Abstract
Aims
To investigate whether diabetes confers higher relative rates of cardiovascular events in women compared with men using contemporary data, and whether these sex-differences depend on age.
Methods and results
All Danish residents aged 40–89 years without a history major adverse cardiovascular events, including heart failure, as of 1 January 2012 until 31 December 2016 were categorized by diabetes-status and characterized by individual-level linkage of Danish nationwide administrative registers. We used Poisson regression to calculate overall and age-dependent incidence rates, incidence rate ratios, and women-to-men ratios for myocardial infarction, heart failure, ischaemic stroke, or cardiovascular death (MACE-HF). Among 218 549 (46% women) individuals with diabetes, the absolute rate of MACE-HF was higher in men than in women (24.9 vs. 19.9 per 1000 person-years). Corresponding absolute rates in men and women without diabetes were 10.1 vs. 7.0 per 1000 person-years. Comparing individuals with and without diabetes, women had higher relative rates of MACE-HF than men [2.8 (confidence interval, CI 2.9–2.9) in women vs. 2.5 (CI 2.4–2.5) in men] with a women-to-men ratio of 1.15 (CI 1.11–1.19, P < 0.001). The relative rates of MACE-HF were highest in the youngest and decreased with advancing age for both men and women, but the relative rates were higher in women across all ages, with the highest women-to-men ratio between age 50 and 60 years.
Conclusion
Although men have higher absolute rates of cardiovascular complications, the relative rates of cardiovascular complications associated with diabetes are higher in women than in men across all ages in the modern era.
Keywords: Cardiovascular disease, Diabetes
See page 1354 for the editorial comment on this article (doi: 10.1093/eurheartj/ehz914)
Introduction
Type 2 diabetes (diabetes) and male sex are well-established risk factors for the development of cardiovascular disease (CVD), but several studies have shown that the impact of diabetes on CVD may be greater in women than in men. Older studies have predominantly observed that women have excess rates of coronary heart disease,1 heart failure,2 stroke,1 CVD-related death,3 and all-cause mortality associated with diabetes.4 However, these studies were based on data collected prior to year 2000 and may not apply in the modern era due to changes in the definition, incidence, and management of diabetes over the past two decades.5 In fact, newer studies using data from the past two decades are inconsistent regarding sex-differences in the relative rates of coronary heart disease,6–8 heart failure,6,8,9 stroke,6,7,9 death from coronary heart disease,10,11 and all-cause mortality10–12 associated with diabetes. It remains uncertain whether sex-differences persist in the relative impact of diabetes on CVD and mortality, and whether these sex-differences depend on age is poorly investigated. Lastly, whether these sex-differences on the relative impact of diabetes are also present in recurrent events of cardiovascular complications remain largely unknown.
The aims of this study were, therefore, based on contemporary data, first to investigate whether diabetes is associated with higher rates of major adverse cardiovascular events, including heart failure (MACE-HF), and all-cause mortality in women compared with men, and if so, whether potential sex-differences in the relative impact of diabetes depend on age, and whether they persist in recurrent events of cardiovascular complications.
Methods
Data sources
All residents in Denmark receive a unique and permanent civil registration number at birth or immigration that enables individual-level linkage between nationwide registries. Data for this study were obtained from: (i) the Danish Civil Registration System registry (sex, date of birth, immigration, emigration, and vital status), (ii) the Danish National Patient Registry [discharge diagnoses coded according to the International Classification of Diseases (ICD)-8 since 1977, and ICD-10 system since 1994], (iii) the Danish National Prescription Registry [claimed prescriptions since 1995 according to the Anatomical Therapeutic Classification (ATC)], and (iv) the Danish National Causes of Death Registry (primary and underlying causes of death from death certificates). All registries have been validated previously.13,14
Population
Throughout the article, we refer to type 2 diabetes as ‘diabetes’, since we excluded individuals with type 1 diabetes. The study population comprised all individuals in Denmark aged 40–89 years between 1 January 2012 and 31 December 2016. Patients entered the study on 1 January 2012 or when they turned 40, whichever came first. Diabetes-exposure time was defined as time in study. Incident diabetes was defined by initiation of treatment with an antidiabetic medication (ATC = A10); this definition has a positive predictive value (PPV) of 95% and a sensitivity of 72% in Danish registries.15 We excluded individuals with type 1 diabetes, defined as monotherapy with insulin (ATC = A10A) before age 30 years. If the only drug dispensations were metformin (ATC = A10BA02) in women <40 years of age, the individual was considered to have possible polycystic ovary syndrome, and these dispensations were not counted. Thus, claimed prescriptions after age 40 years for women with a diagnosis of possible polycystic ovary syndrome were considered as diabetes medications and lead to inclusion at the first date of purchase after the 40th birthday. For women without diabetes prior to pregnancy [42 weeks prior to giving birth (ICD-10 codes O80–84)], who claimed a prescription for insulin between 42 weeks prior to and 30 days after giving birth were considered as having gestational diabetes, and dispensations of glucose-lowering medication during and in relation to pregnancy were not considered. We excluded patients with a diagnosis of coronary artery disease, heart failure, or ischaemic stroke prior to study entry, as well as individuals who immigrated to Denmark after 1 January 2012.
