Summary
Objectives
To develop a clinical practice guideline on orthodontically induced external apical root resorption (EARR), with evidence-based and, when needed, consensus-based recommendations concerning diagnosis, risk factors, management during treatment, and after-treatment care.
Materials and methods
The Appraisal of Guidelines for Research and Evaluation II instrument and the Dutch Method for Evidence-Based Guideline Development were used to develop the guideline. Based on a survey of all Dutch orthodontists, we formulated four clinical questions regarding EARR. To address these questions, we conducted systematic literature searches in MEDLINE and Embase, and we performed a systematic literature review. The quality of evidence was assessed with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach. After discussing the evidence, a Task Force formulated considerations and recommendations. The drafted guideline was sent for comments to all relevant stakeholders.
Results
Eight studies were included. The quality of evidence (GRADE) was rated as low or very low. Only the patient-related risk factors, ‘gender’ and ‘age’, showed a moderate quality of evidence. The Task Force formulated 13 final recommendations concerning the detection of EARR, risk factors, EARR management during treatment, and after-treatment care when EARR has occurred. Stakeholder consultation resulted in 51 comments on the drafted guideline. After processing the comments, the final guideline was authorized by the Dutch Association of Orthodontists. The entire process took 3 years.
Limitations
The quality of the available evidence was mainly low, and patient-reported outcome measures were lacking.
Conclusions/implications
This clinical practice guideline allows clinicians to respond to EARR based on current knowledge, although the recommendations are weak due to low-quality evidence. It may reduce variation between practices and aid in providing patients appropriate information.
Introduction
Orthodontically induced external apical root resorption (EARR) is an unwanted side effect of orthodontic treatment (1). In the available literature, a distinction is made between histologically and radiologically determined EARR. Over 90 per cent of all orthodontically moved teeth are associated with histologically noticeable EARR (2–4). Lower percentages have been reported for radiologically detected EARR. Between 48 and 66 per cent of orthodontically treated teeth show mild to moderate EARR (less than 2.5 mm), and only 1–5 per cent of all moved teeth end up with severe apical root resorption, defined as a loss of 4 mm of the original root length or more than one-third of the root (2–4).
Despite the prevalence and severity of EARR, little is known about the pathology and aetiology. Previously, it was assumed that EARR was caused by complex multifactorial interactions between patient-related factors and treatment-related factors (2). Additionally, there is much uncertainty about how to prevent EARR and how to manage it when it occurs during orthodontic treatments (5). To identify an EARR, a radiologic examination is necessary. However, there is no consensus about the type or timing of radiographs needed for identifying initial EARR during orthodontic treatments. Furthermore, little is known about the long-term stability and prognosis of affected teeth, including their mobility, vitality, and periodontal status, their suitability for prosthetic abutments, or their resistance to masticatory function (5–8). It was calculated that 3 mm of EARR was equivalent to a loss of 1 mm of periodontal attachment (6). When periodontal attachment is lost due to root resorption, it is important to avoid additional alveolar bone destruction that can occur with periodontal disease (9).
There is much uncertainty among orthodontists on how to reduce the risk of EARR as much as possible, how to manage EARR when it occurs during an orthodontic treatment, and what type of after-treatment care is required (5). This uncertainty has given rise to a demand for a clinical practice guideline (CPG). Generally, a CPG is developed for specific topics in health care that are dominated by uncertainty. However, the quality of existing guidelines in orthodontics differs a lot (10). Thereby, an important factor, which determines the quality of a CPG, is the guideline development process and the reporting of this process. It is shown that guidelines that complied with the quality items of the AGREE II instrument scored highly and can be recommended for use (10).
At the end, the CPG aids the clinician in making treatment decisions or in reacting appropriately to (unexpected) problems. A CPG provides evidence-based recommendations (11). Therefore, the aim of this study was to develop a CPG with clinical recommendations for orthodontically induced EARR diagnosis, risk factors, management, and after-treatment care requirements. This CPG was developed for orthodontists, and the target population includes all patients at the start, during, or after a comprehensive orthodontic treatment with full fixed appliances.
Materials and methods
Initiative and Task Force
The Dutch Association of Orthodontists (NVvO, Nederlandse Vereniging van Orthodontisten) initiated the development of a CPG regarding EARR. In 2015, the NVvO established a Task Force, which included four orthodontists (members of the NVvO) and one resident in orthodontics, as representatives of the professional group. The Task Force received methodological and academic support from the Knowledge Institute of the Dutch Association of Medical Specialists and the Radboud University Medical Center, Nijmegen, Department of Dentistry, section of Orthodontics and Craniofacial Biology (The Netherlands). The Patients’ Federation (patients association) was invited to participate in the Task Force, but the Federation declined participation in the design of the guideline; instead, they opted to participate only in commenting on the drafted guideline.
This report follows the Reporting Items for practice Guidelines in Healthcare (RIGHT) statement, which comprise reporting guidelines for CPGs (12). The CPG was developed and written from October 2015 to July 2018.
Guideline development
The CPG was developed in accordance with the Appraisal of Guidelines for Research and Evaluation II (AGREE II) instrument and Evidence-Based Richtlijnontwikkeling (EBRO), the Dutch Method for Evidence-Based Guideline Development (11, 13). The development process for this CPG included a preparation phase, a development phase, a commentary phase, and an authorization phase.
During the preparation phase, in the beginning of 2015, a survey was sent out by the NVvO to all orthodontists in the Netherlands to determine the need for a CPG for EARR, especially for clinically relevant EARR, defined as a loss of 2 mm or more root length. Based on this survey, the most relevant issues were translated by the Task Force into four clinical questions (CQ #1–CQ #4).
