupid's bow, thin upper lip vermilion | Thin corpus callosum |
| P20 | Neuromotor developmental delay, mild learning disability, seizure, generalized hypotonia, progressive vision loss, walking abnormalities | Broad face, full cheeks, midface prominence, broad jaw, short chin, laterally extended eyebrows, long eyelashes, telecanthus, angulated antihelix, prominent antihelix stem, crus helx expanded terminal portion, prominent crus helix, thick ala nasi, short columella, wide nasal base, wide nasal ridge, broad nasal tip, smooth philtrum, absent Cupid's bow, thin upper lip vermilion, wide month | Cortical and central atrophy, enlarged posterior fossa, Dandy-Walker variant |
| P21 | Neuromotor developmental delay, mild learning disability, microcephaly, speech delay, 5th finger clinodactyly | Narrow forehead, metopic depression, depressed glabella, midface prominence, epicanthus, upslanted palpebral fissure, prominent antihelix inferior crus, prominent antihelix stem, everted antitragus, low-set ears, wide nasal base, broad nasal tip, malaligned philtral ridge, thin upper lip vermilion | Dysplastic corpus callosum and polymicrogyria |
| P22 | Neuromotor developmental delay, mild learning disability, speech delay, attention deficit disorder, growth retardation | Full cheeks, malar flattening, midface prominence, epicanthus, telecanthus, angulated antihelix stem, prominent antihelix stem, low-set ears, prominent crus helix, thick ala nasi, broad columella, wide nasal bridge, deep philtrum, exaggerated Cupid's bow | |
| P23 | Neuromotor developmental delay, microcephaly, hypotonia in infancy, seizure, hypospadias, strabismus, nystagmus | Narrow forehead, sloping forehead, full cheeks, midface prominence, short chin, epicanthus inversus, thick eyebrows, long palpebral fissures, upslanted palpebral fissures, prominent inferior crus antihelix, prominent antihelix stem, underdeveloped superior crus antihelix, underdeveloped antitragus, low-set ears, expanded terminal portion crus helix, small lobes, anteverted nares, short columella, wide nasal bridge, broad nasal tip, long philtrum, exaggerated Cupid's bow, wide mouth | – |
| P24 | Neuromotor developmental delay, microcephaly, hypotonia, seizure, strabismus, nystagmus | Brachycephaly, narrow forehead, full cheeks, midface prominence, short chin, epicanthus inversus, thick eyebrows, long palpebral fissures, prominent antihelix stem, prominent antihelix crus inferior, underdeveloped antihelix superior crus, low-set ears, prominent crus helix, expanded terminal portion crus helix, shell ear, Stahl's ear, anteverted nares, short columella, wide nasal base, wide nasal bridge, broad nasal tip, long philtrum, tented upper lip vermilion | Severe cerebral atrophy, left frontoparietal polymicrogyria, bilateral hyperintense thalamus |
| P25 | Neuromotor developmental delay, autistic behaviors, moderate intellectual disability, language impairment | Brachycephaly, flat occiput, malar flattening, midface prominence, epicanthus, thick eyebrows, long palpebral fissures, angulated antihelix, prominent inferior crus of antihelix, prominent antihelix stem, everted antitragus, underdeveloped crus helix, large lobe, high insertion columella, narrow nasal base, depressed nasal bridge, convex nasal ridge, narrow nasal tip, deep philtrum, thick vermilion lower lip, downturned corners of mouth | Normal |
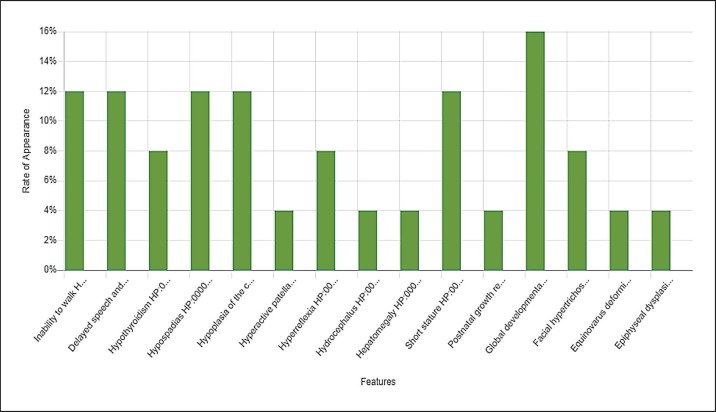
Clinical findings of all patients were annotated in Face2Gene application. The most common clinical finding was global developmental delay (16%). The second most common findings were inability to walk, delayed speech and language development, hypospadias, hypoplasia of corpus callosum, and short stature (12% for all). The third most common findings were hypothyroidism, hyperreflexia and facial hypertrichosis (8% for all), and the fourth most common findings were hyperactive patellar reflex, hydrocephalus, hepatomegaly, postnatal growth retardation, equinovarus deformity and epiphyseal dysplasia (4% for all). The distribution of clinical features is shown in Figure 1.
