Abstract
Objective:
Surgical smoke generated during electrocautery contains toxins which may cause adverse health effects to operating room (OR) personnel. The objective of this study was to investigate the performance of surgical masks (SMs), which are routinely used in ORs, more efficient N95 surgical mask respirator (SMRs) and N100 filtering facepiece respirator (FFRs), against surgical smoke.
Methods:
Ten subjects were recruited to perform surgical dissections on animal tissue in a simulated OR chamber, using a standard electrocautery device, generating surgical smoke. Six respiratory protective devices (RPDs) were tested: two SMs, two SMRs, and two N100 FFRs [including a newly developed faceseal (FS) prototype]. Fit testing was conducted before the experiment. Each subject was then exposed to the surgical smoke while wearing an RPD under the tests. Concentrations inside (Cin) and outside (Cout) of the RPD were measured by a particle size spectrometer. The simulated workplace protection factor (SWPF) was determined by the ratio of Cout and Cin for each RPD-wearing subject.
Results:
For the SMs, the geometric means of SWPFtotal (based on the total aerosol concentration) were 1.49 and 1.76, indicating minimal protection. The SWPFtotal values of the SMRs and N100 FFRs were significantly higher than those of the SMs: for the two SMRs, the SWPFtotal were 208 and 263; for the two N100s, the SWPFtotal values were 1,089 and 2,199. No significant difference was observed between either the two SMs or the two SMRs. The SWPFtotal for the novel FS prototype N100 FFR was significantly higher than the conventional N100 FFR. The correlation between SWPFtotal and fit factor (FF) determined for two N95 SMRs was not significant.
Conclusions:
SMs do not provide measurable protection against surgical smoke. SMRs offer considerably improved protection versus SMs, while the N100 FFRs showed significant improvement over the SMRs. The FS prototype offered a higher level of protection than the standard N100 FFR, due to a tighter seal. While we acknowledge that conventional N100 FFRs (equipped with exhalation valves) are not practical for human OR use, the results obtained with the FS prototype demonstrate the potential of the new FS technology for implementation on various types of respirators.
Keywords: filtering facepiece respirators, simulated workplace protection factor, surgical mask, surgical smoke
INTRODUCTION
Surgical smoke is an aerosol hazard unique to the surgical operating room (OR). It is generated by electrocautery used in virtually all standard surgical facilities as a means of performing surgical dissection of various tissues. Electrocautery is a process in which an electrical current is passed through a resistant metal wire electrode. The heated electrode is then applied to the tissue for dissection or hemostasis (Pollock et al., 2008). Given the positioning of surgical personnel over and around the surgical patient, surgical smoke is often directly in the path of their respiratory field. The Occupational Safety and Health Administration (OSHA) estimates that 500,000 workers are exposed to laser and electrocautery smoke each year (OSHA, 2007).
There have been significant concerns about exposure to surgical smoke, and about the adequacy of standard surgical masks (SMs) to protect personnel in the OR. Surgical smoke contains known carcinogens as well as viable biologic particles (Barrett and Garber, 2003). Carcinogenic and neurotoxic compounds were found in surgical smoke aerosols generated from porcine tissue as well as during human surgical procedures (Krones et al., 2007; Sahaf et al., 2007). A review by Biggins and Renfree (2002) reported the failure of SMs to provide appropriate protection to healthcare personnel and suggested establishing new standards to reduce the risks. Other studies have revealed that SMs are insufficient for providing adequate protection against surgical smoke (Barrett and Garber, 2003; Alp et al., 2006).
Exposure to surgical smoke aerosol has relevance to public health settings due to the presence of small particles. Weber et al. (1993) tested eight SMs and found that for fine particles (<1,000nm) the penetration through these masks ranged from 20% to nearly 100%. Studies conducted with two SMs sealed on a manikin headform indicated that for particles of 10–80nm in diameter (including MS2 virions), the filter penetration was 20.5–84.5% (Balazy et al., 2006a, b). Since SMs have a comparatively poor fit, faceseal (FS) leakage represents a prominent penetration pathway. This is especially true for small particles, e.g. those in the size range of influenza A virions (Booth et al., 2013) as well as virions causing Human Papilloma Virus (HPV), Severe Acute Respiratory Syndrome (SARS), and Middle East Respiratory Syndrome (MERS). Although N95 filtering facepiece respirators (FFRs) are more efficient than SMs [their N95 filter is certified by the National Institute of Occupational Safety and Health (NIOSH) to allow no more than 5% penetration], penetration of ultrafine particles (<100nm) through some N95 FFRs may exceed this threshold (Balazy et al., 2006a). The highest filter penetration values were observed for particles of 30–70nm in diameter, which includes the size of several respiratory pathogenic virions (Zheng and Baker, 2006; Mettenleiter and Sobrino, 2008), as well as a substantial fraction of surgical smoke particles (Bruske-Hohlfeld et al., 2008; Andreasson et al., 2009).