Literature search
In the development phase, we conducted a broad systematic literature search (Supplementary Table 1) based on the clinical questions. We searched MEDLINE and Embase with the help of a senior librarian who was specialized in health sciences. Languages were restricted to Dutch and English. The databases were searched up to 15 September 2015. Two members of the Task Force (CS, AMK-J) independently reviewed the literature according to predefined inclusion and exclusion criteria (Table 1).
Table 1.
Inclusion and exclusion criteria for the literature review. SR: systematic review; RCT: randomized control study; CQ #2: clinical question 2; OPT: orthopantomography; PA: periapical radiography; CBCT: cone beam computed tomography
| Inclusion criteria |
|---|
| SR, RCT, cohort study, case-control study |
| Root resorption (decrease in root length) yes/no on a PA, OPT, or CBCT |
| Consecutively selected patients |
| Patients were treated with buccal fixed appliances for at least 6 months |
| Exclusion criteria |
| Cleft lip and palate and other craniofacial disorders |
| Trauma-related orthodontic movements |
| Cervical root resorption |
| Internal root resorption |
| Ectopic eruption of teeth |
| Root damage due to placement of a miniscrew or other surgical procedure |
| Autotransplantation |
| Medication that influences bone metabolism |
| Biological markers |
| Genetic studies |
| In vitro research |
| No multivariate analysis (only relevant for CQ #2 eligibility) |
Initial screening for eligibility was based on the title and abstract. Then, separate screenings were conducted for all clinical questions.
The selected titles were screened again based on the full text. Differences between observers were discussed and resolved by consensus. To collect evidence for CQ #2, we additionally examined all individual studies included in the selected systematic reviews (1–4). The articles that met the inclusion criteria were then used to address the clinical questions.
Data extraction and quality assessment
One examiner (CS) extracted the study characteristics (including the type of study, country, setting), patient characteristics (including the number of participants, mean age, gender distribution), type of intervention, follow-up period, and outcome measures. The second examiner (AMK-J) checked the extracted data.
Data for the risk of bias assessment were organized into tables. Tables of all included randomized controlled trials (RCTs) were constructed with the Cochrane risk of bias tool; tables for non-randomized observational studies were constructed with A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI) (14, 15).
Assessment of the quality of evidence
The assessment of the quality of evidence was undertaken by one examiner (CS) and was checked by the second (AMK-J) and third (SP) examiners. We assessed the quality of evidence according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach (16). The quality assessment included the following aspects: limitations in study design, inconsistencies, indirectness, imprecision, and publication bias. The quality of evidence reflects the degree of confidence in an estimation rather than an evaluation of individual studies (16). The final quality of evidence level (high, moderate, low, very low) was estimated for each clinical question item.
Recommendations
In Task Force meetings, the evidence was discussed and consensus considerations were drawn to guide the development of recommendations. Thus, the recommendations were based on the available evidence combined with the most important considerations. The considerations deemed most important included patient values, costs, facilities availability, and organizational matters. Decisions were made by consensus.
The strength of each recommendation is presented with special expressions according to the GRADE methodology (16). A recommendation starts with a verb. If the recommendation is weak, the recommendation starts with ‘consider’. The strength (strong, weak) of the recommendation depends on, for instance, the quality of evidence, the consensus considerations, and the importance of the Task Force assigned to the different aspects and/or arguments regarding the recommendation. According to the GRADE methodology, it was possible to make a strong recommendation with a low level of evidence and vice versa. Based on the recommendations, an implementation plan will be written.
Commentary and authorization phases
The drafted guideline was sent for commentary to all members of the NVvO, all relevant national dental and health insurer associations, the Health and Youth Care Inspectorate (IGJ), and the Patients’ Federation Netherlands. Each group provided comments on the draft of the guideline within 6 weeks. After reviewing and processing the comments, the final CPG will be approved by the NVvO, and it will be published on their website (www.orthodontist.nl).
Results
Literature search
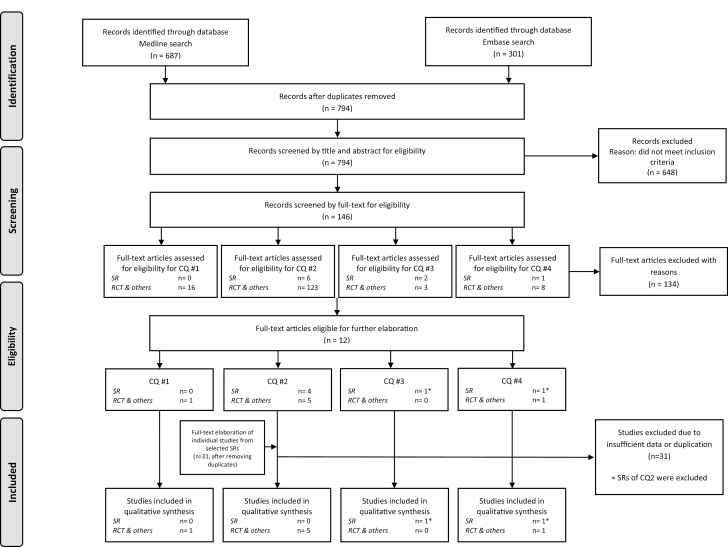
Based on the results of the questionnaire, four clinical questions were formulated (Table 2). The developed search strategy retrieved 687 citations in MEDLINE and 301 in Embase (Supplementary Table 1). After removing the duplicates, 794 studies remained. After screening the titles and abstracts, 648 studies were excluded because they did not meet the inclusion criteria. After a full text screen for eligible studies, we excluded studies because the sample was not consecutively selected (criterion for CQ #1−CQ #4), and because the description of the methodology was unclear or they lacked a multivariate analysis of the data (criteria for CQ #2). A manual search of the reference lists in the included systematic reviews did not reveal additional studies. A total of eight studies were included in the qualitative synthesis (Figure 1).
