Abstract
Tertiary hyperparathyroidism is defined as a state of excessive secretion of parathyroid hormone after long-standing secondary hyperparathyroidism, which typically occurs in patients with chronic kidney disease. Tertiary hyperparathyroidism is typically characterized by marked parathyroid hyperplasia or parathyroid adenomas. Here we present a case of multiple parathyroid adenomas in a 23-year-old woman with tertiary hyperparathyroidism due to chronic kidney disease and describe the ultrasonography and computed tomography findings. To our knowledge, this is the first case of four parathyroid adenomas showing variable radiological features in a patient with tertiary hyperparathyroidism.
Keywords: Parathyroid neoplasm, Chronic kidney failure, Hyperparathyroidism, Ultrasonography, Computed tomography
Introduction
Tertiary hyperparathyroidism involves continuous parathyroid hyperfunction against a background of secondary hyperparathyroidism. Most cases show diffuse or nodular chief cell hyperplasia that affects multiple parathyroid glands; however, up to 32% patients exhibit a single adenoma or double adenomas [1], [2], [3].
Here we describe a case involving a 23-year-old woman with tertiary hyperparathyroidism who developed 4 parathyroid adenomas showing variable imaging findings.
Case presentation
A 23-year-old woman had been treated with long-term hemodialysis to manage chronic kidney disease (CKD) due to membranoproliferative glomerulonephritis for the past 10 years. She was also treated with active vitamin D sterols because of secondary hyperparathyroidism, for the previous 6 years. However, her serum parathyroid hormone (PTH) levels remained elevated over 600 pg/mL (normal range: 10–65 pg/mL) despite this treatment. On admission, the patient’s serum calcium was 10.7 mg/dL (normal range: 8.6–10.2 mg/dL), and serum phosphate was 7.1 mg/dL (normal range: 2.5–4.5 mg/dL). Serum intact PTH concentration was 630 pg/mL. She complained of pain in both knees, and the mean T-score of the left femur neck, measured by dual-energy X-ray absorptiometry, was -2.7. On the basis of these findings, the patient was diagnosed with tertiary hyperparathyroidism.