NIOSH recommends combining general room ventilation with local exhaust ventilation (LEV) to control the airborne particles generated by surgical smoke (NIOSH, 1996). However, due to the variability of surgical smoke and its potential hazards, the implementation of personal protective equipment (PPE) is also needed to protect healthcare workers in ORs. The Association for periOperative Registered Nurses (AORN) recognizes the hazard of the surgical smoke. AORN also urges the use of PPE and evacuation and filtration of smoke through an appropriate system (AORN, 2016a,b,c). They recommend using fit-tested surgical N95 FFRs or high-filtration masks to protect against surgical smoke (AORN, 2008; Benson et al., 2013). However these recommendations are not regulatory requirements, and presently the use of N95 FFRs in ORs is primarily limited to procedures involving HPV. Overall, SMs remains the standard protection devices in ORs. Recently, so-called ‘N95 surgical mask respirators’ (SMRs) have been introduced. The SMRs are cleared by the Food and Drug Administration (FDA) for use in ORs, and certified by NIOSH to receive an N95 grade (although the NIOSH does not evaluate FFRs for surgical use). However, little is known about the performance of either SMs or SMRs against surgical smoke. Rozzi et al. (2012) investigated the absorption capabilities of organic vapor FFRs against the aromatic hydrocarbons generated in surgical smoke, but neither this nor similar investigations addressed the particulate matter component. A higher grade FFR (N100) was pilot-studied against surgical smoke from porcine tissue (Koehler et al., 2014). One of these facepieces was modified by creating a FS made of ethylene vinyl acetate foam that was affixed to the inner perimeter of the respirator, replacing the stock face seal. The modification significantly improved the respirator performance by minimizing the FS leakage. It is acknowledged that N100 FFRs have limitations for deployment in ORs due to their exhalation valve component. However, it is still important to generate data about the efficiency of these highest grade facepieces against surgical smoke because it will help determine the feasibility of making appropriate design modifications to other respirators, e.g. N95 SMRs (that have no exhalation valves), in order to maximize their performance.
The protection provided by a respirator at a workplace is typically assessed by determining its workplace protection factor (WPF) measured under specific conditions. One way to quantify the WPF is through the simulated workplace protection factor (SWPF). SWPF is measured in a controlled laboratory setting while the wearer performs exercises mimicking the actual work procedures.
The purpose of our study was to determine the SWPFs against surgical smoke for two SMs and two N95 SMRs (both currently approved for OR use), as well as for a conventional and newly developed N100 FFR.
MATERIALS AND METHODS
Respirator selection
Commercially available SMs (Model 1800NL, 3M, St. Paul, MN, and Model 14683, Kimberly Clark, Neenah, WI, USA) and N95 FFRs marketed as SMRs (Model 1860 and Model 1870, 3M, St. Paul, MN, USA) were selected for this study. The above devices were labeled as SM1, SM2, N95 SMR1, and N95 SMR2, respectively. The SM1 and SM2 were originally designed to reduce the contamination of others in the wearer’s surrounding to airborne pathogens that he/she may aerosolize during exhalation; SMs are also used to reduce the potential exposure of the wearer to blood and body fluids. The N95 SMR1 and N95 SMR2 are intended to be deployed during laser surgery, electrocautery and other procedures which utilize powered medical instruments. All four selected SMs and SMRs (see Table 1) are equipped with a malleable metallic nosepiece to form the bridge of the nose.
Table 1.
RPDs selected for the study
| ID | Company | Model number | Size |
|---|---|---|---|
| SM1 | 3M | 1800NL | Regular |
| SM2 | KC | 14683 | Regular |
| N95 SMR1 | 3M | 1860 | Regular, small |
| N95 SMR2 | 3M | 1870 | Regular |
| Control N100 | 3M | 8233 | Regular |
| FS Prototype N100 | 3M (modified) | 8233 | Regular |
Additionally, two higher-grade FFRs were evaluated in this study. One was an original commercially available N100 FFR (Model 8233, 3M, St. Paul, MN, USA); the other was the same FFR modified with a novel FS, labeled as FS Prototype N100 (Koehler et al., 2014). The model of the selected N100 FFR was also shown in Table 1.
Challenge aerosol
The surgical smoke was generated by electrocautery dissection of porcine muscle tissue, as described previously by several investigators (Hensman et al., 1998; Weld et al., 2007). A standard electrosurgical generator was used as the energy source for the cautery procedures (Valleylab Force FX, Covidien, Boulder, CO, USA). Electrocautery dissection was performed utilizing a standard electrosurgical pencil (Valleylab E2516, Covidien, Boulder, CO, USA) at a setting of 40 watts for both cutting and coagulation, using a blend mode.
