Summary
The importation of infectious diseases during a mass gathering may result in outbreaks. Infectious diseases associated with mass gatherings vary depending on the type and location of the mass gathering. The annual Hajj to Makkah in Saudi Arabia is one of the largest annual religious mass gatherings in the world. Preparation for the Hajj encompasses multiple sectors to develop comprehensive plans. These plans include risk assessment, utilizing existing medical infrastructure, developing electronic and paper-based surveillance activity, and the use of information technology. In this review, we describe key features of the preparedness for the 2014 Hajj and Umra, review the recent impact of emerging viruses such as Ebola in West Africa and the Middle East respiratory syndrome coronavirus (MERS-CoV) in affected countries, and highlight the updated requirements and the required vaccines.
Keywords: Hajj, Pilgrimage, Mass gathering, Surveillance, Saudi Arabia
1. Introduction
A mass gathering is defined as a group of more than 1000 people present in one location; however, most of the published literature reflects much larger congregations (>25 000 people).1 A more inclusive definition is a large number of people attending an event that is focused at specific sites for a finite time.2, 3, 4 The World Health Organization (WHO) definition is “events attended by a sufficient number of people to strain the planning and response resources of a community, state or nation”.5
Mass gatherings can be classified into two types: spontaneous gatherings (e.g., the Pope's funeral) and planned gatherings. Planned gatherings may be recurrent at different locations (e.g., Olympics and World Cup) or recurrent events at the same location (e.g., Hajj pilgrimage in Saudi Arabia). The numerous examples of mass gathering events and the number of attendees have been reviewed.6
One of the major concerns regarding mass gatherings is the importation of infectious diseases resulting in outbreaks, or the exportation thereof, especially at events drawing visitors from different nations, regions, and cultures.7 Infectious diseases associated with mass gatherings vary depending on the type and location of the mass gathering.8 For example, religious gatherings are usually associated with respiratory and gastrointestinal diseases.
The annual Hajj to Makkah in Saudi Arabia is considered one of the largest annually recurring religious mass gatherings in the world. The number of pilgrims attending the annual Hajj or Umra each year is about 10 million, and these pilgrims originate from 184 countries.9 The annual number of pilgrims increased from 58 584 in 1920 to 3 161 573 in 2012.10 The annual Hajj is an excellent example for a discussion on the public health preparation from a mass gathering medicine perspective. Thus, in this review we present an overview of the preparation for the Hajj as an example of a mass gathering. Further, we discuss the methodology for surveillance and the control measures for infectious diseases. Given the importance of Middle East respiratory syndrome (MERS) at recent and upcoming Hajj gatherings, we also provide an overview of Middle East respiratory syndrome coronavirus (MERS-CoV) preparedness.
2. Preparations for mass gatherings and public health interventions
There are three core areas that should be considered for mass gathering preparedness: risk assessment for what might happen, robust surveillance to identify when a disease occurs, and the response when there is a disease outbreak.1
During the Hajj, public health efforts take place to maintain the highest level of excellence and these efforts are coordinated by 24 committees.9, 10, 11 Regarding the Hajj, and based on the US Centers for Disease Control and Prevention (CDC) Risk Assessment Framework for the Severity and Probability Analysis,8 the preventive program framework consists of many players who are involved from the beginning in the preparation and risk assessment (Figure 1 ).
Figure 1.
Structure of the Saudi committees for the Hajj from the local Makkah region to the Supreme Hajj Committee. These different committees coordinate the preparation and risk assessment of each Hajj season.