Table 2.
Clinical questions identified in a survey of Dutch orthodontists; these questions should be addressed in the clinical practice guideline. EARR: external apical root resorption
| 1. What types of radiographs enable the diagnosis/detection of orthodontically induced EARR? |
| 2. What factors increase the risk of developing EARR during orthodontic treatment? |
| 3. What treatment protocol should be followed when EARR has been detected during treatment? |
| 4. What is the follow-up protocol for patients with EARR? |
Figure 1.
Flowchart of the study selection process for the systematic review. *The same SR was used for CQ #3 and CQ #4; CQ: clinical question; SR: systematic review; RCT: randomized controlled trial; others: e.g. observational studies.
For CQ #1, comparisons between cone beam computed tomography (CBCT) and orthopantomography (OPT) and between CBCT and periapical radiography (PA) were previously elaborated as part of another CPG established by the NVvO on radiology in orthodontics (17). Therefore, in the present study, we focussed on the comparison between OPT and PA and the optimal timing of radiological examinations for detecting EARR.
To address CQ #1, we included one observational study (18). To address CQ #2, we included one RCT and four observational studies (8, 19–22). To address CQ #3, we included one systematic review on interventions for EARR management (8). However, the authors of that systematic review could not perform an analysis because no study met the criteria for an adequate level of evidence. To address CQ #4, we included one systematic review and one observational study (5, 23).
Literature analysis and quality of evidence
The data on the risk of bias are in Supplementary Tables 2.1 and 2.2. The evidence from the literature and the quality of evidence for the four clinical questions are described in Table 3. In this table, for each specific clinical question item, the evidence is summarized and the GRADE level (‘Quality of evidence’) is indicated. For CQ #3, we could not draw a conclusion from the literature on an appropriate treatment strategy after the EARR occurred because the only relevant study, a systematic review by Ahangari et al., did not include any eligible studies for addressing this question (5). Moreover, Ahangari et al. did not include any studies that could be used to address CQ #4 (5). One other study was descriptive in character (23); therefore, we decided not to grade the evidence for CQ #4.
Table 3.
Literature conclusions and quality of evidence were determined based on GRADE. GRADE: Grading of Recommendations Assessment, Development, and Evaluation; CQ: clinical question; OPT: orthopantomography; PA: periapical radiography; CBCT: cone beam computed tomography; EARR: external apical root resorption; NiTi: nickel titanium; CuNiTi: copper nickel titanium; SS: stainless steel
| Clinical question item | Evidence | Quality of evidence | Reference |
|---|---|---|---|
| CQ #1—Diagnosis | |||
| OPT versus PA | Given the lack of data, it is not possible to draw a conclusion about the potential added diagnostic value of a periapical radiograph compared to an orthopantomogram. The estimated degree of EARR appeared to be larger when measured on an orthopantomogram than when measured on a periapical radiograph. | Low | (18) |
| CBCT versus OPT | See Guideline for Radiology in orthodontics | (17) | |
| CBCT versus PA | See Guideline for Radiology in orthodontics | (17) | |
| CQ #2—Risk factors | |||
| Patient-related factors | |||
| Gender | There are indications that gender is not an independent predictor of EARR severity. | Moderate | (8, 20–22) |
| Age | There are indications that age is not an independent predictor of EARR severity. | Moderate | (8, 20–22) |
| Trauma | There are indications that trauma preceding an orthodontic treatment is not an independent predictor of EARR severity, although the included studies reported contradictory results. | Low | (8, 20, 21) |
| Endodontically treated teeth | It is not clear whether endodontically treated teeth comprise a risk factor for EARR severity. There are some indications that endodontically treated teeth might be a preventive factor. | Very low | (21) |
| Root and tooth morphology | There are indications that root width is not an independent predictor of EARR severity, but the included studies reported contradictory results. There are indications that abnormal root shape is not an independent predictor of EARR severity, but the included studies reported contradictory results. |
Low | (8, 21) |
| Pre-treatment tooth/root length | It is not clear whether pre-treatment tooth or root length is associated with EARR severity. The studies reported contradictory results. | Very low | (8, 21, 22) |
| Agenesis | There are indications that agenesis is not an independent predictor of EARR severity. | Low | (8) |
| Earlier orthodontic treatment | There are indications that earlier orthodontic treatment is not an independent predictor of EARR severity. There are indications that an earlier orthodontic treatment is a preventive factor for the degree of EARR during the next orthodontic treatment. | Low | (8, 21) |
| Lip/tongue dysfunction/habits | It is not clear whether patients with lip and/or tongue dysfunctions are at increased risk of developing more severe EARRs. The studies reported contradictory results. | Very low | (20, 21) |
| Impacted canines | It is not clear whether the correction of impacted canines is associated with EARR severity. The studies reported contradictory results. | Very low | (20, 21) |
| Overjet | It is not clear whether an increased overjet has an influence on EARR severity. The included studies reported no association between overjet and EARR severity. | Very low | (20, 21) |
| Overbite | There are indications that an increased overbite has no influence on EARR severity. The included studies reported no association between overbite and EARR severity. | Low | (20, 21) |
| Angle classification | It is not clear whether the Angle classification is associated with EARR severity. The included study reported no association between the Angle classification and EARR severity; however, we have low confidence in this finding. | Very low | (21) |
| Treatment-related factors | |||
| Duration of active treatment | There are indications that the duration of active treatment is not an independent predictor of EARR severity. | Low | (8, 20–22) |
| Duration of rectangular wire use | It is not clear whether the degree of EARR is related to the amount of treatment time with rectangular wires. These studies reported contradictory results. | Low | (8, 20, 21) |
