Abstract
Appropriate hygiene practices and vaccine acceptance are key factors impacting the health of homeless individuals. A recent outbreak of hepatitis A in Michigan, especially impacting Detroit, prompted us to investigate the practices and attitudes of Detroit's homeless population toward hygiene measures and vaccinations, as well as barriers to such resources. We developed a questionnaire as a means to collect our data, and participants were interviewed at shelters and soup kitchens. While the majority of participants adhered to healthy hygiene practices, approximately 89% reported barriers to accessing public showers. More than half the participants (64%) reported receiving their hepatitis A vaccine prior to the study, while 23% reported previously refusing or hesitating to receive vaccinations. Despite an overall favorable adherence to hygiene practices, substantial barriers are yet to be overcome. Moreover, active measures should be taken to establish higher levels of trust between providers and the homeless to encourage vaccine acceptance.
Keywords: Vaccines, Public health, Infectious disease, Virology, Vaccination, Health disparity, Health promotion
Vaccines; Public Health; Infectious Disease; Virology; Vaccination; Health Disparity; Health Promotion.
1. Introduction
Hepatitis A is an inflammatory disease of the liver caused by hepatitis A Virus (HAV), a picornavirus commonly spread through the fecal-oral route. Annual reported cases of HAV infections have dropped precipitously since the advent of the HAV vaccine, which provides long-lasting immunity to infection. Between 2009 and 2016, the number of new hepatitis A cases in the United States each year hovered at or below 2,000 [1,2] with most significant outbreaks being associated with contaminated food. While it had previously been recommended for high-risk children since licensure in 1995, HAV only became a recommended routine vaccination for all children over the age of one year in 2006 [3]. It is also recommended for adults with an increased risk of infection, such as international travelers, men who have sex with men, and persons who use and inject drugs [2].
The past three years have seen an unprecedented spike in reported cases of HAV, with outbreaks primarily localized to six states: California, Michigan, Ohio, Kentucky, West Virginia, and Utah. Instead of contaminated food, these outbreaks have been attributed to direct person-to-person transmission, and have led to a reported combined total of over 3,000 cases in 2017 and 10,582 in 2018 alone [4]. Given the fecal-oral transmission route, risk factors for such transmission include unsanitary living conditions, use of contaminated needles for intravenous drug use, and specific types of sexual activity [5].
Homeless individuals are at a high risk for contracting a wide variety of communicable diseases due to poor access to sanitation and high rates of intravenous drug use. As a result, they are particularly susceptible to outbreaks of HAV [6]. Additionally, the spread of infectious diseases within a population of homeless individuals is exacerbated and accelerated by the close-quarter living arrangements of shelters and homeless camps. In the current outbreak, 57% of patients reported drug use, homelessness, or both [7]. As such, in October of 2018 the CDC's Advisory Committee on Immunization Practices (ACIP) added individuals experiencing homelessness to the list of at-risk patients who should routinely receive the HAV vaccine [8] as HAV vaccination campaigns have been shown to stop the spread of HAV in homeless populations [9].
Detroit quickly emerged as a hotspot of the Michigan HAV outbreak, with almost 200 cases identified within the city and a hospitalization rate of over 80% between August 2016 and December 2018 [10]. Homelessness is a particular problem in the city, with roughly 13,175 individuals experiencing homelessness over the course of 2017, 13% of which were chronically homeless [11].The majority of these were African-American (91%) and male (60%), and one-third were over the age of 55, putting them at even greater risk for poor health outcomes [11]. While a majority of homeless individuals within the city on a given night are sheltered, up to 9% are unsheltered, residing on the streets or in other areas generally regarded as unsuitable for habitation [11].
Though vaccination initiatives have been launched in various medical settings around the country to prevent the spread of HAV, including in Detroit, factors impacting the attitudes of homeless individuals toward vaccinations are not well understood. Further, little is known about factors impacting the usability of sanitation infrastructure in Detroit, and the particular beliefs and practices of homeless individuals regarding personal hygiene and public facilities.
