Summary
Human metapneumovirus (hMPV), discovered in 2001, most commonly causes upper and lower respiratory tract infections in young children, but is also a concern for elderly subjects and immune-compromised patients. hMPV is the major etiological agent responsible for about 5% to 10% of hospitalizations of children suffering from acute respiratory tract infections. hMPV infection can cause severe bronchiolitis and pneumonia in children, and its symptoms are indistinguishable from those caused by human respiratory syncytial virus. Initial infection with hMPV usually occurs during early childhood, but re-infections are common throughout life. Due to the slow growth of the virus in cell culture, molecular methods (such as reverse transcriptase PCR (RT-PCR)) are the preferred diagnostic modality for detecting hMPV. A few vaccine candidates have been shown to be effective in preventing clinical disease, but none are yet commercially available. Our understanding of hMPV has undergone major changes in recent years and in this article we will review the currently available information on the molecular biology and epidemiology of hMPV. We will also review the current therapeutic interventions and strategies being used to control hMPV infection, with an emphasis on possible approaches that could be used to develop an effective vaccine against hMPV.
Keywords: Human metapneumovirus, Viral pneumonia, Bronchiolitis, Respiratory diseases
1. Introduction
Acute respiratory tract infection (ARI) is a leading cause of morbidity and mortality worldwide. Globally, ARIs were responsible for about 20% of total deaths in children less than 5 years of age in 2000 alone; moreover, about 70% of these deaths occurred in Sub-Saharan Africa and the southern regions of Asia.1 ARIs affect children regardless of their economic status, with similar incidence rates in both developed and developing countries, but with a higher mortality rate in developing countries.2 The risk of pneumonia is higher in children in developing countries (10–20%, compared to 3–4% in developed countries).3
A wide range of etiological agents are responsible for respiratory problems in children.4 Although upper respiratory tract infections are generally less serious, they nonetheless carry significant societal costs in terms of lost work, lost school days, and additional health care costs. For this reason, determining the etiological agents of these infections is important. With decades of research and epidemiological studies, we have been able to establish the importance of known viral pathogens like human respiratory syncytial virus (hRSV), parainfluenza virus, influenza virus, coronavirus, and rhinovirus. However, despite these studies, a substantial proportion of respiratory tract infections still cannot be attributed to any known pathogen.
Human metapneumovirus (hMPV) was first discovered in 2001 in the Netherlands, when the virus was isolated from a paediatric patient who had symptoms similar to those of hRSV infection.5 Since then, hMPV has been detected in 4–16% of patients with ARIs.6, 7, 8 The incidence of hMPV may vary from year to year in the same area.9 hMPV causes disease primarily in children, but can infect adults and immunocompromised individuals as well. The clinical features of the illness caused by hMPV infection range from a mild upper respiratory tract infection to life-threatening severe bronchiolitis and pneumonia.
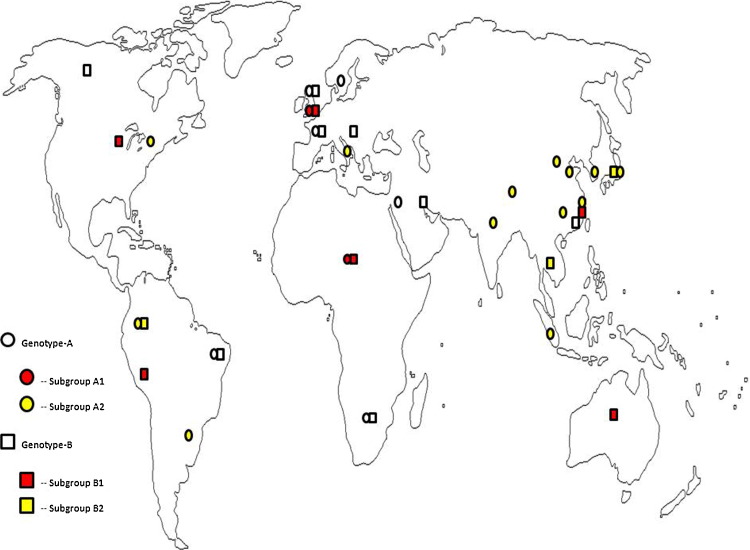
Belonging to the order Mononegavirales, the Paramyxoviridae family is divided into the subfamilies Paramyxovirinae and Pneumovirinae. The Pneumovirinae subfamily is further divided into two genera, Pneumovirus and Metapneumovirus. hRSV is placed under the genus Pneumovirus, while hMPV is placed under the genus Metapneumovirus. Whole genome analysis has shown that hMPV exists as two genotypes, A and B. Based upon the sequence variability of the attachment (G) and fusion (F) surface glycoproteins, these two genotypes are further divided into subgroups A1, A2, B1, and B2. Subgroup A2 is again subdivided into A2a and A2b.10, 11 One study has described a strain that is under major subgroup A, but does not fall into subgroups A1 or A2, and hence there may be a new subgroup evolving in the A major subgroup.12 Study of the molecular biology of hMPV advanced significantly with the establishment of reverse genetics platforms, but we still lack a reliable vaccine to control hMPV infection. Recent findings in hMPV molecular virology, diagnosis, and control strategies are reviewed here.
