Abstract
Background
Clinical trials have indicated some traditional Chinese medicine formulas reduce airway hyperresponsiveness and relieve asthma symptoms. This study investigated Chinese herbal Medicine (CHM) for childhood asthma and clarified the relationship between CHM use and consequent asthma hospitalization by a population-based cohort study.
Methods
We used the data of one million individuals randomly selected from Registry of Beneficiaries of the National Health Insurance Research Database. Patients aged less than 18 years and diagnosed as asthma were followed from 2000 to 2012 and divided into the CHM group and the non-CHM group. Cox proportional hazard regression model was conducted to estimate the adjusted hazard ratio (aHR) of the two groups, and the Kaplan-Meier survival curve was used to determine the association between CHM cumulative days and consequent asthma hospitalization.
Results
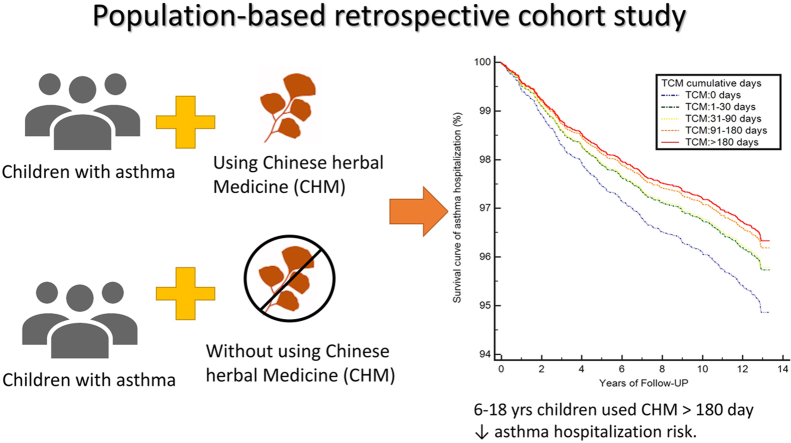
Of the total of 33,865 patients, 14,783 (43.6%) were included in the CHM group, and 19,082 (56.4%) were included in the non-CHM group. After adjustment for gender, age, comorbidities, and total numbers of asthma medication, CHM users had a lower risk of asthma hospitalization than non-CHM users (aHR: 0.90, 95% confidence interval [CI]: 0.83–0.95). Children older than 6 years who used CHM therapy for more than 180 days exhibited a reduction of 29% for the risk of consequent asthma hospitalization (aHR: 0.71, 95% CI: 0.51–0.98).
Conclusion
Children aged 6–18 years who used more than 6 months CHM therapy reduced the risk of consequent asthma hospitalization. Long-term CHM therapy has benefit in school-age children with asthma.
Keywords: Asthma, Childhood asthma, Traditional Chinese medicine, Chinese herbal medicine, National health insurance research database (NHIRD)
Graphical abstract
1. Introduction
Asthma is a common respiratory diseases worldwide and is the leading cause of repetitive or prolonged cough, wheezing even shortness of breath in children. According to the national statistics in Taiwan, the prevalence of childhood asthma has increased each year. One study reported that the 8 years asthma prevalence in children and adolescents in 2000–2007 was 15.7%,1 another reported that the childhood asthma prevalence was from 12.99% in 2002 to 16.86% in 2008, and the rate was still up to 15–20% in recent years.2 Besides, asthma is a major cause of hospital outpatients visits and health-care expenditure in children, resulting in 2.2–fold higher than non-asthmatic children.3 Despite considerable improvement of asthma medications and the management strategy of health education, the prevalence and healthcare burden of asthma still appear to be increasing.4 According to the Global Initiative for Asthma (GINA) guidelines, conventional antiasthmatic drugs, including controllers and relievers, are the standard treatment for asthma.5 Antiasthmatic drugs have been the predominant treatment for childhood asthma for many years; however, parents of some children with asthma have opted for other types of therapy such as complementary and alternative therapies because of concerning the side effect of the corticosteroids.6 Among these treatments, the most common alternative or complementary therapies for childhood asthma are traditional Chinese medicine (TCM) therapies such as Chinese herbal medicine (CHM) and acupuncture.6,7 Clinical trials have indicated that some CHM formulas reduce airway hyperresponsiveness and relieve asthma symptoms.8, 9, 10 However, insufficient evidence is available for the beneficial effects of long-term use of CHM for childhood asthma.11
The National Health Insurance (NHI) programme of Taiwan established in 1996, provides comprehensive health insurance to all residents of Taiwan. The claims data of the enrolees of the NHI programme collected over 20 years are compiled in the National Health Insurance Research Database (NHIRD), which serves as a valuable research resource.12 In particular, TCM therapy is covered by the NHI programme of Taiwan, which is the only country worldwide that possesses a large amount of TCM medical records for more than 20 million people.13,14 To date, some descriptive studies have used the NHIRD to analyse the utilization of TCM for childhood asthma and have investigated the characteristics of TCM users and the most commonly prescribed CHM formulas and single herbs.15, 16, 17, 18 However, there is still no large-scale study evaluating the long-term efficacy of CHM on childhood asthma. The aim of the study is to investigate CHM therapy for childhood asthma and clarify the relationship between CHM use and consequent asthma hospitalization.
2. Material and methods
2.1. Study design and data resource
This retrospective cohort study was conducted using the Longitudinal Health Insurance Database 2005 (LHID 2005), a data of NHIRD released from the National Health Research Institutes. LHID2005 is a medical data of one million people randomly sampled from all of the insurance population in Taiwan, and the National Health Research Institutes claimed there is no significant difference in age or gender between the sample in the LHID database and the original insured population.19 LHID 2005 contained patients' data and medical records, including patients’ gender, birthdate, insured region, date of service, diagnosis, medication, treatment, expenditures, date of outpatient department (OPD) visit, date of emergency department visit, and date of hospitalization from 2000 to 2012.19 From 1996 to the present day, the coverage of NHI is up to 99.6% of total population. All the identification numbers are encrypted to protect patient privacy, and the study protocol was approved by the Institutional Review Board of Taipei City Hospital, Taiwan (Case Number TCHIRB-10512111-E).