We conducted a cross-sectional study aimed at developing a better understanding of the practices, attitudes, and beliefs regarding personal hygiene, such as hand and full-body washes, and vaccination for infectious disease within the homeless population in Detroit. Given the extent of the recent HAV outbreaks across the country and the paucity of existing knowledge in this area, we hoped to gain insight into how the homeless encounter and address risk factors for the transmission of infectious disease. This knowledge will help inform future efforts to improve hygiene practices and vaccination adherence, ultimately strengthening the capacity of healthcare systems to prevent future outbreaks through the provision of sensitive and effective services to homeless individuals.
2. Methods
2.1. Population studied
The organization Street Medicine Detroit (SMD) aims to provide quality medical care to homeless individuals through “street runs,” or outreach visits with medical providers to shelters and street-based locations across the city. Clients were identified during street runs at various soup kitchens and shelters and interviewed privately. To be included, clients needed to be living in Detroit, Michigan, over the age of 18, and currently lacking permanent housing at the time of interview. Minors and those not wishing to participate were excluded. Interviews were approximately 30 min in length and occurred over a period of four months during the late summer and early fall of 2018.
2.2. Survey instrument
All surveys were carried out under a protocol approved by the Institutional Review Board (IRB) at Wayne State University School of Medicine, and voluntary informed consent was obtained from each participant before participation. The interview questionnaire (Supplement 1) consisted of demographic information, quantification of hygiene habits, assessment of attitudes and beliefs about vaccines, and short-form responses to capture unique client experiences. Questions included in the survey instrument were drawn from previously validated surveys to allow for ease of comparison to past and future studies, as well as from discussions with local CDC and public health department officials regarding high-priority questions that would be helpful to their efforts. In particular, efforts were made to match questions concerning hygiene practices with corresponding studies performed in Boston, MA [12]. Efforts were made to match questions concerning vaccine hesitancy with those suggested by the World Health Organization and the SAGE Working Group on Vaccine Hesitancy [13]. Vaccine attitudes were assessed using the quantitative Vaccine Conspiracy Beliefs Scale [14].
2.3. Statistical analysis
Information on statistical tests used to determine significance can be found in corresponding figure legends or manuscript text when applicable. All statistical analyses were performed in Graphpad Prism software version 5 (GraphPad Software, Inc., La Jolla, CA).
3. Results
Based on self-reported demographics from the 44 individuals interviewed, the average age of study participants was 50 years old. In addition, 90% were African-American and 59% were female. 84% of participants had not had secure housing in the past six months, and 59% of participants reported a shelter as their most frequent overnight location over the past 30 days.
As regards full-body washes, only 34.1% of the survey population reported daily showers and 29.5% reported showering 3–6 times per week. 29.5% of clients reported showering 1–2 times per week, and 6.8% reported that they showered less than once per week (Table 1). Regular hand washing was slightly more common among the respondents, with 47.7% reporting hand-washing greater than five times per day and another 34.1% at least 2–4 times per day (Table 1). Additionally, 84% of respondents reported use of hand sanitizer rubs in the week prior to interview. Clients rated the overall difficulty of accessing public showering facilities in Detroit at a mean of seven out of ten, with ten being most difficult.
Table 1.
Demographics and hygiene practices.
