Abstract
Objectives
To evaluate registered nurse compliance with standard precautions and to analyze the factors that affect compliance.
Methods
Study data were collected over a 3-month period from June to September 2007. The survey research method was used. A total of 1500 randomly sampled registered nurses from 18 hospitals in Hunan, China completed self-report questionnaires.
Results
Of the 1500 nurses included in the study, 1444 returned valid self-report questionnaires. Compliance with standard precautions was found to be low in the surveyed nurses. With a maximum possible score of 80, the quartile range of the overall score for compliance for all nurses was 48.29 (upper quartile score 76.36, lower quartile score 28.07), which was occupied by 64.7% of the participants. The factors most affecting compliance were: standard precautions training (odds ratio (OR) 2.17, 95% confidence interval (CI) 1.85–2.55) and knowledge (OR 1.94, 95% CI 1.01–3.41), followed by hospital grade (OR 1.61, 95% CI 1.79–1.86), presence of sharps disposal box in the department (OR 1.43, 95% CI 1.10–3.41), general self-efficacy (OR 1.29, 95% CI 1.04–1.59), exposure experience (OR 0.69, 95% CI 0.56–0.85), and department in which the nurse worked (OR 1.24, 95% CI 1.05–1.46).
Conclusions
The relevant authorities and hospital infection control department should pay more attention to nurse compliance with standard precautions. Standard precautions training should be strengthened and sufficient practical personal protection equipment provided in order to reduce hospital infections and protect the health of patients and medical staff.
Keywords: Standard precautions, Compliance, Hospital infection, Nursing
1. Introduction
The standard precautions, proposed by the United States Centers for Disease Control and Prevention (CDC) in 1996, are guidelines for reducing the risk of transmission of blood-borne and other pathogens in hospitals. The standard precautions propose that patient blood, body fluid, secretions, and excrement have infectivity, hence isolation measures are necessary. These precautions affect both patients and medical personnel. Isolation measures include avoidance of direct contact with patients and air-borne particles, and require hand washing and sterilization, the use of self-protection equipment, the safe disposal of sharp instruments, etc.
Hospital infections, which pose a serious problem, threatening the health and safety of patients and medical workers worldwide, are infections that arise within the hospital environment. These infections affect the quality of medical care and increase medical care costs. Data from the US CDC show that to the end of the year 2002, of 57 medical workers diagnosed with HIV infection following occupational exposure (including 24 nurses), piercing by a sharp instrument had resulted in 48 infections (84.2%).1 Other studies have also shown evidence of clinical nurses becoming infected due to occupational exposure.2 In a prevalence survey conducted by the World Health Organization (WHO) in 55 hospitals across 14 countries, it was found that 8.7% of in-patients acquire infections in hospital.3 According to Mao et al.,4 the incidence of clinic nurses being pierced with sharp instruments potentially contaminated with infected blood is high. They reported the incidence rate of needlestick injury in nurses to be 80.6%.4
Standard precautions protect patients as well as medical workers and help to control the occurrence of hospital infections. As the incidence of infectious blood diseases has increased and with the spread of non-blood infectious diseases such as avian influenza and severe acute respiratory syndrome worldwide, there has been increased emphasis on standard precautions for medical workers, and research into standard precautions has been carried out in many countries. Research in this area has mostly been limited to the survey of medical worker knowledge, attitude, and practices.
We undertook the current survey, investigating standard precautions knowledge and practice in registered nurses, in order to identify possible corrective factors. This research may provide reference evidence for the associated departments and assist them in instituting policies for preventing nosocomial infections. It may also provide useful information for professional groups formulating training programs to promote the prevention of nosocomial infections.
2. Participants and methods
2.1. Participants
Data were collected over a 3-month period from June to September 2007. One thousand five hundred registered nurses in 18 hospitals in four districts of Hunan Province, China were randomly sampled. Among these 18 hospitals, four are first-class hospitals, eight are second-class hospitals, and six are third-class hospitals. Participants had to be qualified nurses with over 1 year of working experience in a clinical department and had to be willing to fully cooperate in the survey. Those who could not meet the above requirements were excluded from the study.
