Abstract
In recent years a number of beneficial health effects have been ascribed to the renin-angiotensin system (RAS) that extend beyond lowering blood pressure, primarily mediated via the angiotensin-converting enzyme-2 (ACE2)/angiotensin (1–7) or Ang(1–7)/MAS receptor axis. Moreover, once thought as merely a systemic effector, RAS components exist within tissues. The highest tissue concentrations of ACE2 mRNA are located in the gut making it an important target for altering RAS function. Indeed, genetically engineered recombinant probiotics are promising treatment strategies offering delivery of therapeutic proteins with precision. An Ang(1–7) secreting Lactobacillus paracasei (LP) or LP-A has been described for regulation of diabetes and hypertension; however, we are the first to the best of our knowledge to propose this paradigm as it relates to aging. In this Research Practice manuscript, we provide proof of concept for using this technology in a well-characterized rodent model of aging: the Fisher344 x Brown Norway Rat (F344BN). Our primary findings suggest that LP-A increases circulating levels of Ang(1–7) both acutely and chronically (after 8 or 28 treatment days) when administered 3× or 7×/week over 4 weeks. Our future preclinical studies will explore the impact of this treatment on gut and other age-sensitive distal tissues such as brain and muscle.
Keywords: Probiotics, Dysbiosis, Renin-angiotensin system, Ang-(1–7), Lactobacillus
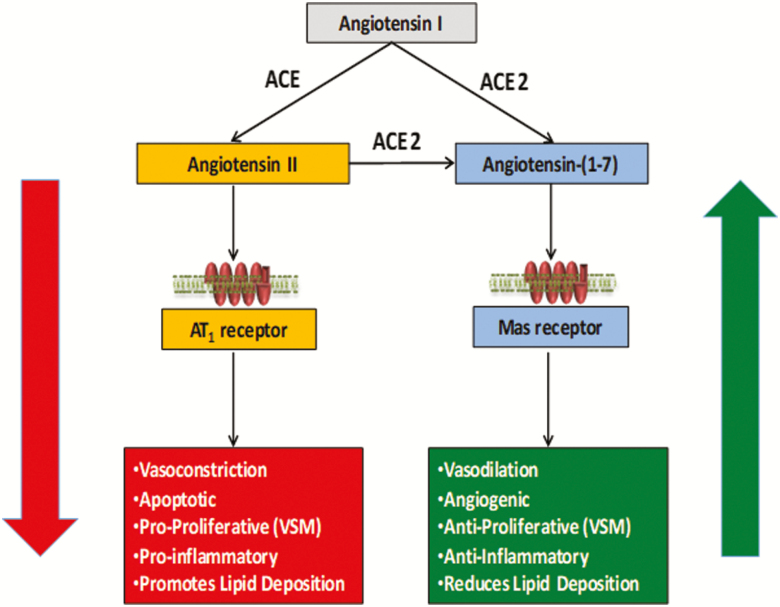
In recent years a number of pleiotropic effects have been ascribed to the renin-angiotensin system (RAS) beyond modulating blood pressure (1,2). Classically, the canonical RAS was thought to function primarily by balancing the vasoconstrictive actions of angiotensin II (AngII) binding to the AT1 receptor (AT1R) with the actions of bradykinin—a potent vasodilatory substance. However, an adjunctive RAS axis was recently discovered, which functions by binding of the peptide angiotensin (1–7) or Ang(1–7) to the Mas (AT7) receptor. In contrast to the vasoconstrictive actions of the AngII/AT1R axis, the angiotensin-converting enzyme-2 (ACE2) axis induces several beneficial physiologic effects (Figure 1). Though once thought merely a systemic effector, components of the RAS [including ACE2 and Ang(1–7)] exist within a variety of tissues, most notably within the gastrointestinal tract. ACE2 mRNA and protein are present in significant amounts in small intestinal brush border, muscularis mucosa, and propria, as well as microvascular endothelium and vascular smooth muscle cells (3). Additionally, the highest tissue concentrations of ACE2 mRNA are found in the terminal ileum, duodenum, and colon (4,5); thus making the gut an important target for altering RAS function.
Figure 1.
Ang(1–7) promotes beneficial actions of the renin-angiotensin system (RAS). Once thought to merely regulate blood pressure, the RAS is now known to have a variety of physiologic functions, including beneficial effects of the Ang(1–7) axis.
