Coagulation factor V (FV) is a 330 kDa procofactor of the coagulation cascade that, upon activation, contributes to the formation of the prothrombinase complex, essential for the rapid generation of thrombin.1 FV deficiency (Online Mendelian Inheritance in Man #227400; https://www.omim.org/) is an autosomal recessive disorder, with an estimated prevalence in the general population of 1:1 million.2 The most common forms of FV deficiency are characterized by FV antigen (FV:Ag) levels that can vary from mildly reduced to unmeasurable (quantitative defect), whereas qualitative defects, showing normal/moderately decreased antigen levels associated with reduced FV coagulant activity (FV:C), are far rarer.2 Clinical manifestations range from mild bleeding (such as epistaxis, hematomas, easy bruising, and menorrhagia) to severe gastrointestinal or central nervous system hemorrhages.2 Both monoallelic and biallelic mutations in the FV gene (F5; 25 exons, 75 kb of length, chromosome 1q24.2) have been associated with FV quantitative defects, for a total of 139 mutations (Human Gene Mutation Database, public version, http://www.hgmd.cf.ac.uk/ac/index.php; accessed on April 05, 2019). Here, we present phenotype/genotype data on the largest cohort of FV deficient patients analyzed so far. In addition, integrating our results with the huge amount of data coming from F5-specific and genomic databases, we defined the mutational landscape of FV deficiency and estimated its world-wide prevalence.
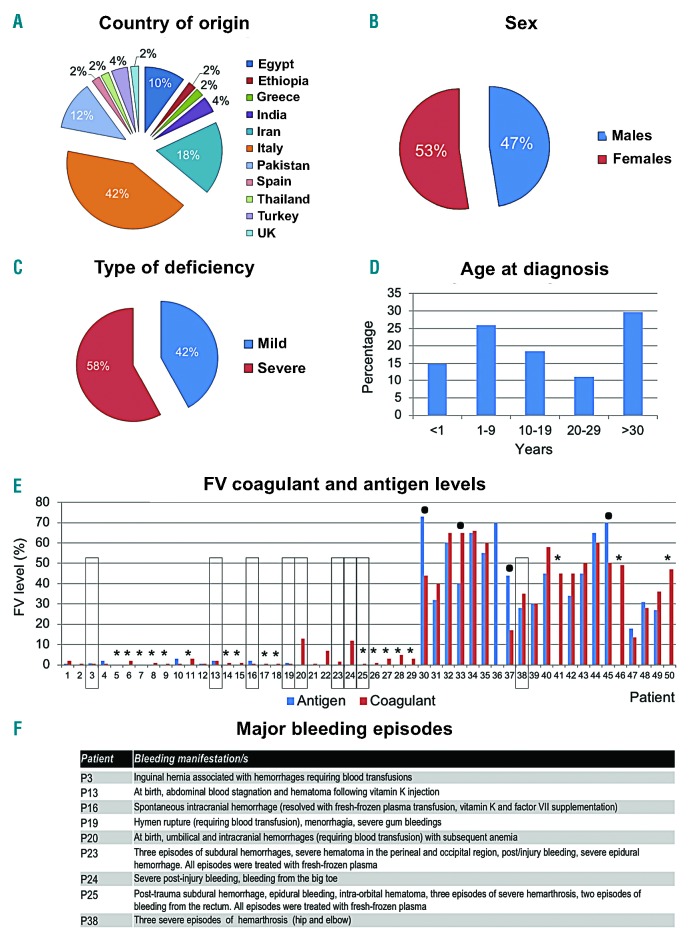
We enrolled 50 patients (P1-P50) with partial/severe FV deficiency, whose main demographic/clinical characteristics are summarized in Figure 1. A total of 29 patients suffered from severe FV deficiency (FV:C, <13%); 21 had partial deficiency: among them, six patients were characterized by levels of FV:C close to the lower limit of the normal range (FV:C normal range=60-140%).3 Only nine patients referred major bleeding, the most recurrent type being intracranial hemorrhage (Figure 1). Of note, three patients suffering from severe bleeding had FV levels (FV:C=12%, 13%, and 35%) that should be able to sustain a quasi-normal hemostasis (recommended FV levels in case of surgery or severe bleeding are ~20-25%).4 Hence, our data confirm yet again the lack of correlation between the clinical expression of the deficiency and plasma FV level.5
Figure 1.
