Summary
Background
The surveillance of infection is very important for public health management and disease control. It has been 10 years since China implemented its new web-based infection surveillance system, which covers the largest population in the world.
Methods
In this study, time series data were collected for 28 infectious diseases reported from 2005 to 2014 . Seasonality and long-term trends were explored using decomposition methods. Seasonality was expressed by calculating the seasonal indices. Long-term trends in the diseases were assessed using a linear regression model on the deseasonalized series.
Results
During the 10-year period, 38 982 567 cases and 126 372 deaths were reported in the system. The proportion of deaths caused by AIDS increased from 12% in 2005 to 78% in 2014. There were six diseases for which the seasonal index range was greater than 2: dengue fever, Japanese encephalitis, leptospirosis, anthrax, cerebrospinal meningitis, and measles . Among the 28 diseases, the incidence of syphilis increased fastest, with an average increase of 0.018626/100 000 every month after adjustment for seasonality.
Conclusions
Effective surveillance is helpful in gaining a better understanding of the infection behaviour of infectious diseases; this will greatly facilitate disease control and management.
Keywords: Infectious disease, Seasonality, Long-term trend, Time series
1. Introduction
After the outbreak of severe acute respiratory syndrome (SARS) in 2003, the Chinese government strengthened the country's infectious disease surveillance system.1 A new web-based reporting system was established utilizing modern information technology. The new surveillance system was implemented formally in 2004. The new surveillance system has played an important role in detecting infectious diseases in a timely fashion, which has helped to protect the lives and health of the entire population and has reduced the economic and health impacts of the diseases on the whole of society. This new system is the largest infectious disease surveillance system covering the largest population in the world.2 It has become possible to detect more infections and the data have become more complete and reliable since the new reporting system was established.3 A survey showed that the average omission rate was 13% among the medical institutions throughout the country; the compliance rate for outpatient daily registration was 96%, the registry integrity rate was 97%, and the timely reporting rate for the medical institutions was 91%.4
Thirty-nine notifiable infectious diseases are currently included in the surveillance system. These are divided into classes A, B, and C.5 Class A notifiable diseases include the plague and cholera, which can cause large epidemics within a short period of time. Class B notifiable diseases include 28 infectious diseases that might cause epidemics, including AIDS, anthrax, etc. Class C notifiable diseases include less severe and less infectious diseases, such as mumps, rubella, acute haemorrhagic conjunctivitis, leprosy, leishmaniasis, hydatid disease, etc.
It has been over 10 years since the implementation of the new web-based surveillance system. Since this system covers a large population, the surveillance data can stably show the behaviour of a disease in terms of occurrence. Statistical modelling has been used previously to summarize the time series behaviour of disease.6 In the current study, the monthly time series data for 28 class B infectious diseases reported from 2005 to 2014 were collected. The class B infectious diseases were selected for study, as most of these diseases occur more frequently than class A diseases and they cause more severe epidemics than class C diseases. Class B infectious diseases are the main focus of the surveillance process. A descriptive analysis and time series study was performed.7 Decomposition methods were used to analyse the seasonal pattern and long-term trends of the class B notifiable infectious diseases for the years 2005–2014.
2. Data and methods
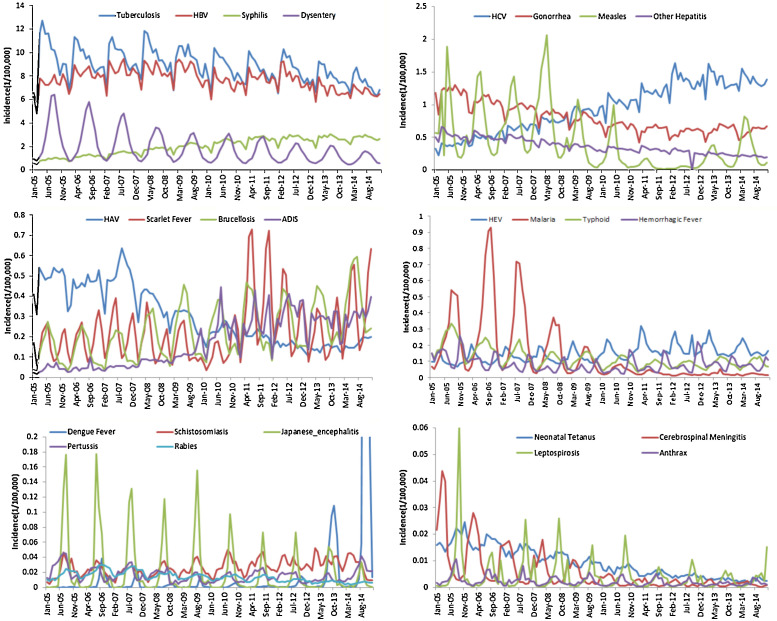
Available time series data for the monthly reported cases of 28 class B infectious diseases were gathered for the years 2005–2014. These 28 class B infectious diseases are AIDS, anthrax, avian influenza, brucellosis, cerebrospinal meningitis, dengue fever, diphtheria, dysentery, gonorrhoea, hepatitis disease (including hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis E virus (HEV), and other types of hepatitis), haemorrhagic fever, Japanese encephalitis, leptospirosis, malaria, measles, neonatal tetanus, pertussis, polio, rabies, scarlet fever, schistosomiasis, syphilis, tuberculosis, and typhoid fever. The data were reported by the Chinese Centre for Disease Control and Prevention (CDC). The incidences of these diseases are shown in Figure 1 .
Figure 1.
Incidences of 25 of the 28 class B notifiable diseases (avian influenza, polio, and diphtheria are not included in the figure due to their low incidences). The incidence of dengue fever (bottom left) was 1.08 in September 2014 and 2.12 in October 2014, which is not shown in the figure.