2. Molecular virology
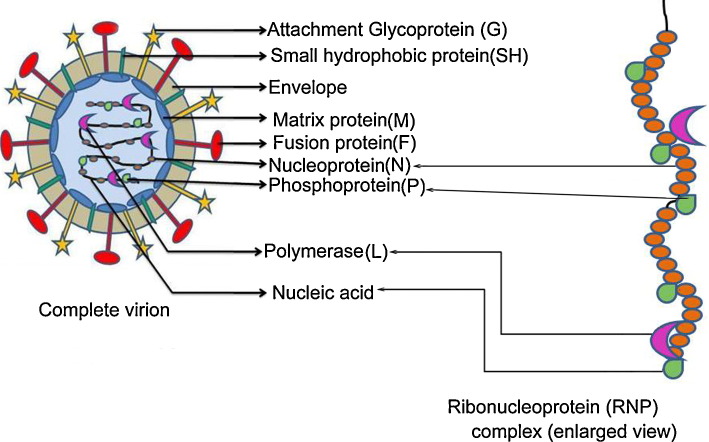
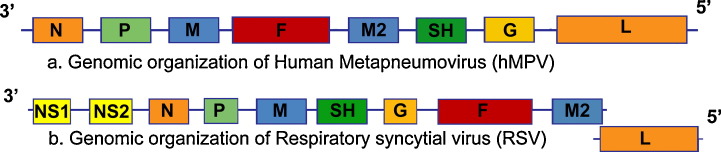
The hMPV virion is pleomorphic in nature and its size varies from 150 nm to 600 nm.5 The genomic orientation of hMPV resembles other members of the Paramyxoviridae family (Figure 1 ). The genome organization of hMPV is quite similar to that of avian pneumovirus (aMPV), particularly type C. The genomes of hMPV and hRSV closely resemble each other, excluding a few differences in the order of the genes and the absence of the non-structural genes from the hMPV genome (Figure 2 ). For hRSV, the two non-structural proteins (NS1 and NS2) have been identified as potent multifunctional antagonists of the interferon (IFN) signalling pathways.13 The absence of these proteins may be the reason for the difference in level of host innate immune response observed during hRSV and hMPV infections.14 The hMPV genome is comprised of negative-sense single-stranded RNA and contains eight genes that code for nine proteins. The order of the genes in the genome (from 3′ to 5′ end) is N–P–M–F–M2–SH–G–L. The proteins are: the nucleoprotein (N protein), the phosphoprotein (P protein), the matrix protein (M protein), the fusion glycoprotein (F protein), the putative transcription factor (M2-1 protein), the RNA synthesis regulatory factor (the M2-2 protein), the small hydrophobic glycoprotein (SH protein), the attachment glycoprotein (G protein), and the viral polymerase (L protein).15 The RNA core is surrounded by M protein and covered by a lipid envelope. This envelope contains the three surface glycoproteins (F, SH, and G), in the form of spikes of approximately 13–17 nm. The core nucleic acids are associated with the P, N, L, M2-1, and M2-2 proteins and form a nucleocapsid 17 nm in diameter. With the help of the G and F proteins, hMPV attaches and fuses to heparan sulphate receptors on the cell surface. After the fusion process, the viral nucleocapsid enters into the cytoplasm of the host cell and undergoes replication. The newly synthesized viral genome assembles with the viral P, N, L, and M2 proteins, and moves towards the host cell membrane. The virion now buds out of the cell, with the F, SH, and G proteins exposed on the outer side of the membrane.16, 17 The P protein acts as a co-factor to stabilize the L protein, allowing the formation of the virus ribonucleoprotein (RNP) complex during virus replication. The M protein plays a crucial role in virus assembly and budding by interacting with the RNP complex. The N protein encapsidates the viral genome and protects it from nuclease activity. In addition to regulating viral transcription and replication, the M2-2 protein plays a major role in virulence by decreasing the host's innate immunity.18, 19 Like other members of the Paramyxoviridae family, hMPV interferes with the host's innate immune system using specific mechanisms. The virus antagonizes cellular responses by regulating pattern recognition receptors, such as toll-like receptor and retinoic acid-inducible gene-like receptors and other signalling molecules.20 Infection interferes with dendritic cell activity and reduces antigen-specific T cell activation.21 Thus, virus clearance remains incomplete and the chances of re-infection occurring increase.