Human subject selection
Ten human subjects representing healthcare workers were recruited for this study: five adult males and five adult females. All of the subjects except one experienced surgeon were recruited from research staff and students of the University of Cincinnati’s College of Medicine. The subjects were notified about the potential hazard of surgical smoke exposure before conducting the experiment and were provided with a written consent to participate. The research protocol was approved by the University of Cincinnati Institutional Review Board (IRB). Before the experiment, each subject completed the OSHA respirator medical clearance questionnaire administered by the University Occupational Pulmonary Program.
Fit testing
Prior to evaluating the respirator/mask performance in the exposure chamber with surgical smoke, the subjects underwent fit testing while wearing the two N95 SMRs and two N100 FFRs according to the OSHA fit testing protocol (OSHA 29 CFR 1910.134). An SM is not subject for the OSHA fit testing. After the fit testing, the subjects were introduced into the chamber for the SWPF study immediately.
Sodium chloride (NaCl) particles were generated using a particle generator (Model 8026, TSI Inc., Shoreview, MN, USA) to create a sufficient ambient concentration to obtain measurable protection factors with highly efficient respirators. The overall fit factor (FF) was measured and recorded by the PortaCount Plus (Model 8020, TSI Inc., Shoreview, MN, USA) operating with an N95-Companion (Model 8095, TSI Inc., Shoreview, MN, USA). The FF is calculated as the aerosol concentration outside of the respirator divided by its concentration inside of the respirator when a subject is performing a specific set of procedures (OSHA29 CFR 1910.134). The passing criterion of FF is 100.
Experimental setup
The experimental setup is presented in Fig. 1. While inside the exposure chamber (volume = 3.6×2.4×2.6 m3), a subject wearing a tested respirator or SM under the test performed electrocautery dissection on a section of animal muscle tissue located on a surgical table mimicking a conventional surgical procedure. Each of the 10 subjects wore each of the 6 tested RPDs in a random order. The height of the surgical table was approximately 1 m above the ground, a typical height in ORs. The choice of the surgical equipment utilized, the distance from the cautery to the test subject, and the cautery settings, were all determined by an experienced board-certified surgeon with over 10,000h of surgical electrocautery experience. The subjects were trained in the techniques of electrocautery dissection by the same surgeon, who was also a subject in the study.
Figure 1.
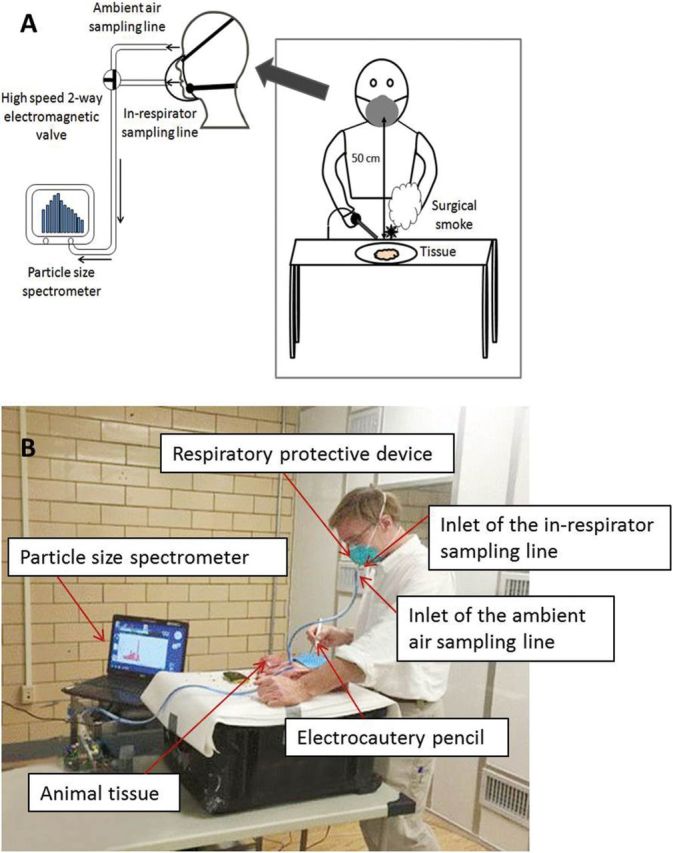
Experimental setup.
