Abstract
Background. Human bocavirus (HBoV) was recently described as a new member of the Parvoviridae family, and its possible association with respiratory illness in infants has been discussed. To date, HBoV genomes have been detected worldwide in respiratory tract samples obtained from children with pulmonary diseases, whereas only limited data on virus-specific immunity are available, mainly because of the lack of recombinant viral antigens.
Methods. HBoV viruslike particles (VLPs) were produced in insect cells and characterized by electron microscopy and cesium chloride gradient centrifugation. HBoV viral protein 2 (VP2)-specific antibodies and CD4+ T helper cell responses were analyzed by enzyme-linked immunsorbent assay and enzyme-linked immunospot assay.
Results. VP2 capsid proteins of HBoV were produced in insect cells infected with a recombinant baculovirus, and the formation of icosahedral VLPs (diameter, 21–25 nm; sedimentation density, 1.33 g/cm3) was demonstrated. A significant increase in secretion of VP2-specific interferon-γ was detected in cultures of peripheral blood mononuclear cells obtained from 69 healthy adults found to be positive for HBoV-specific immunoglobulin G antibodies, compared with control stimulations. In parallel, T cell responses against identically expressed parvovirus B19 VP2 VLPs were frequently observed in the individuals studied, without there being obvious cross-reactions between HBoV and parvovirus B19.
Conclusions. Data suggest the presence of HBoV-specific immune responses in adults and strongly support a high prevalence of HBoV among humans.
Human bocavirus (HBoV), a newly discovered member of the Parvoviridae family, was recently identified in children and infants with infections of the lower respiratory tract [1]. HBoV is the second parvovirus currently being discussed as a cause of disease in humans. Comprehensive phylogenetic analysis of the HBoV genome has revealed a close association between HBoV and the canine minute virus and the bovine parvovirus, both of which are members of the Bocavirus genus. To date, several HBoV isolates with high sequence homology have been described [2].
Parvoviruses are small, nonenveloped viruses that are characterized by linear single-stranded DNA genomes of 4–6 kb. Common characteristics of parvoviruses are their exceptional stability and the structural simplicity of the virions [3]. The icosahedral virus capsids generally consist of 2 proteins (viral protein 1 [VP1] and viral protein 2 [VP2]) that have identical sequences, except for the aminoterminal domain of VP1 (known as the “VP1 unique region”), which spans 129 and 227 amino acids in HBoV and parvovirus B19 (B19V), respectively [4]. B19V VP2 proteins have been shown to possess all the characteristics required for particle formation. Viruslike particles (VLPs) consisting of VP2 alone or of VP2 and VP1 may be produced in various eukaryotic expression systems (e.g., recombinant baculovirus or yeast) [5, 6].
HBoV has been a target of epidemiologic studies since its initial detection. To date, by use of polymerase chain reaction-based techniques, HBoV has been detected not only in clinical respiratory tract samples but, also, in fecal excretions from young children in Australia, North America, Asia, Europe, Africa, and the Middle East, thereby indicating a worldwide distribution of the virus [7–17]. The prevalence of HBoV DNA in samples obtained from children and infants with symptoms of respiratory illness has been found to be 1.5%–18.3%, and it may vary depending on seasonal fluctuation and the age of the patients studied. Because the majority of epidemiologic studies have been performed retrospectively, HBoV has not been clearly identified as a sole infectious agent responsible for respiratory diseases. In fact, HBoV tends to be associated with a high rate of coinfection with other respiratory viruses (e.g., picornaviruses, adenoviruses, and respiratory syncytial virus) in children. Clinical symptoms associated with HBoV infections include cough, fever, pneumonia, and bronchitis. To date, only single reported cases of HBoV infections in adults have been observed, mainly in immunocompromised individuals [18, 19].
Immunologic studies have described the use of recombinant HBoV VP1 protein in the detection of virus-specific IgG responses in the Japanese population [20]. Thereby, ubiquitous VP1-specific antibody responses (with a seroprevalence of up to 100%) were detected in adult individuals and in children (age, >6 years), whereas a seronegative status was predominantly noted among young children at 1 year of age. No data are currently available on HBoV-specific T cell immunity. Numerous studies of B19V, however, have described viral capsid proteins as immunodominant targets of the cellular and humoral immune response [21–24], suggesting a possibly similar role for HBoV capsid proteins in virus-specific immunity.
In the present study, we describe the recombinant expression and characterization of HBoV VP2 VLPs and their use in the detection of cellular immune responses against HBoV in healthy adults.
Materials and Methods
Study subjects and serologic testing. A total of 69 healthy, white individuals (39 men and 30 women; mean age, 39 years [range, 23–73 years]) from the southeastern region of Bavaria, Germany, were studied to identify HBoV- and B19V-specific T cell responses (table 1) and to detect the presence of virus-specific antibodies by means of ELISA. For HBoV, 100 ng of HBoV VP2 VLPs were coated on Nunc-Immuno MediSorp plates (Nunc) in PBS overnight at 4°C, washed 6 times with washing buffer (PBS containing 0.05% Tween 20), and blocked with dilution buffer (PBS containing 2% Tween 20 and 3% FCS) for 1 h at 37°C. After incubation with serum samples (1:100 in dilution buffer) was done for 2 h at 37°C, the plates were washed, and an anti-human IgG-specific, horseradish peroxidase-coupled secondary antibody (Dako Deutschland) (1:6000 in dilution buffer) was added for 1 h at 37°C. Development was performed using BD OptEIA Substrate (BD Biosciences) according to the manufacturer's instructions. B19V-specific IgG and IgM antibodies were detected in donor serum samples by use of a standardized ELISA (Biotrin International) and RecomBlot analysis (Mikrogen).