2.2. Methods
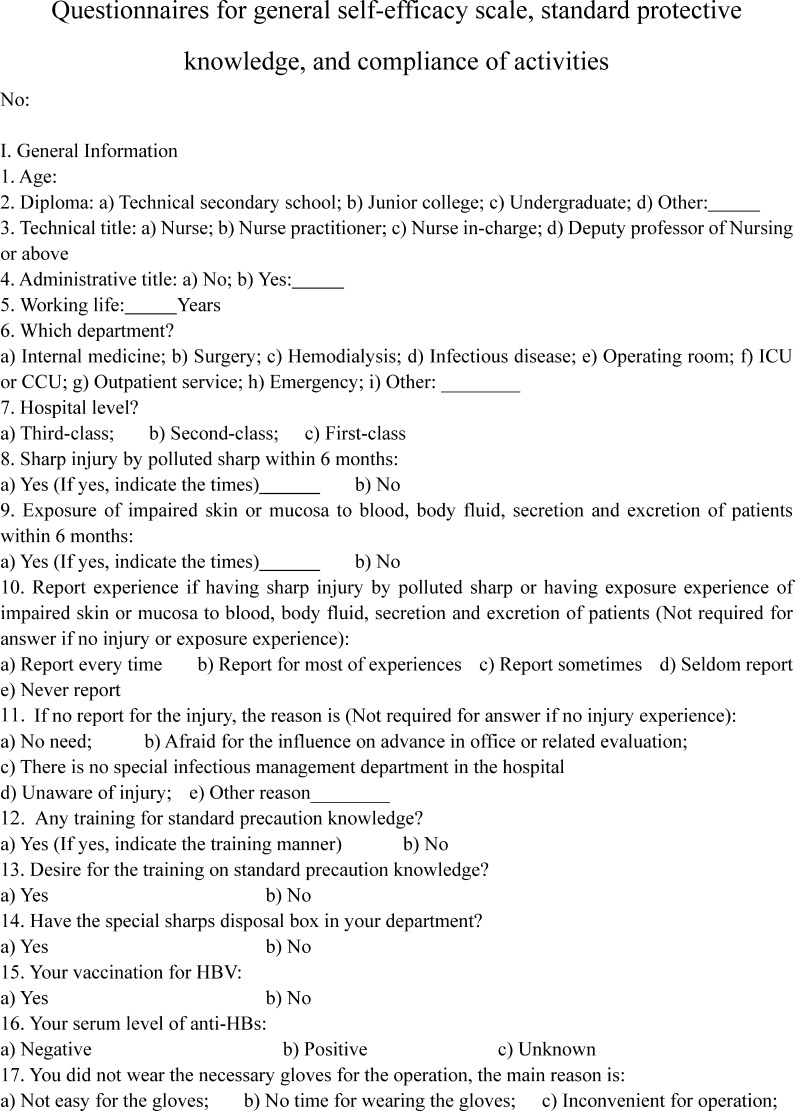
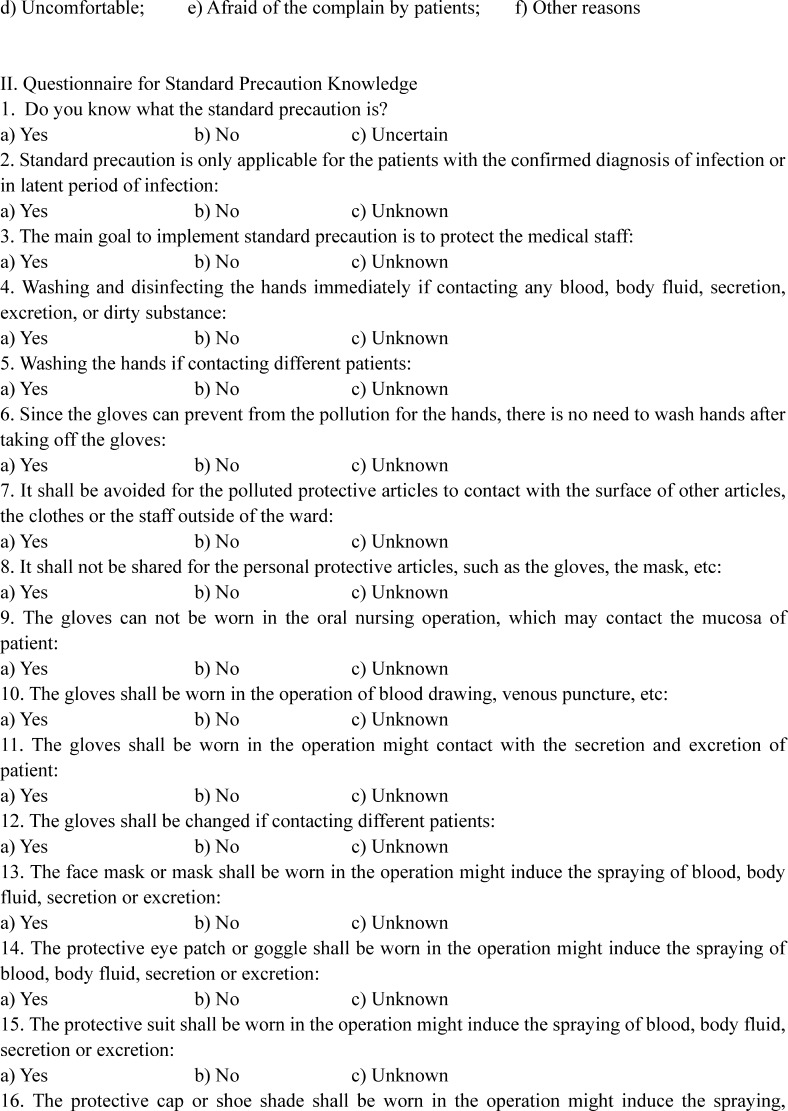
Stratified random proportion sampling was adopted in this survey by use of self-report questionnaires. These consisted of four parts and included (1) standard questions to gather participant information, (2) questions pertaining to standard precautions knowledge, (3) questions on compliance with standard precautions, and (4) a general self-efficacy scale.