Figure 1.
Schematic diagram of the human metapneumovirus particle and the ribonucleoprotein (RNP) complex.
Figure 2.
Genomic organization of (a) human metapneumovirus (hMPV) and (b) respiratory syncytial virus (RSV), showing the important differences between the two viruses. In comparison to hMPV, RSV expresses two extra proteins, NS1 and NS2, differs in the organization of SH and G proteins, and the reading frames for M2 and L overlap each other. N, nucleoprotein; P, phosphoprotein; M, matrix protein; F, fusion protein; SH, small hydrophobic protein; G, attachment protein; L, large polymerase protein; NS1 and NS2, non-structural proteins 1 and 2.
Members of the two genotypes show much less amino acid and nucleotide similarity (nucleotide 84–86%, amino acid 94–97%) than members of the same subgroup (A1 and A2, or B1 and B2) within the same genotype (nucleotide 94–96%, amino acid 97–99%) based on the F gene sequence.8 Comparing all the subgroups (A1, A2, B1, and B2), the N gene is found to be most conserved at both the nucleotide and the amino acid levels (91.2% and 98.4%, respectively), while the G gene is the least conserved (79% and 59.2%, respectively).22
3. Epidemiology
hMPV has been isolated on all continents and has a seasonal distribution. The geographic distribution of the various hMPV genotypes is given in Figure 3 . Outbreaks occur mainly in the spring and winter months – January to March in the northern hemisphere and June to July in the southern hemisphere.23, 24 A recent study reported that the peak of the hMPV seasonal cases is observed between March and April following the RSV and influenza infection seasons.25 Another study reported that the hMPV infection season overlaps with that of the RSV infection season.26 Being a respiratory infection, hMPV is transmitted by infectious airborne droplets.27 Seroprevalence studies have shown that a high percentage (90–100%) of children have been infected by the time they are 5–10 years old, but re-infection can occur throughout adulthood.5 This may be due to insufficient immunity acquired during the initial infection and/or due to infection by different viral genotypes. The incubation period varies from individual to individual, but is commonly between 3 and 5 days. During animal experimentation, peak viral titres are seen between days 4 and 5 in BALB/c mice and cotton rats.28
Figure 3.
Geographical distribution of hMPV genotypes. Map showing the geographical distribution of hMPV genotypes among humans. Human metapneumovirus isolates are divided into four major subgroups (A1, A2, B1, and B2) and each has its own geographical localization.
hMPV is commonly found in the paediatric population, with high susceptibility rates in children less than 2 years old. hMPV infection in adults normally shows only mild flu-like symptoms. However, in some adult cases (especially elderly adults), severe complications such as chronic obstructive pulmonary disease (COPD) can occur.29 Dyspnoea is more likely in adults as compared to children.30 hMPV infection has also been reported in several immunocompromised patients, such as lung transplant recipients, patients with haematological malignancies, and hematopoietic stem cell transplant recipients.31, 32 Two studies found that both genotypes of hMPV (A and B) co-circulated during a typical respiratory virus season,12, 33 and frequent re-infections with different hMPV genotypes occur.34
Risk factors associated with severe hMPV infection include premature birth, young age, pre-existing nosocomial infection, and underlying chronic pulmonary, heart, or neural disorders.35 Studies investigating the relationship between genotype and disease severity in children have not found any significant correlations. Vicente et al. reported that genotype A may be more virulent that genotype B,36 while Papenburg et al. indicated that it was genotype B that was associated with severe hMPV infection.37 Compared to hMPV-negative children, hMPV-infected children were found to be more likely to require supplemental oxygen, to have a longer stay in the intensive care unit (ICU), and more likely to have undergone chest radiography. About 40% of children hospitalized with hMPV infection were found to have underlying high risk conditions, like asthma and chronic lung disease.38 The average annual rate of hospitalization was about three times more in children less than 6 months old (3/1000) compared to children 6 months to 5 years old (1/1000). Nosocomial infection has been reported in several studies as a mode of transmission.39, 40 The annual rate of hospitalization due to hMPV infection is equal to that of influenza and parainfluenza 1, 2, and 3 combined,38 and a recent analysis of an hMPV outbreak in two skilled nursing facilities showed an 11% mortality rate.41 The severity of disease caused by this recently discovered virus and the importance of hMPV pathogenesis and vaccine research is now becoming clear.