Indeed, genetically engineered recombinant probiotics have been purported as highly promising treatment strategies (6,7) as they offer a potentially efficacious method to deliver therapeutic proteins with precision and a high degree of site specificity (8). Several groups have proposed RAS-related probiotics, namely an Ang(1–7)-secreting Lactobacillus paracasei (LP) or LP-A, for the regulation of diabetes, blood pressure and other hypertension symptoms (9,10). In this Research Practice manuscript, we are the first, to the best of our knowledge, to propose this paradigm as it relates to aging as we provide proof of concept in a well-characterized rodent model of aging: the Fisher 344 x Brown Norway Rat (F344BN). We also provide evidence for establishing an optimal dosing strategy using circulating Ang(1–7) levels as our primary outcome and other RAS analytes (AngII, ACE, ACE2) to identify changes in both arms of the RAS acute (8 days) and chronic (4 weeks) treatment.
Methods
Animals
Subjects were male F344BN rats obtained from the National Institute on Aging Colony at Harlan Laboratories (Indianapolis, IN). No females were used in this experiment because the colony at NIA is not currently supplying these animals (expected date is late in 2019 where we will repeat these experiments in females). This rat strain was chosen because of its increased longevity and decreased cumulative lesion incidence compared with other strains (11). Animals (n = 29) were received at 24 months of age and housed individually on a 12 hours light and 12 hours dark cycle in a specific pathogen-free facility accredited by the American Association for Accreditation of Laboratory Animal Care at the University of Florida. Animals were fed a standard rodent chow (18% kcal from fat, no sucrose, 3.1 kcal/g, diet 2018; Harlan Teklad, Madison, WI). Animals were allotted 1 week to acclimate to their housing conditions and to establish baseline rates of food intake and body weight. Health status, body weight, and food intake were monitored daily. Health assessments included checking for a sudden decline in body weight, redness around the eyes and nostrils, ruffled coat, open tail sores, and haunched posture. All experimental protocols were approved by the University of Florida’s Animal Care and Use Committee, and in accordance with the “Guide for the Care and Use of Laboratory Animals.”
Design
Rats (n = 6–8/group) were randomized at 24 months of age to the following treatment groups for 4 weeks: TAS vehicle or LP-A delivered 0×, 1×, 3×, or 7×/week. The concentration of the LP-A did not change, only the number of days/week that the LP-A was delivered. This range of doses were was chosen based on preliminary data from our laboratory indicating that LP-A given 3×/week was sufficient to raise Ang(1–7) in male F344BN rats by 25%, although this change was not statistically significant due to small numbers of animals (data not shown). To refine the dosing strategy, we chose a smaller (1×/week) and larger dose (7×/week). On days when rats in the 1× and 3×/week group did not receive the LP-A, they were gavaged with PBS to control for the stress of being handling handled and gavaged to a similar degree as the 7×/week group. Animals were weighed and their food intake measured daily to ensure there were no anorectic or other adverse effects of the drug administration. On days 8 and 29, sublingual blood was drawn for analyses analysis of circulating RAS components. At the end of the 4 weeks, animals were euthanized by rapid decapitation, and tissues were dissected for future analyses.
Probiotic Formulation and Administration
Construction of recombinant probiotics secreting Ang-(1–7) is reported elsewhere (manuscript in preparation). Briefly, the plasmid pTRKH3-ldhGFP (Addgene, plasmid #27170) was used as a backbone for construction of the expression vector in which the Ang-(1–7) peptide is expressed as a secreted fusion protein with the chorea toxin binding protein subunit B (CTB), separated by a furin cleavage site. Fusion with CTB facilitates the transmucosal transport into circulation and tissue uptake by GM1 receptor-mediated endocytosis. The resulting plasmid was electroporated into LP by electroporation as described by Welker et al. (12). Wild Wild-type LP and LP-A were cultured in MRS (deMan Rogosa Sharpe) broth (BD Difco, Houston, TX) supplemented with 5 μg/mL erythromycin at 37°C for 18 hours. The bacteria were harvested by centrifugation at 5,000 × g for 20 minutes and re-suspended in sterile PBS for oral gavage. For extended storage, harvested bacteria were washed once with PBS and then suspended in TAS buffer (4% Trehalosetrehalose, 4% Sodium sodium Ascorbate ascorbate, and 6% skim milk) and frozen in small aliquots at −20°C. Colony counting was conducted before the animal experiments to ensure the numbers of surviving bacteria.