Standard precautions knowledge questions were those developed by Askarian et al.,5 Wang,6 and Li and Wang,7 with modifications. They referred to the basic concepts, content, and activity requirements of the standard precautions, covering 20 items, with possible responses of ‘yes’, ‘no’, or ‘unknown’. ‘Yes’ is given a value of 1 point, and ‘no’ or ‘unknown’ 0 points; the maximum possible score is 20. The higher the score, the greater the knowledge about standard precautions the participant has. The validity of the expertise judgments of the standard precautions questions is 0.98, reliability is 0.86, and Cronbach's α is 0.92.
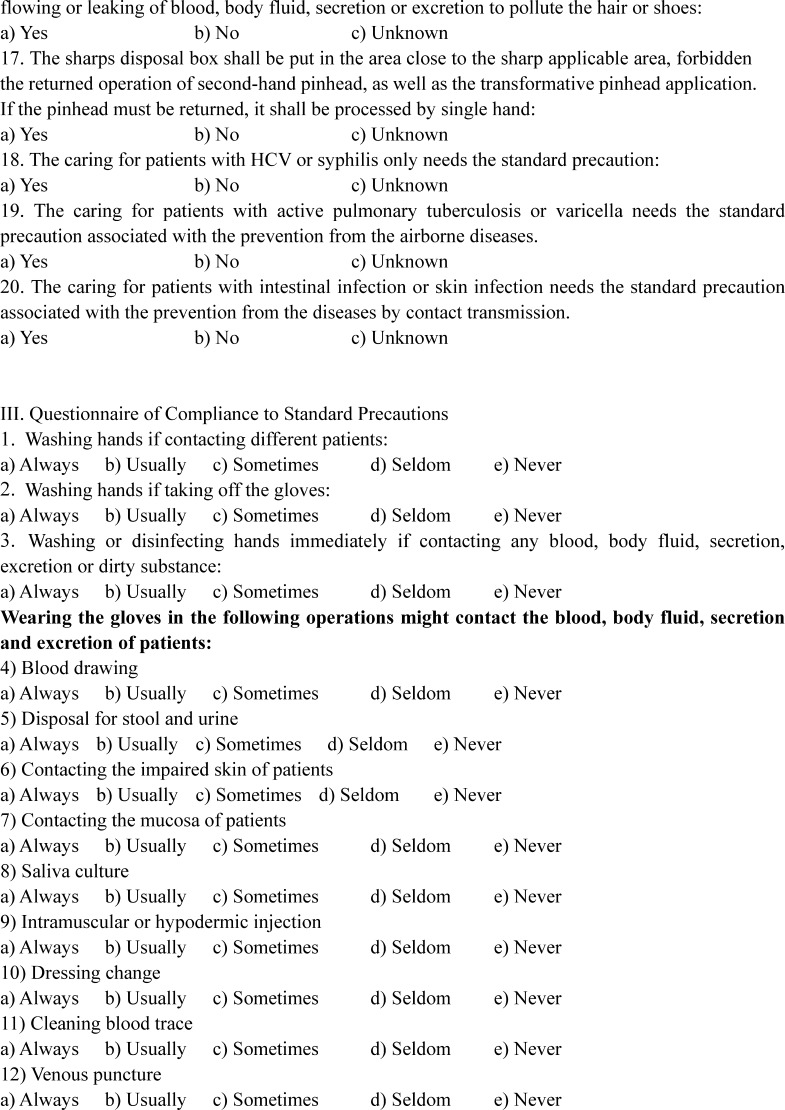
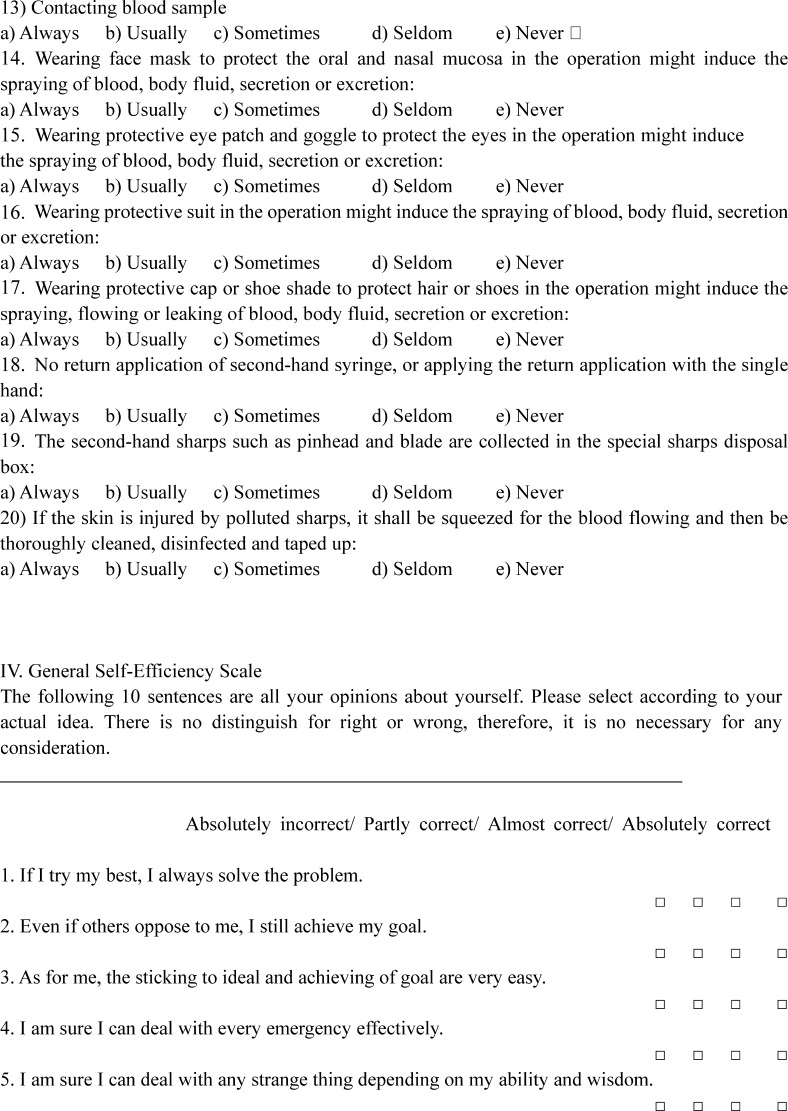
Compliance with standard precautions was determined using the standard precautions questionnaires developed by Askarian et al.,5 Wang,6 and Li and Wang,7 with modifications. There are 20 compliance items with a scale of 0–4 points: 0 = never, 1 = seldom, 2 = sometimes, 3 = usually, and 4 = always, giving a score range of 0–80. The higher the score, the better that person carries out the standard precautions. The validity of the expertise judgments of compliance with standard precautions questions is 0.98, reliability is 0.87, and Cronbach's α is 0.93.
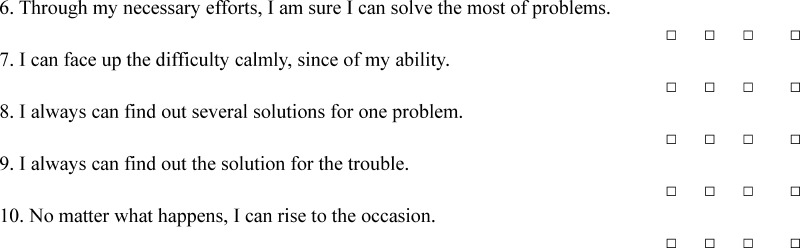
The general self-efficacy scale (GSES) used was that originally devised by German psychologist Schwarzer and colleagues in 1981;8 it has been demonstrated to give a good representation of self-efficacy in a variety of settings.9, 10 The scale is a single-dimension scale, with 10 questions. Each question is assigned points from 1 to 4, and the final score is the average score of the 10 questions. The Chinese version, translated by Chinese scholars, has been proved to have good validity and reliability;11 Cronbach's α is 0.87 and the test–retest reliability is 0.83, while the correlative factor of items with the full score has a range of 0.60–0.77.12
