Abstract
We report a large subconjunctival-orbital granuloma in a 51-year-old male presenting with a blind painful right eye and marked chemosis 15 months after undergoing vitrectomy and silicone oil retinal tamponade for retinal detachment with no reported intraoperative complications. Gross and histopathologic examination of the enucleated eye and episcleral tumor revealed a bosselated mass measuring 17 × 10 × 5 mm containing prominent vacuoles with surrounding epithelioid histiocytes and foreign body multinucleated giant cells. Such a large silicone-induced orbital granuloma following uncomplicated retinal surgery in a grossly intact eye has not been previously reported to the authors' knowledge. High intraocular pressure and emulsification of oil may facilitate silicone extravasation through scleral wounds after retinal surgery.
Keywords: Silicone-induced orbital granuloma, Scanning electron microscope-energy dispersive spectroscopy, Case report
Established Facts
Intravitreal silicone oil can migrate or extravasate out of the eye.
Silicone oil can incite a granulomatous inflammatory response.
Novel Insights
The size and appearance of a subconjunctival-orbital silicone oil granuloma can mimic malignancy. A history of silicone oil injection may be relevant when evaluating orbital masses.
In addition to light microscopy, scanning electron microscope-energy dispersive spectroscopy confirmed that silicone oil was present in the patient's mass.
Introduction
Intravitreal silicone oil tamponade is often employed for patients with complex retinal detachments. Large orbital lipogranulomas masquerading as lymphoid lesions or neoplasms have developed following corticosteroid injections, the use of paraffin-containing ointment plugs in sinus surgery, and after trauma to the eye [1, 2]. In the case of silicone oil used for retinal tamponade, mostly small to moderate extraocular granulomas have been reported [3, 4]. However, Couch et al. [3] have described a large posterior orbital silicone oil granuloma found incidentally during enucleation. Additionally, a subconjunctival silicone granuloma in the setting of endophthalmitis with a scleral melt has been recently reported. It was notably larger than another silicone granuloma that developed secondary to silicone oil leakage through an Ahmed glaucoma drainage device [4]. To the authors' knowledge, a silicone oil-induced granuloma presenting as a large orbital tumor-like mass on external examination has not been described in the presence of a grossly intact scleral wall.
Case Report and Results
A 51-year-old white male with diabetes mellitus and renal failure requiring hemodialysis presented 15 months after undergoing right eye pars plana vitrectomy, membrane peel, endolaser, and silicone oil tamponade, performed elsewhere, for a tractional retinal detachment. He complained of a blind and painful right eye as well as a large mass tensing the right orbit, but could not date the onset. A large smooth, pale subconjunctival mass was evident in the superior lateral and nasal orbital areas associated with marked chemosis (Fig. 1). The mass restricted abduction and supraduction of the eye. B-scan ultrasonography revealed that the mass extended posteriorly to the mid-orbit. Visual acuity in the right eye was no light perception. Examination demonstrated a relative afferent pupillary defect in the right eye. Intraocular pressure was 22 mm Hg. Other findings included diffuse 3+ injection of the bulbar conjunctiva and neovascularization of the right corneal stroma along the inferior edge of the mass.
Fig. 1.

Clinical presentation. The patient presented with a large mass in the right superior lateral orbit 15 months after right eye retinal detachment repair with silicone oil tamponade. Abduction and supraduction of the blind and painful eye were severely restricted.
The patient underwent a right transconjunctival tumor excision and concomitant enucleation of his blind and painful eye. The tumor was dissected free of the orbital tissues temporally to the level of the globe equator. During surgery, examination revealed orbital tumor abutting thinned sclera. On deeper surgical dissection to the level of the orbital apex, silicone oil was encountered that evidently leaked from the globe. After oil was removed from the orbit, the eye was enucleated en-bloc with the attached tumor and sent for pathology analysis. Gross examination in the pathology laboratory after formalin fixation revealed a firm, gray tumor adherent to the sclera temporally. The unencapsulated mass measured approximately 17 × 10 × 5 mm. The tumor attached to the globe was divided with a sharp blade leaving approximately a third of the mass attached to the sclera to allow placement of the globe and a portion of the tumor on separate standard-width (75 × 25 mm) microscope slides. Representative sections of the separated tumor and horizontal sections of the globe were submitted for routine paraffin processing. Microscopy revealed that the tumor was tightly bound to the sclera and consisted of variably sized vacuoles that were predominantly spherical and coalescent in several areas. These vacuoles were lined by connective tissue containing epithelioid histiocytes including several foreign body multinucleated giant cells, some containing presumed phagocytosed oil droplets and pigment granules (Fig. 2). Most of the vacuoles were empty, typical for silicone oil, which is often lost in processing of standard tissue sections [5]. Collections of round cells including many plasma cells and lymphocytes surrounded a number of vacuoles. Some large vessels containing red cells were present in intervacuolar tissues.