The animals were orally gavaged with 2 × 1011 CFU/ kg body weight or an equal volume of buffer. An 18-gauge gavage/feeding needle (3 inch length/ 3 mm ball diameter) was inserted into the esophagus, ensuring that there was no resistance to its advancement. The fluid was injected slowly and when complete, the needle was pulled straight out. The rats were tolerant of this procedure and no averse outcomes were observed over the 4-week study (Supplementary Video).
Sublingual Blood Draw
The tongue of an anesthetized (5% isofluorane) rat was grasped with tweezers, the vein punctured with a ¾ in 26 gauge needle, and blood allowed to drip into a serum tube. A cotton swab was used to stop bleeding. Rats recovered, within 5 minutes, in their home cages with a warming disk placed underneath the cage.
RAS Analytes
Concentrations of Ang(1–7) were evaluated to provide proof of principle that the LP-A was effective at elevating Ang(1–7) in the circulation. We also measured changes to circulating levels/activity of main effectors of the canonical and adjuvant RAS axes, namely AngII, ACE and ACE2.
Ang(1–7) and AngII concentrations
Serum levels of Ang-(1–7) and Ang II were measured using commercial ELISA kits according to instructions provided by the manufacturer [CES085Ra, Cloud-Clone Corp., Katy, TX, for Ang-(1–7); and ADI-900-204, Enzo Life Sciences, Inc., Farmingdale, NY for Ang II]. Briefly, for Ang-(1–7), the assay plates were coated with the monoclonal antibody specific to Ang-(1–7) and incubated overnight at 4°C The next day, the plates were washed and blocked followed by the addition of standards and samples and were incubated with biotinylated anti- Ang-(1–7) at 37°C for an hour, followed by a wash step. Streptavidin/Horseradish horseradish Peroxidase peroxidase (HRP) was then added to each well. After another wash, TMB (3, 3′, 5, 5′-Tetramethylbenzidinetetramethylbenzidine) substrate was added and the absorbance was read at 450 nm using a plate reader (SpectraMax M3, Molecular deviceDevices, Sunnyvale, CA).
For the AngII assay, the samples and standards were added on to the pre-coated assay plate and incubated with the anti-Ang II antibody for an hour at room temperature, followed by a wash step. Streptavidin/HRP was then added to each well. After another wash, TMB substrate was added and the absorbance was read at 450 nm using a plate reader (SpectraMax M3, Molecular device, United States).
All standards and samples were tested in duplicate and Ang-(1–7) and Ang II concentrations were calculated relative to the standard curve generated by serially diluting the standard provided in the kit.
ACE and ACE2 activity assay
Serum ACE and ACE2 activities were determined using assays based on fluorescent substrates, Abz-Phe-Arg-Lys[Dnp]-Pro-OH, M-2590 for ACE (Bachem, Torrance, CA), and Abz-Ser-Pro-3-nitro-Tyr-OH, M-2660 for ACE2 (R&D Systems, Inc., Minneapolis, MN), as published previously (13–15). Briefly, for ACE activity, the assay was performed in black 96-well plates with 10 μM fluorescent substrate in a final volume of 100 μL per well. For each well, 10 ul serum sample was loaded along with the assay buffer (75 mM Tris, 1 M NaCl, 0.5 μM ZnCl2, pH 7.5). The fluorescent intensity was measured using SpectraMax M3 fluorescence microplate reader (Molecular Devices) every 90 seconds with excitation at 320 nm and emission at 420 nm at 37°C for 2 hours.
The ACE2 activity assay was performed in black 96-well plates with 50 μM ACE2-specific fluorogenic peptide substrate (M-2660) in a final volume of 100 μL per well. For each well, 10 ul serum sample was loaded along with the assay buffer (75 mM Tris, 1 M NaCl, 0.5 μM ZnCl2, pH 7.5). The fluorescent intensity was measured using SpectraMax M3 fluorescence microplate reader (Molecular Devices, LLC, Sunnyvale, CA) for every 90 seconds with excitation at 340 nm and emission at 400 nm at 37°C for 2 hours.
All samples were run in duplicate and results are expressed as relative fluorescent units (RFU).
Statistics
Differences in RAS dependent measures were analyzed using univariate analysis of variance (ANOVA) with pre-planned contrasts comparing each dosing condition (1×, 3×, and 7×) to the 0×/week “control” condition. For body weight and food intake, the data were non-normally distributed; thus, we performed a nonparametric test of the differences of medians at baseline and across the 4 weeks of the study (Days 1, 8, 15, 22, and 29). All analyses were conducted using commercially available software (IBM SPSS Statistics 25, Armonk, NY). Differences were considered statistically significant when the p < .05.