The questionnaires were handed out by the investigators (the authors) at each site, and collected on the spot once they had been completed individually and anonymously by the sampled nurses.
2.3. Statistical analysis
All data were entered into EpiData 3.0 (EpiData Association, Odense, Denmark) and processed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA) with statistical interpretation of frequency distribution and quartile range. Pearson's correlation was used in the analysis of standard precautions knowledge, compliance with standard precautions, and general self-efficacy. Multiple linear stepwise regression was adopted to analyze the factors impacting compliance, with α as standard at 0.05 and p as bilateral probability. Backward stepwise regression analysis was carried out (αin = 0.05, αout = 0.10).
3. Results
3.1. General information
One thousand five hundred registered nurses were surveyed in this study, with a questionnaire return rate of 100%. Of the questionnaires, 1444 were valid, giving a rate of 96.3% qualifying questionnaires. The nurses were all female with an average age of 29 ± 7 years and had been working an average of 9 ± 7 years.
Of the nurses, 60.6% had attended junior college; senior and junior college nurses together accounted for 76.1%. Five hundred and seventy-two nurses (39.6%) worked in the internal medicine departments and 647 (44.8%) worked in surgical departments. Higher grade hospitals are of a higher general level; of the nurses, 14.4% worked in grade I hospitals, 58.6% in grade II hospitals, and 27.0% in grade III hospitals. Prior to this survey, most of the nurses had not suffered any injury as a result of piercing with a sharp instrument and had had no experience of exposure to contamination with patient blood, body fluids, secretions, or excretions. Half of the nurses were fully qualified and half were not in training. The vast majority of the nurses (93.7%) worked in departments equipped with sharps disposal boxes.