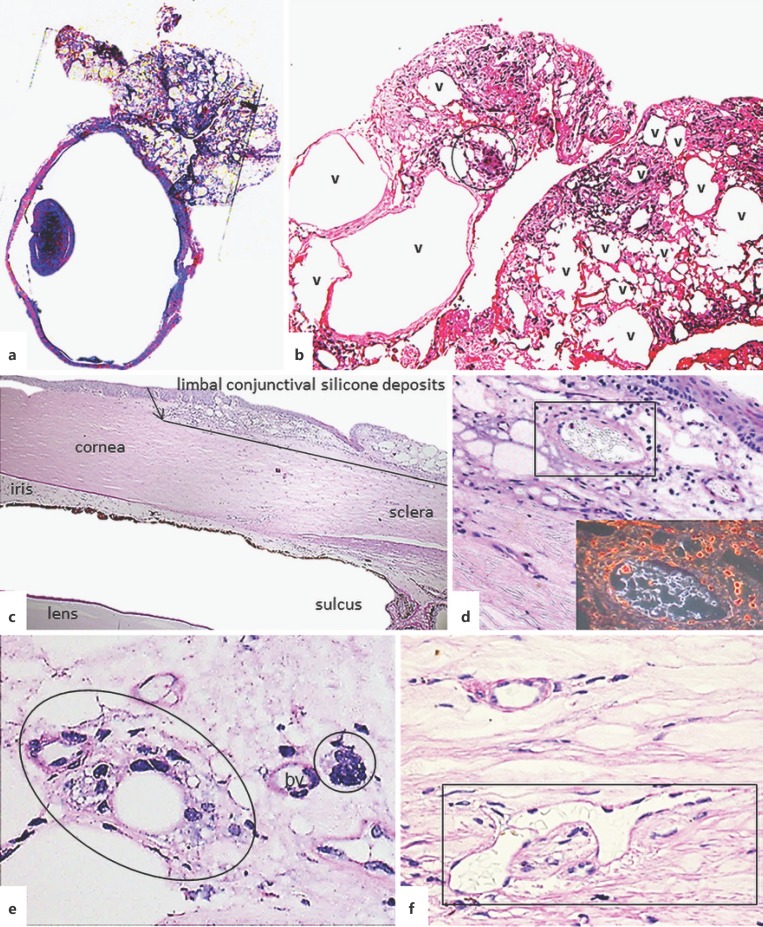
Fig. 2.
Histopathologic features of the enucleated eye showing extra- and intraocular granulomatous inflammation due to silicone. a Relationship of orbital mass adherent to intact sclera. Periodic Acid-Schiff, whole slide image. b Orbital tissue with granulomatous reaction (circled) to silicone deposits in the variably sized vacuoles (v), now empty due to processing. Hematoxylin-eosin. Original magnification, ×125. c–f Intraocular tissue deposits of silicone. c Silicone deposits in the limbal conjunctiva as well as angle closure (other structures are labeled for orientation). Periodic Acid-Schiff. Original magnification, ×40. d Subepithelial conjunctiva shows retained refractile silicone in several vacuoles shown best by dark-field illumination (inset). Periodic Acid-Schiff. Original magnification, ×200. e Silicone phagocytosed by macrophage giant cells (circled). bv, blood vessel. Periodic Acid-Schiff. ×400. f Refractile silicone in Schlemm's canal (in rectangle). Periodic Acid-Schiff. ×400.
Scanning electron microscopy with energy dispersive X-ray spectroscopy (SEM-EDS) of the tissue in situin the paraffin block was done, which allowed examination of the vacuolar contents, which had been lost in further processing. SEM-EDS confirmed the presence of the element silicon in some of the vacuoles (Fig. 3). EDS identifies elements but cannot identify compounds. Thus, the findings by light microscopy plus the demonstration of the element silicon supports the identification of the deposits as silicone [5]. The mass was diagnosed as a benign silicone oil granuloma.