2.2. Study population
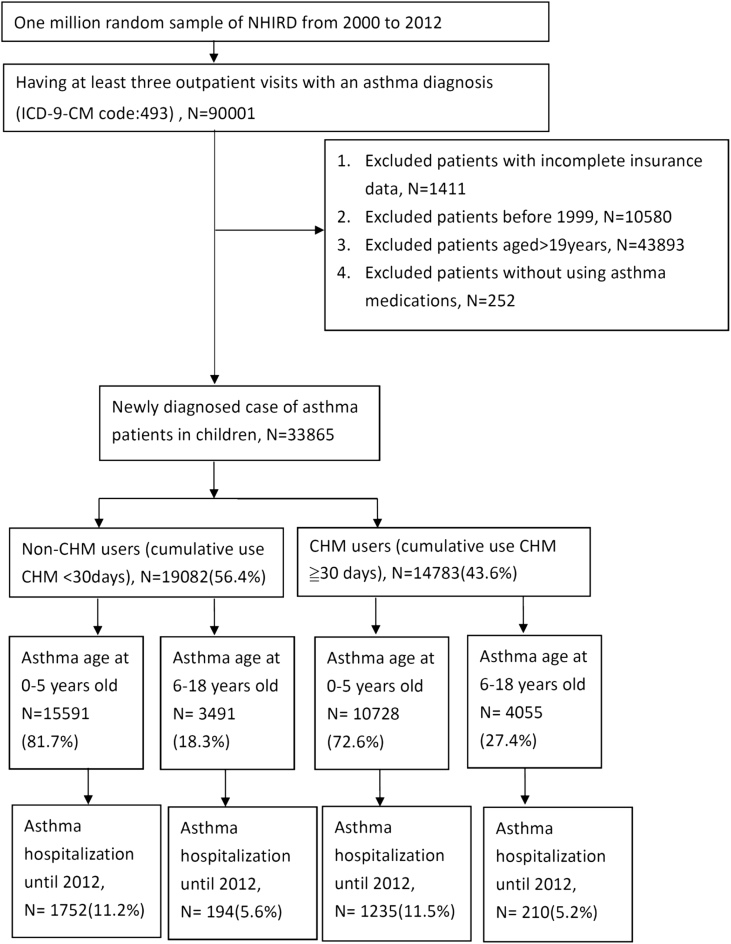
This retrospective cohort study used the LHID2005 without any randomization, all the study population were detailed in Fig. 1. In this study, the inclusion criteria were children aged less than 18 years who were diagnosed with asthma (identified using the International Classification of Disease, Ninth Revision, Clinical Modification [ICD-9-CM] code 493) and those with more than three OPD visits. To ensure that all children were newly diagnosed with asthma, those without complete insurance data (n = 1411) and those diagnosed with asthma before the end of 1999 (n = 10,580) were excluded. Moreover, to ensure that all patients had asthma, those without any antiasthmatic medication prescription record (n = 252) were excluded. The antiasthmatic medications recommended in the GINA guidelines, including controllers (inhaled corticosteroids, long-acting β2 agonist, mast-cell stabiliser, antileukotriene, anti-IgE monoclonal antibody) and relievers (short-acting β2 agonist and short-acting anticholinergics).
Fig. 1.
Flow chart of recruitment of subjects from the one million individuals randomly sampled from the National Health Insurance Research Database (NHIRD) from 2000 to 2012 in Taiwan.
2.3. CHM exposure and follow-up period
A total of 33,865 children met the inclusion criteria and were divided into two groups by the medical records of CHM use: the CHM group (CHM use for more than 30 cumulative days) and the non-CHM (CHM use for less than 30 cumulative days or no CHM use). In Taiwan, the CHM prescriptions reimbursed by the NHI programme only include TCM formulas or single herb in a concentrated powder or granule form.7
In the present study, we included all eligible patients in the LHID for analysis without any sampling; besides, our study also used an intent-to-treat analysis method that we fixed the group according to the patient's treatment, and no patient will change during the tracking period. Patients were followed from the first date of asthma diagnosis to the first asthma hospitalization or the last medical records before December 31, 2012. Asthma hospitalization was defined by the identification of the ICD-9-CM code 493 in the admission diagnosis record. For each patient, we calculated the exposure of CHM during the follow-up period. And we also stratified the study population into 0–5 years and 6–18 years old to distinguish preschool age children from school age children. The study design and flow chart are illustrated in Fig. 1.
2.4. Study variables
Demographic characteristics, including gender, age, and insured region, of children with asthma in the two groups were demonstrated based on previous studies.5 GINA published guidelines addressing the treatment of asthma in children younger than 5 years, and previous studies have reported that the pathogenesis of early childhood asthma is different from that of later childhood asthma.20,21 Therefore, the children in this study were stratified into the age groups of 0–5 years and 6–18 years old. The insured region was categorised into seven administrative areas, namely Taipei City, Kaohsiung City, Northern Taiwan, Central Taiwan, Eastern Taiwan, Southern Taiwan, and outlying islands. Each region, which represent the living area of the patients, has different geographical environment and air quality. The type of antiasthmatic drug and comorbidities were also identified in our study. The GINA guidelines recommend stepwise treatment as the standard treatment for asthma, which implies that more types of antiasthmatic drugs should be prescribed for more severe asthma.22 In our study, the total number of antiasthmatic drugs represents asthma severity. Furthermore, the comorbidities that often accompany asthma, including allergic rhinitis, bronchitis, acute sinusitis, atopic dermatitis, gastroesophageal reflux disease, and urticaria, were also identified using the ICD-9-CM code and were listed as our variables in our analyses.23, 24, 25
2.5. Statistical analyses
The demographic characteristics of CHM users and non-CHM users were analysed using a logistic regression model to estimate the adjusted odds ratio (aOR). The frequency distribution of TCM OPD visits (identified using the ICD-9-CM code) of children with asthma was analysed, and the frequency of visits for CHM therapy and acupuncture/manipulation therapy were calculated separately in Table 2. The most commonly prescribed TCM formula and the average dosage for children with asthma were estimated, and the average dose of Ma-Huang (Ephedrae herba) in CHM by person-day was also calculated in our study (Table 3). A Cox proportional regression model was used to estimate adjusted hazard ratio (aHR) with 95% confidence interval (95% CI) to determine the different risk factors for asthma hospitalization (Table 5).
Table 2.
Frequency distribution of traditional Chinese medicine OPD visits by major disease (ICD-9-CM code) in children with asthma from 2000 to 2012.
| Major Disease Category | Icd-9 Code Range | Number of Visits (%) |
||
|---|---|---|---|---|
| Chinese Herbal Medicine Therapies | Acupuncture, or Manipulative Therapies | Total of CHM | ||
| Infectious and Parasitic Diseases | 001–139 | 311 (0.07) | 1 (0.00) | 312 (0.06) |
| Neoplasms | 140–239 | 429 (0.1) | 5 (0.01) | 434 (0.09) |
| Endocrine, Nutritional, Blood and Metabolic Diseases, and Immunity Disorders |
240–289 | 2166 (0.5) | 34 (0.07) | 2200 (0.43) |
| Mental Disorders, Diseases of The Nervous System and Sense Organs | 290–389 | 5968 (1.3) | 767 (1.6) | 6735 (1.32) |
| Diseases of The Circulatory System | 390–459 | 877 (0.2) | 99 (0.2) | 976 (0.19) |
| Diseases of The Respiratory System | 460–519 | 258,557 (56.0) | 502 (1.0) | 259,059 (50.8) |
| Diseases of The Digestive System | 520–579 | 45,207 (9.8) | 84 (0.2) | 45,291 (8.9) |
| Diseases of The Genitourinary System | 580–679 | 17,871 (3.9) | 26 (0.05) | 17,897 (3.5) |
| Diseases of The Skin And Subcutaneous Tissue | 680–709 | 22,903 (5.0) | 67 (0.1) | 22,970 (4.5) |
| Diseases of The Musculoskeletal System and Connective Tissue |
710–739 | 4529 (1.0) | 8200 (17.0) | 12,729 (2.5) |
| Symptoms, Signs, and Ill-Defined Conditions |
780–799 | 100,051 (21.7) | 205 (0.4) | 100,256 (19.7) |
| Injury and Poisoning | 800–999 | 2355 (0.5) | 38,074 (79.1) | 40,429 (7.9) |
| Supplementary Classification | V01—V82, E800-E999 | 11 (0.00) | 0 (0.0) | 11 (0.0) |
| Others | 740–779 | 412 (0.1) | 70 (0.15) | 482 (0.1) |
| Total | 461,647 (90.6) | 48,134 (9.4) | 509,781 (100.0) | |
Table 3.
