Abstract
Foodborne and waterborne viral infections are increasingly recognized as causes of illness in humans. This increase is partly explained by changes in food processing and consumption patterns that lead to the worldwide availability of high‐risk food. As a result, vast outbreaks may occur due to contamination of food by a single foodhandler or at a single source. Although there are numerous fecal–orally transmitted viruses, most reports of foodborne transmission describe infections with Norwalk‐like caliciviruses (NLV) and hepatitis A virus (HAV), suggesting that these viruses are associated with the greatest risk of foodborne transmission. NLV and HAV can be transmitted from person to person, or indirectly via food, water, or fomites contaminated with virus‐containing feces or vomit. People can be infected without showing symptoms. The high frequency of secondary cases of NLV illness and – to a lesser extent – of hepatitis A following a foodborne outbreak results in amplification of the problem. The burden of illness is highest in the elderly, and therefore is likely to increase due to the aging population. For HAV, the burden of illness may increase following hygienic control measures, due to a decreasing population of naturally immune individuals and a concurrent increase in the population at risk. Recent advances in the research of NLV and HAV have led to the development of molecular methods which can be used for molecular tracing of virus strains. These methods can be and have been used for the detection of common source outbreaks. While traditionally certain foods have been implicated in virus outbreaks, it is clear that almost any food item can be involved, provided it has been handled by an infected person. There are no established methods for detection of viruses in foods other than shellfish. Little information is available on disinfection and preventive measures specifically for these viruses. Studies addressing this issue are hampered by the lack of culture systems. As currently available routine monitoring systems exclusively focus on bacterial pathogens, efforts should be made to combine epidemiological and virological information for a combined laboratory‐based rapid detection system for foodborne viruses. With better surveillance, including typing information, outbreaks of foodborne infections could be reported faster to prevent further spread.
Keywords: Norwalk‐like virus, Foodborne virus
1General introduction
1.1Introduction
The importance of foodborne transmission of viruses is increasingly recognized [1], and the World Health Organization has signaled an upward trend in their incidence [2]. It is also understood that the burden of infection is grossly underestimated by routine surveillance [[3], [4]]. The aging population (with increasing numbers of people at risk for complications of enteric infections) and the globalization of infectious diseases due to rapid international travel and (food) trade add to the notion that the burden of illness is likely to increase in the years to come [5]. Vast outbreaks may occur due to contamination of food by a single foodhandler or at a single source, as has been documented on several occasions.
Numerous viruses can be found in the human intestinal tract (Table 1). The food‐ and waterborne viruses can be divided into three disease categories:
Table 1.
Enteric viruses grouped according to the associated clinical syndrome
| Gastroenteritis | Possibly gastroenteritis |
| Rotavirus group A, B, C | Picobirnavirus |
| Adenovirus types 40, 41 | Torovirus |
| Astrovirus serotypes 1–8 | Coronavirus |
| Norwalk‐like caliciviruses | Cytomegalovirus |
| Sapporo‐like caliciviruses | Human immunodeficiency virus |
| Aichivirus | |
| Parvo‐like viruses, Small round featureless viruses | |
| Hepatitis | Other |
| Hepatitis A virus | Enteroviruses: |
| Hepatitis E virus | • polio 1–3 |
| • Coxsackie A 1–22, 24 | |
| • Coxsackie B 1–6 | |
| • echo 1–9, 11–27, 29–34 | |
| • entero 68–71 | |
| • Aichi virus | |
| Parvovirus? |
The name Aichivirus has been given to (different) viruses in the calicivirus family and in the picornavirus family.
-
1
viruses that cause gastroenteritis (e.g. astrovirus, rotavirus, the enteric adenoviruses, and the two genera of enteric caliciviruses, i.e. the small round structured viruses or ‘Norwalk‐like viruses’ (NLV), and typical caliciviruses or ‘Sapporo‐like viruses’ (SLV);
-
2
fecal–orally transmitted hepatitis viruses: hepatitis A virus (HAV), hepatitis E virus (HEV);
-
3
viruses which cause other illness, e.g. enteroviruses.
In addition, several viruses are listed that also replicate in the intestinal tract, but are not implicated in foodborne transmission, or whose role is unknown.
Viruses, unlike bacteria, are strict intracellular parasites and cannot replicate in food or water. Therefore, viral contamination of food will not increase during processing, and may actually decrease. This implies that viral infection via contaminated food depends on viral stability, amounts of virus shed by an infected individual, method of processing of food or water, dose needed to produce infection, and susceptibility of the host. Most food‐ or waterborne viruses are non‐enveloped and are relatively resistant to heat, disinfection and pH changes. Problems in the detection of viral contamination of food or water are that – generally – the contaminated products will look, smell, and taste normal, and that (molecular) diagnostic methods for most of these viruses are not routinely available in food microbiology laboratories. In this paper, the major viral causes of foodborne infections will be reviewed. We have focussed on those viruses that are most commonly transmitted by food, namely NLV and HAV.
1.2Cost of illness
The cost of illness due to viral foodborne infections is not known exactly, but it is likely to be high. In the USA, Mead et al. [6] recently estimated that foodborne diseases cause approximately 79 million illnesses, 325 000 hospitalizations, and 5000 deaths each year. For just the few foodborne pathogens for which cost estimates have been made, medical charges and lost productivity already cost society US$ 5–6 billion annually in the USA [7]. The total costs of salmonellosis are estimated to be US$ 1.2–1.5 billion. Although viral infections until recently were not commonly diagnosed, it is becoming clear from epidemiological studies that caliciviruses alone may be as frequent causes of foodborne illness as Salmonella[[6], [8]]. Costs of illness can be high due to their frequent occurrence and high transmissibility [[9], [10]]. In addition, there are studies that suggest that viral enteric infections cause deaths in the elderly, deaths that are largely preventable [[8], [11], [12], [13]].
In the USA, some 84 000 cases of hepatitis A are reported annually, of which an estimated 5% are foodborne or waterborne [6]. Common source foodborne hepatitis A outbreaks attract a great deal of public attention and concern, and require considerable public health control efforts. The estimated total cost of a single common source outbreak involving 43 persons, associated with an HAV‐infected foodhandler, was approximately US$ 800 000 (Centers for Disease Control and Prevention (CDC), unpublished). Outbreaks associated with contaminated foodstuffs have resulted in nationwide recalls.
2Food‐ and waterborne gastroenteritis with a focus on caliciviruses
2.1Introduction
Epidemic and sporadic gastroenteritis is an important public health problem in both developed and developing countries [[14], [15]]. In the last 27 years, several viruses have been identified as etiological agents of viral gastroenteritis in humans [16]. In most studies of food‐ and waterborne viruses, samples have been screened for viruses by tissue culture isolation techniques or by electron microscopy (EM). Some enteric viruses, however, cannot be grown in tissue culture, and EM is rather insensitive with a detection limit of around 105–106 particles per ml of stool suspension. Broadly reactive and user‐friendly diagnostic tests, such as enzyme‐linked immunosorbent assays (ELISA), have routinely been used for group A rotavirus and adenovirus in clinical specimens only. Recently, ELISA‐based assays have been developed for detection of astroviruses and NLV [[17], [18], [19]], but the latter lack the broadness that is required for generic detection. No similar assays exist for testing food samples. As a result of these limitations, foodborne viral gastroenteritis is usually not diagnosed.
In the absence of virus detection assays, a tentative diagnosis of viral gastroenteritis can be made based on epidemiological criteria described by Kaplan et al. [20]. Characteristic features are: acute onset after a 24–36‐h incubation period, vomiting and/or diarrhea lasting a few days, a high attack rate (average 45%), and a high number of secondary cases [[20], [21]]. Using this definition, an estimated 32–42% of foodborne enteric infections in the USA are caused by viruses. Outbreaks of gastroenteritis may be caused by rotaviruses, astroviruses, adenoviruses, and the human enteric caliciviruses. The human caliciviruses are assigned to two genera, which are currently described as ‘Norwalk‐like viruses’ (NLV), also known as small round structured viruses, and ‘Sapporo‐like viruses’ (SLV), also known as typical caliciviruses [[22], [23], [24], [25]]. The NLV cause illness in people of all age groups, whereas the SLV predominantly cause illness in children [26].
The relative importance of the different viruses as causes of food‐ and waterborne infections is not exactly known, but clearly NLV are the main cause of viral outbreaks [[5], [20], [21], [27]], and their incidence reportedly has been increasing in recent years [[1], [2], [28]]. This ‘emergence’ of NLV as the main foodborne virus most likely is not a true increase in incidence, but rather an increased awareness combined with improved diagnostic assays. The remainder of this chapter will focus on NLV, unless otherwise indicated.
2.2Background
Epidemic non‐bacterial gastroenteritis or ‘winter vomiting disease’ was described as early as 1929 but the numerous attempts to propagate the presumed viral etiologic agent in vitro have met with little success [29]. A major breakthrough was the discovery of the Norwalk virus (NV) using immune EM (IEM) in fecal samples collected during an outbreak of gastroenteritis, which occurred in 1968 in an elementary school in Norwalk, OH, USA [30]. These viruses were non‐enveloped and the particles had a ‘fuzzy’ amorphous appearance and measured 34–38 nm in diameter. Volunteer studies established NV as an enteric pathogen and, except for the unsuccessful cultivation of the virus, fulfilled Koch's postulates [[31], [32]]. Since then, additional studies have been carried out using fecal samples from other outbreaks of gastroenteritis, containing particles which were morphologically indistinguishable from NV [[33], [34]]. These viruses have often been named after the geographic setting in which the outbreak occurred, for example, Hawaii virus, Snow Mountain virus, Montgomery county virus, Toronto virus. This practice became a routine procedure and persists to the present day.
In 1976, viruses with the typical calicivirus morphology were observed in the stools of infants suffering from diarrhea [[35], [36]]. Typical calicivirus particles measure 30–34 nm in diameter; they can be identified by their characteristic cup‐shaped depressions. Astroviruses may have the five/six‐pointed surface star on up to 20% of the particles, which makes it possible to distinguish them from typical caliciviruses [36]. However, because these viruses were detected as frequently in asymptomatic as in sick children, no clinical significance could be attached to this finding. The first convincing association with disease came from a study of ‘winter vomiting disease’ which occurred in a school in London in January 1978 [37], and since then, typical caliciviruses have been linked with cases of mild diarrhea in both infants and children and shown to induce illness in volunteers [38].
2.3The viruses
Human caliciviruses are small, non‐enveloped spherical viruses, measuring between 28 and 35 nm in size that contain a single‐stranded RNA genome of 7.3–7.6 kb. The genome is of positive polarity, and contains coding information for a set of non‐structural proteins, located at the 5′‐end of the genome, and one major structural protein at the 3′‐end [22]. The distinguishing feature between the genome organization of NLV and SLV is the arrangement of the open reading frames (ORFs). In both genera, ORF1 encodes a large polyprotein (1789 amino acids for NV) with conserved regions of amino acid similarity with the picornavirus 2C helicase, 3C protease, and 3D polymerase [[22], [24]]. For NLV, the ORF2 region encodes the single major capsid protein (≅56 kDa) [24]. A third ORF encodes a minor structural protein with a predicted molecular mass of 22.5 kDa [39]. In SLV, the region encoding the capsid protein (60 kDa for the prototype of this group, Manchester virus) is found in the same reading frame as ORF1, and is contiguous with the non‐structural proteins. Together, the non‐structural genes and the major capsid gene form one long polyprotein, which occupies over 90% of the total genome [25]. Similar to NLV, SLV possess a small ORF at the 3′‐end of the genome encoding a protein of 17.5 kDa.
2.4Clinical symptoms
Following a 1–3‐day incubation period, infected persons may develop (low‐grade) fever and vomiting, diarrhea, and headache as prominent symptoms. The illness generally is considered mild and self‐limiting, with symptoms lasting 2–3 days [[20], [26]]. Data from a recently completed community‐based cohort study in The Netherlands were surprising in that 20% of NLV‐infected persons reported symptoms for more than 2 weeks, suggesting that NLV infections may be less innocuous (Rockx et al., in preparation). In adults, projectile vomiting occurs frequently. Sometimes parenteral fluid therapy or even hospitalization is required, with up to 12% of cases hospitalized in a recent outbreak in military recruits [[27], [33], [40], [41]]. Deaths associated with NLV outbreaks have been reported, but the etiologic association needs to be confirmed [[8], [12]]. The average attack rate is high (typically 45% or more) [10]. Virus is shed via stools and vomit, starting during the incubation period, and lasting up to 10 days, and possibly longer [[20], [26], [42], [43]]. NLV infections are highly contagious, resulting in a high rate of transmission to contacts. Mixtures of symptoms may occur, since contaminated foods may contain multiple agents [44].
2.5Pathogenesis
Little is known about the mechanisms by which NLV cause diarrhea. In duodenal biopsies taken from infected volunteers, lesions were seen in the intestinal epithelium at 1 day post infection with the Norwalk virus or Hawaii virus as inoculum. The changes were villous broadening, abnormal epithelial cells, loss of and an inflammatory response in the lamina propria with infiltration of polymorphonuclear leukocytes and lymphocytes. At 5–6 days after ingestion villous shortening and crypt hypertrophy were observed. d‐Xylose absorption was significantly reduced throughout this period [[32], [45]]. The observed inflammatory response in the lamina propria was similar to the damage that has been observed following rotavirus infections, where pro‐inflammatory cytokines and chemokines are thought to trigger this process [46]. There are no known systemic effects.
2.6Diagnosis in humans
Despite numerous attempts by several groups of investigators, NLV have never been isolated in cell or tissue culture, and diagnosis has been made historically by visualization of virus particles by EM [[30], [47]]. However, EM is a relatively insensitive technique, requiring the presence of a minimum of around 105–106 particles per ml of stool sample, and – unlike some other enteric viruses – NLV are not shed to very high maximum titers. This may not be a problem in outbreak investigations, when similar results may be obtained when stool samples have been collected promptly [48]. For community‐based studies, however, this was an impediment until the complete genome of the NLV prototype, the Norwalk virus, was sequenced from cDNA clones derived from RNA that had been extracted from a bulk stool specimen [[23], [24]]. From early work with IEM, and later sequence analysis of genomes of different NLV strains, it became evident that the NLV are in fact an antigenically and genetically diverse group of viruses [[49], [50], [51], [52], [53]]. At present, genome‐based detection methods are available, in which fragments of the viral RNA are amplified directly from stool samples by reverse‐transcriptase polymerase chain reaction (RT‐PCR) ([[54], [55]], reviewed in [47]). Initial studies using these methods to detect viral RNA in outbreak specimens confirmed the unusual level of divergence, even when a highly conserved region of the viral genome was selected as a target for the RT‐PCR [[51], [56], [57], [58]]. Since then, second generation assays have been developed, which have been optimized for detection of a broad range of NLV, by targeting conserved motifs in the non‐structural protein genes [[9], [57], [59], [60]]. Following detection of NLV by RT‐PCR, the PCR products can be characterized further by sequencing (described in Section 2.9).
