Abstract
Aims
The relative benefits of computed tomography coronary angiography (CTCA)-guided management in women and men with suspected angina due to coronary heart disease (CHD) are uncertain.
Methods and results
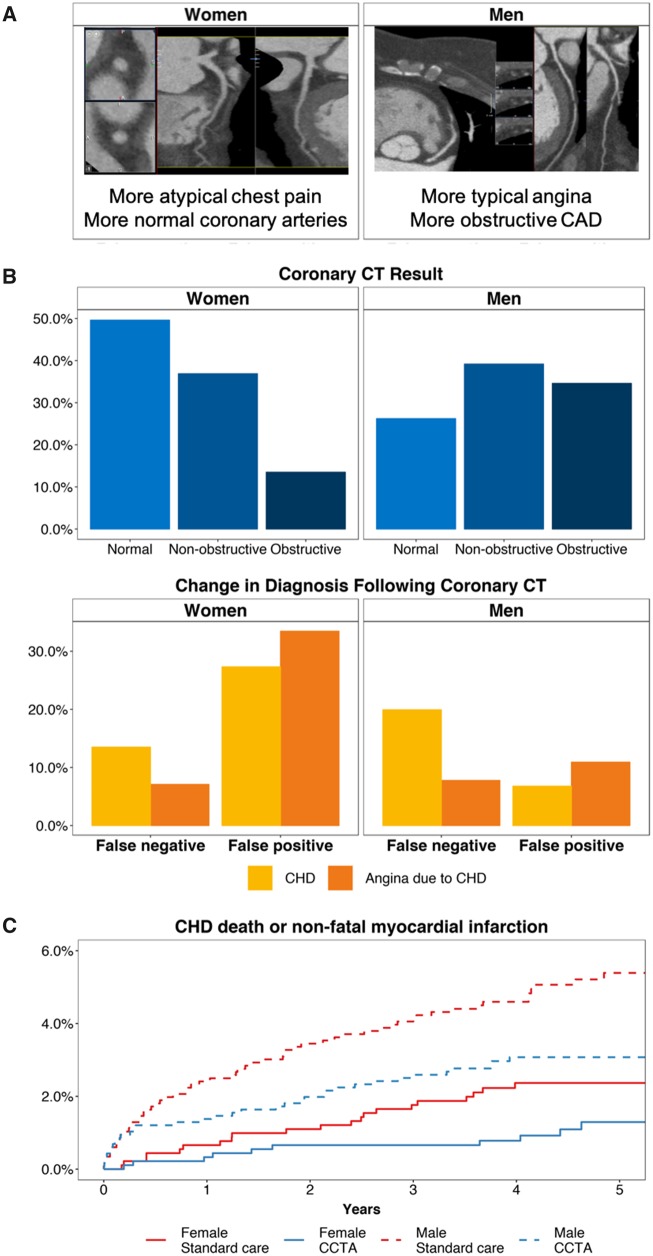
In this post hoc analysis of an open-label parallel-group multicentre trial, we recruited 4146 patients referred for assessment of suspected angina from 12 cardiology clinics across the UK. We randomly assigned (1:1) participants to standard care alone or standard care plus CTCA. Fewer women had typical chest pain symptoms (n = 582, 32.0%) when compared with men (n = 880, 37.9%; P < 0.001). Amongst the CTCA-guided group, more women had normal coronary arteries [386 (49.6%) vs. 263 (26.2%)] and less obstructive CHD [105 (11.5%) vs. 347 (29.8%)]. A CTCA-guided strategy resulted in more women than men being reclassified as not having CHD {19.2% vs. 13.1%; absolute risk difference, 5.7 [95% confidence interval (CI): 2.7–8.7, P < 0.001]} or having angina due to CHD [15.0% vs. 9.0%; absolute risk difference, 5.6 (2.3–8.9, P = 0.001)]. After a median of 4.8 years follow-up, CTCA-guided management was associated with similar reductions in the risk of CHD death or non-fatal myocardial infarction in women [hazard ratio (HR) 0.50, 95% CI 0.24–1.04], and men (HR 0.63, 95% CI 0.42–0.95; Pinteraction = 0.572).
Conclusion
Following the addition of CTCA, women were more likely to be found to have normal coronary arteries than men. This led to more women being reclassified as not having CHD, resulting in more downstream tests and treatments being cancelled. There were similar prognostic benefits of CTCA for women and men.
Keywords: Coronary heart disease, Angina, Gender, CTCA, CT coronary angiography
Introduction
In the management of suspected stable angina, women are less likely than men to be referred for cardiac investigations or undergo coronary revascularization.1 This is despite a higher prevalence of angina2 and a 50% higher lifetime risk of dying from coronary heart disease (CHD).3 Differences in clinical presentation in women contribute to under-recognition and less intensive treatment,4,5 and research studies in CHD may represent women less.6
Patients with stable chest pain are evaluated using anatomical imaging with computed tomography coronary angiography (CTCA) or functional testing including stress electrocardiography, radionuclide scintigraphy, echocardiography, or magnetic resonance imaging.7–11 In the Scottish Computed Tomography of the Heart (SCOT-HEART) trial, we reported that among patients referred for the evaluation of stable chest pain, CTCA clarified the diagnosis and altered subsequent management.12 At 5 years, CTCA-guided management added to standard care reduced the rate of death from CHD or non-fatal myocardial infarction (MI).13
We investigated whether treatment and outcomes following CTCA-guided management differ between women and men. We hypothesized that there are sex differences for the diagnosis of CHD, patient management (including investigations and treatment), and clinical outcomes, including CHD death and MI, at 5 years.