The exposure time of individuals was categorized according to the presence of diabetes; i.e. each individual contributed to diabetes-free exposure time until the date of diabetes diagnosis and contributed to diabetes with exposure time after the date of diagnosis. Patients with a diagnosis of diabetes and an event of interest on the same day were analysed as being free of diabetes prior to the event.
Comorbidities (atrial fibrillation, hypertension, dyslipidaemia, chronic renal failure, and chronic obstructive pulmonary disease) and medications (antidiabetic, antihypertensive, and anticoagulant drugs and statins) were identified based on ICD- and ATC-codes (Supplementary material online, Table S1) for individuals entering the study in 1 January 2012. Hypertension was defined as treatment with at least two classes of antihypertensive drugs within 180 days prior to 1 January 2012, as previously validated,16 and dyslipidaemia was defined as claimed prescriptions of lipid-modifying agents. Medications were defined as dispensed prescriptions within 180 days prior to 1 January 2012.
Outcomes
The primary outcome was MACE-HF, comprising the composite of first-time myocardial infarction, heart failure, ischaemic stroke, or cardiovascular death (ICD-10-codes in Supplementary material online, Table S1), whichever came first. The secondary outcomes were first and second occurrence of myocardial infarction, heart failure, ischaemic stroke, and all-cause mortality. A grace period of 30 days was used for recurrent outcomes, thus a recurrent outcome could only be classified as a recurrent outcome 30 days following the first-time event. The diagnoses for the first-time endpoints have been validated in Danish registers with high positive predictive value, i.e. 97% (men 97%, women 97%) for myocardial infarction, 83.6% (men 85.4%, women 81.5%) for heart failure, and 97% for ischaemic stroke.17–19 The definition of ischaemic stroke included diagnoses of ischaemic stroke and unspecified stroke, as the majority of unspecified strokes in prior validation studies were of ischaemic origin.19 Discharge diagnoses for recurrent events have been validated with lower positive predictive values, i.e. 88% (men 88%, women 87%) for myocardial infarction and 66% for heart failure,17,18 with no validity on recurrent ischaemic stroke.
Statistics
All individuals were followed from the date of entry until either the first-time event of interest, death, emigration, age 90 years or 31 December 2016, whichever came first. For recurrent events, all individuals alive 30 days after the first-time event were followed from that day until either the recurrent event, death, emigration, age 90 years or 31 December 2016, whichever came first.
We present population characteristics on 1 January 2012 as medians with interquartile ranges for continuous variables, and as counts with percentages for categorical variables. We use Poisson regression to calculate overall and age-dependent incidence rates (IRs), rate ratios (IRRs), and women-to-men ratios (WMR). We report incidence rates (IR = events/1000 person-years), incidence rate ratios (IRR = IRdiabetes/IRnon-diabetes), and women-to-men ratios (WMR = IRRwomen/IRRmen) with 95% confidence intervals (CIs). In age-dependent Poisson regression, age (40–89 years of age) is divided in 1-year bands and updated consecutively throughout the study period, allowing to study a non-linear age effect using thin plate splines.20 We calculate a two-sided P-value for the overall WMRs. We set the significance level to 5%.
In secondary analyses, we repeat all analyses with first-time myocardial infarction, first-time heart failure, first-time ischaemic stroke, and all-cause mortality as outcome, and age-dependent analyses on recurrent myocardial infarction, heart failure, and ischaemic stroke in the subgroup of patients with a first-time event, respectively.
We conduct an age-dependent sensitivity analysis for first-time MACE-HF, excluding individuals with a diagnosis of diabetes and a diagnosis of MACE-HF on the same day. We further conduct sensitivity analyses on first-time MACE-HF and ischaemic stroke, in which age-dependent analyses are stratified by status of atrial fibrillation, excluding individuals with a diagnosis of atrial fibrillation and an event of interest on the same day. All statistical analyses were conducted using R.
Ethics
Retrospective register studies do not need ethical approval in Denmark. The Danish Data Protection Agency has approved the project (reference number 2007-58-015/GEH 2014-014, I-Suite no: 02734).
Results
The study included 148 385 (47% women) individuals with prevalent diabetes on 1 January 2012 (Table 1), 66 078 individuals (46% women) with incident diabetes between 2012 and 2017, and 4086 individuals (35% women) with diabetes prior to age 40 years, who were included at age 40 years (Supplementary material online, Figure S1). Population characteristics in 1 January 2012 showed that individuals with diabetes had higher levels of comorbidities and treated comorbidities than those without diabetes, but that the comorbidities and treated comorbidities were somewhat similar between men and women irrespective of diabetes-status (Table 1).