| Characteristic | Prevalence % (n) |
|---|---|
| Black | 90% (39) |
| Female |
59% (26) |
|
Housed in the past 30 days | |
| Homeless shelter | 59% (26) |
| Street/outdoors | 18% (8) |
| Doubled up | 9% (4) |
| Transitional/Treatment program |
7% (3) |
|
Frequency of showers (in last week) | |
| Daily | 34% (15) |
| 3-6 times | 30% (13) |
| Twice | 16% (7) |
| Once | 14% (6) |
| None |
7% (3) |
|
Most common location of shower (n=42) | |
| Shelter | 81% (34) |
| Friends/family |
14% (6) |
|
Frequency of hand washing (in a typical day) | |
| ≥5 times | 48% (21) |
| 2-4 times | 34% (15) |
| Once | 18% (8) |
| Hand sanitizer in the last week (yes) | 84% (37) |
| Clothes/bedding sharing (yes) |
18% (8) |
|
Frequency of clothes washing (in past month) | |
| 6 + times | 11% (5) |
| 3-5 times | 45% (20) |
| 1-2 times | 32% (14) |
| 0 times |
9% (4) |
|
Laundry method (n=42) | |
| Shelter washing machine | 57% (24) |
| Laundromat | 12% (5) |
| Laundry facilities at drop-in center | 10% 4) |
| Washing machine at home of family or friend | 7% (3) |
| Public sink | 5% (2) |
| Shelter's sinks | 2% (1) |
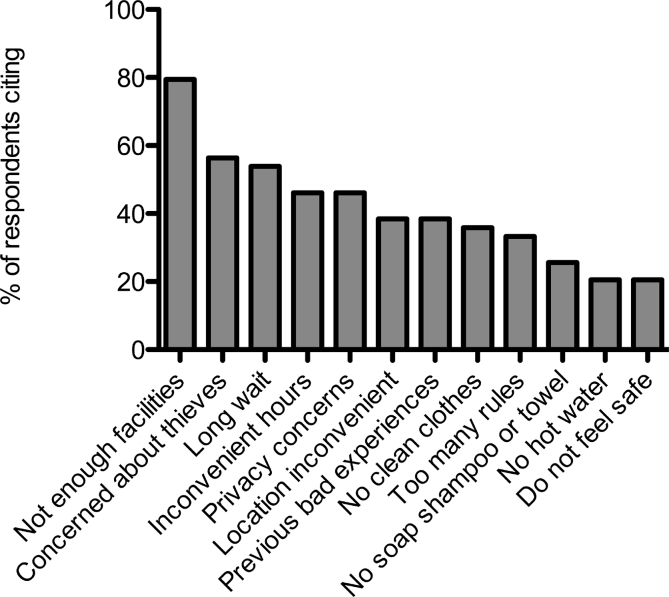
To better understand this difficulty, we asked patients who reported problems accessing public showers (89% of those surveyed, n = 39) about a series of potential barriers they may have faced. The top three reported barriers included too few public showering facilities (79%), concern about items being stolen (56%), and long wait times to access the showers (54%) (Table 2; Figure 1). In an optional section for additional comments and discussion on this topic, as well as in a free-form response period at the conclusion of the interview, the most commonly cited barrier was the cleanliness of showering facilities, with some clients stating that they had chosen in the past to forego showers because of sanitary concerns. When asked about specific improvements they would like to see, clients stated that having a greater number of clean facilities with longer hours would be helpful (Figure 2).
Table 2.
Perceived barriers to hygiene.
| Barrier | Prevalence % (n) |
|---|---|
|
Barriers to showers (n=39) | |
| Not enough facilities | 79% (31) |
| Concerned about thieves | 56% (22) |
| Long wait | 54% (21) |
| Inconvenient hours | 46% (18) |
| Privacy concerns | 46% (18) |
| Location inconvenient | 38% (15) |
| Previous bad experiences | 38% (15) |
| No clean clothes | 36% (14) |
| Too many rules | 33% (13) |
| No soap, shampoo, or towel | 26% (10) |
| No hot water | 21% (8) |
| Do not feel safe |
21% (8) |
|
Barriers to clothes washing (n=19) | |
| Cannot afford laundromats | 89% (17) |
| Inconvenient location | 63% (12) |
| Too many rules | 58% (11) |
| No clean clothes to change into | 53% (10) |
| No washing soap | 47% (9) |
| Previous bad experiences | 37% (7) |
| Privacy concerns | 26% (5) |
| Do not feel safe | 21% (4) |
| No hot water | 16% (3) |
Figure 1.
Self-reported barriers to accessing public showering facilities. Clients expressing difficulty accessing showers (N = 39) were queried as to a list of specific barriers preventing their access to public showering facilities. Values represent proportion of clients citing each barrier. Most commonly cited barrier not in survey instrument was cleanliness.
Figure 2.
In Their Own Words: Suggestions for Improving Public Showering Facilities. Study participants were asked to identify the best way to improve public showering services for individuals experiencing homelessness in Detroit. Responses are depicted above as a word cloud with size representing the frequency of the word in open-ended responses.
We also queried clients about their laundry practices as well as any barriers present that made it difficult for them to wash their clothes. 56% reported washing their clothes at least 3 times in the past month, and roughly one-tenth (9.3%) said they had not washed their clothes at all in that time (Table 1). Over half of those surveyed (57%) reported using shelter laundry facilities to wash their clothes.