Demographic and clinical characteristics of the case series. Local Ethics Committees approved this study. All individuals (or their parents, if minor) signed an informed consent according to the Declaration of Helsinki. Data on the enrolled 50 coagulation factor V (FV)-deficient patients are presented as aggregated. Pie-charts and histograms illustrate the country of origin (A), the female to male ratio (B), the classification of patients according to the severity of the deficiency (C), and the distribution of age at diagnosis (D). Data on sex and age are missing for one patient. FV coagulant (FV:C) and FV antigen (FV:Ag) levels are detailed in panel (E), where the number of each patient is reported on the X axis, and corresponds to the numbering (P1-P50) reported in Table 1. FV:C and FV:Ag were measured as described;3 normal ranges for both tests are 60-140%. All patients were measured for FV:C, except P36 (for whom only FV:Ag is reported). Patients lacking FV:Ag measurements are indicated by an asterisk. Patients showing a discordance >30% between FV:C and FV:Ag are marked by a dot. In panel (F), the list of all major bleeding episodes, affecting nine patients (evidenced with a rectangle in panel E), is reported.
Screening for mutations was performed by Sanger sequencing of the F5 coding regions and splice junctions. We disclosed a total of 42 different variants, five of which (p.Gly600Glu, p.Ser927AlafsX4, p.Arg1133X, p.Tyr1702Cys, p.Arg2074Cys) were found in more than one patient, and 29 were novel (17 missense, six nonsense, six indels) (Table 1; Online Supplementary Figure S1A). We checked for the newly identified variants in the GnomAD repository (reporting data on >125,000 exomes and >15,000 genomes from European, African, Asian, and Admixed American populations; https://gnomad.broadinstitute.org/; accessed on April 05, 2019) and only found p.Cys2033Tyr, p.Pro419Arg, and p.Ser1641Pro at an extremely low frequency (1-3 alleles in >250,000), and the more common p.Arg313Cys variant at a frequency of 7.6*10-4.
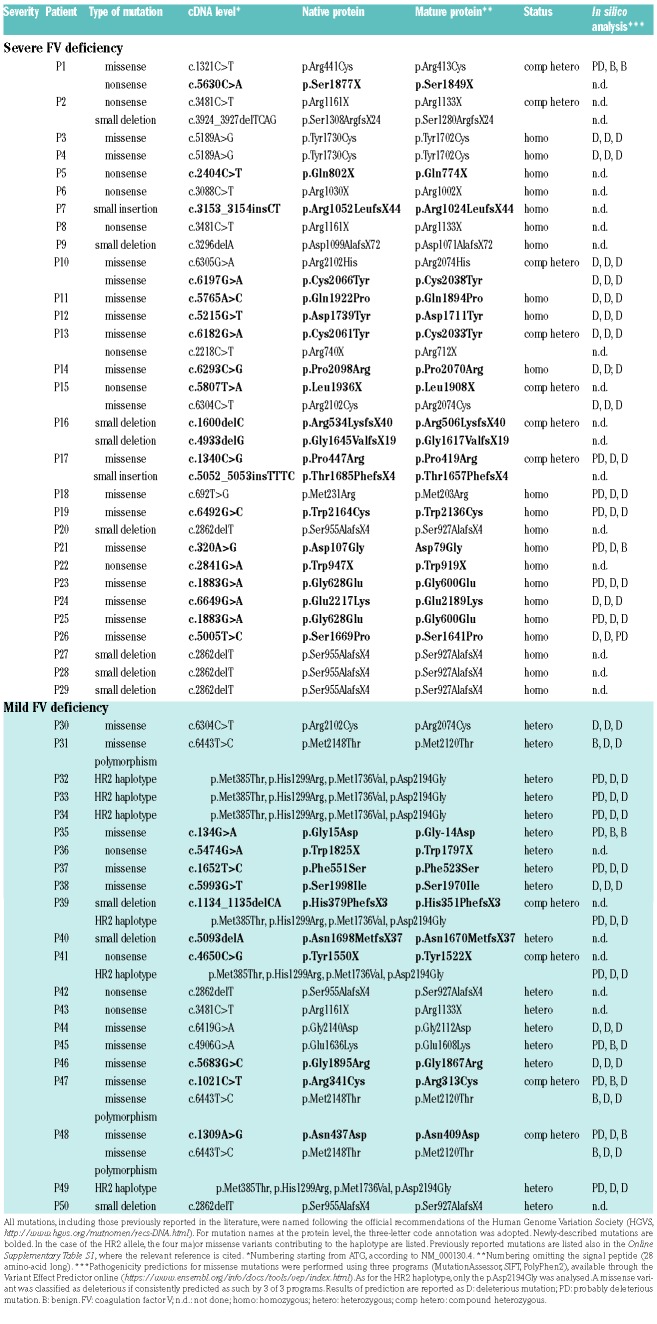
Table 1.