Although NLV cannot be grown in cell culture, efforts have been made to develop antigen‐based detection methods. For this purpose, recombinant NLV capsids have been developed for use as control antigens [[18], [19], [60], [61], [62], [63], [64], [65]]. However, the current problem is that (hyper)immune responses are predominantly type‐specific, and that assays based on these reagents are narrow in their applicability [[19], [60], [65]]. NLV are a diverse group of viruses, and can be divided into two, possibly three broad genogroups, based on antigenic and genetic criteria (see Section 2.9). Recently, a NV‐specific monoclonal antibody was characterized with reactivity to strains from four out of five other variants within genogroup I NLV that were tested [66]. Similarly, for genogroup II NLV, a common epitope has been identified [67]. When tested in an ELISA, this monoclonal appeared to detect GGI viruses as well, suggesting that it detects a genus‐specific epitope. These monoclonal antibodies offer the first hope for development of a more broadly reactive detection assay. For a complete overview of NLV diagnostics see Atmar and Estes [47].
2.7Epidemiology
Following the development of molecular detection methods, it has become clear that NLV infections are among the most important causes of gastroenteritis in adults and often occur as outbreaks which may be foodborne. However, an important message is also that the estimate of the proportion of foodborne NLV outbreaks varies greatly from one country to the other, due to differences in case definition, surveillance systems, and methods used. In The Netherlands, approximately 80% of outbreaks of gastroenteritis that were reported in the past seven years to RIVM through health services NLV [[9], [10], [68], [69]]. More than half of these outbreaks occurred in nursing homes [[10], [68]]. The proportion of foodborne outbreaks was 14% in 1994–2000, with 83% of these attributed to NLV. This clearly is an underestimate as foodborne outbreaks are usually reported through the regional food inspection services, rather than municipal health services. In a survey of all outbreaks of infectious intestinal disease in England and Wales between 1992 and 1994, 27% outbreaks were caused by NLV (for comparison: 32% of the outbreaks were due to Salmonella spp.) [8]. NLV were the cause of 6% of foodborne outbreaks. Since outbreak specimens were mostly examined by EM, the actual number of NLV outbreaks may be higher [[8], [19]]. In the US, 86 of 90 (96%) outbreaks of non‐bacterial acute gastroenteritis reported to CDC between January 1997 and June 1998 were caused by NLV infection. Of those outbreaks for which a mode of transmission was reported, 24 of 51 (47%) were considered foodborne. Several large outbreaks with a serious impact on troops on military aircraft carriers have been described [70]. Nosocomial outbreaks are common [[10], [71], [72]]. In Finland, hospital outbreaks (mostly on geriatric wards) are almost exclusively caused by NLV, but there is serious underreporting. Also in Finland, 56% of the epidemics reported as foodborne, from which stool samples (and foodstuffs, in some instances) were submitted for virological screening, were NLV‐positive [73]. Of water epidemics 12/15 have been NLV‐positive. Since 1998 15 berry‐related epidemics have occurred, which has resulted in a ban on the use of unheated berries in all catering and other large‐scale kitchens [74]. Since then, some berry‐associated outbreaks have occurred, in cases where the ban was ignored. Most of these outbreaks were linked to imported berries. From molecular typing, based on a 125‐bp fragment of a highly conserved region of the polymerase gene, it was shown that many different lineages of NLV could be found, which illustrates that contamination of these foods was not linked to a single common source (Fig. 1).
Figure 1.

Phylogenetic tree showing NLV lineages, based on a 125‐bp fragment within a conserved region of the viral polymerase gene, that were found in outbreaks of gastroenteritis in Finland (identified by number), including 12 outbreaks in which raspberries were implicated as the most likely source of infection (indicated by arrows). GG=genogroup. MV=Mexico virus, TV=Toronto virus, HV=Hawaii virus, SOV=Southampton virus, NV=Norwalk virus and DSV=Desert Shield virus, all reference strains of NLV.
In addition to outbreaks, recent publications suggest that caliciviruses are among the most common causes of sporadic gastroenteritis [[3], [4], [68], [75], [76]]. In The Netherlands, a set of population‐based case–control studies showed that – overall – the incidence of gastroenteritis was quite high, at 280 cases/1000 persons per year for community cases of gastroenteritis, of which 8 cases/1000 persons per year seek treatment by a physician (1:35) [[3], [77], [78]]. Five percent of the patients who visit their physician for gastroenteritis were infected with NLV (compared with 4% for Salmonella), as well as 17% of persons in a sentinel population who developed diarrhea during the course of a 1‐year cohort study [[3], [68], [79], [80]]. People from all age groups were affected, with a slightly higher incidence in very young children. Similar studies in the UK suggested a slightly lower incidence of community cases of gastroenteritis (190 cases/1000 persons per year) but with a higher rate of referral to the physician [4]. Again, NLV were surprisingly common causes of illness in people of all age groups. The NLV are the second most common cause of gastroenteritis in young children [[3], [75], [81], [82]]. The course of illness appears to be somewhat milder than rotavirus gastroenteritis [75]. This may explain the lower percentage of hospitalized children with NLV that has been reported [[83], [84]]. Asymptomatic infections are common [[3], [82]].
2.8Risk groups
Outbreaks of NLV gastroenteritis (not only foodborne) are common in institutions such as nursing homes and hospitals. The attack rates typically are high (40–50% on average, but up to 100%) in both residents and personnel of such institutions, which in turn leads to major understaffing problems during outbreaks [[10], [85]]. Sporadic cases of viral gastroenteritis also occur frequently in these settings. The risk factors for these infections are currently under investigation in the UK and in The Netherlands. According to Gerba et al. [86] the groups of individuals who would be at the greatest risk of serious illness and mortality from water‐ and foodborne enteric microorganisms include young children, the elderly, pregnant women, and the immunocompromised. This segment of the population currently represents almost 20% of the population (in the USA) and is expected to increase significantly in the years to come, due to increases in life‐span and the number of immunocompromised individuals. Worldwide, diarrheal diseases account for millions of deaths annually, mostly in developing countries [15]. In developed countries, mortality due to diarrhea is low, but does occur in young children [[14], [87], [88]] and in the elderly (where >50% of all mortality occurs [[11], [13], [86]]). While specific mortality data on NLV are not available, given the high incidence of calicivirus infections in the elderly, it is likely that deaths resulting from calicivirus infection do occur [[8], [12]].
2.9Molecular epidemiology
The early studies demonstrating the great variability of NLV soon led to the notion that it was important to be able to distinguish between strains in order to better understand their epidemiology. Typically, variant viruses would be characterized by neutralization assays using hyperimmune sera or panels of monoclonal antibodies in a tissue culture infectivity assay. However, because no one has succeeded in culturing these viruses in vitro, their antigenic relationships have been evaluated primarily by cross‐challenge studies and IEM or solid phase IEM with viruses purified from stool samples [[20], [30], [33], [34], [52], [53]]. Since this could not be done with every new variant that is identified, genome characterization by sequence analysis has been used to provide an interim system of genotyping. As the genotypes ideally would correlate with serotypes, the sequence of the major structural protein gene was used as the basis for phylogenetic analysis. [[89], [90]]. Sequence analyses of viruses from different outbreaks and different geographical locations have confirmed that NLV can be divided into two major genetic groups (termed genogroups) based on capsid sequence and polymerase sequence data [[51], [56], [57], [58]]. NV, Southampton virus, and Desert Shield virus are members of genogroup I. Snow Mountain virus, Hawaii virus, Toronto virus are members of genogroup II. In addition, a highly divergent virus (Alphatron) was assigned to a putative third genogroup. Within genogroups I and II stable lineages have been identified, based on phylogenetic analysis based on the complete capsid gene of at least two representatives per cluster [[85], [91], [92]]. To date, 15 distinct genotypes have been recognized, but as more strains are characterized, this number is likely to increase [[89], [90]].
It is well established that many different genotypes of NLV cocirculate in the general population, causing sporadic cases and outbreaks [[59], [68], [72], [75], [81], [82], [91], [92], [93]]. Typically, strain sequences are (almost) identical within outbreaks, and different when specimens from different outbreaks are analyzed. Thus, when identical sequences are found in different patients or different clusters of illness, a common source for the infection should be suspected [[74], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110]]. Conversely, finding different sequences in people with a supposedly common source infection suggests independent contamination, unless there is an association with sewage‐contaminated water: in epidemics due to sewage contamination, often more than one NLV genotype is encountered [[73], [100], [110]]. Molecular epidemiology has been used on several occasions to confirm (e.g. [[94], [95], [96], [104], [105], [106]]) or disprove links between outbreaks (e.g. [108]). Occasionally, epidemics occur in which the majority of outbreaks are caused by a highly related group of viruses within a genotype, with only minimal differences in the conserved polymerase gene fragment that is used for genotyping [[10], [111], [112], [113]]. These epidemics may be widespread and even global [113]. The mechanisms behind emergence of epidemic types or fluctuations in the prevalent genotypes of NLV are unknown. Hypotheses include large‐scale foodborne transmission of a single strain, and the possibility of spillover from a non‐human reservoir.
2.10Immunity
Little is known about immunity to NLV infections. Antibody ELISA assays have been developed by using recombinant capsids as antigen, and preliminary studies suggest that – in outbreaks and in volunteer studies – people develop antibodies mostly restricted to the infecting genotype with some cross‐reactivity. From experimental infections in volunteers it is known that infected persons may become protected from reinfection, but only for a short period, and again only when the challenge virus is closely related to the genotype of the strain that was used for the infection [[60], [62]]. Seroprevalence studies with the recombinant antigens have shown that antibodies to NLV are very common in the population, even when the recombinant NV capsids are used in populations where viruses from the Norwalk cluster have not been identified for a long time. Volunteers with antibodies to the infecting genotype reportedly may have a higher risk of illness and a steeper dose–response curve [[42], [114]]. It is unclear what this means. Hinkula et al. [115] have shown that the seroprevalence may differ markedly for different antibody isotypes, suggesting that the lack of protection in part may be explained because a different type of antibody was the better correlate of protection. The lack of broadly reactive, long‐lived immunity to natural infection suggests that development of a protective vaccine may be problematic.
2.11Modes of transmission
NLV are transmitted by direct person‐to‐person contact or indirectly via contaminated water [[94], [96], [100], [102], [105], [106]], food [[74], [95], [98], [103], [108], [109], [110]] or contaminated environments [[97], [101], [107], [116]]. Clearly, person‐to‐person transmission is by far the most common route of infection. The infectious dose can be probably as low as 10–100 virus particles [[114], [117]]. However, many foodborne NLV outbreaks have been described, often resulting from contamination by an infected foodhandler. In addition, several waterborne outbreaks of NLV have been described, both directly (e.g. consumption of tainted water) or indirectly (e.g. via washed fruits, by swimming or canoeing in recreational waters) [[94], [96], [100], [102], [105], [106]]. Of special interest is the finding that a substantial proportion of bottled mineral waters contained caliciviral RNA [118], although these findings need to be confirmed by others.
Since projectile vomiting is a common feature following NLV infection and viruses can be present in vomit [[43], [119]], aerosolized vomit is recognized as an important vehicle for transmission, both by mechanical transmission from the vomit‐contaminated environment and even by airborne transmission [[97], [116], [117], [119], [120], [121], [122]]. The most compelling evidence for airborne transmission came from a study by Marks et al. [107]: they described an outbreak of gastroenteritis following a meal in a large hotel during which one of the guests vomited, and found an inverse relationship between attack rate per table and the distance from the person who got sick.
It is important to note that contamination may occur not only at the end of the food distribution chain, but at almost any step from farm to table. Foodborne illness associated with consumption of oysters has been traced back to a crewmember of a harvesting boat [104]. From that same outbreak investigation, it was reported that 85% of oyster‐harvesting boats in the area routinely disposed of sewage overboard. Little is known about the hygienic conditions in harvesting areas in other parts of the world, not only for shellfish, but also for products such as fresh fruits. Infected foodhandlers may transmit infectious viruses during the incubation period and after recovery from illness [[99], [109], [123]]. Another aspect of NLV epidemiology is that foodhandlers may unknowingly transmit viruses, e.g. when they have a sick child at home [98].
Besides person‐to‐person transmission via food vehicles, zoonotic transmission has been reported for some enteric viruses, although this appears to be of no significance for foodborne infections [124]. This may change, however, based on new data for NLV. Until recently, the NLV were considered to be pathogens with humans as the sole host. Recently, however, NLV were found in healthy pigs in Japan and in historic calf stool specimens from the UK and from Germany [[125], [126], [127], [128]]. The calf viruses, named Newbury agent and Jena virus, are pathogenic for young calves. The two bovine enteric caliciviruses and the pig enteric calicivirus are genetically distinct from human strains, but cluster within the NLV genus. In a pilot study in The Netherlands, pooled stool samples from calves, fattening pigs, and adult cows were tested for the presence of NLV [119]. Thirty‐three (45%) of the calf herds tested positive for a NLV strains belonging to one cluster, with highest homology with the Newbury genotype. The Netherlands calf viruses were sufficiently distinct to suggest that they may be a separate lineage (based on capsid sequencing). If confirmed, that implies that in calves also several lineages or genotypes of NLV cocirculate, and that zoonotic transmission cannot be excluded by finding distinct strains in animals and humans. In addition, one pig herd was found positive for a virus, which was very similar to the pig calicivirus from Japan [119]. These findings raise important questions on the host range of the NLV. At this stage the animal NLV appear to form genetically distinct stable lineages, but are sufficiently related to the human NLV to suggest that under the right conditions interspecies transmission could occur. Animal caliciviruses in another genus within the family Caliciviridae (the genus vesivirus) have a wide host range, and interspecies transmissions have repeatedly been documented [129].
3Foodborne hepatitis
3.1Introduction
The viruses which cause hepatitis can be divided into enterically transmitted viruses (HAV, HEV), and parenterally transmitted hepatitis viruses (hepatitis B, C, D, G). For food‐ or waterborne transmission, only the enterically transmitted viruses are relevant. HAV is a virus in the family Picornaviridae, to which the enteroviruses also belong (including poliovirus) [130]. HEV shows some resemblance with viruses from the family Caliciviridae (to which the NLV belong), but has not (yet) been included in a virus family because of unique characteristics [22].