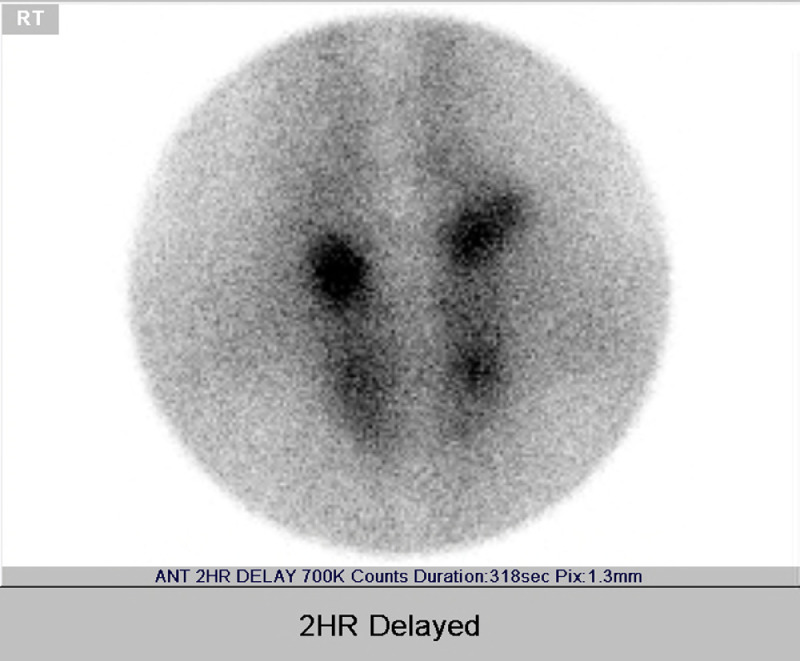
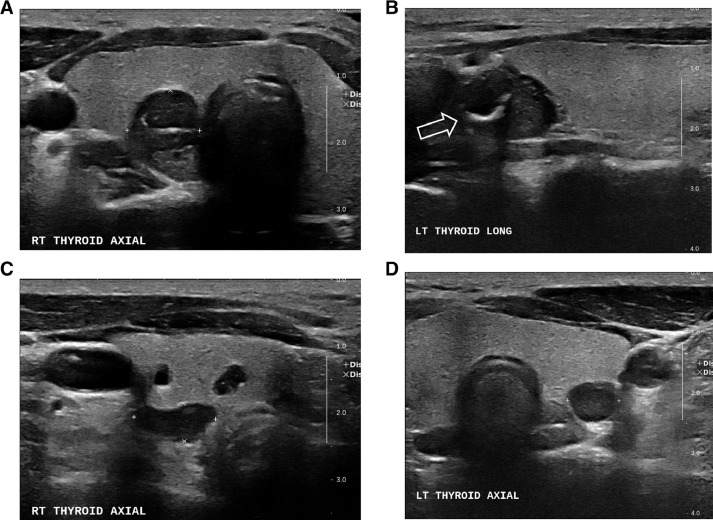
Two-hour-delayed 99mTc sestamibi scintigraphy showed increased uptake in both superior and inferior parathyroid glands (Fig. 1). Gray-scale ultrasonography of the neck revealed 4 masses located immediately posterior and inferior to both lobes of the thyroid gland. The right upper parathyroid lesion showed hypoechoic and isoechoic components (Fig. 2A). The left superior parathyroid lesion showed hypoechoic echotexture, with dense linear internal calcification and areas of cystic degeneration (Fig. 2B). Right and left inferior parathyroid lesions showed well-circumscribed, bean-shaped, predominantly cystic masses (Fig. 2C and 2D).
Fig. 1.
Multiple parathyroid adenomas in a 23-year-old woman with tertiary hyperparathyroidism. 99mTc sestamibi scintigraphy shows increased uptakes in both superior and inferior parathyroid glands.
Fig. 2.
Ultrasonography of multiple parathyroid adenomas in a 23-year-old woman with tertiary hyperparathyroidism. Transverse ultrasonographic image shows a mass with hypoechoic and isoechoic components in the right superior parathyroid lesion (A). Longitudinal ultrasonographic image shows hypoechoic mass with dense linear internal calcification and area of cystic degeneration in the left superior parathyroid lesion (open arrow) (B). Transverse ultrasonographic image shows a bean-shaped, predominantly cystic mass in the right inferior parathyroid lesion (C). Transverse ultrasonographic image shows a round, predominantly cystic mass in the left inferior parathyroid lesion (D).
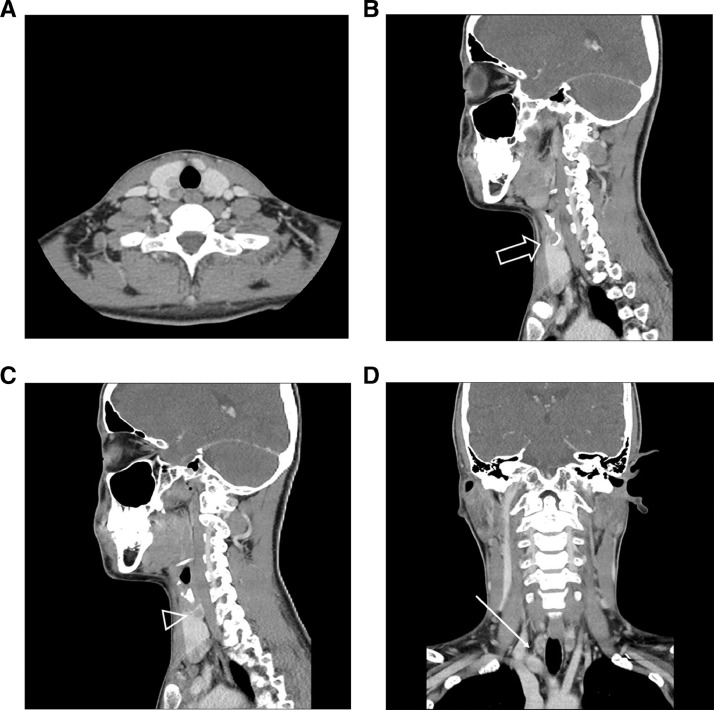
Computed tomography (CT) of the neck showed heterogeneous enhancement in the right upper parathyroid gland (Fig. 3A). The left upper parathyroid gland showed a cystic area, dense linear calcification, and enhancing solid portion (Fig. 3B and 3C). A prominent feeding vessel was identified from the right inferior thyroidal artery to the right lower parathyroid gland (Fig. 3D).