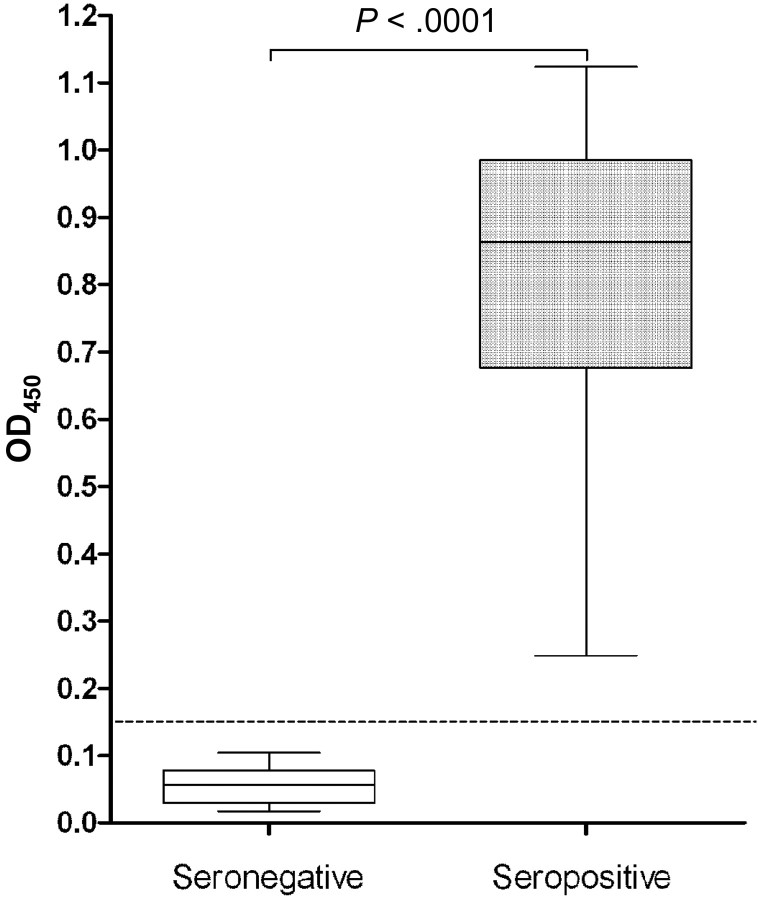
Table 1.
Antigen-specific interferon (IFN)-γ secretion in healthy adults seropositive for human bocavirus (HBoV).
Generation of a recombinant baculovirus for the expression of HBoV VP2 antigens. A recombinant baculovirus encoding the VP2 gene of the HBoV ST2 isolate was generated using the Bac-to-Bac Baculovirus Expression System (Invitrogen). In brief, the VP2 gene was amplified from a pCR 4-TOPO vector (Invitrogen) that included the genome sequence of HBoV ST2 (GenBank accession number NC_007455) (provided by Tobias Allander, Karolinska Institute, Stockholm, Sweden), by use of the primers 5′-GAGGAGCGGCCGCATGTCTGACACTGACATTC-3′ and 3′-CCGCCCTCGAGTTACAACACTTTATTGATG-5′ with Phusion High-Fidelity DNA Polymerase (Finnzymes OY). The amplicon was introduced into the pFastBac1 vector (Invitrogen) by the Xho I and Not I restriction sites. Generation of recombinant HBoV VP2 bacmid pFastBac/VP2bac and its subsequent transfection into Sf9 insect cells were performed according to the manufacturer's instructions. The resulting virus, bacVP2/HBoV, was amplified in 3 consecutive passages of infection and subsequently was used for protein production. For the expression of B19V VP2 VLPs, the previously established and described recombinant baculovirus bacVP2/B19V was used [25].
Production and purification of recombinant HBoV VLPs. Production of both HBoV and B19V VLPs was achieved in High-5 insect cells. Cells were cultured in Insect-Xpress medium (Cambrex Bio Science Walkersville), infected with bacVP2/HBoV or bacVP2/B19V at an MOI of 3, and harvested 72 h after infection. Recombinant VLPs were purified by cesium chloride (CsCl) cushion centrifugation. A total of 6 × 107 cells were lysed in 5 mL of buffer containing 10 mmol/L Tris/HCl (pH 7.4), 10 mmol/L NaCl, 15 mmol/L MgCl2, and 0.5% Triton X-100 with 40 µl/mL Complete Protease Inhibitor Cocktail (Roche Applied Science) and then were subjected to successive freeze-thaw cycles. The precleared lysates were loaded on double cushions consisting of CsCl solutions with densities of 1.52 g/cm3and 1.22 g/cm3 in Tris-EDTA buffer (10 mmol/L Tris/HCl [pH 8.7], 1 mmol/L EDTA, and 0.5% Triton X-100). Ultracentrifugation was performed at 100,000 g for 4 h at 10°C without brakes. After centrifugation, protein samples were collected in fractions and subjected to SDS-PAGE and Western blot analysis. Endotoxin contaminations of fractions containing antigen were excluded using the QCL-1000 Chromogenic LAL Endpoint Assay (Lonza), and they were determined to be 1.57 EU/mg and 8.2 EU/mg for HBoV and B19V VP2 VLPs, respectively. Characterized antigens underwent dialysis against PBS and were stored in aliquots at −80°C. Freeze-thaw cycles of the purified proteins were avoided.
Isolation and culture of human peripheral blood mononuclear cells (PBMCs). PBMCs were isolated from fresh heparinized blood samples by means of Pancoll centrifugation (PAN Biotech) (at 800 g for 30 min) with the use of Leucosep tubes (Greiner Bio-One). Cells were washed twice in PBS and were cultured in RPMI 1640 medium (PAN Biotech) containing 2 mmol/L l-glutamine, 100 U/mL penicillin, 100 µg/mL streptomycin, and 10% heat-inactivated human AB serum (PAA Laboratories), in an atmosphere with 5% CO2 at 37°C.