Hepatitis E has only relatively recently been established as a cause of hepatitis, when large waterborne outbreaks occurred in India and Pakistan. The virus is endemic over a wide geographic area, primarily in countries with inadequate sanitation where HAV is endemic as well (south‐east Asia, Indian subcontinent, Africa), but not as widespread as HAV. In industrialized countries HEV infections are rare, and are usually travel‐related [[131], [132], [133]]. HEV outbreaks can be distinguished based on the higher attack rate of clinically evident disease in persons 15–40 years of age compared with other groups, higher overall case fatality rates (0.5–3%), and the unusually high death toll in pregnant women (15–20%). In younger age groups, the majority of people with symptoms due to HEV infection may present without jaundice, unlike those infected with HAV [[134], [135], [136]]. Since HEV can cause illness with high mortality in pregnant women, a study of foodborne virus transmission in our opinion should include HEV. The recent discovery that HEV is common in pigs and rats and that pig HEV have been found in humans is reason for a careful evaluation of HEV cases in countries where the virus is not endemic in the human population [[137], [138]]. However, the primary source for HEV infection appears to be fecally contaminated water, and few human cases have been reported in regions where pig HEV is endemic, suggesting that interspecies transmissions of HEV are not common in countries with high standards of living. The subsequent discussion will focus on HAV [[139], [140], [141]]. Since excellent reviews are available for HAV in general, the focus of this section will be mostly on the possibility of foodborne transmission [135].
3.2The virus
HAV are small, non‐enveloped spherical viruses, measuring between 27 and 32 nm in diameter. They contain a single (positive‐) stranded RNA genome of approximately 7.5 kb in length that encodes a large polyprotein [142]. The genome organization differs from that of the Caliciviridae, in that the genes encoding the non‐structural proteins are located at the 3′‐portion of the genome, and the genes encoding the structural proteins at the 5′‐end [143]. The polyprotein is processed to four structural and seven non‐structural proteins by proteinases encoded in and around the 3C region [144]. Replication efficiency seems to be controlled by amino acid substitutions in the 2B and 2C regions [145].
3.3Clinical symptoms
Infection with HAV can produce asymptomatic or symptomatic infection after a median incubation period of 30 days (range 15–50 days). The illness caused by HAV infection is characterized by non‐specific symptoms that can include fever, headache, fatigue, nausea and abdominal discomfort, followed by symptoms and signs of hepatitis 1–2 weeks later [134]. The likelihood of having symptoms with HAV infection is related to the age of the infected individual. Among children younger than 6 years of age, most infections are asymptomatic, and children with symptoms rarely develop jaundice. Among older children and adults, infection is usually symptomatic, and jaundice occurs in the majority of patients [[136], [146]].
The illness is generally self‐limited, lasting up to several months, and infrequently causes fulminant disease. All patients with hepatitis A in a 4‐year hospital‐ and physician‐based surveillance regained normal liver function within 20 months of the acute illness [134]. However, the case fatality rate among persons >50 years old with hepatitis A reported to the CDC in the USA is 1.8%[136]. Persons with chronic liver disease are at increased risk of fulminant hepatitis with hepatitis A [[147], [148], [149]]. HAV has not been shown to cause a persistent infection, and has not been associated with chronic liver disease. Prolonged or relapsing disease lasting up to 6 months occurs in 10–15% of patients [[150], [151], [152], [153]].
Peak virus shedding of HAV in feces occurs during the 2 weeks before the onset of jaundice or liver enzyme elevation. The concentration of virus in stool declines after jaundice appears, although prolonged shedding may occur, particularly among infants and children (reportedly up to 5 months post infection [[134], [136]]). Robertson et al. [154] found low levels of HAV RNA in stools from children for up to 10 weeks after the onset of symptoms. Reactivation of viral shedding can occur during relapsing illness. Viremia occurs soon after infection and persists through liver enzyme elevation. In a recent study, HAV RNA in serum was detected an average of 17 days before the alanine aminotransferase peak, and viremia persisted for an average of 79 days after the liver enzyme peak. The average duration of viremia was 95 days (range, 36–391 days) [150].
3.4Pathogenesis
The exact pathogenesis of hepatitis A is not understood. Virus enters via the intestinal tract, and is transported to the liver following a viremic stage, in which virus can be detected in the blood stream. Hepatocytes are the site of replication, and virus is thought to be shed via the bile. In experimental infections in non‐human primates, HAV viral antigen and/or genomic material has been found in the spleen, kidney, tonsils and saliva, suggesting that other sites of replication may exist. In vitro, cells are generally not destroyed by the virus, and the damage to liver epithelial cells in vivo often is limited [155].
3.5Diagnosis in humans
Hepatitis A cannot be distinguished from other types of viral hepatitis on the basis of clinical features [136]. Diagnosis of acute hepatitis A is made by detection in serum of IgM antibody to the capsid proteins of HAV (IgM anti‐HAV). In most persons with acute HAV infection, IgM anti‐HAV becomes detectable 5–10 days before the onset of symptoms and can persist for up to 6 months [156]. Commercial diagnostic tests are available for the detection of IgM and total (IgM and IgG) anti‐HAV in serum. Virus (up to 109 particles per ml) can be detected by molecular methods in stool and serum samples of infected individuals, but these methods are not generally used for diagnostic purposes [155]. Detection of sporadic cases or small clusters of foodborne hepatitis A is problematic because of difficulties in recalling exposures during the long incubation period, the simultaneous occurrence of cases from person‐to‐person transmission, and the lack of routinely collected data about foodborne exposures. For this, the use of molecular strain typing offers new possibilities (as described in Section 3.8).
3.6Epidemiology
Worldwide, differing patterns of HAV endemicity can be identified, each characterized by distinct patterns of the prevalence of antibody to HAV (anti‐HAV) and hepatitis A incidence, and associated with different levels of prevailing environmental (sanitary and hygienic) and socioeconomic conditions. In much of the developing world, HAV infection is endemic, and the majority of persons are infected in early childhood; virtually all adults are immune [136]. In these areas, HAV transmission is primarily from person to person. Outbreaks are rare because most infections occur among young children who generally remain asymptomatic. Paradoxically, as socioeconomic and environmental conditions improve and HAV decreases in endemicity (Fig. 2), the overall incidence and average age of reported cases often increase because older individuals are susceptible and develop symptoms with infection [157]. An illustration of this can been seen from national surveillance data: for instance in England and Wales, the annual notification rate of HAV infection has risen fourfold between 1987 and 1991 from 3.6 to 14.6 per 100 000 population [165]. In Italy, data collected from a surveillance system for type‐specific acute viral hepatitis (SEIEVA) showed that the incidence of HAV declined from 10/100 000 in 1985 to 2/100 000 during the period 1987–1990, while an increase was observed after 1991. The highest attack rate was observed in the 15–24‐year age group [158].
Figure 2.
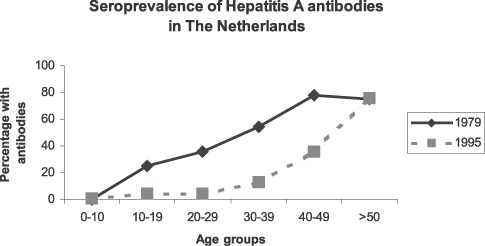
Seroprevalence of antibodies to HAV in The Netherlands in different age groups in 1979 and 1995. Data adapted from [[210], [211]].
Thus, in the industrialized parts of the world where HAV endemicity is relatively low, hepatitis A occurs sporadically and in the context of community‐wide epidemics that recur periodically [157]. Transmission remains primarily from person to person, but large common source outbreaks also can occur. Outbreaks of hepatitis A are common in crowded situations such as institutions, schools, prisons, and in military forces. The increased number of susceptible individuals allows common source epidemics to evolve rapidly, and the likelihood of such epidemics is increasing [136]. Foodborne outbreaks have been reported in most parts of the world except those with the highest and lowest HAV endemicity [[159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171]]. An outbreak in Shanghai in 1988 involving 250 000 cases occurred in association with consumption of contaminated clams [161]. In a recent outbreak in the USA, 213 persons developed hepatitis A after eating contaminated frozen strawberries that were distributed in school lunch programs [163]. In 1996 and 1997, a large HAV epidemic occurred in southern Italy, Puglia region, with 11 .000 notifications especially among young adults. The main risk factor in this epidemic outbreak was consumption of mussels [166]. A large HAV epidemic occurred in Finland among drug abusers (around 300 cases) due to contaminated amphetamine [[172], [173]]. In outbreak situations, up to 20% of cases are due to secondary transmission. Waterborne outbreaks are unusual, but have been reported in association with drinking fecally contaminated water and swimming in contaminated swimming pools and lakes [[136], [160]].
3.7Risk groups
In the developed world, groups at increased risk of HAV can be identified. In case–control studies in England and Italy, factors associated with increased risk of HAV included international travel to areas of intermediate or high HAV endemicity, a household contact with hepatitis A, sharing a household with a child aged 3–10 years, consumption of bivalve mollusks, and consumption of untreated water [165]. In Italy, shellfish consumption was the most frequently reported source of infection over the period considered [158]. In the USA, 25 000–35 000 cases are reported each year, of which approximately 12–25% can be attributed to household or sexual contact with a case. Other identified potential sources of infection include association with child care centers (11–16%) and international travel (4–6%). Although several food‐ and waterborne outbreaks of HAV have been described [[159], [160], [163], [167]], in the USA only 5% of reported cases occur in association with a recognized food‐ or waterborne outbreak [6]. However, approximately 50% of reported cases do not have a recognized source of infection. In many countries in the developed world, cyclic outbreaks have occurred among users of injection drugs and men who have sex with men [[173], [174]]. In The Netherlands, around 20% of HAV cases are related to international travel to high‐risk areas; in areas of very low endemicity such as Scandinavia, in many years international travel accounts for the majority of reported cases.
Since the case fatality rate of HAV infection increases with age, risks of more serious illness are higher for older age groups, provided they have not encountered HAV throughout their life [157]. Persons with hepatitis C infection and possibly those with chronic hepatitis B are at increased risk of fulminant hepatitis following superinfection with HAV [[147], [148], [149]].
3.8Molecular epidemiology
Molecular detection and typing assays have been developed for HAV [[163], [175], [177]]. These assays can detect HAV in stool and serum specimens from patients with hepatitis [[150], [177], [178]]. Seven genotypes of HAV have been recognized, four of which occur in humans. The other three genotypes have been found in captive Old World monkeys [179]. Genetically distinct lineages are found in different geographic regions and among patients in particular risk groups [[154], [173], [174], [176], [180], [181]]. The genetic diversity of HAV has been used to verify the occurrence of outbreaks including foodborne [[142], [153], [159], [163], [167], [169]] and waterborne outbreaks [160], and to link apparently sporadic cases to recognized foodborne and waterborne outbreaks [[167], [182]].
3.9Immunity
Only one serotype of HAV has been found so far, of which the antigenicity is determined by an immunodominant antigenic site [183]. A single HAV infection appears to induce lifelong immunity to the strains containing this epitope, but it remains to be seen if antigenic variants exist. IgM appears rapidly, with the majority of cases positive at 3 days post onset of symptoms [156]. Levels of IgM readily decline, and after 6 months 75% of patients have no detectable IgM antibodies left. IgG anti‐HAV begins to rise early in the course of infection and remains detectable for life, conferring protection against repeated HAV infection. Susceptibility to HAV infection can be determined using commercially available assays that detect IgM and total (IgG and IgM) antibody to HAV in serum.
3.10Modes of transmission
HAV is transmitted by the fecal–oral route, most often from person to person. This is exemplified by the high transmission rates among young children in developing countries, in areas where crowding is common and sanitation is poor, and in households and child care settings [[136], [155]]. Transmission also occurs from ingestion of contaminated food [[159], [161], [162], [163], [164], [165], [166], [168], [169], [170], [171]] and water [[136], [160]]. One report suggests the possibility of HAV infection via contaminated drinking glasses in a bar [184]. On rare occasions, HAV infection has been transmitted by transfusion of blood or blood products collected from donors during the viremic phase of infection, which appears to be much longer than was previously assumed [[150], [159], [177], [180], [185], [186]]. Although HAV has been detected in saliva of experimentally infected non‐human primates, transmission by saliva has not been demonstrated. A large outbreak among intravenous drug users in Finland was attributed to the possibility of fecal contamination of amphetamine associated with transportation of drugs in the gastrointestinal tract, which of course will be difficult to prove [172].
4General aspects
4.1High risk foodstuffs
Bivalve molluscan shellfish are notorious as a source of foodborne viral infections, because filter‐feeding shellfish can concentrate HAV up to 100‐fold from large volumes of water, allowing accumulation of virus from fecally contaminated water ([[95], [104], [110], [164], [166], [169], [187]]; for review see [188]). Depuration, a practice that may reduce bacterial contamination, is far less effective in reducing viral contamination. Quality control of food and water on the basis of the detection of indicator organisms for fecal contamination has proven to be an unreliable predictor of viral contamination [[187], [189]]. For shellfish, screening both of growing waters and of shellfish could be done, but the relative sensitivities of these approaches need to be evaluated.
Several other foods, however, have also been implicated as vehicles of transmission (desserts, fruits, vegetables, salads, sandwiches): the bottomline message is that any food that has been handled manually and not (sufficiently) heated subsequently is a possible source of infection [8]. It is important to note, however, that contamination may occur not only at the end of the food chain, but at almost every step in the path from farm to table.
Outbreaks associated with food, particularly raw produce, contaminated before reaching the food service establishment have been recognized increasingly in recent years [[74], [99], [159], [163], [168]]. This produce appears to have been contaminated during harvest, which could occur from handling by virus‐infected individuals. However, a better understanding of the precise mechanisms whereby viral contamination of raw produce occurs is needed to better focus prevention efforts in this area. Widespread transmission can occur when commercial facilities prepare food that is distributed to geographically distant locations. It is clear that some currently used industrial food processing methods will not sufficiently inactivate viruses if present in the foods before processing [190].
Recent studies with novel techniques show that infected foodhandlers may shed virus for longer periods of time [[42], [178]] and therefore may remain infectious even after full recovery [109]. Enteric viruses may persist for extended periods on materials that are commonly found in institutions and domestic environments (such as paper, cotton cloth, aluminum, china, glazed tiles, latex, and polystyrene [191]).
4.2Virus detection in food and water
Although diagnostic methods have been developed for the detection of virus or viral RNA in food and water, they have not found their way to routine laboratories in most parts of the world [[192], [193], [194], [195], [196], [197], [198], [199], [200], [201]]. Most studies of virus detection in food have focussed on shellfish, for which several groups have developed slightly different protocols, and comparative studies are needed to determine which assays should be recommended (reviewed in [188]). Recently, some methods were reported for virus detection in other foods, but their application in the field remains anecdotal [[202], [203]]. It remains unclear what the predictive value is of a negative test. This information is needed before screening of such specimens can be done to monitor contamination.