A descriptive study was first performed, and decomposition methods were used to extract the underlying pattern in the infectious disease time series. The decomposition methods have been reported in previous studies.6, 8 Decomposition breaks down the underlying patterns of time series into seasonality and long-term trends. The seasonal trend in the infection series can be expressed using seasonal indices. To calculate the seasonal factors, overall incidences are first averaged, and then the averaged incidence is divided by the mean incidence for each month. For example, the average incidence of malaria was 0.1344/100 000 during the 10 years and the mean incidence in May was 0.1059/100 000, thus the seasonal index for May is 0.788 (0.1344/0.1059). Seasonality shows the periodic fluctuations that are usually caused by known factors such as rainfall, temperature, timing of the holidays, etc. If the seasonal index is greater than 1, it means that the incidence is higher than the average level. Otherwise, it means that the incidence is lower than the average level. The trend cycle represents the long-term changes in the infection. After the seasonal indices have been calculated, one can deseasonalize the data by dividing by the corresponding index. A linear regression model is a simple way to express the long-term trend, in which a common linear regression model is established between the deseasonalized incidence and time t.
3. Results
The numbers of cases of the 28 class B notifiable diseases during the years 2005–2014 are shown in Table 1 . During the 10-year period, 38 982 567 cases and 126 372 deaths were reported in the system. Tuberculosis, HBV, syphilis, dysentery, and HCV were the top 5 ranking diseases in terms of the number of cases. The numbers of deaths caused by the 28 class B notifiable diseases for the years 2005–2014 are shown in Table 2 . AIDS, tuberculosis, rabies, HBV, Japanese encephalitis, haemorrhagic fever, and neonatal tetanus were the top 7 ranking diseases in terms of the number of deaths; these diseases each caused more than 1000 deaths during the 10 years.
Table 1.
Numbers of cases of the class B notifiable diseases in China (ranked by total number)
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tuberculosis | 1 509 485 | 1 454 231 | 1 499 264 | 1 533 475 | 1 482 869 | 1 392 210 | 1 357 922 | 1 371 488 | 1 297 123 | 1 190 246 | 14 088 313 |
| Hepatitis B virus | 1 132 805 | 1 261 735 | 1 327 225 | 1 330 654 | 1 330 352 | 1 193 266 | 1 252 236 | 1 257 320 | 1 113 319 | 1 084 543 | 12 283 455 |
| Syphilis | 135 210 | 177 988 | 220 561 | 272 938 | 320 802 | 375 309 | 419 306 | 434 280 | 437 646 | 441 818 | 3 235 858 |
| Dysentery | 462 854 | 427 570 | 371 598 | 317 367 | 275 123 | 255 331 | 240 557 | 210 006 | 190 601 | 155 247 | 2 906 254 |
| Hepatitis C virus | 59 159 | 77 315 | 100 258 | 118 201 | 141 609 | 163 174 | 188 807 | 219 110 | 223 094 | 222 528 | 1 513 255 |
| Gonorrhoea | 185 952 | 163 132 | 149 079 | 134 783 | 121 948 | 107 373 | 100 004 | 93 608 | 101 108 | 96 874 | 1 253 861 |
| Measles | 106 002 | 107 538 | 118 031 | 144 221 | 59 950 | 44 597 | 11 849 | 6678 | 29 627 | 56 143 | 684 636 |
| Other hepatitis | 82 969 | 78 907 | 75 715 | 63 824 | 55 556 | 51 331 | 50 318 | 41 979 | 39 321 | 34 804 | 574 724 |
| Hepatitis A virus | 76 102 | 70 889 | 79 349 | 58 820 | 45 372 | 36 250 | 32 659 | 25 452 | 22 891 | 26 740 | 474 524 |
| Scarlet fever | 25 713 | 28 172 | 34 170 | 28 507 | 22 441 | 20 774 | 64 358 | 47 430 | 34 521 | 54 541 | 360 627 |
| Brucellosis | 20 050 | 20 699 | 21 560 | 30 002 | 37 734 | 35 693 | 43 827 | 42 267 | 46 289 | 59 981 | 358 102 |
| AIDS | 6618 | 6974 | 7803 | 12 409 | 19 313 | 36 594 | 41 812 | 49 852 | 44 491 | 47 215 | 273 081 |
| Hepatitis E virus | 15 397 | 18 455 | 20 513 | 19 679 | 20 854 | 24 260 | 30 459 | 29 859 | 28 991 | 27 943 | 236 410 |
| Malaria | 40 394 | 60 813 | 47 468 | 26 909 | 14 453 | 7759 | 4552 | 2820 | 3692 | 3123 | 211 983 |
| Typhoid | 35 921 | 26 888 | 21 254 | 16 409 | 17 409 | 14 712 | 12 217 | 12 452 | 14 629 | 14 159 | 186 050 |
| Haemorrhagic fever | 22 288 | 16 129 | 11 756 | 9696 | 9203 | 9782 | 11 323 | 13 918 | 13 558 | 12 194 | 129 847 |
| Dengue fever | 36 | 1068 | 544 | 206 | 312 | 237 | 124 | 577 | 4683 | 47 331 | 55 118 |
| Schistosomiasis | 3422 | 3451 | 3200 | 3367 | 3879 | 4569 | 4753 | 5068 | 5862 | 4565 | 42 136 |
| Japanese encephalitis | 5320 | 5316 | 4660 | 3237 | 4236 | 2738 | 1887 | 1934 | 2320 | 1044 | 32 692 |
| Pertussis | 4058 | 2653 | 3031 | 2514 | 1641 | 1838 | 2591 | 2286 | 1753 | 3426 | 25 791 |
| Rabies | 2622 | 3393 | 3399 | 2544 | 2281 | 2119 | 1964 | 1462 | 1214 | 966 | 21 964 |
| Neonatal tetanus | 2859 | 2612 | 2202 | 1871 | 1450 | 1149 | 852 | 706 | 515 | 439 | 14 655 |
| Cerebrospinal meningitis | 2502 | 1816 | 1288 | 1018 | 717 | 379 | 265 | 227 | 227 | 205 | 8644 |
| Leptospirosis | 1463 | 668 | 914 | 894 | 593 | 695 | 425 | 455 | 397 | 523 | 7027 |
| Anthrax | 555 | 465 | 431 | 342 | 364 | 301 | 316 | 250 | 207 | 263 | 3494 |
| Avian influenza | 7 | 13 | 5 | 4 | 7 | 1 | 1 | 1 | 2 | 2 | 43 |
| Polio | 0 | 0 | 0 | 0 | 0 | 0 | 20 | 0 | 0 | 0 | 20 |
| Diphtheria | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 |
| Total | 3 939 763 | 4 018 891 | 4 125 279 | 4 133 891 | 3 990 468 | 3 782 441 | 3 875 405 | 3 871 485 | 3 658 081 | 3 586 863 | 38 982 567 |
Table 2.