Fig. 3.
Contrast-enhanced CT of multiple parathyroid adenomas in a 23-year-old woman with tertiary hyperparathyroidism. An axial image shows a heterogeneous enhancing mass in the right superior parathyroid lesion (A). A sagittal image shows a cystic portion of the mass with linear dense calcification (open arrow) (B) and an enhancing solid portion (arrowhead) (C) in the left upper parathyroid lesion. A coronal image shows a prominent feeding vessel to the right lower parathyroid gland, arising from the right inferior thyroidal artery (long arrow) (D).
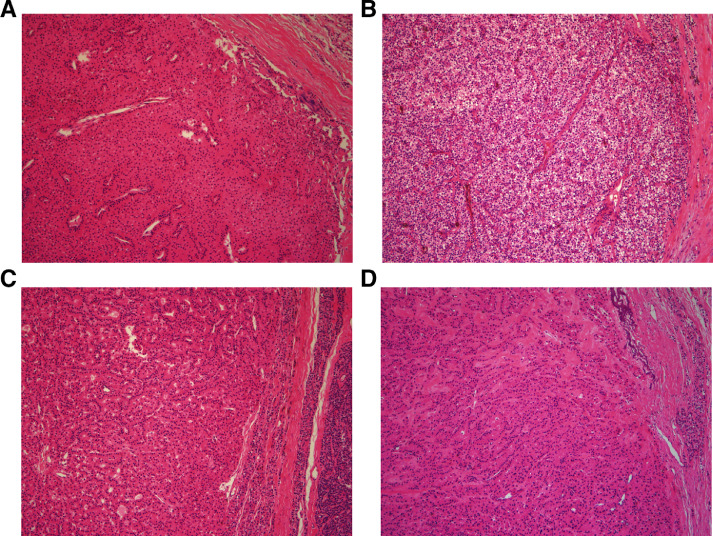
To treat symptomatic tertiary hyperparathyroidism with osteoporosis, she underwent subtotal parathyroidectomy. During the surgery, 4 enlarged, soft, oval, yellowish parathyroid glands were observed (right upper: 1.6 × 1.3 × 1.0 cm3; right inferior: 2.5 × 1.0 × 0.6 cm3; left upper: 2.3 × 1.4 × 1.2 cm3; left lower: 1.2 × 1.0 × 0.8 cm3). Microscopic examination of the four resected masses demonstrated round contours and monotonous growth of oxyphilic cells or chief cells (Fig. 4). Histological findings revealed the four resected tissues to be parathyroid adenomas. The right upper parathyroid gland was partially preserved, while other lesions were removed completely.
Fig. 4.
Microscopic examination of four resected parathyroid adenomas found in a 23-year-old woman with tertiary hyperparathyroidism. The masses show round contours and monotonous growth of oxyphilic cells or chief cells. The non-neoplastic parathyroid tissue adjacent to the tumors appears compressed and atrophic (hematoxylin and eosin, × 100).