A special problem is that NLV cannot be grown in tissue culture, and HAV only with moderate success. As a result, data on the correlation between the presence of viral genes (as tested by RT‐PCR) and viable virus are lacking. Arnal et al. [204] assayed the stability of HAV in artificial sterile seawater by RT‐PCR and by cell culture. The HAV genome was detectable by RT‐PCR for 232 days while virus particles were detectable in cell culture for only 35 days, suggesting that detection of the HAV genome by RT‐PCR is not a reliable indicator of the presence of viable virus. Polish et al. [205] found that only stool specimens that were positive for HAV by ELISA were infectious for tamarins, suggesting that the viral load may be a determining factor of infectivity.
For outbreak diagnosis, the current approach is the screening of stool specimens from cases and controls, combined with an epidemiological investigation to assess food‐specific attack rates. Foods with a significant odds ratio may then be examined by molecular methods, although no information is available about the sensitivity of these methods for outbreak diagnosis and – in the case of HAV – implicated foods usually have been consumed or discarded by the time the outbreak is recognized due to the long incubation period. Therefore, the combination of epidemiological outbreak investigations and molecular strain typing provides a powerful tool to establish transmission routes.
4.3Prevention and disinfection
Increasing the awareness of all foodhandlers about transmission of enteric viruses is needed, with special emphasis on the risk of ‘silent’ transmission by asymptomatically infected persons and those continuing to shed virus following resolution of symptoms. While it may be unclear what proportion of foodborne infections can be attributed to workers in different parts of the food chain, it is important that viruses become part of science‐based hazard analysis and critical control point (HACCP) systems to identify risks and to help identify gaps in knowledge. At present, insufficient data are available to determine which steps are going to be critical for all foods. Preventive measures differ for the different transmission routes.
(i) Shellfish: for shellfish, strict control of the quality of growing waters can prevent contamination of shellfish. This includes control of waste disposal by commercial and recreational boats. Guidelines specifically aimed at reduction of viral contamination are needed, as it has become clear that the current indicators for water and shellfish quality are insufficient as predictors of viral contamination [[189], [199], [200], [201]].
(ii) Food items contaminated by infected foodhandlers: personal hygiene is most important in preventing foodborne viral infection, and includes frequent handwashing and wearing gloves. This should apply for all points in the food chain where foodstuffs are handled manually. The infectious dose of NLV appears to be extremely low [114]. As a result, even with strict sanitary measures, infection may not always be prevented. Foodborne outbreaks have occurred due to contaminated food sources that passed all microbiological assays. A common‐sense guideline is to remove people with symptoms consistent with viral gastroenteritis from the production chain until at least 2 days after remission of the symptoms. A practical problem with this guideline is that an unknown proportion of viral infections will be subclinical, viral shedding may last longer, and – even in the incubation period – infected persons may shed sufficient amounts of virus to cause food contamination [[42], [123], [171], [177], [178]]. The kinetics of viral shedding have only been studied in a few infected volunteers, and may not reflect the real‐life situation when people may have been infected with a low dose of infectious virus. Given the highly infectious nature of NLV and HAV, and the documented risk of virus transmission to food during the incubation period, it is envisioned that guidelines should be developed that consider the occurrence of gastroenteritis in contacts (e.g. children) of people working in critical points in the food chain. This should be based on data on the kinetics of viral shedding following natural infection. In addition to encouraging handwashing and other hygienic measures, policies involving ‘no bare hands contact’ by handlers of food that will be eaten without further cooking have been implemented in many areas. It is important to note that contamination can be particularly widespread after vomiting, due to aerosol formation and subsequent transport of virus particles by air.
The globalization of the food market has hampered the implementation of control measures to assure safe food. It is not clear whether routine monitoring of food specimens for viral contamination will be feasible. However, for prevention of foodborne transmission, it is also essential that food items are not grown or washed in fecally contaminated water.
Highly effective inactivated hepatitis A vaccines are available for use before exposure. To reduce the frequency with which foodhandlers with hepatitis A are identified, vaccination of foodhandlers has been advocated and implemented in some cities in the USA [185]. However, such policies have not been shown to be cost‐effective and generally are not recommended in the USA or other developed countries. Whether HAV vaccination is feasible for preventing foodborne transmission for specific countries or regions depends on many local factors (e.g. level of endemicity, hygienic conditions) and needs to be evaluated for these specific situations, based on HACCP analysis. Ig reportedly is more than 85% effective in preventing hepatitis A when given within 2 weeks of exposure [206]. In the USA, when a foodhandler is identified with hepatitis A, it is recommended that Ig be given to other foodhandlers at the establishment, and, under limited circumstances, to patrons. Once cases are identified that are associated with a food service establishment, it is generally too late to administer Ig to patrons, since the 2‐week period during which Ig is effective will have passed. This factor may explain some of the lack of success of Ig treatment as outbreak interventions [207].
HAV is resistant to low pH (up to pH 1) and to heating, surviving 1 h at 60°C [179]. It appears to be extremely stable in the environment, with only a 100‐fold decline in infectivity over 4 weeks at room temperature, and 3–10 months in water [[155], [190]]. HAV appears to be relatively resistant to free chlorine, especially when the virus is associated with organic matter. Heating foods (such as shellfish) to temperatures >85°C for 1 min and disinfecting surfaces with a 1:100 solution of sodium hypochlorite in tap water will inactivate HAV. Little is known about the stability of NLV outside the host, and infectivity can hardly be measured due to the absence of a cell culture system. From experiments with adult volunteers in the 1980s it has been suggested that NV is resistant to low pH (2.7), ether extraction, and heat treatment (30 min at 60°C) [26]. Steaming oysters may not prevent NLV gastroenteritis [208]. The virus reportedly is quite resistant to chlorine as remains infectious after 30 min in the presence of 0.5–1 mg free chlorine per liter. At higher concentrations, the virus is inactivated (>2 mg per liter free chlorine [26]). These findings have to be interpreted with caution, as data from recent dose–response studies makes it clear that very high doses of virus were used in earlier volunteer challenge experiments. Therefore, reduction of infectivity due to various treatments may not have been detected. Based on semiquantitative detection by using PCR units, drinking water treatment processes using coagulation–flocculation–sedimentation, filtration, and disinfection with free chlorine, monochloramine, ozone, chlorine dioxide or UV irradiation all reduce the amount of NV more than four log steps [209].
5Legislation, rules and regulations
Statutory sanitary control for shellfish relies on microbiological criteria to define the suitability of these products, as for instance in EU Council Directive 91/492/EC. This European directive establishes that microbial quality of shellfish should be monitored by measuring counts of total fecal coliform bacteria, Escherichia coli, and Salmonellae. The Directive establishes no specific microbiological criteria concerning the presence of enteric viruses, even though it has clearly been shown that there is no correlation between the presence of viruses and the presence of coliform bacteria and/or E. coli; in fact HAV, enteroviruses and NLV have been detected in mussels that otherwise meet bacteriological standards [[187], [188], [189], [199], [200]]. Similarly, it is not clear if and how depuration will reduce the levels of viral contaminants, especially for NLV, since quantitative methods for their detection are not yet available.
6Recommendations
To provide baseline data for future intervention and prevention programs, studies are needed to estimate the burden of illness and cost of illness due to foodborne viral infections with special emphasis on determining the burden of illness in the elderly. To enable this, better surveillance for illness is needed, as well as tools for molecular tracing of viruses throughout the food chain and through populations. Rapid methods for detection and typing of foodborne viruses should be developed and rapid exchange of typing information between laboratories and between countries should be encouraged. To enable this, current and newly developed methods need to be evaluated for comparability and need to be standardized. The feasibility of using these methods for food screening should be studied. The mechanism of emergence of epidemic strains should be studied, including the possible link with animal calicivirus infections.
Preventive measures directed at reduction of bacterial infections and general hygienic measures not always suffice to reduce viral infections and contamination. Studies are needed to evaluate if public campaigns directed at prevention of viral foodborne infections are likely to be successful. To reduce the risk of shellfish‐related foodborne outbreaks efforts should be made to maintain/improve the quality of growing waters. In order to achieve this, studies are needed that address the detection of viral contaminants, the effects of wastewater treatment on viral load, and the study of environmental factors that contribute to bioaccumulation and depuration of viruses. The use of sludge waste as fertilizer and of wastewater for irrigation should be evaluated for risks of viral contamination. Hepatitis A vaccination should be considered as part of the HACCP approach to reduce the risk of foodborne hepatitis A.
Given the high incidence of foodborne viral infections, it is time for a conscious effort to raise the awareness about the risk of foodborne transmission of viruses. Viruses should be included in all steps of the HACCP process. While the role of virus‐infected foodhandlers in transmission of NLV and HAV is well established, the risk of virus contamination is not limited to the final stages of the production process, and the potential role of infected harvesters or workers anywhere in the food chain should be considered. The food industry and the scientific community should work together in a joint effort to develop an integrated plan of action to address foodborne viral infections. This plan should identify both research priorities and strategies for implementation of the findings in HACCP systems.
7Conclusions
Although there are numerous fecal–orally transmitted viruses, the risk of foodborne transmission is highest for NLV and HAV. The ease of foodborne transmission can in part be attributed to the extreme stability of the viruses outside their host, and to the highly infectious nature. NLV and HAV can be transmitted from person to person, or indirectly via food, water, or fomites contaminated with virus‐containing feces or vomit. People can be infected without showing symptoms. The high frequency of secondary cases of NLV illness and – to a lesser extent – of hepatitis A following a foodborne outbreak results in amplification of the problem. The burden of illness is highest in the elderly, and is therefore likely to increase in the years to come due to the aging population. For HAV, the burden of illness may increase following hygienic control measures, due to a decreasing population of naturally immune individuals and a concurrent increase in the population at risk.
Recent advances in the research of NLV and HAV have led to the development of molecular methods which can be used for molecular tracing of virus strains. These methods can be and have been used for the detection of common source outbreaks. While traditionally certain foods have been implicated in virus outbreaks, it is clear that almost any food item can be involved, provided it has been handled by an infected person. There are no established methods for detection of viruses in foods other than shellfish, and current microbiological quality control relies on bacterial counts, which are not correlated with the presence of viruses. Little information is available on disinfection and preventive measures specifically for these viruses. Studies addressing this issue are hampered by the lack of culture systems. For HAV a vaccine is available, which confers full protection from illness.
Where does this leave us? Let's all face it: international foodborne viral outbreaks are an event waiting to happen, and may very well go unnoticed with the existing surveillance systems that focus almost exclusively on bacterial pathogens. Well‐standardized surveillance networks are needed that combine epidemiological and virological information for a combined laboratory‐based rapid detection system for foodborne viral outbreaks. With better surveillance, documented outbreaks of foodborne infections could be reported faster, in time to take preventive measures to stop further spread.
A concise version of this paper was discussed by the Codex Alimentarius, committee on food hygiene, 1999. FAO/WHO document CX/FH 99/11, Rome.
References
- [1]. Anon. (1995) Small round structured viruses (SRSV): numbers are increasing. Commun. Dis. Rep. CDR Wkly 5, 10. [PubMed]
- [2]. Motarjemi, Y., Käferstein, F., Moy, G., Miyagishima, K., Miyagawa, S. and Reilly, A. (1995) Food Technologies and Public Health. WHO/FNU/FOS/95.12, Rome.
- [3]. De Wit, M. , Koopmans, M. , Kortbeek, T. , van Leeuwen, W. , Bartelds, A. , van Duynhoven, Y. (2001) c Sensor: a population‐based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am. J. Publ. Health 154, 666–674. [DOI] [PubMed] [Google Scholar]
- [4]. Wheeler, J.G. , Sethi, D. , Cowden, J.M. , Wall, P.G. , Rodrigues, L.C. , Tompkins, D.S. , Hudson, M.J. , Roderick, P.J. (1999) Study of infectious intestinal disease in England: rates in the community, presenting to the general practitioner, and reported to national surveillance. Br. Med. J. 318, 1046–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Hedberg, C. , MacDonald, K. , Osterholm, M. (1994) Changing epidemiology of food‐borne disease: a Minnesota perspective. Clin. Infect. Dis. 18, 671–682. [DOI] [PubMed] [Google Scholar]
- [6]. Mead, P.S. , Slutsker, L. , Dietz, V. , McCaig, L.F. , Bresee, J.S. , Saphiro, C. et al. (1999) Food‐related illness and death in the United States. Emerg.Infect. Dis. 5, 607–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Roberts, T. , Unnevehr, L. (1994) New approaches to regulating food safety. Food Rev. 17, 2–8. [Google Scholar]
- [8]. Djuretic, T. , Wall, P.G. , Ryan, M. , Evans, H.S. , Adak, G.K. , Cowden, J.M. (1996) General outbreaks of infectious intestinal disease in England and Wales 1992 to 1994. CDR Rev. 6, R57–63. [PubMed] [Google Scholar]
- [9]. Vinjé, J. , Koopmans, M. (1996) Molecular detection and epidemiology of NLV in outbreaks of gastroenteritis in The Netherlands. J. Infect. Dis. 174, 610–615. [DOI] [PubMed] [Google Scholar]
- [10]. Vinjé, J. , Altena, S. , Koopmans, M. (1997) The incidence and genetic variability of small‐round‐structured viruses (SRSV) in outbreaks of gastroenteritis in The Netherlands. J. Infect. Dis. 176, 1374–1378. [DOI] [PubMed] [Google Scholar]
- [11]. Gangarosa, R.E. , Glass, R.I. , Lew, J.F. , Boring, J.R. (1992) Hospitalizations involving gastroenteritis in the United States, 1985: the special burden of the disease among the elderly. Am. J. Epidemiol. 135, 281–290. [DOI] [PubMed] [Google Scholar]
- [12]. Koopmans, M. (1997) Deaths asociated with outbreaks of gastroenteritis: an underestimated problem. Infect. Dis. Bull. (NL) 8, 251–252. [Google Scholar]
- [13]. Lew, J.F. , Glass, R.I. , Gangarosa, R.E. , Cohen, I.P. , Bern, C. , Moe, C.L. (1991) Diarrheal deaths in the United States 1979–1987. J. Am. Med. Assoc. 265, 3280–3284. [PubMed] [Google Scholar]
- [14]. Bern, C. , Lew, J. , McFeeley, P. , Ing, D. , Ing, R.T. , Glass, R.I. (1993) Diarrheal deaths in children living in New Mexico: toward a strategy of preventive interventions. J. Pediatr. 122, 920–922. [DOI] [PubMed] [Google Scholar]
- [15]. Bern, C. and Glass, R.I. (1994) Impact of diarrheal diseases worldwide. In: Viral Infections of the Gastrointestinal Tract, 2nd edn. (Kapikian, A.Z., Ed.), pp. 1–26. Marcel Dekker, New York.
