Abstract
During the 16th century, Mexico suffered a demographic catastrophe with few parallels in world's history. In 1519, the year of the arrival of the Spaniards, the population in Mexico was estimated to be between 15 and 30 million inhabitants. Eighty‐one years later, in 1600, only two million remained. Epidemics (smallpox, measles, mumps), together with war, and famine have been considered to be the main causes of this enormous population loss. However, re‐evaluation of historical data suggests that approximately 60–70% of the death toll was caused by a series of epidemics of hemorrhagic fevers of unknown origin. In order to estimate the impact of the 1576 epidemic of hemorrhagic fevers on the population we analyzed the historical record and data from the 1570 and 1580 censuses of 157 districts. The results identified several remarkable aspects of this epidemic: First, overall, the population loss for these 157 districts was 51.36%. Second, there was a clear ethnic preference of the disease, the Spanish population was minimally affected whereas native population had high mortality rate. Third, the outbreak originated in the valleys of central Mexico whence it evolved as an expansive wave. Fourth, a positive correlation between altitude and mortality in central Mexico was found. Fifth, a specific climatic sequence of events was associated with the initiation and dissemination of the hemorrhagic fevers. Although the last epidemic of hemorrhagic fevers in Mexico ended in 1815, many questions remain to be answered. Perhaps the most relevant ones are whether there is a possible reemergence of the hemorrhagic fevers and how vulnerable we are to the disease.
Keywords: Hemorrhagic fevers, Mexico, Epidemics
1Introduction
During the 16th century Mexico suffered a demographic catastrophe with few parallels in world history. In 1519, the year of the arrival of the Spaniards, the Mexican population was estimated to be between 15 and 30 million inhabitants. Eighty‐one years later, in 1600, only two million people lived in the country [[1], [2], [3], [4], [5]]. Epidemics (smallpox, measles, mumps), together with war, and famine have been considered to be the main causes of this enormous population loss [[6], [7], [8]]. However, approximately 60–70% of the death toll registered during this period was caused by a series of epidemics of hemorrhagic fevers of unknown origin. The disease, called cocoliztli, appeared for the first time in 1545 and in three years, it killed an estimated 5–15 million people, or up to 80% of the native population at the time. This represents the worst epidemic in recorded Mexican history [[9], [10]]. Other major cocoliztli epidemics were those of 1576, 1736 and 1813. Lesser outbreaks were registered in 1559, 1566, 1587, 1592, 1601, 1604, 1606, 1613, 1624, and 1642. During the seventeenth, eighteenth and nineteenth centuries, cocoliztli was known as “matlazahuatl”. The last epidemic of hemorrhagic fevers in Mexico ended in 1815 [[10], [11], [12]].
The second major cocoliztli epidemic started in 1576. Fortunately, the effects of this epidemic were documented by two nationwide censuses, one performed in 1570, six years before the epidemic, and another between 1579 and 1580, two years after the epidemic [[3], [5], [11]]. This review has three purposes: First, to compile and restate the information about the epidemic of 1576 from first hand testimonies scattered among numerous historical documents. Second, to analyze the available quantitative data on this epidemic. Third, to describe some new proxy information on the climatological conditions associated with the cocoliztli epidemic of 1576.
2The disease
Cocoliztli, from the Nahuatl: pest [13], was a disease unknown to Indian or Spanish physicians before 1545. A consensus description based exclusively on first hand witnesses is the following: The disease had a very short course, lasting three to five days. It started abruptly with high fever, vertigo, severe headache, insatiable thirst, red eyes and weak pulse. Patients became intensely jaundiced, very anxious, demented and restless. They did not tolerate any blanket over their skin. Subsequently, hard painful nodules appeared behind one or both ears, sometimes so large that they occupied the entire neck and half of the face. When these nodules were punctured, they drained purulent material. Intense chest and abdominal pain and dysentery, ulcers in lips and genitals accompanied this. Blood then flowed from the ears, anus, vagina, mouth and nose. The presence of abdominal distention or darkening of the urine were symptoms of bad prognosis. Some autopsies were performed and the reports described a very enlarged and hard liver, lung hemorrhage and splenomegaly. Reportedly, none of the physicians that did those bare‐hand autopsies acquired the disease. The disease was almost inevitably fatal among for the Indian population. In contrast, the Spaniards were minimally affected, and when they occasionally acquired the disease, it had a benign course. Cocoliztli had some degree of polymorphism; fever and jaundice were always present but other manifestations had a variable frequency and intensity. Survivors were left extremely thin and weak, relapses were common. Domestic animals were unaffected [[14], [15], [16], [17], [18], [19], [20], [21], [22]].