The surgical smoke aerosol generated during this procedure was sampled in the breathing zone directly outside the respirator/mask (representing the inhalation exposure of an unprotected individual) as well as inside the respirator/mask (representing the inhalation exposure of a wearer). The inrespirator sampling line was connected to the probe located inside the respirator; the ambient air sampling line was connected to the probe located at the breathing zone (Fig. 1B). The inlets of the two respective sampling lines were located 6cm from each other. The same sampling configuration was used in fit testing. The aerosol concentrations and particle size distributions of the inside- and outside-sampled aerosol (Cin and Cout respectively) were measured by a particle size spectrometer (Nanoparticle Aerosol Monitor/Mini Wide Range Aerosol Spectrometer, Model 1320, Grimm Technologies, Inc., Ainring, Germany) in combination with an optical particle counter (OPC) (Model 1.108, Grimm Technologies, Inc.). The inside and outside concentration measurements were controlled by a high speed two-way electromagnetic valve. The outside concentration was measured for 6min following by a 12-min inside measurement; subsequently, the outside concentration was measured again for 6min. The average concentration of the two 6-min outside concentration measurements was calculated and recorded as Cout. The average concentration of the continuous 12-min inside concentration measurement was calculated and recorded as Cin. The SWPF was determined as Cout/Cin. The data were recorded in a particle size range of 25–1,150nm. Based on the total aerosol concentrations measured across this size range, the total protection factor (SWPFtotal) was calculated. Additionally, the particle size selectivity of the aerosol measurement allowed determining SWPFs for different particle sizes (SWPFdp). These were recorded within a narrower range of 25–290nm because the particle concentrations inside of the tested N95 and N100 FFRs were almost zero for particles larger than 290nm. The corresponding mean sizes for the 10 selected channels were 25, 35, 45, 60, 85, 115, 145, 180, 265, and 290nm.
During the smoke generation process, the exposure chamber was ventilated using a preinstalled ventilation and high-efficiency particulate air (HEPA) filtration system operating at an air exchange rate of five Air Exchanges per hour (AEH). The modern OR facilities operate at least at 20 AEH of which 4 AEH comes from the ambient air (Facility Guidelines Institute, 2014). At the same time, some ORs operate at lower air exchange rates. We have intentionally chosen a relatively low exchange rate to establish the most conservative assessment with the highest feasible concentration level of smoke particles.
Data analysis
The data analysis was performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA). For each respiratory protective device (RPD), geometric mean (GM) and geometric standard deviation (GSD) of SWPF were calculated. The statistical analyses were applied after performing a log-transformation of the data. Paired t-test was used to test the difference between different RPDs. Two-way ANOVA was deployed to evaluate the effects of subjects and particle sizes on the size-selective SWPFs. P values below 0.05 represented a significant difference.
RESULTS AND DISCUSSION
Concentration and particle size distribution of the surgical smoke in the breathing zone
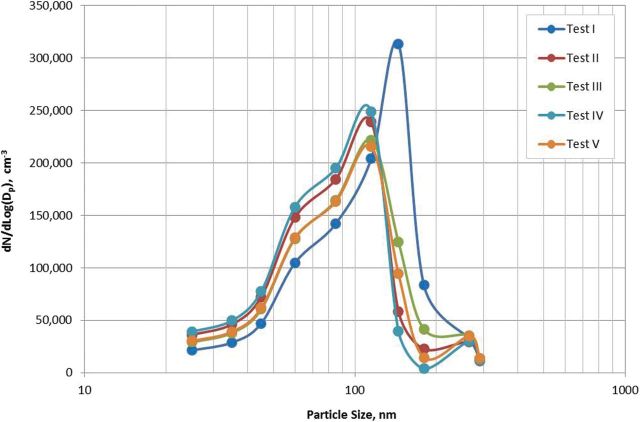
The total aerosol particle concentration measured in the breathing zone of the experienced surgeon who was exposed to the surgical smoke level ranged from 0.708×106 to 1.080×106 particles cm−3 (mean = 0.946×106 particles cm−3 and SD = 0.111×106), which was around 1,000 times higher than the background level. At the same time, the size-specific concentration levels were substantially below the upper threshold limits of the aerosol instrument. The particle size distributions generated in five experiments (Tests I through V) are presented in Fig. 2. The curves have a similar shape; four of them peak at a particle size of 115nm observed and one at 145nm. The tests with other subjects generally generated similar particle size distribution curves although the total particle concentration levels were lower, which can be attributed to their limited experience in operating the electrocautery equipment. It was noticed that some subjects did not apply the electrocautery pencil to the tissue as frequently as it was demonstrated by surgeon, which could produce a lower level of smoke. With regard to the above between-subject variability and other factors influencing the aerosol concentration and particle size distribution in the breathing zone, it should be acknowledged that in an actual operating setting, electrocautery use in different surgical procedures involving various tissues would likewise have an effect on the concentration and particle size distribution of the generated surgical smoke.
Figure 2.
Particle size distribution of surgical smoke measured in the breathing zone of the board-certified surgeon (the most experienced subject).
The surgical smoke particle concentration measured in this study was relatively high compared to the levels found by Hohlfeld et al. (2008). One explanation for the difference may be that the measurements were conducted during different surgical procedures utilizing different aerosol instruments (Hohlfeld et al. used a condensation particle counter). Additionally, the higher concentration measured in the present study may be attributed to lower air exchange rate established in our chamber. It is also noted that in the quoted study the aerosol sampling was performed at the side of the anesthetist, rather than directly in front of the surgeon’s mask, as in our OR setup. This greater distance from the surgeon’s breathing zone may explain their findings of lower particle concentrations. While acknowledging the above differences, it is recognized that the ambient aerosol concentration level does not affect the outcome of this effort because SWPF is a non-dimensional parameter.