Fig. 1.
The distribution of clinical features.
Among the 30 diseases, the syndromes recommended by Face2Gene were analyzed for the presence and sequence of the syndrome diagnosed. Twelve of the cases (48%) had a correct match. The remaining 13 cases had a diagnosis that was not part of the 300 syndromes that DeepGestalt currently identifies. Thus, we only relied on the feature match algorithm. The application ranks the suggested syndromes based on 2 scores: Gestalt score and Feature score. Gestalt score is a value obtained by analyzing the photograph of the patient (dysmorphic facial features). The Feature score is a value obtained by analyzing the annotated clinical findings [Gurovich et al., 2019]. Gestalt score was calculated for only one (P9) of the patients included in this study. The other 11 patients had a Gestalt score as 0. Therefore, the Feature score is important for these patients. This situation shows the importance of the entry of the clinical feature findings of the patients to the application.
Discussion
In this study, we presented the importance of dysmorphic findings in rare genetic diseases and the power of the DeepGestalt program, which enables facial analysis for genetic syndrome classification. This application helps clinicians to make a definitive diagnosis of the disease. With further development of this application, it may be possible to use it routinely in genetic polyclinics.
Prevalence of rare genetic diseases is between 6 and 8% [Lodato and Kaplan, 2013]. In this group of diseases, any clinical (prenatal, natal, and postnatal) and dysmorphic findings are of importance at the stage of prediagnosis. In this study, we presented the clinical, radiological, and dysmorphic features of patients with rare genetic diseases diagnosed by WES analyses. Regarding that clinical geneticists and pediatricians rarely encounter this group of diseases, collecting this information on a platform such as Face2Gene would be beneficial for the attending physicians. Because these applications are based on deep learning, the more patients analyzed, the higher the accuracy. Especially in rare genetic diseases, it is important to increase the Gestalt score after the analysis of the patient.
Gurovich et al. [2019] reported that the success of Face2Gene top-10 matches was 91%. In 2019, Mishima et al. reported that Face2Gene success rate was 85.7% in patients with congenital dysmorphic syndromes in Japan. In the same study, if patients had a diagnosis for which Face2Gene had not been trained, the success of Face2Gene was 60.0% [Mishima et al., 2019]. We found low success of Face2Gene in consanguineous marriages. In our study, the recognition rate of Face2Gene application in our patient group was 48% (This rate was calculated from all diseases in a suggested list of 30 diseases). The probable reason for this low rate may be that the diseases in our patient group are not sufficiently introduced to Face2Gene; the rare genetic diseases are seen uncommonly in the population, and therefore have only been defined with a few patient photographs in this application.
The Face2Gene application was developed based on facial gestalt analysis. As a result of the face analysis, it determines the Gestalt score for 30 diseases matching the facial features of the patient. Furthermore, this application determines the Feature score for the 30 diseases by analyzing the anamnesis, clinical, laboratory and radiological findings of the patients. We strongly recommend that the clinical findings of the patient should be entered when using Face2Gene application, especially in rare genetic diseases. As seen in Table 3, data of patients with rare genetic diseases are limited in the application. We therefore recommend that physicians register the facial gestalt of patients to Face2Gene during or after diagnosis.
Table 3.