Numbers of deaths caused by class B notifiable diseases in China (ranked by total number)
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AIDS | 968 | 942 | 1200 | 4158 | 4486 | 9531 | 10 726 | 12 483 | 11 718 | 12 317 | 68 529 |
| Tuberculosis | 2618 | 2475 | 2073 | 2368 | 3075 | 1742 | 1930 | 1935 | 1887 | 1772 | 21 875 |
| Rabies | 2191 | 2692 | 2873 | 2350 | 2103 | 1986 | 1902 | 1372 | 1082 | 873 | 19 424 |
| Hepatitis B virus | 849 | 841 | 838 | 930 | 830 | 723 | 686 | 638 | 593 | 398 | 7326 |
| Japanese encephalitis | 160 | 387 | 165 | 135 | 171 | 95 | 73 | 67 | 77 | 36 | 1366 |
| Hepatitis C virus | 102 | 151 | 123 | 131 | 155 | 142 | 137 | 110 | 163 | 134 | 1348 |
| Haemorrhagic fever | 227 | 145 | 129 | 107 | 107 | 120 | 127 | 99 | 119 | 85 | 1265 |
| Neonatal tetanus | 231 | 187 | 160 | 195 | 130 | 95 | 59 | 57 | 49 | 14 | 1177 |
| Syphilis | 81 | 89 | 74 | 91 | 76 | 86 | 102 | 102 | 82 | 87 | 870 |
| Cerebrospinal meningitis | 172 | 138 | 104 | 117 | 90 | 34 | 25 | 24 | 22 | 15 | 741 |
| Dysentery | 131 | 112 | 68 | 57 | 37 | 42 | 28 | 17 | 14 | 5 | 511 |
| Other hepatitis | 103 | 88 | 75 | 59 | 41 | 32 | 18 | 23 | 19 | 13 | 471 |
| Measles | 47 | 31 | 64 | 111 | 40 | 27 | 12 | 7 | 28 | 27 | 394 |
| Hepatitis E virus | 44 | 40 | 39 | 31 | 24 | 34 | 41 | 23 | 20 | 15 | 311 |
| Malaria | 40 | 30 | 14 | 20 | 10 | 16 | 32 | 14 | 22 | 23 | 221 |
| Hepatitis A virus | 36 | 33 | 23 | 13 | 22 | 6 | 14 | 9 | 4 | 8 | 168 |
| Leptospirosis | 41 | 17 | 31 | 17 | 11 | 12 | 5 | 5 | 7 | 8 | 154 |
| Typhoid | 13 | 18 | 7 | 7 | 10 | 3 | 2 | 6 | 5 | 1 | 72 |
| Anthrax | 11 | 12 | 1 | 1 | 3 | 6 | 3 | 1 | 1 | 3 | 42 |
| Avian influenza | 5 | 8 | 2 | 4 | 4 | 1 | 1 | 1 | 2 | 0 | 28 |
| Gonorrhoea | 1 | 5 | 0 | 3 | 3 | 1 | 3 | 1 | 1 | 3 | 21 |
| Schistosomiasis | 2 | 3 | 1 | 0 | 2 | 0 | 2 | 5 | 1 | 0 | 16 |
| Brucellosis | 5 | 0 | 0 | 1 | 1 | 1 | 0 | 2 | 2 | 2 | 14 |
| Pertussis | 1 | 4 | 0 | 0 | 1 | 1 | 2 | 1 | 0 | 2 | 12 |
| Scarlet fever | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 0 | 8 |
| Dengue fever | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 7 |
| Polio | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Diphtheria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 8082 | 8448 | 8064 | 10 906 | 11 432 | 14 736 | 15 932 | 17 004 | 15 921 | 15 847 | 126 372 |
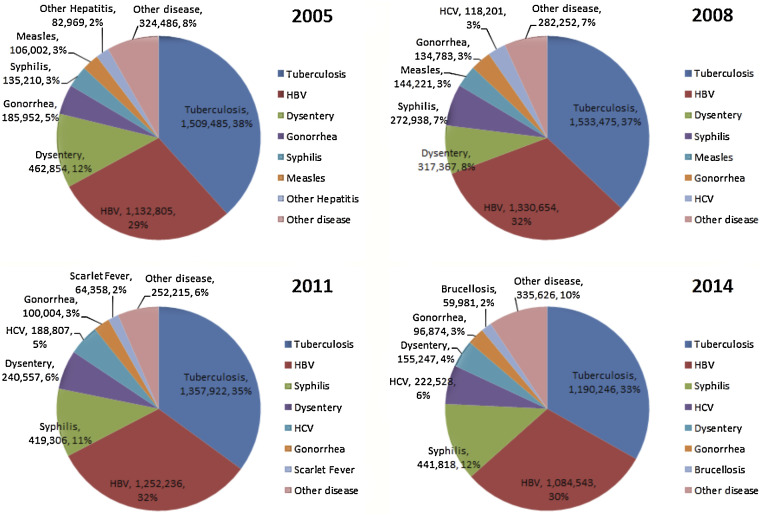
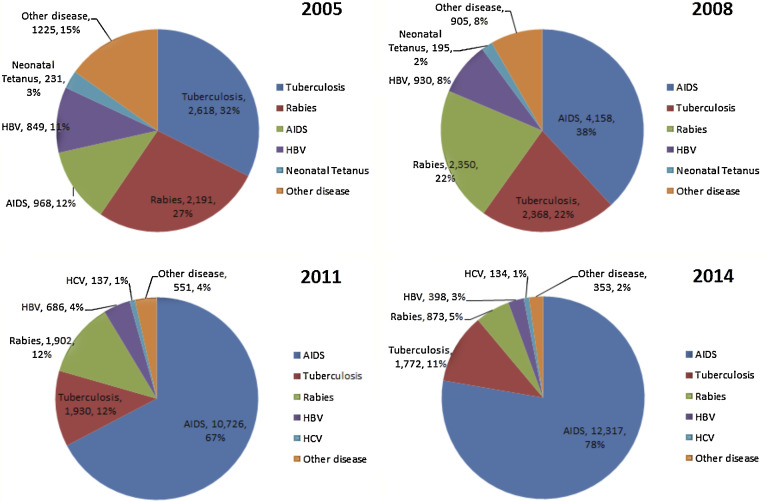
