Abstract
Introduction
A taller-than-wide (TTW) shape is a suspicious feature of thyroid nodules commonly defined as an anteroposterior/transverse diameter (AP/T) ratio >1. An intraobserver variability of up to 18% in AP diameter evaluations has been described, which may lead to overreporting of this feature. To potentially improve the reliability of the TTW definition, we propose an arbitrary ratio of ≥1.2.
Objective
The aim of this study was to estimate the impact of this definition on diagnostic performance.
Methods
We prospectively analyzed 553 thyroid nodules referred for cytology evaluation at an academic center. Before fine-needle aspiration, two examiners jointly defined all sonographic features considered in risk stratification systems developed by the American Thyroid Association (ATA), the American Association of Clinical Endocrinologists (AACE), the American College of Radiology (ACR TIRADS), the European Thyroid Association (EU-TIRADS), and the Korean Society of Thyroid Radiology (K-TIRADS). TTW was defined according to the current definition (AP/T diameter ratio >1) and an arbitrary alternative definition (AP/T ratio >1.2).
Results
The alternative definition classified fewer nodules as TTW (28, 5.1% vs. 94, 17%). The current and proposed definitions have a sensitivity of 26.2 and 11.9% (p = 0.03) and a specificity of 83.8 and 95.5% (p < 0.001). Thus, as a single feature, the arbitrary definition has a lower sensitivity and a higher specificity. When applied to sonographic risk stratification systems, however, the proposed definition would increase the number of avoided biopsies (up to 58.2% for ACR TIRADS) and the specificity of all systems, without negative impact on sensitivity or diagnostic odds ratio.
Conclusions
Re-defining TTW nodules as those with an AP/T ratio ≥1.2 improves this marker's specificity for malignancy. Using this definition in risk stratification systems will increase their specificity, reducing the number of suggested biopsies without significantly diminishing their overall diagnostic performance.
Keywords: Ultrasonography, Ultrasound, Thyroid nodule, Reproducibility of results, Sensitivity and specificity
Introduction
Currently available sonographic risk stratification systems for thyroid nodules were developed to more accurately identify those for which fine-needle aspiration cytology (FNAC) can safely be deferred [1, 2, 3, 4, 5]. The likelihood that a nodule is malignant is indicated by the risk class it is assigned to on the basis of multiple sonographically defined features. Within each risk class, a size threshold is specified above which FNAC is recommended. For low-risk nodules, the size thresholds for FNA range from 1.5 to 3.0 cm, depending on the risk stratification system used. For those assigned to high-risk classes, FNAC is generally recommended if the maximum diameter is ≥1 cm [1, 2, 3, 4, 5]. To apply these systems, an essential prerequisite is the adoption of a uniform language and definition of suspicious features [6].
In two meta-analyses [7, 8], the thyroid nodule feature with the highest odds ratio for malignancy was a taller-than-wide (TTW) shape − also referred to as non-parallel orientation − although the results across the studies included in the analysis were quite heterogeneous. As shown in online supplementary Table 1 (for all online suppl. material, see www.karger.com/doi/10.1159/000504219), the five sonographic systems most widely used to estimate the probability of thyroid nodule malignancy define TTW nodules as those with an anteroposterior (AP) diameter that exceeds the transverse (T) diameter [1, 2, 3, 4, 5], without specifying any minimum magnitude for the excess. As a result, the term TTW can potentially be applied to nodules whose AP and T diameters differ by only a few millimeters. Under these circumstances, the clinical impact of inter- and/or intraobserver variability − a well-documented limitation of ultrasound-based measurements − is likely to be considerable: an intraobserver variability of up to 18% [9] and an interobserver variability of 20.9% were reported for AP diameter measurements [10]. Indeed, in our recent study of changes over time in risk-class assignments, nodules reclassified as TTW during follow-up accounted for almost half of those with a higher risk class at 5 years and almost two-thirds of those whose status change included a recommendation for FNAC [11].
These considerations suggested that a slightly higher AP/T diameter ratio threshold for TTW nodules might improve the specificity of risk stratification systems in ruling out malignancy and, in particular, in pinpointing nodules for which FNAC can safely be deferred. The study described below was undertaken to explore this possibility.