| Horizontal apical displacement | It is not clear whether horizontal apical root displacements are associated with EARR severity. The included study reported a positive correlation; however, we have low confidence in this finding. | Very low | (21) |
| Vertical apical displacement | It is not clear whether vertical apical root displacements are associated with EARR severity. The included study reported no association between vertical apical displacement and EARR severity. | Very low | (21) |
| Overjet reduction | It is not clear whether reducing a large overjet during the fixed appliance phase has an influence on EARR severity. The included study reported no association between overjet reduction and EARR severity. | Very low | (20) |
| Extraction versus non-extraction | There are indications that the extraction of premolars is an independent predictor of EARR severity. | Low | (8) |
| Elastics, Class II | It is not clear whether wearing Class II elastics have an influence EARR severity. The included studies reported contradictory results. | Very low | (20, 21) |
| Elastics, anterior vertical | There are weak indications that wearing anterior vertical elastics is no independent predictor of EARR severity, except for the maxillary cuspids. | Low | (8, 21) |
| Wire sequence or type | The wire sequence or wire type do not have an influence on EARR severity (0.016 NiTi, 0.018 × 0.025 NiTi, 0.019 × 0.025 SS; or 0.016 NiTi, 0.016 SS, 0.020 SS, 0.019 × 0.025 SS; or 0.016 × 0.022 CuNiTi, 0.019 × 0.025 CuNiTi, 0.019 × 0.025 SS). | Low | (19) |
| Distance to palatal cortical bone | It is not clear whether the distance of the apex to the palatal cortical bone is associated with EARR severity. The study reported no association between the distance to the palatal cortical bone and EARR severity. | Very low | (21) |
| CQ #3—Treatment strategy | |||
| Treatment strategy/management | There is insufficient evidence on orthodontic management when EARR occurs during orthodontic treatment. | — | — |
| CQ #4—After-treatment care requirements | |||
| Progress of EARR after orthodontic treatment | There are indications that the EARR process will stop after active orthodontic treatment is stopped. | n/a | (23) |
| Long-term effects (mobility, vitality) | There is insufficient evidence on the long-term effects of EARR. | — | — |
| Prognosis of teeth with (severe) EARR | There is insufficient evidence on the prognosis of EARR. | — | — |
| Pain/discomfort and costs after orthodontic treatment for the patient | There is insufficient evidence on pain/discomfort and on the costs to the patient after orthodontic treatment. | — | — |
The last column lists the studies that investigated the clinical question item and contributed to the final conclusion. The wording of the evidence reflects the quality level of the evidence.
In general, the quality of evidence was rated as low or very low. Only the patient-related risk factors, ‘gender’ and ‘age’, showed a moderate quality of evidence. The most common reasons for downgrading were inconsistency, when studies reported contradictory results; indirectness, when studies did not look for predictors of clinically relevant EARR (EARR ≥ 2 mm); imprecision, when the clinical question item was only described in one study or when the statistical analysis or the description of the statistics was unclear; and limitations in study design, when a reporting bias was present.
Commentary and authorization phase and implementation
The Task Force received a total of 51 comments from seven professional associations. The comments were reviewed and processed during a Task Force meeting. The final guideline was presented to the NVvO for formal authorization.
The implementation plan demands that strong recommendations must be implemented within 1 year after publication of the CPG. Moreover, all other recommendations must be implemented within 3 years after authorization. To ensure the guideline is up to date, the CPG will be revised in 2022.
Discussion
This discussion is divided into subsections, according to the clinical questions we addressed with the CPG. Together with the evidence, the discussions lead to the final recommendations.
CQ #1. What types of radiographs enable the diagnosis/detection of orthodontically induced EARR?
For this clinical question, we found that a panoramic radiograph is commonly used as a diagnostic tool for orthodontic purposes because the whole maxillo-mandibular complex is visible, including the temporomandibular joints. A common limitation of the panoramic X-ray is the visibility of the upper and lower front teeth due to the superimposition of the bony structures of the skull or vertebrae (18). When it is not possible to assess the roots adequately, a PA of the blurred region is recommended.
We also investigated the ideal time point for taking a radiograph to assess EARR at an early stage. There was evidence that the degree of EARR present after 6 to 12 months of orthodontic treatment with fixed appliances was related to the degree of EARR at the end of the treatment (8, 24). Therefore, it might be good clinical practice to take a panoramic radiograph at 6–12 months after placement of the fixed appliance. This radiograph may also be used to check the bracket position at the end of the alignment phase. However, due to the low incidence of EARR and based on the As Low As Reasonably Achievable principles, taking a radiograph for screening purposes only is not recommended (25). This position is also endorsed by the Dutch guideline for dental radiology (26). However, taking into consideration the possible risk factors for EARR (see CQ #2), the Task Force reached a consensus on the recommendation to consider taking an OPT in patients with premolar extractions as part of the treatment plan at 12 months after starting treatment with fixed appliances (during the closing phase). This recommendation was supported by the relationship between the amount of EARR after 12 months of active treatment and the amount of EARR at the end of treatment (8).
We did not investigate the potential use of genetic analyses and biological markers for predicting or detecting EARR (27, 28). This research field is presently in development and routine clinical applications remain in the distant future.
CQ #2. What factors increase the risk of developing EARR during orthodontic treatment?
It is important to identify risk factors for EARR prior to orthodontic treatment to minimize the risk that EARR occurs during treatment. For this purpose, we considered patient-related and treatment-related factors that might increase the risk of developing EARR. With this information, it might be possible to develop a patient-centred treatment plan, particularly for patients at high risk.