Enzyme-linked immunospot (ELISPOT) assays. A total of 2 × 105 PBMCs were seeded in 4 replicate wells on Mahan 4550 MultiScreen ELISPOT plates (Millipore) that had been previously coated with 5 µg/mL anti-human interferon (IFN)-γ monoclonal antibody D1K (Mabtech), stimulated with 5 µg/mL VP2 VLPs of either HBoV or B19V, and incubated at 37°C for 60 h. As negative and positive controls, cells were stimulated with 5 µg/mL HIV p24-derived murine e10F peptide [26] and 5 ng/mL staphylococcal enterotoxin B (Sigma Aldrich), respectively. For development, the plates were incubated for 2 h with 1 µg/mL biotinylated anti-IFN-γ 7-B6-1 Biotin antibody (Mabtech) and for 1 h with streptavidin-alkaline phosphatase (diluted 1:1000 in PBS). Staining was performed using the NBT/BCIP Stock Solution (Roche Diagnostics) in buffer containing 0.1 mol/L NaCl, 0.1 mol/L Tris/HCl [pH 9.5], and 0.05 mol/L MgCl2. The number of spot-forming cells (SFCs) was determined under magnification, by use of a Bioreader 2000 (BioSys).
T cell depletion assays. Depletion of CD4+ or CD8+ T cells from donor PBMC cultures was performed using CD4 and CD8 Dynabeads (Dynal Biotech ASA). For control, the purity of depleted cell populations was assessed by staining with the CytoStat Multicolor Reagent CD45-FITC/CD4-PE/CD8-ECD/CD3-PC5 (Beckman Coulter) and an anti-CD14-PE antibody (BD Biosciences) (data not shown). A FACS Epics XL-MCL flow cytometer (Beckman Coulter) was used for analysis. All experiments were conducted according to the manufacturer's instructions.
Statistical data analysis. Serologic and cellular responses were statistically evaluated using the Mann-Whitney U-test for independent samples.
Results
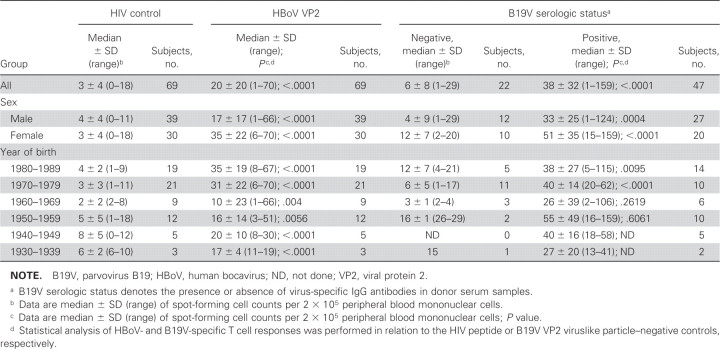
Generation of recombinant baculovirus bacVP2/HBoV for the production of HBoV VP2 proteins in insect cells. The recombinant baculovirus bacVP2/HBoV encoding the VP2 gene of the HBoV Stockholm 2 isolate (nt 3443-5071) was generated and used for infection of High-5 cells. In parallel, cells were infected with a previously established recombinant baculovirus bacVP2/B19V encoding the VP2 protein of B19V. SDS-PAGE studies of bacVP2/HBoV- and bacVP2/B19V-infected cells lysed 72 h after infection revealed high-yield expression of the VP2 proteins, with an apparent molecular weight of ∼62 kDa noted after Coomassie staining (figure 1A[lane 1] and 1B[lane 1]). The identity of both HBoV with B19V VP2 proteins was demonstrated using Western blot analysis of serum samples obtained from individuals seropositive for HBoV or B19V IgG (figure 1A[lane 2] and 1B[lane 2]).
Figure 1.
Production of viral protein 2 (VP2) proteins of human bocavirus (HBoV) and parvovirus B19 (B19V) and the purification of viruslike particles. SDS-PAGE analysis of lysates of High-5 cells infected with bacVP2/HBoV (A) or bacVP2/B19V (B), stained with Coomassie blue (lanes 1), or analyzed by Western blotting with IgG derived from HBoV- or B19V-seropositive individuals (lanes 2). SDS-PAGE analysis and subsequent Coomassie blue staining of HBoV and B19V VP2 proteins after purification via cesium chloride ultracentrifugation (lanes 3). MW, molecular weight.
Purification and characterization of recombinant HBoV VP2 VLPs. To analyze whether the expressed HBoV VP2 proteins posses the capacity to spontaneously aggregate to VLPs, as shown for the VP2 proteins of numerous parvoviruses, bacVP2/HBoV-infected High-5 cells underwent a previously established procedure for the purification of VP2 VLPs of human B19V [25]. Separation of proteins in precleared lysates of High-5 cells expressing either HBoV or B19V VP2, by means of CsCl ultracentrifugation, resulted in pure preparations of VP2 proteins, as was shown by SDS-PAGE and subsequent Coomassie staining (figure 1A[lane 3] and 1B[lane 3]).
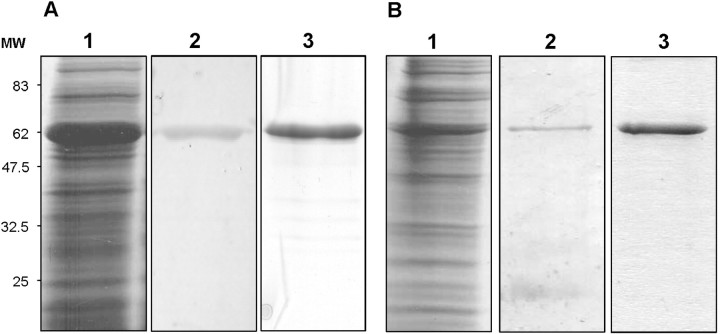
BacVP2/HBoV-infected High-5 cells and purified preparations of HBoV VP2 proteins were assessed by electron microscopy. Analysis of cross-sections prepared from bacVP2/HBoV-infected High-5 cells revealed a high number of particulate structures in the cytoplasm, suggesting spontaneous formation of HBoV VLPs in cells expressing VP2 (figure 2A). This could be confirmed by electron microscopic analysis of CsCl gradient fractions in which VP2 proteins could be detected by SDS-PAGE and Western blot analysis. Here, distinct icosahedral capsid structures with an approximate diameter of 21–25 nm (figure 2B) were detectable. The density of HBoV VP2 VLPs was assessed by ultracentrifugation in continuous CsCl gradients (1.29–1.4 g/cm3) for 48 h at 150,000 g and revealed a value of ∼1.33 g/cm3.