Many studies have reported co-infection of hMPV with other respiratory pathogens, including RSV,42 bocavirus,23 rhinovirus or enterovirus, parainfluenza virus,43 coronavirus,44 influenza A,45 and influenza B.46 hMPV co-infection has also been reported during an outbreak of severe acute respiratory syndrome (SARS).47 Studies have also found hMPV co-infection with bacterial pathogens like Streptococcus pneumoniae, Mycoplasma pneumoniae, and Chlamydia pneumoniae.45 However, the interaction of hMPV with these other etiological agents is unclear, as co-infection does not seem to affect hMPV disease severity.10, 48 There are conflicting reports on the association between RSV–hMPV co-infection and disease severity; some studies found that co-infection leads to an increased rate of ICU admission and hospital stay,49, 50 but others found no association between co-infection and disease severity.51, 52
4. Clinical features
The clinical manifestations of an hMPV infection are indistinguishable from those of an RSV infection, especially in young children. hMPV patients are generally diagnosed with bronchiolitis, bronchitis, and pneumonia. They show common symptoms like fever, cough, hypoxia, upper respiratory tract infection, lower respiratory tract infection, and wheezing.53 However, the most common causes of hospitalization are bronchiolitis and pneumonia.54 The average duration of fever in hMPV-positive cases is about 10 days, with a peak during the course of the illness.55 Young adults with hMPV re-infection show mild cold and flu-like symptoms, with fever in a small proportion of infected cases. However, in the case of elderly patients, re-infection can lead to severe symptoms (such as pneumonitis) and even to death.30 One study reported that 50% of children with hMPV infection were diagnosed with otitis media56 and another study reported that hMPV infection was found in about 8% of children who came to the hospital with wheezing.57 Wheezing is a common clinical symptom observed in multiple studies of children with hMPV-associated lower respiratory tract infections.58 hMPV infections can lead to asthma exacerbations in small children and adults.31 hMPV acts as an enhancer of COPD59 and patients with COPD are more prone to hMPV infection.60, 61 A few reports have also suggested that hMPV infection in children may be associated with a spectrum of central nervous system diseases ranging from febrile seizures to severe encephalitis.62
hMPV was detected by real-time RT-PCR in asymptomatic children, but they had significantly lower viral loads that those found in symptomatic children.63 Higher hMPV viral loads were significantly correlated with the course of illness and disease severity, irrespective of genotype.64 High levels of hMPV viral shedding lasted from 1 to 2 weeks after acute illness.65, 66 hMPV-associated fatal pneumonia has been indicated in the case of a child receiving chemotherapy for acute lymphoblastic leukemia.34 hMPV was found to be the sole etiological agent responsible for the fatal infection of an allogeneic haematopoietic stem cell transplant patient showing interstitial and intra-alveolar pneumonitis with profound alveolar cell damage.32 hMPV infection during the first week after haematopoietic stem cell transplant may be associated with much higher morbidity and mortality rates.66 hMPV can cause a range of illnesses in lung transplant recipients, from a mild upper respiratory tract infection to a severe lower respiratory tract infection.67, 68 In a prospective study involving patients with severe motor and intellectual disabilities, the early stages of hMPV infection were characterized by a low to moderate increase in C-reactive protein (CRP) levels, reduced peripheral blood lymphocytes, and an elevated monocyte ratio.55 Although the peripheral blood lymphocytes and monocyte ratio normalized with the mitigation of symptoms, the CRP levels persisted for some time.55 Along with elevated serum CRP levels, a few hospitalized children infected with hMPV were also reported to have leukopenia and leukocytosis.69