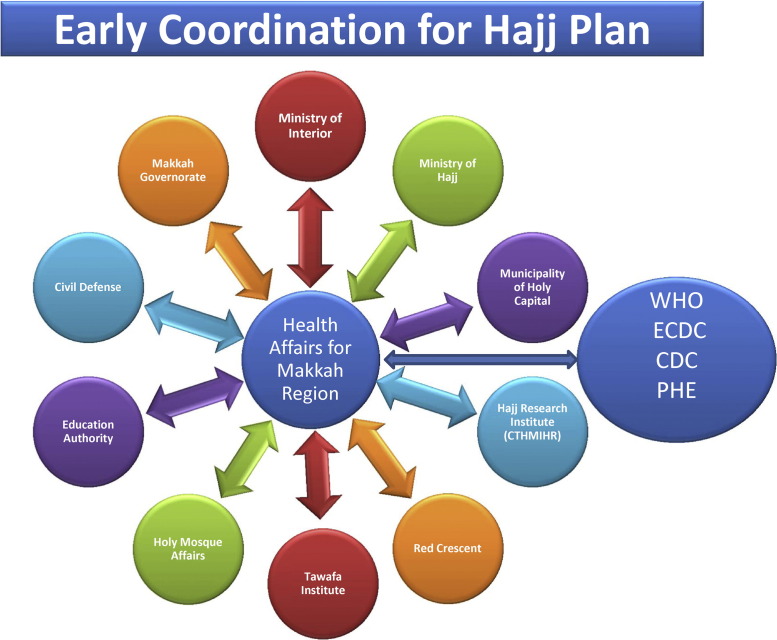
The Supreme Hajj Committee is charged with coordinating and developing the annual Hajj plan and all studies, and in formulating the recommendations for developing Hajj facilities. The Hajj Preventive Medicine Committee is responsible for public health and preventive matters during the Hajj.12 The Committee is also responsible for the control of ports of entry for all pilgrims and confirms compliance with Hajj requirements.13 In addition, input regarding outbreak management and emerging diseases is received from the WHO, European Centre for Disease Prevention and Control (ECDC), Public Health England (PHE), and the CDC, through the Public Health Directorate of the Ministry of Health of the Kingdom of Saudi Arabia (KSA MoH) (Figure 2 ).
Figure 2.
Structure and coordination for Hajj plan, where input regarding outbreak management and emerging diseases is received from different organizations such as the World Health Organization (WHO), European Centre for Disease Prevention and Control (ECDC), Public Health England (PHE), and the United States Centers for Disease Control and Prevention (CDC) through the Public Health Directorate of the Kingdom of Saudi Arabia Ministry of Health. CTHMIHR refers to Custodian of the Two Holy Mosques Institute of the Hajj Research.
3. Medical infrastructure, surveillance activity during Hajj, and use of information technology
During the Hajj, surveillance depends on both electronic and paper systems (Table 1 ).
Table 1.
Diseases under surveillance at Hajj and the application of paper and/or mobile surveillance systems
| Disease | Mobile system | Paper-based system | |
|---|---|---|---|
| 1 | Novel coronavirus | Yes | Yes |
| 2 | Meningococcal meningitis | Yes | Yes |
| 3 | Viral hemorrhagic fever (Ebola Virus Disease, Rift Valley fever, dengue fever, Crimean-Congo hemorrhagic fever and others) |
Yes | Yes |
| 4 | Plague | Yes | Yes |
| 5 | Yellow fever | Yes | Yes |
| 6 | Cholera | Yes | Yes |
| 7 | Food-borne illness | Yes | Yes |
| 8 | Polio | Yes | Yes |
| 9 | Influenza-like illness | Yes | - |
Information technology (IT) is used for public health surveillance during the Hajj. IT plays an essential and important role in the success of the pilgrimage season in many ways, most notably by providing a robust medium that transfers and analyzes data in a timely manner to prepare accurate statistics, which facilitates appropriate decision-making. A centralized and dedicated data center was built to eliminate the process of connecting to different sites in order to obtain the data needed for the Hajj operation team. The first step in gathering and sending data to the Hajj operation team at the command center involves the end-user stations. Therefore, major local area network (LAN) projects were implemented to connect all end-user stations with both wired and wireless connections to the data center. These projects included all the hospitals and medical centers at the Holy sites (Mena, Arafat, and Mozdalefah). Due to constant connectivity problems related to the service provider, a major wireless wide area network project was started in 2011 to cover all participating hospitals, medical centers, and directorates in both Makkah and Madina cities. The new network is owned by the Ministry of Health and has various connection speeds – starting from 54 MB and going up to 1.2 GB – depending on each site's criticality and workload.
In the past, raw data were gathered and submitted to the statistics team in the form of printed papers and the team had to perform the analysis manually. Nowadays, following the implementation of the business intelligence (BI) system, the data are gathered automatically and the BI system performs all the analyses required, presenting the end result statistics in the form of dashboards displayed on a video wall and interactive board for the Hajj operation team at the command center.