Patients and Methods
This study was conducted as part of a prospective project aimed at characterizing the performances of the systems most widely used for the sonographic risk stratification of thyroid nodules. Participants were recruited in the thyroid cancer unit of an academic healthcare center. Enrolment was offered to all individuals consecutively referred to the unit for FNAC of a thyroid nodule between November 1, 2015, and September 10, 2018. Subcentimeter nodules were excluded because their biopsy is generally not indicated in any of these risk stratification systems (online suppl. Fig. 1).
Cytology was reported according to the Italian Consensus for Thyroid Cytopathology criteria [12, 13]. A composite reference standard was applied. If the nodule was resected, the final diagnosis was based on surgical histology. Otherwise, the reference standard was FNA cytology. Nodules were considered malignant if they were classified as TIR4 or TIR5 (suspected malignancy or malignancy, similar to Bethesda classes V and VI [14]), and benign if they were classified as TIR2, comparable to Bethesda class II. Unresected nodules without surgical histology and cytologically classified as nondiagnostic, low-risk indeterminate (TIR3A), or high-risk indeterminate (TIR3B), similar to Bethesda classes I, III, and IV, respectively, were excluded due to the absence of a conclusive diagnosis (online suppl. Fig. 1).
Prior to aspiration, each nodule was explored jointly in real time by two clinicians using HI VISION Avius® equipment, and consensus decisions were reached to reduce interobserver variability, which has been documented in assessments of individual sonographic features of thyroid nodules [15, 16]. Full details on the procedures used for sonographic assessment, risk stratification, and FNAC examination of the nodules have been published elsewhere [11, 17, 18]. Using a subset of this cohort, we previously conducted a study to compare the diagnostic performance of 5 sonographic stratification systems and to evaluate the role of nodule location, and those results have already been reported [18, 19]. In summary, all nodule sonographic features were collected: diameters, margins, composition, echogenicity, presence of calcifications and other hyperechoic foci, and suspected extrathyroidal extension. For mixed nodules, the location of the solid component (non-nodular, eccentric, and central) was also recorded. The malignancy risk of each nodule was estimated according to five sonographic risk stratification systems: (1) the American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi (AACE/ACE/AME) guidelines; (2) the American College of Radiology (ACR) TIRADS; (3) the American Thyroid Association (ATA) guidelines; (4) the European Thyroid Association (EU-TIRADS); and (5) the Korean TIRADS (K-TIRADS). For the purposes of this study, nodules that could not be classified according to the ATA Guidelines (e.g., isoechoic nodules with other suspicious features such as microcalcification, irregular margins, and TTW shape) were considered intermediate-suspicion nodules.
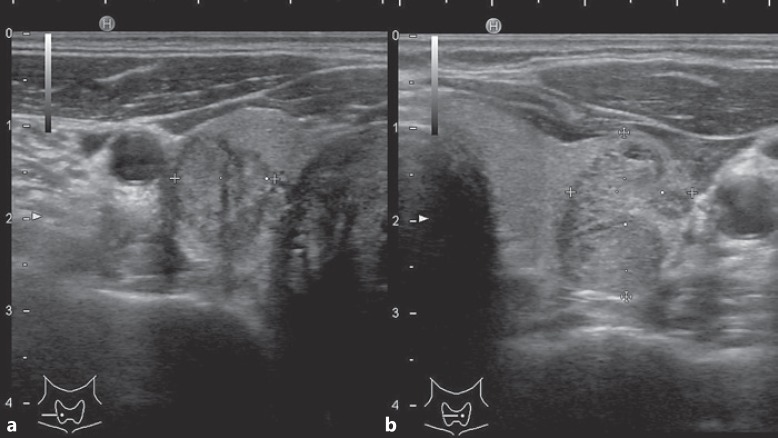
The feature of interest in the present study − i.e., nodule shape − was assessed by on-screen caliper measurement of the T diameter (always made in the T plane) and the AP diameter (made in either the AP or T plane). For the present analysis, each nodule was classified as TTW or non-TTW using two definitions: the first based on the currently accepted AP/T diameter ratio threshold for TTW (AP/T >1.0), the second an arbitrarily selected alternative consisting of an AP/T diameter threshold of >1.2; Fig. 1). The alternative proposed was chosen arbitrarily based on reported variability in the sonographic measurement of thyroid nodule diameters [9, 10].