- [16]. Blacklow, N.R. , Dolin, R. , Fedson, D.S. , DuPont, H. , Northrup, R.S. , Hornick, R.B. , Chanock, R.M. (1972) Acute infectious nonbacterial gastroenteritis: etiology and pathogenisis. A combined clinical staff conference at the Clinical Center of the National Institutes of Health. Ann. Intern. Med. 76, 993–1008. [DOI] [PubMed] [Google Scholar]
- [17]. Herrmann, J.E. , Nowak, N.A. , Perron‐Henry, D.M. , Hudson, R.W. , Cubitt, W.D. , Blacklow, N.R. (1990) Diagnosis of astrovirus gastroenteritis by antigen detection with monoclonal antibodies. J. Infect. Dis. 161, 226–229. [DOI] [PubMed] [Google Scholar]
- [18]. Kobayashi, S. , Sakae, K. , Natori, K. , Takeda, N. , Miyamura, T. , Suzuki, Y. (2000) Serotype‐specific antigen ELISA for detection of chiba virus in stools. J. Med. Virol. 62, 233–238. [DOI] [PubMed] [Google Scholar]
- [19]. Vipond, I.B. , Pelosi, E. , Williams, J. , Ashley, C. , Lambden, P. , Clarke, I. , Caul, O. (2000) A diagnostic EIA for detection of the prevalent SRSV strain in UK outbreaks of gastroenteritis. J. Med. Virol. 61, 132–137. [DOI] [PubMed] [Google Scholar]
- [20]. Kaplan, J.E. , Feldman, R. , Campbell, D.S. , Lookabaugh, C. , Gary, G.W. (1982) The frequency of a Norwalk‐like pattern of illness in outbreaks of acute gastro‐enteritis. Am. J. Publ. Health 72, 1329–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Hedberg, C.W. , Osterholm, M.T. (1993) Outbreaks of food‐borne and waterborne viral gastroenteritis. Clin. Microbiol. Rev. 6, 199–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Green, K. , Ando, T. , Balayan, M. , Berke, T. , Clarke, I. , Estes, M. , Matson, D. , Nakata, S. , Neill, J. , Studdert, M. , Thiel, H. (2000) Taxonomy of caliciviruses. J. Infect. Dis. 181, S322–330. [DOI] [PubMed] [Google Scholar]
- [23]. Jiang, X. , Graham, D.Y. , Wang, K.N. , Estes, M.K. (1990) Norwalk virus genome cloning and characterization. Science 250, 1580–1583. [DOI] [PubMed] [Google Scholar]
- [24]. Jiang, X. , Wang, M. , Wang, K. , Estes, M.K. (1993) Sequence and genomic organization of Norwalk virus. Virology 195, 51–61. [DOI] [PubMed] [Google Scholar]
- [25]. Rockx, B., de Wit, M., Vennema, H., Vinjé, J., de Bruin, E., van Duynhoven, Y. and Koopmans, M. (2002) Natural history of human calicivirus infection. Clin. Inf. Dis., in press. [DOI] [PubMed]
- [26]. Kapikian, A.Z., Estes, M.K. and Chanock, RM. (1996) Norwalk group of viruses. In: Fields Virology, 3rd edn., Vol 1 (Fields, B.N., Knipe, D.M., Howley, P.M., Chanock, R.M., Melnick, J.L., Monath, T.P., Roizman, B. and Straus, S.E., Eds.), pp. 783–810. Lippincott‐Raven, Philadelphia, PA.
- [27]. Kaplan, J.E. , Gary, G.W. , Baron, R.C. , Singh, N. , Schronberger, L.B. , Feldman, R. , Greenberg, H.B. (1982) Epidemiology of Norwalk gastroenteritis and the role of Norwalk virus in outbreaks of acute nonbacterial gastroenteritis. Ann. Intern. Med. 96, 756–761. [DOI] [PubMed] [Google Scholar]
- [28]. Low, A. , McNamara, M. , Schweiger, M.S. (1993) Foodborne viral gastroenteritis. Commun. Dis. Rep. CDR Rev. 3, R44–R46. [PubMed] [Google Scholar]
- [29]. Zahorsky, J. Hyperemesis hiemis or the winter vomiting disease,. Arch. Pediatr. 46, 1929. 391
- [30]. Kapikian, A.Z. , Wyatt, R.G. , Dolin, R. , Thornhill, T.S. , Kalica, A.R. , Chanock, R.M. (1972) Visualization by immune electron microscopy of a 27 nm particle associated with acute infections nonbacterial gastroenteritis. J. Virol. 10, 1075–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31]. Agus, S.G. , Dolin, R. , Wyatt, R.G. , Tousimis, A.J. , Northrup, R.S. (1973) Acute infectious nonbacterial gastroenteritis: intestinal histopathology. Histologic and enzymatic alterations during illness produced by the Norwalk agent in man. Ann. Intern. Med. 79, 18–25. [DOI] [PubMed] [Google Scholar]
- [32]. Schreiber, D.S. , Blacklow, N.R. , Trier, S. (1973) The mucosal lesion of the proximal small intestine in acute infectious nonbacterial gastroenteritis. New Engl. J. Med. 288, 1318–1323. [DOI] [PubMed] [Google Scholar]
- [33]. Dolin, R. , Blacklow, N.R. , DuPont, H. , Formal, S. , Buscho, R.F. , Kasel, J.A. , Chames, R.P. , Hornick, R. , Chanock, R.M. (1971) Transmission of acute infectious nonbacterial gastroenteritis to volunteers by oral adminstration of stool filtrates. J. Infect. Dis. 123, 307–312. [DOI] [PubMed] [Google Scholar]
- [34]. Wyatt, R.G. , Dolin, R. , Blacklow, N.R. , DuPont, H.L. , Buscho, R.F. , Thornhill, T.S. , Kapikian, A.Z. , Chanock, R.M. (1974) Comparison of three agents of acute infectious nonbacterial gastroenteritis by cross‐challenge in volunteers. J. Infect. Dis. 129, 709–714. [DOI] [PubMed] [Google Scholar]
- [35]. Madeley, C.R. , Cosgrove, B.P. (1975) 28 nm particles in faeces in infantile gastroenteritis. Lancet i, 451–452. [DOI] [PubMed] [Google Scholar]
- [36]. Madeley, C.R. (1979) Comparison of the features of astroviruses and caliciviruses seen in samples of faeces by electron microscopy. J. Infect. Dis. 139, 519–523. [DOI] [PubMed] [Google Scholar]
- [37]. Cubitt, W.D. , McSwiggan, D.A. , Moore, W. (1979) Winter vomiting disease caused by calicivirus. J. Clin. Pathol. 32, 786–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Cubitt, W.D. (1989) Diagnosis, occurrence and clinical significance of human ‘candidate’ caliciviruses. Prog. Med. Virol. 36, 103–119. [PubMed] [Google Scholar]
- [39]. Glass, P.J., White, L.J., Ball, J.M., LeParc‐Goffart, I., Hardy, M.E. and Estes, M.K. (1999) The Norwalk virus ORF3 encodes a minor structural protein. American Society for Virology, 18th Annual Meeting, University of Massachusetts, July 10–14, 1999, Abstract P21‐1.
- [40]. Arness, M. , Feighner, B. , Canham, M. , Taylor, D. , Monroe, S. , Cieslka, T. , Hoedebecke, E. , Polyak, C. , Cuthie, J. , Fankhauser, R. , Humphrey, C. , Barker, T. , Jenkins, C. , Skillman, D. (2000) NLV gastroenteritis outbreak in US army recruits. Emerg. Infect. Dis. 6, 204–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. Middleton, P.J. , Szymanski, M.T. , Petric, M. (1977) Viruses associated with acute gastroenteritis in young children. Am. J. Dis. Child. 131, 733–737. [DOI] [PubMed] [Google Scholar]
- [42]. Graham, D.Y. , Jiang, X. , Tanaka, T. , Opekun, A.R. , Madore, H.P. , Estes, M.K. (1994) Norwalk virus infection of volunteers: New insights based on improved assays. J. Infect. Dis. 170, 34–43. [DOI] [PubMed] [Google Scholar]
- [43]. Greenberg, H.B., Wyatt, R.G., Kapikian, A.Z. Norwalk virus in vomitus, letter,. Lancet. i, 1979. 55 [DOI] [PubMed]
- [44]. Bettelheim, K. , Bowden, D. , Doultree, J. , Catton, M. , Chibo, D. , Ryan, N. , Wright, P. , Gunesekere, I. , Griffith, J. , Lightfoot, D. , Hogg, G. , Bennett‐Wood, Y. , Marshall, J. (1999) Combined infection of NLV and VT producing bacteria associated with a gastroenteritis outbreak. J. Diarrh. Dis. Res. 17, 34–36. [PubMed] [Google Scholar]
- [45]. Schreiber, D.S. , Blacklow, N.R. , Trier, S. (1974) The mucosal lesion of the proximal small intestine in acute infectious nonbacterial gastroenteritis. J. Infect. Dis. 129, 705–708. [DOI] [PubMed] [Google Scholar]
- [46]. Rollo, E.E. , Kumar, K.P. , Reich, N.C. , Cohen, J. , Angel, J. , Greenberg, H.B. , Sheth, R. , Anderson, J. , Oh, B. , Hempson, S.J. , Mackow, E.R. , Shaw, R.D. (1999) The epithelial cell response to rotavirus infection. J. Immunol. 163, 4441–4452. [PubMed] [Google Scholar]
- [47]. Atmar, R. , Estes, M. (2001) Diagnosis of non‐cultivable gastroenteritis viruses, the human caliciviruses. Clin. Microbiol. Rev. 14, 15–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48]. Otsu, R. , Ishakawa, A. , Mukae, K. (2000) Detection of SRSV in stool specimens from outbreaks of gastroenteritis by EM and RT‐PCR. Acta Virol. 44, 53–55. [PubMed] [Google Scholar]
- [49]. Dingle, K.E. , Lambden, P.R. , Caul, E.O. , Clarke, I.N. (1995) Human enteric Caliciviridae: the complete genome sequence and expression of virus‐like particles from a genetic group II small round structured virus. J. Gen. Virol. 76, 2349–2355. [DOI] [PubMed] [Google Scholar]
- [50]. Lambden, P.R. , Caul, E.O. , Ashley, C.R. , Clarke, I.N. (1993) Sequence and genome organization of a human small round‐structured (Norwalk‐like) virus. Science 259, 516–519. [DOI] [PubMed] [Google Scholar]
- [51]. Lew, J.F. , Kapikian, A.Z. , Valdesuso, J. , Green, K.Y. (1994) Molecular characterization of Hawaii virus and other Norwalk‐like viruses: evidence for genetic polymorphism among human caliciviruses. J. Infect. Dis. 170, 535–542. [DOI] [PubMed] [Google Scholar]
- [52]. Lewis, D.C. (1990) Three serotypes of Norwalk‐like virus demonstrated by olid‐phase immune electron microscopy. J. Med. Virol. 30, 77–81. [DOI] [PubMed] [Google Scholar]
- [53]. Lewis, D. , Ando, T. , Humphrey, C.D. , Monroe, S.S. , Glass, R.I. (1995) Use of solid‐phase immune electron microscopy for classification of Norwalk‐like viruses into six antigenic groups from 10 outbreaks of gastroenteritis in the United States. J. Clin. Microbiol. 33, 501–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54]. Jiang, X. , Wang, J. , Graham, D.Y. , Estes, M.K. (1992) Detection of Norwalk virus in stool by polymerase chain reaction. J. Clin. Microbiol. 30, 2529–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55]. De Leon, R. , Matsui, S.M. , Baric, R.S. , Herrmann, J.E. , Blacklow, N.R. , Greenberg, H.B. , Sobsey, M.D. (1992) Detection of Norwalk virus in stool specimens by reverse transcriptase‐polymerase chain reaction and nonradioactive oligoprobes. J. Clin. Microbiol. 30, 3151–3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56]. Ando, T. , Mulders, M.N. , Lewis, D.C. , Estes, M.K. , Monroe, S.S. , Glass, R.I. (1994) Comparison of the polymerase region of small round structured virus strains previously classified in three antigenic types by solid‐phase immune electron microscopy. Arch. Virol. 135, 217–226. [DOI] [PubMed] [Google Scholar]
- [57]. Green, J. , Norcott, J.P. , Lewis, D. , Arnold, C. , Brown, D.W. (1993) Norwalk‐like viruses: demonstration of genomic diversity by polymerase chain reaction. J. Clin. Microbiol. 31, 3007–3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Wang, J. , Jiang, X. , Madore, H.P. , Gray, J. , Desselberger, U. , Ando, T. , Seto, Y. , Oishi, I. , Lew, J.F. , Green, K.Y. , Estes, M.K. (1994) Sequence diversity of small, round structured viruses in the Norwalk virus group. J. Virol. 68, 5982–5990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59]. Fankhauser, R.L. , Noel, J.S. , Monroe, S.S. , Ando, T.A. , Glass, R.I. (1998) Molecular epidemiology of small round structured viruses in outbreaks of gastroenteritis in the United States. J. Infect. Dis. 178, 1571–1578. [DOI] [PubMed] [Google Scholar]
- [60]. Noel, J.S. , Ando, T. , Leite, J.P. , Green, K.Y. , Dingle, K.E. , Estes, M.K. , Seto, Y. , Monroe, S.S. , Glass, R.I. (1997) Correlation of patient immune responses with genetically characterized small round‐structured viruses involved in outbreaks of nonbacterial acute gastroenteritis in the United States, 1990 to 1995. J. Med. Virol. 53, 372–383. [DOI] [PubMed] [Google Scholar]
- [61]. Green, K.Y. , Lew, J.F. , Jiang, X. , Kapikian, A.Z. , Estes, M.K. (1993) Comparison of the reactivities of baculovirus‐expressed recombinant Norwalk virus capsid antigen with those of the native Norwalk virus antigen in serologic assays and some epidemiologic observations. J. Clin. Microbiol. 31, 2185–2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62]. Jiang, X. , Zhong, W. , Kaplan, M. , Pickering, L. , Matson, D. (1998) Expression and characterization of Sapporo‐like human calicivirus capsid proteins in baculovirus. J. Virol. Methods 78, 81–91. [DOI] [PubMed] [Google Scholar]
- [63]. Jiang, X. , Wang, M. , Graham, D.Y. , Estes, M.K. (1992) Expression, self‐assembly, and antigenicity of the Norwalk virus capsid protein. J. Virol. 66, 6527–6532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64]. Jiang, X. , Matson, D.O. , Cubitt, W.D. , Estes, M.K. (1996) Genetic and antigenic diversity of human caliciviruses (HuCVs) using RT‐PCR and new EIAs. Arch. Virol. Suppl. 12, 251–262. [DOI] [PubMed] [Google Scholar]
- [65]. Jiang, X. , Wilton, N. , Zhong, W. , Farkas, T. , Huang, P. , Barrett, E. , Guerrero, M. , Ruiz‐Palacios, G. , Green, K. , Green, J. , Hale, A. , Estes, M. , Pickering, L. , Matson, D. (2000) Diagnosis of human caliciviruses by use of ELISA. J. Infect. Dis. 181, S349–359. [DOI] [PubMed] [Google Scholar]