With regard to the numbers of cases, tuberculosis represented the highest proportion among the 28 class B notifiable diseases throughout the 10 years (Figure 2 ). The proportion of tuberculosis cases decreased from 38% in 2005 to 33% in 2014. HBV represented the second highest proportion of the 28 class B notifiable diseases; the proportion of HBV remained quite stable at 29% in 2005, 32% in 2008, 32% in 2011, and 30% in 2014. The proportion of dysentery was 12% in 2005, ranking it third. The proportion of this disease decreased to 4% in 2014, ranking it fifth. The increases in syphilis and HCV were quite significant; syphilis increased from 3% in 2005 to 12% in 2014 (ranking it third in proportion in 2014), and HCV increased from 2% in 2005 to 6% in 2014 (ranking it fourth in proportion in 2014).
Figure 2.
Change in the proportion of cases of the different diseases from 2005 to 2014.
With regard to the numbers of deaths, the disease proportions changed dramatically over the 10 years (Figure 3 ). In 2005, tuberculosis caused the highest proportion of deaths among the 28 class B notifiable diseases. The proportion of tuberculosis deaths decreased from 32% in 2005 to 11% in 2014. The proportion of deaths caused by rabies ranked second among the 28 class B notifiable diseases in 2005. The proportion of deaths caused by rabies decreased from 27% in 2005 to 6% in 2014. The proportion of deaths caused by HBV also decreased, from 12% in 2005 to 3% in 2014. The proportion of deaths caused by AIDS increased dramatically from 12% in 2005 to 78% in 2014.
Figure 3.
Change in the percentage of deaths caused by the different diseases from 2005 to 2014.
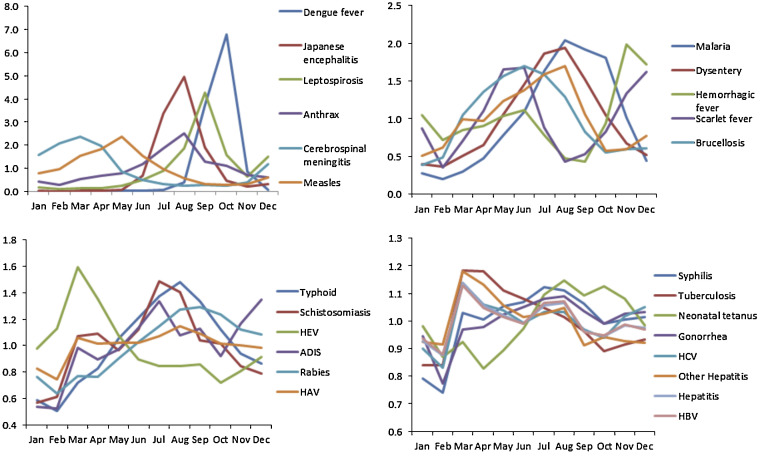
Seasonal indices for each disease are presented in Table 3 and Figure 4 . The standard deviation and range are given in Table 3. There were six diseases for which the seasonal index range was greater than 2: dengue fever (high in September and October, and low in all of the other months), Japanese encephalitis (high from July to September, and low in the other months), leptospirosis (high in September and low from January to June), anthrax (high in August and low from December to April), cerebrospinal meningitis (high from February to April, and low from June to November), and measles (high from March to June, and low from August to December). The seasonal indices for malaria (high from July to September, and low from December to April), dysentery (high from June to September, and low from January to March), haemorrhagic fever (high in November and December, and low in August and September), scarlet fever (high in May and June, and low in February), and brucellosis (high from May to July, and low in January) were between 1 and 2. The variations in hepatitis disease, tuberculosis, and sexually transmitted diseases (STDs) (including gonorrhoea, syphilis, and AIDS) were relatively lower than those of the other diseases.
Table 3.