Genetic data of the coagulation factor V-deficient patients.
During the genetic screening we also found: i) three patients heterozygous for the p.Met2120Thr variant, a functional polymorphism determining a ~25% reduction in FV levels;6 ii) six patients heterozygous for the HR2 haplotype (Table 1). This haplotype is composed of a group of >10 linked genetic polymorphisms and is known to confer a partial FV deficiency.2,7 The functional dissection of the four missense variants constituting the haplotype (i.e. p.Met385Thr, p.His1299Arg, p.Met1736Val, p.Asp2194Gly) demonstrated a major contribution to the quantitative defect of the p.Asp2194Gly substitution (~70% reduction in FV levels), whereas moderately decreased secretion rates were detected for the p.Met385Thr and p.His1299Arg FV proteins.8
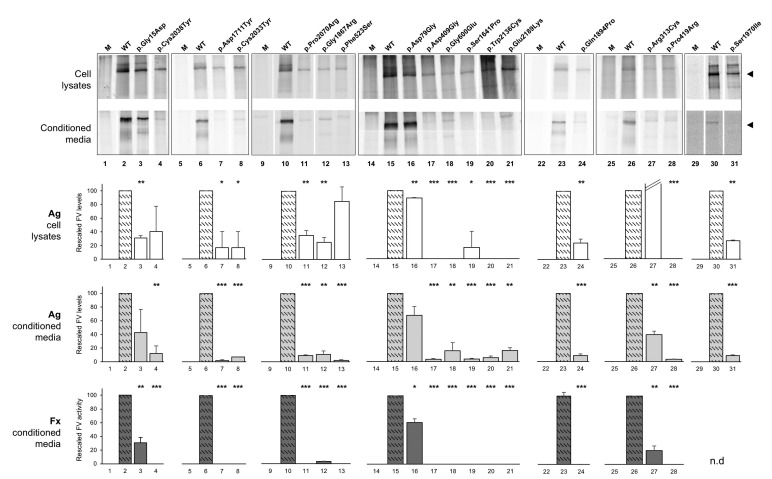
All missense variants, including the p.Met2120Thr and p.Asp2194Gly polymorphisms, as well as previously reported mutations (Online Supplementary Table S1), involve highly-conserved residues. They were all in silico analyzed by using three prediction programs (MutationAssessor, SIFT, PolyPhen2) through the Variant Effect Predictor tool (https://www.ensembl.org/info/docs/tools/vep/index.html). This analysis consistently predicted as deleterious a subset of 12 missense variants, whereas the remaining substitutions (including some already reported as a cause of FV deficiency) were predicted with conflicting results (Table 1). With these premises, to give conclusive results on the possible pathogenic role of the newly identified missense substitutions, we studied their impact on FV synthesis/secretion ex vivo. Site-directed mutagenesis was used to introduce in the pcDNA3-FV vector each missense substitution. We mirrored the wild-type/mutant homozygous conditions in COS-1 cells (not expressing FV) by transiently transfecting either the wild-type or each of the mutant constructs. We hence harvested recombinant [35S]-pulse-labelled FV molecules by immunoprecipitation both from cell lysates and conditioned media and performed SDS-PAGE analysis.9
With regards to intracellular FV, we observed a band corresponding to the wild-type or mutant protein in all cases (Figure 2A). As for conditioned media, we detected a severe reduction in the quantity of all mutant molecules, suggesting a secretion impairment (i.e. the “typical” consequence at the protein level of F5 missense mutations);2 the only exception regarded the p.Asp79Gly mutant, which was detected as a band almost comparable to the one observed for the wild-type condition (Figure 2B). These results were confirmed both by FV:Ag evaluation in cell lysates and serum-free conditioned media by ELISA, and by FV:C assays performed on culture media (Figure 2C-E). Specifically concerning the p.Asp79Gly substitution, only a slight reduction in antigen/functional levels were observed (~30/38% reduction), making the effects of this variant comparable to those of the p.Met2120Thr polymorphism.