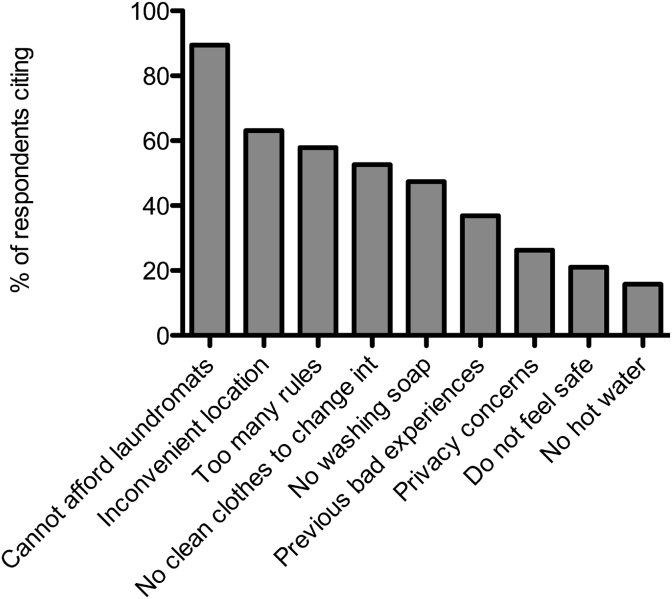
Slightly Less than half of the clients (43%) found it difficult to find a place to do laundry, with the most-cited barrier being an inability to afford laundromats (Table 2; Figure 3). In an optional section for additional comments and discussion on this topic, the most commonly cited barrier was the long wait for facilities at shelters. No clients commented on this topic in the free-form response period at the conclusion of the survey.
Figure 3.
Self-reported barriers to washing clothes. Clients expressing difficulty washing clothes regularly (N = 19) were queried as to a list of barriers limiting their access to clothes washing facilities. Values represent proportion of clients citing each barrier. Most commonly cited barrier not in survey instrument was long wait for facilities.
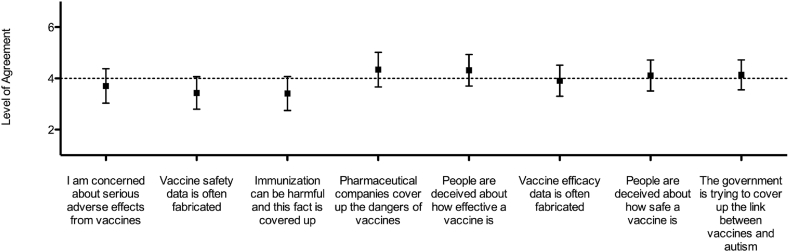
Lastly, clients were asked about their practices, attitudes, and beliefs concerning vaccination (Table 3). Seventy-seven percent of respondents felt that vaccines could protect from serious diseases, yet 41% felt that it was difficult for some in Detroit to get vaccines. In the past year, five clients (11%) had come in contact with someone they knew or suspected to have been infected with HAV. Of these, only one claimed to have been contacted by a public health official and advised to receive the HAV vaccine, which they did. Three of the other four with this exposure were vaccinated for HAV without having been advised by a public health official, though one still had not received the vaccine at the time of the interview, as it had not been offered and they had not sought it out. We were able to vaccinate this individual at the conclusion of the interview. 20% of clients reported close contact with individuals who were known not to have been vaccinated for HAV. A majority of the clients (64%) had been vaccinated for HAV prior to the current visit, while 23% had hesitated in the past to get a vaccine and 7% had refused a vaccine outright. Those who hesitated to receive a vaccine cited beliefs in the danger of materials in the vaccines, such as metals or viruses, or the uselessness of vaccines. The only reason given by clients that had outright refused a vaccine was mistrust of the intentions of the provider or manufacturer. No other clients volunteered this particular concern as a main motivator for delay. On the quantitative Vaccine Conspiracy Beliefs Scale, our survey population did not significantly differ from the neutral response on any question (Figure 4). It is important to note that scores on this instrument did not correlate with vaccination status.
Table 3.