Methods
Study population
The SCOT-HEART study was a prospective clinical trial investigating the role of CTCA in patients aged between 18 and 75 years, referred to a cardiology clinic with suspected angina due to CHD. Patients with a prior history of CHD were eligible to participate. The standard care clinical assessment included exercise electrocardiography. The study design and principal findings12,13 have been reported previously. The study population was randomized 1:1 to standard care or standard care plus ≥64-slice CTCA using a web-based system. Patients gave written informed consent.
Procedures
Cardiovascular risk was calculated with the ASSIGN score. ASSIGN has been developed, calibrated and validated for use in the UK.14
Obstructive coronary artery disease was defined as a luminal stenosis >70% in one or more major epicardial vessel, or >50% stenosis in the left main stem.15
At 6 weeks, attending clinicians were asked to review patients' diagnosis and management in view of all available information including the CTCA report (standard care plus CTCA) or the ASSIGN score (standard care alone). The clinician documented changes in diagnosis, investigations (stress testing or invasive coronary angiography), or treatments (preventive and antianginal treatments). Anginal symptoms were assessed by a self-administered Seattle Angina Questionnaire16 with telephone follow-up for non-responders after two mailings 2 weeks apart.
Outcomes
The primary outcome of the trial was the proportion of patients diagnosed with angina secondary to CHD at 6 weeks. A false-positive or negative baseline diagnosis was determined to have occurred when the treating clinician changed the diagnosis at 6 weeks. Key secondary outcomes included changes in treatment or investigations at 6 weeks; CTCA findings; and changes from baseline in Seattle Angina Questionnaire after 6 weeks and 6 months.12 The principal clinical endpoints included the composite of death due to CHD or non-fatal MI and coronary revascularization procedures. These events were identified with data from the Information and Statistics Division of the National Health Service (NHS) Scotland and, when appropriate, confirmed by review of patient health records.13
Statistical analyses
We performed a post hoc analysis stratified by sex. The analyses were performed according to the intention-to-treat principle. Missing data were removed from the analyses, except for data on deaths, which were censored at the time the patient was lost from the trial.
The diagnoses of CHD and angina due to CHD were assessed for certainty (yes/no vs. unlikely/probable in the primary analysis) and frequency (yes/probable vs. unlikely/no) of diagnoses.
Changes in diagnosis, planned investigations, and medical therapies were analysed within mixed-effects logistic regression models to calculate odds ratio with sex included as an interaction term. We obtained standard errors for absolute risk reduction for each sex assuming that the difference in risk between CTCA and control arm was approximately normal. The standard error for difference in absolute risk reduction between men and women was estimated as the square root of the sum of the standard errors squared for each sex. As some of the numbers were small, we repeated this analysis using simulation (sampling from Beta distributions) obtaining very similar results. Results are reported as odds ratios and absolute risk reductions with 95% confidence intervals (CIs). Clinical endpoint events were analysed with Cox regression models, similarly adjusted, and cumulative event curves were constructed.
All analyses were performed using R software, version 3.5.0 (R Foundation for Statistical Computing). Anonymized data will be made available on request.
Results
Characteristics of the study participants
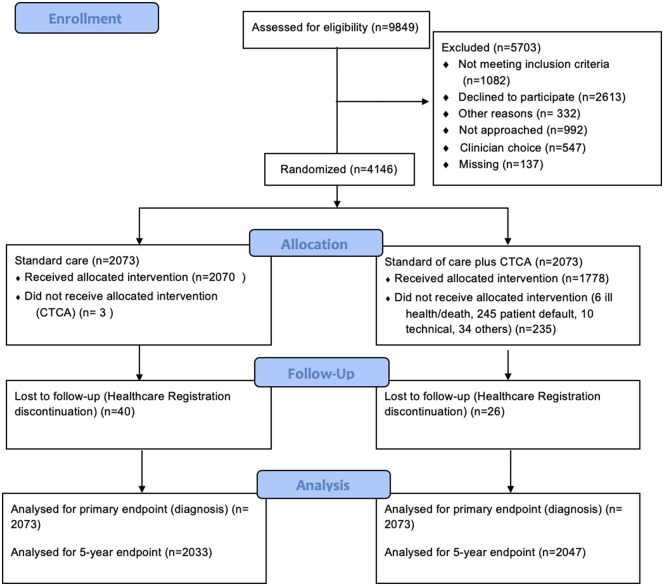
Between 18 November 2010 and 24 September 2014, 4146 (42%) of 9849 patients who had been referred for assessment of suspected angina at 12 cardiology centres across the UK were enrolled and randomly assigned to standard care or standard care and CTCA.
Of 4146 randomized patients, 1821 (44%) were women (Table 1 and Figure 1). Demographics and comorbidities were evenly distributed between the randomized groups. Compared to men, women had a lower frequency of prior CHD in the standard care [49 (5.4%) vs. 137 (11.8%), P < 0.001] and CTCA-guided groups [49 (5.4%) vs. 137 (11.8%), P < 0.001]. Fewer women were classified as having ‘typical’ chest pain symptoms in the CTCA-guided group [women: 281 (30.9%) vs. men: 456 (39.2%); P < 0.001] although no difference was demonstrated within the standard care group [women: 301 (33.1%) vs. men: 424 (36.5%); P = 0.117]. Women were half as likely to be referred for invasive angiography in both groups [standard care, women 76 (8.4%) vs. men 184 (15.8%); CTCA, women 59 (6.5%) vs. men 196 (16.9%)].