3The epidemic of 1576
The cocoliztli epidemic of 1576 evolved as an expansive wave originating in the valleys of central Mexico. It reached Sonora to the north and towards the south it extended into the Yucatan Peninsula and Guatemala (Fig. 1). The illness was first reported in the Valley of Mexico City in April 1576. By July, the outbreak remained circumscribed around Mexico City. In August, the epidemic started slowly to spread, reaching the town of Culhuacan, 20 km south east Mexico City and the town of Tecamachalco, 100 km east from Mexico City. Up to this point, the disease had caused relatively few cases and few deaths. During September of 1576, the peak of the rainy season, cocoliztli literally exploded, extending from central Mexico to Sonora and Guatemala in only few weeks. Also in September, the mortality increased dramatically everywhere, even in places where cocoliztli had just arrived. The highest death rate occurred from September 1576 to March 1577, after which mortality stabilized. In small towns, 20, 40 or more persons died daily, in larger towns, hundreds perished every day, urban centers and rural areas were affected equally. By October 1577, the number of deaths was considerably lower. The end of the outbreak was declared in December 1578. The following rainy season, in August 1579, cocoliztli returned, this time causing fewer human losses. The disease lurked in the country with a fragmentary distribution until April 1581 [[2], [14], [15], [16], [17], [18], [19], [20], [21], [22]].
Figure 1.
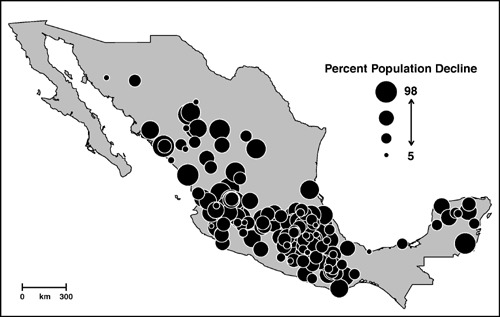
Geographical distribution of mortality in Mexico during the cocoliztli epidemic of 1576. The size of each circle corresponds to the percent population decline between the census of 1570 and the census of 1580 (5, 11).
The demographic impact of the epidemic was immense. Second‐hand contemporaneous estimates based on the 1570 and 1579–1580 censuses indicated that from the four million inhabitants that lived in México before the outbreak, two million died [[18], [20], [22]]. We retrieved all the available data from both censuses, and were able to obtain information for 196 cities and districts distributed across the country [[3], [5], [11]]. Of those, specific quantitative data were available for 157 communities while only estimates of the percent of population loss were obtained for 39 communities. The results indicated that in 1570, a total of 2,098,426 individuals lived in those 157 communities. Two years after the epidemic, by 1580, the population in the same places was reduced to 1,020,524. This represents 1,077,902 deaths, or a population loss of 51.36%. These results indicate that the initial estimates of the 16th century were correct and that the epidemic of 1576 did indeed kill half of the population of Mexico.
All witnesses indicated that the highest mortality occurred among the Indian population and that the Spanish population was almost unaffected [[2], [14], [22]]. Our analyses support this observation. Table 1 illustrates the decline of the Indian population in 10 selected cities, while the Spanish population in the same cities always increased. These cities are representative of the demographic changes in most communities of late 16th century in Mexico [5].
Table 1.
Spanish and native population change in 10 towns distributed across Mexico
| Spanish population | Native population | |||||
|---|---|---|---|---|---|---|
| 1570 | 1580 | Change (%) | 1570 | 1580 | Change (%) | |
| Colima | 60 | 70 | 16.66 | 1800 | 1000 | −44.44 |
| Izucar | 50 | 150 | 200 | 6175 | 3000 | −51.41 |
| Mexico City | 3000 | 4000 | 33.33 | 9952 | 7349 | −26.15 |
| Oaxaca | 300 | 400 | 33.33 | 8000 | 4500 | −43.75 |
| Panuco | 26 | 1000 | 3746.15 | 5140 | 1220 | −76.26 |
| San Miguel el Grande | 20 | 60 | 200 | 100 | 50 | −50.00 |
| Texcoco | 100 | 300 | 200 | 18851 | 8860 | −52.99 |
| Tlalpujahua | 40 | 100 | 150 | 2900 | 1260 | −56.55 |
| Toluca | 70 | 250 | 257.14 | 5207 | 2208 | −57.59 |
| Valles | 60 | 100 | 66.66 | 4238 | 134 | −96.83 |
The numbers indicate the quantity of families registered in 10 communities in the censuses of 1570 and 1580 (5, 11).