An investigation of patient-related risk factors, unfortunately, indicated that the evidence level was ‘low’ to ‘very low’ for all potential risk factors, except for ‘age’ and ‘gender’. For these two factors, we found moderate evidence that they were not associated with the amount of EARR. The other potential risk factors listed in Table 3 also showed no evidence of an association. Consequently, no reliable recommendations could be made. Although one study reported that earlier orthodontic treatment may be a preventive factor for EARR, this does not lead to a particularly useful recommendation (21). Apparently, retreatments do not negatively influence the risk of EARR. This finding might be explained by the fact that after active orthodontic treatment has ended, the damaged periodontal tissue will reorganize and resorption lacunae will heal, at least partially (29–31).
An investigation of treatment-related risk factors indicated that the evidence levels varied from ‘low’ to ‘very low’. The only potential risk factors that were rated with a ‘low’ evidence level were: treatment duration, duration of rectangular wire use, extraction therapy, anterior vertical elastics, and wire sequence. There were some indications that treatment duration was not associated with the amount of EARR; however, prolonged treatment times might have negative effects on patient compliance or oral hygiene and, therefore, must be avoided. In one of the included studies, several particular wire sequences were investigated for their effects on the risk of developing EARR (19). However, no significant difference in EARR was found for the three wire sequences in their RCT. Moreover, many different wire sequences and wire types that are used for alignment worldwide were not investigated in that study. Consequently, we could not provide a recommendation for a safe, universally applicable wire sequence.
The data indicated that extraction therapy followed by orthodontic treatment might increase the risk of developing EARR. Therefore, it is important to inform the patient about this increased risk. The risk might be increased by large apical displacements and/or by the reduction of a large overjet when closing the extraction spaces; however, the level of evidence in support of these possibilities was very low (Table 3) (32). Other risk factors that are mentioned in the literature include the use of anterior vertical or Class II elastics and the distance of the apex to the palatal cortical bone. The quality of evidence for these risk factors, however, was low or very low.
Due to the uncertainty about the contribution of specific treatment-related risk factors to EARR development, every patient should be informed prior to orthodontic treatment about the risk of developing EARR, particularly when an extraction is indicated.
CQ# 3. What treatment protocol should be followed when EARR has been detected during treatment?
When EARR occurs during orthodontic treatment, there is a risk that the process of resorption will continue. Therefore, the practitioner must consider whether to continue or stop orthodontic treatment after detecting EARR. This question could not be resolved based on the existing evidence. The Task Force discussed this issue and considered that the practitioner should re-evaluate treatment goals and determine the subsequent treatment strategy together with the patient. Treatment may be continued, modified, or terminated. First, the risks of continuing treatment must be balanced against the risks of ending treatment, taking into consideration the occlusion (occlusal disturbances, deep bite). Some malocclusions, like a deep bite or occlusal trauma, will harm oral health on a long-term basis (23, 33); therefore, it might be better to continue treatment. Second, the patient’s aesthetic perspective should be considered. Based on this perspective, the practitioner should review the treatment and estimate how much more apical displacement is necessary of the affected teeth, and whether accomplishing that amount of displacement is justified. With a localized severe EARR, excluding the affected teeth from the active appliance may be an option. This could allow further correction of the malocclusion without further damage to the affected teeth. When generalized (almost all teeth affected) severe EARR occurs, the Task force recommends an immediate end to the active treatment to prevent further harm.
When the decision is to continue active treatment, with or without a modified treatment plan, the Task Force consensus was to discontinue treatment for at least 3 months. Within this resting period, no orthodontic force should be applied; this rest will allow the resorption lacunae to heal (29–31). The study of Levander et al., which was excluded from the systematic review of Ahangari et al., due to unclear methodology, showed that significantly less EARR (−0.4 mm, SD = 0.7, P < 0.05) occurred after a treatment interruption of 3 months compared to the EARR observed with immediate treatment continuation (−1.5 mm, SD = 0.8) (5, 29). However, even after a rest period, caution is required when continuing orthodontic treatment. At 6 months after restarting treatment, an evaluation of EARR progress with a new radiograph might be indicated.
CQ #4. What is the follow-up protocol for patients with EARR?
Copeland and Green showed that EARR progress stopped after the active orthodontic treatment stopped, that is, after force application was discontinued (23). Therefore, movement of affected teeth due to active retention appliances is unwanted. Consequently, the Task Force recommends that regular retention check-ups should be performed to ensure that the retention devices remain passive. These check-ups may be performed by either the orthodontist or the general practitioner.
Furthermore, the amount of EARR should be considered (2–4). Severe EARR causes an unfavourable root-crown ratio, which may result in higher tooth mobility (34). Therefore, the long-term prognosis of a resorbed tooth is an important issue to consider for after-treatment care recommendations. A tooth with less than 10 mm of remaining root length might display higher than normal mobility, and mobility might increase over time (6, 7, 34). The case series and case reports regarding long-term tooth survival have shown high individual variation, but none of the affected teeth were lost during follow-up (5–25 years). However, when alveolar bone loss occurs, due to periodontal disease, the prognosis and longevity of the affected teeth may be compromised (9). Therefore, the dentist should be informed about clinically significant (≥2 mm) root resorption, should focus on periodical screening of the periodontal status of the patient, and should emphasize optimal oral hygiene to prevent periodontal disease.
Patients might want to know whether they will feel pain following EARR. However, we found no evidence of pain associated with an EARR (5). Nevertheless, in some cases of EARR, clinical signs of pain might be present. This scenario will most likely occur when the nerve is also affected (pulpitis). In general, the Task Force came to the consensus that orthodontically induced EARR was not associated with pain.