Figure 2.
Electron microscopic analysis of human bocavirus (HBoV) viral protein 2 (VP2) viruslike particles (VLPs). A, High-5 insect cells were infected with the recombinant baculovirus bacVP2/HBoV and harvested 72 h after infection. Ultrathin sections of the infected cells were examined by electron microscopy. Particulate structures (identified by arrows) were observed in the cytoplasm. B, HBoV VP2 VLPs purified from lysates of High-5 cells infected with bacVP2/HBoV by cesium chloride ultracentrifugation. Fractions containing VP2 proteins were prepared for electron microscopic analysis by negative staining with 2% phosphotungstic acid.
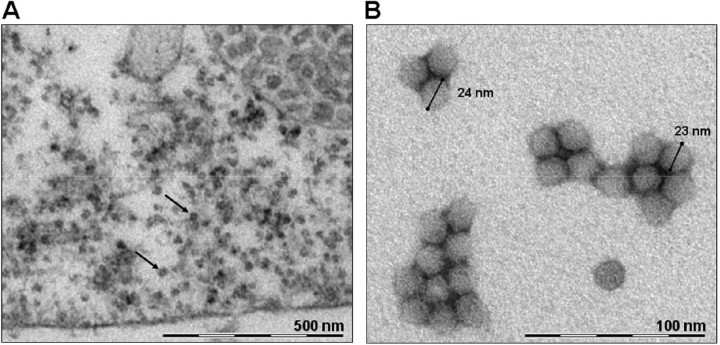
Detection of HBoV- and B19V-specific antibodies. In total, 69 adults were included in the study, and they were found to exhibit strong IgG-mediated humoral immune responses against HBoV VP2 VLPs, by use of ELISA (median OD450 value, 0.863 [range, 0.248–1.124]) (figure 3). Because HBoV-seronegative individuals have been described and were found predominantly among infants and young children (those ≤ 2 years of age) [20, 27, 28, 29], serum samples obtained from 10 healthy infants (mean age, 11.8 months [range, 6–45 months]) without detectable virus-specific antibodies (median OD450 value, 0.056 [range, 0.017–0.104]) were selected and representatively included in the study, to ensure the specificity of the serologic analysis performed. With respect to B19V, 47 of 69 volunteers displayed IgG antibodies against the VP1/VP2 proteins, indicating past B19V infection (table 1). B19V-specific IgM antibodies were not detectable in any of the serum samples.
Figure 3.
Detection of human bocavirus (HBoV)-specific IgG antibodies in healthy adults. By use of viral protein 2 (VP2) viruslike particles (VLPs), all 69 healthy adults who were studied were found to be positive (seropositive) for HBoV-specific IgG antibodies by ELISA. Because seronegative individuals have been predominantly described and could only be found among young children and infants, a total of 10 representative (seronegative) children (mean age, 11.8 months) were included in the study to ensure the specificity of the serologic analysis performed. The cutoff value for positive results (dashed line) was defined as an optical density value that was 2.5-fold greater than the median optical density value (horizontal line) noted for infants without HBoV-specific IgG reactions who were evaluated.
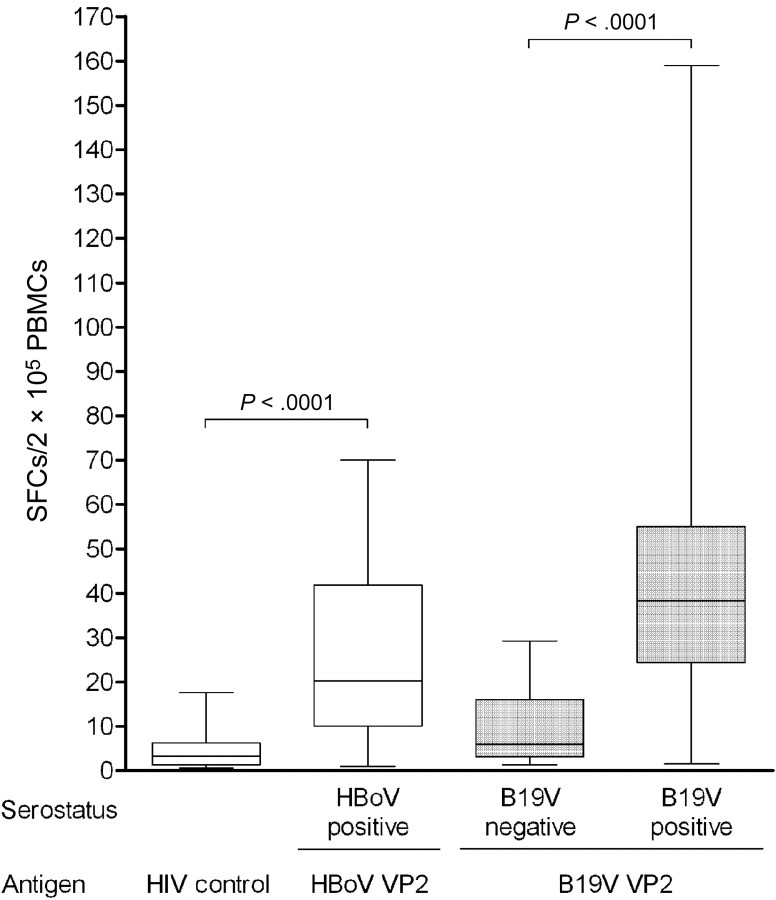
IFN-γ mediated CD4+ T helper cell responses against HBoV VP2 VLPs in healthy adult individuals. Because sufficient volumes of blood samples could not be obtained from very young children, only HBoV-seropositive adults underwent analysis for HBoV- and B19V-specific cellular immune responses by use of the ELISPOT assay. Using PBMCs stimulated with either HBoV or B19V VP2 VLPs (5 µg/mL), virus-specific ex vivo IFN-γ immune responses with median values of 20 and 38 SFCs/2 × 105 PBMCs were detected in HBoV- and B19V-seropositive individuals, respectively (figure 4). The correlation of the number of HBoV-specific IFN-γ-secreting cells with anti-HBoV IgG responses did not reveal any statistical significance (P = .5809). For this analysis, HBoV-seropositive individuals were divided in 2 groups: those with OD450 values below the median value and those with OD450 values above the median, respectively. Both groups displayed a median of 20 SFCs/2 × 105 PBMCs.