Most commonly prescribedtraditional Chinese medicine formulas forchildren with asthma in Taiwanfrom 2000 to 2012.
| Herbal formula (Pin-yin name) | Ingredients of herbal formula Pin-yin name (Official name) | N (%) | Average dosage/day | Ma-Huang dose/day |
|---|---|---|---|---|
| Xin-Yi-Qing-Fei-Tang | Xin-Yin (MagnoliaeFlos); Bai-He (LiliiBulbus); Zhi- Mu (AnemarrhenaRhizoma); Shi-Gao(GypsumFibrosum); Pi-Pa-Ye (EriobotryaeFolium); Sheng-Ma (CimicifugaeRhizoma); Mai-men-dong (Ophiopogonis Radix); Zhi-Zi (GardeniaeFructus); Huang-Qin (Scutellariae Radix); Gan-Cao (Glycyrrhizae Radix) | 54034 (6.03) | 2.6 g | |
| Xiao-Qing-Long-Tang | Ma-Huang (EphedraeHerba); Gui-Zhi (CinnamomiRamulus); Bai-Shao (Paeoniae Alba Radix); Gan-Cao (Glycyrrhizae Radix); Gan-Jiang (ZingiberisRhizoma); Xi-Xin (Asari Radix Rhizoma); Ban-Xia (PinelliaeRhizoma); Wu-Wei-Zi (SchisandraeFructus) | 44912 (5.01) | 2.4 g | 0.5 g |
| Ma-Xing-Gan-Shi-Tang | Ma-Huang (EphedraeHerba); Ku-Xing-Ren (ArmeniacaeAmarum Semen); Gan-Cao (Glycyrrhizae Radix); Shi-Gao (GypsumFibrosum) | 37080 (4.14) | 2.8 g | 1.0 g |
| Cang-Er-San | Cang-Er-Zi (XanthiiFructus); Xin-Yin (MagnoliaeFlos); Bai-Zhi (AngelicaeDahuricae Radix); Bo-He (MenthaeHerba) | 36979 (4.13) | 2.5 g | |
| Xin-Yi-San | Xin-Yin (MagnoliaeFlos); Bai-Zhi (AngelicaeDahuricae Radix); Sheng-Ma (CimicifugaeRhizoma); Gao-Ben (LigusticiRhizoma et Radix); Fang-Feng (Saposhnikoviae Radix); ChuanXiong (Chuanxiong Rhizoma); Xi-Xin (Asari Radix et Rhizoma); Chuan-Mu-Tong (Clematidis Caulis); Gan-Cao (Glycyrrhizae Radix) | 35815 (4) | 2.4 g | |
| Yin-Qiao-San | Jin-Yin Hua (LoniceraeFlos); Lian-Qiao (ForsythiaeFructus); Jing-Jie (SchizonepetaeHerba); Dan-Dou-Chi (Sojae Semen Preparatum); Jie-Geng (Platycodi Radix); Bo-He (MenthaeHerba); Niu-Bang-Zi (ArctiiFructus); Gan-Cao (Glycyrrhizae Radix); Dan-Zhu-Ye (Lophatheri Caulis Folium); Lu-Gen (PhragmitisRhizoma) | 25134 (2.81) | 2.8 g | |
| Ge-Gen-Tang | Ge-Gen (Puerariae Radix); Ma-Huang (EphedraeHerba); Gan-Jiang (ZingiberisRhizoma); Gui-Zhi (CinnamomiRamulus); Bai-Shao (Paeoniae Alba Radix); Gan-Cao (Glycyrrhizae Radix); Da-Zao (JujubaeFructus) | 23701 (2.65) | 2.6 g | 0.5 g |
| Xing-Su-San | Zi-Su-Ye (Perillae Folium); Jie-Geng (Platycodi Radix); Da-Zao (JujubaeFructus); Ban-Xia (PinelliaeRhizoma); Zhi-Ke (CitriImmaturusFructus); Ju-Pi (CitriReticulataePericarpium); Fu-Ling (Poria); Gan-Cao (Glycyrrhizae Radix); Ku-Xing-Ren (ArmeniacaeAmarum Semen); Qian-Hu (Peucedani Radix); Gan-Jiang (ZingiberisRhizoma) | 21641 (2.42) | 2.9 g | |
| Zhi-Sou-San | Jie-Geng (Platycodi Radix); Jing-Jie (SchizonepetaeHerba); Zi-Wan (Asteris Radix et Rhizoma); Bai-Bu (Stemonae Radix.); Bai-Qian (CynanchiStauntoniiRhizoma et Radix); Gan-Cao (Glycyrrhizae Radix); Ju-Pi (CitriReticulataePericarpium) | 17960 (2.01) | 2.7 g | |
| Ding-Chuan-Tang | Ma-Huang (EphedraeHerba); Sang-Bai-Pi (Mori Radicis Cortex); Bai-Guo (Ginkgo Semen); Huang-Qin (Scutellariae Radix); Zi-Su-Zi (PerillaeFructus); Ku-Xing-Ren (ArmeniacaeAmarum Semen); Ban-Xia (PinelliaeRhizoma); Kuan-Dong-Hua (FarfaraeFlos); Gan-Cao (Glycyrrhizae Radix) | 17657 (1.97) | 2.7 g | 0.4 g |
Table 5.
Adjusted Cox proportional hazard model analyseswith 95% confidence interval for asthma hospitalization in children with asthma.
| Variables | Adjusted Hazard Ratioa | 95% Confidence Interval | p – Value |
|---|---|---|---|
| Gender | |||
| Males | reference | ||
| Females | 0.90 | 0.84–0.96 | |
| Age at diagnosis | |||
| 0–5 years | reference | ||
| 6–18 years | 0.66 | 0.59–0.74 | <0.0001 |
| Total number of comorbiditiesb | |||
| 1 | reference | ||
| 2 | 0.98 | 0.13–7.49 | |
| 3 | 1.30 | 0.18–9.29 | |
| 4 | 1.29 | 0.18–9.19 | |
| ≧5 | 1.45 | 0.20–10.35 | |
| Total number of asthma medicationc | |||
| 1 | reference | ||
| 2 | 1.70 | 1.04–2.77 | 0.0352 |
| 3 | 3.32 | 2.10–5.27 | <0.0001 |
| 4 | 5.05 | 3.20–7.95 | <0.0001 |
| ≧5 | 10.37 | 6.57–16.35 | <0.0001 |
| CHM usage | |||
| No(<30 days) | reference | ||
| Yes(≧30 days) | 0.90 | 0.83–0.95 | 0.0048 |
Abbreviations: CHM, Chinese herbal medicine.
adjusting all listed variables.