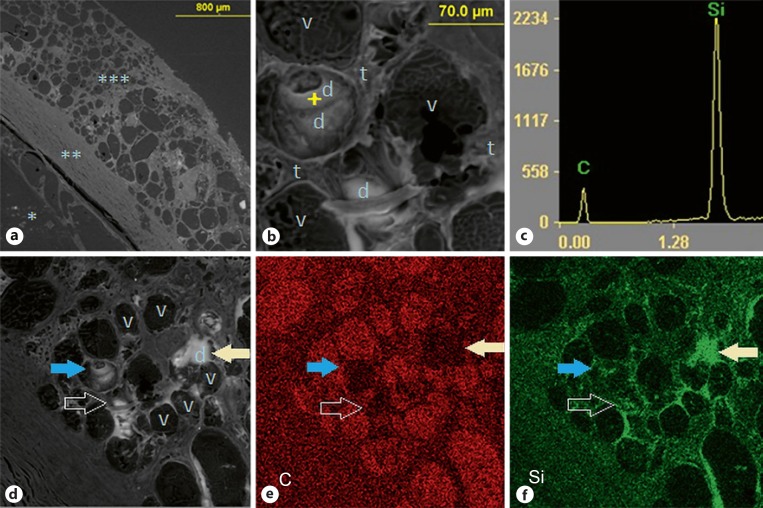
Fig. 3.
SEM-EDS images (backscattered electron images; brightness depends on average atomic number of tissue). a Low-power section, labeled * vitreous cavity, ** sclera, *** limbal-episcleral nodule, or an extension of a larger mass, with variably sized vacuoles. b A high-power section of the limbal-episcleral nodule showing scattered deposits, one of which (indicated by the “+” sign) was analyzed by EDS. The tissue components are labeled as follows: v, vacuoles (mostly empty); t, intervacuolar tissue; d, deposits. c EDS spectrum of the deposit indicated in b, showing a prominent silicon (Si) peak relative to the carbon (C) peak from the paraffin substrate. d Lower magnification of the area shown in b that reveals further deposits (d, brighter white) as well as empty vacuoles (v). e, f EDS distribution maps for carbon (C, shown in red) and silicon (Si, shown in green), which confirm the spatial distribution of silicon in (brighter) deposits and to a lesser degree in intervacuolar tissue, and absence in empty vacuoles, where carbon from the paraffin substrate is the major finding. The matching arrows point to corresponding areas in images d–f.
Other notable findings included encasement of the inferior oblique muscle belly anterior nasally by an extension of the mass and probable granuloma interference with the superior oblique between the trochlea and its posterior insertion on the globe. The pathology examination could not precisely explain the motility disorder but, given that there were conjunctival bulges nasally and temporally, simple mass effect may have contributed to his motility deficits.
A presumed inadvertent intraoperative perforation was present superiorly although no leaking fluid was noted at gross examination even by tensing the globe. There was a staphyloma at 12 o'clock, just nasal to the mass. However, there were small vacuoles or bubbles within the temporal mid- and peripherally degenerated retina, presumably from incorporated silicone oil droplets. No multinucleated giant cells were seen within the retina or choroid. Histopathology also revealed peripheral anterior synechiae-induced angle closure (Fig. 2) and a cupped optic nerve, suggesting that both his vision loss and pain may have stemmed from secondary glaucoma.
Discussion/Conclusion
To the authors' knowledge, this is the first report of such a massive orbital silicone oil-induced granuloma without an obvious communication between the intraocular and extraocular space. It restricted extraocular movements due to its size and perhaps also due to extraocular muscle impairment. Like other granulomas described previously, this presentation initially raised concerns of malignancy [1, 2].
The histology of silicone oil-induced granulomas is characterized by nonbirefringent, variably sized round vacuoles that are often empty in routine histology paraffin sections, accompanied by histiocytes and multinucleated giant cells containing intracytoplasmic microvacuoles [6].
Silicone oil does not consistently provoke an immune reaction, and multinucleated giant cells have not always been present in silicone granulomas [7, 8]. Enhanced binding of serum IgG to silicone has been postulated to correlate with an exaggerated immune response and postoperative complications [9]. However, Shaikh et al. [10] did not find such an association. Only one patient with a connective tissue disorder exhibited significant IgG binding levels and scleral buckle extrusion. IgG levels in the current patient were not obtained as no indications of an autoimmune disease were present. Silicone oil migration does not appear to depend on the length of time silicone oil is in the eye [7], and migration out of the eye is uncommon. Federman and Schubert [11] reported a 2.7% incidence of extravasation of oil into the subconjunctival space that is usually through sclerotomy sites. Fortunately, silicone oil leak is uncommon as a complication of retinal surgery involving instillation of oil, and is most likely due to inadequate wound closure. In this case, the silicone oil could have migrated through the superior staphyloma. Risk factors for staphyloma, including scleritis, infectious processes, or connective tissue disorders, could not be definitely excluded in our patient. The patient did not have severe myopia. As described by Robertson [12], a staphyloma present at the time of retinal detachment surgery may require reinforcement.
The superior staphylomatous sclera, elevated intraocular pressure, and possible emulsification of oil may all have contributed to migration of silicone oil to the orbit in our patient. Time (15 months) may have allowed the mass in our patient to expand markedly. It is unclear why the silicone oil did not diffuse and instead developed into a solid mass. Cases of silicone oil migrating to the eyelid, a reasonable end of a forward path, occurred between 12 months and 19 years following silicone oil injection [4].