Figure 4.
Interferon (IFN)-γ secretion in the peripheral blood mononuclear cells (PBMCs) of adults after stimulation with human bocavirus (HBoV) and parvovirus B19 (B19V) viral protein 2 (VP2) capsid antigens. PBMCs isolated from the blood of 69 HBoV-seropositive, B19V-seropositive (n = 47) or seronegative (n = 22) donors were subjected to stimulation with either HBoV or B19V VP2 viruslike particles (VLPs) for 60 h. The HIV p24-derived peptide e10F served as a negative control for all HBoV-seropositive (HIV control) individuals studied. Data are the median (horizontal line) and the range of IFN-γ spot-forming cell (SFC) counts per 2 × 105 PBMCs, as detected by enzyme-linked immunospot assay.
No significant IFN-γ responses (median response, 3 SFCs/2 × 105 PBMCs) were measured against the synthetic HIV peptide e10F, which was used as a control for HBoV stimulations. Control stimulations of B19V-seronegative individuals that involved the use of B19V VP2 VLPs resulted only in background levels of IFN-γ secretion (median response, 6 SFCs/2 × 105 PBMCs).
To exclude the possibility that cross-reactions between VP2 proteins of HBoV and B19V contributed to the positive test results, HBoV-specific immune responses were analyzed in association with B19V serologic findings. Thereby, no statistically significant correlation (P = .4237) was observed as median values of 17 and 26 SFCs/2 × 105 PBMCs were measured in B19V-seronegative and -seropositive individuals, respectively, after HBoV VP2 VLP stimulation.
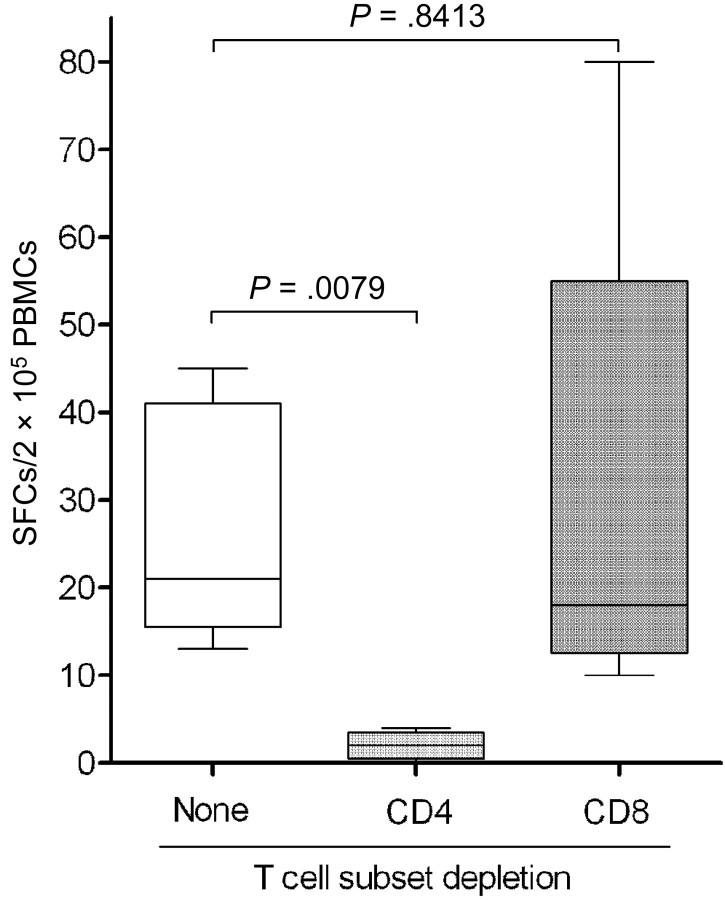
To associate the HBoV VP2-specific cytokine responses with specific cell populations, stimulations of cultures of PBMCs depleted from either CD4+ or CD8+ T cells were performed (figure 5). In cultures of PBMCs obtained from 5 HBoV-seropositive individuals who were tested, a substantial reduction in the median number of cells secreting IFN-γ (from 21 to 2 SFCs/2 × 105 PBMCs) (P = .0079) was observed after depletion of CD4+ T helper cells, whereas HBoV-specific T cell responses remained detectable (median response, 18 SFCs/2 × 105 PBMCs) after depletion of CD8+ cytotoxic T lymphocytes (P = .8413). This finding suggests a pivotal role of the CD4+ lymphocyte subset in the cellular immune response against VP2 proteins of HBoV.
Figure 5.
Human bocavirus (HBoV) viral protein 2 (VP2)-specific interferon (IFN)-γ secretion in HBoV-seropositive individuals after T cell subset depletion. Peripheral blood mononuclear cells (PBMCs) obtained from HBoV-seropositive individuals were depleted from either CD4+ or CD8+ T cells and were subjected to stimulation with HBoV VP2 viruslike particles (VLPs). IFN-γ secretion was assessed by enzyme-linked immunospot assay. Data are the median (horizontal line) and the range of spot-forming cell (SFC) counts per 2 × 105 PBMCs, as determined from independent stimulations performed on 5 study subjects.