Table 1.
Population characteristics in 1 January 2012
| Women |
Men |
|||
|---|---|---|---|---|
| No diabetes (N = 1 266 291) | Diabetes (N = 69 057) | No diabetes (N = 1 132 245) | Diabetes (N = 79 328) | |
| Age, median (IQR) | 57.3 (48.1–67.3) | 65.4 (56.1–73.7) | 55.2 (47.2–65.0) | 63.7 (55.2–70.5) |
| Comorbidity (%) | ||||
| Atrial fibrillation | 23 380 (1.9) | 2998 (4.3) | 29.767 (2.6) | 4342 (5.5) |
| Chronic renal failure | 4815 (0.4) | 1116 (1.6) | 5263 (0.5) | 1484 (1.9) |
| COPD | 34 610 (2.7) | 3.942 (5.7) | 24 963 (2.2) | 3631 (4.6) |
| Dyslipidaemia | 201 645 (15.9) | 51 255 (74.2) | 155 692 (13.8) | 58 121 (73.3) |
| Hypertension | 189 761 (15.0) | 32 948 (47.7) | 142 542 (12.6) | 36 740 (46.3) |
| Diabetes duration, years (%) | ||||
| <5 | — | 31 873 (46.2) | — | 37 162 (46.9) |
| 5–10 | — | 17 469 (25.3) | — | 20 739 (26.1) |
| 10–15 | — | 9984 (14.5) | — | 11 503 (14.5) |
| >15 | — | 9731 (14.1) | — | 9924 (12.5) |
| Highest attained education (%) | ||||
| Basic school | 385 199 (30.4) | 33 419 (48.4) | 278 194 (24.6) | 27 378 (34.5) |
| High school | 45 917 (3.6) | 1647 (2.4) | 45 913 (4.1) | 2573 (3.2) |
| Vocational education | 438 464 (34.6) | 21 109 (30.6) | 471 632 (41.7) | 32 776 (41.3) |
| Short/medium length higher education | 295 451 (23.3) | 9021 (13.1) | 194 885 (17.2) | 9951 (12.5) |
| Long higher education, research | 70 318 (5.6) | 1528 (2.2) | 99 966 (8.8) | 3980 (5.0) |
| Unknown | 30 942 (2.4) | 2333 (3.4) | 41 655 (3.7) | 2670 (3.4) |
| Ethnicity (%)a | ||||
| Danish | 1 173 585 (92.7) | 60 738 (88.0) | 1 041 692 (92.0) | 70 363 (88.7) |
| Immigrants | 90 555 (7.2) | 8234 (11.9) | 88 438 (7.8) | 8824 (11.1) |
| Offspring of first-generation immigrants | 2137 (0.2) | 85 (0.1) | 2101 (0.2) | 141 (0.2) |
| Medicine (%) | ||||
| Antidiabetics | ||||
| Metformin | — | 44 787 (64.9) | — | 52 720 (66.5) |
| Insulin | — | 15 711 (22.8) | — | 19 592 (24.7) |
| Sulfonylureas | — | 12 902 (18.7) | — | 17 103 (21.6) |
| GLP1-analogues | — | 4456 (6.5) | — | 5243 (6.6) |
| DPP4-inhibitors | — | 3128 (4.5) | — | 3933 (5.0) |
| Anticoagulants | ||||
| Aspirin | 78 235 (6.2) | 20 089 (29.1) | 65 458 (5.8) | 24 878 (31.4) |
| ADP-receptor inhibitors | 82 326 (6.5) | 20 555 (29.8) | 68 857 (6.1) | 25 353 (32.0) |
| Vitamin K-antagonists | 15 122 (1.2) | 2194 (3.2) | 20 583 (1.8) | 3437 (4.3) |
| NOAC | 2691 (0.2) | 234 (0.3) | 2479 (0.2) | 293 (0.4) |
| Other | ||||
| Beta-blockers | 96 292 (7.6) | 13 183 (19.1) | 61 182 (5.4) | 12 969 (16.4) |
| Calcium channel blockers | 111 520 (8.8) | 18 281 (26.5) | 96 816 (8.6) | 23 274 (29.3) |
| RASi | 198 103 (15.6) | 39 503 (57.2) | 169 647 (15.0) | 48 304 (60.9) |
| Statins | 151 668 (12.0) | 41 897 (60.7) | 118 798 (10.5) | 47 090 (59.4) |
ADP, adenosine diphosphate; COPD, chronic obstructive pulmonary disease; DPP4, dipeptidyl peptidase 4; GLP1, glucagon-like peptide 1; IQR, interquartile range; NOAC, novel oral anticoagulant; RASi, renin–angiotensin system inhibitors.
Data missing for 56 individuals.