Table 1.
Characteristics of the participants prior to randomization according to sex
| Standard care |
P-value (women vs. men) | Standard care + CTCA |
P-value (women vs. men) | |||
|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||
| Number | 910 | 1163 | 911 | 1162 | ||
| Demographics | ||||||
| Age (years) | 57.0 (9.2) | 56.9 (10.0) | 0.794 | 57.5 (9.7) | 56.8 (9.7) | 0.121 |
| Body mass index (kg/m2) | 29.9 (6.5) | 29.6 (5.6) | 0.229 | 30.4 (6.8) | 29.2 (4.8) | <0.001 |
| Atrial fibrillation | 13 (1.4) | 28 (2.4) | 0.153 | 11 (1.2) | 33 (2.8) | 0.016 |
| Cardiovascular risk factors | ||||||
| Cigarette smokera | 458 (50.4) | 632 (54.5) | 0.067 | 452 (49.7) | 643 (55.4) | 0.011 |
| Hypertension | 303 (33.6) | 380 (33.0) | 0.795 | 304 (33.7) | 408 (35.5) | 0.428 |
| Diabetes mellitus | 83 (9.1) | 138 (11.9) | 0.053 | 77 (8.5) | 146 (12.6) | 0.003 |
| Hypercholesterolaemia | 502 (55.2) | 679 (58.4) | 0.154 | 513 (56.3) | 716 (61.6) | 0.017 |
| Family history | 432 (47.7) | 397 (34.6) | <0.001 | 427 (47.5) | 460 (39.9) | 0.001 |
| History of coronary heart disease | 49 (5.4) | 137 (11.8) | <0.001 | 49 (5.4) | 137 (11.8) | <0.001 |
| Medications | ||||||
| Anti-platelet medication | 401 (44.1) | 583 (50.1) | 0.021 | 399 (43.8) | 610 (52.5) | <0.001 |
| Statin | 341 (37.5) | 543 (46.7) | <0.001 | 338 (37.1) | 564 (48.5) | <0.001 |
| Beta-blockade | 180 (19.8) | 304 (26.1) | 0.003 | 198 (21.7) | 306 (26.3) | 0.029 |
| ACE-inhibitor/ARB | 130 (14.3) | 214 (18.4) | 0.040 | 118 (13.0) | 223 (19.2) | <0.001 |
| Calcium channel blocker | 84 (9.2) | 110 (9.5) | 0.919 | 80 (8.8) | 103 (8.9) | 0.527 |
| Nitrates | 241 (26.5) | 349 (30.0) | 0.193 | 219 (24.0) | 351 (30.2) | 0.004 |
| Other antianginal therapy | 31 (3.4) | 44 (3.8) | 0.736 | 29 (3.2) | 49 (4.2) | 0.267 |
| Anginal symptomsb | 0.118 | <0.001 | ||||
| Typical | 301 (33.1) | 424 (36.5) | 281 (30.9) | 456 (39.2) | ||
| Atypical | 231 (25.4) | 255 (22.0) | 254 (27.9) | 248 (21.3) | ||
| Non-anginal | 377 (41.5) | 482 (41.5) | 375 (41.2) | 458 (39.4) | ||
| Electrocardiogram | ||||||
| Normal | 783 (87.0) | 952 (82.7) | 0.009 | 789 (88.1) | 968 (84.0) | 0.010 |
| Stress electrocardiogram | <0.001 | <0.001 | ||||
| Performed | 746 (82.3) | 1007 (87.0) | 756 (83.3) | 1008 (87.1) | ||
| Normal | 477 (69.4) | 612 (64.4) | 491 (69.0) | 616 (65.3) | ||
| Inconclusive | 129 (18.8) | 154 (16.2) | 139 (19.5) | 146 (15.5) | ||
| Abnormal‡ | 81 (11.8) | 185 (19.5) | 82 (11.5) | 182 (19.3) | ||
| Further investigations | ||||||
| Stress imaging | ||||||
| Radionuclide | 129 (14.2) | 84 (7.2) | <0.001 | 115 (12.6) | 61 (5.2) | <0.001 |
| Other | 7 (0.8) | 6 (0.5) | 0.719 | 6 (0.7) | 9 (0.8) | 0.504 |
| Invasive coronary angiography | 76 (8.4) | 184 (15.8) | <0.001 | 59 (6.5) | 196 (16.9) | <0.001 |
| Baseline diagnosis of angina due to CHD | <0.001 | <0.001 | ||||
| No | 103 (11.3) | 163 (14.0) | 110 (12.1) | 157 (13.5) | ||
| Unlikely | 524 (57.6) | 537 (46.3) | 525 (57.7) | 538 (46.3) | ||
| Probable | 239 (26.3) | 363 (31.3) | 240 (26.4) | 362 (31.2) | ||
| Yes | 43 (4.7) | 98 (8.4) | 35 (3.8) | 105 (9.0) | ||
| Baseline diagnosis of CHD | <0.001 | <0.001 | ||||
| No | 49 (5.4) | 83 (7.1) | 58 (6.4) | 80 (6.9) | ||
| Unlikely | 487 (53.6) | 495 (42.6) | 475 (52.2) | 477 (41.0) | ||
| Possible | 314 (34.5) | 420 (36.2) | 328 (36.0) | 444 (38.2) | ||
| Yes | 59 (6.5) | 163 (14.0) | 49 (5.4) | 161 (13.9) | ||
Values are expressed as n (%) or mean ± standard deviation. Missing data (standard care alone, standard care + CTCA): atrial fibrillation n = 4 (3, 1); prior coronary heart disease n = 4 (3, 1); smoking habit n = 7 (5, 2); hypertension n = 41 (20, 21); hypercholesterolaemia n = 4 (3, 1); family history n = 43 (21, 22); angina symptoms n = 4 (3, 1); concomitant therapies n = 4 for all (3, 1 for all); resting electrocardiogram n = 46 (22, 24); exercise electrocardiogram n = 18 (10, 8); exercise electrocardiogram outcome n = 234 (121, 113); further investigations n = 6 (4, 2); stress imaging n = 4 (3, 1); coronary angiography n = 4 (3, 1); and baseline diagnosis n = 4 (3, 1).