Fig. 1.
Sonographic images of two nodules. Both were suspicious for papillary thyroid cancer, which was histologically confirmed. a This nodule would fulfill the current definition only (TTW ratio = 1.15); however, applying TIRADS, it would still be submitted to biopsy, being predominantly solid, partially hypoechoic, with lobulated margins. b This nodule would fulfill the arbitrary definition (TTW ratio = 1.35).
The shape thus obtained was entered into each of the five risk stratification systems to estimate each nodule's likelihood of malignancy and whether or not it required FNAC. For each system, we compared the results obtained with the current and alternative definitions of TTW; more specifically, the percentage of nodules classified as FNAC-deferrable and the appropriateness of this classification based on the reference standard.
Statistical Analysis
For each sonographic risk stratification system, the indication for FNAC under each of the test conditions (i.e., current vs. proposed definition of TTW) was defined as a test positivity. We assessed sensitivity, specificity, and the proportion of nodules classified as FNAC-deferrable (test negativity) by each of the five systems using both the current and the proposed definition of TTW. These parameters were compared with the McNemar test [20]. Analyses were done with the IBM SPSS Statistics package, version 25.0 (IBM Corporation). We also calculated the areas under the receiver-operating characteristic (AUROC) curve that were compared using the DeLong approach [21], utilizing the easyROC package [22].
Results
Overall, 917 thyroid nodules were sonographically evaluated prior to biopsy. Eighty-two nodules were excluded from the analysis because their maximum diameter was >1 cm, and 282 were excluded due to an inconclusive (nondiagnostic or indeterminate) diagnosis. The final cohort included 553 thyroid nodules (median maximum diameter 19.7 mm, interquartile range 14.5–27.5; online suppl. Fig. 1): 42 (7.6%) were classified as malignant. Thirty-nine nodules were histologically confirmed as anaplastic thyroid cancer (n = 1); follicular thyroid cancer (n = 1); follicular-variant papillary thyroid cancer (n = 6); medullary thyroid cancer (n = 2); papillary thyroid cancer (n = 26); and metastases from other solid tumors (n = 3). The other 3 nodules had cytological diagnoses of malignancy (TIR5, n = 1) or suspected malignancy (TIR4, n = 2) and were managed with active surveillance following patient preferences.
Applying the current definition, 94 (17%) nodules were defined as TTW, as opposed to 28 (5.1%) under the arbitrary definition. Classification of a nodule as TTW alone predicted a reference diagnosis of malignancy with 26.2% sensitivity (95% CI 13.9–42.0) and 83.8% specificity (95% CI 80.3–86.8) when the current definition of TTW was used. The positive likelihood ratio was 1.61 (95% CI 0.93–2.78), the negative likelihood ratio was 0.88 (95% CI 0.733–1.06), and the diagnostic odds ratio was 1.83 (95% CI 0.88–3.78). The sensitivities and specificities according to different cutoff values of the AP/T ratio to define TTW shape are plotted in online supplementary Figure 2. When the alternative definition of TTW was used (AP/T ratio >1.20), the specificity rose to 95.5% (95% CI 93.3–97.1, p < 0.001), whereas sensitivity dropped even lower to 11.9% (95% CI 4–25.6; p = 0.03). The positive likelihood ratio of the arbitrary definition was 2.64 (95% CI 1.06–6.60), the negative likelihood ratio was 0.92 (0.82–1.03), and the diagnostic odds ratio was 2.87 (95% CI 1.03–7.98).
Performance of Sonographic Classification Systems Applying the Proposed Definitions
The malignancy rates of the nodules classified in the intermediate and high-risk classes of the five systems applying the current and proposed definition of TTW shape are reported in Table 1. In particular, the proposed definition increased the malignancy rate of the highest risk class of all classifications.