Clinical recommendations
These recommendations are based on the literature evidence, the Task Force discussions, and the Task Force considerations. Recommendations for the best treatment protocol for an EARR that occurs during treatment (CQ #3) and recommendations for after-treatment care (CQ #4) were mainly based on consensus because there was very little or no evidence available.
CQ #1. Diagnosis
For recommendations regarding comparisons between CBCT and OPT and between CBCT and PA, we refer to the orthodontic radiology guideline of the NVvO (17).
1.1 Consider taking an OPT at 12 months after starting fixed appliances in a patient with any extraction treatment. Compare this OPT to the OPT taken at the start of orthodontic treatment, when available. Weak recommendation
1.2 Consider taking additional periapical radiographs when the available radiographs do not provide adequate information about the shape and size of the roots. Weak recommendation
CQ #2. Risk factors
2.1 Inform the patient prior to orthodontic treatment about the risk of EARR. Strong recommendation
2.2 When an extraction treatment is planned, inform the patient of the possibility that it is associated with increased risk of severe EARR. Strong recommendation
CQ #3. Treatment strategy
3.1 Re-evaluate the treatment goals and treatment plan when EARR is detected (≥2 mm) during an orthodontic treatment. Inform the patient and discuss the consequences, the patient’s preferences, and the treatment goals. Strong recommendation
3.2 Consider stopping orthodontic treatment when generalized severe EARR occurs. Weak recommendation
3.3 Consider avoiding further loading on teeth that exhibit severe EARR. Weak recommendation
3.4 When deciding to continue active orthodontic treatment, consider discontinuing treatment for 3 months. Make sure that the appliance is passive during that time to avoid loading the affected teeth. Weak recommendation
3.5 When deciding to continue orthodontic treatment, attempt to avoid displacement of the affected teeth. Strong recommendation
3.6 When deciding to continue active orthodontic treatment after a treatment interruption of 3 months, consider taking a new radiograph at 6 months after the restart. Weak recommendation
CQ #4. After-treatment care requirements
4.1 Follow the patient according to your normal retention protocol. Strong recommendation
-
4.2 Patient information about the long-term prognosis must include at least the following:
EARR will stop after the appliances are removed.
EARR will not lead to pain or discomfort (sensibility).
The affected tooth may be mobile, and mobility might increase over time (for root lengths less than 10 mm).
Affected teeth might be lost earlier, if periodontal bone destruction (periodontitis) occurs. Strong recommendation
-
4.3 Take care of a good communication with the dentist at the end of treatment to inform the dentist about affected teeth and advice:
periodical screening for periodontal diseases, especially around the affected teeth.
assurance that retention devices remain passive after the regular retention check-ups with the orthodontist have ended. Strong recommendation
Limitations of the CPG and suggestions for further research
Orthodontic specialists are the main professionals that deal with orthodontically induced EARR. The orthodontist must take care to prevent EARR during treatment and take measures when an EARR has occurred. Undoubtedly, the main issues for patients and their dentists are after-treatment care and the consequences of EARR. Therefore, the drafted guideline was sent out to receive comments from professional dental organizations and the Patients’ Federation. Throughout the entire CPG development period, we found that evidence was lacking regarding patient-reported outcome measures (PROMs). This might partly be explained by the fact that most studies were retrospective with unclear inclusion criteria and most were performed during an era when PROMs were not included as an outcome measure in orthodontic studies.
Another limitation was that most studies on EARR were observational. Although the RCT is the gold standard for therapeutic clinical questions, for prognostic factors, observational studies are a better choice. Nevertheless, according to the guideline methodology, a recommendation is not based on evidence alone but also on expert opinion and patient preferences. Expert opinions regarding EARR or EARR-related problems might differ among different countries, for instance, due to differences in legal regulations or in the organization and financing of the health care system. An example of a difference in expert opinions is the weighting of the PAR index; this weighting differs between orthodontists in the USA and those in the UK (35, 36). Nevertheless, to our knowledge, the present study is the first published report to apply the recently published RIGHT statement to the development of a CPG in orthodontics (12). The approach we used to apply this reporting statement to the present paper could serve as a template for the reporting of other CPGs in orthodontics.
The literature search was confined to Medline and Embase and the search was restricted to English and Dutch languages. In the planned revision of the CPG (2022), the search methodology will be expanded to include additional electronic databases and a search of the grey literature, while language restrictions will not be imposed. This may reduce possible selection bias.
The time span from literature search until the publication of the CPG was long. However, the development of a CPG according to the Agree II and EBRO system is complex and therefore does not allow a faster development. A systematic review is only the start of the guideline development process. When only performing a systematic review, conclusions can be drawn and reported. However, when developing a guideline, after the collection of the evidence, several meetings of the Task Force were needed for evaluation of the evidence and formulating considerations and recommendations. Then a draft guideline is written and the commentary phase starts. As shown above, many stakeholders were involved in this phase and it took 9 months before all comments were received and processed. Furthermore, a guideline includes more than one clinical question. So in a strict sense, this is comparable to a separate systematic review for each clinical question. Finally, the last step is authorization of the guideline, which could be done only 9 months later at the General Assembly meeting of the professional association. Consequently, the whole process of guideline development is taking much longer than a systematic review would take. We have updated the literature search (PROSPERO registration number: CRD42019114169) from September 2015 to 12 October 2018 to see if there was any new evidence, but this information cannot be included in the CPG as presented here as it would require to redo the whole process of guideline development and then the search would be outdated again when finally having the updated guideline authorized. For that reason, each CPG must include a statement when it will be updated. The present guideline will be updated in 2022. The outcome of the search update is presented in Supplementary Tables 3–5.