Hospitals at Holy sites previously lacked a unified system to gather patient-related data and depended heavily on manual efforts to gather the data required. The Hajj System was built to address this issue and provides a computer-based entry for all data, thus eliminating any delay and human error in gathering and sending the necessary data. The system is web-based with multisite capabilities and was implemented in Mena Emergency Hospital this year and will be rolled out to the other seven hospitals by next year.
The Healthcare Electronic Surveillance Network (HESN) is a web-based electronic health solution that is being implemented in KSA. HESN is the KSA MoH configured system of the Public Health Solution for Disease Surveillance and Management, which is organized into seven major components: communicable disease case management, outbreak management, immunization management, family health, materials/vaccine inventory management, notifications management, work management, and the National Health Safety Network (NHSN). To simplify data gathering at the primary medical center, the use of digital pens was implemented in 2012 for the transformation of conventional forms into digital forms that provide demographic and medical data in a timely fashion. The system was enhanced in 2013, adding dressing and observation forms, and was also implemented in the outpatient departments of two hospitals (Mena Emergency Hospital and Jabil Arrahma Hospital). Figure 3 depicts an example of the data produced using digital pens to monitor the categories of diagnoses for patients visiting primary care clinics during the Hajj. Database-level integration with both statistics and the Hajj System was achieved and data smoothly transferred from the digital pen system to the other two systems. It is important to note that 1000 forms can be loaded electronically. Thus, it is easy to capture the different diagnoses of patients attending the clinics and to display this in a graph.
Figure 3.
An example of data produced using digital pens to monitor the categories of diagnoses of patients visiting primary care clinics during the 2013 Hajj season.
The ambulance information system (AIS) saves all medical and administrative procedures performed for the patient in the ambulance and sends the data – via the Internet – to the responsible parties in the emergency room (ER) of the destination hospital. Automatic vehicle location (AVL) techniques have the potential to improve urban vehicle fleet operations.10 The main purpose of this project has been to identify the location of ambulances and guide them via a map with live traffic densities. In addition, the technology allows the tracking of each ambulance's status – moving, idle or off, speed, etc.
4. Methodology of Hajj surveillance — the example of MERS-CoV
Surveillance during the Hajj is a case-based surveillance. Data are collected from all hospitals located in the Hajj area. For example, during the 2012 Hajj season and due to the emergence of MERS-CoV a few weeks before the Hajj,14 the KSA MoH utilized the case definition of MERS-CoV. The main objectives were the following: to monitor MERS-CoV closely during this mass gathering event, to detect any cases among pilgrims and local residents in a timely manner, and to collect information about the virus in the area in which the first case was located if this were to occur. Clinical samples were taken from all suspected cases during 2013 Hajj season and tested for all possible viral etiologies including MERS-CoV; all samples tested negative for MERS-CoV.15 In addition, following the 2013 Hajj, a cohort of 129 French Hajj pilgrims were systematically sampled with nasal swabs prior to returning to France and were screened for MERS-CoV. The majority of them (90.7%) had respiratory symptoms and none tested positive for MERS-CoV.16
Respiratory illnesses are common among pilgrims. The most common viral respiratory tract infections are influenza and rhinovirus.17 The estimated incidence of upper respiratory tract infections (URTIs) during the Hajj ranges from 20% to 80%, depending on the type of method used to confirm the diagnosis.15 During the 2009 Hajj season, the emergence of pandemic H1N1 was of great concern. There was no increased risk of this virus during the Hajj season.17 A cohort survey was conducted in collaboration between France and Saudi Arabia during the Hajj 2012.18, 19 Participants were followed up and sampled before departing from France to the KSA, during their pilgrimage in the KSA, and just before leaving the KSA.18, 19 Nasal swabs were collected from participants and tested for 11 respiratory viruses and four bacteria by real-time reverse transcription PCR. Of 165 participants who had nasal swabs collected before departing to the KSA, eight (4.8%) were positive for one virus or more, including rhinovirus, influenza virus, adenovirus, and enterovirus, and 7.3% had Streptococcus pneumoniae.18, 19 Among symptomatic pilgrims, 27 (38.6%) were positive for one or more viruses.18 The rate of S. pneumoniae carriage was 7.1% in the country of origin and 19.5% before departing from the KSA.19 These data indicate the risk of acquiring respiratory tract infections during the Hajj and the potential for the spread of the acquired organisms upon returning home.18, 19