Table 1.
Malignancy rate of the various classes of the five sonographic risk stratification systems, applying the current and proposed definition of TTW shape
| Malignancy rate |
||
|---|---|---|
| current TTW definition | proposed TTW definition | |
| ATA Guidelines | ||
| Benign | 0 | 0 |
| Very low suspicion | 1.9 | 2 |
| Low suspicion | 3.5 | 3 |
| Intermediate suspiciona | 10.9 | 14 |
| High suspicion | 32.2 | 35.8 |
| AACE/ACE/AME | ||
| Low risk | 0 | 0 |
| Intermediate risk | 3.7 | 3.5 |
| High risk | 16.8 | 22.0 |
| ACR TIRADS | ||
| TR1 benign | 0 | 0 |
| TR2 not suspicious | 2 | 2.4 |
| TR3 mildly suspicious | 1.9 | 1.6 |
| TR 4 moderately suspicious | 6.4 | 6.5 |
| TR 5 highly suspicious | 28.9 | 37.5 |
| EU-TIRADS | ||
| 2 Benign | 0 | 0 |
| 3 Low risk | 2.3 | 2.3 |
| 4 Intermediate risk | 7.7 | 7.2 |
| 5 High risk | 17.2 | 22.8 |
| K-TIRADS | ||
| 2 Benign | 0 | 0 |
| 3 Low suspicion | 2.3 | 2.3 |
| 4 Intermediate suspicion | 10.6 | 13.6 |
| 5 High suspicion | 47.2 | 50.0 |
Values are percentages. AACE/ACE/AME, American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi; ACR, American College of Radiology; ATA, American Thyroid Association; EU-TIRADS, European Thyroid Imaging Reporting and Data Systems; K-TIRADS, Korean Thyroid Imaging Reporting and Data Systems; TTW, taller-than-wide shape.
Intermediate suspicious nodules include not classifiable nodules.
This proposed definition had an impact on the number of indicated biopsies and the diagnostic accuracy of the sonographic risk stratification systems, significantly increasing the number of deferrable biopsies for all classifications (up to 58.2% of the nodules would avoid FNA indication according to ACR TIRADS), as reported in Table 2. Furthermore, the proposed TTW definition significantly increased the specificity of all risk stratification systems (Table 2). On the other hand, the sensitivity of each sonographic system and the overall diagnostic accuracy, evaluated according to the AUROC, did not significantly change.
Table 2.
Number of avoided biopsies, missed malignancies, sensitivity, specificity, and AUROC curve according to five sonographic risk stratification systems, applying the current and proposed definition of TTW shape
| Avoided biopsies (%) |
Delta | False negatives, (%) |
Sensitivity (95% CI) |
Specificity (95% CI) |
AUROC (95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| TTW definition | current | proposed | current | proposed | current | proposed | current | proposed | current | proposed | |
| ATA (modified)a | 141 | 160** | 19 | 4 (2.8) | 5 (3.1) | 90.5% | 88.1%# | 26.8% | 30.3%** | 0.586 | 0.592§ |
| (25.5) | (28.9) | (77.4–97.4) | (74.4–96) | (23–30.9) | (26.4–34.5) | (0.537–0.635) | (0.539–0.645) | ||||
| AACE/ACE/AME | 189 | 217** | 28 | 6 (3.2) | 7 (3.2) | 85.7% | 83.3%# | 35.8% | 41.1%** | 0.608 | 0.622§ |
| (34.2) | (39.2) | (71.5–94.6) | (68.6–93) | (31.6–40.1) | (36.8–45.5) | (0.550–0.665) | (0.56–0.683) | ||||
| ACR TIRADS | 287 | 322** | 35 | 8 (2.8) | 9 (2.8) | 80.9% | 78.6%# | 54.6% | 61.2%** | 0.678 | 0.699§ |
| (51.9) | (58.2) | (65.9–91.4) | (63.2–89.7) | (50.2–59) | (56.9–65.5) | (0.614–0.742) | (0.633–0.765) | ||||
| EU-TIRADS | 165 | 189** | 24 | 6 (3.6) | 7 (3.7) | 85.7% | 83.3%# | 31.1% | 35.6%** | 0.584 | 0.595§ |
| (29.8) | (34.2) | (71.5–94.6) | (68.6–93) | (27.1–35.3) | (31.5–39.9) | (0.527–0.641) | (0.534–0.655) | ||||
| K-TIRADS | 92 | 100* | 8 | 3 (3.3) | 3 (3) | 92.9% | 92.9%* | 17.4% | 19%* | 0.551 | 0.559§ |
| (16.6) | (18.1) | (80.5–98.5) | (80.5–98.5) | (14.2–21) | (15.7–22.7) | (0.509–0.594) | (0.516–0.602) | ||||
Comparison of the current and proposed definition of TTW shape; McNemar test. AACE/ACE/AME, American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi; ACR, American College of Radiology; ATA, American Thyroid Association; AUROC, area under the receiver-operating characteristic curve; EU-TIRADS, European Thyroid Imaging Reporting and Data Systems; K-TIRADS, Korean Thyroid Imaging Reporting and Data Systems; TTW, taller-than-wide shape.