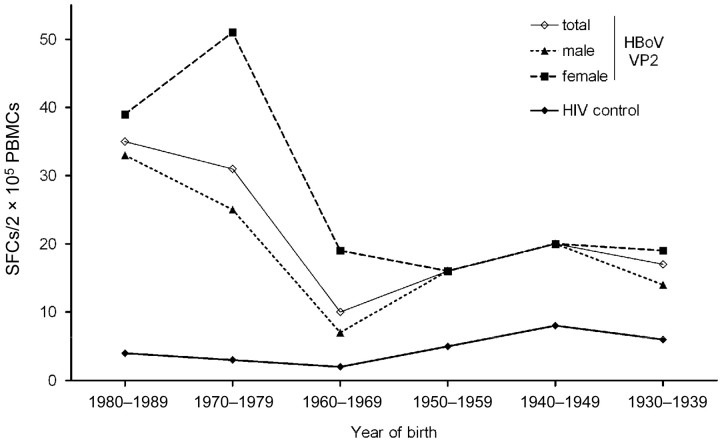
Correlation of the HBoV VP2-specific immune responses with the age of the study subjects revealed an age-dependent decrease in the median number of cells secreting IFN-γ (from 35 SFCs/2 × 105 PBMCs in young adults [age, 18–27 years] born between 1980 and 1989 to 17 SFCs/2 × 105 PBMCs in elderly adults [age, 68–77 years] born between 1930 and 1939) (figure 6). In general, when compared with men, women displayed higher or equal numbers of HBoV-specific T cells against HBoV VP2 VLPs, in all age groups. This observation was most prominent among individuals born between 1970 and 1979 (age, 28–37 years), as was revealed by median responses of 25 SFCs/2 × 105 PBMCs and 51 SFCs/2 × 105 PBMCs for men and women, respectively (P = .0667).
Figure 6.
Age-dependent decrease in human bocavirus (HBoV) viral protein 2 (VP2)-specific interferon (IFN)-γ-secreting cells in HBoV-seropositive individuals. The HBoV VP2-specific IFN-γ responses of all seropositive adult study subjects studied were correlated with the year of birth and the sex of the respective individuals. Data are median IFN-γ spot-forming cell (SFC) counts per 2 × 105 peripheral blood mononuclear cells (PBMCs) from study subjects grouped according to their year of birth.
Discussion
HBoV VLPs consisting of VP2 proteins can be produced using the baculovirus expression system. Similar capacities for other parvoviruses, such as B19V, the canine parvovirus, and the porcine parvovirus, have been described elsewhere [5, 30, 31]. By use of electron microscopy and CsCl gradient centrifugation, HBoV VP2 VLPs were shown to possess a diameter comparable to that of native HBoV virions [32] and sedimentation densities similar to those of capsids of the canine parvovirus [33].
Recombinant VLPs are potent reagents for virologic and clinical research and have greatly contributed to the improvement of sensitive diagnostic tests and the development of vaccine against many viruses (e.g., human papillomavirus and hepatitis B virus) [34, 35]. Recombinant VP2 particles are known to be crucial in the diagnosis of B19V infections, because virus-specific antibodies lose their affinity against linear antigenic regions in a time-dependent manner and are replaced by humoral responses against conformational epitopes [36]. Whether similar applications can be established for HBoV VP2 VLPs needs to be assessed in further studies.
Using HBoV VLPs, we observed frequent VP2-specific humoral immune responses in healthy adults, whereas seronegative status was predominantly detected in young children (age, ≤ 2 years) [27, 37]. Furthermore, this finding is strongly supported by recent epidemiologic data, which describe a seroprevalence of HBoV-specific IgG antibodies that already reaches up to 100% during early childhood [20]. Because of the very young age of the seronegative individuals, it was not possible to obtain blood samples with volumes sufficient for the analysis of HBoV-specific T cell immunity.
In seropositive adults, frequent cellular immune responses were observed after HBoV VP2 VLP stimulation. The median number of cells secreting IFN-γ against HBoV was thereby shown to be slightly lower than the median number of cells secreting IFN-γ against VP2 particles of B19V, which previously have been shown to serve as targets for IFN-γ- and IL-10-mediated CD4+ T helper cell responses [38, 39]. However, this observation was mainly based on 4 study subjects who exhibited high cytokine responses against the B19V VP2 proteins. These single high responses might be explained by possible recent B19V infections or viral restimulation, because the average seroprevalence of B19V in the German adult population is 77%, and, therefore, acute infections may occur in adults [40].
Compared with synthetic peptide controls, slightly elevated IFN-γ responses against B19V VP2 VLPs were observed in seronegative individuals. This finding suggests that minor, unspecific cytokine secretion may be induced in blood cells by means of residual pyrogens (e.g., endotoxin) included in recombinant antigen but not in synthetic peptide preparations [41]. However, HBoV VP2-specific T cell responses were not detected in all individuals studied, because, for many donors, only low or undetectable IFN-γ secretion was observed, suggesting antigen specificity of the detected T cell responses.
In the study group, an age-dependent decrease in HBoV-specific T cell responses was observed. This might be the result of an age-related decrease in and an impairment of the amount and functions of virus-specific T cell populations, because it has been described for other viral infections (e.g., for populations with adenovirus) [42]. Furthermore, it is known that active T cell responses against pathogens undergo confinement to specific memory populations with increasing time after primary infection in the absence of exogenous restimulation events or endogenous reactivations of latent viral infections. Because all currently published data on the epidemiologic profile of HBoV strongly suggest that primary infection occurs in the very early years of childhood [9–17, 20], the time-dependent reduction in the number of virus-specific T cells might be explained by a lack of frequent pathogen contact. This may be considered to provide additional proof of the early time point when HBoV infection occurs during childhood. Independent of age, female subjects had higher numbers of cells secreting IFN-γ than did male subjects, especially among younger individuals; this finding possibly indicates more-frequent spontaneous viral restimulation (e.g., by increased contact with children with acute infection), resulting in an overall increase in the HBoV-specific cellular immune response. This hypothesis is further supported by the fact that the most prominent difference in sex-specific cellular responses was observed in individuals born between 1970 and 1979, an age group in which women presumably have the most frequent contact with small children. However, because no information on the family status of the study subjects is available, these data will have to be confirmed by additional epidemiologic investigations.