During follow-up, the patient did not have any serious postoperative complications. Postoperative blood tests performed a day after the operation showed decreased levels of serum calcium and phosphate, and intact PTH, which were 7.5 mg/dL, 4.7 mg/dL, and 7 pg/mL, respectively. The patient did not have any serious postoperative complications during 15 months follow-up.
Discussion
Tertiary hyperparathyroidism is defined as persistent parathyroid hyperfunction developing from the longstanding secondary parathyroid hyperplasia, mostly in patients with CKD. Decreased urinary phosphate excretion and impaired activity of renal 1 alpha-hydroxylase in patients with CKD, cause hypocalcemia, leading to secondary hyperparathyroidism [4]. Tertiary hyperparathyroidism typically manifests as hypercalcemia following prolonged secondary hyperparathyroidism in patients with long-term hemodialysis and/or successful kidney transplantation [5]. A lack of response to changes in serum calcium levels can lead to elevated serum calcium, phosphate, and PTH levels [5]. In patients with secondary hyperparathyroidism, laboratory tests may show hypocalcemia or normocalcemia and elevated intact PTH levels. In contrast, patients with tertiary hyperparathyroidism show normal or elevated serum calcium level and moderately elevated intact PTH levels [6]. Moreover, patients with tertiary hyperparathyroidism may experience bone pain or fractures with osteopenia or osteoporosis [6]. Our patient had been receiving long-term hemodialysis for CKD, in addition to active vitamin D sterols for secondary hyperparathyroidism since the last 6 years. However, her serum PTH levels remained above 600 pg/mL. On admission, the patient showed hypercalcemia, hyperphosphatemia, and an elevated serum intact PTH level. She also complained of pain in both knees, and the mean T-score for the left femur neck suggested osteoporosis. On the basis of her clinical history and laboratory test results, she was diagnosed with tertiary hyperparathyroidism.
The chronic stimulation of parathyroid secretion in tertiary hyperparathyroidism patients causes parathyroid gland hyperplasia, and this commonly evolves into a parathyroid tumor. The parathyroid lesion may be heterogeneous, because of the continuous evolution from a diffuse hyperplastic state to single nodular glands in patients with secondary hyperparathyroidism [7]. The incidence of single adenoma or double adenomas in patient with tertiary hyperparathyroidism is reported to reach 32% [1], [2], [3]. Nichol et al. reported that the incidences of single adenoma and double adenomas were 10% and 17%, respectively, in patients with tertiary hyperparathyroidism treated by surgical resection [8]. In contrast, patients with primary hyperparathyroidism usually have a single parathyroid adenoma [2,9]. In our patient, 4 adenomas were identified after parathyroidectomy. To the best of our knowledge, there is no published report of 3 or 4 adenomas in a patient with tertiary hyperparathyroidism.
Common ultrasonography findings of an abnormal parathyroid gland with hyperparathyroidism include a well-defined margin and an oval or bean-shaped hypoechoic mass that is usually hypervascular and shows a peripheral vascular arc [10]. In our patient, adenomas in both inferior parathyroid glands showed similar ultrasonography findings. In contrast, atypical ultrasound findings, such as heterogeneous echotexture, cystic changes, and calcification are thought to be increased among patients with parathyroid carcinoma as compared to those with parathyroid adenoma [11]. In our patient, the right superior parathyroid adenoma showed heterogeneous echogenicity and the left superior parathyroid adenoma showed internal calcification and areas of cystic change. Calcification in the parathyroid gland is more common in carcinomas than in adenomas [12]. However, in the setting of CKD, parathyroid adenoma can show internal calcification, probably due to calcification secondary to chronic renal failure, and does not suggest parathyroid carcinoma [13].
Parathyroid adenomas are usually hypervascular lesions with prominent feeding vessels at the margins. In our patient, CT identified a prominent feeding vessel to the parathyroid adenoma in the right lower parathyroid gland.
In conclusion, we presented a very rare case of 4 parathyroid adenomas showing variable ultrasonography and CT features in a patient with tertiary hyperparathyroidism due to CKD.