p < 0.01;
p < 0.001;
p = n.s. comparison of the AUROC of the current and proposed definition of TTW shape; DeLong et al. [21];
p = n.s.
For the purpose of this study, nodules that could not be classified according to the ATA Guidelines (e.g., isoechoic nodules with other suspicious features such as microcalcification, irregular margins, and TTW shape) were considered intermediate-suspicion nodules.
Discussion
Ultrasonography plays pivotal roles in the management of thyroid nodules [23] by identifying those requiring FNA cytology [1, 3] and guiding decisions on long-term follow-up strategies [1, 3]. To improve reproducibility and simplify reporting, sonographic systems for risk stratification of thyroid nodules have been developed by several scientific societies [1, 2, 3, 4, 5], and their diagnostic performance has been explored and validated in numerous studies [18, 24, 25, 26, 27, 28, 29, 30, 31, 32].
However, these systems still rely on the recognition of specific suspicious features. A TTW shape has proven to be significantly associated with malignancy, with a diagnostic odds ratio appreciably higher than those of other features acknowledged as suspicious [7, 8]. This feature was introduced for the first time in 2002, because, similarly to the breast, the growth of benign nodules has been documented within normal tissue planes, while malignancies grow across tissue planes [33]. However, the definition of TTW is not consistent across systems (online suppl. Table 1), and because it depends on the measurement (or at least the estimate) of nodule diameters, it is subjected to inter- and even intraobserver variability. Indeed, shape displayed variable interobserver agreement (online suppl. Table 2) and has been demonstrated to be one of the features that frequently causes variation in the estimated malignancy risk of nodules over time [11]. Since an intraobserver variability of up to 18% has been reported for the AP diameter evaluation, we proposed that the TTW shape be defined as an AP/T diameter ratio of ≥1.2 (i.e., the AP diameter is at least 20% greater than the T diameter). Our results showed that although this proposed definition would reduce the number of nodules with this feature by about 70%, it would not negatively influence the diagnostic performance of sonographic classification systems, additionally increasing the number of potentially avoidable biopsies. The main challenge in the clinical management of thyroid nodules nowadays is to avoid overdiagnosis in patients with benign nodules (or low-risk disease) while promptly identifying those patients with clinically relevant malignancies: the reduction in the number of biopsies is a desirable goal, particularly because, applying sonographic risk-assessment systems, sensitivity is not significantly reduced (and the number of malignancy that would be missed is overall low, Table 2). In fact, even if 66 nodules would lose the TTW shape designation, no more than 35 would have deferred biopsy for this reason, while the remaining are still candidates for immediate biopsy due to other suspicious features.