5. Infection control for the Hajj in the healthcare setting
Each year the KSA MoH provides the required supplies for proper infection control measures in the healthcare settings of the Hajj cities. These supplies include substances for hand disinfection, surgical tool sterilization, and hospital disinfection.20 Many years ago, due to the need to isolate patients with infectious diseases, mobile isolation devices were provided for installation during the pilgrimage season.20 In a study that evaluated the annual infection control practices in all KSA MoH hospitals in the Holy City of Makkah from 2003 to 2006, there was a significant increase in the average scores of hospitals in 11 infection control items, from 43% (20–67%) in the first audit to 78% (61–93%) in the fourth audit.21 A survey of 392 healthcare workers working in hospitals during the 2003 Hajj season showed that 81.8% correctly answered at least five of the 11 knowledge statements.22
6. Infection control in camps during the care of Pilgrims with respiratory symptoms
For the prevention of respiratory tract infections among pilgrims it is important to observe personal hygiene, cough etiquette, and hand hygiene. In a cohort of 274 French pilgrims in 2009, 77.4% used hand disinfectant, 89.8% used disposable handkerchiefs, and 79.6% used face masks; 97.4% were vaccinated against seasonal influenza, 5.8% against influenza H1N1, and 31.4% against pneumococcus.23
It is thought that the use of masks may reduce exposure to droplet nuclei and thus decrease respiratory tract infections.17 The use of a facemask was significantly higher during the 2009 influenza A H1N1 outbreak (8.4%) than during the 2013 MERS-CoV outbreak (0.02%).24 A recent review of the effectiveness of the facemask in the prevention of respiratory infections among pilgrims revealed variable results.25
The practice of social distancing, hand hygiene, and contact avoidance has been associated with a reduced risk of respiratory illness.17 Following the recommended vaccines would decrease the risk of acquiring respiratory tract infections.17, 26, 27 In a recent study, 65 vaccinated Hajj pilgrims and 41 controls were studied and there was no significant difference in the pattern of occurrence of symptoms of respiratory illness by duration of pilgrimage or the number of symptoms between the two groups.28
7. Vaccine recommendations
The vaccinations required for the 2014 Hajj and Umra seasons have been issued by the KSA MoH.29 These recommendations include immunization against yellow fever, poliomyelitis, and meningococcal meningitis (Table 2 ).
Table 2.
Health requirements and recommendations for entry visas for the Hajj and Umra seasons in 2014a
| Countries or areas at risk | Requirement | |
|---|---|---|
| Yellow fever |
Africa: Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Congo, Cote d’Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Gabon, Guinea, Guinea-Bissau, Gambia, Ghana, Kenya, Liberia, Mali, Mauritania, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, Sudan, South Sudan, Togo, and Uganda South and Central America: Argentina, Venezuela, Brazil, Colombia, Ecuador, French Guiana, Guyana, Panama, Paraguay, Peru, Bolivia, Suriname, and Trinidad and Tobago |
A valid yellow fever vaccination certificate (≥10 days prior to arrival). In the absence of such a certificate, the individual will be placed under strict surveillance for 6 days from the last date of potential exposure to infection |
| Meningococcal meningitis | (a) Visitors from all countries | (a) Certificate of vaccination with the quadrivalent (ACYW135) vaccine issued not more than 3 years previously and not less than 10 days before arrival in Saudi Arabia |
| (b) Visitors from the African meningitis belt: Benin, Burkina Faso, Cameroon, Chad, Central African Republic, Côte d’Ivoire, Eritrea, Ethiopia, Gambia, Guinea, Guinea-Bissau, Mali, Niger, Nigeria, Senegal, and Sudan | (b) ACYW135 vaccine (as above) AND ciprofloxacin 500 mg chemoprophylaxis will be administered at the port of entry | |
| (c) Interior pilgrims and Hajj workers | (c) Vaccination with quadrivalent (ACYW135) vaccine is required for: • All citizens and residents of Madina and Makkah (not vaccinated during the past 3 years) • All citizens and residents undertaking the Hajj • All Hajj workers (not vaccinated in the past 3 years) • Any individual working at entry points or in direct contact with pilgrims in Saudi Arabia |
|
| Poliomyelitis | (a) Polio-affected countries and reestablished transmission countries: Pakistan, Equatorial Guinea, Ethiopia, Iraq, Nigeria, Somalia (b) Exporting countries (currently exporting wild poliovirus): Cameroon, Pakistan, Syria (c) Countries with unknown vaccination coverage: Yemen |