3.2. Scoring
With a maximum possible score of 80, the quartile range of the overall score for compliance for all nurses was 48.29 (upper quartile score 76.36, lower quartile score 28.07), which was occupied by 64.7% of the participants. The lowest score was obtained for the use of protection equipment such as eye shields, protective masks, and quarantine clothes. The score was higher for hand washing and sterilization. The score total and scores by item are shown in Table 1 .
Table 1.
Current compliance with standard precautions among nurses (N = 1444)
| Item | Minimum | Maximum | Upper quartile | Lower quartile | Quartile range |
|---|---|---|---|---|---|
| Score total | 22.80 | 80.00 | 76.36 | 28.07 | 48.29 |
| Hand washing and sterilization | 1.33 | 4.00 | 3.95 | 1.94 | 2.01 |
| Shoe covers | 0.30 | 4.00 | 3.62 | 1.21 | 2.41 |
| Other protection equipment | 0.00 | 4.00 | 2.48 | 0.85 | 1.63 |
| Disposal of sharps | 0.33 | 4.00 | 3.87 | 0.89 | 2.98 |
3.3. Analysis
In the analysis, the standard precautions total scores were regarded as dependent variables. Participant general information such as level of experience, number of years in work, education, professional title, administrative function, department of work, presence of sharps disposal box in the department, hospital grade, sharps injuries, exposure to contamination from patients, standard precautions knowledge training, hepatitis B virus vaccine inoculation and serum surface antibody against hepatitis B virus, and participant knowledge and general self-efficacy were regarded as independent variables. Standard precautions and self-efficacy were considered continuous variables, with scores in the range 0–20 and 1–4, respectively. Other variables (non-continuous variables) were processed for quantification; among these were sharps injuries and exposure experience (contamination with blood, body fluids, secretions, or excretions of patients), with 0 times scoring 0 points, one time scoring 1 point, two times scoring 2 points, and three or more times scoring 3 points. Results are shown in Table 2 .
Table 2.
Seven variables and parameters in the linear regression model of factors impacting compliance
| Factors impacting compliance | Standardized regression coefficient | SE | Partial regression coefficient | OR | 95% CI |
|---|---|---|---|---|---|
| Constant | −13.00 | 6.93 | |||
| Training | 3.81 | 1.03 | 0.15 | 2.17 | 1.85–2.55 |
| Knowledge | 0.82 | 0.27 | 0.12 | 1.94 | 1.01–3.41 |
| Hospital grade | 2.36 | 0.88 | 0.12 | 1.61 | 1.79–1.86 |
| Presence of sharps disposal box | 6.09 | 2.25 | 0.12 | 1.43 | 1.10–3.41 |
| General self-efficacy | 0.23 | 0.10 | 0.09 | 1.29 | 1.04–1.59 |
| Exposure experience | −1.35 | 0.58 | −0.09 | 0.69 | 0.56–0.85 |
| Working department | 1.49 | 0.71 | 0.08 | 1.24 | 1.05–1.46 |
SE, standard error; OR, odds ratio; CI, confidence interval.
The standardized regression coefficients in Table 2 show the influence of all the factors impacting compliance – the higher the absolute value the greater the influence on compliance. Table 2 shows the results of seven variables: training, knowledge, hospital grade, sharps disposal box in the department, general self-efficacy, exposure experience, and department in which the nurse worked. The standardized regression coefficient for exposure experience was found to be −1.35, suggesting that less exposure experience results in higher compliance to the standard precautions. When testing this regression equation, F = 24.08 (p = 0.00). This shows that the regression equation and the coefficient of standardized regression were significant (p < 0.05). The multiple correlation coefficient R (0 ≤ R ≤ 1) represents the degree of correlation of multiple impacting factors with activity compliance, with values closer to 1 suggesting a higher degree of correlation. In this investigation, the multiple correlation coefficient R = 0.60, which suggests a high degree of correlation of the above multiple impacting factors with activity compliance. Furthermore, the coefficient of determination R 2 (0 ≤ R 2 ≤ 1) represents the percentage of all impacting factors for the explanation of activity compliance. In this investigation, R 2 = 0.36, which shows that the seven factors impacting compliance can interpret 35.7% of the variation in standard precautions.
Correlation analysis of standard precautions knowledge, general self-efficacy, and compliance with the standard precautions found that standard precautions knowledge was positively correlated with compliance (r = 0.24), suggesting that the greater the standard precautions knowledge the better the activity compliance. General self-efficacy was also positively correlated with compliance (r = 0.21), suggesting that the higher the self-efficacy the better the activity compliance. These results are shown in Table 3 .
Table 3.