It is important to recall that ours was a selected cohort of patients with thyroid nodules: all had been referred to our unit for FNAC, for reasons known only to the referring physician. However, the full range of sonographic risk classes was represented in this cohort, and the final malignancy rate was similar to that reported in unselected series [34]. Moreover, most (but not all) malignancy rates of diagnoses were surgical, but the possibility of false positives cannot be excluded for the 3 patients with cytological evidence of malignancy who opted for nonsurgical management. For nodules classified as benign, the diagnoses were cytological: thus, false-negative cases are possible, with a false-negativity rate of 3.7% reported in this setting [35]. Furthermore, subcentimeter nodules and lesions with inconclusive diagnosis were excluded. However, TTW rates using both definitions are unchanged by these exclusions. Finally, the visual assessment of TTW shape is commonly used in clinical practice: this study is not able to compare the performance of a quantitative evaluation to a qualitative one. The quantitative evaluation, however, would avoid confusion about the TTW and taller-than-long shape (the latter is defined as an AP diameter longer than the longitudinal one) that some earlier studies considered a single entity (online suppl. Table 1). The arbitrary definition was proposed based on the described variability in AP diameter evaluation; however, its performance in improving reliability is yet to be determined.
In conclusion, adopting an arbitrary definition of TTW as an AP/T diameter ratio ≥1.2 would reduce the number of indicated biopsies according to five widely used sonographic risk stratification systems and improve specificity without negatively influencing overall diagnostic performance.
Statement of Ethics
This study was conducted with institutional review board approval and written informed patient consent.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
The study was funded by the Research Starter Grants of the University of Rome, Sapienza (to G.G., AR216154C9B479B2).
Supplementary Material
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Acknowledgement
G.G., L.L., V.R., and R.F. contributed to this paper as part of their PhD studies in Biotechnologies and Clinical Medicine at the University of Rome, Sapienza.
References
- 1.Gharib H, Papini E, Garber JR, Duick DS, Harrell RM, Hegedüs L, et al. AACE/ACE/AME Task Force on Thyroid Nodules American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22((5 Supplement 1)):622–39. doi: 10.4158/EP161208.GL. [DOI] [PubMed] [Google Scholar]
- 2.Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017 May;14((5)):587–95. doi: 10.1016/j.jacr.2017.01.046. [DOI] [PubMed] [Google Scholar]
- 3.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016 Jan;26((1)):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L. European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: the EU-TIRADS. Eur Thyroid J. 2017 Sep;6((5)):225–37. doi: 10.1159/000478927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology Ultrasonography Diagnosis and Imaging-Based Management of Thyroid Nodules: Revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations. Korean J Radiol. 2016 May-Jun;17((3)):370–95. doi: 10.3348/kjr.2016.17.3.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant EG, Tessler FN, Hoang JK, Langer JE, Beland MD, Berland LL, et al. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J Am Coll Radiol. 2015 Dec;12((12 12 Pt A)):1272–9. doi: 10.1016/j.jacr.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Brito JP, Gionfriddo MR, Al Nofal A, Boehmer KR, Leppin AL, Reading C, et al. The accuracy of thyroid nodule ultrasound to predict thyroid cancer: systematic review and meta-analysis. J Clin Endocrinol Metab. 2014 Apr;99((4)):1253–63. doi: 10.1210/jc.2013-2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campanella P, Ianni F, Rota CA, Corsello SM, Pontecorvi A. Quantification of cancer risk of each clinical and ultrasonographic suspicious feature of thyroid nodules: a systematic review and meta-analysis. Eur J Endocrinol. 2014 Apr;170((5)):R203–11. doi: 10.1530/EJE-13-0995. [DOI] [PubMed] [Google Scholar]