Should ensure that all residents and long-term visitors (of over 4 weeks) receive an oral polio vaccine (OPV) or an inactivated poliovirus vaccine (IPV) 4 weeks to 12 months before international travel and should ensure that such travelers are provided with proof of vaccination AND all will receive one dose of OPV at the border on arrival to Saudi Arabia |
| Seasonal influenza | All | The Ministry of Health of Saudi Arabia recommends that all pilgrims be vaccinated against seasonal influenza |
This is an updated version of a table published in the following article: Al-Tawfiq JA, Memish ZA. The Hajj: updated health hazards and current recommendations for 2012. Euro Surveill 2012;17. pii: 20295. Available online at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20295 (with permission).
The yellow fever vaccination is required for travelers coming from yellow fever endemic countries in Africa and South America. A certificate of valid yellow fever vaccination showing vaccination at least 10 days prior to arrival is required. Pilgrims coming from these countries with no proof of vaccination are monitored for 6 days from the last date of potential exposure to yellow fever infection.29 The yellow fever vaccination is said to be valid for 10 years. However, at the WHO World Health Assembly in May 2014 an amendment was adopted, stipulating that the validity of the certificate be changed from 10 years to the duration of the life of the person vaccinated.30
The meningococcal meningitis vaccine is required for all pilgrims and they should show proof of vaccination with the quadrivalent (ACYW135) meningococcal vaccine received not less than 10 days and not more than 3 years previously.29 In addition to this requirement, pilgrims from the African meningitis belt will receive ciprofloxacin 500 mg as chemoprophylaxis at the port of entry.29
On May 5, 2014, the Director-General of the WHO declared the international spread of wild poliovirus (WPV) to be a public health emergency of international concern (PHEIC).31, 32 Pilgrims arriving from countries where poliomyelitis is established, has become reestablished, or is being exported should receive an oral or an inactivated polio vaccine (OPV or IPV) 4 weeks to 12 months before travel.12, 32 In addition, these pilgrims will receive one dose of OPV on arrival in to KSA.12, 32
8. Travel advice on MERS-CoV for 2014 Hajj pilgrimages
At the time of the initial emergence of MERS-CoV in 2012, there was no restriction on travel or performance of Hajj or Umra due to the limited number of human cases.14, 33 The recommendations included that pilgrims practice proper hand hygiene and apply protective behaviors and cough etiquette.14, 17, 33, 34 The practice of hand hygiene and cough etiquette resulted in less respiratory illness among United States travelers to the 2009 Hajj.35 In addition, in 2013 the KSA MoH recommended that people aged over 65 years, those with chronic diseases (e.g., heart disease, kidney disease, respiratory disease, diabetes) and pilgrims with an immune deficiency (congenital or acquired), malignancy, or terminal illness, pregnant women, and children aged under 12 years postpone the performance of the Hajj and Umra for their own safety, as well avoiding unnecessary contact with farm, domestic, and wild animals; these recommendations remain in place for 2014.10, 36
The WHO recently endorsed the KSA MoH recommendations for MERS-CoV prevention and stressed that its member states use all practical and effective means of communication possible to communicate information on a range of issues before, during, and after Umra and Hajj to all key groups, including travelers to Umra and Hajj, and particularly, vulnerable groups within this population. In addition, member states should support the efforts of the KSA MoH in making health-related advice available to all travelers departing for Umra or Hajj by working with the travel and tourism sectors and placing such materials at strategic locations. Various strategies for the communication of the health recommendations should be utilized, including pamphlets and radio and television programs.37 In their guidance to countries, the WHO stressed the enforcement of the recommendation that pilgrims who develop a significant acute respiratory illness with fever and cough (severe enough to interfere with usual daily activities) during Umra or Hajj, or after return to their country of origin, should report to the medical health facility closest to them and cover their mouth and nose when coughing or sneezing and wash hands afterwards, or if this is not possible, cough or sneeze into the upper sleeves of their clothing; further they should avoid attending crowded places and preferably isolate themselves until the end of the respiratory symptoms and, if isolation is not possible, use a tissue to cover the nose and mouth or a surgical mask when in crowded places.