Correlation analysis of standard precautions knowledge, general self-efficacy, and precaution compliance (r)
| Variable | r | p-Value |
|---|---|---|
| Knowledge | 0.24 | 0.00 |
| General self-efficacy | 0.21 | 0.00 |
4. Discussion
4.1. Compliance with standard precautions
Compliance with the standard precautions means that nurses should wash and sterilize their hands, use personal protection equipment correctly, and deal effectively with sharp instruments. The self-report questionnaires adopted for this research collected information on hand washing and sterilization, the use of personal protection equipment, and the disposal of sharp instruments.
The scores obtained were similar to those found in the study of Li and Wang7 among clinic nurses (from 116 questionnaires) and the study of Kermode et al.13 among healthcare workers in rural north India (from 266 questionnaires), as well as the results of investigations by Askarian et al.5 on the use of standard precautions by clinicians. Activity compliance was much higher than that found in the research of Shang et al.14 and Wu et al.,15 which may be the result of the different monitoring methods used to study compliance. Moreover, Shang et al.14 also found that there was a significant difference between the actual hand washing rate and the self-evaluated hand washing rate.
In this investigation, we observed that the use of protective items such as eye shields, masks, and quarantine clothes had the lowest compliance. The use of gloves was higher. In fact, gloves were generally found to be readily available in the departments. Reasons given for nurses not using gloves the last time were: the application of gloves will influence the operation (62.6%), too busy to use gloves (19.8%), the patients will complain about the application of gloves (9.9%), gloves are uncomfortable (4.1%), the gloves are not readily available (1.6%), and other reasons (2.0%). In this survey, we also found that most of the clinic departments were not equipped with personal protection items such as eye shields, protective masks, quarantine clothes, and shoe covers. There was relatively higher compliance with hand washing and sterilization and the disposal of sharp instruments. This is mainly related to hospital regulations and repeated education.
4.2. Factors impacting compliance
According to previous investigations, knowledge of standard precautions is lacking in clinicians, nurses, professional personnel involved in infection management, and intern students, as well as other hospital workers. Li and Zhao16 investigated the professional personnel involved in infection management in 22 second-class hospitals in Luoyang City, and found that 25.0% of them did not understand the concepts of standard precautions. Tang et al.17 investigated 108 nurses in internship, and found that only 16.7% knew about the standard precautions. Xu18 investigated knowledge of standard precautions in 55 hospital workers; only 32.0% accepted pre- and post-training, only 16.0% of workers knew the indications for hand washing, though none had learned the correct hand washing method, and only 4.0% knew the scope of the standard precautions. Askarian et al.5 investigated medical practitioners at hospitals in Iran and found that the median levels of knowledge ranged from 6 to 7 (maximum score 9). Monsalve Arteaga et al.19 investigated medical students in Venezuela and found a lack of standard precautions knowledge among these students. Melo et al.20 investigated nurses in one hospital in Goiania, Brazil, and found that only 75.6% understood the standard precautions as protective measures, 52.4% for both professionals and patients and 9.8% for patients with a diagnosed infection.
In our survey of 1444 nurses, only half (n = 722) had knowledge of all the standard precautions or had received training. This indicates that half of the nurses had received no education on the standard precautions at all; some had not even heard about them from other sources. This is consistent with the results of other research. In our survey, 98.2% of nurses indicated their wish to be trained in the standard precautions. Whether in the univariate analysis or multivariate analysis, knowledge of the standard precautions was found to exert a great impact on the individual's compliance with the precautions (r = 0.24). Nurses with standard precautions training had greater precaution compliance than those without standard precautions training. This result is similar to the results found by Zhu and Chen12 and Vaughn et al.21 Our results indicate that senior staff involved in infection management should gain knowledge themselves and also train their employees.
These study results show that knowledge exerts a positive impact on compliance with precautions (OR 1.94). This is consistent with the findings of related research by Chan et al.22 In their survey on the standard precautions in nurses, only 48.0% had knowledge of the concepts, 69.0% had knowledge of the objects, and 31.0% had knowledge of the goals of these precautions; this is because hospitals and schools neglect professional protection education. In a large-scale survey carried out by Chen23 involving 17 medical schools, 88.2% of the schools did not provide courses on occupational protection and 22.2% teachers and 27.7% students had no understanding of occupational nursing protection. Occupational education pays more attention to basic theory and skills training in medical care and nursing. We found that only 50.0% of nurses had received training on the standard precautions.
Our results also show the high impact of hospital grade (OR 1.61), nurse working department (OR 1.24), and presence of a sharps disposal box (OR 1.43) on the individual's compliance with the precautions. In this survey, it was found that nurse protection practices in the smaller hospitals were not as good as in the general hospitals. The reason for this may be that smaller hospitals are more basic, lack good infrastructure, and have no specialized infection administration departments. Additionally, not enough emphasis is put on the control of hospital infections. In terms of nurse working department, the compliance of nurses in the medical departments was lower than for those in the surgical departments. This difference was found to be statistically significant (p < 0.05), and is probably as a result of the greater number of chronic internal medicine and elderly patients in the medical departments. Also, there is no obvious presence of blood in the medical department, which may result in protection being neglected. These results indicate that the administration departments should focus on comprehensive monitoring, especially the monitoring of hospital infections in primary level hospitals.