Seasonal indices for each infectious diseasea
| Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Range | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dengue fever | 0.010 | 0.007 | 0.011 | 0.013 | 0.019 | 0.018 | 0.079 | 0.382 | 3.743 | 6.797 | 0.849 | 0.072 | 6.790 | 2.022 |
| Japanese encephalitis | 0.038 | 0.010 | 0.016 | 0.025 | 0.074 | 0.674 | 3.355 | 4.950 | 1.894 | 0.466 | 0.192 | 0.303 | 4.940 | 1.532 |
| Leptospirosis | 0.173 | 0.094 | 0.121 | 0.129 | 0.238 | 0.487 | 0.887 | 1.866 | 4.272 | 1.592 | 0.649 | 1.491 | 4.178 | 1.157 |
| Anthrax | 0.419 | 0.277 | 0.547 | 0.686 | 0.796 | 1.169 | 1.880 | 2.494 | 1.289 | 1.115 | 0.721 | 0.607 | 2.216 | 0.617 |
| Cerebrospinal meningitis | 1.564 | 2.072 | 2.370 | 1.962 | 0.874 | 0.500 | 0.310 | 0.255 | 0.265 | 0.263 | 0.399 | 1.167 | 2.115 | 0.766 |
| Measles | 0.770 | 0.947 | 1.530 | 1.827 | 2.360 | 1.536 | 0.956 | 0.563 | 0.322 | 0.264 | 0.314 | 0.611 | 2.096 | 0.644 |
| Malaria | 0.276 | 0.203 | 0.297 | 0.479 | 0.788 | 1.095 | 1.633 | 2.041 | 1.923 | 1.810 | 1.016 | 0.439 | 1.838 | 0.664 |
| Dysentery | 0.396 | 0.366 | 0.503 | 0.646 | 1.058 | 1.460 | 1.868 | 1.941 | 1.526 | 1.049 | 0.673 | 0.516 | 1.575 | 0.549 |
| Haemorrhagic fever | 1.043 | 0.714 | 0.848 | 0.902 | 1.039 | 1.113 | 0.783 | 0.479 | 0.430 | 0.938 | 1.986 | 1.723 | 1.556 | 0.435 |
| Scarlet fever | 0.874 | 0.355 | 0.703 | 1.107 | 1.658 | 1.679 | 0.881 | 0.428 | 0.534 | 0.822 | 1.335 | 1.623 | 1.323 | 0.458 |
| Brucellosis | 0.388 | 0.487 | 1.047 | 1.354 | 1.566 | 1.694 | 1.585 | 1.290 | 0.825 | 0.553 | 0.601 | 0.610 | 1.306 | 0.460 |
| Pertussis | 0.503 | 0.613 | 0.994 | 0.974 | 1.239 | 1.377 | 1.587 | 1.702 | 1.061 | 0.576 | 0.597 | 0.777 | 1.199 | 0.390 |
| Typhoid | 0.583 | 0.505 | 0.715 | 0.823 | 1.050 | 1.209 | 1.375 | 1.481 | 1.338 | 1.118 | 0.937 | 0.864 | 0.975 | 0.303 |
| Schistosomiasis | 0.569 | 0.611 | 1.069 | 1.089 | 0.964 | 1.122 | 1.486 | 1.407 | 1.037 | 1.012 | 0.846 | 0.790 | 0.917 | 0.264 |
| Hepatitis E virus | 0.974 | 1.126 | 1.593 | 1.355 | 1.075 | 0.892 | 0.844 | 0.845 | 0.859 | 0.716 | 0.806 | 0.914 | 0.876 | 0.242 |
| AIDS | 0.533 | 0.524 | 0.984 | 0.893 | 0.969 | 1.132 | 1.334 | 1.075 | 1.126 | 0.922 | 1.163 | 1.346 | 0.823 | 0.252 |
| Rabies | 0.761 | 0.634 | 0.768 | 0.762 | 0.900 | 1.026 | 1.147 | 1.271 | 1.292 | 1.233 | 1.123 | 1.081 | 0.658 | 0.218 |
| Hepatitis A virus | 0.828 | 0.745 | 1.059 | 1.017 | 1.020 | 1.019 | 1.070 | 1.149 | 1.092 | 1.016 | 1.003 | 0.982 | 0.404 | 0.106 |
| Syphilis | 0.793 | 0.741 | 1.030 | 1.005 | 1.054 | 1.070 | 1.122 | 1.110 | 1.063 | 0.992 | 1.005 | 1.015 | 0.381 | 0.112 |
| Tuberculosis | 0.839 | 0.841 | 1.183 | 1.181 | 1.111 | 1.080 | 1.048 | 1.016 | 0.965 | 0.890 | 0.916 | 0.932 | 0.344 | 0.117 |
| Neonatal tetanus | 0.983 | 0.869 | 0.925 | 0.827 | 0.893 | 0.973 | 1.097 | 1.146 | 1.094 | 1.127 | 1.082 | 0.984 | 0.319 | 0.103 |
| Gonorrhoea | 0.945 | 0.774 | 0.970 | 0.978 | 1.024 | 1.052 | 1.081 | 1.089 | 1.036 | 0.991 | 1.028 | 1.033 | 0.315 | 0.080 |
| Hepatitis C virus | 0.901 | 0.830 | 1.139 | 1.059 | 1.037 | 0.992 | 1.033 | 1.031 | 0.971 | 0.939 | 1.018 | 1.050 | 0.308 | 0.078 |
| Other hepatitis | 0.923 | 0.915 | 1.181 | 1.132 | 1.056 | 1.014 | 1.027 | 1.049 | 0.911 | 0.942 | 0.927 | 0.921 | 0.270 | 0.088 |
| Hepatitis B virus | 0.935 | 0.880 | 1.129 | 1.048 | 1.016 | 0.990 | 1.066 | 1.072 | 0.961 | 0.947 | 0.988 | 0.969 | 0.249 | 0.066 |
| Diphtheria | 0.000 | 0.000 | 0.000 | 4.019 | 4.041 | 0.000 | 0.000 | 0.000 | 0.000 | 3.940 | 0.000 | 0.000 | 4.041 | 1.732 |
| Avian influenza | 3.337 | 3.325 | 0.843 | 0.563 | 0.000 | 0.557 | 0.000 | 0.281 | 0.000 | 0.000 | 0.849 | 2.245 | 3.337 | 1.203 |
| Polio | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 2.400 | 3.600 | 4.800 | 0.000 | 1.200 | 4.800 | 1.612 |
SD, standard deviation.