9. Hajj-related advice regarding other emerging infectious diseases
In the event of a PHEIC, or in the case of any disease outbreak subject to notification under the International Health Regulations 2005, the health authorities in Saudi Arabia usually undertake additional preventive precautions following consultation with the national communicable diseases committees and on receiving the necessary governmental approval to avoid the spread of infection during the pilgrimage or on return to the country of origin. This has been applied to Ebola this year, with a restriction on pilgrims from countries where outbreaks of Ebola are ongoing, such as Guinea, Liberia, and Sierra Leone. The current outbreak was initially reported from Guinea, including the capital city of Conakry, and then in March 30, 2014, cases were reported in the district of Foya in neighboring Liberia; in May 2014, the first cases were identified in Sierra Leone.38 On August 8, 2014 the World Health Organization declared that the epidemic of ebola to be a Public Health Emergency of International Concern (PHEIC). In addition, the recent polio outbreak in Pakistan and Syria and the WHO International Health Regulation Emergency Committee recommendations have been enforced. Recently, Brazil was exposed to a poliovirus importation with no evidence of transmission and thus no additional measures were needed for travelers.39
10. Conclusions
Mass gatherings in general and the Hajj in particular continue to grow in number and magnitude. It is crucial that knowledge and experiences are shared and evaluated. It is important to turn mass gathering health into a proper scientific discipline and to create a global mass gathering network to serve as a platform for the exchange of learning and experience. It is important to update the immunization status of pilgrims against vaccine-preventable diseases. Preparation for international travel and for the Hajj in particular is an excellent opportunity to review the immunization status of travelers. It is important to keep in mind the vaccinations required for attendance at the Hajj (e.g., meningococcal vaccination and polio vaccination).
Conflict of interest: The authors have no conflicts of interest; the work was not supported or funded by any drug company.
Corresponding Editor: Eskild Petersen, Aarhus, Denmark
References
- 1.World Health Organization. Communicable disease alert and response for mass gatherings: key considerations, June 2008. Geneva: WHO;. Available at: http://www.who.int/csr/Mass_gatherings2.pdf (accessed June 3, 2014).
- 2.Memish Z.A., Stephens G.M., Steffen R., Ahmed Q.A. Emergence of medicine for mass gatherings: lessons from the Hajj. Lancet Infect Dis. 2012;12:56–65. doi: 10.1016/S1473-3099(11)70337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michael J.A., Barbera J.A. Mass gathering medical care: a twenty-five year review. Prehosp Disaster Med. 1997;12:305–312. [PubMed] [Google Scholar]
- 4.Arbon P., Bridgewater F.H., Smith C. Mass gathering medicine: a predictive model for patient presentation and transport rates. Prehosp Disaster Med. 2001;16:150–158. doi: 10.1017/s1049023x00025905. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Communicable disease alert and response for mass gatherings. WHO/CDS/EPR. WHO; 2008. Available at: http://www.who.int/csr/Mass_gatherings2.pdf (accessed September 17, 2013).