The availability and ease of use of protective equipment are factors that continue to play an important role in compliance with the standard precautions. Naing et al.24 investigated compliance with glove utilization and factors related to non-compliance in Hospital Universiti Sains Malaysia, and found that ‘stock irregularity’, followed by ‘gloves not available at the emergency sites’, and ‘reduction of tactile sensation’ were the most important factors impacting compliance. Investigations by Ferguson et al.25 into the reasons for non-adherence to standard precautions in community hospitals, showed two related factors – equipment was not available (7%) and the available equipment was not effective (3%). In our survey, it was found that 93.7% of nurses were in departments equipped with sharps disposal boxes; however, when the survey was carried out on location, they did not use these boxes at all. It is known that one-off collection boxes increase department expenses, especially in the grass-roots units. Due to economic constraints, protection equipment cannot always be purchased and provided as required by the regulations. Using needles with bare hands and the recapping of needles by hand are quite common.
This research also shows that sharps injuries and experience of exposure to contamination from a patient 6 months prior to survey exert a great impact on compliance with the standard precautions (OR 0.69). It appears that greater compliance with the standard precautions results in less contamination experience. Compliance to the precautions in nurses without exposure was found to be greater than in nurses with exposure. This proves that the use of the standard precautions will reduce the chances of occupational exposure.
Self-efficacy is the core concept of Bandura's social cognitive theory,26 and is the confidence to control and guide ones own activities. Schwarzer et al.9 believe in the existence of general self-efficacy. General self-efficacy is a general confidence when the individual deals with changeable environments and faces new experiences. Our research results reveal a positive correlation between general self-efficacy and compliance with precautions (r = 0.21). Regression analysis showed general self-efficacy exerts a positive impact on compliance with the standard precautions (OR 1.29). These results are consistent with those of the investigations of Yang27 and Wang and Huang.28
It is very important to ensure the provision of high quality medical care and security by the prevention and control of hospital infections. Nurses play an important role in the prevention and control of hospital infections because they undertake a high proportion of the treatment and care of patients. The standard precautions are a basic measure in the control of hospital infections. Results of our research show that compliance with the standard precautions is low in nurses. According to the activity theory model–health belief model, the formation of health beliefs is critical for the acceptance of advice, the correction of misconduct, and the adoption of health activities. Most health behavior theories suggest that the most proximal influences on health behavior are attitudinal, social influence, self-efficacy, and intention/stage of change variables.29 According to our investigation and analysis, the factors impacting compliance with the standard precautions include: standard precautions training and knowledge, hospital grade, presence of a sharps disposal box in the department, general self-efficacy, exposure to patients, and department in which the nurse works.
In order to reduce hospital infections and protect the health of patients and medical staff, the relevant authorities and hospital infection control departments should pay more attention to nurse compliance with the standard precautions, strengthen standard precautions training, and provide sufficient practical personal protection equipment. Through learning, the attainment of knowledge and skills, and the formation of health beliefs and attitudes, health activity habits can be formed. Only when individuals are familiar with the content and meanings of the standard precautions, with strengthening of the individual's health concepts, can individual practice change so as to improve compliance with precautions. In the mean time, hospital infection administration departments should gather more information on hospital infections and provide immediate feedback from the monitoring results in order to strengthen the education and dissemination of the standard precautions among medical workers. For nurses, the study should be strengthened so as to improve concepts of health and general self-efficacy, to increase compliance with the standard precautions and hence reduce the chances of occupational exposure and hospital infection.
Conflict of interest: No conflict of interest to declare.
Corresponding Editor: Michael Whitby, Brisbane, Australia
Appendix A.
References
- 1.Centers for Disease Control and Prevention. Surveillance of healthcare personnel with HIV/AIDS, as of December 2002. Available at: http://www.cdc.gov/ncidod/dhqp/bp_hiv_hp_with.html (accessed April 2009).
- 2.Mishal Y., Yosefy C., Hay E., Catz D., Ambon E., Schneider R. Risk of transmission of viral disease by needle punctures and cuts in hospital health care works. Harefuah. 1998;135:337–339. [PubMed] [Google Scholar]
- 3.World health Organization. Prevention of hospital-acquired infections. WHO/CDS/CSR/EPH/2002.12. Geneva: World Health Organization; 2002. Available at: http://www.who.int/csr/resources/publications/WHO_CDS_CSR_EPH_2002_12/en/ (accessed October 2010).