This study showed a striking lack of evidence regarding our four clinical questions. Consequently, we could only provide weak recommendations regarding the prevention of EARR and the handling of EARR once it has occurred. Future research should focus on the diagnostic procedures, risk factors, the management of EARR when it occurs during treatment, and the prognosis of affected teeth. Furthermore, more insight into the contributions of specific genes and the presence of biological markers in the crevicular fluid may lead to effective diagnostic tools for identifying patients at risk.
Conclusion
We could only provide weak recommendations regarding the prevention of EARR and the handling of EARR once it has occurred because of low quality of the available evidence. Nevertheless, this clinical practice guideline allows clinicians to respond to EARR based on current knowledge. The recommendations may reduce variations between practices and assist in providing patients with appropriate information. Future research should focus on the diagnostic procedures, risk factors, the management of EARR when it occurs during treatment, and the prognosis of affected teeth.
Funding
This work was supported by the Dutch Association of Orthodontists (NVvO). The NVvO established the Task Force, engaged the Knowledge Institute of the Association of Medical Specialists for methodological and technical support, and is responsible for the development, dissemination, and implementation of the CPG.
Supplementary Material
Acknowledgements
We would like to thank Ing. L. H. M. Niesink-Boerboom, MSc, the literature specialist of the Knowledge Institute of the Dutch Association of Medical Specialists for the systematic literature search.
Conflict of interest
According to the Code of Conduct of ‘The Royal Dutch Medical Association’ (KNMG), all members of the Task Force were required to disclose potential conflicts of interest that might have arisen over the past 3 years regarding financial (relationship to commercial companies, personal financial interests, research funding) and indirect interests (personal relations, reputation management, knowledge valorization) (37). All participants of the Task Force declared no conflict that could influence participation in this study. These declarations can be obtained from the secretary of the Knowledge Institute of the Association of Medical Specialists.
References
- 1. Segal G.R., Schiffman P.H. and Tuncay O.C (2004) Meta analysis of the treatment-related factors of external apical root resorption. Orthodontics & Craniofacial Research, 7, 71–78. [DOI] [PubMed] [Google Scholar]
- 2. Weltman B., Vig K.W., Fields H.W., Shanker S. and Kaizar E.E (2010) Root resorption associated with orthodontic tooth movement: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics, 137, 462–476; discussion 12A. [DOI] [PubMed] [Google Scholar]
- 3. Walker S.L., Tieu L.D. and Flores-Mir C (2013) Radiographic comparison of the extent of orthodontically induced external apical root resorption in vital and root-filled teeth: a systematic review. European Journal of Orthodontics, 35, 796–802. [DOI] [PubMed] [Google Scholar]
- 4. Tieu L.D., Saltaji H., Normando D. and Flores-Mir C (2014) Radiologically determined orthodontically induced external apical root resorption in incisors after non-surgical orthodontic treatment of class II division 1 malocclusion: a systematic review. Progress in Orthodontics, 15, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahangari Z., Nasser M., Mahdian M., Fedorowicz Z. and Marchesan M.A (2015) Interventions for the management of external root resorption. Cochrane Database of Systematic Reviews, 24, CD008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Remington D.N., Joondeph D.R., Artun J., Riedel R.A. and Chapko M.K (1989) Long-term evaluation of root resorption occurring during orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 96, 43–46. [DOI] [PubMed] [Google Scholar]
- 7. Levander E. and Malmgren O (2000) Long-term follow-up of maxillary incisors with severe apical root resorption. European Journal of Orthodontics, 22, 85–92. [DOI] [PubMed] [Google Scholar]
- 8. Artun J., Van‘t Hullenaar R., Doppel D. and Kuijpers-Jagtman A.M (2009) Identification of orthodontic patients at risk of severe apical root resorption. American Journal of Orthodontics and Dentofacial Orthopedics, 135, 448–455. [DOI] [PubMed] [Google Scholar]
- 9. Roscoe M.G., Meira J.B. and Cattaneo P.M (2015) Association of orthodontic force system and root resorption: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics, 147, 610–626. [DOI] [PubMed] [Google Scholar]
- 10. Tejani T., Mubeen S., Seehra J. and Cobourne M.T (2017) An exploratory quality assessment of orthodontic clinical guidelines using the AGREE II instrument. European Journal of Orthodontics, 39, 654–659. [DOI] [PubMed] [Google Scholar]
- 11. Kwaliteitsinstituut voor de Gezondheidszorg CBO (Centraal Begeleidingsorgaan) (2007) Evidence-based Richtlijnontwikkeling, Handleiding voor werkgroepleden Kennisbank richtlijnontwikkeling; http://www.ha-ring.nl/download/literatuur/EBRO_handl_totaal.pdf (5 September 2018, date last accessed). [Google Scholar]
- 12. Chen Y., et al. ; RIGHT (Reporting Items for Practice Guidelines in Healthcare) Working Group (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Annals of Internal Medicine, 166, 128–132. [DOI] [PubMed] [Google Scholar]
- 13. Brouwers M.C., et al. ; AGREE Next Steps Consortium (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. Canadian Medical Association Journal, 182, E839–E842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins J.P.T., Altman D.G. and Sterne J.A.C (2017) Chapter 8: assessing risk of bias in included studies. In Higgins J.P.T., Churchill R., Chandler J., Cumpston M.S. (eds.), Cochrane Handbook for Systematic Reviews of Interventions, Version 5.2.0 (updated June 2017). http://www.training.cochrane.org/handbook (5 September 2018, date last accessed). [Google Scholar]
- 15. Sterne J.A.C., Higgins J.P.T. and Reeves B.C.; on behalf of the development group for ACROBAT-NRSI (2014) A cochrane risk of bias assessment tool: for non-randomized studies of interventions (ACROBATNRSI). Cochrane Colloquium, Version 1.0.0. http://www.riskofbias.info (7 May 2019, date last accessed). [Google Scholar]
- 16. Schünemann H., Brożek J., Guyatt G. and Oxman A. (eds.) (2013) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Grade Working Group; https://gradepro.org/ [Google Scholar]
- 17. Nederlandse Vereniging van Orthodontisten (2018) Richtlijn Orthodontische Radiologie www.orthodontist.nl (5 September 2018, date last accessed).