Face2Gene analysis results
| Case ID | Face2Gene detected disease | Face2Gene detected same syndrome with WES results |
|||
|---|---|---|---|---|---|
| rank at suggested syndromes list | Gestalt score | Feature score | Combined score | ||
| P1 | + | 2 | 0 | 0.63 | 0.5 |
| P2 | – | ||||
| P3 | – | ||||
| P4 | + | 23 | 0 | 0.43 | 0.04 |
| P5 | – | ||||
| P6 | – | ||||
| P7 | – | ||||
| P8 | – | ||||
| P9 | + | 1 | 0.173054 | 0.38 | 0.51 |
| P10 | – | ||||
| P11 | – | ||||
| P12 | – | ||||
| P13 | + | 4 | 0 | 0.68 | 0.25 |
| P14 | – | ||||
| P15 | – | ||||
| P16 | – | ||||
| P17 | + | 2 | 0 | 0.71 | 0.5 |
| P18 | + | 19 | 0 | 0.51 | 0.06 |
| P19 | – | ||||
| P20 | + | 21 | 0 | 0.46 | 0.05 |
| P21 | + | 17 | 0 | 0.49 | 0.07 |
| P22 | + | 15 | 0 | 0.51 | 0.07 |
| P23 | + | 10 | 0 | 0.55 | 0.08 |
| P24 | + | 4 | 0 | 0.59 | 0.25 |
| P25 | + | 12 | 0 | 0.69 | 0.1 |
The diagnosis of rare genetic diseases is one of the most challenging fields in clinical genetics. The success rate of WES has been reported to be between 25% and 57% in the diagnosis of rare genetic diseases [Boycott et al., 2013; Stark et al., 2016]. However, in this patient group, it may be more helpful to analyze with NGP before, e.g., the DeepLearning program, and then follow traditional diagnostic methods considering the result of NGP. When considering the cost difference between targeted gene panels and WES, with this strategy, a diagnosis with lower costs can be provided [van Nimwegen et al., 2016], and at the same time, we believe the diagnostic procedures can be shortened.
Rare genetic diseases are often inherited in an autosomal recessive manner [Boycott et al., 2013]. Consanguinity between parents is one of the important risk factors for autosomal recessive inherited diseases. In the study of Hamamy et al. [2011], it was reported that the prevalence of congenital anomaly in first-degree cousin marriage offspring increased by 1.7-2.8% compared to the general population. The rate of consanguineous marriages in Turkey as Muslim and Middle Eastern countries is high. In the study by Kelmemi et al. [2015], the rate of consanguineous marriages in autosomal recessive inherited diseases was reported as 58% in Tunisia. In our study, 24 of 25 patients had autosomal recessive inherited disease; the rate of consanguineous marriages between the parents of patients with autosomal recessive inheritance was calculated as 80%. This higher rate may be due to the frequent consanguineous marriages in the region. In the study by Kelmemi et al. [2015], the rate of parents sharing the same geographical origin in the autosomal recessive-inherited nonconsanguineous patient group was reported to be 63%.
Microcephaly is one of the most common clinical findings seen by medical genetic doctors. Whensearching for “microcephaly” in OMIM, the result was 1,007 from 8,976 entries. On the other hand, von der Hagen et al. [2014] found that 28.5% of the children with microcephaly had genetic etiology. Also, in a study by Ashwal et al. [2009], 15.5-53.3% of children with microcephaly had a genetic cause. In our study, the rate of patients with microcephaly who have a genetic disease was 40%. Symptoms such as microcephaly and dysmorphic facial features are common in genetic diseases. Therefore, online databases (such as OMIM) of clinical findings of diseases are helpful tools for clinical genetics. However, medical genetic doctors must decide which of the possible diagnoses is most plausible in the patient. This judgment requires extensive clinical experience.
Evaluating genetic diseases is like working as a detective who investigates a criminal event: every clue is very beneficial for reaching the diagnosis. One of these clues is MRI. Considering that most patients who consulted the genetic clinic are patients with neurological diseases, the importance of MRI is evident [Srivastava et al., 2014]. Corpus callosum abnormality is one of these MR findings. In a review article by Edwards et al. [2014], 30-45% of the cases with corpus callosum agenesis were identified as genetic causes. In 25-30%, the reason is a single gene mutation. In a study by Schell-Apacik et al. [2008], 32% of the patients with agenesis of the corpus callosum and dysgenesis of the corpus callosum had a genetic etiology. In our study, corpus callosum abnormality was found in 47% of the patients with a single gene mutation. The abnormal corpus callosum is a condition that should be taken into consideration by physicians because it may accompany a syndrome.
Nowadays, good anamnesis, examination, radiological and laboratory tests are necessary when diagnosing rare diseases. In addition, recently developed artificial intelligence technology can give us valuable clues in terms of diagnosis. The NGP technology may have a say in the diagnosis of genetic diseases with the use and contribution of people working in this field. So, we recommend employing such NGP programs.