Incidence rates
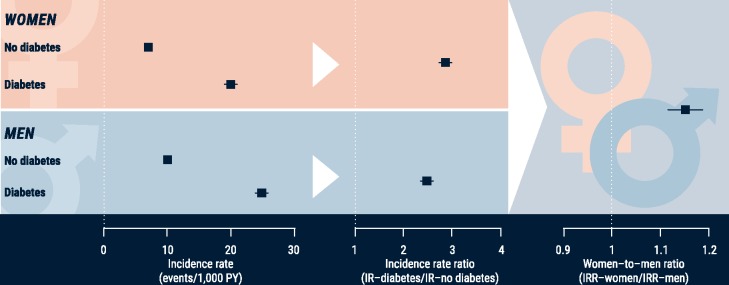
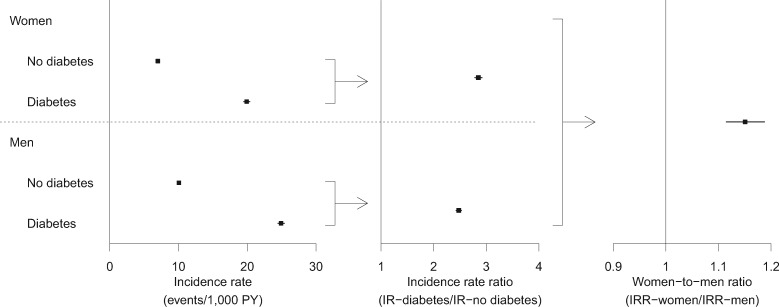
During above 13 million person-years of follow-up, 121 745 new-onset MACE-HF events were identified (Table 2), consisting of 30 884 myocardial infarctions, 27 731 heart failures, 40 938 ischaemic strokes, and 37 096 CVD deaths. There were 7744 MACE-HF events in women with diabetes over 389 thousand person-years of follow-up, equal to an IR of 19.9/1000 person-years (Take home figure, Figure 1, Table 2, Supplementary material online, Table S3); there were 45 027 MACE-HF events in women without diabetes over 6.4 million person-years of follow-up, yielding an IR of 7.0/1000 person-years; the IRR for women (diabetes:no diabetes) was therefore 2.8 (CI 2.8–2.9). The corresponding IRR for men was 2.5 (CI 2.4–2.5) based on IRs of 24.9/1000 person-years in men with diabetes and 10.1/1000 person-years in men without diabetes. The IRR for women was significantly higher than the IRR for men: WMR = IRRwomen/IRRmen = 1.15 (CI 1.11–1.19, P < 0.001) (Take home figure, Figure 1). This relationship was evident for all the secondary outcomes, with WMRs of 1.34 (CI 1.25–1.43, P < 0.001) for myocardial infarction, 1.13 (CI 1.07–1.19, P < 0.001) for heart failure, 1.09 (CI 1.03–1.15, P = 0.004) for ischaemic stroke, but not for all-cause mortality 1.03 (CI 1.00–1.06, P = 0.069) (Supplementary material online, Figure S1A–D, Supplementary material online, Tables S2 and S3).
Table 2.
Number of events, risk time, and age at MACE-HF according to sex and diabetes-status
| Women |
Men |
|||
|---|---|---|---|---|
| No diabetes | Diabetes | No diabetes | Diabetes | |
| Number of first-time events and risk time according to age-group (1000 PY) | ||||
| 40–49 | 2262 (1874) | 193 (44) | 4567 (1877) | 402 (51) |
| 50–59 | 4469 (1708) | 681 (84) | 9996 (1643) | 1439 (110) |
| 60–69 | 8463 (1503) | 1429 (115) | 15 297 (1300) | 3185 (149) |
| 70–79 | 12 830 (940) | 2604 (99) | 15 691 (700) | 3725 (105) |
| 80–89 | 17 003 (411) | 2837 (47) | 12 279 (225) | 2393 (32) |
| Total | 45 027 (6438) | 7744 (389) | 57 830 (5745) | 11 144 (447) |
| Median age at time at first-time event (IQR) | 75.9 (66.1–83.4) | 76.1 (67.9–82.9) | 69.3 (59.8–78.4) | 71.1 (63.8–78.7) |
IQR, interquartile range; MACE-HF, major adverse cardiovascular events including heart failure; PY, person-years.
Take home figure.
Sex-differences with diabetes. Although men have higher absolute rates of major adverse cardiovascular events including heart failure, the relative rates of major adverse cardiovascular events including heart failure associated with diabetes are higher in women. IR, incidence rates; IRR, incidence rate ratios; MACE-HF, major adverse cardiovascular events including heart failure; PY, person-years.
Figure 1.