Footnotes
Declaration of competing interest: The authors declare that they have no conflict of interest.
Ethical approval: This study was approved by the Institutional Review Board, which waived the requirement for written informed consent from the participants.
Informed consent and other ethical considerations: This retrospective study was approved by the institutional review board at our institution, and the need for informed consent was waived.
Funding: There are no financial conflicts of interest to disclose.
Funding sources:There was no funding support for the research.
Authors’ contribution: Byung Hoon Lee: design of the study, patient enrollment, data acquisition, data analysis/interpretation, and manuscript preparation. Byungsoo Kim: data acquisition, data analysis/interpretation, and manuscript preparation.
References
- 1.Yuen NK, Ananthakrishnan S, Campbell MJ. Hyperparathyroidism of renal disease. Perm J. 2016;20(3):15–127. doi: 10.7812/TPP/15-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kebebew E, Duh QY, Clark OH. Tertiary hyperparathyroidism: histologic patterns of disease and results of parathyroidectomy. Arch Surg. 2004;139(9):974–977. doi: 10.1001/archsurg.139.9.974. [DOI] [PubMed] [Google Scholar]
- 3.Kilgo MS, Pirsch JD, Warner TF, Starling JR. Tertiary hyperparathyroidism after renal transplantation: surgical strategy. Surgery. 1998;124(4):677–683. doi: 10.1067/msy.1998.91483. discussion 683–4. [DOI] [PubMed] [Google Scholar]
- 4.Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A. The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol. 2012;269(6):1565–1576. doi: 10.1007/s00405-011-1833-2. [DOI] [PubMed] [Google Scholar]
- 5.Tai TS, Hsu YH, Chang JM, Chen CC. Recurrent tertiary hyperparathyroidism due to supernumerary parathyroid glands in a patient receiving long-term hemodialysis: a case report. BMC Endocr Disord. 2019;19(1):16. doi: 10.1186/s12902-019-0346-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitt SC, Sippel RS, Chen H. Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am. 2009;89(5):1227–1239. doi: 10.1016/j.suc.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tokumoto M, Taniguchi M, Matsuo D, Tsuruya K, Hirakata H, Iida M. Parathyroid cell growth in patients with advanced secondary hyperparathyroidism: vitamin D receptor, calcium sensing receptor, and cell cycle regulating factors. Ther Apher Dial. 2005;9(Suppl 1):S27–S34. doi: 10.1111/j.1744-9987.2005.00302.x. [DOI] [PubMed] [Google Scholar]
- 8.Nichol PF, Starling JR, Mack E, Klovning JJ, Becker BN, Chen H. Long-term follow-up of patients with tertiary hyperparathyroidism treated by resection of a single or double adenoma. Ann Surg. 2002;235(5):673–678. doi: 10.1097/00000658-200205000-00009. discussion 678–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol. 2007;188(6):1706–1715. doi: 10.2214/AJR.06.0938. [DOI] [PubMed] [Google Scholar]
- 10.Sung JY. Parathyroid ultrasonography: the evolving role of the radiologist. Ultrasonography. 2015;34(4):268–274. doi: 10.14366/usg.14071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chandramohan A, Sathyakumar K, John RA, Manipadam MT, Abraham D, Paul TV. Atypical ultrasound features of parathyroid tumours may bear a relationship to their clinical and biochemical presentation. Insights Imaging. 2014;5(1):103–111. doi: 10.1007/s13244-013-0297-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nam M, Jeong HS, Shin JH. Differentiation of parathyroid carcinoma and adenoma by preoperative ultrasonography. Acta Radiol. 2017;58(6):670–675. doi: 10.1177/0284185116666418. [DOI] [PubMed] [Google Scholar]
- 13.Ford EJ, Chandran PK, Graefe HH. Parathyroid calcification as a complication of secondary hyperparathyroidism. Nephron. 1991;57(4):498–499. doi: 10.1159/000186364. [DOI] [PubMed] [Google Scholar]