Results
Body Weight and Food Intake
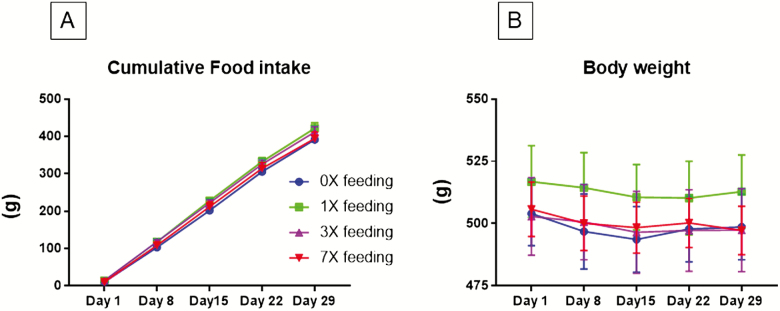
There were no observed differences between treatment levels in weekly body weight or cumulative food intake over the course of the study (Days 1, 8, 15, and 29; all ps > .05; Figure 2). This indicates that there were no adverse effects on general health.
Figure 2.
(A) Weekly body weight (Days 1, 8, 15, and 29) and (B) cumulative food intake were measured in 24-month-old male F344BN rats administration of 2 × 1011 CFU/ kg body weight LP-A in four dosing conditions: 0×, 1×, 3×, or 7×/week. There were no observed differences in either measure indicating animals were tolerant of the treatment with no impact to gross overall health.
RAS Analytes
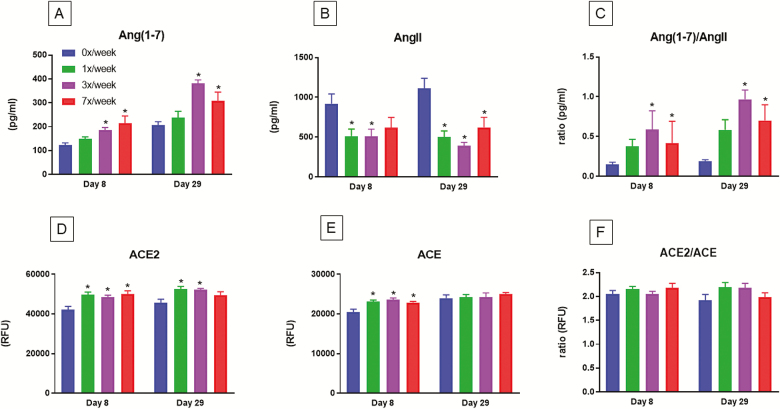
Figure 3 summarizes the results described below.
Figure 3.
Circulating RAS analytes were measured in 24-month-old male F344BN rats after 8 days (acute) and 29 days (chronic) administration of 2 × 1011 CFU/ kg body weight LP-A in four dosing conditions: 0×, 1×, 3×, or 7×/week. The graphs describe results for (A) Ang(1–7); (B) AngII; (C) Ang(1–7)/Ang(II) ratio; (D) ACE2; (E) ACE; (F) ACE2/ACE ratio. Overall, dosing 3× and 7×/week resulted in significantly higher levels of Ang(1–7), lower levels AngII and a higher ratio of the Ang(1–7)/AngII at both time points. ACE2 levels were significantly higher acutely in the 1×, 3×, and 7×/weeks groups but these effects persisted chronically only in the 3× and 7×/week groups. ACE levels were higher only acutely in the 1×, 3×, and 7×/week groups. There were no differences observed with chronic treatment nor in the ratio of ACE2/ACE at either time point. Data are presented as mean ± SEM. * denotes dosing condition significantly different from the 0×/week condition at their respective time points. ACE2 = angiotensin-converting enzyme-2; Ang(1–7) = angiotensin (1–7); LP = Lactobacillus paracasei; RAS = renin-angiotensin system.
Ang (1–7) and AngII
Rats in the 3× and 7× week groups had significantly higher levels of Ang(1–7) at Days 8 (p = .046 and p = .004, respectively) and 29 (p < .001 and p = .014) than control rats. AngII levels were significantly lower in the 1× and 3× groups at Day 8 (both ps = .009) while all groups were lower at Day 29 (p < .001, p < .001, and p = .003). However, the Ang(1–7)/AngII ratio was higher only in the 3× and 7× groups at Day 8 (p = .046 and p = .004) and Day 29 (p < .001 and p = .014).