Comorbidities including:allergic rhinitis, acute upper respiratory infection, acute bronchitis, acute sinusitis, atopicdermatitis, gastroesophageal reflux disease, urticaria.
Asthma medication including:short-acting β2 agonists, short-acting anticholinergics, inhaled glucocorticosteroids,long-acting β2 agonists, antileukotriene, mast-cell stabilizers, anti-IgE monoclonal antibody.
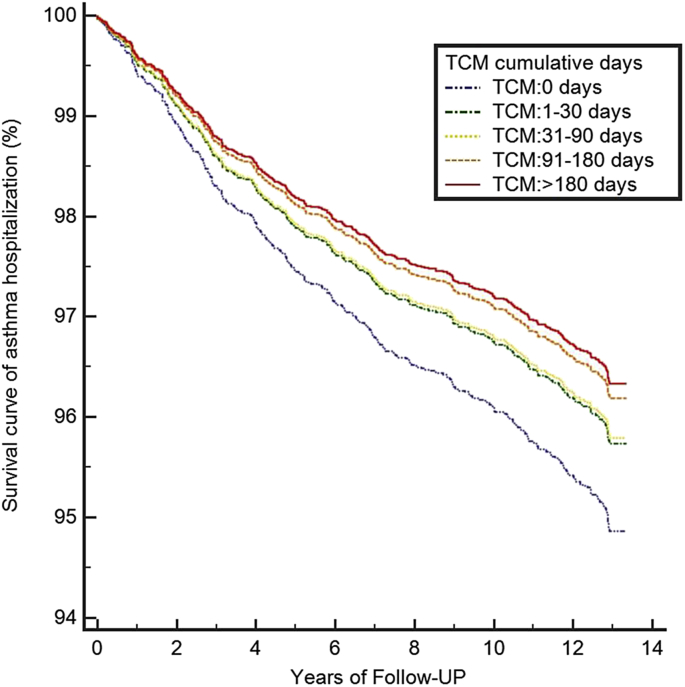
To examine the relationship between CHM use and asthma hospitalization, the cumulative days for which children with asthma were prescribed CHM were stratified into 0 days, 1–30 days, 31–90 days, 91–180, and >180 days to analyse the dose–response effect (Table 6). All statistical analyses were performed using SAS, version 9.4(SAS Institute Inc., Cary, NC, USA). P < 0.05 was considered statistically significant and calculated against 95% CIs.
Table 6.
Number of asthma hospitalization cases, population-at-risk, and adjusted hazard ratios and 95% confidence intervals for asthma hospitalization estimated according to different CHM cumulative days in children with asthma.
| Variables | No. Case/population | Adjusted Hazard Ratioa | 95% CI | p – Value |
|---|---|---|---|---|
| 0–5 years (N = 26,319) | ||||
| CHM usage (days) | ||||
| 0 | 947/8831 | reference | ||
| 1-30 | 637/5331 | 1.04 | 0.94–1.15 | |
| 31-90 | 583/5161 | 0.93 | 0.84–1.04 | |
| 91-180 | 358/3008 | 0.98 | 0.87–1.11 | |
| >180 | 462/3988 | 0.93 | 0.83–1.04 | |
| 6–18 years (N = 7546) | ||||
| CHM usage (days) | ||||
| 0 | 86/1447 | reference | ||
| 1-30 | 84/1600 | 0.83 | 0.62–1.13 | |
| 31-90 | 107/1958 | 0.82 | 0.62–1.09 | |
| 91-180 | 59/1177 | 0.74 | 0.53–1.03 | |
| >180 | 68/1364 | 0.71 | 0.51–0.98 | 0.000149 |
Abbreviations: CHM, Chinese herbal medicine.
Adjusting gender, comorbidity, and asthma medication.
3. Results
In the descriptive statistical analysis (Table 1), of the total of 33,865 patients, 14,783 (43.6%) were included in the CHM group, and 19,082 (56.4%) were included in the non-CHM group. The demographic characteristics indicated that CHM users tended to be female, >6 years of age, and living in Central Taiwan, Southern Taiwan, and Kaohsiung City in comparison with non-CHM users. Regarding asthma medication use, CHM users tended to use more types of conventional antiasthmatic drugs in comparison with non-CHM users. The proportion of the CHM group that used more than five types of asthma medication was 1.65-fold higher than that of the non-CHM group (aOR: 1.65, 95% CI: 1.44–1.90). CHM users also exhibited more comorbidities than non-CHM users. The proportion of CHM users with more than five comorbidities was 6.73-fold higher than that of non-CHM users (aOR: 6.73, 95% CI: 2.60–17.42).
Table 1.
Demographic characteristics for Chinese herbal medicine use among children with asthma in Taiwan.