The highest value for each disease is highlighted in red and the lowest is highlighted in green. The diseases are ordered according to the value of the range of the seasonal indices.
Figure 4.
Seasonal index for each infectious disease.
From the coefficient of regression (Table 4 ), we can derive how much the incidence changes on average by month after removing the effect of seasonality. The incidence of syphilis increased fastest among the 28 diseases. The syphilis incidence rate increased on average by 0.018626/100 000 every month after adjustment for seasonality. Seven other diseases had an increasing incidence, including HCV (0.010042/100 000), AIDS (0.002891/100 000), brucellosis (0.002242/100 000), scarlet fever (0.001311/100 000), dengue fever (0.000959/100 000), HEV (0.000801/100 000), and schistosomiasis (0.000136/100 000). The incidences of 18 diseases decreased, among which tuberculosis (−0.019143/100 000), dysentery (−0.015704/100 000), and HBV (−0.009740/100 000) dropped fastest.
Table 4.
Regression results for each series on removing the effect of seasonalitya
| Constant | Constant 95% CI | Coefficient | Coefficient 95% CI | p-Value | R2 | |||
|---|---|---|---|---|---|---|---|---|
| Syphilis | 0.890 | 0.805 | 0.975 | 0.018626 | 0.017409 | 0.019843 | 0.05 | 0.89 |
| Hepatitis C virus | 0.335 | 0.299 | 0.371 | 0.010042 | 0.009522 | 0.010563 | 0.01 | 0.93 |
| AIDS | −0.005 | −0.021 | 0.011 | 0.002891 | 0.002661 | 0.003120 | <0.01 | 0.84 |
| Brucellosis | 0.088 | 0.073 | 0.102 | 0.002242 | 0.002036 | 0.002448 | <0.01 | 0.80 |
| Scarlet fever | 0.146 | 0.117 | 0.174 | 0.001311 | 0.000902 | 0.001719 | 0.01 | 0.25 |
| Dengue fever | −0.024 | −0.040 | −0.008 | 0.000959 | 0.000727 | 0.001191 | <0.01 | 0.36 |
| Hepatitis E virus | 0.099 | 0.091 | 0.107 | 0.000801 | 0.000690 | 0.000912 | <0.01 | 0.63 |
| Schistosomiasis | 0.018 | 0.015 | 0.021 | 0.000136 | 0.000095 | 0.000176 | <0.01 | 0.27 |
| Polio | 0.000 | 0.000 | 0.000 | 0.000000 | 0.000000 | 0.000001 | 0.00 | 0.03 |
| Diphtheria | 0.000 | 0.000 | 0.000 | 0.000000 | 0.000000 | 0.000000 | 0.00 | 0.03 |
| Avian influenza | 0.000 | 0.000 | 0.000 | −0.000001 | −0.000001 | 0.000000 | 0.00 | 0.15 |
| Anthrax | 0.003 | 0.003 | 0.003 | −0.000016 | −0.000020 | −0.000013 | <0.01 | 0.43 |
| Leptospirosis | 0.006 | 0.005 | 0.007 | −0.000026 | −0.000038 | −0.000013 | <0.01 | 0.13 |
| Pertussis | 0.019 | 0.016 | 0.021 | −0.000041 | −0.000073 | −0.000009 | <0.01 | 0.05 |
| Japanese encephalitis | 0.027 | 0.021 | 0.033 | −0.000107 | −0.000190 | −0.000024 | <0.01 | 0.05 |
| Cerebrospinal meningitis | 0.012 | 0.012 | 0.013 | −0.000113 | −0.000125 | −0.000101 | <0.01 | 0.76 |
| Rabies | 0.022 | 0.021 | 0.023 | −0.000132 | −0.000146 | −0.000119 | <0.01 | 0.76 |
| Neonatal tetanus | 0.018 | 0.018 | 0.019 | −0.000152 | −0.000159 | −0.000145 | <0.01 | 0.94 |
| Haemorrhagic fever | 0.102 | 0.093 | 0.112 | −0.000346 | −0.000484 | −0.000208 | <0.01 | 0.17 |
| Typhoid | 0.185 | 0.174 | 0.195 | −0.001115 | −0.001264 | −0.000966 | <0.01 | 0.65 |
| Malaria | 0.312 | 0.286 | 0.339 | −0.002941 | −0.003319 | −0.002563 | 0.01 | 0.67 |
| Other hepatitis | 0.546 | 0.532 | 0.559 | −0.003045 | −0.003241 | −0.002848 | <0.01 | 0.89 |
| Hepatitis A virus | 0.522 | 0.502 | 0.541 | −0.003680 | −0.003964 | −0.003396 | <0.01 | 0.85 |
| Gonorrhoea | 1.119 | 1.089 | 1.149 | −0.005472 | −0.005900 | −0.005043 | 0.01 | 0.84 |
| Hepatitis | 9.788 | 9.493 | 10.082 | −0.005616 | −0.009844 | −0.001389 | 0.66 | 0.06 |
| Measles | 0.841 | 0.758 | 0.925 | −0.006769 | −0.007962 | −0.005575 | 0.05 | 0.52 |
| Hepatitis B virus | 8.285 | 8.024 | 8.547 | −0.009740 | −0.013487 | −0.005992 | 0.52 | 0.18 |
| Dysentery | 2.779 | 2.692 | 2.866 | −0.015704 | −0.016949 | −0.014459 | 0.06 | 0.84 |
| Tuberculosis | 9.990 | 9.743 | 10.236 | −0.019143 | −0.022684 | −0.015602 | 0.46 | 0.49 |
CI, confidence interval.