ACE and ACE2
ACE, ACE2, and the ratio of ACE/ACE2 was measured as an additional measure of activation of the two arms of the RAS. Rats in the 1×, 3×, and 7× week groups had significantly higher levels of ACE at Day 8 (all ps < .001) relative to control. No differences were observed at Day 29. ACE2 levels were significantly higher in all groups at Day 8 (p = .002, p = .008, and p < .001); but only higher in the 1× and 3× groups at Day 29 (p = .003 and p = .006). There were no differences in the ACE/ACE2 ratio at either time point.
Discussion
The primary purpose of this study was to provide a proof of concept for using a recombinant probiotic secreting Ang(1–7) to increase circulating concentrations of Ang(1–7) in a well-characterized rodent model of aging: the F344BN rat. A secondary purpose was to observe the impact on other circulating RAS factors, namely AngII, ACE, and ACE2.
The use of an orally administered probiotic provides several potential advantages to traditional drug delivery including ease of administration, cost of production, and burden for regulatory approval. However, many preclinical studies utilize methods that may not correspond closely to those utilized in human studies. We designed the methods of this study, including the animal strain, intervention strategy, and statistical approach based on those utilized clinically facilitating the translation of study findings to future clinical trials.
Indeed, we found that LP-A increased circulating levels of Ang(1–7) and decreased levels of AngII. The dose was optimized at 3×/week indicating that this is the most reasonable and efficacious regimen for future preclinical studies. Moreover, this effect was recapitulated when we compared Ang(1–7)/AngII across groups as well as in acute versus chronic administration. The impact on ACE2, ACE activity, and the ratio of the two was less dramatic. ACE2 was both acutely and chronically higher in the 3× and 7×/week groups. ACE was higher in all dosing groups; however, only acutely. The ratio of the two was not changed at either time point. The reason for these secondary effects is not easily explainable, although it could be that we may have identified a positive feedback loop by which higher circulating Ang(1–7) modulates levels of these two enzymes. Whether these effects are specific to gut-delivered Ang(1–7) or if they are the result of specifically impacting circulating levels of Ang(1–7) remains an empirical question. We are currently conducting studies to address this issue by systemically administering Ang(1–7) using a similar design and outcome variables.
What are the clinical, human applications of this technology? This study has high impact for the treatment of aging and age-related human disease. Indeed, the human intestinal tract (ie, “gut”) is inhabited by over 100 trillion microorganisms, including over 1,000 species of known bacteria (16). Commonly overlooked in human health and disease treatment, gut microorganisms encode > 150 times more genes than the human genome that impact host physiology and metabolism (17,18). Advanced age is associated with loss of diversity and number of gut microbiota leading to a “leaky gut” and increased systemic inflammation, reaching distal organs such as brain (19,20). Moreover, gut dysbiosis is tightly linked with the development of cognitive impairment (21,22), physical frailty (23,24), and Alzheimer’s disease (25). In support of this concept, we recently demonstrated that serum zonulin, a key physiologic regulator of intestinal permeability (26,27) is elevated among healthy older adults compared to young adults (28). Zonulin concentrations were also positively correlated with indices of inflammation and negatively correlated to strength and physical activity. These findings in humans indicate that a “leaky gut” could be a primary source of age-related inflammation, as in preclinical models (29). Thus, the gut appears to be a key target for intervention to prevent, delay, or reverse aging and age-related disease.
The ACE2/Ang(1–7) axis has also recently received attention for its connection to the gut microbiome (30–32), particularly through its regulation of amino acid transport and immune function in the intestines (33–35). Moreover, evidence indicates that gut ACE2 is involved in regulating the ecology of the gut microbiome and attenuating intestinal inflammation suffered in response to epithelial damage (36). In fact, ACE2 deficient-mice demonstrated increased susceptibility to intestinal inflammation while transplantation of microbiota from these mice into germ-free, wild-type hosts induced colitis. As such, modulating the ACE2/Ang(1–7) axis appears to be a promising intervention for gut health.