| Characteristics | Total No.(%) | CHM users No.(%) | Non-CHM Users, No.(%) | CHM users/CHM nonusers aOR (95%CI) |
|---|---|---|---|---|
| Number of patients | 33,865 (100%) | 14,783 (43.6%) | 19,082 (56.4%) | |
| Number of asthma hospitalization | 3391 (10.0%) | 1445 (9.8%) | 1946 (10.2%) | |
| Gender | ||||
| Male | 19,346 (57.1%) | 8228 (55.7%) | 11,118 (58.3%) | 1.00 |
| Female | 14,519 (42.9%) | 6555 (44.3%) | 7964 (41.7%) | 1.12 (1.07–1.17) |
| Age at diagnosis (years) | ||||
| 0-5 | 26,319 (77.7%) | 10,728 (72.6%) | 15,591 (81.7%) | 1.00 |
| 6-18 | 7546 (22.3%) | 4055 (27.4%) | 3491 (18.3%) | 2.03 (1.92–2.15) |
| Insured region | ||||
| Taipei city | 7072 (20.9%) | 2948 (19.9%) | 4124 (21.6%) | 1.00 |
| Kaohsiung city | 1503 (4.4%) | 695 (4.7%) | 808 (4.2%) | 1.18 (1.05–1.32) |
| Northern Taiwan | 12,248 (36.2%) | 4746 (32.1%) | 7502 (39.3%) | 0.90 (0.85–0.96) |
| Central Taiwan | 5614 (16.6%) | 2946 (19.9%) | 2668 (14.0%) | 1.59 (1.48–1.70) |
| Southern Taiwan | 6523 (19.3%) | 3135 (21.2%) | 3388 (17.8%) | 1.34 (1.25–1.44) |
| Eastern Taiwan | 720 (2.1%) | 272 (1.8%) | 448 (2.4%) | 0.88 (0.75–1.04) |
| Outlying islands | 185 (0.6%) | 41 (0.3%) | 144 (0.8%) | 0.41 (0.29–0.59) |
| Total number of asthma medication a | ||||
| 1 | 1266 (3.7%) | 537 (3.6%) | 729 (3.8%) | 1.00 |
| 2 | 3593 (10.6%) | 1494 (10.1%) | 2099 (11.0%) | 1.03 (0.90–1.18) |
| 3 | 7498 (22.1%) | 3007 (20.3%) | 4491 (23.5%) | 1.07 (0.94–1.22) |
| 4 | 11,539 (34.1%) | 4916 (33.3%) | 6623 (34.7%) | 1.26 (1.10–1.44) |
| ≧5 | 9969 (29.4%) | 4829 (32.7%) | 5140 (26.9%) | 1.65 (1.44–1.90) |
| Total number of comorbiditiesb | ||||
| 1 | 36 (0.1%) | 5 (0.03%) | 31 (0.2%) | 1.00 |
| 2 | 353 (1.0%) | 98 (0.7%) | 255 (1.3%) | 2.40 (0.90–6.38) |
| 3 | 2134 (6.3%) | 653 (4.4%) | 1481 (7.8%) | 3.08 (1.19–7.99) |
| 4 | 9827 (29.0%) | 4109 (27.8%) | 5718 (30.0%) | 5.36 (2.07–13.86) |
| ≧5 | 21,514 (63.5%) | 9918 (67.1%) | 11,596 (60.8%) | 6.73 (2.60–17.42) |
Abbreviations: CHM, Chinese herbal medicine; aOR, adjusted odds ratio; Cl, confidence interval.
Asthma medication including:short-acting β2 agonists, short-acting anticholinergics, inhaled glucocorticosteroids, long-acting β2 agonists,antileukotriene, mast-cell stabilizers, anti-IgE monoclonal antibody.
Comorbidities including:allergic rhinitis, acute upper respiratory infection, acute bronchitis, acute sinusitis, atopic dermatitis, gastroesophageal reflux disease, urticaria.
On the basis of the frequency distribution of TCM outpatient visits in Table 2, children with asthma were mostly treated with CHM, rather than acupuncture or manipulation therapy. The ratio of CHM therapy to acupuncture or manipulation therapy was 9:1. Moreover, respiratory-related disease; symptoms, signs, and ill-defined disease; and digestive-related disease were the most common diseases treated using CHM therapy. Table 3 shows the most commonly prescribed TCM formulas for children with asthma. Xin-Yi-Qing-Fe-Tang, Xiao-qing-long-tang, and Ma-Xing-Gan-Shi-Tang were the top three TCM formulas prescribed to children with asthma. The average dosage was less than 3.0 g person/day in each TCM formula. Among the top 10 TCM formulas, Xiao-qing-long-tang, Ma-Xing-Gan-Shi- Tang, Ge-Gen-Tang, and Ding-Chuan-Tang contained the Ma-Huang compound. Although the proportion of Ma-Huang differed in different TCM formulas, the average dose of Ma-Huang in each TCM formula was less than 1.0 g person/day after conversion. To determine the different risk factors for asthma hospitalization, we analysed the adjusted hazard ratio (aHR) of each demographic variable (Table 5). Patients younger than 6 years and those using multiple types of asthma medications were at a high risk of asthma hospitalization. Notably, children with asthma using more types of asthma medication exhibited a higher risk of asthma hospitalization (≧5 asthma medications: aHR: 10.37, 95% CI: 6.57–16.35). After adjustment for gender, age, comorbidities, and total numbers of asthma medication, CHM users had a lower risk of asthma hospitalization than non-CHM users (aHR: 0.90, 95% CI: 0.83–0.95). As shown in Table 6 and Fig. 2, more CHM cumulative days were associated with a lower risk of asthma hospitalization in patients aged 6–18 years. Moreover, children older than 6 years who used CHM therapy for more than 180 days exhibited a reduction of 29% for the risk of consequent asthma hospitalization (aHR: 0.71, 95% CI: 0.51–0.98) (see Table 4).
Fig. 2.
Survival curve of asthma hospitalization in asthmatic children.
Kaplan-Meier survival curves and log-rank analyses revealed the rates of asthma hospitalization between different CHM cumulative days (log-rank test, p <
0.001).
Table 4.
Mechanism and therapeutic effect of frequently prescribed TCM formulas for children with asthma in Taiwan.
| Herbal formula (Pin-yin name) | Function in TCM theory | Mechanism or therapeutic effect |
|---|---|---|
| Xin-Yi-Qing-Fei-Tang | Clears lung heat, relieves stuffy nose | |
| Xiao-Qing-Long-Tang | Dispels the exterior wind cold, warms lung rheum | Regulation of T-cell by activation of theCD8+ cells and double-negative T-cell population in the lung (animal model)32 Suppressed the increase of eosinophils in the airway, stimulation of β2-adrenoceptors leading to bronchial relaxation (animal model)40 |
| Ma-Xing-Gan-Shi-Tang | Clears lung heat, suppress cough | Stimulation of β2-adrenoceptors on bronchial smooth muscle and inhibiting the neutrophil into the airway (animal model)33 Inhibitory activity against different strains of human influenza A viruses (in vitro)41 |
| Cang-Er-San | Dispels the wind, relieves stuffynose | Suppression of thromboxane B2, eosinophil infiltration, and endothelial nitric oxide synthase in the nasal tissues (animal model)42 Relieved symptoms of nasal congestion among patients with perennial allergic rhinitis (clinical trial) |
| Xin-Yi-San | Dispels the wind cold, relieves stuffy nose | Reduction of nasal airflow resistance, suppression of serum IgE levels and increased production of IL-10, sICAM-1, and IL-8 in patient with perennial allergic rhinitis (clinical trial)43 |
| Yin-Qiao-San | Clears heat and resolving toxin | Relief fever and well-tolerated in patient with paracetamol and ibuprofen hypersensitivity.(clinical trial)44 |
| Ge-Gen-Tang | Resolves exterior cold with sweating | Stimulates mucosalcells to secrete IFN-β to counteract viral infection, against human respiratory syncytial virus inhuman respiratory tract cell lines (in vitro)45 |
| Xing-Su-San | Diffuses lung and transforming phlegm | |
| Zhi-Sou-San | Suppress cough | |
| Ding-Chuan-Tang | Suppress cough and wheeze, diffuses lung and clearing lung heat | Suppressed the eosinophil infiltration into lung tissue, and inhibited the antigen induced immediate asthmatic responses (animal model)46 Improving airway hyper-responsiveness, symptoms for asthma children (clinical trial)8 |
4. Discussion
With the rapidly increasing healthcare expenditure in Taiwan, there are increasing concerns regarding the benefits and risks of the combination antiasthmatic drugs with CHM. However, the verification and quantification of the research and public health implications of these concerns have been limited because of the absence of comprehensive information on exposure to the full range of CHM in children with asthma. According to our literature review, this study is the first to use a random population-based cohort to study the correlation of CHM use with asthma hospitalization in children with asthma and to investigate the integration of CHM with conventional antiasthmatic drugs in asthma treatment. We observed that children prescribed antiasthmatic drugs were frequently CHM users in Taiwan. As shown in Fig. 1, from 2000 to 2012, 14,783 (43.6%) children with asthma had used CHM therapy, and children using CHM often tended to be females, older (6–18 years), and live in Central Taiwan. However, more than half of patients had not used CHM therapy, probably because it was not as convenient as inhaled antiasthmatic drugs for younger children. The highest density of CHM users was located in Central Taiwan, and it probably because of most TCM doctors was located in Central Taiwan.26 The GINA guidelines recommend stepwise treatment as the standard treatment for asthma, which implies that more types of antiasthmatic drugs should be prescribed for more severe asthma. In our study, we discovered that CHM users were prescribed more types of antiasthmatic drugs than non-CHM users, indicating that conventional antiasthmatic drugs did not succeed in controlling asthma symptoms in some children, or they could not tolerate the adverse effects of antiasthmatic drugs, leading them to opt for TCM treatment. The present findings showed that nearly 6 of 10 children with asthma who developed at least five comorbidities and those with multiple chronic allergic conditions were more likely to use CHM therapy than those without chronic disease.