Simulated workplace protection factor (SWPFtotal)
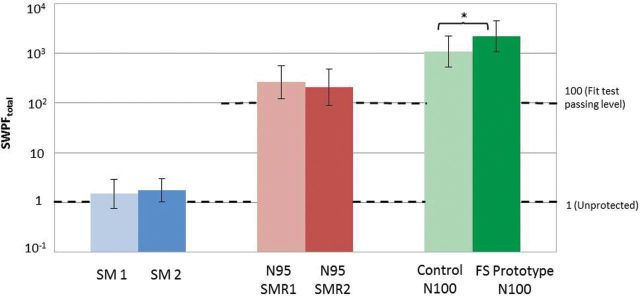
Figure 3 presents the values of SWPFtotal for the six tested RPDs. The SWPFtotal values for SM1 and SM2 were close to 1 with GM = 1.49, GSD = 1.95 (SM1), and GM = 1.76, GSD = 1.71 (SM2), indicating essentially no protection. The difference in SWPFtotal between SM1 and SM2 was not significant (P > 0.05, Table 2). Some particle size-selective SWPF values obtained for SMs were actually below 1, indicating that the aerosol concentrations inside the SMs were higher than outside. This counter-intuitive finding can be attributed to the fact that the same aerosol instrument was deployed alternating between the inside and outside measurements, which were conducted at different time points introducing an uncertainty, which affects the SWPF. The uncertainty is particularly apparent when the SWPF is close to 1. Overall, a very low efficiency of SMs observed in this study is consistent with previous reports (Dixon and Nelson, 1984; Zhuang et al., 2003; Reponen et al., 2011).
Figure 3.
SWPFtotal for commercially available SMs and N95 SMRs widely used in ORs as well as for the new FS prototype N100 and a conventional N100 FFR (control). Asterisk denotes statistically significant difference (P < 0.05). Note: SM and N95 SMR data represent the GMs of 10 subjects (n = 10) while the FS Prototype N100 and Control N100 data represent the GMs of nine subjects (n = 9) since one subject did not wear the N100 FFRs appropriately.
Table 2.
Results paired t-test comparing SWPFtotal between the tested protective devices
| RPDs compared | Number of subjects | P value |
|---|---|---|
| SM1 and SM2 | 10 | 0.84 |
| N95 SMR1 and N95 SMR2 | 10 | 0.41 |
| FS Prototype N100 and Control N100 | 9 | 0.04* |
| SMs and N95 SMRs | 10 | 0.0013** |
| SMs and N100 FFRs (FS Prototype N100 + Control N100) | 9 | 0.0009** |
| N95 SMRs and N100 FFRs (FS Prototype N100 + Control N100) | 9 | 0.0022** |
*P < 0.05, **P < 0.01.
The SWPFtotal of both N95 SMRs were significantly higher than the values of SMs (P < 0.01, Table 2). Both N95 SMRs offered a measurable level of protection: GM = 263, GSD = 2.17, and GM = 208, GSD = 2.31, respectively. Their SWPFtotal values exceeded 100 (the fit test passing level) and, by far, exceeded 10 (the OSHA’s assigned protection factor). It is noted that the protection factors offered by these N95 respirators are higher than the minimum requirement for their filter material alone. The difference between SWPFtotal values obtained for the two N95 SMRs was not significant (P > 0.05, Table 2).
The two N100 FFRs demonstrated significantly—about an order of magnitude—higher protection compared to N95 SMRs (P < 0.01, see Table 2): GM = 1,089 and GSD = 2.08 for the control N100 FFR and GM = 2,199 and GSD = 2.05 for the FS Prototype N100 FFR. The difference between SWPFtotal values obtained for the two N100 FFRs was also significant (P < 0.05, Table 2). Thus, the modified FS component of the N100 FFR (FS Prototype N100 FFR) was capable of significantly improving the protection provided by a highly efficient N100 FFR. Since the N100 FFR’s design modification was concerned exclusively with the peripheral area, the difference in SWPFtotal can be attributed solely to the improved fit of the respirator to the user’s face.
In summary, the SWPFtotal results suggest that, in contrast to the NIOSH certified respiratory protection devices such as N95 and N100, SMs could not protect healthcare workers against surgical smoke in ORs. It is acknowledged though that while SMs are widely used in healthcare environments, they were not originally designed to reduce the wearer’s exposure to aerosols. While we recognize that conventional N100 FFRs (equipped with exhalation valves) are not practical for human OR use, the data obtained with the FS prototype demonstrate the potential of the new FS technology for implementation on various types of respirators.