- 9.Lee HJ, Yoon DY, Seo YL, Kim JH, Baek S, Lim KJ, et al. Intraobserver and Interobserver Variability in Ultrasound Measurements of Thyroid Nodules. J Ultrasound Med. 2018 Jan;37((1)):173–8. doi: 10.1002/jum.14316. [DOI] [PubMed] [Google Scholar]
- 10.Brauer VF, Eder P, Miehle K, Wiesner TD, Hasenclever H, Paschke R. Interobserver variation for ultrasound determination of thyroid nodule volumes. Thyroid. 2005 Oct;15((10)):1169–75. doi: 10.1089/thy.2005.15.1169. [DOI] [PubMed] [Google Scholar]
- 11.Grani G, Lamartina L, Biffoni M, Giacomelli L, Maranghi M, Falcone R, et al. Sonographically Estimated Risks of Malignancy for Thyroid Nodules Computed with Five Standard Classification Systems: Changes over Time and Their Relation to Malignancy. Thyroid. 2018 Sep;28((9)):1190–7. doi: 10.1089/thy.2018.0178. [DOI] [PubMed] [Google Scholar]
- 12.Nardi F, Basolo F, Crescenzi A, Fadda G, Frasoldati A, Orlandi F, et al. Italian consensus for the classification and reporting of thyroid cytology. J Endocrinol Invest. 2014 Jun;37((6)):593–9. doi: 10.1007/s40618-014-0062-0. [DOI] [PubMed] [Google Scholar]
- 13.Fadda G, Basolo F, Bondi A, Bussolati G, Crescenzi A, Nappi O, et al. SIAPEC-IAP Italian Consensus Working Group. Proposal of the SIAPEC-IAP Italian Consensus Working Group Cytological classification of thyroid nodules. Pathologica. 2010 Oct;102((5)):405–8. [PubMed] [Google Scholar]
- 14.Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid. 2017 Nov;27((11)):1341–6. doi: 10.1089/thy.2017.0500. [DOI] [PubMed] [Google Scholar]
- 15.Grani G, Lamartina L, Cantisani V, Maranghi M, Lucia P, Durante C. Interobserver agreement of various thyroid imaging reporting and data systems. Endocr Connect. 2018 Jan;7((1)):1–7. doi: 10.1530/EC-17-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grani G, D'Alessandri M, Carbotta G, Nesca A, Del Sordo M, Alessandrini S, et al. Grey-Scale Analysis Improves the Ultrasonographic Evaluation of Thyroid Nodules. Medicine (Baltimore) 2015 Jul;94((27)):e1129. doi: 10.1097/MD.0000000000001129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grani G, Lamartina L, Ascoli V, Bosco D, Nardi F, D'Ambrosio F, et al. Ultrasonography scoring systems can rule out malignancy in cytologically indeterminate thyroid nodules. Endocrine. 2017 Aug;57((2)):256–61. doi: 10.1007/s12020-016-1148-6. [DOI] [PubMed] [Google Scholar]
- 18.Grani G, Lamartina L, Ascoli V, Bosco D, Biffoni M, Giacomelli L, et al. Reducing the Number of Unnecessary Thyroid Biopsies While Improving Diagnostic Accuracy: toward the “Right” TIRADS. J Clin Endocrinol Metab. 2019 Jan;104((1)):95–102. doi: 10.1210/jc.2018-01674. [DOI] [PubMed] [Google Scholar]
- 19.Ramundo V, Lamartina L, Falcone R, Ciotti L, Lomonaco C, Biffoni M, et al. Is thyroid nodule location associated with malignancy risk? Ultrasonography. 2019 Jul;38((3)):231–5. doi: 10.14366/usg.18050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trajman A, Luiz RR. McNemar chi2 test revisited: comparing sensitivity and specificity of diagnostic examinations. Scand J Clin Lab Invest. 2008;68((1)):77–80. doi: 10.1080/00365510701666031. [DOI] [PubMed] [Google Scholar]
- 21.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988 Sep;44((3)):837–45. [PubMed] [Google Scholar]
- 22.Goksuluk D, Korkmaz S, Zararsiz G, Karaagaoglu AE. easyROC: An Interactive Web-tool for ROC Curve Analysis Using R Language Environment. R J. 2016;8((2)):213–30. [Google Scholar]