Vaccine beliefs and hesitancy.
| Characteristics | Prevalence % (n) |
|---|---|
|
Vaccine characteristics | |
| Vaccinated for HAV | 64% (28) |
| Contact with someone known or suspected to have HAV in past year | 11% (5) |
| Close contacts known to not have been vaccinated for HAV | 20% (9) |
| Contact with untreated human waste (past year) | 11% (5) |
| Contact with drinking water or food you would consider unclean (past year) |
23% (10) |
|
Vaccine hesitancy | |
| Believe vaccines can protect from serious disease | 77% (34) |
| Think most people have been vaccinated with all recommended vaccines | 30% (13) |
| Been reluctant or hesitated to get a vaccination | 23% (10) |
| Refused a vaccination | 7% (3) |
| Believe it is difficult for some in Detroit to get vaccines | 41% (18) |
Figure 4.
Attitudes and beliefs concerning vaccination. Clients were read the statements on the horizontal axis and asked to rank their level of agreement on a scale from 1 “(strongly disagree”) to 7 (“strongly agree”). The neutral response (4) is indicated with a dashed line. Values shown are the mean of all client responses. Error bars represent the 95% confidence interval of the mean (N = 44).
4. Discussion
4.1. Hygiene practices
The top reported barriers to showering and laundry facilities included facility cleanliness, the number of facilities offering these resources, concerns about theft and the long wait time to shower and/or wash clothes. Clients surveyed were able to, and often did, wash their hands throughout the day, and hand sanitizer rubs were widely accepted as an alternative means of hand hygiene. Though regular showering was also common, the mean difficulty rating of 7 of 10 in accessing showering facilities suggests that significant time and effort was needed to maintain these habits. Such barriers led many clients to shower far less frequently than they would otherwise have preferred. Barriers to the use of laundry services also limited the frequency of clothes washing. Though shelter facilities are often free of charge, clients were faced with long waits for a limited number of machines, and cited being unable to afford laundromats as an alternative means of washing. This issue becomes particularly important when one considers that it is rare for homeless individuals to have more than a few full changes of clothes at any given time.
Moving forward, while an increase in the number and hours of facilities for both showering and clothes-washing would lead to greater overall access, an improvement in the safety and cleanliness of existing facilities could prove a quicker and easier way to address important concerns raised by homeless clients and improve their ability to carry out personal hygiene practices. This conclusion is also supported by comments made by clients when they were given a chance to share any additional thoughts at the conclusion of the survey, as seen by the word-cloud taken from those statements (Figure 2). While “more” was the most common word used, it was followed by “facilities,” “clean/cleaner,” “existing,” “access,” “frequency,” and “floor” (with reference to cleanliness). Several clients also shared anecdotes about refusing to shower when given the opportunity because of concerns regarding sanitation. Therefore, while the number of hygiene facilities is clearly a key barrier, homeless individuals in Detroit are equally, if not more, concerned about the acceptability of existing facilities for their needs. Other studies have shown the importance of regular hygiene practices to physical and mental health, and highlighted in particular the psychological impact homeless individuals may experience when lacking appropriate spaces for maintaining hygiene [15]. As an added benefit, making access and use of sanitation facilities less cumbersome and potentially degrading will afford homeless individuals greater time to focus their attention on other urgent needs, such as seeking healthcare, mental health support, and long-term housing.
The individuals surveyed in this study reported lower rates of daily showering as well as fewer instances of daily hand washing when compared to a similar study conducted by Leibler et al. in Boston, MA [12]. The population sampling of our study differed from that of the Boston study, as our study surveyed a greater percentage of outdoor sleepers (18% vs 7%), a risk factor identified by Leibler et al. for fewer hygiene-related self-care practices [12]. However, the outdoor sleepers surveyed in this study (n = 9) did not differ in their average frequency of hand washing (p = 0.90, unpaired t-test) or showering (p = 0.94, unpaired t-test) compared to those who resided in shelters. Therefore, we are unable to attribute the lower rates of hygiene practice to the greater proportion of outdoor sleepers surveyed. However, the outdoor sleepers in this study were interviewed in shelters or soup kitchens, and reflect the habits of individuals who regularly access these institutions and are perhaps more able and likely to be engaged in self-care; therefore, this may not hold true for individuals who choose to avoid these organizations [12]. Our study sample and that of the Boston group also differed with regard to healthcare-seeking behavior, in that the Boston study drew only from those already seeking healthcare from the Boston Healthcare for the Homeless program, whereas our study draws at random from the homeless population at various shelters and soup kitchens in Detroit. This difference could explain the disparity in hygiene practices between the studies, as those actively seeking healthcare may be more likely to also be actively engaged in frequent and regular personal hygiene practices.