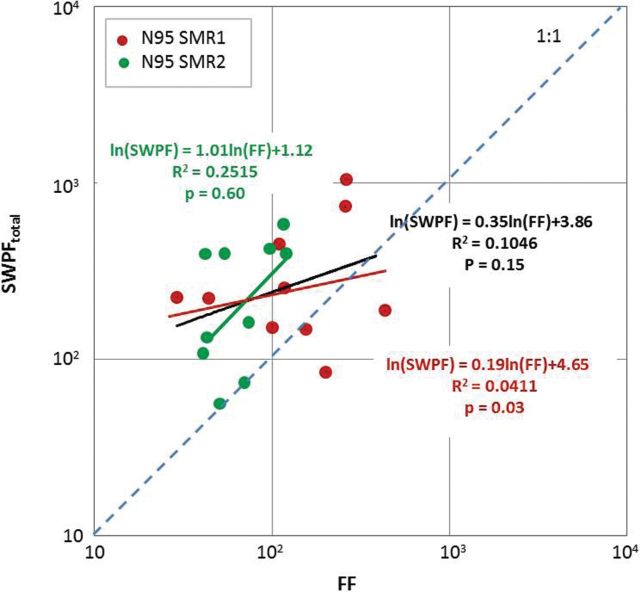
Correlation between SWPFtotal and FF determined for N95 SMRs
Two out of 10 subjects (20%) did not pass the fit test with SMR1, and 8 out of 10 (80%) did not pass it with SMR2 (FF < 100). In three cases out of 20 (15%), the SWPFtotal was below 100 (including two cases in which the subjects failed the fit test). The relationship between SWPFtotal and FF is presented in Fig. 4. None of the correlations (either for SMR1, or for SMR2, or for both data sets combined) were significant (P > 0.05). The slopes of log(SWPFtotal) against log(FF) were as follows: 0.19 for SMR1, 1.01 for SMR2, and 0.35 for the two combined; all had rather low coefficient of correlation R2.
Figure 4.
Correlation between SWPFtotal and the FF for 10 subjects wearing N95 SMRs: the lines in red and green are the regression lines fit for the corresponding data points (SMR1 and SMR2, respectively); the line in black is the regression line fit for all the data points (red and green combined).
All 10 subjects wearing SMR2, and 7 out of 10 subjects wearing SMR1 produced data points above the 1:1 line, indicating that the SWPF exceeded the corresponding FF in the majority of the tests. This suggests that while no significant correlation was found between the two factors, the FF can serve as a conservative estimate of the SWPF.
The relationship between FF and SWPFtotal obtained in this study confirms the observations of Zhuang et al., who conducted fit testing on 15 workers and then assigned them, with the same respirators, to their routine jobs while measuring the WPFs. The investigators reported lack of correlation between FF and WPF for FFs ≥ 500 (P > 0.05) (Dixon and Nelson, 1984). One reason may be that the OSHA fit testing protocol requires very specific body movements, which may not fully represent actual workplace activities. Likewise, the breathing rates may be different when a worker performs fit testing versus when he/she conducts the workplace activities.
Particle size specific simulated workplace protection factor (SWPFdp)
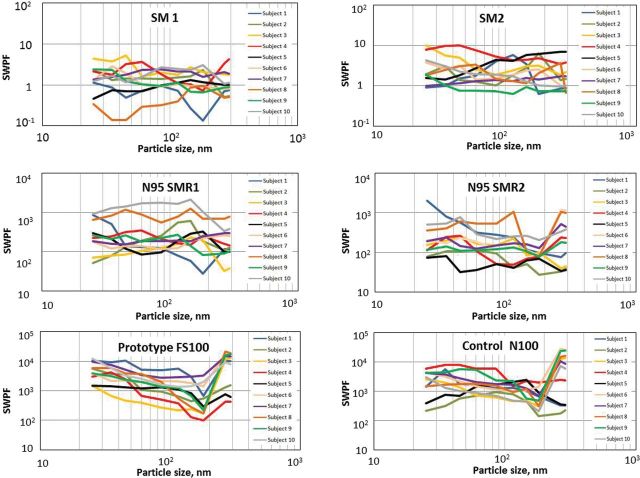
The protection factors offered by the six tested RPDs worn on 10 subjects are plotted in Fig. 5 against the particle sizes. Each curve represents the SWPFdp data obtained for a subject wearing a specific RPD. A clear trend representing the effect of particle size was observed only on the two N100 FFRs. Statistical analysis shows that between-subject variability was a strongly significant factor affecting their SWPFdp (P < 0.01), indicating the SWPFdp varies significantly depending on the subject regardless of the type of RPDs (see Table 3).
Figure 5.
Particle size selective SWPFs.
Table 3.