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CHD, coronary heart disease.
Current/ex-smokers.
National Institute for Health and Care Excellence criteria.
Figure 1.
Trial design
Findings on computed tomography coronary angiography
Of 2073 participants [n = 911 (44%) women] randomized to CTCA-guided management, 1778 participants underwent CTCA (Table 2). Eighty-one percent of women had a low coronary calcium score (<100 AU), vs. 53% of men (P < 0.001). On CTCA, the proportion of women with normal coronary arteries was two-fold higher than in men, whereas 105 (11.5%) of 911 women had obstructive CHD, which was nearly three-fold lower than in men [n = 347 (29.9%) of 1162, P < 0.001]. The proportions of men with single-, two-, and three-vessel obstructive CHD were two to five-fold higher than in women (Table 2 and Take home figure).
Table 2.
Findings disclosed by computed tomography coronary angiography in men and women
| Women (N = 911) | Men (N = 1162) | P-value | |
|---|---|---|---|
| Coronary calcium score | N = 787 | N = 1006 | <0.001 |
| Low (<100 AU) | 638 (81.1) | 529 (52.6) | |
| Medium (100–400 AU) | 94 (11.9) | 210 (20.9) | |
| High (>400 AU) | 55 (7.0) | 267 (26.5) | |
| Computed tomography coronary angiography | N = 774 | N = 997 | <0.001 |
| Normal | 384 (49.6) | 263 (26.3) | |
| Non-obstructive CHD | |||
| Mild (<50%) | 172 (22.2) | 200 (20.0) | |
| Moderate (50–70%) | 113 (14.6) | 187 (18.8) | |
| Obstructive CHD | |||
| One-vessel | 60 (7.8) | 147 (14.7) | |
| Two-vessel | 31 (4.0) | 97 (9.7) | |
| Three-vessel | 14 (1.8) | 103 (10.3) |
Values are expressed as n (%).
AU, Agatston Units; CHD, coronary heart disease.
Take home figure.
Women were more likely than men to have (A) atypical chest pain and normal coronary arteries leading to (B) greater false-positive diagnoses of coronary heart disease and angina due to coronary heart disease. Overall, women had low rates of clinical events (coronary heart disease death or non-fatal myocardial infarction) at 5 years but derived a similar prognostic benefit from computed tomography coronary angiography as men. (C) Cumulative event curves for the principal long-term clinical endpoint in those assigned to standard care plus computed tomography coronary angiography (blue) and standard care alone (red) amongst women (solid lines) and men (dashed lines).
Baseline and 6-week diagnoses of coronary heart disease and angina due to CHD
Overall, CTCA resulted in more frequent diagnostic changes in women than men (absolute risk difference 5.68, 95% CI: 2.71–8.65, P-interaction < 0.001). Because standard care-guided management also resulted in more frequent changes in the diagnosis of CHD amongst women than men, the relative benefits of CTCA were similar [relative risk 14.6, 95% CI 8.6–27.5 (women) vs. 16.9, 95% CI 9.2–35.6 (men), Table 3]. However, there were important differences in the direction of this change in diagnosis. CTCA-guided management was more likely to identify a false-positive baseline CHD diagnosis amongst women [103 of 377 (27.3%) (CTCA) vs. 9 of 373 (2.4%) (standard care), number needed to scan 4.0, 95% CI 3.4–5.0] compared with men [41 of 605 (6.8%) (CTCA) vs. 5 of 583 (0.9%) (standard care), number needed to scan 16.9, 95% CI 12.4–26.7] (Supplementary material online, Table S2, Take home figure). Conversely, the proportion of false-negative baseline diagnoses was similar for women [72 of 533 (13.5%) (CTCA) vs. 3 of 536 (0.5%) (standard care), number needed to scan 7.7, 95% CI 6.3–10.0] compared with men [111 of 557 (19.9%) (CTCA) vs. 3 of 578 (0.5%) (standard care), number needed to scan 5.2, 95% CI 4.4–6.3].
Table 3.