Overall incidence rates, incidence rate ratios, and women-to-men ratios of first-time major adverse cardiovascular events including heart failure, stratified by diabetes-status (incidence rates only) and sex (incidence rates and incidence rate ratios only). Higher incidence rate ratio in men if women-to-men ratios <1, and higher incidence rate ratio in women if women-to-men ratios >1. IR, incidence rates; IRR, incidence rate ratios; MACE-HF, major adverse cardiovascular events including heart failure; PY, person-years; WMR, women-to-men ratios.
Age-specific incidence rates
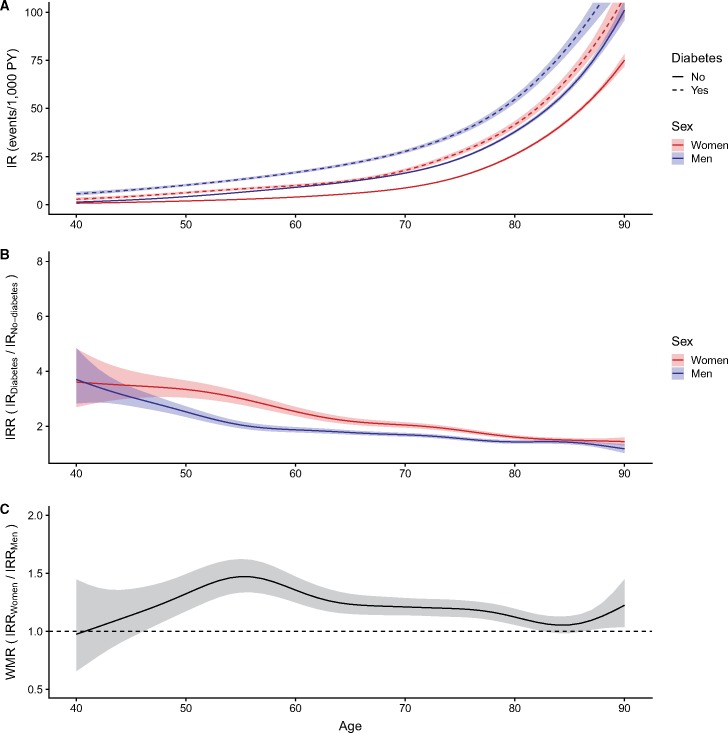
The IRs of MACE-HF and all secondary outcomes increased with advancing age and were higher in men than in women irrespective of diabetes-status and age (Figure 2A, Supplementary material online, Figures S3–S6A). Regardless of diabetes-status and outcome, women were older than men at time of event with myocardial infarction presenting at the lowest median age (74.4 for women with diabetes, 68.4 for men with diabetes) and heart failure (76.8 for women with diabetes, 71.2 for men with diabetes) and all-cause death at the highest (77.1 for women with diabetes, 73.2 for men with diabetes; Table 2, Supplementary material online, Tables S2A–S2D).
Figure 2.
(A–C) Incidence rates (A), incidence rate ratios (B), and women-to-men ratios (C) of first-time major adverse cardiovascular events including heart failure according to age, stratified by diabetes-status (incidence rates only) and sex (incidence rates and incidence rate ratios only). Higher incidence rate ratio in men if women-to-men ratios <1, and higher incidence rate ratio in women if women-to-men ratios >1. IR, incidence rates; IRR, incidence rate ratios; MACE-HF, major adverse cardiovascular events including heart failure; PY, person-years; WMR, women-to-men ratios.
The sex-specific relative rates (diabetes:no diabetes) for all outcomes were highest in the youngest individuals and decreased with advancing age (Figure 2B, Supplementary material online, Figures S3–S6B). The IRRs for MACE-HF were higher in women than in men at all ages, with the highest women-to-men ratio between age 50 and 60 years (Figure 2C), although insignificant from age < 45 years. Somewhat similar findings were evident for all secondary outcomes, although not in the young for ischaemic stroke (age < 45 years) in which men had higher relative rates compared with women (Supplementary material online, Figures S3–S6). Excluding events on the same day as the diagnosis of diabetes did not change the results (Supplementary material online, Figures S7–S11).
In individuals without atrial fibrillation, the women-to-men-ratio for MACE-HF and ischaemic stroke were largely unchanged. In individuals with atrial fibrillation, we identified 33 513 events of MACE-HF and 9736 events of ischaemic stroke with a risk-time of 62 000 and 65 000 person-years, respectively (Supplementary material online, Table S4A and B), and we confirmed the findings for MACE-HF, whereas we observed no sex difference in IRRs of ischaemic stroke in individuals with atrial fibrillation across all ages (Supplementary material online, Figures S12 and S13).