According to the distribution of diseases by TCM outpatient visits, children with asthma opting for TCM treatment mostly exhibited respiratory-related diseases. The main reason may be that a high proportion of patients with asthma concurrently experienced allergic rhinitis,23 and asthmatic symptoms are often triggered by weather changes or upper airway infections.27,28 In our study, we found that the top 10 TCM formulas were all prescribed for treating respiratory-related diseases. The most frequently prescribed TCM formulas were Xin-Yi-Qing-Fei-Tang, Xiao-qing-long-tang, and Ma-Xing-Gan-Shi-Tang (Table 3). Xin-Yi-Qing-Fei-Tang is mostly frequently prescribed TCM formula for allergic rhinitis or sinusitis29,30; its mechanism of action involves clearing the heat of the lung and relieving the stuffy nose. Xiao-qing-long-tang (XQLT)is suitable for asthma or allergic rhinitis combined with external cold and internal rheum, and it warms the lung and suppresses cough or wheezing by the mechanism of regulation of T-cell by activation of theCD8+ cells in the lung and suppressed the increase of eosinophils in the airway.29, 30, 31, 32 Ma-Xing-Gan-Shi-Tang (MXGST) is specifically prescribed for heat-wheezing; it clears the heat of the lung and suppresses cough or wheezing,33 the possible mechanism of MXGST is to stimulate β2-adrenoceptors on bronchial smooth muscle and inhibit the neutrophil into the airway.33 Among the top 10 TCM formulas, Xiao-qing-long-tang, Ma-Xing-Gan-Shi-Tang, Ge-Gen-Tang, and Ding-Chuan-Tang contain the Ma-Huang composition, which dilates the smooth muscle of bronchus and had been widely used for treating asthma in Europe and Japan before other antiasthmatic drugs developed.34
Generally, the purpose of CHM is to improve symptoms or to treat the disease through physical adjustment or immunomodulaiton,35 and sometimes, medication has to be continually used for a longer time for treating diseases, particularly chronic diseases or allergic diseases. Patients or their parents may be concerned about the potential risk or adverse effects of the long-term use of CHM.36 In our study, we discovered that children older than 6 years who used CHM therapy lowers the risk of asthma hospitalization, particularly those using CHM for more than 180 days. The result in coordinated with a previous multicenter, double-blind and placebo-controlled study that CHM therapy for 6 months improved the clinical symptoms in children with asthma, especially peak expiratory flow rate (PEFR). The possible mechanism of CHM in that study including increasing total T cell and PGE2, decreasing B cell, LTC4, IFN-gamma and IL-410. Another clinical study discovered that formula contained Mai-Men-Dong-Tang and Liu-Wei-Di-Huang Wan in 5–20 years old children with asthma for 6 months improved forced expiratory volume in 1 s (FEV1) and inhibited the synthesis of the IgE.9 It seems that CHMs takes times to achieve the immunomodulatory effect via different mechanism. However, CHM may not exert the same effect in children younger than 6 years of age. Younger children have an immature immune system and lung development37 who are vulnerable groups and usually exhibit an average of 6–10 times of common cold every year.38 Furthermore, upper airway infection caused by virus triggers approximately 80% of asthma exacerbation in children,20 and it probably explains why CHM exerts less effects in younger children.
Formulas containing Ma-Huang have been widely used for treating asthma or respiratory-related diseases in China since 3000 BCE.34 The effective component of Ma-Huang (Ephedrae herba) is epinephrine and pseudoephedrine, which dilating the respiratory smooth muscle quickly in asthma patients but function as non-selective sympathetic stimulants on α and β receptors.34 Notably, the adverse effects of ephedrine are weight-loss, insomnia, and dry mouth for α receptors and irregular tachycardia or cardiovascular effect for β1 receptor.34,39 In our study, the average dose of Ma-Huang in each TCM formula was less than 1.0 g person/day for children. However, some children may concurrently using long-acting β2 adrenoceptor agonists (LABA) and Ma-Huang related CHM. It suggested that TCM physicians should evaluate the risk of adverse effects and follow up the clinical reaction when prescribing Ma-Huang-related CHM to children with asthma.
This present study has four limitations. First, this study did not include some over-the-counter of CHM available in Taiwan, implying the frequency of CHM use might have been underestimated. However, because the NHIRD system covers all prescriptions including mostly CHM by qualified TCM physicians after careful examination and diagnosis, providing affordable, accessible, and convenient asthma healthcare, the likelihood of parents purchasing over-the-counter CHM for their children is relatively low. Second, the medical records, including prescription days and frequency of the drugs, were retrospective, and we could not determine whether patients had taken their prescribed CHM regularly. However, all prescriptions were recommended on the basis of expert opinions. Therefore, the compliance of children with asthma was assumed to be high. Third, owing to the lack of actual clinical data, we could not draw any conclusions on the severity of asthma symptoms in children. Therefore, we used the total number of antiasthmatic drugs to represent asthma severity on the basis of the stepwise treatment recommended by GINA guidelines to realise the clinical situation to some extent. Four, the single herb–drug interaction between TCM therapy and conventional asthma treatment was not obtained in this study. According to the literature review, the clinical efficacy of TCM formula is attributed to the synergistic effects of multiple herbs. On the other hand, the clinical efficacy of a single herb of TCM is not attributed to a single effect on one pathway, but to multiple effects.3. To date, some herb–drug interaction research in vivo or in vitro is available.39 However, few studies have investigated the single herb–drug interaction among children with asthma because of the complexity.