- 6.Smith M.W., Fulde G.W., Hendry P.M. World Youth Day 2008: did it stress Sydney hospitals? Med J Aust. 2008;189:630–632. doi: 10.5694/j.1326-5377.2008.tb02221.x. [DOI] [PubMed] [Google Scholar]
- 7.Michael J.A., Barbera J.A. Mass gathering medical care: a twenty-five year review. Prehosp Disaster Med. 1997;12:305–312. [PubMed] [Google Scholar]
- 8.Abubakar I., Gautret P., Brunette G.W., Blumberg L., Johnson D., Poumerol G. Global perspectives for prevention of infectious diseases associated with mass gatherings. Lancet Infect Dis. 2012;12:66–74. doi: 10.1016/S1473-3099(11)70246-8. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed Q., Arabi Y., Memish Z. Health risks at the Hajj. Lancet. 2006;367:1008–1015. doi: 10.1016/S0140-6736(06)68429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Memish Z.A., Zumla A., Alhakeem R.F., Assiri A., Turkestani A., Al Harby K.D. Hajj: infectious disease surveillance and control. Lancet. 2014;383:2073–2082. doi: 10.1016/S0140-6736(14)60381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebrahim S.H., Memish Z.A., Uyeki T.M., Khoja T.A., Marano N., McNabb S.J. Public health. Pandemic H1N1 and the 2009 Hajj. Science. 2009;326:938–940. doi: 10.1126/science.1183210. [DOI] [PubMed] [Google Scholar]
- 12.Al-Tawfiq J.A., Memish Z.A. The Hajj: updated health hazards and current recommendations for 2012. Euro Surveill. 2012;17 pii: 20295. [PubMed] [Google Scholar]
- 13.Memish Z.A. The Hajj: communicable and non-communicable health hazards and current guidance for pilgrims. Euro Surveill. 2010;15 pii: 19671. [PubMed] [Google Scholar]
- 14.Al-Tawfiq J.A., Smallwood C.A., Arbuthnott K.G., Malik M.S., Barbeschi M., Memish Z.A. Emerging respiratory and novel coronavirus 2012 infections and mass gatherings. East Mediterr Health J. 2013;19(Suppl 1):S48–S54. [PubMed] [Google Scholar]
- 15.Memish Z.A., Almasri M., Turkestani A., Al-Shangiti A.M., Yezli S. Etiology of severe community-acquired pneumonia during Hajj—part of the MERS-CoV surveillance program. Int J Infect Dis. 2014;25:186–190. doi: 10.1016/j.ijid.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benkouiten S., Charrel R., Belhouchat K., Drali T., Nougairede A., Salez N. Respiratory viruses and bacteria among pilgrims during the 2013 Hajj. Emerg Infect Dis [Internet] 2011 doi: 10.3201/eid2011.140600. http://www.cdc.gov/Other/disclaimer.html (accessed Nov 2011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Tawfiq J.A., Zumla A., Memish Z.A. Respiratory tract infections during the annual Hajj: potential risks and mitigation strategies. Curr Opin Pulm Med. 2013;19:192–197. doi: 10.1097/MCP.0b013e32835f1ae8. [DOI] [PubMed] [Google Scholar]
- 18.Benkouiten S., Charrel R., Belhouchat K., Drali T., Salez N., Nougairede A. Circulation of respiratory viruses among pilgrims during the 2012 Hajj pilgrimage. Clin Infect Dis. 2013;57:992–1000. doi: 10.1093/cid/cit446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benkouiten S., Gautret P., Belhouchat K., Drali T., Memish Z.A., al Masri M. Acquisition of Streptococcus pneumoniae carriage in pilgrims during the 2012 Hajj pilgrimage. Clin Infect Dis. 2014;58:e106–e109. doi: 10.1093/cid/cit749. [DOI] [PubMed] [Google Scholar]
- 20.Saudi Ministry of Health. Saudi Arabia: Ministry of Health; 2013 Available at: http://www.moh.gov.sa/en/hajj/news/pages/news-2013-10-17-003.aspx (accessed June 2, 2014).