During the 30-day grace period for analyses of recurrent events, patients were largely excluded due to death, with the highest mortality among patients with diabetes and the elderly, whereas men and women had a largely comparable mortality across age-groups regardless of diabetes-status (Supplementary material online, Tables S5A–S5C). Irrespective of diabetes, the IRs of recurrent myocardial infarction, heart failure, and ischaemic stroke generally increased with advancing age in men and women (Supplementary material online, Figures S14–S16A). We observed comparable IRs as well as IRRs in women and men for all recurrent events across all ages and irrespective of diabetes status, except for recurrent myocardial infarction in subgroups of men. In men with diabetes above age 55 years, the IRs of recurrent myocardial infarction were higher than in men without diabetes, and in individuals older than age 75 years, we observed higher IRRs of recurrent myocardial infarction in men than in women (Supplementary material online, Figures S14–S16B and C).
Discussion
In this nationwide study, we observed that although men have higher rates of first-time cardiovascular complications, the relative rate of first-time cardiovascular complications associated with diabetes are higher in women than in men across all ages in the modern era. However, in recurrent events these sex-differences in the relative rate of cardiovascular complications were no longer present.
These results are similar to a study using recent data, which reported a non-significantly higher relative rate of first-time MACE (without heart failure), myocardial infarction, and stroke associated with diabetes in women compared with men,7 but only patients with newly diagnosed diabetes were included limiting comparisons between the studies. Interestingly, while their association in relative rates were attenuated in both sexes from the unadjusted to the fully adjusted model, their results in WMRs remained unchanged, indicating that the relation of relative ratios between sexes may not be affected majorly by these potential confounders. Furthermore, conflicting findings from other studies using data from the past two decades are evident, as some studies have observed a significant excess rate in women regarding coronary heart disease,6,8 heart failure,8,9 death from coronary heart disease,11 and all-cause death10,11 associated with diabetes, while others observed no differences between sexes for heart failure,6 stroke,6 death from myocardial infarction,10 and all-cause mortality.12 Although most of these studies were large, our study had sufficient power to study sex-differences in all ages, including sufficient events in the young, and observed that women had a higher relative rate of MACE-HF and all secondary outcomes across all ages compared with men, although not at age < 45 years for ischaemic stroke.
Most studies investigating how sex-differences in the relative impact of diabetes on cardiovascular complications and mortality vary with age have used wide age-groups, thus not illustrating the full age effect.6–8,12 A recent study found that the WMRs for cardiovascular complications were age-dependent, with higher relative rates for coronary heart disease, stroke, and heart failure in women among younger individuals, with no difference in relative rates from age > 75 years,8 but age at diagnosis among newly diagnosed diabetes were included limiting the comparison with our study. In contrast to this and other studies,6,7,12 we observed WMRs to peak in the middle-aged (age 50–59 years) with lower WMRs at young and old age for MACE-HF, ischaemic stroke, and all-cause mortality. It is uncertain why, but all outcomes are rare in young individuals, especially in women, who generally experience their cardiovascular event and death later than men,21 thus the increased cardiovascular rate associated with diabetes may not yet have become apparent in young women. Furthermore, the level of hypertension is known to increase at a faster pace with advancing age, especially after menopause, in women compared with men.22 However, both arguments are in contrast with our results for myocardial infarction and heart failure for which the highest WMRs were observed at youngest age and decreased with advancing age.
Older studies have observed higher relative rates of recurrent myocardial infarction23,24 and stroke25 associated with diabetes, although none of them showed an age-effect. Contrarily, we observed broadly comparable rates of all recurrent events between patients with and without diabetes across all ages, with the exception of recurrent myocardial infarction in men, in which rates were significantly higher from age > 55 years in diabetic men compared with non-diabetic men. Our study cannot address why we observed a reduced impact of diabetes on recurrent cardiovascular outcomes compared with prior studies, but may be secondary to improvements in risk factor management in patients with diabetes and cardiovascular complications.5 Two of the prior studies stratified their analyses by sex and found higher relative rates of recurrent myocardial infarction in women compared with men.23,24 Conversely, we observed higher relative rates of myocardial infarction in men from age > 75 years compared with women, and no difference in relative rates of recurrent discharge of heart failure and ischaemic stroke across all ages between men and women.
Diabetes may confer higher relative rates of first-time cardiovascular complications in women because of interaction with sex hormones, since diabetes appears to attenuate the protective effect of oestrogen regarding atherosclerosis,26 as supported by the declining WMR of first-time events with advancing age as observed in our results. Other explanations could be differences in the cardiovascular risk factor burden, sex-differences in the healthcare provided for the prevention, management and treatment of diabetes and its complications (e.g. worse glycaemic control in women),27 or women being less adherent to guideline-recommended treatment.28 Given the lower absolute rate of CVD in women than in men, these findings may merely be explained by a comparable rate difference that leads to higher relative rates in women. It is unknown why these sex-differences appeared to diminish for recurrent events, but potentially secondary prophylaxis in patients with established cardiovascular complications attenuates the observed sex-differences, men and women are more equal regarding recurrent CVD events associated with diabetes in individuals with established CVD, or our population with first-time events was too small to detect statistically significant sex-differences.