Change in diagnosis of coronary heart disease and angina
| Change in diagnosis of CHD | |||
| Standard care, N (%) | No change | Change | |
| Female | 898 | 12 | |
| Male | 1154 | 9 | |
| CTCA, N (%) | |||
| Female | 736 | 175 | |
| Male | 1010 | 152 | |
| Female | Male | Interaction | |
| Odds ratio | 17.8 (10.3–34.0) | 19.3 (10.4–41.0) | 1.1 (P = 0.860) |
| Absolute risk change | 17.9% | 12.3% | P < 0.001 |
| Difference in absolute risk | 5.7 (2.7–8.7) | ||
| Change in diagnosis of angina due to CHD | |||
| Standard care, N (%) | No change | Change | |
| Female | 900 | 10 | |
| Male | 1154 | 9 | |
| CTCA, N (%) | |||
| Female | 774 | 137 | |
| Male | 1057 | 105 | |
| Female | Male | Interaction | |
| Odds ratio | 15.9 (8.8–32.6) | 12.7 (6.8–27.2) | 0.8 (P = 0.642) |
| Absolute risk change | 13.9% | 8.3% | P < 0.001 |
| Difference in absolute risk | 5.6 (2.2–8.8) | ||
Similarly, regarding the classification of angina due to CHD, CTCA changed the diagnosis in 54 (7.8%) of 694 men and 45 (7.1%) of 634 women thought not to have CHD and excluded the diagnosis in 51 (10.9%) of 467 men and 92 (33.7%) of 273 women (Take home figure). As before, CTCA changed the diagnosis of angina due to CHD more frequently in women compared with men (absolute risk difference 5.66, 95% 2.72–8.65, P-interaction = 0.007).
Changes in investigations and treatment at 6 weeks
There were no differences in invasive coronary angiography or coronary revascularization rates between standard care and CTCA-guided care. CTCA-guided management resulted in cancellation of tests (myocardial perfusion imaging and stress echocardiography) with an absolute risk difference of 4.45 (95% CI: 2.25–6.65); P < 0.001) and changes in antianginal therapy [absolute risk difference: 4.5 (95% CI: 1.9–7.2), P < 0.001]. CTCA-guided management resulted in similar rates of changes to preventative therapy (Table 4).
Table 4.
Changes in investigations and treatments at 6 weeks
| Preventative medications—change | |||
| Standard care, N (%) | No change | Change | |
| Female | 872 | 38 | |
| Male | 1111 | 52 | |
| CTCA, N (%) | |||
| Female | 749 | 162 | |
| Male | 955 | 207 | |
| Female | Male | Interaction | |
| Odds ratio | 5.0 (3.5–7.3) | 4.6 (3.4–6.4) | P = 0.779 |
| Absolute risk change | 13.6% | 13.3% | |
| Difference in absolute risk reduction | 0.3 (−3.5 to 4.0) | P = 0.890 | |
| Antianginal medications—change | |||
| Standard care, N (%) | No change | Change | |
| Female | 902 | 8 | |
| Male | 1155 | 8 | |
| CTCA, N (%) | |||
| Female | 802 | 109 | |
| Male | 1078 | 84 | |
| Female | Male | Interaction | |
| Odds ratio | 15.3 (7.9–34.4) | 11.2 (5.8–25.3) | P = 0.556 |
| Absolute risk change | 11.1% | 6.5% | |
| Difference in absolute risk reduction | 4.5 (1.9–7.2) | P < 0.001 | |
| Stress imaging investigations—change | |||
| Standard care, N (%) | No change | Change | |
| Female | 906 | 4 | |
| Male | 1161 | 2 | |
| CTCA, N (%) | |||
| Female | 832 | 79 | |
| Male | 1116 | 46 | |
| Female | Male | Interaction | |
| Odds ratio | 21.5 (8.9–70.7) | 23.9 (7.4–146.8) | P = 0.904 |
| Relative risk | 19.7 (7.3–53.6) | 23.9 (5.8–98.8) | |
| Absolute risk change | 8.2% | 3.8% | |
| Difference in absolute risk reduction | 4.5 (2.3–6.7) | P < 0.001 | |
CTCA, computed tomography coronary angiography.
Angina
There were no sex differences in physical limitation, angina stability, frequency, satisfaction with treatment, and quality of life, as assessed using the Seattle Angina Questionnaire, at 6 weeks and 6 months, when compared with baseline observations (Table 1).
Clinical endpoints
After a median of 4.8-year follow-up, women had a lower composite endpoint rate of death due to CHD or MI or death due to CHD, MI, or stroke than men (Take home figure). Crude differences in health outcomes and adjusted hazard ratios were observed between women and men for CTCA-guided management vs. standard care (Table 5).
Table 5.