5. Pathogenesis
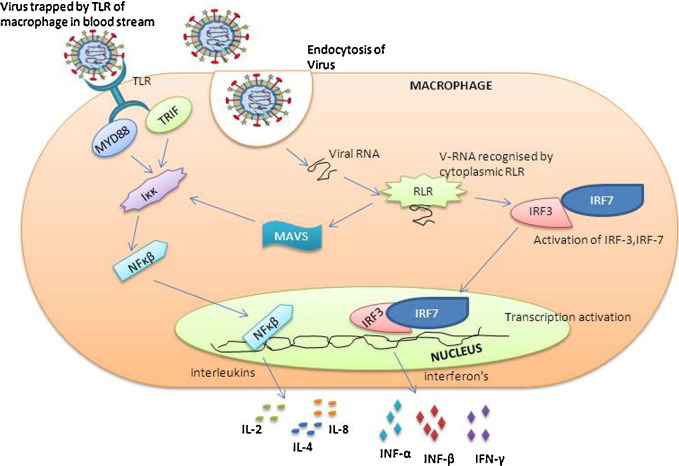
Persistent infection by hMPV may be attributed to a minimal and late immune response, as well as delayed cytotoxic T-lymphocyte activity with impaired virus clearance during primary infection.70 hMPV interferes with superantigen-induced T cell activation by infecting dendritic cells. Thus, the proliferation of antigen-specific CD4+ T cells is restricted and the production of long-term immunity is impaired.21 Respiratory viruses are known to modulate cytokine responses. Compared to RSV and influenza, hMPV is a less effective inducer of different cytokines like interleukin (IL)-12, tumour necrosis factor alpha (TNF-α), IL-6, IL-1β, IL-8, and IL-10.71 hMPV infection induces pulmonary inflammatory changes in BALB/c mice and cotton rats and leads to an increase in the levels of interleukins (IL-2, IL-8, IL-4), interferon (IFN-α), macrophage inflammatory protein 1α, and monocyte chemotactic proteins in the bronchoalveolar lavage fluid and in the lungs. These changes further lead to perivascular and peribronchiolar infiltration and inflammation.31, 72 The formation of intra-alveolar foamy and haemosiderin-laden macrophages, smudge cells, alveolar damage, and hyaline membrane disease are seen in immunological and histopathological investigations.67 It is known that hMPV infection induces toll-like receptor-dependent cellular signalling. However, the role of toll-like receptor-mediated signalling in the host's defence against pulmonary hMPV infection and pathogenesis is unknown. In a recent study, MyD88-deficient mice were shown to have significantly reduced pulmonary inflammation and associated disease compared to wild-type C57BL/6 mice after intranasal infection with hMPV.73 The molecular events in the pathogenesis of hMPV are shown in Figure 4 . To date, there is no clear evidence to determine if hMPV remains limited to the respiratory tract during infection or if the virus can cause a systemic infection. There is some evidence that the latter is possible – one study showed the presence of hMPV in middle ear fluid56 and another showed the presence of hMPV RNA in the brain tissue of a patient who died of encephalitis,74 but further investigation is needed.
Figure 4.
Molecular events in the pathogenesis of hMPV infection. Virus attachment to toll-like receptors (TLR) of macrophage and/or dendritic cells activates several adapter molecules of the immune system (TRIF and MYD88), which in turn activates Nuclear factor kappa beta (NFκβ). RNA of internalized virus is detected by cytoplasmic RIG1-like receptor (RLR), which in turn activates NFκβ by activation of mitochondrial antiviral signalling protein (MAVS) and transcription activators interferon regulatory factors 3 and 7 (IRF-3 and IRF-7). Finally NFκβ and IRFs induce the production of several interferons and interleukins.
6. Diagnosis
Various cell lines, such as Vero cells,75 HEp-2 cells, Hep G2 cells,76 293 cells,29 and LLC-MK2 cells5 have been used for the growth and isolation of hMPV. In a recent study using 19 different cell lines to grow hMPV, it was shown that the most suitable cell lines for the growth of hMPV were a human Chang conjunctiva cell line (clone 1-5C4) and a feline kidney CRFK cell line.77 In cell culture, hMPV has a slow growth rate, with late cytopathic effects varying from the rounding of cells and their detachment from the culture matrix to small syncytium formation. For this reason, the detection of hMPV antigen using anti-hMPV antibody in direct fluorescence or ELISA-based assays is widely used along with cell culture methods.75 The sensitivity and specificity of cell culture detection methods were found to be 68% and 99%, respectively, as compared to real-time RT-PCR detection of hMPV.78 Currently, the use of cell culture for the diagnosis of hMPV infection is uncommon and molecular methods like RT-PCR and/or real-time RT-PCR are more widely used.