Effects of subject and particle size on the performance of RPDs (two-way ANOVA)
| Protection device | Factor | P value |
|---|---|---|
| SM1 | Subject | <0.0001** |
| Size | 0.822 | |
| SM2 | Subject | <0.0001** |
| Size | 0.384 | |
| N95 SMR1 | Subject | <0.0001** |
| Size | 0.170 | |
| N95 SMR2 | Subject | <0.0001** |
| Size | 0.129 | |
| FS Prototype N100 | Subject | <0.0001** |
| Size | <0.0001** | |
| Control N100 FFR | Subject | 0.004** |
| Size | <0.0001** |
**P < 0.01.
If the dominant particle penetration pathway was a filter, the SWPF would be dependent on the particle size since the filter penetration is generally size-dependent (Kulkarni et al., 2011). Electret filters used in high-efficiency respirators offer very high protection against very small particles (20–30nm) as well as against much larger particles (>200nm) leaving the room for the most penetrating particle size (MPPS) in-between; the exact MPPS value depends on the filter characteristics and face velocity. This is consistent with the SWPF data shown for FS100 and N100 FFRs for which the particle size had a significant effect, indicating that an appreciable percentage of particles measured inside the respirator penetrated through the filter (relative to penetration through the FS leakage). In contrast, if the FS leakage served as the major penetration pathway, the penetration may not be significantly affected by the particle size, at least for the essentially inertialess surgical smoke particles. Thus, the data suggest that most of the particles, which penetrated through an SM or an N95 SMR, utilize the FS leakage pathway.
Finally, although the present investigation specifically addressed surgical smoke, as was noted earlier, the particle sizes involved are in the same range as virions causing influenza, HPV, SARS, and MERS (Rota et al., 2003; Zheng and Baker, 2006; Zaki et al., 2012). Since the RPDs studied here are frequently incorporated for public health use, the findings herein may have application to various public health scenarios, e.g. those involving infectious aerosols.
CONCLUSIONS
Our study results strongly suggest that SMs do not provide measurable protection to OR workers against surgical smoke. More efficient N95 SMRs are capable of reducing the inhalation exposure to surgical smoke by over two orders of magnitude (SWPFtotal = 208–263). Given the fact that the particle size was not a significant factor affecting the performance of SMs and SMRs, we concluded that the FS leakage was the main penetration pathway for the surgical smoke particles to enter into the tested SMs and the N95 SMRs.
The N100 FFRs, both the control and FS Prototype versions, offered the highest protection against surgical smoke (SWPFtotal = 1,089–2,199). In contrast to SMs and the N95 SMRs, the particle size was a significant factor affecting the performance of these N100 FFRs, which suggest that the filter penetration pathway likely dominated over the FS leakage component.
The SWPFtotal obtained for the newly developed FS Prototype N100 FFR significantly exceeded that of the control N100 FFR, the difference being due to the improved fit of the FFR to the user’s face. This finding may have relevance to the design of N95 SMRs, as well as other RPDs, since FS leakage was the predominant pathway of smoke particle penetration in the SMRs we tested. If the improvements demonstrated herein on the N100 FFRs are achievable on N95 SMRs, it would represent an important advance in the design of RPDs for OR personnel.
FUNDING
This study was supported by the National Institute for Occupational Safety and Health Pilot Research Project Training Program of the University of Cincin nati Education and Research Center Grant #T42/OH008432-09. Additional funding was received through the University Environmental Health Foundation.
ACKNOWLEDGEMENTS
The authors declare no conflict of interest. The content of the paper, including any opinions and/or conclusions expressed, are solely those of the authors.
REFERENCES
- Alp E, Bijl D, Bleichrodt RP, et al. (1993) Surgical smoke and infection control. J Hosp Infect; 2006; 62:1–5. [DOI] [PubMed] [Google Scholar]
- Andreasson SN, Anundi H, Sahlberg B, et al. (2009) Peritonectomy with high voltage electrocautery generates higher levels of ultrafine smoke particles. J Cancer Surgery; 35: 780–84. [DOI] [PubMed] [Google Scholar]
- AORN. (2016. a) Guideline for care electrosurgery. In Guidelines for perioperative practice. Denver, CO: AORN; pp. 119–135. [Google Scholar]
- AORN. (2016. b) Guideline for laser safety. In Guidelines for perioperative practice. Denver, CO: AORN; pp. 137–150. [Google Scholar]
- AORN. (2016. c) Guideline for minimally invasive surgery. In Guidelines for perioperative practice. Denver, CO: AORN; pp. 589–616. [Google Scholar]
- Balazy A, Toivola M, Reponen T, et al. (2006. a) Manikin-based performance evaluation of N95 filtering-facepiece respirators challenged with nanoparticles. Ann Occup Hyg; 50: 259–69. [DOI] [PubMed] [Google Scholar]