Clinical outcomes by sex and treatment group after a median of 4.8 years
| Standard care vs. CTCA |
Interaction P-valuea | ||||||
|---|---|---|---|---|---|---|---|
| Women |
Men |
||||||
| N (CTCA) | N (standard care) | HR (95% CI) | N (CTCA) | N (standard care) | HR (95% CI) | ||
| CHD death or myocardial infarction | 11 (1.2) | 22 (2.4) | 0.50 (0.24–1.04) | 37 (3.2) | 59 (5.1) | 0.63 (0.42–0.95) | 0.572 |
| CHD death myocardial infarction or stroke | 19 (2.1) | 26 (2.9) | 0.72 (0.40–1.30) | 44 (3.8) | 71 (6.1) | 0.63 (0.43–0.91) | 0.686 |
| Cardiovascular events | |||||||
| Myocardial infarction | 11 (1.2) | 21 (2.3) | 0.53 (0.25–1.10) | 33 (2.8) | 52 (4.5) | 0.64 (0.41–0.99) | 0.638 |
| Stroke | 8 (0.9) | 5 (0.5) | 1.57 (0.50–4.89) | 7 (0.6) | 15 (1.3) | 0.47 (0.19–1.15) | 0.099 |
| Death | |||||||
| CHD | 0 (0.0) | 1 (0.1) | — | 4 (0.3) | 8 (0.7) | 0.51 (0.15–1.71) | — |
| Cardiovascular | 1 (0.1) | 1 (0.1) | 1.42 (0.08–24.38) | 4 (0.3) | 11 (0.9) | 0.38 (0.12–1.20) | 0.532 |
| Non-cardiovascular | 12 (1.3) | 8 (0.9) | 1.45 (0.59–3.56) | 26 (2.2) | 23 (2.0) | 1.17 (0.67–2.06) | 0.701 |
| All-cause | 13 (1.4) | 9 (1.0) | 1.42 (0.60–3.33) | 30 (2.6) | 34 (2.9) | 0.92 (0.56–1.50) | 0.403 |
| Procedures | |||||||
| Coronary angiography | 144 (15.8) | 159 (17.5) | 0.86 (0.69–1.09) | 347 (29.9) | 343 (29.5) | 1.06 (0.91–1.22) | 0.171 |
| Coronary revascularization | 53 (5.8) | 45 (4.9) | 1.15 (0.77–1.72) | 226 (19.4) | 222 (19.1) | 1.05 (0.87–1.27) | 0.652 |
Hazard ratios (HRs) were determined with Cox regression models adjusted for centre and minimization variables (age, body mass index, diabetes mellitus, prior coronary heart disease, and atrial fibrillation).
P-value for the interaction between sex and allocated treatment.
Discussion
We have undertaken an analysis by sex of the main findings in the SCOT-HEART trial. Compared with men, women had differences in the typicality of their anginal symptoms, a higher likelihood of having normal coronary arteries, and more frequent diagnostic and therapeutic changes with CTCA-guided management. In particular, CTCA modified apparent over-diagnosis and treatment of women who had been incorrectly diagnosed with CHD and angina due to CHD. Both women and men appear to benefit equally from the addition of CTCA to standard care with no evidence of an interaction between sex and health outcomes identified.
In line with prior reports,17–19 women reported less typical anginal symptoms making clinical assessment more challenging. This diagnostic uncertainty, and lower prevalence of obstructive CHD, led to an over-diagnosis of CHD and angina. Exercise electrocardiography testing has limited sensitivity and specificity for the presence of coronary artery disease, especially in women17 which may have contributed to misdiagnosis. Indeed, women were more likely to have downstream non-invasive stress testing cancelled, and antianginal therapies reduced following reclassification by CTCA. On the other hand, ischaemia and no obstructive coronary artery disease (INOCA) caused by small vessel disease more commonly affects women.20 We suggest that CTCA-guided diagnosis and management is helpful in women for the diagnosis of angina due to CHD, but less so for INOCA. These findings extend the sex subanalysis of the CRESCENT (Calcium Imaging and Selective CT Angiography in Comparison to Functional Testing for Suspected Coronary Artery Disease) trial.21
When compared with exercise electrocardiography testing, CTCA-guided therapy impacted on false-positive classifications without affecting false-negative classifications in women. This is in contrast to data published from the PROspective Multicentre Imaging Study for Evaluation of chest pain (PROMISE) trial, where statin therapy was lower in women than in men and women were less likely to be referred for coronary angiography19. In PROMISE, 88% of participants had chest pain (72%) or an anginal equivalent (16%), whilst 10% had typical angina compared with SCOT-HEART where 100% had chest pain, 35% had typical angina and 9% had known CHD. The standard of care was exercise electrocardiography and the results of a trial involving different functional tests as standard of care might be different.
In our study, patients were recruited from cardiology clinics rather than general outpatient clinics. In SCOT-HEART, clinicians were free to request other non-invasive stress imaging at their discretion and indeed 10% of additional testing was requested, mostly radionuclide scintigraphy. In contrast, in the functional testing arm of PROMISE, radionuclide scintigraphy predominated (67%) with stress echocardiography and electrocardiography accounting for the remainder. We found that normal coronary arteries were two-fold more common in women whereas obstructive CHD was three-fold more common in men, similar to Pagidipati et al.19 This has important therapeutic implications for coronary revascularization rates and use of medical therapy across genders.10 Symptoms and quality of life improve when CTCA-guided management discloses normal coronary arteries22 and this favourable outcome associates with female sex. Typical anginal symptoms and obstructive CHD were less common in women, reflecting aetiological differences, and manifest by lower rates of coronary revascularization.17,18 These findings extend those of PROMISE.23
Women are more likely to experience angina due to small vessel disease,20 whereas obstructive CHD is more common in men. The CorMicA trial recently provided evidence that in patients with angina and no obstructive CHD, stratified medicine including adjunctive tests of small vessel function leads to improvements in angina and quality of life.20 The prevalence and clinical significance of small vessel disease in patients with chest pain and normal coronary arteries or non-obstructive CHD is being prospectively assessed in in the Coronary Microvascular Function and CT Coronary Angiography (CorCTCA) trial.24
There are sex differences in prognosis following a diagnosis of stable angina, which is notably worse in younger women than in men.17 These differences may be explained by under-use of relevant tests and treatments.17 In our study, women had lower crude rates of adverse cardiovascular events when compared with men, and a lower rate of MI in both treatment arms. The magnitude and direction of the benefits of CTCA on fatal and non-fatal MI were similar between the sexes. There were no differences in the longer-term in coronary angiography and revascularization rates between groups for both women and men. There was a small numerically higher rate of non-cardiac death and stroke events in women in the CT group vs. the standard care group. The number of events was very low and difficult to interpret.