- [66]. Hale, A. , Tanaka, T. , Kitamoto, N. , Ciarlett, M. , Jiang, X. , Takeda, N. , Brown, D. , Estes, M. (2000) Identification of an epitope common to genogroup I ‘Norwalk‐like viruses’. J. Clin. Microbiol. 38, 1656–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67]. Yoda, T. , Terano, Y. , Suzuki, Y. , Yamazaki, K. , Oishi, I. , Utagawa, E. , Shimada, A. , Matsuura, S. , Nakajima, M. , Shibata, T. (2000) Characterization of monoclonal antibodies generated against Norwalk virus GII capsid protein expressed in Escherichia coli. Microbiol. Immunol. 44, 905–914. [DOI] [PubMed] [Google Scholar]
- [68]. Koopmans, M. , Vinjé, J. , de Wit, M. , Leenen, I. , van der Poel, W. , van Duynhoven, Y. (2000) Molecular epidemiology of human enteric caliciviruses in The Netherlands. J. Infect. Dis. 181, S262–269. [DOI] [PubMed] [Google Scholar]
- [69]. Vennema, H. , Vinjé, J. , Wilbrink, B. , Koopmans, M. (2001) Etiology of outbreaks of viral gastro‐enteritis in 2000 in The Netherlands. Infect. Dis. Bull. 12, 33–38. [Google Scholar]
- [70]. McCarthy, M. , Estes, M. , Hyams, K. (2000) NLV infection in military forces: epidemic potential, sporadic disease, and the future direction of prevention and control efforts. J. Infect. Dis. 181, S387–391. [DOI] [PubMed] [Google Scholar]
- [71]. Hedlund, K. , Rubilar‐Abreu, E. , Svensson, L. (2000) Epidemiology of calicivirus infections in Sweden, 1994–8. J. Infect. Dis. 181, S275–280. [DOI] [PubMed] [Google Scholar]
- [72]. Traore, O. , Belliot, G. , Mollat, C. , Piloquet, H. , Chamoux, C. , Laveran, H. , Monroe, S. , Bilaudel, S. (2000) RT‐PCR identification and typing of astroviruses and NLV in hospitalised patients with gastroenteritis: evidence of nosocomial infections. J. Clin. Virol. 17, 151–158. [DOI] [PubMed] [Google Scholar]
- [73]. Maunula, L. , Piiparinen, H. , von Bonsdorff, C.‐H. (1999) Confirmation of Norwalk‐like virus amplicons after RT‐PCR by microplate hybridization and direct sequencing. J. Virol. Methods 83, 125–134. [DOI] [PubMed] [Google Scholar]
- [74]. Pönkä, A. , Maunula, L. , von Bonsdorff, C.‐H. , Lyytikäinen, O. (1999) Outbreak of calicivirus gastroenteritis associated with eating frozen raspberries. Eurosurveillance 4, 66–69. [DOI] [PubMed] [Google Scholar]
- [75]. Pang, X.L. , Joensuu, J. , Vesikari, T. (1999) Human calicivirus‐associated sporadic gastroenteritis in Finnish children less than two years of age followed prospectively during a rotavirus vaccine trial. Pediatr. Infect. Dis. J. 5, 420–426. [DOI] [PubMed] [Google Scholar]
- [76]. Sethi, D. , Wheeler, J.G. , Cowden, J.M. , Rodrigues, L.C. , Sockett, P.N. , Roberts, J.A. et al. (1999) A study of infectious intestinal disease in England: plan and methods of data collection. Commun. Dis. Publ. Health 2, 101–107. [PubMed] [Google Scholar]
- [77]. De Wit, M. , Koopmans, M. , Kortbeek, T. , van Leeuwen, W. , Bartelds, A. , van Duynhoven, Y. (2001) Gastroenteritis in sentinel practices in The Netherlands. Emerg. Infect. Dis. J. 7, 82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78]. De Wit, M.A.S. , Koopmans, M.P.G. , Kortbeek, T. , van Leeuwen, N. , Vinjé, J. , van Duynhoven, Y. (2001) Etiology of gastroenteritis in Sentinel general practices in the Netherlands. Clin. Infect. Dis. 33, 280–288. [DOI] [PubMed] [Google Scholar]
- [79]. Abbink, F., Duynhoven, Y., de Wit, M.A.S., Koopmans, M.P.G., van Leeuwen, W.J. and Kortbeek, L.M. (1998) A population cohort study with a nested case‐control study: a study design to estimate the incidence and aetiology of gastroenteritis in the Netherlands. Abstracts 4th World Congress on Foodborne Infections and Intoxications, Berlin, 171, P‐A032.
- [80]. Hoogenboom‐Verdegaal, A.M.M., During, M., Engels, G.B., Hoekstra, J.A., Leentvaar‐Kuypers, A., Peerbooms, P.G.H., Kooij, W.C.M., van Vlerken, R., Sobczak, H. Epidemiologisch en microbiologisch onderzoek met betrekking tot gastro‐enteritis bij de mens in de regio's Amsterdam en Helmond in 1987 en 1988,. RIVM Rapp. 148612, 1990. 002
- [81]. Bon, F. , Fascia, P. , Dauvergne, M. , Tenenbaum, D. , Planson, H. , Petion, A. , Pothier, P. , Kohli, E. (1999) Prevalence of group A rotavirus, human calicivirus, astrovirus, and adenovirus types 40 and 41 infections among children with acute gastroenteritis in Dijon, France. J. Clin. Microbiol. 37, 3055–3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82]. Farkas, T. , Jiang, X. , Guerrero, M. , Zhong, W. , Wilton, N. , Berke, T. , Matson, D. , Pickering, L. , Ruiz‐Palacios, G. (2000) Prevalence and genetic diversity of HuCVs in Mexican children. J. Med. Virol. 62, 217–223. [PubMed] [Google Scholar]
- [83]. Foley, B. , O'Mahoney, J. , Morgan, S. , Hill, C. , Morgan, J. (2000) Detection of NLV and astrovirus infection in a single Irish hospital from 1996 tot 1998. J. Clin. Virol. 17, 109–117. [DOI] [PubMed] [Google Scholar]
- [84]. Schnagl, R. , Barton, N. , Patrikis, M. , Tizzard, J. , Erlich, J. , Morey, F. (2000) Prevalence and genomic variation of NLV in central Australia in 1995–7. Acta Virol. 44, 265–271. [PubMed] [Google Scholar]
- [85]. Green, J. , Vinjé, J. , Gallimore, C. , Koopmans, M. , Hale, A. , Brown, D. (2000) Capsid protein diversity among small round structured viruses. Virus Genes 20, 227–236. [DOI] [PubMed] [Google Scholar]
- [86]. Gerba, C.P. , Rose, J.B. , Haas, C.N. (1996) Sensitive populations: who is at the greatest risk. Int. J. Food Microbiol. 30, 113–123. [DOI] [PubMed] [Google Scholar]
- [87]. Crowley, D.S. , Ryan, M.J. , Wall, P.G. (1997) Gastroenteritis in children under 5 years of age in England and Wales. Commun. Dis. Rep. CDR Rev. 7, R82–R86. [PubMed] [Google Scholar]
- [88]. Parashar, U.D. , Kilgore, P.E. , Holman, R.C. , Clarke, M.J. , Bresee, J.S. , Glass, R.I. (1998) Diarrheal mortality in US infants. Influence of birth weight on risk factors for death. Arch. Pediatr. Adolesc. Med. 152, 47–51. [DOI] [PubMed] [Google Scholar]
- [89]. Ando, T. , Noel, J. , Fankhauser, R. (2000) Genetic classification of ‘Norwalk‐like viruses’. J. Infect. Dis. 181, S336–S348. [DOI] [PubMed] [Google Scholar]
- [90]. Koopmans, M. (2001) Molecular epidemiology of caliciviruses. In: Viral gastroenteritis. Novartis Foundation Symposium Series 238, 197–214; discussion 214–218. [DOI] [PubMed]
- [91]. Greening, G.E. , Mirams, M. , Berke, T. (2001) Molecular epidemiology of NLV associated with gastroenteritis outbreaks in New Zealand. J. Med. Virol. 64, 58–66. [DOI] [PubMed] [Google Scholar]
- [92]. Parks, C. , Moe, C. , Rhodes, D. , Lima, A. , Barrett, L. , Tseng, F. , Baric, R. , Talal, A. , Guerrant, R. (1999) Genomic diversity of NLV: pediatric infections in a Brazilian shantytown. J. Med. Virol. 58, 426–434. [DOI] [PubMed] [Google Scholar]
- [93]. Schreier, E. , Doring, F. , Kunkel, U. (2000) Molecular epidemiology of outbreaks of gastroenteritis associated with small round structured viruses in Germany in 1997/98. Arch. Virol. 145, 443–453. [DOI] [PubMed] [Google Scholar]
- [94]. Beller, M. , Ellis, A. , Lee, S.H. , Drebot, M.A. , Jenkerson, S.A. , Funk, E. , Sobsey, M.D. Simmons O.D. III, Monroe, S.S. , Ando, T. , Noel, J. , Petric, M. , Middaugh, J.P. , Spika, J.S. (1997) Outbreak of viral gastroenteritis due to a contaminated well. International consequences. J. Am. Med. Assoc. 20, 563–568. [PubMed] [Google Scholar]
- [95]. Berg, D. , Kohn, M. , Farley, T. , McFarland, L. (2000) Multi‐state outbreaks of acute gastroenteritis traced to fecal‐contaminated oysters harvested in Louisiana. J. Infect. Dis. 181, S381–S386. [DOI] [PubMed] [Google Scholar]
- [96]. Brugha, R. , Vipond, I.B. , Evans, M.R. , Sandifer, Q.D. , Roberts, R.J. , Salmon, R.L. , Caul, E.O. , Mukerjee, A.K. (1999) A community outbreak of food‐borne small round‐structured virus gastroenteritis caused by a contaminated water supply. Epidemiol. Infect. 122, 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97]. Cheesbrough, J.S. , Green, J. , Gallimore, C. , Wright, P. , Brown, D. (2000) Widespread environmental contamination with NLV detected in a prolonged hotel outbreak of gastroenteritis. Epidemiol. Infect. 125, 93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98]. Daniels, N.A. , Bergmire‐Sweat, D. , Schwab, K. , Hendrikcks, K. , Reddy, S. , Rowe, S. , Fankhauser, R. , Monroe, S. , Atmar, R. , Glass, R. , Mead, P. (2000) A foodborne outbreak of gastroenteritis associated with NLV: first molecular traceback to deli sandwiches contaminated during preparation. J. Infect. Dis. 181, 1467–1470. [DOI] [PubMed] [Google Scholar]
- [99]. Gaulin, C.D. , Ramsay, D. , Cardinal, P. , D'Halevyn, M.A. (1999) Epidemic of gastroenteritis of viral origin associated with eating imported raspberries [in French]. Can. J. Publ. Health 90, 37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100]. Gray, J.J. , Green, J. , Cunliffe, C. , Gallimore, C. , L ee, J.V. , Neal, K. , Brown, D.W. (1997) Mixed genogroup SRSV infections among a party of canoeists exposed to contaminated recreational water. J. Med. Virol. 52, 425–429. [PubMed] [Google Scholar]
- [101]. Green, J. , Wright, P. , Gallimore, C. , Mitchell, O. , Morgan‐Capner, P. , Brown, D. (1998) The role of environmental contamination with small‐round structured viruses in a hospital outbreak investigated by RT‐PCR. J. Hosp. Infect. 39, 39–45. [DOI] [PubMed] [Google Scholar]
- [102]. Hafliger, D. , Hubner, P. , Luthy, J. (2000) Outbreak of viral gastroenteritis due to sewage‐contaminated drinking water. Int. J. Food Microbiol. 54, 123–126. [DOI] [PubMed] [Google Scholar]
- [103]. Iversen, A.M. , Gill, M. , Bartlett, C.L. , Cubitt, W.D. , McSwiggan, D.A. (1987) Two outbreaks of foodborne gastroenteritis caused by a small round structured virus: evidence of prolonged infectivity in a food handler. Lancet ii, 556–558. [DOI] [PubMed] [Google Scholar]
- [104]. Kohn, M. , Farley, T. , Ando, T. , Curtis, M. , Wilson, S. , Jin, Q. , Monroe, S. , Baron, R. , McFarland, L. , Glass, R. (1995) An outbreak of Norwalk virus gastroenteritis associated with eating raw oysters. J. Am. Med. Assoc. 273, 466–471. [DOI] [PubMed] [Google Scholar]
- [105]. Kukkula, M. , Arstila, P. , Klossner, M.L. , Maunula, L. , Bonsdorff, C.H. , Jaatinen, P. (1997) Waterborne outbreak of viral gastroenteritis. Scand. J. Infect. Dis. 29, 415–418. [DOI] [PubMed] [Google Scholar]
- [106]. Kukkula, M. , Maunula, L. , Silvennoinen, E. , von Bonsdorff, C.H. (1999) Outbreak of viral gastroenteritis due to drinking water contaminated by Norwalk‐like viruses. J. Infect. Dis. 180, 1771–1776. [DOI] [PubMed] [Google Scholar]
- [107]. Marks, P. , Vipond, I. , Varlisle, D. , Deakin, D. , Fey, R. , Caul, E. (2000) Evidence for airborne transmission of NLV in a hotel restaurant. Epidemiol. Infect. 124, 481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108]. Marshall, J.A. , Yuen, L.K. , Catton, M.G. , Gunesekere, I.C. , Wright, P.J. , Bettelheim, K.A. , Griffith, J.M. , Lightfoot, D. , Hogg, G.G. , Gregory, J. , Wilby, R. , Gaston, J. (2001) Multiple outbreaks of NLV gastroenteritis associated with a Mediterranean style restaurant. J. Med. Microbiol. 50, 143–151. [DOI] [PubMed] [Google Scholar]
- [109]. Parashar, U.D. , Dow, L. , Fankhauser, R.L. , Humphrey, C.D. , Miller, J. , Ando, T. , Williams, K.S. , Eddy, C.R. , Noel, J.S. , Ingram, T. , Bresee, J.S. , Monroe, S.S. , Glass, R.I. (1998) An outbreak of viral gastroenteritis associated with consumption of sandwiches: implications for the control of transmission by food handlers. Epidemiol. Infect. 121, 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110]. Sugieda, M. , Nakajima, K. , Nakajima, S. (1996) Outbreaks of Norwalk‐like virus‐associated gastroenteritis traced to shellfish: coexistence of two genotypes in one specimen. Epidemiol. Infect. 116, 339–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111]. Hale, A. , Mattick, K. , Lewis, D. , Estes, M. , Jiang, X. , Green, J. , Eglin, R. , Brown, D. (2000) Distinct epidemiological patterns of NLV infection. J. Med. Virol. 62, 99–103. [DOI] [PubMed] [Google Scholar]
- [112]. Iritani, N. , Seto, Y. , Haruki, K. , Kimura, M. , Ayata, M. , Ogura, H. (2000) Major changes in the predominant type of NLV in outbreaks of acute non‐bacterial gastroenteritis in Osaka City, Japan, between April 1996 and March 1999. J. Clin. Microbiol. 38, 2649–2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113]. Noel, J.S. , Fankhauser, R.L. , Ando, T. , Monroe, S.S. , Glass, R.I. (1999) Identification of a distinct common strain of ‘Norwalk‐like viruses’ having a global distribution. J. Infect. Dis. 179, 1334–1344. [DOI] [PubMed] [Google Scholar]
- [114]. Moe, C., Sobsey, M., Stewart, P. and Crawford‐Brown, D. (1999) Estimating the risk of human calicivirus infection from drinking water. Proc. 1st Int. Workshop on Human Caliciviruses, Atlanta, GA, pp. 4–6.