In conclusion, each syndrome has a mask. In other words, all syndromes leave a trace or a clue in the phenotype. For years, dysmorphologists have been looking at photographs in dysmorphology books to diagnose patients' syndromes. With the widespread use of NGP technology in recent years, the diagnosis has become easier, not only by looking, but also by scanning patient pictures. However, introducing clinical findings to the program is crucial for more accurate diagnostic recommendations. Finally, with the expansion of such NGP programs, a large and powerful data library will be created, making future diagnostic procedures easier.
Statement of Ethics
The project was approved by the University of Afyonkarahisar Health Sciences Ethics Committee, which covered the participating hospitals. All procedures followed were in accordance with the University of Sydney Human Research Ethics Committee and with the Helsinki Declaration of 1975, as revised in 2000 (5). Signed or electronic consent was obtained from all participants in the study.
Disclosure Statement
The authors have no conflicts of interest to declare.
Author Contributions
M. Elmas conceived and designed the study. B. Gogus performed clinical assessments, experiments, and contributed to data acquisition, analysis and interpretation. B. Gogus drafted the manuscript. Both authors contributed to critical revision of the manuscript for intellectual content and final approval of the manuscript.
Acknowledgment
We thank Nicole Fleischer for her support and assistance.
References
- 1.Allanson JE, Biesecker LG, Carey JC, Hennekam R. Elements of morphology: introduction. Am J Med Genet A. 2009;149A:2–5. doi: 10.1002/ajmg.a.32601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashwal S, Michelson D, Plawner L, Dobyns WB, Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society Practice parameter: evaluation of the child with microcephaly (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2009 doi: 10.1212/WNL.0b013e3181b783f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baird PA, Anderson TW, Newcombe HB, Lowry RB. Genetic disorders in children and young adults: a population study. Am J Hum Genet. 1988;42:677–693. [PMC free article] [PubMed] [Google Scholar]
- 4.Botstein D, Risch N. Discovering genotypes underlying human phenotypes: past successes for mendelian disease, future approaches for complex disease. Nat Genet. 2003;33(Suppl):228–237. doi: 10.1038/ng1090. [DOI] [PubMed] [Google Scholar]
- 5.Boycott KM, Vanstone MR, Bulman DE, MacKenzie AE. Rare-disease genetics in the era of next-generation sequencing: discovery to translation. Nat Rev Genet. 2013;14:681–691. doi: 10.1038/nrg3555. [DOI] [PubMed] [Google Scholar]
- 6.Clark MM, Stark Z, Farnaes L, Tan TY, White SM, et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genomic Med. 2018;3:16. doi: 10.1038/s41525-018-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards TJ, Sherr EH, Barkovich AJ, Richards LJ. Clinical, genetic and imaging findings identify new causes for corpus callosum development syndromes. Brain. 2014;137:1579–1613. doi: 10.1093/brain/awt358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Featherstone K, Latimer J, Atkinson P, Pilz DT, Clarke A. Dysmorphology and the spectacle of the clinic. Sociol Heal Illn. 2005;27:551–574. doi: 10.1111/j.1467-9566.2005.00456.x. [DOI] [PubMed] [Google Scholar]
- 9.Ferry Q, Steinberg J, Webber C, FitzPatrick DR, Ponting CP, et al. Diagnostically relevant facial gestalt information from ordinary photos. Elife. 2014;3:e02020. doi: 10.7554/eLife.02020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guest SS, Evans CD, Winter RM. The Online London Dysmorphology Database. Genet Med. 1999;1:207–212. doi: 10.1097/00125817-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Gurovich Y, Hanani Y, Bar O, Fleischer N, Gelbman D, et al. DeepGestalt - identifying rare genetic syndromes using deep learning. arXiv:1801.07637. 2018 [Google Scholar]