The interaction tests for sex, treatment group allocation, and health outcomes were not statistically significant (i.e. the null hypothesis was not rejected). Thus, the benefits of CTCA-guided management on health outcomes appear to be similar in women and men. This finding contrasts with the PROMISE25 where women appeared to gain more prognostic benefit than men from a CTCA-guided strategy. A gender-specific post hoc analysis from DISCHARGE (Diagnostic Imaging Strategies for Patients With Stable Chest Pain and Intermediate Risk of Coronary Artery Disease, ClinicalTrials.gov identifier: NCT02400229)26 would extend whether women benefit from CTCA-guided strategy vs. invasive coronary angiography in the investigation of CHD.
Limitations
There are a number of limitations associated with this study. First, this was a post hoc analysis of an open-label trial and gender was not randomized. Second, this study was not designed or powered for this secondary analysis, and our findings are exploratory. Third, the small numbers of changes in the standard care arm resulted in a large variability in the relative changes that it was not possible to draw any firm conclusions from the logistic regression analyses. However, absolute differences allow for different proportions of changes in the diagnosis and establishes the gender differences we report. Finally, information on microvascular dysfunction as an alternative cause of angina was not available. Further studies are on-going.24
Conclusions
Women are less likely to have typical symptoms or obstructive CHD but are more likely to be over-diagnosed. CTCA is useful in reducing over-diagnosis and medication in women and identifies unrecognized CHD equally in both sexes with similar prognostic benefits. More research is needed to determine the causes of, and treatments for, angina in women and men with angiographically normal coronary arteries.
Supplementary Material
Acknowledgements
The authors thank the patients and the staff who participated in this trial.
Funding
The Chief Scientist Office of the Scottish Government Health and Social Care Directorates funded the trial with supplementary awards from the British Heart Foundation [RE/13/3/30183], Edinburgh and Lothian's Health Foundation Trust and the Heart Diseases Research Fund. K.M. was funded by a British Heart Foundation Clinical Training Fellowship [FS/15/54/31639]. C.B. [RE/18/6134217] and D.E.N. [CH09/002, RG/16/10/32375, and RE/13/3/30183] are supported by the British Heart Foundation. D.E.N. is the recipient of a Wellcome Trust Senior Investigator Award [WT103782AIA]. E.vB. is supported by SINAPSE (www.sinapse.ac.uk).
Conflict of interest: The University of Glasgow and Dr Berry have institutional research and/or consultancy agreements with Abbott Vascular, HeartFlow, Opsens, Philips, and Siemens Healthcare. The other authors have no conflict of interest to declare.
References
- 1. Caroline D, Felicity C, Lopez Sendon JL, Luigi T, Eric B, Nicholas D, Francois D, Anselm G, Desmond J, David M, Witold R, Kristian T, Freek V, Fox Kim M.. Gender differences in the management and clinical outcome of stable angina. Circulation 2006;113:490–498. [DOI] [PubMed] [Google Scholar]
- 2. Hemingway H, Langenberg C, Damant J, Frost C, PyöRäLä K, Barrett-Connor E.. Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation 2008;117:1526–1536. [DOI] [PubMed] [Google Scholar]
- 3. Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN.. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women’s Heart Disease and Stroke Campaign Task Force. Arch Fam Med 2000;9:506–515. [DOI] [PubMed] [Google Scholar]
- 4. King KM, Ghali WA, Faris PD, Curtis MJ, Galbraith PD, Graham MM, Knudtson ML.. Sex differences in outcomes after cardiac catheterization: effect modification by treatment strategy and time. JAMA 2004;291:1220–1225. [DOI] [PubMed] [Google Scholar]
- 5. Zhao M, Vaartjes I, Graham I, Grobbee D, Spiering W, Klipstein-Grobusch K, Woodward M, Peters SA.. Sex differences in risk factor management of coronary heart disease across three regions. Heart 2017;103:1587–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Scott PE, Unger EF, Jenkins MR, Southworth MR, McDowell T-Y, Geller RJ, Elahi M, Temple RJ, Woodcock J.. Participation of women in clinical trials supporting FDA approval of cardiovascular drugs. J Am Coll Cardiol 2018;71:1960–1969. [DOI] [PubMed] [Google Scholar]
- 7. Mark DB, Shaw L, Harrell FE, Hlatky MA, Lee KL, Bengtson JR, McCants CB, Califf RM, Pryor DB.. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med 1991;325:849–853. [DOI] [PubMed] [Google Scholar]
- 8. Greenwood JP, Ripley DP, Berry C, McCann GP, Plein S, Bucciarelli-Ducci C, Dall’Armellina E, Prasad A, Bijsterveld P, Foley JR, Mangion K, Sculpher M, Walker S, Everett CC, Cairns DA, Sharples LD, Brown JM.. Effect of care guided by cardiovascular magnetic resonance, myocardial perfusion scintigraphy, or NICE guidelines on subsequent unnecessary angiography rates: the CE-MARC 2 randomized clinical trial. JAMA 2016;316:1051.. [DOI] [PubMed] [Google Scholar]
- 9. Fleischmann KE, Hunink MG, Kuntz KM, Douglas PS.. Exercise echocardiography or exercise SPECT imaging? A meta-analysis of diagnostic test performance. JAMA 1998;280:913–920. [DOI] [PubMed] [Google Scholar]
- 10. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ.. ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2019; 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 11. Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet J-P, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferović PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165. [DOI] [PubMed] [Google Scholar]
- 12.The SCOT-HEART Investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 2015;385:2383–2391. [DOI] [PubMed] [Google Scholar]
- 13.The SCOT-HEART Investigators. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924–933. [DOI] [PubMed] [Google Scholar]
- 14. Woodward M, Brindle P, Tunstall-Pedoe H.. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart 2005;93:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chest Pain of Recent Onset: Assessment and Diagnosis. Guidance and Guidelines NICE. https://www.nice.org.uk/Guidance/CG95 (4 November 2019).