- 21.Madani T.A., Albarrak A.M., Alhazmi M.A., Alazraqi T.A., Althaqafi A.O., Ishaq A.H. Steady improvement of infection control services in six community hospitals in Makkah following annual audits during Hajj for four consecutive years. BMC Infect Dis. 2006;6:135. doi: 10.1186/1471-2334-6-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghabrah T.M., Madani T.A., Albarrak A.M., Alhazmi M.A., Alazraqi T.A., Alhudaithi M.A. Assessment of infection control knowledge, attitude and practice among healthcare workers during the Hajj period of the Islamic year 1423 (2003) Scand J Infect Dis. 2007;39:1018–1024. doi: 10.1080/00365540701466173. [DOI] [PubMed] [Google Scholar]
- 23.Gautret P., Vu Hai V., Sani S., Doutchi M., Parola P., Brouqui P. Protective measures against acute respiratory symptoms in French pilgrims participating in the Hajj of 2009. J Travel Med. 2011;18:53–55. doi: 10.1111/j.1708-8305.2010.00480.x. [DOI] [PubMed] [Google Scholar]
- 24.Elachola H., Assiri A.M., Memish Z.A. Mass gathering-related mask use during 2009 pandemic influenza A (H1N1) and Middle East respiratory syndrome coronavirus. Int J Infect Dis. 2014;20:77–78. doi: 10.1016/j.ijid.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Benkouiten S., Brouqui P., Gautret P. Non-pharmaceutical interventions for the prevention of respiratory tract infections during Hajj pilgrimage. Travel Med Infect Dis. 2014 Jun 24 doi: 10.1016/j.tmaid.2014.06.005. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eurosurveillance editorial office Muslim Hajj pilgrimage: minimising the risks of infectious disease. Euro Surveill. 2005 doi: 10.2807/esw.10.03.02623-en. 10:E050120.5. [DOI] [PubMed] [Google Scholar]
- 27.Razavi S.M., Salamati P. Prevention of influenza at Hajj: applications for mass gatherings. J R Soc Med. 2013;106:386. doi: 10.1177/0141076813504327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasan H., Deris Z.Z., Sulaiman S.A., Abdul Wahab M.S., Naing N.N., Ab Rahman Z. Effect of influenza vaccination on acute respiratory symptoms in Malaysian Hajj pilgrims. J Immigr Minor Health. 2014 Jun 20 doi: 10.1007/s10903-014-0059-y. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Memish Z.A., Al Rabeeah A.A. Health conditions for travellers to Saudi Arabia for the Umra and pilgrimage to Mecca (Hajj)—2014. J Epidemiol Glob Health. 2014;4:73–75. doi: 10.1016/j.jegh.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. Yellow fever vaccination booster. Geneva: WHO; 2014 Available at: http://www.who.int/ith/updates/20140605/en/ (accessed July 17, 2014).
- 31.Global Polio Eradication Initiative. Temporary recommendations to reduce international spread of poliovirus. GPEI; 2014 Available at: http://www.polioeradication.org/Infectedcountries/PolioEmergency.aspx#sthash.y7Q7sUdp.dpu (accessed July 17, 2014).
- 32.World Health Organization. Polio vaccination for travellers. Geneva: WHO; 2014 Available at: http://www.who.int/ith/updates/20140612/en/ (accessed July 17, 2014).
- 33.Memish Z.A., Zumla A., Al-Tawfiq J.A. How great is the risk of Middle East respiratory syndrome coronavirus to the global population? Expert Rev Anti Infect Ther. 2013;11:979–981. doi: 10.1586/14787210.2013.836965. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Travel advice on MERS-CoV for pilgrimages. Geneva: WHO; 2014 Available at: http://www.who.int/ith/updates/20140603/en/ (accessed July 25, 2014).
- 35.Balaban V., Stauffer W.M., Hammad A., Afgarshe M., Abd-Alla M., Ahmed Q. Protective practices and respiratory illness among US travelers to the 2009 Hajj. J Travel Med. 2012;19:163–168. doi: 10.1111/j.1708-8305.2012.00602.x. [DOI] [PubMed] [Google Scholar]
- 36.Memish Z.A., Al-Rabeeah A.A. Health conditions of travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj and Umra) for 1434 (2013) J Epidemiol Glob Health. 2013;3:59–61. doi: 10.1016/j.jegh.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. World travel advice on MERS-CoV for pilgrimages. Geneva: WHO; 2013 Available at: http://www.who.int/ith/updates/20130725/en/ (accessed July 11, 2014).
- 38.Outbreak news Ebola virus disease, West Africa. Wkly Epidemiol Rec. 2014;89:205–206. [PubMed] [Google Scholar]
- 39.World Health Organization. Detection of poliovirus in sewage, Brazil. Geneva: WHO; 2014 Available at: http://www.who.int/csr/don/2014_6_23polio/en/ (accessed July 20, 2014).