The results from this study focus on LP-A influence on circulating levels of Ang(1–7) and do not necessarily address how this treatment impacts gut RAS modulation nor the impact on downstream targets such as gut and distal tissue inflammation (muscle and brain for example). In addition, our studies do not dissociate the impact of LP versus LP-A activation of the RAS alone. We are currently conducting studies to address these questions.
Funding
This work was supported by the National Institutes of Health/National Institute on Aging (R01AG054538 to C.S.C. and T.W.B.)
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
We would like to thank Mr. Brian Bouverat and Ms. Liana Juarez for technical assistance during the course of this study.
References
- 1. Sica D. Are there pleiotropic effects of antihypertensive medications or is it all about the blood pressure in the patient with diabetes and hypertension? J Clin Hypertens (Greenwich). 2011;13:301–304. doi:10.1111/j.1751-7176.2011.00450.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zoccali C, Mallamaci F. Pleiotropic effects of angiotensin II blockers in hemodialysis patients: myth or reality? Kidney Int. 2014;86:469–471. doi:10.1038/ki.2014.155 [DOI] [PubMed] [Google Scholar]
- 3. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi:10.1002/path.1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107–110. doi:10.1016/s0014-5793(02)03640-2 [DOI] [PubMed] [Google Scholar]
- 5. Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275:33238–33243. doi:10.1074/jbc.M002615200 [DOI] [PubMed] [Google Scholar]
- 6. Steidler L. Genetically engineered probiotics. Best Pract Res Clin Gastroenterol. 2003;17:861–876. [DOI] [PubMed] [Google Scholar]
- 7. Syvanen M. Churning out safer microbes for drug delivery. Nat Biotechnol. 2003;21:758–759. doi:10.1038/nbt0703-758 [DOI] [PubMed] [Google Scholar]
- 8. Kumar M, Yadav AK, Verma V, et al. Bioengineered probiotics as a new hope for health and diseases: an overview of potential and prospects. Future Microbiol. 2016;11:585–600. doi:10.2217/fmb.16.4 [DOI] [PubMed] [Google Scholar]
- 9. Daliri EB, Lee BH, Oh DH. Current perspectives on antihypertensive probiotics. Probiotics Antimicrob Proteins. 2017;9:91–101. doi:10.1007/s12602-016-9241-y [DOI] [PubMed] [Google Scholar]
- 10. Raizada MK, Joe B, Bryan NS, et al. Report of the national heart, lung, and blood institute working group on the role of microbiota in blood pressure regulation: current status and future directions. Hypertension. 2017;70:479–485. doi:10.1161/HYPERTENSIONAHA.117.09699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Turturro A, Witt WW, Lewis S, Hass BS, Lipman RD, Hart RW. Growth curves and survival characteristics of the animals used in the biomarkers of aging program. J Gerontol A Biol Sci Med Sci. 1999;54:B492–B501. doi:10.1093/gerona/54.11.b492 [DOI] [PubMed] [Google Scholar]
- 12. Welker DL, Hughes JE, Steele JL, Broadbent JR. High efficiency electrotransformation of Lactobacillus casei. FEMS Microbiol Lett. 2015;362:1–6. doi:10.1093/femsle/fnu033 [DOI] [PubMed] [Google Scholar]
- 13. Shil PK, Kwon KC, Zhu P, Verma A, Daniell H, Li Q. Oral delivery of ACE2/Ang-(1-7) bioencapsulated in plant cells protects against experimental uveitis and autoimmune uveoretinitis. Mol Ther. 2014;22:2069–2082. doi:10.1038/mt.2014.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Verma A, Shan Z, Lei B, et al. ACE2 and Ang-(1-7) confer protection against development of diabetic retinopathy. Mol Ther. 2012;20:28–36. doi:10.1038/mt.2011.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li Q, Xu K, Du TAO, Zhu P, Verma A. Recombinant probiotics expressing angiotensin-(1–7) improves glucose metabolism and diabetes-induced renal and retinal injury. Diabetes. 2018;67(Supplement 1):33-LB. doi:10.2337/db18-33-LB. [Google Scholar]
- 16. Gill SR, Pop M, Deboy RT, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312:1355–1359. doi:10.1126/science.1124234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Egert M, de Graaf AA, Smidt H, de Vos WM, Venema K. Beyond diversity: functional microbiomics of the human colon. Trends Microbiol. 2006;14:86–91. doi:10.1016/j.tim.2005.12.007 [DOI] [PubMed] [Google Scholar]
- 18. Thaiss CA, Zeevi D, Levy M, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159:514–529. doi:10.1016/j.cell.2014.09.048 [DOI] [PubMed] [Google Scholar]