Figure 2.
Transient expression of wild-type and mutant coagulation factor V proteins in COS-1 cells. Radiolabelled coagulation factor V (FV) was immunoprecipitated from cell lysates (A) and conditioned media (B) of COS-1 cells transfected with plasmids expressing FV (wild-type or mutant). Mock-transfected COS-1 cells represent the negative control (lane M). Proteins were electrophoresed on 4% SDS-PAGE gels under non-reducing conditions. Arrowheads indicate FV monomeric molecules. Antigen (Ag) levels of recombinant FV were measured both in cell extracts (C) and in the corresponding conditioned media (D) by an ELISA assay. FV activity (Fx) was measured in conditioned media by a functional assay based on the prothrombin time (E). In all graphs, bars represent means + standard deviations of at least two independent experiments, each performed in duplicate. The mean value of wild-type FV was set as 100%. Significance levels of t-tests are shown: *P<0.05, **P<0.01, ***P<0.001. Details on all methodological aspects can be found in9.
Altogether, our results indicate that all of the 29 newly identified substitutions (including 17 missense) can be regarded as truly pathogenic, thus increasing the number of mutations causing FV deficiency by 21%. The distribution of these defects according to their position along the F5 gene is reported in the Online Supplementary Figure S1B. Here, the almost complete lack of missense variants in the unstructured B domain is evident. Interestingly, the most upstream homozygous truncating mutation is located at position 77310 strengthening the concept that in humans a complete FV deficiency is incompatible with life.2
To have a comprehensive picture of the burden of potentially deleterious mutations in the F5 gene, we also collected data from the GnomAD database. Among the reported variants, we retrieved all null mutations (nonsense, indels, and splice mutations involving the first or last two intronic nucleotides) plus non-synonymous variants annotated as damaging by 3 of 3 prediction programs. We found 178 variants in ~250,000 different alleles, all present in the heterozygous state. We excluded from this calculation the common p.Met2120Thr variant and the four missense polymorphisms of the HR2 haplotype. The F5 mutational landscape in the general population mirrors the mutational spectrum observed for the deficiency, both in terms of mutation scattering along the gene, and of the distribution of mutation types (Online Supplementary Figure S1C-E). Hence, we used the GnomAD data to infer the world-wide prevalence of severe FV deficiency (i.e. due to homozygous or compound heterozygous mutations), using an approach similar to that already adopted for other rare inherited coagulation defects.11,12 We estimated a world-wide prevalence rate of 1 in 2 million for severe FV deficiency in the general population, even rarer than that reported in the literature so far.5 Certainly we have to recognize some limitations relative to our prevalence estimate, also considering that FV is a double-faced molecule with both pro-thrombotic and anti-thrombotic characteristics.2,7 Some among the rare mutations included in the calculation could indeed be associated with the production of a dysfunctional molecule with a pro-thrombotic behavior (as in the case of the relatively common Leiden mutation, p.Arg506Gln),13 thus overestimating the prevalence rate of the deficiency. On the other hand, we used stringent conditions in predicting the pathogenicity of mutations (as demonstrated above; Table 1), thus possibly underestimating the prevalence rate. In addition, it is well-known that exome data lack information not only on deep-intronic/promoter mutations and gross deletion/rearrangements by design, but also on indel mutations for problems intrinsic to variant-caller programs, thus again possibly leading us to underestimate the FV-deficiency prevalence. In any case, the Leiden mutation was not included in our prevalence calculation; importantly, this genetic defect is not properly reported in GnomAD, where p.Gln506 (p.Gln534Arg according to official nomenclature) is erroneously considered the reference allele and the Gln-to-Arg substitution is flagged as “dubious”.
As for common FV-lowering functional defects, i.e. p.Met2120Thr and the HR2-tagging variant p.Asp2194Gly, in GnomAD they show an allele frequency of 3.1% and 6.3%, respectively, testifying that a mild deficiency for FV could be rather common in the general population. In the Online Supplementary Figure S2 we also report the frequencies of the HR2 haplotype in different populations, estimated by using either in-house or publicly available data. This analysis shows that HR2 is absent among Africans, is relatively rare in East Asians (2.7%) and it is quite common in other populations, reaching the notable frequency of 8.2% among Admixed Americans. This observation could be of particular importance, especially considering that the HR2 allele can be present in trans with the Leiden mutation, exacerbating its pro-thrombotic effect, as in the case of the pseudo-homozygous activated protein C resistance.14
In conclusion, this work reports the largest case series of FV-deficient patients described so far, increases the number of FV-causing mutation by one fifth, and paints -for the first time- the complete world-wide mutational landscape for the F5 gene.