5. Conclusions
Asthma is a chronic, airway-inflammatory disease, and often triggered by allergen. Except Ma-Huang (Ephedrae herba), other CHMs act as anti-inflammatory, anti-allergic reaction or immunomodulatory effect via different mechanism in relieving asthma symptoms. In our large-scale cohort study, we found that children aged 6–18 years who used more than 6 months CHM therapy reduced the risk of consequent asthma hospitalization. Long–term CHM therapy has benefit in school-age children with asthma. However, there was no association between CHM therapy and asthma hospitalization in children younger than 6 years in the study. Recognizing the benefits of TCM and CHM therapy, exploring its potential mechanism and herb-drug interaction may be beneficial to the overall health and quality of life of children with asthma.
Conflicts of interest
Authors declare that they have no conflict of interest.
Funding
This work was supported by the Department of Chinese Medicine and Pharmacy, Ministry of Health and Welfare [grant numbers: MOHW105-CMAP-M-114-112415].
Acknowledgements
This research was based on a portion of data from the National Health Insurance Research Database, Taiwan. The interpretation and conclusion in the study do not represent those of the National Health Insurance, Department of Health, or National Health Research Institutes.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtcme.2019.04.005.
Contributor Information
Pei-Chia Lo, Email: rinko0207@gmail.com.
Shun-Ku Lin, Email: gigilaskl@gmail.com.
Jung-Nien Lai, Email: ericlai111@gmail.com, jnlai@mail.cmu.edu.tw.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Hwang C.Y., Chen Y.J., Lin M.W. Prevalence of atopic dermatitis, allergic rhinitis and asthma in Taiwan: a national study 2000 to 2007. Acta Derm Venereol. 2010;90(6):589–594. doi: 10.2340/00015555-0963. [DOI] [PubMed] [Google Scholar]
- 2.Ma Y.C., Lin C.C., Li C.I., Chiang J.H., Li T.C., Lin J.G. Time-trend analysis of prevalence, incidence and traditional Chinese medicine use among children with asthma: a population-based study. J Public Health. 2015;38(3):e263–e271. doi: 10.1093/pubmed/fdv144. [DOI] [PubMed] [Google Scholar]
- 3.Wang J.Y., Liu L.F. Health care utilization and medical costs for childhood asthma in taiwan: using taiwan national health insurance research database. Asia Pac Allergy. 2012;2(3):167–171. doi: 10.5415/apallergy.2012.2.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson D.J., Sykes A., Mallia P., Johnston S.L. Asthma exacerbations: origin, effect, and prevention. J Allergy Clin Immunol. 2011;128(6):1165–1174. doi: 10.1016/j.jaci.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo P.C., Tsai Y.T., Lin S.K., Lai J.N. Risk of asthma exacerbation associated with nonsteroidal anti-inflammatory drugs in childhood asthma: a nationwide population-based cohort study in Taiwan. Medicine (Baltim) 2016;95(41):e5109. doi: 10.1097/MD.0000000000005109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X.M. Complementary and alternative medicine in pediatric allergic disorders. Curr Opin Allergy Clin Immunol. 2009;9(2):161. doi: 10.1097/ACI.0b013e328329226f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen F.P., Chen T.J., Kung Y.Y. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv Res. 2007;7(1):1. doi: 10.1186/1472-6963-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan C.K., Kuo M.L., Shen J.J., See L.C., Chang H.H., Huang J.L. Ding Chuan Tang, a Chinese herb decoction, could improve airway hyper-responsiveness in stabilized asthmatic children: a randomized, double-blind clinical trial. Pediatr Allergy Immunol. 2006;17(5):316–322. doi: 10.1111/j.1399-3038.2006.00406.x. [DOI] [PubMed] [Google Scholar]
- 9.Chang T.T., Huang C.C., Hsu C.H. Clinical evaluation of the Chinese herbal medicine formula STA-1 in the treatment of allergic asthma. Phytother Res. 2006;20(5):342–347. doi: 10.1002/ptr.1843. [DOI] [PubMed] [Google Scholar]
- 10.Hsieh K.H. Evaluation of efficacy of traditional Chinese medicines in the treatment of childhood bronchial asthma: clinical trial, immunological tests and animal study. Taiwan Asthma Study Group. Pediatr Allergy Immunol. 1996;7(3):130–140. doi: 10.1111/j.1399-3038.1996.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 11.Kopnina H. Contesting asthma medication: patients' view of alternatives. J Asthma. 2010;47(6):687–694. doi: 10.3109/02770901003734322. [DOI] [PubMed] [Google Scholar]
- 12.Lee Y.C., Huang Y.T., Tsai Y.W. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225. doi: 10.1186/1472-6963-10-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen M.C., Lai J.N., Chen P.C., Wang J.D. Concurrent use of conventional drugs with Chinese herbal products in taiwan: a population-based study. J Tradit Complementary Med. 2013;3(4):256–262. doi: 10.4103/2225-4110.119734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsieh S.C., Lai J.N., Lee C.F., Hu F.C., Tseng W.L., Wang J.D. The prescribing of Chinese herbal products in Taiwan: a cross-sectional analysis of the national health insurance reimbursement database. Pharmacoepidemiol Drug Saf. 2008;17(6):609–619. doi: 10.1002/pds.1611. [DOI] [PubMed] [Google Scholar]
- 15.Huang T.P., Liu P.H., Lien A.S., Yang S.L., Chang H.H., Yen H.R. Characteristics of traditional Chinese medicine use in children with asthma: a nationwide population-based study. Allergy. 2013;68(12):1610–1613. doi: 10.1111/all.12273. [DOI] [PubMed] [Google Scholar]
- 16.Chen H.Y., Lin Y.H., Wu J.C. Characteristics of pediatric traditional Chinese medicine users in Taiwan: a nationwide cohort study. Pediatrics. 2012;129(6):e1485–e1492. doi: 10.1542/peds.2011-3008. [DOI] [PubMed] [Google Scholar]
- 17.Chen H.Y., Lin Y.H., Thien P.F. Identifying core herbal treatments for children with asthma: implication from a Chinese herbal medicine database in taiwan. Evid Based Complement Alternat Med. 2013;2013:125943. doi: 10.1155/2013/125943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin S.I., Tsai T.H., Chou Y.J., Huang N. Characteristics associated with utilization of asthma-related traditional Chinese medicine services among asthma children in taiwan: a nationwide cohort study. Evid Based Complement Alternat Med. 2015;2015:108961. doi: 10.1155/2015/108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Health Research Institutes National Health Insurance Research Database. http://nhird.nhri.org.tw/date_01.html