Some 16th century sources indicated that the epidemic caused an elevated mortality in the highlands of Mexico but was less lethal in the lowlands [[14], [21]]. To evaluate these reports, the latitude, longitude, altitude, and mean temperature of the 196 communities with known mortality statistics were obtained [[5], [11], [23]]. A positive relationship between altitude and mortality was identified for 44 communities located within parallels 19–20 and longitudes 96–103 (Pearson's correlation index 0.44, P < 0.05). Although the relationship was not very strong, it was enough to be noticed by keen observers. Moreover, since the mean temperature diminishes as altitude increases, a negative correlation between mortality and mean temperature was also found (Pearson's correlation index −0.30, P < 0.05).
Climate appears to have played a role in the epidemics of hemorrhagic fevers in Mexico. Using tree‐ring chronologies from Mexico, we recently demonstrated that the cocoliztli epidemics of 1545 and 1576 occurred in years of abundant rain in the midst of the 16th century megadrought [12], the most severe and sustained drought to impact central Mexico in the past 600 years. Furthermore, cocoliztli traveled faster and caused higher mortality during the rainy season [[12], [24]].
4Discussion
According to the historical record, the epidemic of 1576 was the only episode of high mortality in Mexico between 1570 and 1580. Therefore, it is possible to attribute the massive population loss of this period primarily to the cocoliztli epidemic of 1576. Four general aspects of this epidemic were remarkable: First, the outbreak originated in the valleys of central Mexico whence it evolved as an expansive wave. Second there was a clear ethnic preference of the disease, the Spanish population was minimally affected whereas Indians had high mortality rate. Third, a positive correlation between altitude and mortality in central Mexico was identified. Fourth, severe and prolonged drought preceded the epidemic, but the year of the outbreak precipitation was intense. This may be a classic example of the “sequence of climate extremes” sometimes associated with catastrophic epidemics [25].
Similar to other epidemics of hemorrhagic fevers, the outbreak of 1576 started in the highlands of central Mexico [10]. In a few weeks the disease cocoliztli reached communities thousands of kilometers away. The dissemination pattern of this epidemic in the form of an expanding wave resembles other epidemic diseases with human‐to‐human transmission such as smallpox, influenza, measles, and cholera, diseases that travel as a chain of new infections in the advancing wave front. Altitude, drought and rain played a significant role in the expansion of the disease [12]. Altogether, these data suggest the existence of a natural reservoir of the etiological agent in the highlands of central Mexico. It is possible that the prolonged drought followed by abundant precipitation created favorable conditions for the proliferation of grass and secondarily, the natural reservoir. These circumstances also seemed to have promoted the infection of humans and the fast advance of the epidemic. Interestingly, this sequence of climate extremes and proliferation of a natural reservoir is similar to the conditions that attended the 1993 outbreak of Hantavirus pulmonary syndrome in the Colorado Plateau [26].
The identity of the etiological agent of cocoliztli remains controversial. Yellow fever, plague, leptospirosis, hepatitis, malaria and dengue have been postulated [[6], [7], [8]]. Other possible causes may be Hantavirus, Arenavirus or a form of bartonelosis. Although cocoliztli shares some similarities with those diseases, they probably only reflect common physiopathological processes. The devastating nature of the disease suggests that it is poorly adapted to humans. Cocoliztli may be an example of how some microorganisms cause mild disease in their natural hosts but are very destructive in other species. In the past few years, we have witnessed the emergence of new pathogens that cause mild or no disease in their natural hosts but severe disease in humans. The severe acute respiratory syndrome in humans (SARS) caused by a coronavirus from the Himalayan palm civet (Paguma larvata) and the Hendra and Nipah paramixoviruses from fruit bats of the genus Pteropus that cause encephalitis in human are some examples [[27], [28], [29]].
Broadly, the clinical manifestations of cocoliztli suggest severe liver damage (intense jaundice, hepatomegaly, dark urine) associated with hepatic encephalopathy (anxiety and demented status) and in some cases with portal hypertension (splenomegaly and abdominal distention, ascitis?). Bleeding (lung hemorrhage and bleeding from the ears, anus, vagina, mouth and nose) can be also explained by severe liver damage, although it may be also caused by interference of clotting mechanisms of different origin. At the present time, cocoliztli cannot be definitely linked to any known disease. For the time being, it has been grouped within the heterogeneous family of hemorrhagic fevers [[9], [10]].