Acknowledgments
We thank Tobias Allander and colleagues from the Karolinska Institute (Stockholm, Sweden) for the generous gift of the pCR 4-TOPO vector (Invitrogen), including the genome sequence of human bocavirus ST2. We also thank Klaus Hedman and colleagues at the University of Helsinki for experimental and theoretical support. The excellent technical assistance of Julia Mischner and Richard Klar, as well as the critical proofreading of the manuscript by Valeria Runza, is appreciated.
Footnotes
Potential conflicts of interest: none reported.
Financial support: German Research Foundation (grant Mo620/7-1); Deutscher Akademischer Auslandsdienst (grant PPP-Finland D/04/04483).
References
- 1.Allander T, Tammi MT, Eriksson M, Bjerkner A, Tiveljung-Lindell A, Andersson B. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc Natl Acad Sci USA. 2005;102:12891–6. doi: 10.1073/pnas.0504666102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chieochansin T, Chutinimitkul S, Payungporn S, et al. Complete coding sequences and phylogenetic analysis of Human Bocavirus (HBoV) Virus Res. 2007;129:54–7. doi: 10.1016/j.virusres.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 3.Boschetti N, Wyss K, Mischler A, Hostettler T, Kempf C. Stability of minute virus of mice against temperature and sodium hydroxide. Biologicals. 2003;31:181–5. doi: 10.1016/s1045-1056(03)00037-x. [DOI] [PubMed] [Google Scholar]
- 4.Dorsch S, Liebisch G, Kaufmann B, et al. The VP1 unique region of parvovirus B19 and its constituent phospholipase A2-like activity. J Virol. 2002;76:2014–8. doi: 10.1128/JVI.76.4.2014-2018.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown CS, Van Lent JW, Vlak JM, Spaan WJ. Assembly of empty capsids by using baculovirus recombinants expressing human parvovirus B19 structural proteins. J Virol. 1991;65:2702–6. doi: 10.1128/jvi.65.5.2702-2706.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lowin T, Raab U, Schroeder J, Franssila R, Modrow S. Parvovirus B19 VP2-proteins produced in Saccharomyces cerevisiae: comparison with VP2-particles produced by baculovirus-derived vectors. J Vet Med B Infect Dis Vet Public Health. 2005;52:348–52. doi: 10.1111/j.1439-0450.2005.00871.x. [DOI] [PubMed] [Google Scholar]
- 7.Bastien N, Brandt K, Dust K, Ward D, Li Y. Human Bocavirus infection, Canada. Emerg Infect Dis. 2006;12:848–50. doi: 10.3201/eid1205.051424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan NM, Dove W, Abu-Zeid AF, Shamoon HE, Abd-Eldayem SA, Hart CA. Human bocavirus infection among children, Jordan. Emerg Infect Dis. 2006;12:1418–20. doi: 10.3201/eid1209.060417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kesebir D, Vazquez M, Weibel C, et al. Human bocavirus infection in young children in the United States: molecular epidemiological profile and clinical characteristics of a newly emerging respiratory virus. J Infect Dis. 2006;194:1276–82. doi: 10.1086/508213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma X, Endo R, Ishiguro N, et al. Detection of human bocavirus in Japanese children with lower respiratory tract infections. J Clin Microbiol. 2006;44:1132–4. doi: 10.1128/JCM.44.3.1132-1134.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sloots TP, McErlean P, Speicher DJ, Arden KE, Nissen MD, Mackay IM. Evidence of human coronavirus HKU1 and human bocavirus in Australian children. J Clin Virol. 2006;35:99–102. doi: 10.1016/j.jcv.2005.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kleines M, Scheithauer S, Rackowitz A, Ritter K, Häusler M. High prevalence of human bocavirus detected in young children with severe acute lower respiratory tract disease by use of a standard PCR protocol and a novel real-time PCR protocol. J Clin Microbiol. 2007;45:1032–4. doi: 10.1128/JCM.01884-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maggi F, Andreoli E, Pifferi M, Meschi S, Rocchi J, Bendinelli M. Human bocavirus in Italian patients with respiratory diseases. J Clin Virol. 2007;38:321–5. doi: 10.1016/j.jcv.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Naghipour M, Cuevas LE, Bakhshinejad T, Dove W, Hart CA. Human bocavirus in Iranian children with acute respiratory infections. J Med Virol. 2007;79:539–43. doi: 10.1002/jmv.20815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qu XW, Duan ZJ, Qi ZY. Human bocavirus infection, People's Republic of China. Emerg Infect Dis. 2007;13:165–8. doi: 10.3201/eid1301.060824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vicente D, Cilla G, Montes M, Pérez-Yarza EG, Pérez-Trallero E. Human bocavirus, a respiratory and enteric virus. Emerg Infect Dis. 2007;13:636–7. doi: 10.3201/eid1304.061501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arden KE, McErlean P, Nissen MD, Sloots TP, Mackay IM. Frequent detection of human rhinoviruses, paramyxoviruses, coronaviruses, and bocavirus during acute respiratory tract infections. J Med Virol. 2006;78:1232–40. doi: 10.1002/jmv.20689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kupfer B, Vehreschild J, Cornely O, et al. Severe pneumonia and human bocavirus in adult. Emerg Infect Dis. 2006;12:1614–6. doi: 10.3201/eid1210.060520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manning A, Russell V, Eastick K, et al. Epidemiological profile and clinical associations of human bocavirus and other human parvoviruses. J Infect Dis. 2006;194:1283–90. doi: 10.1086/508219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Endo R, Ishiguro N, Kikuta H, et al. Seroepidemiology of human bocavirus in Hokkaido prefecture, Japan. J Clin Microbiol. 2007;45:3218–23. doi: 10.1128/JCM.02140-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manaresi E, Gallinella G, Zerbini M, Venturoli S, Gentilomi G, Musiani M. IgG immune response to B19 parvovirus VP1 and VP2 linear epitopes by immunoblot assay. J Med Virol. 1999;57:174–8. [PubMed] [Google Scholar]