One of our study's limitations includes the lack of data on our participants' mental health status and the prevalence of drug abuse. Leibler et al. found that predictors of reduced hygiene included substance use, which was not queried in our study and may have been significantly present in our survey population, along with mental health issues. Homeless individuals experience a greater burden of substance use and mental illness compared to the general population, and these issues can further interfere with the ability to carry out basic hygiene practices [12]. Limited hygiene, in turn, is also a risk factor for poor mental well-being [16]. Improving the ability of homeless individuals experiencing mental illness to carry out personal hygiene could therefore positively contribute to self-care behaviors and treatment engagement for substance use, an area in need of further study.
4.2. Vaccinations
41% of clients felt it was difficult to find and receive vaccines in Detroit, and only 30% felt that most people had actually received all of the recommended vaccines. This finding indicates that there is ample room for improvement in vaccine provision. However, given the variety of locations already available for vaccination, including our own services that were available to clients at the time of interview, an important measure to address this concern might be better communication to the homeless population about where, when, and which vaccines are offered to the public. In conversation, many clients seemed to be unclear on each of these points, which might lead to the perception of limited availability. Effective communication strategies might involve coordinated efforts with local organizations to deliver information on locations and schedules for free vaccination services, as well as noting available transportation services.
While the majority of clients did not report having previously hesitated and/or declined to receive a vaccine, a proportion of those surveyed reported hesitating to receive immunizations (23%), while a minority (7%, or 30% of hesitators) reported outright refusal to be vaccinated. The fact that hesitators were in the minority, and that refusers were in the minority among the hesitators, indicates that any doubts were more often than not able to be assuaged either by attention from medical personnel or accurate literature regarding the safety and efficacy of vaccination. Previous studies have shown the effectiveness of targeted educational initiatives in improving vaccination rates amongst homeless individuals who have had similar concerns as our hesitant clients regarding the dangers and true efficacy of vaccinations, emphasizing the importance of providing dialogue-based education to address knowledge gaps in this population [17]. Some recent education initiatives regarding vaccination that focused on Detroit's homeless population include a wellness seminar addressing HAV vaccines that was held by SMD in one of the local homeless shelters, in addition to the distribution of educational fliers to clients during service encounters.
While those who hesitated but ultimately received vaccination cited concerns such as chemical/biological safety and efficacy that could be addressed with education initiatives and explanations from medical personnel at the time of hesitation, those who had previously refused to be vaccinated cited mistrust of the intentions of provider or manufacturer as their key reason for doing so. This absence of trust is a far more deep-rooted issue, which cannot be addressed in a similar manner, and indicates that certain strategies that convinced other vaccine hesitators would be ineffective for these clients. Long-term relationships built on trust through repeated one-on-one interactions over time with individual homeless patients can help eliminate the negative perceptions toward healthcare providers and ultimately improve vaccine acceptance, as was relayed to us by at least one patient who had previously refused vaccinations.
Interestingly, the scores regarding attitudes and conspiracy beliefs about vaccines did not correlate with the vaccination status of the surveyed population, though this conclusion is admittedly limited by the small sample size of the vaccine refuser group (n = 3). Factors such as social support, mental health status, coping skills, and provider recommendations have been related to likelihood of vaccine uptake in this population, and may also have contributed to vaccination status [18, 19].
Further, we sought to evaluate efforts targeted at reaching out to those who'd been in contact with HAV + individuals, as contact-tracing is an important measure in reducing the transmission of the disease and containing outbreaks. Five survey respondents claimed to have come into contact with someone they know or suspect to have been actively ill with HAV in the past year, and only one of those five was then contacted by a public health authority for follow-up and vaccination. It is without question that contact-tracing is of paramount importance in addressing outbreaks of infectious disease, but this task may have been made more difficult by the often crowded yet at times remarkably migratory/transient lifestyle lived by many homeless individuals, particularly if the individual with an active infection did not present themselves to public health authorities in a timely manner. Additionally, it is possible that participants were mistaken in their characterization of a contact's illness. Nonetheless, further study may be needed on how best to employ contact-tracing among the homeless specifically, in light of their importance to this and potential future outbreaks.