- 19. Biagi E, Nylund L, Candela M, et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS One. 2010;5:e10667. doi:10.1371/journal.pone.0010667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jeffery IB, Lynch DB, O’Toole PW. Composition and temporal stability of the gut microbiota in older persons. ISME J. 2016;10:170–182. doi:10.1038/ismej.2015.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cattaneo A, Cattane N, Galluzzi S, et al. ; INDIA-FBP Group Association of brain amyloidosis with pro-inflammatory gut bacterial taxa and peripheral inflammation markers in cognitively impaired elderly. Neurobiol Aging. 2017;49:60–68. doi:10.1016/j.neurobiolaging.2016.08.019 [DOI] [PubMed] [Google Scholar]
- 22. Lawrence K, Hyde J. Microbiome restoration diet improves digestion, cognition and physical and emotional wellbeing. PLoS One. 2017;12:e0179017. doi:10.1371/journal.pone.0179017 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23. van Tongeren SP, Slaets JP, Harmsen HJ, Welling GW. Fecal microbiota composition and frailty. Appl Environ Microbiol. 2005;71:6438–6442. doi:10.1128/AEM.71.10.6438-6442.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jackson MA, Jeffery IB, Beaumont M, et al. Erratum to: signatures of early frailty in the gut microbiota. Genome Med. 2016;8:21. doi:10.1186/s13073-016-0275-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Spielman LJ, Gibson DL, Klegeris A. Unhealthy gut, unhealthy brain: the role of the intestinal microbiota in neurodegenerative diseases. Neurochem Int. 2018;120:149–163. doi:10.1016/j.neuint.2018.08.005 [DOI] [PubMed] [Google Scholar]
- 26. Sturgeon C, Fasano A. Zonulin, a regulator of epithelial and endothelial barrier functions, and its involvement in chronic inflammatory diseases. Tissue Barriers. 2016;4:e1251384. doi:10.1080/21688370.2016.1251384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fasano A. Intestinal permeability and its regulation by zonulin: diagnostic and therapeutic implications. Clin Gastroenterol Hepatol. 2012;10:1096–1100. doi:10.1016/j.cgh.2012.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Qi Y, Goel R, Kim S, et al. Intestinal permeability biomarker zonulin is elevated in healthy aging. J Am Med Dir Assoc. 2017;18:810.e1–810.e4. doi:10.1016/j.jamda.2017.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Thevaranjan N, Puchta A, Schulz C, et al. Age-associated microbial dysbiosis promotes intestinal permeability, systemic inflammation, and macrophage dysfunction. Cell Host Microbe. 2017;21:455–466.e4. doi:10.1016/j.chom.2017.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Simon CB, Lee-McMullen B, Phelan D, Gilkes J, Carter CS, Buford TW. The renin-angiotensin system and prevention of age-related functional decline: where are we now? Age (Dordr). 2015;37:9753. doi:10.1007/s11357-015-9753-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perlot T, Penninger JM. ACE2 - from the renin-angiotensin system to gut microbiota and malnutrition. Microbes Infect. 2013;15:866–873. doi:10.1016/j.micinf.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cole-Jeffrey CT, Liu M, Katovich MJ, Raizada MK, Shenoy V. ACE2 and microbiota: emerging targets for cardiopulmonary disease therapy. J Cardiovasc Pharmacol. 2015;66:540–550. doi:10.1097/FJC.0000000000000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Camargo SM, Singer D, Makrides V, et al. Tissue-specific amino acid transporter partners ACE2 and collectrin differentially interact with hartnup mutations. Gastroenterology. 2009;136:872–882. doi:10.1053/j.gastro.2008.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kowalczuk S, Bröer A, Tietze N, Vanslambrouck JM, Rasko JE, Bröer S. A protein complex in the brush-border membrane explains a Hartnup disorder allele. FASEB J. 2008;22:2880–2887. doi:10.1096/fj.08-107300 [DOI] [PubMed] [Google Scholar]
- 35. Hashimoto T, Perlot T, Rehman A, et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487:477–481. doi:10.1038/nature11228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xie W, Zhu D, Ji L, Tian M, Xu C, Shi J. Angiotensin-(1-7) improves cognitive function in rats with chronic cerebral hypoperfusion. Brain Res. 2014;1573:44–53. doi:10.1016/j.brainres.2014.05.019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.