- 22.Franssila R, Hokynar K, Hedman K. T helper cell-mediated in vitro responses of recently and remotely infected subjects to a candidate recombinant vaccine for human parvovirus B19. J Infect Dis. 2001;183:805–9. doi: 10.1086/318819. [DOI] [PubMed] [Google Scholar]
- 23.Corcoran A, Mahon BP, Doyle S. B cell memory is directed toward conformational epitopes of parvovirus B19 capsid proteins and the unique region of VP1. J Infect Dis. 2004;189:1873–80. doi: 10.1086/382963. [DOI] [PubMed] [Google Scholar]
- 24.Lindner J, Barabas S, Saar K, et al. CD4+ T-cell responses against the VP1-unique region in individuals with recent and persistent parvovirus B19 infection. J Vet Med B Infect Dis Vet Public Health. 2005;52:356–61. doi: 10.1111/j.1439-0450.2005.00860.x. [DOI] [PubMed] [Google Scholar]
- 25.Kaufmann B, Baxa U, Chipman PR, Rossmann MG, Modrow S, Seckler R. Parvovirus B19 does not bind to membrane-associated globoside in vitro. Virology. 2005;332:189–98. doi: 10.1016/j.virol.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 26.Wild J, Bojak A, Deml L, Wagner R. Influence of polypeptide size and intracellular sorting on the induction of epitope-specific CTL responses by DNA vaccines in a mouse model. Vaccine. 2004;22:1732–43. doi: 10.1016/j.vaccine.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 27.Kantola K, Hedman L, Allander T, et al. Serodiagnosis of human bocavirus infections. Clin Infect Dis. 2008;46:540–6. doi: 10.1086/526532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindner J, Karalar L, Zehentmeier S, et al. Humoral immune response against human bocavirus VP2 virus-like particles. Viral Immunol. 2008 doi: 10.1089/vim.2008.0045. (in press) [DOI] [PubMed] [Google Scholar]
- 29.Lindner J, Modrow S. Human bocavirus—a novel parvovirus to infect humans. Intervirology. 2008;51:116–22. doi: 10.1159/000137411. [DOI] [PubMed] [Google Scholar]
- 30.Hurtado A, Rueda P, Nowicky J, Sarraseca J, Casal JI. Identification of domains in canine parvovirus VP2 essential for the assembly of virus-like particles. J Virol. 1996;70:5422–9. doi: 10.1128/jvi.70.8.5422-5429.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maranga L, Brazão TF, Carrondo MJ. Virus-like particle production at low multiplicities of infection with the baculovirus insect cell system. Biotechnol Bioeng. 2003;84:245–53. doi: 10.1002/bit.10773. [DOI] [PubMed] [Google Scholar]
- 32.Brieu N, Gay B, Segondy M, Foulongne V. Electron microscopy observation of human bocavirus (HBoV) in nasopharyngeal samples from HBoV-infected children. J Clin Microbiol. 2007;45:3419–20. doi: 10.1128/JCM.00545-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saliki JT, Mizak B, Flore HP, et al. Canine parvovirus empty capsids produced by expression in a baculovirus vector: use in analysis of viral properties and immunization of dogs. J Gen Virol. 1992;73:369–74. doi: 10.1099/0022-1317-73-2-369. [DOI] [PubMed] [Google Scholar]
- 34.Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against high-grade vulval and vaginal lesions: a combined analysis of three randomised clinical trials. Lancet. 2007;369:1693–1702. doi: 10.1016/S0140-6736(07)60777-6. [DOI] [PubMed] [Google Scholar]
- 35.Shouval D, Hepatitis B vaccines. J Hepatol. 2003;39:S70–6. doi: 10.1016/s0168-8278(03)00152-1. [DOI] [PubMed] [Google Scholar]
- 36.Soderlund M, Brown CS, Spaan WJ, Hedman L, Hedman K. Epitope type-specific IgG responses to capsid proteins VP1 and VP2 of human parvovirus B19. J Infect Dis. 1995;172:1431–6. doi: 10.1093/infdis/172.6.1431. [DOI] [PubMed] [Google Scholar]
- 37.Lindner J, Karalar L, Schimanski S, Pfister H, Struff W, Modrow S. Clinical and epidemiological aspects of human bocavirus infection. J Clin Virol. 2008 doi: 10.1016/j.jcv.2008.08.009. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Franssila R, Hedman K. T-helper cell-mediated interferon-γ, interleukin-10 and proliferation responses to a candidate recombinant vaccine for human parvovirus B19. Vaccine. 2004;22:3809–15. doi: 10.1016/j.vaccine.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 39.Franssila R, Auramo J, Modrow S, et al. T helper cell-mediated interferon-gamma expression after human parvovirus B19 infection: persisting VP2-specific and transient VP1u-specific activity. Clin Exp Immunol. 2005;142:53–61. doi: 10.1111/j.1365-2249.2005.02886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eis-Hübinger AM, Oldenburg J, Brackmann HH, Matz B, Schneweis KE. The prevalence of antibody to parvovirus B19 in hemophiliacs and in the general population. Zentralbl Bakteriol. 1996;284:232–40. doi: 10.1016/s0934-8840(96)80098-3. [DOI] [PubMed] [Google Scholar]
- 41.Ulmer AJ, Flad H, Rietschel T, Mattern T. Induction of proliferation and cytokine production in human T lymphocytes by lipopolysaccharide (LPS) Toxicology. 2000;152:37–45. doi: 10.1016/s0300-483x(00)00290-0. [DOI] [PubMed] [Google Scholar]
- 42.Sester M, Sester U, Alarcon SS, et al. Age-related decrease in adenovirus-specific T cell responses. J Infect Dis. 2002;185:1379–87. doi: 10.1086/340502. [DOI] [PubMed] [Google Scholar]