Finally, we employed the Vaccine Conspiracy Beliefs Scale to characterize adherence to commonly held conspiratorial beliefs about the safety and efficacy of vaccinations. Our study population did not differ overall from the neutral response to any of the 8 statements included in the scale (Figure 4). Several past studies have claimed that low socioeconomic status, a demographic factor common among our study participants, correlates with opposition to vaccination [20, 21], and some using the same Vaccine Conspiracy Beliefs Scale have seen small but significant differences in adherence to conspiracies based on socio-demographic factors [22]. Conversely, others have recently claimed that low socioeconomic status does not correlate with adherence to conspiratorial beliefs as assessed by this scale [23]. However, socio-demographic factors are inarguably an independent predictor of vaccine uptake more broadly [14]. At first blush, our data appear to be a validation of education efforts, given that they indicate that the clients surveyed did not agree with the stated conspiracies on the whole. However, this result remains concerning in and of itself in that they also didn't disbelieve these conspiracies. We are unable to discern whether this result was due to ambivalence or a well-considered neutrality, though the relatively narrow confidence interval of the mean for each question (<1.4 points) indicate that answers clustered near the middle rather than being split widely between total belief and disbelief in conspiracies.
5. Conclusion
This study adds to the limited information regarding hygiene practices and barriers to hygiene for the homeless population, as well as their attitudes and beliefs regarding vaccination, and should provide strategies for action going forward in the fight for better health outcomes among the homeless. Adequate hygiene practices and vaccination are vital factors in the prevention of HAV spread, and it is clear from the data that there are significant barriers yet to be overcome with regard to both. Pairing increased availability of and access to clean shower and laundry facilities with increased opportunities for HAV vaccination among the homeless is expected to decrease the incidence of HAV infections in the city of Detroit, based on known risks for transmission [7]. Addressing the concerns highlighted above should be a high public health priority and should prove effective in the mitigation of the current outbreak as well as in prevention or mitigation of future similar outbreaks.
Declarations
Author contribution statement
C. Buechler: conceived and designed the experiments; performed the experiments; analyzed and interpreted the data; wrote the paper.
A. Ukani: performed the experiments; analyzed and interpreted the data; wrote the paper.
R. Elesharawi, J. Gable, A. Petersen, M. Franklin: analyzed and interpreted the data; wrote the paper.
R. Chung: performed the experiments.
J. Bell, N. Hefzi, D. Carpenter: analyzed and interpreted the data.
A. Manly, R. Bryce: conceived and designed the experiments; analyzed and interpreted the data; wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Footnotes
Author dedication: The surviving authors would like to dedicate this manuscript to the memory of Dean Carpenter, whose mentorship has been irreplaceable and whose career spent treating and advocating for the homeless of Detroit remains an inspiration to all who knew him.
Appendix A. Supplementary data
The following is the supplementary data to this article:
Questionnaire Tool for Interview.