- 16. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonnell M, Fihn SD.. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol 1995;25:333–341. [DOI] [PubMed] [Google Scholar]
- 17. Vaccarino V, Badimon L, Corti R, de Wit C, Dorobantu M, Manfrini O, Koller A, Pries A, Cenko E, Bugiardini R.. Presentation, management, and outcomes of ischaemic heart disease in women. Nat Rev Cardiol 2013;10:508–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, Shah RU, Regitz-Zagrosek V, Grewal J, Vaccarino V, Wei J, Bairey Merz CN.. Sex differences in cardiovascular disease—impact on care and outcomes. Front Neuroendocrinol 2017;46:46–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pagidipati NJ, Coles A, Hemal K, Lee KL, Dolor RJ, Pellikka PA, Mark DB, Patel MR, Litwin SE, Daubert MA, Shah SH, Hoffmann U, Douglas PS.. Sex differences in management and outcomes of patients with stable symptoms suggestive of coronary artery disease: insights from the PROMISE trial. Am Heart J 2019;208:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ford TJ, Stanley B, Good R, Rocchiccioli P, McEntegart M, Watkins S, Eteiba H, Shaukat A, Lindsay M, Robertson K, Hood S, McGeoch R, McDade R, Yii E, Sidik N, McCartney P, Corcoran D, Collison D, Rush C, McConnachie A, Touyz RM, Oldroyd KG, Berry C.. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA Trial. J Am Coll Cardiol 2018;72:2841–2855. [DOI] [PubMed] [Google Scholar]
- 21. Lubbers M, Coenen A, Bruning T, Galema T, Akkerhuis J, Krenning B, Musters P, Ouhlous M, Liem A, Niezen A, Dedic A, van Domburg R, Hunink M, Nieman K.. Sex differences in the performance of cardiac computed tomography compared with functional testing in evaluating stable chest pain. Circ Cardiovasc Imaging 2017;10:e005295.. [DOI] [PubMed] [Google Scholar]
- 22. Williams MC, Hunter A, Shah A, Assi V, Lewis S, Mangion K, Berry C, Boon NA, Clark E, Flather M, Forbes J, McLean S, Roditi G, van Beek EJ, Timmis AD, Newby DE.. Symptoms and quality of life in patients with suspected angina undergoing CT coronary angiography: a randomised controlled trial. Heart 2017;103:995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hemal K, Pagidipati NJ, Coles A, Dolor RJ, Mark DB, Pellikka PA, Hoffmann U, Litwin SE, Daubert MA, Shah SH, Ariani K, Bullock-Palmer RP, Martinez B, Lee KL, Douglas PS.. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease. JACC Cardiovasc Imaging 2016;9:337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sidik NP, McEntegart M, Roditi G, Ford TJ, McDermott M, Morrow A, Byrne J, Adams J, Hargreaves A, Oldroyd KG, Stobo D, Wu O, Messow CM, McConnachie A, Berry C.. Rationale and Design of the British Heart Foundation (BHF) coronary microvascular function and CT coronary angiogram (CorCTCA) study. Am Heart J 2019;doi:10.1016/j.ahj.2019.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pagidipati NJ, Hemal K, Coles A, Mark DB, Dolor RJ, Pellikka PA, Hoffmann U, Litwin SE, Udelson J, Daubert MA, Shah SH, Martinez B, Lee KL, Douglas PS.. Sex differences in functional stress test versus CT angiography in symptomatic patients with suspected CAD: insights from PROMISE. J Am Coll Cardiol 2016;67:2607–2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Napp AE, Haase R, Laule M, Schuetz GM, Rief M, Dreger H, Feuchtner G, Friedrich G, Špaček M, Suchánek V, Fuglsang Kofoed K, Engstroem T, Schroeder S, Drosch T, Gutberlet M, Woinke M, Maurovich-Horvat P, Merkely B, Donnelly P, Ball P, Dodd JD, Quinn M, Saba L, Porcu M, Francone M, Mancone M, Erglis A, Zvaigzne L, Jankauskas A, Sakalyte G, Harań T, Ilnicka-Suckiel M, Bettencourt N, Gama-Ribeiro V, Condrea S, Benedek I, Adjić NC, Adjić O, Rodriguez-Palomares J, Garcia del Blanco B, Roditi G, Berry C, Davis G, Thwaite E, Knuuti J, Pietilä M, Kępka C, Kruk M, Vidakovic R, Neskovic AN, Díez I, Lecumberri I, Geleijns J, Kubiak C, Strenge-Hesse A, Do T-H, Frömel F, Gutiérrez-Ibarluzea I, Benguria-Arrate G, Keiding H, Katzer C, Müller-Nordhorn J, Rieckmann N, Walther M, Schlattmann P, Dewey M.. Computed tomography versus invasive coronary angiography: design and methods of the pragmatic randomised multicentre DISCHARGE trial. Eur Radiol 2017;27:2957–2968. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.