- 12.Gurovich Y, Hanani Y, Bar O, Nadav G, Fleischer N, et al. Identifying facial phenotypes of genetic disorders using deep learning. Nat Med. 2019;25:60–64. doi: 10.1038/s41591-018-0279-0. [DOI] [PubMed] [Google Scholar]
- 13.Hamamy H, Antonarakis SE, Cavalli-Sforza LL, Temtamy S, Romeo G, et al. Consanguineous marriages, pearls and perils: Geneva International Consanguinity Workshop Report. Genet Med. 2011;13:841–847. doi: 10.1097/GIM.0b013e318217477f. [DOI] [PubMed] [Google Scholar]
- 14.Hammond P. The use of 3D face shape modelling in dysmorphology. Arch Dis Child. 2007:1120–1126. doi: 10.1136/adc.2006.103507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelmemi W, Chelly I, Kharrat M, Chaabouni-Bouhamed H. Consanguinity and homozygosity among Tunisian patients with an autosomal recessive disorder. J Biosoc Sci. 2015;47:718–726. doi: 10.1017/S002193201400056X. [DOI] [PubMed] [Google Scholar]
- 16.Lodato E, Kaplan W. Priority Medicines for Europe and the World: 2013 Update Report. chapter 6.1. :pp 68–74. (WHO 2013) [Google Scholar]
- 17.Mishima H, Suzuki H, Doi M, Miyazaki M, Watanabe S. Evaluation of Face2Gene using facial images of patients with congenital dysmorphic syndromes recruited in Japan. J Hum Genet. 2019;64:789–794. doi: 10.1038/s10038-019-0619-z. [DOI] [PubMed] [Google Scholar]
- 18.Ng SB, Turner EH, Robertson PD, Flygare SD, Abigail W, et al. Targeted capture and massively parallel sequencing of 12 human exomes. Nature. 2009;461:272–276. doi: 10.1038/nature08250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng SB, Nickerson DA, Bamshad MJ, Shendure J. Massively parallel sequencing and rare disease. Hum Mol Genet. 2010;19:119–124. doi: 10.1093/hmg/ddq390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pantel JT, Zhao M, Mensah MA, Hajjir N, Hsieh TC, et al. Advances in computer-assisted syndrome recognition by the example of inborn errors of metabolism. J Inherit Metab Dis. 2018;41:533–539. doi: 10.1007/s10545-018-0174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schell-Apacik CC, Wagner K, Bihler M, Ertl-Wagner B, Heinrich U, et al. Agenesis and dysgenesis of the corpus callosum: clinical, genetic and neuroimaging findings in a series of 41 patients. Am J Med Genet A. 2008;146A:2501–2511. doi: 10.1002/ajmg.a.32476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smigiel R, Demkow U. Next generation sequencing in dysmorphology. In: Demkow U, Ploski R, editors. Clinical Applications for Next-Generation Sequencing. London: Elsevier Inc; 2016. [Google Scholar]
- 23.Srivastava S, Cohen JS, Vernon H, Barañano K, McClellan R, et al. Clinical whole exome sequencing in child neurology practice. Ann Neurol. 2014;76:473–483. doi: 10.1002/ana.24251. [DOI] [PubMed] [Google Scholar]
- 24.Stark Z, Tan TY, Chong B, Brett GR, Yap P, et al. 2016. Original Research Article A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet Med. 2016;18:1090–1096. doi: 10.1038/gim.2016.1. [DOI] [PubMed] [Google Scholar]
- 25.Strømme P. The diagnosis of syndromes by use of a dysmorphology database. Acta Paediatr Scand. 1999;80:106–109. doi: 10.1111/j.1651-2227.1991.tb11741.x. [DOI] [PubMed] [Google Scholar]
- 26.van Nimwegen KJ, van Soest RA, Veltman JA, Nelen MR, van der Wilt GJ, et al. Is the $1000 Genome as near as we think ? A cost analysis of next-generation sequencing. Clin Chem. 2016;62:1458–1464. doi: 10.1373/clinchem.2016.258632. [DOI] [PubMed] [Google Scholar]
- 27.von der Hagen M, Pivarcsi M, Liebe J, von Bernuth H, Didonato N, et al. Diagnostic approach to microcephaly in childhood : a two-center study and review of the literature. Dev Med Child Neurol. 2014;56:732–741. doi: 10.1111/dmcn.12425. [DOI] [PubMed] [Google Scholar]
- 28.Yang Y, Muzny DM, Xia F, Niu Z, Person R, et al. Molecular findings among patients referred for clinical whole-exome sequencing. JAMA. 2014;312:1870–1879. doi: 10.1001/jama.2014.14601. [DOI] [PMC free article] [PubMed] [Google Scholar]