Acknowledgments
We thank all family members for their participation in this study. We would like to thank Dr. Massimo Boscolo for his precious help in performing FV measurements in patients’ plasma, cell lysates, and conditioned media. Dr Davide De Bortoli, Fabiola Valenza, Nicola Fenderico, Nadia Locatelli, Ilaria Guella, Stefania Di Maggio, Roberta Marotta, and Claudia Dall’Osso are acknowledged for their irreplaceable assistance, support, and enthusiasm. We are indebted with Dr Nihal Ozdemir, Ponlapat Rojnuckarin, Mehran Karimi, Helen Pergantou, Raquel Saez Villaverde, Simon Fletcher, Kaan Kavakli, and Alok Srivastava for their precious participation in collecting the patients and their clinical history.
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Duga S, Asselta R, Tenchini ML. Coagulation factor V. Int J Biochem Cell Biol. 2004;36(8):1393–1399. [DOI] [PubMed] [Google Scholar]
- 2.Asselta R, Tenchini ML, Duga S. Inherited defects of coagulation factor V: the hemorrhagic side. J Thromb Haemost. 2006;4(1):26–34. [DOI] [PubMed] [Google Scholar]
- 3.Paraboschi EM, Menegatti M, Peyvandi F, Duga S, Asselta R. Understanding the impact of aberrant splicing in coagulation factor V deficiency. Int J Mol Sci. 2019;20(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolton-Maggs PH, Perry DJ, Chalmers EA, et al. The rare coagulation disorders–review with guidelines for management from the United Kingdom Haemophilia Centre Doctors’ Organisation. Haemophilia. 2004;10(5):593–628. [DOI] [PubMed] [Google Scholar]
- 5.Asselta R, Peyvandi F. Factor V deficiency. Semin Thromb Hemost. 2009;35(4):382–389. [DOI] [PubMed] [Google Scholar]
- 6.Scanavini D, Girelli D, Lunghi B, et al. Modulation of factor V levels in plasma by polymorphisms in the C2 domain. Arterioscler Thromb Vasc Biol. 2004;24(1):200–206. [DOI] [PubMed] [Google Scholar]
- 7.Vos HL. Inherited defects of coagulation Factor V: the thrombotic side. J Thromb Haemost. 2006;4(1):35–40. [DOI] [PubMed] [Google Scholar]
- 8.Yamazaki T, Nicolaes GA, Sørensen KW, Dahlbäck B. Molecular basis of quantitative factor V deficiency associated with factor V R2 haplotype. Blood. 2002;100(7):2515–2521. [DOI] [PubMed] [Google Scholar]
- 9.Duga S, Montefusco MC, Asselta R, et al. Arg2074Cys missense mutation in the C2 domain of factor V causing moderately severe factor V deficiency: molecular characterization by expression of the recombinant protein. Blood. 2003;101(1):173–177. [DOI] [PubMed] [Google Scholar]
- 10.van Wijk R, Nieuwenhuis K, van den Berg M, et al. Five novel mutations in the gene for human blood coagulation factor V associated with type I factor V deficiency. Blood. 2001;98(2):358–367. [DOI] [PubMed] [Google Scholar]
- 11.Paraboschi EM, Duga S, Asselta R. Fibrinogen as a pleiotropic protein causing human diseases: the mutational burden of Aα, Bb, and g Chains. Int J Mol Sci. 2017;18(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asselta R, Paraboschi EM, Rimoldi V, et al. Exploring the global landscape of genetic variation in coagulation factor XI deficiency. Blood. 2017;130(4):e1–e6. [DOI] [PubMed] [Google Scholar]
- 13.Bertina RM, Koeleman BP, Koster T, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature. 1994;369(6475):64–67. [DOI] [PubMed] [Google Scholar]
- 14.Guasch JF, Lensen RP, Bertina RM. Molecular characterization of a type I quantitative factor V deficiency in a thrombosis patient that is “pseudo homozygous” for activated protein C resistance. Thromb Haemost. 1997;77(2):252–257. [PubMed] [Google Scholar]