- 20.Busse W.W., Lemanske R.F., Jr., Gern J.E. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376(9743):826–834. doi: 10.1016/S0140-6736(10)61380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson D.J., Gangnon R.E., Evans M.D. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178(7):667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bateman E.D., Hurd S.S., Barnes P.J. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 23.Bousquet J., Van Cauwenberge P., Khaltaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(5):S147–S334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 24.Illi S., von Mutius E., Lau S. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004;113(5):925–931. doi: 10.1016/j.jaci.2004.01.778. [DOI] [PubMed] [Google Scholar]
- 25.Thakkar K., Boatright R.O., Gilger M.A., El-Serag H.B. Gastroesophageal reflux and asthma in children: a systematic review. Pediatrics. 2010;125(4):e925–e930. doi: 10.1542/peds.2009-2382. [DOI] [PubMed] [Google Scholar]
- 26.Wang H.M., Lin S.K., Yeh C.H., Lai J.N. Prescription pattern of Chinese herbal products for adult-onset asthma in Taiwan: a population-based study. Ann Allergy Asthma Immunol. 2014;112(5):465–470. doi: 10.1016/j.anai.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 27.Busse W.W., Lemanske R.F., Gern J.E. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376(9743):826–834. doi: 10.1016/S0140-6736(10)61380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenthal L.A., Avila P.C., Heymann P.W. Viral respiratory tract infections and asthma: the course ahead. J Allergy Clin Immunol. 2010;125(6):1212–1217. doi: 10.1016/j.jaci.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yen H.R., Liang K.L., Huang T.P., Fan J.Y., Chang T.T., Sun M.F. Characteristics of traditional Chinese medicine use for children with allergic rhinitis: a nationwide population-based study. Int J Pediatr Otorhinolaryngol. 2016;79(4):591–597. doi: 10.1016/j.ijporl.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Kung Y.Y., Chen Y.C., Hwang S.J., Chen T.J., Chen F.P. The prescriptions frequencies and patterns of Chinese herbal medicine for allergic rhinitis in Taiwan. Allergy. 2006;61(11):1316–1318. doi: 10.1111/j.1398-9995.2006.01152.x. [DOI] [PubMed] [Google Scholar]
- 31.Chen F.P., Chen F.J., Jong M.S., Tsai H.L., Wang J.R., Hwang S.J. Modern use of Chinese herbal formulae from Shang-Han Lun. Chin Med J (Engl). 2009;122(16):1889–1894. [PubMed] [Google Scholar]
- 32.Kao S.T., Wang S.D., Wang J.Y., Yu C.K., Lei H.Y. The effect of Chinese herbal medicine, xiao-qing-long tang (XQLT), on allergen-induced bronchial inflammation in mite-sensitized mice. Allergy. 2000;55(12):1127–1133. doi: 10.1034/j.1398-9995.2000.00728.x. [DOI] [PubMed] [Google Scholar]
- 33.Kao S.T., Yeh T.J., Hsieh C.C., Shiau H.B., Yeh F.T., Lin J.G. The effects of Ma-Xing-Gan-Shi-Tang on respiratory resistance and airway leukocyte infiltration in asthmatic Guinea pigs. Immunopharmacol Immunotoxicol. 2001;23(3):445–458. doi: 10.1081/iph-100107343. [DOI] [PubMed] [Google Scholar]
- 34.Lee M.R. The history of Ephedra (ma-huang) J R Coll Phys Edinb. 2011;41(1):78–84. doi: 10.4997/JRCPE.2011.116. [DOI] [PubMed] [Google Scholar]
- 35.Guo H., Liu M.P. Mechanism of traditional Chinese medicine in the treatment of allergic rhinitis. Chin Med J (Engl). 2013;126(4):756–760. [PubMed] [Google Scholar]
- 36.Lai J.N., Tang J.L., Wang J.D. Observational studies on evaluating the safety and adverse effects of traditional Chinese medicine. Evid Based Complement Alternat Med. 2013;2013:697893. doi: 10.1155/2013/697893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hogg J.C., Williams J., Richardson J.B., Macklem P.T., Thurlbeck W.M. Age as a factor in the distribution of lower-airway conductance and in the pathologic anatomy of obstructive lung disease. N Engl J Med. 1970;282(23):1283–1287. doi: 10.1056/NEJM197006042822302. [DOI] [PubMed] [Google Scholar]
- 38.Fendrick A.M., Monto A.S., Nightengale B., Sarnes M. The economic burden of non–influenza-related viral respiratory tract infection in the United States. Arch Intern Med. 2003;163(4):487–494. doi: 10.1001/archinte.163.4.487. [DOI] [PubMed] [Google Scholar]
- 39.Ulbricht C., Chao W., Costa D., Rusie-Seamon E., Weissner W., Woods J. Clinical evidence of herb-drug interactions: a systematic review by the natural standard research collaboration. Curr Drug Metabol. 2008;9(10):1063–1120. doi: 10.2174/138920008786927785. [DOI] [PubMed] [Google Scholar]
- 40.Kao S.T., Lin C.S., Hsieh C.C., Hsieh W.T., Lin J.G. Effects of xiao-qing-long-tang (XQLT) on bronchoconstriction and airway eosinophil infiltration in ovalbumin-sensitized Guinea pigs: in vivo and in vitro studies. Allergy. 2001;56(12):1164–1171. doi: 10.1034/j.1398-9995.2001.00982.x. [DOI] [PubMed] [Google Scholar]
- 41.Hsieh C.F., Lo C.W., Liu C.H. Mechanism by which ma-xing-shi-gan-tang inhibits the entry of influenza virus. J Ethnopharmacol. 2012;143(1):57–67. doi: 10.1016/j.jep.2012.05.061. [DOI] [PubMed] [Google Scholar]
- 42.Zhao Y., Woo K.S., Ma K.H. Treatment of perennial allergic rhinitis using Shi-Bi-Lin, a Chinese herbal formula. J Ethnopharmacol. 2009;122(1):100–105. doi: 10.1016/j.jep.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Yang S.H., Yu C.L., Chen Y.L., Chiao S.L., Chen M.L. Traditional Chinese medicine, Xin-yi-san, reduces nasal symptoms of patients with perennial allergic rhinitis by its diverse immunomodulatory effects. Int Immunopharmacol. 2010;10(8):951–958. doi: 10.1016/j.intimp.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Liew W.K., Loh W., Chiang W.C., Goh A., Chay O.M., Iancovici Kidon M. Pilot study of the use of Yin Qiao San in children with conventional antipyretic hypersensitivity. Asia Pac Allergy. 2015;5(4):222–229. doi: 10.5415/apallergy.2015.5.4.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.San Chang J., Wang K.C., Shieh D.E., Hsu F.F., Chiang L.C. Ge-Gen-Tang has anti-viral activity against human respiratory syncytial virus in human respiratory tract cell lines. J Ethnopharmacol. 2012;139(1):305–310. doi: 10.1016/j.jep.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 46.Kao S.T., Chang C.H., Chen Y.S., Chiang S.Y., Lin J.G. Effects of ding-chuan-tang on bronchoconstriction and airway leucocyte infiltration in sensitized Guinea pigs. Immunopharmacol Immunotoxicol. 2004;26(1):113–124. doi: 10.1081/iph-120029949. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.