Cocoliztli had a higher mortality among the native population while the Spanish population was almost not affected. The selectivity of the disease was clearly marked by the great social divide of that time. At one end of the social spectrum were the malnourished, under clothed and overworked native population, and in the other, the Spaniards, well fed, lived in spacious homes and had many servants. In the case of the first generation of Spaniards in Mexico, a hypothetical immunity to the disease could be explained by previous exposure to European viruses and bacteria. Presumably those of Spanish ancestry born in Mexico would not have this immunity, therefore becoming susceptible to the disease. Interestingly, this was not the case. For centuries the disease affected systematically the poorer strata of Mexican society but was less severe among the affluent sector of the population. This was observed up to the last epidemic in 1813, or 292 years after the conquest, at that time, Mexico had a large population of mixed ancestry [10]. Whether this is related to a genetic susceptibility to the disease or is the result of malnutrition and a weaker immune system is an open question. The relationship between mortality and altitude in central Mexico, suggests a possible ecological niche for a reservoir, however, this also remains to be identified.
Cocoliztli was an emerging infectious disease of its time. It appeared unexpectedly, ran without control for two and a half centuries causing enormous devastation, and then, disappeared mysteriously. Cocoliztli seems to have been the result of complex interactions between land, climate, flora, fauna, human population and microorganisms from other species. This process is not exclusive of the past and will probably generate more emerging infectious diseases in the future. The effects of the hemorrhagic fevers on the Mexican society were huge and far‐reaching. It took approximately 350 years to recover the population of 1544. Demographically, the country changed from being a predominantly Indian country to a predominantly mestizo country. The native way of life collapsed and was replaced by the Spanish culture. In the process, a robust millenary civilization disappeared forever.
It appears that cocoliztli requires at least two major factors to become a deadly epidemic: a rainy year in the midst of a prolonged drought, and a malnourished population. These conditions have occurred several times in Mexico during the last 188 years when war, famine and drought coexisted. Yet, cocoliztli has not reappeared. Is there a decisive, but still unknown factor that remains to be discovered? Is the etiologic agent extinct? Indeed, many questions remain to be answered; perhaps the most compelling ones are the possible reemergence of cocoliztli and the degree of vulnerability of modern society.
Edited by G.M. Ihler
References
- [1]. Cook, S.F. , Simpson, L.B. (1948) The population of Central Mexico in the sixteenth century. Ibero Americana 31, 43–55. [Google Scholar]
- [2]. Clavijero, F.J. Historia Antigua de Mexico. 4 1945, Ed. Porrua, México City, pp. 123.
- [3]. Gibson, C. The Aztecs under Spanish Rule. A History of the Indians of the Valley of Mexico, 1964, Stanford University Press, Stanford, 593 pp.
- [4]. Cook, S. , Borah, W. (1957) The rate of population change in Central México 1550–1570. Hispanic Am. Hist. Rev. 37, 460–470. [Google Scholar]
- [5]. Gerhard, P. Geografía Histórica de la Nueva España 1519–1821, 1986, Universidad Nacional Autónoma de Mexico, Mexico City, 412 pp.
- [6]. Malvido, E. (1973) Cronologia de las Epidemias y Crisis Agrícolas de la Epoca Colonial. Hist. Mexicana 89, 96–101. [Google Scholar]
- [7]. Ocaranza, F. (1933) Las Grandes Epidemias del Siglo XVI en la Nueva España. Medicina (Mex) 13, 176–178. [Google Scholar]
- [8]. León, N. Que era el Matlazahuatl y que el Cocoliztli en los Tiempos Precolombinos y en la Epoca Hispana?. Flores, C.E., Malvido, E., Eds. Ensayos Sobre la Historia de las Epidemias en México. 1 1992, Instituto Mexicano del Seguro Social, Mexico City, 383–395.
- [9]. Marr, J.S., Kiracofe, J.B. Was the Huey Cocoliztli a hemorrhagic fever?. Med. Hist. 44, 2000. [PMC free article] [PubMed]
- [10]. Acuna‐Soto, R. , Calderón‐Romero, L. , Maguire, J.H. (2000) Large epidemics of hemorrhagic fevers in Mexico, 1545–1815. Am. J. Trop. Med. Hyg. 62, 733–739. [DOI] [PubMed] [Google Scholar]
- [11]. Acuña, R. Relaciones Geográficas del Siglo XVI. 10 1982, Universidad Nacional Autónoma de México, Mexico City.