- Bałazy A, Toivola M, Adhikari A, et al. (2006. b) Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control; 34: 51–7. [DOI] [PubMed] [Google Scholar]
- Barrett WL, Garber SM. (2003) Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc; 17: 979–87. [DOI] [PubMed] [Google Scholar]
- Benson SM, Novak DA, Ogg MJ. (2013) Proper use of surgical N95 respirators and surgical masks in the OR. AORN J; 97: 457–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggins J, Renfree S. (2002) The hazards of surgical smoke. Not to be sniffed at! Br J Perioper Nurs; 12: 136–8. [DOI] [PubMed] [Google Scholar]
- Bruske-Hohlfeld I, Preissler G, Jauch KW, et al. (2008) Surgical smoke and ultrafine particles. J Occup Med Tox; 3: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth CM, Clayton M, Crook B, et al. (2013) Effectiveness of surgical masks against influenza bioaerosols. J Hosp Infect; 82: 22–6. [DOI] [PubMed] [Google Scholar]
- Dixon SW, Nelson TJ. (1984) Workplace protection factors for negative pressure half-mask facepiece respirator. J Int Soc Resp Prot; 2: 347–61. [Google Scholar]
- Facility Guidelines Institute, Guidelines for Design and Construction of Hospitals and Outpatient Facilities (2014) US Department of Health and Human Services, American Society for Healthcare Engineering; Chicago, IL. [Google Scholar]
- Hensman C, Baty D, Willis RG, et al. (1998) Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. Surg Endosc; 12: 1017–19. [DOI] [PubMed] [Google Scholar]
- Hohlfeld B, Preissler G, Jauch KW, et al. (2008) Surgical smoke and ultrafine particles. J Occup Med Tox; 3: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehler R, He X, Grinshpun SA. (2014) A novel face seal design for filtering facepiece respirators: development and pilot testing in a hospital operating room. J Intern Soci Resp Protect; 31: 116–27. [Google Scholar]
- Krones CJ, Conze J, Hoelzl F, et al. (2007) Chemical composition of surgical smoke produced by electrocautery, harmonic scalpel and argon beaming - a short study. Eur Surg; 39: 118–21. [Google Scholar]
- Kulkarni P, Baron PA, Willeke K. (Eds) Aerosol measurement: principles, techniques, and applications. 3rd edn, Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Mettenleiter TC, Sobrino F. (2008) Animal viruses: molecular biology. UK: Caister Academic Press. [Google Scholar]
- NIOSH. (1996) Control of smoke from laser/electric surgical procedures. Atlanta, GA: DHHS (NIOSH) Publication. [Google Scholar]
- OSHA. (2007) Laser/Electrosurgery Plume. https://www.osha.gov/SLTC/laserelectrosurgeryplume/. Accessed 20 July 2015.
- OSHA. (1998) Respiratory protection; final rule. Federal Register; 63: 1152–300. [PubMed] [Google Scholar]
- Pollock SV. (2008) Electrosurgery. In Bolognia JL, Jorizzo JL, Rapini RP, editors. dermatology. 2nd ed Philadelphia, PA: Mosby Elsevier. [Google Scholar]
- Raynor PC, Leith D, Lee KW, et al. (2011) Chapter 7: Sampling and analysis using filters. Aerosol measurement: principles, techniques, and applications. 3rd ed Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Reponen T, Lee SA, Grinshpun SA, et al. (2011) Effect of fit testing on the protection offered by n95 filtering facepiece respirators against fine particles in a laboratory setting. Ann Occup Hyg; 55: 264–71. [DOI] [PubMed] [Google Scholar]
- Rota PA, Oberste MS, Monroe SS, et al. (2003) Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science; 300: 1394–99. [DOI] [PubMed] [Google Scholar]
- Rozzi T, Snyder J, Novak D. (2012) Pilot study of aromatic hydrocarbon adsorption characteristics of disposable filtering facepiece respirators that contain activated carbon. J Occup Environ Hyg; 9: 624–9. [DOI] [PubMed] [Google Scholar]
- Sahaf OA, Carrascal IV, Cunningham F, et al. (2007) Chemical composition of smoke produced by high-frequency electrosurgery. Irish J Med Sci; 176: 229–32. [DOI] [PubMed] [Google Scholar]
- Weber A, Willeke K, Marchioni R, et al. (1993) Aerosol penetration and leakage characteristics of masks used in the health care industry. Am J Infect Control; 21: 167–73. [DOI] [PubMed] [Google Scholar]
- Weld KJ, Dryer S, Ames CD, et al. (2007) Analysis of surgical smoke produced by various energy-based instruments and effect on laparoscopic visibility. J Endourol; 21: 347–51. [DOI] [PubMed] [Google Scholar]
- Zaki AH, Boheemen S, Theo M, et al. (2012) Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med; 367:1814–20. [DOI] [PubMed] [Google Scholar]
- Zheng ZM, Baker CC. (2006) Papillomavirus genome structure, expression, and post-transcriptional regulation. Front Biosci; 11: 2286–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang Z, Coffey CC, Jensen PA. (2003) Correlation between quantitative fit factors and workplace protection factors measured in actual workplace environments at a steel foundry. AIHA J.; 64: 730–38. [DOI] [PubMed] [Google Scholar]