Strengths and limitations
The major strengths of this nationwide study include minimal risk of selection bias, minimal loss to follow-up ensured by the comprehensive Danish registries and the large sample size with more than 13 million person-years. This enabled us to study sex-differences in associations between diabetes on cardiovascular events and mortality with sufficient power in all ages following the introduction of the new diabetes definition in Denmark at 1 January 2012 over a relatively short study period, but important limitations need to be addressed.
The primary limitation to this study is that our results rely on discharge diagnoses of myocardial infarction, heart failure, ischaemic stroke, and cardiovascular death reported in the medical charts at the hospitals and not on clinical data,29 but potential minor misclassifications are non-systematic and do not influence the overall validity of the data.13 Although the diagnoses of diabetes, myocardial infarction, and ischaemic stroke have high positive predictive values, and myocardial infarction a high sensitivity,29 PPVs by sex for diabetes and ischaemic stroke are unknown, and recurrent outcomes are validated with relatively lower PPVs. An older study revealed a high PPV and specificity, but a low sensitivity for the heart failure diagnosis of 29%,30 which should be acknowledged in the interpretation of the results. Furthermore, we cannot rule out that the true rates of diabetes, particularly all diet-treated cases, and cardiovascular events may have been underestimated, which may have biased our results. However, despite these limitations, our results generally concur with previous studies exploring sex-differences in the relative impact of diabetes on CVD and mortality.
Secondly, we did not have access to information on metabolic control (glucose-levels, lipids, and blood pressure), imaging (echocardiography including measures of diastolic function), or lifestyle factors (smoking, alcohol consumption, body mass index, physical activity level, or diet).
Thirdly, since the majority of diagnoses of gestational diabetes and polycystic ovary syndrome are diagnosed in private practice, we used prescribed antidiabetics to define both diagnoses, which have not been validated. Our definitions capture women with gestational diabetes treated with insulin during pregnancy along with women with polycystic ovary syndrome treated with metformin. Although this also excluded women in monotherapy of metformin age < 40 years due to a diagnosis of diabetes from the diabetes exposure-time, these women would re-enter from age 40 years if still claiming prescriptions for antidiabetic medication. Women with polycystic ovary syndrome treated with metformin age > 40 years were not accounted for, thus may have contributed with risk time without many events, as polycystic ovary syndrome is not as strongly associated with CVD as diabetes. However, this is considered to be a minor group of women, thus it unlikely affected our results significantly.
Lastly, the majority of the Danish population is Caucasian, and we did not include individuals immigrating to Denmark during our study period due to unknown medical history, thus our results may not be generalizable to non-Caucasian people.
Conclusions
In this nationwide study, we observed that although men have higher absolute rates of first-time cardiovascular complications, the relative rate of first-time cardiovascular complications are higher in women than in men across all ages in the modern era. Secondly, these sex-differences are not present in recurrent cardiovascular outcomes. Further studies are warranted to more clearly elucidate the mechanisms responsible for the substantial sex-differences in diabetes-related first-time cardiovascular complications.
Funding
This work was funded by the Danish Heart Foundation (Grant number: 18-R121-A8218).
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplementary Material
References
- 1.The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010;375:2215–2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kannel WB, Hjortland M, Castelli WP.. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol 1974;34:29–34. [DOI] [PubMed] [Google Scholar]
- 3. Kannel WB, McGee DL.. Diabetes and cardiovascular disease. The Framingham study. JAMA 1979;241:2035–2038. [DOI] [PubMed] [Google Scholar]
- 4.Prospective Studies Collaboration and Asia Pacific Cohort Studies Collaboration. Sex-specific relevance of diabetes to occlusive vascular and other mortality: a collaborative meta-analysis of individual data from 980 793 adults from 68 prospective studies. Lancet Diabetes Endocrinol 2018;6:538–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson A-M, Miftaraj M, McGuire DK, Sattar N, Rosengren A, Gudbjörnsdottir S.. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 2017;376:1407–1418. [DOI] [PubMed] [Google Scholar]
- 6. Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, Deanfield J, Smeeth L, Timmis A, Hemingway H.. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1·9 million people. Lancet Diabetes Endocrinol 2015;3:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wright AK, Kontopantelis E, Emsley R, Buchan IE, Mamas MA, Sattar N, Ashcroft DM, Rutter MK.. Cardiovascular risk and risk factor management in type 2 diabetes: a population-based cohort study assessing sex disparities. Circulation 2019;139:2742.. [DOI] [PubMed] [Google Scholar]