- 18. Sameshima G.T. and Asgarifar K.O (2001) Assessment of root resorption and root shape: periapical vs panoramic films. The Angle Orthodontist, 71, 185–189. [DOI] [PubMed] [Google Scholar]
- 19. Mandall N., Lowe C., Worthington H., Sandler J., Derwent S., Abdi-Oskouei M. and Ward S (2006) Which orthodontic archwire sequence? A randomized clinical trial. European Journal of Orthodontics, 28, 561–566. [DOI] [PubMed] [Google Scholar]
- 20. Linge L. and Linge B.O (1991) Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 99, 35–43. [DOI] [PubMed] [Google Scholar]
- 21. Mirabella A.D. and Artun J (1995) Risk factors for apical root resorption of maxillary anterior teeth in adult orthodontic patients. American Journal of Orthodontics and Dentofacial Orthopedics, 108, 48–55. [DOI] [PubMed] [Google Scholar]
- 22. Lund H., Gröndahl K., Hansen K. and Gröndahl H.G (2012) Apical root resorption during orthodontic treatment. A prospective study using cone beam CT. The Angle Orthodontist, 82, 480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Copeland S. and Green L.J (1986) Root resorption in maxillary central incisors following active orthodontic treatment. American Journal of Orthodontics, 89, 51–55. [DOI] [PubMed] [Google Scholar]
- 24. Levander E. and Malmgren O (1988) Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. European Journal of Orthodontics, 10, 30–38. [DOI] [PubMed] [Google Scholar]
- 25. International Commission on Radiological Protection (1977) Recommendations of the ICRP. ICRP publication 26. Annals of the ICRP, 1, 3. [DOI] [PubMed] [Google Scholar]
- 26. Koninklijke Nederlandse Maatschappij tot bevordering der Tandheelkunde (KNMT) (2015) Richtlijn Tandheelkundige Radiologie www.knmt.nl (5 September 2018, date last accessed).
- 27. Wu F.L., Wang L.Y., Huang Y.Q., Guo W.B., Liu C.D. and Li S.G (2013) Interleukin-1β +3954 polymorphisms and risk of external apical root resorption in orthodontic treatment: a meta-analysis. Genetics and Molecular Research, 12, 4678–4686. [DOI] [PubMed] [Google Scholar]
- 28. Kaczor-Urbanowicz K.E., Deutsch O., Zaks B., Krief G., Chaushu S. and Palmon A (2017) Identification of salivary protein biomarkers for orthodontically induced inflammatory root resorption. Proteomics Clinical Applications, 11, 14. [DOI] [PubMed] [Google Scholar]
- 29. Levander E., Malmgren O. and Eliasson S (1994) Evaluation of root resorption in relation to two orthodontic treatment regimes. A clinical experimental study. European Journal of Orthodontics, 16, 223–228. [DOI] [PubMed] [Google Scholar]
- 30. Owman-Moll P., Kurol J. and Lundgren D (1995) Repair of orthodontically induced root resorption in adolescents. The Angle Orthodontist, 65, 403–408; discussion 409. [DOI] [PubMed] [Google Scholar]
- 31. Mehta S.A., Deshmukh S.V., Sable R.B. and Patil A.S (2017) Comparison of 4 and 6 weeks of rest period for repair of root resorption. Progress in Orthodontics, 18, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stalpers M.J., Booij J.W., Bronkhorst E.M., Kuijpers-Jagtman A.M. and Katsaros C (2007) Extraction of maxillary first permanent molars in patients with class II division 1 malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 316–323. [DOI] [PubMed] [Google Scholar]
- 33. Danz J.C., Greuter C., Sifakakis I., Fayed M., Pandis N. and Katsaros C (2014) Stability and relapse after orthodontic treatment of deep bite cases-a long-term follow-up study. European Journal of Orthodontics, 36, 522–530. [DOI] [PubMed] [Google Scholar]
- 34. Jönsson A., Malmgren O. and Levander E (2007) Long-term follow-up of tooth mobility in maxillary incisors with orthodontically induced apical root resorption. European Journal of Orthodontics, 29, 482–487. [DOI] [PubMed] [Google Scholar]
- 35. Richmond S., Shaw W.C., O’Brien K.D., Buchanan I.B., Jones R., Stephens C.D., Roberts C.T. and Andrews M (1992) The development of the PAR Index (Peer Assessment Rating): reliability and validity. European Journal of Orthodontics, 14, 125–139. [DOI] [PubMed] [Google Scholar]
- 36. DeGuzman L., Bahiraei D., Vig K.W., Vig P.S., Weyant R.J. and O’Brien K (1995) The validation of the Peer Assessment Rating index for malocclusion severity and treatment difficulty. American Journal of Orthodontics and Dentofacial Orthopedics, 107, 172–176. [DOI] [PubMed] [Google Scholar]
- 37. KNAW, KNMG, GR, NHG, FMS (2016) Code ter Voorkoming van Oneigenlijke Beïnvloeding Door Belangenverstrengeling https://www.knaw.nl/shared/resources/actueel/publicaties/pdf/gedragscode-belangenverstrengeling (5 September 2018, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.