The diseases are ordered by coefficient number.
4. Discussion
The infectious disease surveillance system has been in use for over 10 years since it was established. A descriptive analysis and time series study of 28 class B notifiable diseases was performed. From 2005 to 2014, 38 982 567 cases and 126 372 deaths were reported in the new surveillance system. Figure 2, Figure 3 illustrate the changes in proportions of cases and deaths caused by each disease. The disease spectrum shows the change in the relative severity of each disease. Public health resources are usually limited in developing countries such as China, which has the largest population in the world. Available resources should be properly arranged according to the severity of the disease epidemics.
STDs have become the most severe diseases, especially AIDS and syphilis. During the 10-year period, 273 081 AIDS cases, 3 235 858 syphilis cases, and 1 253 861 gonorrhoea cases were reported in the system. Deaths caused by AIDS increased dramatically, accounting for 78% of all deaths caused by the class B notifiable diseases in 2014. The number of reported syphilis cases increased 3.26 times from 135 210 in 2005 to 441 818 in 2014. The first AIDS case in China was reported in 1985, and the first HIV epidemic was identified in 1989 when a group of HIV infections was detected in Yunnan Province.9 Fewer than 20 000 HIV/AIDS cases were reported before 2000, and the number rose to 780 000 in 2012. It was estimated that 780 000 people were living with HIV/AIDS in China in 2012.10 It has been reported that HIV prevalence among men who have sex with men (MSM) has been rising in China, with an estimated prevalence rate of 7.3% in 2013.11 MSM represent over a quarter of new reported infections; however studies aimed at understanding the epidemic in this population are extremely limited. Another great concern is that the prevalence of AIDS among young people has increased rapidly in China. It has been reported that the prevalence among 15–24-year-olds doubled from 0.9% to 1.7% between 2008 and 2012.11 Research reported by Tucker et al. indicated that very few Chinese people with symptoms of a STD sought medical attention 10–15 years ago.12 If people have become more likely to seek medical attention for these diseases in recent years, then this could have contributed in part to the increase in reported AIDS and syphilis cases seen in the current study.
Tuberculosis is another very severe disease in China, in terms of both occurrence and deaths; 14 088 313 cases were reported from 2005 to 2014, with 21 875 deaths in all. China has the world's second largest tuberculosis epidemic, behind India.13 Progress towards the control of tuberculosis was slow before the 2003 SARS outbreaks and the number of detected tuberculosis cases was only about 30% of the estimated total new cases.14 With the establishment of the new surveillance system, the government has improved public health findings as well as leadership to tackle public health problems. It was reported that the detection of cases of tuberculosis had increased to 80% of the estimated total new cases in 2005, which greatly facilitated the treatment and prevention of this disease.14 Among all the class B diseases, tuberculosis ranked number one in terms of the number of cases in every year from 2005 to 2014. However, the incidence decreased on average by 0.019143/100 000 every month with the effect of seasonality removed.
Hepatitis disease is also a severe disease in China, especially that caused by HBV and HCV, but the prevalence differs according to the type of virus; 15 082 368 cases were reported from 2005 to 2014, with 9624 deaths in all. HBV was the dominant hepatitis virus, accounting for 83% of the entire hepatitis virus cases in 2005, dropping to 78% in 2014. HAV cases accounted for 6% of all hepatitis virus disease in 2005, which decreased to 2% in 2014. HCV increased significantly from 4% in 2005 to 16% in 2014, and HEV also increased from 1% to 2%.
Rabies caused 19 424 deaths during the 10 years from 2005 to 2014. The rabies surveillance program has been reported in previous studies.15 The incidence of rabies decreased dramatically during the 10 years. Various control policies have been implemented by the government, which have played an important role in reducing rabies incidence in China.16
The seasonality of this disease series was analysed. Decomposition methods were used to decompose the surveillance time series data into seasonal patterns and long-term patterns; this can help in gaining an understanding of the behaviour of diseases over time.17 The same methods were used on surveillance data for nine infectious disease for the years 2005–2011 in a previous study.6 Seasonal patterns are one major pathway for the subtle but potentially drastic effects of climate change on disease dynamics.18 In the current study, the seasonal patterns were quantified in the form of seasonal indices. Some of the infectious diseases, such as dengue fever, Japanese encephalitis, leptospirosis, anthrax, cerebrospinal meningitis, and measles, showed more obvious seasonality. Other diseases, such as the STDs, hepatitis disease, and tuberculosis showed relatively smooth seasonal index curves.
According to the hypothesis of decomposition, long-term patterns and residuals remain in the series after seasonal indices are extracted. Modelling the long-term trends is helpful in understanding their epidemic behaviour. The model can be used to predict the future incidence, which is helpful for public health management and vaccine preparation. The long-term patterns of the 28 class B infectious diseases were also shown with a linear regression model between the deseasonalized series (dependent variable) and time t (independent variable). The model showed that most diseases have decreased with improvements in socio-economic status and the strengthening of public health management. However, many diseases are still increasing or emerging, including syphilis, HCV, AIDS, brucellosis, scarlet fever, HEV, and schistosomiasis.
Fighting these diseases is a big challenge. The incidences of STDs (such as AIDS and syphilis), viral hepatitis, and zoonoses (such as rabies, brucellosis, and schistosomiasis) increased dramatically and they caused great numbers of deaths during the 10-year period studied. One of the biggest challenges in combating STDs and viral hepatitis is the health management of floating immigrants; such immigrants were reported to account for 10% of the total Chinese population in 2005.11 They have been found to be more vulnerable to infectious diseases, especially STDs and viral hepatitis. Safe sex education, timely physical testing, and the promotion of protection measures are useful in the prevention of STDs and virus hepatitis. The infection surveillance system needs to be strengthened to cover the floating immigrants.