- 4.Mao X., Wu X., Yu L. Some clinical nurses in the survey needle stick injury. Chinese Nurs J. 2003;38:422–425. [Google Scholar]
- 5.Askarian M., McLaws M.L., Meylan M. Knowledge, attitude, and practices related to standard precautions of surgeons and physicians in university-affiliated hospitals of Shiraz, Iran. Int J Infect Dis. 2007;11:213–219. doi: 10.1016/j.ijid.2006.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang H. Protection for occupational health investigation. Chinese Nurs Res. 2002;16:331–333. [Google Scholar]
- 7.Li X., Wang L. Standard precaution investigation and the knowledge countermeasures. J Nurs Sci (integrated version) 2005;20:63–65. [Google Scholar]
- 8.Schwarzer R., Born A. Optimistic self-beliefs: assessment of general perceived self-efficacy in thirteen cultures. World Psychology. 1997;3:177–190. [Google Scholar]
- 9.Schwarzer R., Mueller J., Greenglass E. Assessment of general perceived self-efficacy on the Internet: data collection in cyber space. Anxiety Stress Coping. 1999;3:145–161. [Google Scholar]
- 10.Yang T.Z., Shi W.X., Xu L.W. Improvement of self-efficacy: an idea and method for clinical nursing. Chinese Nurs J. 2004;39:393–396. [Google Scholar]
- 11.Wang C., Hu Z., Liu Y. Appliance of general self-efficacy scale reliability and validity. Appl Psychol. 2001;7:37–40. [Google Scholar]
- 12.Zhu H., Chen L. A survey and analysis on status quo of self-protection behavior of nurses in infectious diseases department. Chinese Nurs Res. 2006;20:1045–1047. [Google Scholar]
- 13.Kermode M., Jolley D., Langkham B., Thomas M.S., Holmes W., Gifford S.M. Compliance with universal/standard precautions among health care workers in rural north India. Am J Infect Control. 2005;33:27–33. doi: 10.1016/j.ajic.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Shang S., Zheng X., Wang Y., Huang J., He Y. A survey and analysis on handwashing of clinical nurses. Chinese J Nosocomiol. 2001;11:455–456. [Google Scholar]
- 15.Wu X.J., Ma L.X., Jia Z.X. Influencing factors in handwashing compliance of nursing staff. Chinese J Pract Nurs. 2005;2l:11–13. [Google Scholar]
- 16.Li X.X., Zhao J.K. Study on current situation and counter measure of infection management in second general hospitals in Luo Yang. Henan J Prev Med. 2005;16:367–369. [Google Scholar]
- 17.Tang X.Y., Tan W., Li Y.X. Investigation on occupational exposure status quo and guard knowledge in nursing students. Chinese J Nurs Sci (integrated version) 2006;21:60–66. [Google Scholar]
- 18.Xu T.M. Survey on medical workers’ knowledge towards standard precautions and its countermeasures. J Anhui Health Vocational Tech Coll. 2006;5:8–9. [Google Scholar]
- 19.Monsalve Arteaga L.C., Martínez Balzano C.D., Carvajal De Carvajal A.C. Medical students’ knowledge and attitude towards standard precautions. J Hosp Infect. 2007;65:371–372. doi: 10.1016/j.jhin.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Melo Dde S., Silva e Souza A.C., Tipple A.F., das Neves Z.C., Pereira M.S. Nurses’ understanding of standard precautions at a public hospital in Goiania – GO, Brazil. Rev Lat Am Enfermagem. 2006;14:720–727. doi: 10.1590/s0104-11692006000500013. [DOI] [PubMed] [Google Scholar]
- 21.Vaughn T.E., McCoy K.D., Beekmann S.E., Woolson R.E., Torner J.C., Doebbeling B.N. Factors promoting consistent adherence to safe needle precaution among hospital workers. Infect Control Hosp Epidemiol. 2004;25:548–555. doi: 10.1086/502438. [DOI] [PubMed] [Google Scholar]
- 22.Chan M.F., Ho A., Day M.C. Investigating the knowledge, attitudes and practice patterns of operating room staff towards standard and transmission-based precautions: results of a cluster analysis. J Clin Nurs. 2008;17:1051–1062. doi: 10.1111/j.1365-2702.2007.01998.x. [DOI] [PubMed] [Google Scholar]
- 23.Chen L. Health school nursing education in occupational protection. Pract Prev Med. 2004;11:406–408. [Google Scholar]
- 24.Naing L., Nordin R., Musa R. The prevalence of, and factors related to, compliance with glove utilization among nurses in Hospital Universiti Sains Malaysia. Southeast Asian J Trop Med Public Health. 2001;32:636–642. [PubMed] [Google Scholar]
- 25.Ferguson K.J., Waitzkin H., Beekmann S.E., Doebbeling B.N. Critical incidents of nonadherence with standard precautions guidelines among community hospital-based health care workers. J Gen Intern Med. 2004;19:726–731. doi: 10.1111/j.1525-1497.2004.20424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1997;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 27.Yang Y.L. The analysis about the health promoting the life form and the interrelated factors of clinical medical persons. J Clin Rehabil Tissue Eng Res. 2002;6:2784–2785. [Google Scholar]
- 28.Wang J.Q., Huang Y.H. Study on nurses’ job burnout and the influencing factors. J Nurs Sci. 2006;21:15–17. [Google Scholar]
- 29.Noar S.M., Chabot M., Zimmerman R.S. Applying health behavior theory to multiple behavior change: considerations and approaches. Prev Med. 2008;46:275–280. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]