- 23.Lamartina L, Deandreis D, Durante C, Filetti S. ENDOCRINE TUMOURS: Imaging in the follow-up of differentiated thyroid cancer: current evidence and future perspectives for a risk-adapted approach. Eur J Endocrinol. 2016 Nov;175((5)):R185–202. doi: 10.1530/EJE-16-0088. [DOI] [PubMed] [Google Scholar]
- 24.Middleton WD, Teefey SA, Reading CC, Langer JE, Beland MD, Szabunio MM, et al. Multiinstitutional Analysis of Thyroid Nodule Risk Stratification Using the American College of Radiology Thyroid Imaging Reporting and Data System. AJR Am J Roentgenol. 2017 Jun;208((6)):1331–41. doi: 10.2214/AJR.16.17613. [DOI] [PubMed] [Google Scholar]
- 25.Ha EJ, Moon WJ, Na DG, Lee YH, Choi N, Kim SJ, et al. A Multicenter Prospective Validation Study for the Korean Thyroid Imaging Reporting and Data System in Patients with Thyroid Nodules. Korean J Radiol. 2016 Sep-Oct;17((5)):811–21. doi: 10.3348/kjr.2016.17.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nam SJ, Kwak JY, Moon HJ, Yoon JH, Kim EK, Koo JS. Large (≥3cm) thyroid nodules with benign cytology: Can Thyroid Imaging Reporting and Data System (TIRADS) help predict false-negative cytology? PLoS One. 2017 Oct;12((10)):e0186242. doi: 10.1371/journal.pone.0186242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mendes GF, Garcia MR, Falsarella PM, Rahal A, Cavalcante Junior FA, Nery DR, et al. Fine needle aspiration biopsy of thyroid nodule smaller than 1.0 cm: accuracy of TIRADS classification system in more than 1000 nodules. Br J Radiol. 2018 Feb;91((1083)):20170642. doi: 10.1259/bjr.20170642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng Y, Xu S, Kang H, Zhan W. A Single-Center Retrospective Validation Study of the American College of Radiology Thyroid Imaging Reporting and Data System. Ultrasound Q. 2018 Jun;34((2)):77–83. doi: 10.1097/RUQ.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 29.Koseoglu Atilla FD, Ozgen Saydam B, Erarslan NA, Diniz Unlu AG, Yilmaz Yasar H, Ozer M, et al. Does the ACR TI-RADS scoring allow us to safely avoid unnecessary thyroid biopsy? single center analysis in a large cohort. Endocrine. 2018 Sep;61((3)):398–402. doi: 10.1007/s12020-018-1620-6. [DOI] [PubMed] [Google Scholar]
- 30.Hoang JK, Middleton WD, Farjat AE, Langer JE, Reading CC, Teefey SA, et al. Reduction in Thyroid Nodule Biopsies and Improved Accuracy with American College of Radiology Thyroid Imaging Reporting and Data System. Radiology. 2018 Apr;287((1)):185–93. doi: 10.1148/radiol.2018172572. [DOI] [PubMed] [Google Scholar]
- 31.Yoon JH, Lee HS, Kim EK, Moon HJ, Kwak JY. Malignancy Risk Stratification of Thyroid Nodules: Comparison between the Thyroid Imaging Reporting and Data System and the 2014 American Thyroid Association Management Guidelines. Radiology. 2016 Mar;278((3)):917–24. doi: 10.1148/radiol.2015150056. [DOI] [PubMed] [Google Scholar]
- 32.Persichetti A, Di Stasio E, Guglielmi R, Bizzarri G, Taccogna S, Misischi I, et al. Predictive Value of Malignancy of Thyroid Nodule Ultrasound Classification Systems: A Prospective Study. J Clin Endocrinol Metab. 2018 Apr;103((4)):1359–68. doi: 10.1210/jc.2017-01708. [DOI] [PubMed] [Google Scholar]
- 33.Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002 Mar;178((3)):687–91. doi: 10.2214/ajr.178.3.1780687. [DOI] [PubMed] [Google Scholar]
- 34.Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS. The Diagnosis and Management of Thyroid Nodules: A Review. JAMA. 2018 Mar;319((9)):914–24. doi: 10.1001/jama.2018.0898. [DOI] [PubMed] [Google Scholar]
- 35.Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW. The Bethesda System for Reporting Thyroid Cytopathology: a meta-analysis. Acta Cytol. 2012;56((4)):333–9. doi: 10.1159/000339959. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data
Supplementary data
Supplementary data