- [115]. Hinkula, J. , Ball, J.M. , Lofgren, S. , Estes, M.K. , Svensson, L. (1995) Antibody prevalence and immunoglobulin IgG subclass pattern to Norwalk virus in Sweden. J. Med. Virol. 47, 52–57. [DOI] [PubMed] [Google Scholar]
- [116]. Sawyer, L.A. , Murphy, J.J. , Kaplan, J.E. , Pinsky, P.F. , Chacon, D. , Walmsley, S. , Schronberger, L.B. , Philips, A. , Forward, K. , Goldman, C. , Brunton, J. , Fralick, R.A. , Carter, A.O. , Gary, G.W. , Glass, R.L. , Low, D.E. (1988) 25 to 30 nm virus particle associated with a hospital outbreak of acute gastroenteritis with evidence for airborne transmission. Am. J. Epidemiol. 127, 1261–1271. [DOI] [PubMed] [Google Scholar]
- [117]. Caul, E.O. (1994) Small round‐structured viruses – airborne transmission and hospital control. Lancet 343, 1240–1242. [DOI] [PubMed] [Google Scholar]
- [118]. Beuret, C. , Kohler, D. , Luthi, T. (2000) Norwalk‐like virus sequences detected by reverse transcription‐polymerase chain reaction in mineral waters imported into or bottled in Switzerland. J. Food Prot. 63, 1576–1582. [DOI] [PubMed] [Google Scholar]
- [119]. Patterson, W. , Haswell, P. , Fryers, P.T. , Green, J. (1997) Outbreak of small round structured virus gastroenteritis arose after kitchen assistant vomited. Commun. Dis. Rep. CDR Rev. 7, R101–103. [PubMed] [Google Scholar]
- [120]. Chadwick, P.R. , McCann, R. (1994) Transmission of a small round structured virus by vomiting during a hospital outbreak of gastroenteritis. J. Hosp. Infect. 26, 251–259. [DOI] [PubMed] [Google Scholar]
- [121]. Chadwick, P.R., Walker, M., Rees, A.E. Airborne transmission of a small round structured virus,. Lancet. ii, 1994. 1292 [DOI] [PubMed]
- [122]. Ho, M‐S. , Glass, R.I. , Monroe, S.S. , Madore, H.P. , Stine, S. , Pinsky, P.F. , Cubitt, W.D. , Ashley, C. , Caul, E.O. (1989) Viral gastroenteritis aboard a cruise ship. Lancet 2, 961–964. [DOI] [PubMed] [Google Scholar]
- [123]. Lo, S.V. , Connolly, A.M. , Palmer, S.R. , Wright, D. , Thomas, P.D. , Joynson, D. (1994) The role of the pre‐symptomatic food handler in a common source outbreak of food‐borne NLV gastroenteritis in a group of hospitals. Epidemiol. Infect. 113, 13–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124]. Glass, R.I. , Gentsch, J. , Smith, J.C. (1994) Rotavirus vaccines: success by reassortment. Science 265, 1389–1391. [DOI] [PubMed] [Google Scholar]
- [125]. Liu, B.L. , Clarke, I.N. , Caul, E.O. , Lambden, P.R. (1995) Human enteric caliciviruses have a unique genome structure and are distinct from the Norwalk‐like viruses. Arch. Virol. 140, 1345–1356. [DOI] [PubMed] [Google Scholar]
- [126]. Liu, B.L. , Lambden, P.R. , Gunther, H. , Otto, P. , Elschner, M. , Clarke, I.N. (1999) Molecular characterization of a bovine enteric calicivirus: relationship to the Norwalk‐like viruses. J. Virol. 73, 819–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127]. Sugieda, M. , Nagaoka, H. , Kakishima, Y. , Ohshita, T. , Nakamura, S. , Nakajima, S. (1998) Detection of Norwalk‐like virus genes in the caecum contents of pigs. Arch. Virol. 143, 1215–1221. [DOI] [PubMed] [Google Scholar]
- [128]. van der Poel, W. , Vinjé, J. , van der Heide, R. , Herrera, I. , Vivo, A. , Koopmans, M. (2000) Norwalk‐like calicivirus genes in farm animals. Emerg. Infect. Dis. 6, 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [129]. Smith, A., Skilling, D., Cherry, N., Mead, J., Matson, D. Emerg. Infect. Dis. 4, 1998. 3–20 [DOI] [PMC free article] [PubMed]
- [130]. Gust, I. , Coulepsis, A. , Feinstone, S. , Locarnini, S. , Moritsugu, Y. , Najera, R. , Siegl, G. (1983) Taxonomic classification of HAV. Intervirology 20, 1–7. [DOI] [PubMed] [Google Scholar]
- [131]. Lavanchy, D. , Morel, B. , Frei, P.C. (1994) Seroprevalence of hepatitis E virus in Switzerland. Lancet 344, 747–748. [DOI] [PubMed] [Google Scholar]
- [132]. Trautwein, C. , Kiral, G. , Tillmann, H.L. , Witteler, H. , Michel, G. , Manns, M.P. (1995) Risk factors and prevalence of hepatitis E in German immigrants from the former Soviet Union. J. Med. Virol. 45, 429–434. [DOI] [PubMed] [Google Scholar]
- [133]. Vandenvelde, C., Heyvaert, F., Maes, F., Kadi, L., Opstelten, R. Hepatitis E virus infection in Belgian soldiers,. Lancet. 344, 1994. 747 [DOI] [PubMed]
- [134]. Boughton, C.R. , Hawkes, R.A. , Schroeter, D.R. , Ferguson, V. , Lehmann, N.I. , Harlor, J. , Watson, V. , Cumpston, M. (1982) Viral hepatitis: a four‐year hospital and general‐practice study in Sydney 1. Epidemiological features, natural history, and laboratory findings. Med. J. Aust. 1, 113–119. [DOI] [PubMed] [Google Scholar]
- [135]. Cuthbert, J. (2001) Hepatitis A: old and new. Clin. Microbiol. Rev. 14, 38–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136]. Mast, E.E. , Alter, M.J. (1993) Epidemiology of viral hepatitis. Semin. Virol. 4, 273–283. [Google Scholar]
- [137]. Hsieh, S. , Meng, X. , Wu, Y. , Liu, S. , Tam, A. , Lin, D. , Liaw, Y. (1999) Identification of a novel HEV in Taiwan forming a monophyletic group with Taiwan isolates of human HEV. J. Clin. Microbiol. 37, 3828–3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138]. Kabrane‐Lazizi, Y. , Fine, J. , Elm, J. , Glass, G. , Higa, H. , Diwan, A. , Gibbs, C. , Meng, X. , Emerson, S. , Purcell, R. (1999) Evidence for widespread infection of wild rats with HEV in the USA. Am. J. Trop. Med. Hyg. 61, 331–335. [DOI] [PubMed] [Google Scholar]
- [139]. Meng, X.J. , Purcell, R.H. , Halbur, P.G. , Lehman, J.R. , Webb, D.M. , Tsareva, T.S. , Haynes, J.S. , Thacker, B.J. , Emerson, S.U. (1997) A novel virus in swine is closely related to the human hepatitis E virus. Proc. Natl. Acad. Sci. USA 94, 9860–9865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140]. Meng, X.J. , Halbur, P.G. , Shapiro, M.S. , Govindarajan, S. , Bruna, J.D. , Mushahwar, I.K. , Purcell, R.H. , Emerson, S.U. (1998) Genetic and experimental evidence for cross‐species infection by swine hepatitis E virus. J. Virol. 72, 9714–9721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141]. Meng, X. , Dea, S. , Engle, R. , Friendship, R. , Lyoo, Y. , Sirinarumitr, T. , Urairong, K. , Wang, D. , Wong, D. , Yoo, D. , Zhang, Y. , Purcell, R. , Emerson, S. (1999) Prevalence of antibodies to the HEV in pigs from countries where HEV is common or rare in the human population. J. Med. Virol. 59, 297–302. [PubMed] [Google Scholar]
- [142]. Najarian, R. , Caput, D. , Gee, W. , Potter, S.J. , Renard, A. , Merryweather, J. , Van Nest, G. , Dina, D. (1985) Primary structure and gene organization of human hepatitis A virus. Proc. Natl. Acad. Sci. USA 82, 2627–2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143]. Siegl, G. (1992) Replication of hepatitis A virus and processing of proteins. Vaccine 10 (Suppl. 1), S32–S35. [DOI] [PubMed] [Google Scholar]
- [144]. Probst, C. , Jecht, M. , Gauss‐Muller, V. (1998) Processing of proteinase precursors and their effect on hepatitis A virus particle formation. Virology 72, 8013–8020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145]. Yokosuka, O. (2000) Molecular biology of hepatitis A virus: significance of various substitutions in the hepatitis A virus genome. J. Gastroenterol. Hepatol. 15 (Suppl.), D91–D97. [DOI] [PubMed] [Google Scholar]
- [146]. Rosenblum, L.S. , Villarino, M.E. , Nainan, O.V. , Melish, M.E. , Hadler, S.C. , Pinsky, P.P. , Jarvis, W.R. , Ott, C.E. , Margolis, H.S. (1991) Hepatitis A outbreak in a neonatal intensive care unit: risk factors for transmission and evidence of prolonged viral excretion among preterm infants. J. Infect. Dis. 164, 476–482. [DOI] [PubMed] [Google Scholar]
- [147]. Keeffe, E.B. (1995) Is hepatitis A more severe in patients with chronic hepatitis B and other chronic liver diseases. Am. J. Gastroenterol. 90, 201–205. [PubMed] [Google Scholar]
- [148]. Lefilliatre, P. , Villeneuve, J.P. (2000) Fulminant hepatitis A in patients with chronic liver disease. Can. J. Publ. Health 91, 168–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149]. Vento, S. , Garofano, T. , Renzini, C. , Cainelli, F. , Casali, F. , Ghironzi, G. , Ferraro, T. , Concia, E. (1998) Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic hepatitis C. New Engl. J. Med. 338, 286–290. [DOI] [PubMed] [Google Scholar]
- [150]. Bower, W.A. , Nainan, O.V. , Han, X. , Margolis, H.S. (2000) Duration of viremia in hepatitis A virus infection. J. Infect. Dis. 182, 12–17. [DOI] [PubMed] [Google Scholar]
- [151]. Inoue, K. , Yoshiba, M. , Yotsuyanagi, H. , Otsuka, T. , Seliyama, K. , Fujita, R. (1996) Chronic hepatitis A with persistent viral replication. J. Med. Virol. 50, 322–324. [DOI] [PubMed] [Google Scholar]
- [152]. Siegl, G. , Weitz, M. (1993) Pathogenesis of hepatitis A: persistent viral infection as basis of an acute disease. Microb. Pathogen. 14, 1–8. [DOI] [PubMed] [Google Scholar]
- [153]. Sjogren, M.H. , Tanno, H. , Fay, O. , Sileoni, S. , Cohen, B.D. , Burke, D.S. , Feighny, R.J. (1987) Hepatitis A virus in stool during clinical relapse. Ann. Intern Med. 106, 221–226. [DOI] [PubMed] [Google Scholar]
- [154]. Robertson, B.H. , Averhoff, F. , Cromeans, T.L. , Han, Xh. , Khoprasert, B. , Nainan, O.V. , Rosenberg, J. , Paikoff, L. , DeBess, E. , Shapiro, C.N. , Margolis, H.S. (2000) Genetic relatedness of hepatitis A virus isolates during a community‐wide outbreak. J. Med. Virol. 62, 144–150. [PubMed] [Google Scholar]
- [155]. Hollinger, F. and Ticehurst, J. (1996) Hepatitis A virus. In: Fields Virology (Fields, B.N., Knipe, D.M., Howley, P. et al., Eds.), pp. 735–782. Lippincott‐Raven, Philadelphia, PA.
- [156]. Liaw, Y.F. , Yang, C.Y. , Chu, C.M. , Huang, M.J. (1986) Appearance and persistence of hepatitis A IgM antibody in acute clinical hepatitis A observed in an outbreak. Infection 14, 156–158. [DOI] [PubMed] [Google Scholar]
- [157]. Forbes, A. , Williams, R. (1990) Changing epidemiology and clinical aspects of hepatitis A. Br. Med. Bull. 46, 303–318. [DOI] [PubMed] [Google Scholar]
- [158]. Mele, A., Stroffolini, T., Palumbo, F., Gallo, G., Ragni, P., Balocchini, E., Tosti, M.E., Corona, R., Marzolini, A., Moiraghi, A. and the SEIEVA Collaborating Group (1997) Incidence and risk factor for hepatitis A in Italy: public health indications from a 10‐year surveillance. J. Hepatol. 26, 743–747. [DOI] [PubMed]
- [159]. CDC (1997) Hepatitis A associated with consumption of frozen strawberries‐Michigan, March 1997. J. Am. Med. Assoc. 277, 1271. [PubMed]
- [160]. De Serres, G. , Cromeans, T.L. , Levesque, B. , Brassard, N. , Barthe, C. , Dionne, M. , Prud’homme, H. , Paradis, D. , Shapiro, C.N. , Nainan, O.V. , Margolis, H.S. (1999) Molecular confirmation of hepatitis A virus from well water: epidemiology and public health implications. J. Infect. Dis. 179, 37–43. [DOI] [PubMed] [Google Scholar]
- [161]. Halliday, M.L. , Kang, L.Y. , Zhou, T.K. , Hu, M.D. , Pan, Q.C. , Fu, T.Y. , Huang, Y.S. , Hu, S.L. (1991) An epidemic of hepatitis A attributable to the ingestion of raw clams in Shanghai, China. J. Infect. Dis. 164, 852–859. [DOI] [PubMed] [Google Scholar]
- [162]. Hemmer, R. and Hansen‐Koenig, D. (2000) Outbreak of hepatitis A in Luxembourg. Eurosurveill. Wkly 33, http://www.eurosurv.org/update/.