References
- 1.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta,GA: 2016. Surveillance for Viral Hepatitis- United States, 2011.https://www.cdc.gov/hepatitis/statistics/2011surveillance/pdfs/2011HepSurveillanceRpt.pdf Available at: [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta,GA: 2016. Surveillance for Viral Hepatitis- United States, 2016.https://www.cdc.gov/hepatitis/statistics/2016surveillance/pdfs/2016HepSurveillanceRpt.pdf Available at: [Google Scholar]
- 3.American Academy of Pediatrics Committee on Infectious Diseases Hepatitis A vaccine recommendations. Pediatrics. 2007 Jul;120(1):189–199. doi: 10.1542/peds.2007-1088. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) CDC Division of Health Informatics and Surveillance; Atlanta, GA: 2018. National Notifiable Diseases Surveillance System: Weekly Tables of Infectious Disease Data.https://www.cdc.gov/nndss/infectious-tables.html Available at: [Google Scholar]
- 5.Fiore A.E. Hepatitis A transmitted by food. Clin. Infect. Dis. 2004 Mar 1;38(5):705–715. doi: 10.1086/381671. [DOI] [PubMed] [Google Scholar]
- 6.Raoult D. Infection in homeless people. Lancet Infect. Dis. 2012 Nov;12(11):822–823. doi: 10.1016/S1473-3099(12)70186-X. [DOI] [PubMed] [Google Scholar]
- 7.Foster M., Ramachandran S., Myatt K. Hepatitis A Virus outbreaks associated with drug use and homelessness - California, Kentucky, Michigan, and Utah, 2017. MMWR Morb. Mortal. Wkly. Rep. 2018 Nov 2;67(43):1208–1210. doi: 10.15585/mmwr.mm6743a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crawford C. 2018. ACIP Recommends Hep A Vaccine for Homeless Patients. Leawood, KS: American Academy of Family Physicians.https://www.aafp.org/news/health-of-the-public/20181031acipmeeting.html Available at: [Google Scholar]
- 9.Tjon G.M., Gotz H., Koek A.G. An outbreak of hepatitis A among homeless drug users in Rotterdam, The Netherlands. J. Med. Virol. 2005 Nov;77(3):360–366. doi: 10.1002/jmv.20464. [DOI] [PubMed] [Google Scholar]
- 10.Michigan Department of Health and Human Services (MDHHS) Michigan Hepatitis A Outbreak. Michigan Department of Health and Human Services; Lansing, MI: 2018. Available at.https://www.michigan.gov/mdhhs/0,5885,7-339-71550_2955_2976_82305_82310-447907-,00.html [Google Scholar]
- 11.Homeless Action Network of Detroit (HAND) Homeless Action Network of Detroit; Detroit, MI: 2017. 2017 State of Homelessness: Annual Report for the Detroit Continuum of Care, January-December 2017.https://static1.squarespace.com/static/5344557fe4b0323896c3c519/t/5c082878cd83666ef1a7fc00/1544038549919/2017_HANDANNUALREPORT_.pdf Available at: [Google Scholar]
- 12.Leibler J.H., Nguyen D.D., Leon C. Personal hygiene practices among urban homeless persons in Boston, MA. Int. J. Environ. Res. Publ. Health. 2017 Aug 18;14(8) doi: 10.3390/ijerph14080928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson H.J., Jarrett C., Schulz W.S. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015 Aug 14;33(34):4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 14.Shapiro G.K., Holding A., Perez S. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016 Dec;2:167–172. doi: 10.1016/j.pvr.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stolte O., Hodgetts D. Being healthy in unhealthy places: health tactics in a homeless lifeworld. J. Health Psychol. 2015 Feb;20(2):144–153. doi: 10.1177/1359105313500246. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen P.V., Gronbaek M., Curtis T. Associations between deprived life circumstances, wellbeing and self-rated health in a socially marginalized population. Eur. J. Publ. Health. 2012 Oct;22(5):647–652. doi: 10.1093/eurpub/ckr128. [DOI] [PubMed] [Google Scholar]
- 17.Metcalfe S.E., Sexton E.H. An academic-community partnership to address the flu vaccination rates of the homeless. Publ. Health Nurs. 2014;31(2):175–182. doi: 10.1111/phn.12088. [DOI] [PubMed] [Google Scholar]
- 18.Stein J.A., Nyamathi A.M. Completion and subject loss within an intensive hepatitis vaccination intervention among homeless adults: the role of risk factors, demographics, and psychosocial variables. Health Psychol. 2010 May;29(3):317–323. doi: 10.1037/a0019283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarrett C., Wilson R., O'Leary M. SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy - a systematic review. Vaccine. 2015 Aug 14;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 20.Peretti-Watel P., Raude J., Sagaon-Teyssier L. Attitudes toward vaccination and the H1N1 vaccine: poor people's unfounded fears or legitimate concerns of the elite? Soc. Sci. Med. 2014 May;109:10–18. doi: 10.1016/j.socscimed.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 21.Dube E., Vivion M., MacDonald N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev. Vaccines. 2015 Jan;14(1):99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro G.K., Tatar O., Dube E. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018 Jan 29;36(5):660–667. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 23.Rozbroj T., Lyons A., Lucke J. Psychosocial and demographic characteristics relating to vaccine attitudes in Australia. Patient Educ. Counsel. 2019 Jan;102(1):172–179. doi: 10.1016/j.pec.2018.08.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Questionnaire Tool for Interview.