The mass in our case is similar to that which developed in an eye that underwent pars plana vitrectomy and silicone oil tamponade for severe endogenous Klebsiella endophthalmitis and underwent evisceration. However, unlike our case, there was an obvious path for silicone oil extrusion through an area of scleral melting [4].
In conclusion, this report of an orbital and periocular silicone oil-induced granuloma, presenting as a superior, temporal, and nasal externally evident, subconjunctival tumor, adds one additional scenario to the list of complications of silicone oil injection.
Statement of Ethics
The authors have no ethical conflicts to declare. University of California, Irvine (UCI) does not require IRB approval for a single clinicopathologic case report. This study adhered to the principles of the Declaration of Helsinki and was HIPAA compliant.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research was supported by an unrestricted RPB grant to the Departments of Ophthalmology at UCI and SUNY Upstate, by the SUNY Upstate Department of Pathology, and also by the Lions District 20-Y1 for the Department of Ophthalmology at SUNY Upstate.
Author Contributions
All authors made significant contributions to this paper according to the ICMJE Criteria for Authorship:
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and
Drafting the work or revising it critically for important intellectual content; and
Final approval of the version to be published; and
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
The authors wish to thank Angele Nalbandian, PhD, for assistance in the preparation of the manuscript.
References
- 1.Abel AD, Carlson JA, Bakri S, Meyer DR. Sclerosing lipogranuloma of the orbit after periocular steroid injection. Ophthalmology. 2003 Sep;110((9)):1841–5. doi: 10.1016/S0161-6420(03)00560-8. [DOI] [PubMed] [Google Scholar]
- 2.Davies GB, Wong PL. Sclerosing lipo-granuloma in the orbit. Br J Ophthalmol. 1958 Nov;42((11)):697–701. doi: 10.1136/bjo.42.11.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Couch SM, Harocopos GJ, Holds JB. Orbital silicone oil granuloma discovered during enucleation. Arch Ophthalmol. 2012 Aug;130((8)):1083–5. doi: 10.1001/archophthalmol.2012.287. [DOI] [PubMed] [Google Scholar]
- 4.Lee JH, Kim YD, Woo KI, Kong M. Subconjunctival and orbital silicone oil granuloma (siliconoma) complicating intravitreal silicone oil tamponade. Case Rep Ophthalmol Med. 2014;2014:686973. doi: 10.1155/2014/686973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Travis WD, Balogh K, Abraham JL. Silicone granulomas. A review of the literature and report of 3 cases. Hum Pathol. 1985;16:19–27. doi: 10.1016/s0046-8177(85)80209-4. [DOI] [PubMed] [Google Scholar]
- 6.Requena C, Izquierdo MJ, Navarro M, Martínez A, Vilata JJ, Botella R, et al. Adverse reactions to injectable aesthetic microimplants. Am J Dermatopathol. 2001 Jun;23((3)):197–202. doi: 10.1097/00000372-200106000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Biswas J, Verma A, Davda MD, Ahuja S, Pushparaj V. Intraocular tissue migration of silicone oil after silicone oil tamponade: a histopathological study of enucleated silicone oil-filled eyes. Indian J Ophthalmol. 2008 Sep-Oct;56((5)):425–8. doi: 10.4103/0301-4738.42425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budde M, Cursiefen C, Holbach LM, Naumann GO. Silicone oil-associated optic nerve degeneration. Am J Ophthalmol. 2001 Mar;131((3)):392–4. doi: 10.1016/s0002-9394(00)00800-x. [DOI] [PubMed] [Google Scholar]
- 9.Shaikh S, Egbert PR, Goldblum RS, Wieland MR. Granulomatous local cell reaction to intravitreal silicone. Arch Ophthalmol. 2000 Aug;118((8)):1133–4. [PubMed] [Google Scholar]
- 10.Shaikh S, Morse LS, Goldblum RM, Benner JD, Burnett H, Caspar J. The effect of silicone ocular surgical devices on serum IgG binding to silicones. Am J Ophthalmol. 1998 Dec;126((6)):798–804. doi: 10.1016/s0002-9394(98)00282-7. [DOI] [PubMed] [Google Scholar]
- 11.Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988 Jul;95((7)):870–876. doi: 10.1016/s0161-6420(88)33080-0. [DOI] [PubMed] [Google Scholar]
- 12.Robertson DM. Retinal detachment with equatorial staphyloma. Arch Ophthalmol. 1996 Apr;114((4)):496–7. doi: 10.1001/archopht.1996.01100130492032. [DOI] [PubMed] [Google Scholar]