- [163]. Hutin, Y.J. , Pool, V. , Cramer, E.H. , Nainan, O.V. , Weth, J. , Williams, I.T. , Goldstein, S.T. , Gensheimer, K.F. , Bell, B.P. , Shapiro, C.N. , Alter, M.J. , Margolis, H.S. (1999) A multistate, foodborne outbreak of hepatitis A. National Hepatitis A Investigation Team. New Engl. J. Med. 340, 595–602. [DOI] [PubMed] [Google Scholar]
- [164]. Leoni, E. , Bevini, C. , Degli Esposti, S. , Graziano, A. (1998) An outbreak of intrafamiliar hepatitis A associated with clam consumption: epidemic transmission to a school community. Eur. J. Epidemiol. 14, 187–192. [DOI] [PubMed] [Google Scholar]
- [165]. Maguire, H.C. , Handford, S. , Perry, K.R. , Nicholas, S. , Waight, P. , Parry, J.V. , O'Mahoney, M. , Begg, N.T. (1995) A collaborative case control study of sporadic hepatitis A in England. CDR Rev. 5, R33–R40. [PubMed] [Google Scholar]
- [166]. Malfait, P., Lopalco, P.L., Salmaso, S., Quarto, M., Barbuti, S. Eurosurveillance. 5, 1996. 33–35
- [167]. Massoudi, M.S. , Bell, B.P. , Paredes, V. , Insko, J. , Evans, K. , Shapiro, C.N. (1999) An outbreak of hepatitis A associated with an infected foodhandler. Publ. Health Rep. 114, 157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168]. Niu, M.T. , Polish, L.B. , Robertson, B.H. , Khanna, B.K. , Woodruff, B.A. , Shapiro, C.N. , Miller, M.A. , Smith, J.D. , Gedrose, J.K. , Alter, M.J. et al. (1992) Multistate outbreak of hepatitis A associated with frozen strawberries. J. Infect. Dis. 166, 518–524. [DOI] [PubMed] [Google Scholar]
- [169]. Normann, A. , Pfisterer‐Hunt, M. , Schade, S. , Graff, J. , Chaves, R. , Crovari, P. , Icardi, G. , Flehmig, B. (1995) Molecular epidemiology of an outbreak of HAV in Italy. J. Med. Virol. 47, 467–471. [DOI] [PubMed] [Google Scholar]
- [170]. Reid, T. , Robinson, H. (1987) Frozen raspberries and HAV. Epidemiol. Infect. 98, 109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171]. Skala, M. , Collier, C. , Hinkle, C.J. , Donnell, H.D. (1993) Foodborne hepatitis A – Missouri, Wisconsin, and Alaska, 1990–1992. MMWR 42, 526–529. [PubMed] [Google Scholar]
- [172]. Leino, T. , Leinikki, P. , Hyypia, T. , Ristola, M. , Suni, J. , Sutinen, J. , Holopainen, A. , Haikala, O. , Yalle, M. , Rostilla, T. (1997) HAV outbreak amongst IV amphetamine abusers in Finland. Scand. J. Infect. Dis. 29, 213–216. [DOI] [PubMed] [Google Scholar]
- [173]. Stene‐Johansen, K. , Skaug, K. , Blystad, H. , Grinde, B. (1998) A unique HAV strain caused an epidemic in Norway associated with IV drug abuse. Scand. J. Infect. Dis. 30, 35–38. [DOI] [PubMed] [Google Scholar]
- [174]. Bruisten, S.M. , van Steenbergen, J.E. , Pijl, A.S. , Niesters, H.G.M. , van Doornum, G.J.J. , Coutinho, R.A. (2001) Molecular epidemiology of hepatitis A virus in the Netherlands. J. Med. Virol. 63, 88–95. [PubMed] [Google Scholar]
- [175]. Birkenmeyer, L.G. , Mushahwar, I.K. (1994) Detection of hepatitis A, B and D virus by the polymerase chain reaction. J. Virol. Methods 49, 101–112. [DOI] [PubMed] [Google Scholar]
- [176]. Robertson, B.H. , Jansen, R.W. , Khanna, B. , Totsuka, A. , Nainan, O.V. , Siegl, G. , Widell, A. , Margolis, H.S. , Isomura, S. , Ito, K. et al. (1992) Genetic relatedness of hepatitis A virus strains recovered from different geographical regions. J. Gen. Virol. 73, 1365–1377. [DOI] [PubMed] [Google Scholar]
- [177]. Yotsuyanagi, H., Iino, S., Koike, K., Yasuda, K., Hino, K. and Kurokawa, K. (1993) Duration of viremia in human hepatitis A viral infection as determined by polymerase chain reaction. J. Med. Virol. 4035–4038. [DOI] [PubMed]
- [178]. Yotsuyanagi, H. , Koike, K. , Yasuda, K. , Moriya, K. , Shintani, Y. , Fujie, H. , Kurokawa, K. , Iino, S. (1996) Prolonged fecal excretion of hepatitis A virus in adult patients with hepatitis A as determined by polymerase chain reaction. Hepatology 24, 10–13. [DOI] [PubMed] [Google Scholar]
- [179]. Lemon, S.M. , Jansen, R.W. , Brown, E.A. (1992) Genetic, antigenic and biological differences between strains of hepatitis A virus. Vaccine 10 (Suppl. 1), 40–44. [DOI] [PubMed] [Google Scholar]
- [180]. Robertson, B.H. , Friedberg, D. , Normann, A. , Graff, J. , Flehmig, B. , Shouval, D. (1994) Sequence variability of hepatitis A virus and factor VIII associated hepatitis A infections in hemophilia patients in Europe. An update. Vox Sang. 67 (Suppl. 1), 39–45. [PubMed] [Google Scholar]
- [181]. Taylor, D. (1997) Molecular epidemiology of South African strains of hepatitis A virus: 1982–1996. J. Med. Virol. 51, 273–299. [DOI] [PubMed] [Google Scholar]
- [182]. Hutin, Y.J. , Bell, B.P. , Marshall, K.L. , Schaben, C.P. , Dart, M. , Quinlisk, M.P. , Shapiro, C.N. (1999) Identifying target groups for a potential vaccination program during a hepatitis A communitywide outbreak. Am. J. Publ. Health 89, 918–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183]. Ping, L. , Lemon, S. (1992) Antigenic structure of human HAV defined by analysis of escape mutants selected against murine monoclonal antibodies. J. Virol. 66, 2208–2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184]. Sundkvist, T. , Hamilton, G. , Hourihan, B. , Hart, J. (2000) Outbreak of HAV spread by contaminated drinking glasses in a public house. Commun. Dis. Publ. Health 3, 60–62. [PubMed] [Google Scholar]
- [185]. ACIP (1996) Prevention of hepatitis A through active or passive immunization. Recommendations of the advisory committee on immunization practices. MMWR 45/RR‐15, 1–30. [PubMed]
- [186]. Fujiwara, K. , Yokosuka, O. , Ehata, T. , Imazeki, F. , Saisho, H. , Miki, M. , Omata, M. (1997) Frequent detection of HAV RNA in serum during the early convalescent phase of acute hepatitis A. Hepatology 26, 1634–1639. [DOI] [PubMed] [Google Scholar]
- [187]. LeGuyader, F. , Miossec, L. , Haugarreau, L. , Dubois, E. , Kopecka, H. , Pommepuy, M. (1998) RT‐PCR evaluation of viral contamination in fibe shellfish beds over a 21‐month period. Water Sci. Technol. 2, 45–50. [Google Scholar]
- [188]. Lees, D. (2000) Viruses and bivalve shellfish. Int. J. Food Microbiol. 59, 81–116. [DOI] [PubMed] [Google Scholar]
- [189]. Croci, L. , De Medici, D. , Scalfaro, C. , Fiore, A. , Divizia, M. , Donia, D. , Cosentino, A.M. , Moretti, P. , Costantini, G. (2000) Determination of enterovirus, hepatitis A virus; bacteriophages and E. coli in Adriatic sea mussels. J. Appl. Microbiol. 88, 293–296. [DOI] [PubMed] [Google Scholar]
- [190]. Koopmans, M. and Duizer, E. (2001) Foodborne Viruses: An emerging problem? Monograph (in press). ILSI Press. [DOI] [PMC free article] [PubMed]
- [191]. Abad, F.X. , Pinto, R. , Bosch, A. (1994) Survival of enteric viruses on environmental fomites. Appl. Environ. Microbiol. 60, 3704–3710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192]. Atmar, R.L. , Metcalf, T. , Neill, F. , Estes, M. (1993) Detection of enteric viruses in oysters by using PCR. Appl. Environ. Microbiol. 59, 631–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193]. Atmar, R.L. , Neill, F.H. , Romalde, J.L. , LeGuyader, F. , Woodley, C.M. , Metcalf, T.G. , Estes, M. (1995) Detection of Norwalk virus and hepatitis A Virus in shellfish tissues with the PCR. Appl. Environ. Microbiol. 61, 3014–3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194]. Gajardo, R. , Dmez, J.M. , Jofre, J. , Bosch, A. (1991) Adsorption‐elution with negatively and positively charged glass powder for the concentration of hepatitis A virus from water. J. Virol. Methods 31, 345–352. [DOI] [PubMed] [Google Scholar]
- [195]. Gilgen, M. , German, D. , Lüthy, J. , Hübner, P. (1997) Three‐step isolation method for sensitive detection of enterovirus, rotavirus, hepatitis A virus and small round structured viruses in water samples. Int. J. Food Microbiol. 37, 189–199. [DOI] [PubMed] [Google Scholar]
- [196]. Gouvea, V. , Santos, N. , Carmo Timenetsky, M. , Estes, M. (1994) Identification of Norwalk virus in artificially seeded shellfish and selected foods. J. Virol. Methods 48, 177–187. [DOI] [PubMed] [Google Scholar]
- [197]. Jehl‐Pietri, C.H. , Hugues, B. , Andri, M. , Diez, J.M. , Bosch, A. (1993) Comparison of immunological and molecular hybridization detection methods for demonstration of hepatitis A virus in sewage. Lett. Appl. Microbiol. 17, 162–166. [DOI] [PubMed] [Google Scholar]
- [198]. Lees, D.N. , Henshilwood, K. , Dore, W. (1994) Development of a method for detection of enteroviruses in shellfish by PCR with poliovirus as a model. Appl. Environ. Microbiol. 60, 2999–3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [199]. LeGuyader, F. , Apaire‐Marchais, V. , Brillet, J. , Billaudel, S. (1993) Use of genomic probes to detect hepatitis A virus and enterovirus RNAs in wild shellfish and relationships of viral contamination to bacterial contamination. Appl. Environ. Microbiol. 59, 3963–3968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200]. LeGuyader, F. , Dubois, E. , Menard, D. , Pommepuy, M. (1994) Detection of hepatitis A virus, rotavirus, and enterovirus in naturally contaminated shellfish and sediment by RT‐PCR. Appl. Environ. Microbiol. 60, 3665–3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201]. LeGuyader, F.A. , Estes, M.K. , Hardy, M.E. , Neill, F.H. , Green, J. , Brown, D.W. , Atmar, R.L. (1996) Evaluation of a degenerate primer for the PCR detection of human caliciviruses. Arch. Virol. 141, 2225–2235. [DOI] [PubMed] [Google Scholar]
- [202]. Bidawid, S. , Farber, J. , Sattar, S. (2000) Rapid concentration and detection of HAV from lettuce and strawberries. J. Virol. Methods 88, 175–185. [DOI] [PubMed] [Google Scholar]
- [203]. Schwab, K. , Neill, F. , Fankhauser, R. , Daniels, N. , Monroe, S. , Bergmire‐Sweat, D. , Estes, M. , Atmar, R. (2000) Development of methods to detect NLV and HAV in delicatessen foods: application to a foodborne NLV outbreak. Appl. Environ. Microbiol. 66, 213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204]. Arnal, C. , Crance, J.M. , Gantzer, C. , Schwartzbrod, L. , Deloince, R. , Billaudel, S. (1998) Persistence of infectious hepatitis A virus and its genome in artificial seawater. Zent.bl. Hyg. Umweltmed. 201, 279–284. [PubMed] [Google Scholar]
- [205]. Polish, L. , Robertson, B. , Khanna, B. , Krwczynski, K. , Spelbring, J. , Olson, F. , Shapiro, C. (1999) Excretion of HAV in adults: comparison of immunologic and molecular detection methods and relationship between HAV positivity and infectivity in tamarins. J. Clin. Microbiol. 37, 3615–3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206]. Anon. (1999) Hepatitis A vaccine: evidence of efficacy after exposure. Commun. Dis. Rep. CDR Wkly 9, 139, 142. [PubMed]
- [207]. Aszkenasy, O.M. (2000) A community outbreak of hepatitis A in a religious community in Indiana: failure of immune serum globulin to prevent the spread of infection. Epidemiol. Infect. 124, 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208]. Kirkland, K. , Meriwether, R. , Leiss, J. , McKenzie, W. (1996) Steaming oysters does not prevent NLV gastroenteritis. Publ. Health Rep. 111, 527–530. [PMC free article] [PubMed] [Google Scholar]
- [209]. Sobsey, M., Shin, G.‐A., Battigelli, D. and Newland, S. (1999) Reduction of Norwalk virus by drinking water treatment processes. Proc. 1st Int. Workshop on Human Caliciviruses, Atlanta, GA, P4‐3.
- [210]. Frösner, G. , Papaevangelou, G. , Butler, R. , Iwarson, S. , Lindholm, A. , Courouce‐Pauty, A. , Haas, H. , Deinhardt, F. (1979) Antibody against hepatitis A in seven European countries. Am. J. Epidemiol. 110, 63–69. [DOI] [PubMed] [Google Scholar]
- [211]. de Melker, H., van der Peet, T., Berbers, G., van de Akker, R., van Knapen, F., Schellekens, J. and Conyn‐van Spaendonck, M. (1998) Pilot‐study for the PIENTER project: seroprevalence of mumps, measles, rubella, Bordetella pertussis, Toxoplasma gondii, Trichinella spiralis, and hepatitis A [in Dutch]. RIVM Report 213675004.