The transmission of zoonotic infections relies on the interaction between infected animals and humans. Strengthening the management of pets and other animals is urgently needed to combat zoonotic diseases, which are also a great challenge. It has been reported that only 30% of dog owners register their animals with government authorities and that only 2–8% of dogs are vaccinated against rabies;19, 20 this is of great concern in the management of zoonotic disease.
Effective disease surveillance is helpful in understanding the infectious behaviour of diseases with the help of statistical models. This is useful for public health management and disease control. Future studies are needed to explore other statistical methods and data mining techniques to identify the behaviour of infectious diseases and to predict disease occurrence.
Acknowledgements
Xingyu Zhang would like to gratefully acknowledge financial support from the China Scholarship Council.
Financial support: This research was funded by the National Science and Technology Major Special Project “Data mining and analysis of the surveillance data of five syndrome pathogens” (grant number 2012ZX10004201-006). The research was supported by Sichuan University grant “the Fundamental Research Funds for the Central Universities” (grant number: 2016SCU11006). Xingyu Zhang was supported financially by the China Scholarship Council (CSC) for his doctoral studies.
Ethical approval: Ethical approval was not required since the data used in this study are publicly reported surveillance data of the Chinese Centre for Disease Control and Prevention.
Conflict of interest: There are no conflicts of interest in relation to the current study.
Corresponding Editor: Eskild Petersen, Aarhus, Denmark.
Contributor Information
Xiaosong Li, Email: lixiaosong1101@126.com.
Tao Zhang, Email: scdxzhangtao@163.com.
References
- 1.Ortiz E., Clancy C.M. Use of information technology to improve the quality of health care in the United States. Health Serv Res. 2003;38:xi–xxii. doi: 10.1111/1475-6773.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang L, Wang Y, Yang G, Ma J, Wang L, Qi XP. China Information System for Disease Control and Prevention (CISDCP). .
- 3.Kass-Hout T., Zhang X. CRC Press; 2010. Biosurveillance: methods and case studies. [Google Scholar]
- 4.Guo Q., Zhang C., Ji Y., Wang L. Investigation of infectious disease direct reporting network management in Chinese medical institutions. Dis Surveill. 2010;25:410–413. [Google Scholar]
- 5.Zhang L., Wilson D.P. Trends in notifiable infectious diseases in China: implications for surveillance and population health policy. PLoS One. 2012;7:e31076. doi: 10.1371/journal.pone.0031076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang X., Zhang T., Young A.A., Li X. Applications and comparisons of four time series models in epidemiological surveillance data. PLoS One. 2014;9:e88075. doi: 10.1371/journal.pone.0088075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X., Liu Y., Yang M., Zhang T., Young A.A., Li X. Comparative study of four time series methods in forecasting typhoid fever incidence in China. PLoS One. 2013;8:e63116. doi: 10.1371/journal.pone.0063116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang X., Zhang T., Pei J., Liu Y., Li X., Medrano-Gracia P. Time series modelling of syphilis incidence in China from 2005 to 2012. PLoS One. 2016;11:e0149401. doi: 10.1371/journal.pone.0149401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jia Z., Wang L., Chen R.Y., Li D., Wang L., Qin Q. Tracking the evolution of HIV/AIDS in China from 1989-2009 to inform future prevention and control efforts. PLoS One. 2011;6:25671. doi: 10.1371/journal.pone.0025671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Response progress report: Ministry of Health of the People's Republic of China, 2012. China: Ministry of Health; 2012.
- 11.Zhang L., Xiao Y., Lu R., Wu G., Ding X., Qian H. Predictors of HIV testing among men who have sex with men in a large Chinese city. Sex Transm Dis. 2013;40:235. doi: 10.1097/OLQ.0b013e31827ca6b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tucker J.D., Hawkes S.J., Yin Y.P., Peeling R.W., Cohen M.S., Chen X.S. Scaling up syphilis testing in China: implementation beyond the clinic. Bull World Health Organ. 2010;88:452–457. doi: 10.2471/BLT.09.070326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman C. CSIS; 2009. China's capacity to manage infectious diseases: global implications; a Report of the Freeman Chair in China Studies. [Google Scholar]
- 14.Wang L., Liu J., Chin D.P. Progress in tuberculosis control and the evolving public-health system in China. Lancet. 2007;369:691–696. doi: 10.1016/S0140-6736(07)60316-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song M., Tang Q., Rayner S., Tao X.Y., Li H., Guo Z.Y. Human rabies surveillance and control in China, 2005-2012. BMC Infect Dis. 2014;14:212. doi: 10.1186/1471-2334-14-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yin W., Dong J., Tu C., Edwards J., Guo F., Zhou H. Challenges and needs for China to eliminate rabies. Infect Dis Poverty. 2013;2:2–23. doi: 10.1186/2049-9957-2-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grassly N.C., Fraser C. Seasonal infectious disease epidemiology. Proc Biol Sci. 2006;273:2541–2550. doi: 10.1098/rspb.2006.3604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pascual M., Dobson A. Seasonal patterns of infectious diseases. PLoS Med. 2005;2:e5. doi: 10.1371/journal.pmed.0020005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y.Z., Xiong C.L., Xiao D.L., Jiang R.J., Wang Z.X., Zhang L.Z., Fu Z.F. Human rabies in China. Emerg Infect Dis. 2005;11:1983–1985. doi: 10.3201/eid1112.040775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu R.L., Fooks A.R., Zhang S.F., Liu Y., Zhang F. Inferior rabies vaccine quality and low immunization coverage in dogs (Canis familiaris) in China. Epidemiol Infect. 2008;136:1556–1563. doi: 10.1017/S0950268807000131. [DOI] [PMC free article] [PubMed] [Google Scholar]