- [12]. Acuna‐Soto, R. , Stahle, D.W. , Cleaveland, M.K. , Therrell, M.D. (2002) Megadrought and megadeath in 16th Century Mexico. Emerg. Infect. Dis. 8, 360–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Molina, A. Vocabulario en Lengua Mexicana y Castellana Compuesto por el muy Reverendo Padre Fray Alonso de Molina de la Orden del Bienaventurado Nuestro Padre San Francisco, 1571, Casa de Antonio Spinoza, Mexico City, p. 24.
- [14]. Somolinos, A.G. (1956) Hallazgo del Manuscrito Sobre el Cocoliztli. Original del Dr. Francisco Hernández. Prensa Med. Mex. 21, 115–123. [PubMed] [Google Scholar]
- [15]. Lopez de Hinojoso, A. Tratado VII. De Pestilencia. Summa y Recopilación de Cirugia con un Arte para Sangrar muy Util y Provechoso, 1578, Imprenta de Antonio Ricardo, Mexico City, pp. 207–213.
- [16]. Lopez de Hinojoso, A. Libro Octavo. De Tabardete y Cocoliztle. Summa y Recopilación de Cirugia con un Arte Para Sangrar muy Util y Provechoso y Examen de Barberos, 1595, Imprenta de Pedro Balli, Mexico City, pp. 148–153.
- [17]. Farfan, A. Libro Tercero De la Calentura de Sangre Corrompida y su Cura. Tractado Breve de Medicina y de Todas las Enfermedades que a Cada Paso se Ofrecen. Hecho por el Padre Fray Agustin Farfan, Doctor en Medicina y Religioso de la Orden de San Agustín en esta Nueva España, 1592, En la Casa de Pedro Ocharte, Mexico City, pp. 238–248.
- [18]. Davila, P.A. De una Grandísima Pestilencia que Hubo por este Tiempo y del Número de Religiosos que Murieron con el de dos Cuentos de Indios. Historia de la Fundación y Discurso de la Provincia, de Santiago, de México de la Orden de los Predicadores por las Vidas de sus Varones Insignes y Casos Notables de Nueva España, 1625, En la casa de Ivan Meerbeque, Brussels, pp. 516–141.
- [19]. de Grijalva, J. (1924) De las Señales que en Esta Tierra se Vieron por Este Tiempo, y de la Gran Peste que Llamaron Cocoliztli. Crónica de la Orden de San Agustín en las Provincias de la Nueva España. En Cuatro Edades Desde el Año de 1533 Hasta el de 1592. pp. 213–220. Imprenta Victoria, Mexico City
- [20]. Cavo, A. Historia de México, 1949, Editorial Patria, Mexico City, pp. 418–434.
- [21]. Chimalpahin, F.S.A.M. Relaciones de Chalco Amaquemecan, 1965, Fondo de Cultura Económica, Mexico City, 460 pp.
- [22]. de Torquemada, F.J. Monarquia Indiana. 5 1969, Editorial Porrúa, Mexico City, pp. 642–643.
- [23]. Instituto Nacional de Geografia. (2002) Estadística e Informática, Anuario Estadístico por Estado. 600 pp. INEGI, Mexico City
- [24]. Stahle, D.W. , Cook, E.R. , Cleaveland, M.K. , Therrell, M.D. , Meko, D.M. , Grissino‐Mayer, H.D. , Watson, E. , Luckman, B.H. (2000) Tree‐ring data document 16th century megadrought over North America. Eos 81, 121–125. [Google Scholar]
- [25]. Epstein, P.R. Shifting times and paradigms: climate change and public health. Leroy, S., Stewart, I.S., Eds. Environmental Catastrophes and Recovery in the Holocene. 2002, Brunel University, London, 30–31, Abstracts volume.
- [26]. Hjelle, B. , Glass, G.E. (2000) Outbreak of Hantavirus infection in the four corners region of the United States in the Wake of the 1997–1998 El Niño‐Southern oscillation. J. Infect. Dis. 181, 1569–1573. [DOI] [PubMed] [Google Scholar]
- [27]. Christian, M.D. , Poutanen, S.M. , Loutfy, M.R. , Muller, M.P. , Low, D.E. (2004) Severe acute respiratory syndrome. Clin. Infect. Dis. 38, 1420–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Murray, K., Eaton, B., Hooper, P., Wang, L., Williamson, M., Young, P. (1998) Flying foxes, and humans: a Zoonosis caused by a new member of the Paramyxoviridae. In: Emerging Infections (Scheld, W.M., Armstrong, D., Hughes, J.M., Eds.), pp.43–58 ASM Press, Washington DC.
- [29]. Chua, K.B. (2003) Nipah virus outbreak in Malaysia. J. Clin. Virol. 26, 265–275. [DOI] [PubMed] [Google Scholar]