- 8. Sattar N, Rawshani A, Franzén S, Rawshani A, Svensson A-M, Rosengren A, McGuire DK, Eliasson B, Gudbjörnsdottir S.. Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks. Circulation 2019;139:2228–2237. [DOI] [PubMed] [Google Scholar]
- 9. McAllister DA, Read SH, Kerssens J, Livingstone S, McGurnaghan S, Jhund P, Petrie J, Sattar N, Fischbacher C, Kristensen SL, McMurray J, Colhoun HM, Wild SH.. Incidence of hospitalization for heart failure and case-fatality among 3.25 million people with and without diabetes mellitus. Circulation 2018;138:2774–2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roche MM, Wang PP.. Sex differences in all-cause and cardiovascular mortality, hospitalization for individuals with and without diabetes, and patients with diabetes diagnosed early and late. Diabetes Care 2013;36:2582–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bragg F, Holmes MV, Iona A, Guo Y, Du H, Chen Y, Bian Z, Yang L, Herrington W, Bennett D, Turnbull I, Liu Y, Feng S, Chen J, Clarke R, Collins R, Peto R, Li L, Chen Z.. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 2017;317:280–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alegre-Díaz J, Herrington W, López-Cervantes M, Gnatiuc L, Ramirez R, Hill M, Baigent C, McCarthy MI, Lewington S, Collins R, Whitlock G, Tapia-Conyer R, Peto R, Kuri-Morales P, Emberson JR.. Diabetes and cause-specific mortality in Mexico City. N Engl J Med 2016;375:1961–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lynge E, Sandegaard JL, Rebolj M.. The Danish National Patient Register. Scand J Public Health 2011;39:30–33. [DOI] [PubMed] [Google Scholar]
- 14. Kildemoes HW, Sørensen HT, Hallas J.. The Danish National Prescription Registry. Scand J Public Health 2011;39:38–41. [DOI] [PubMed] [Google Scholar]
- 15. Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K.. The National Diabetes Register. Scand J Public Health 2011;39:58–61. [DOI] [PubMed] [Google Scholar]
- 16. Olesen JB, Lip GYH, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen A-M, Gislason GH, Torp-Pedersen C.. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 2011;342:d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sundbøll J, Adelborg K, Munch T, Frøslev T, Sørensen HT, Bøtker HE, Schmidt M.. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open 2016;6:e012832.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Delekta J, Hansen SM, AlZuhairi KS, Bork CS, Joensen AM.. The validity of the diagnosis of heart failure (I50.0-I50.9) in the Danish National Patient Register. Dan Med J 2018;65 https://ugeskriftet.dk/dmj/validity-diagnosis-heart-failure-i500-i509-danish-national-patient-register. [PubMed] [Google Scholar]
- 19. Krarup L-H, Boysen G, Janjua H, Prescott E, Truelsen T.. Validity of stroke diagnoses in a National Register of Patients. Neuroepidemiology 2007;28:150–154. [DOI] [PubMed] [Google Scholar]
- 20. Wood SN. Thin plate regression splines. J R Stat Soc Ser B Stat Methodol 2003;65:95–114. [Google Scholar]
- 21. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L; INTERHEART Study Investigators . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet Lond Engl 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 22. Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension 2001;37:1199–1208. [DOI] [PubMed] [Google Scholar]
- 23. Schramm TK, Gislason GH, Køber L, Rasmussen S, Rasmussen JN, Abildstrøm SZ, Hansen ML, Folke F, Buch P, Madsen M, Vaag A, Torp-Pedersen C.. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk. Circulation 2008;117:1945–1954. [DOI] [PubMed] [Google Scholar]
- 24. Liang H, Vallarino C, Joseph G, Manne S, Perez A, Zhang S.. Increased risk of subsequent myocardial infarction in patients with type 2 diabetes: a retrospective cohort study using the U.K. General Practice Research Database. Diabetes Care 2014;37:1329–1337. [DOI] [PubMed] [Google Scholar]
- 25. Chen W, Pan Y, Jing Jing Z, Xingquan L, Liping M, Xia Wang Y, Wang Y.. Recurrent stroke in minor ischemic stroke or transient ischemic attack with metabolic syndrome and/or diabetes mellitus. J Am Heart Assoc 6:e005446.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dantas APV, Fortes ZB, Carvalho MHC.. Vascular disease in diabetic women: why do they miss the female protection? Exp Diabetes Res 2012;2012:570598.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McGill JB, Vlajnic A, Knutsen PG, Recklein C, Rimler M, Fisher SJ.. Effect of gender on treatment outcomes in type 2 diabetes mellitus. Diabetes Res Clin Pract 2013;102:167–174. [DOI] [PubMed] [Google Scholar]
- 28. Hyun KK, Redfern J, Patel A, Peiris D, Brieger D, Sullivan D, Harris M, Usherwood T, MacMahon S, Lyford M, Woodward M.. Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare. Heart Br Card Soc 2017;103:492–498. [DOI] [PubMed] [Google Scholar]
- 29. Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M.. The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol 2003;56:124–130. [DOI] [PubMed] [Google Scholar]
- 30. Kümler T, Gislason GH, Kirk V, Bay M, Nielsen OW, Køber L, Torp-Pedersen C.. Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail 2008;10:658–660. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.