Two studies have developed and evaluated multiplex PCR assays with the aim of providing a tool capable of detecting an increasingly complete panel of respiratory viruses.79, 80 With the development of multiplex RT-PCR (mRT-PCR), it is now possible to design a more sensitive and rapid assay for the detection of hMPV. mRT-PCR methods have a sensitivity and specificity of 100% and 96%, respectively, compared to 54.6% and 100% for rRT-PCR.81 Another advantage of mRT-PCR is the ability to detect co-infections, even with very low viral loads that are undetectable via cell culture or immunostaining.82
However, many clinical laboratories do not at present have the capability to perform routine diagnostic RT-PCR for hMPV detection. For rapid and accurate diagnosis of hMPV infections, a combination of immunofluorescence assays and direct fluorescent antibody methods is used as the first-line of diagnosis, followed by RT-PCR on the negative samples.83 In the future, the availability of shell vial centrifugation culture and hMPV monoclonal antibodies will be of significant benefit for the rapid diagnosis of hMPV in clinical laboratories.
7. Treatment and control strategies
Currently, the treatments available for hMPV infection are primarily supportive. But a few reports have raised the possibility of using ribavirin, immunoglobulin, fusion inhibitors, and small interfering ribonucleic acids for the treatment and control of hMPV infection.84, 85, 86, 87, 88, 89, 90, 91 The different strategies used to treat hMPV infection are reviewed in Table 1 . Several vaccine candidates against hMPV have undergone testing in rodent models and non-human primate models. Although they have shown promising results, none has yet been tested in human volunteers. There may be problems – a heat inactivated viral vaccine against hMPV enhanced lung disease when tested in mice.92
Table 1.
Different treatment strategies under development for the prevention of human metapneumovirus (hMPV) infection
| Control strategy | Product | Human/animal model used | Results | Reference |
|---|---|---|---|---|
| Antivirals | Ribavirin | Tissue culture assay | Ribavirin along with intravenous immunoglobulin was found to have antiviral activity against hMPV in vitro | 84 |
| Human | Oral ribavirin combined with intravenous immunoglobulin led to rapid and complete recovery in an immunocompromised child who was undergoing chemotherapy for Burkitt's lymphoma | 85 | ||
| Antibodies | Monoclonal antibody | Mice | On immunization in BALB/c mice, showed significantly reduced lung viral titres, decreased histopathological changes, and decreased airway obstruction post challenge with hMPV | 86 |
| Hamster | Monoclonal antibodies against hMPV F protein showed protection against heterologous hMPV challenge in hamsters | 87 | ||
| Mice | Human monoclonal antibody was able to cross-neutralize hMPV and hRSV and may be used as prophylaxis and therapy for severe hRSV and hMPV | 88 | ||
| Fusion inhibitors | Inhibitory peptides | Mice | Fusion peptides against heptad repeat A and B domains of F protein gave protection against lethal hMPV intranasal challenge in BALB/c mice. Post-challenge there was a significant decrease in lung viral load, pulmonary inflammation, levels of proinflammatory cytokines, and airway obstruction | 89 |
| RNA interference | SiRNA | LLC-MK2 cells | SiRNA targeting P and N genes of hMPV was able to inhibit replication of all subgroups of HMPV in vitro | 90 |
| Mice | Dicer substrate SiRNA reduced lung viral titre post-challenge in mice | 91 | ||
| Inactivated vaccine | Heat inactivated vaccine | Mice | Immunization gave protective immunity against a homologous strain of hMPV followed by intranasal challenge in BALB/c mice | 92 |
| Epitope vaccine | T lymphocyte epitope vaccine | Mice | Immunization reduced viral load, lung pathology, and expression of Th2-type cytokines (IL-10, IL-4) after hMPV challenge | 93 |
| Chimeric vaccine | hMPV antigen on parainfluenza vaccine | African green monkeys, rhesus monkey | Intranasal immunization of African green monkeys induced hMPV-specific humoral and cell-mediated immune response and complete protection from wild-type hMPV challenge. In the rhesus monkey, this vaccine was found to be sufficiently attenuated | 94 |
| Subunit vaccine | hMPV F subunit vaccine | Hamster | Intranasal immunization with recombinant human PIV-1 expressing hMPV F protein vaccine showed high immunogenicity and protection in comparison to the ones expressing G and SH proteins | 95 |
| Cotton rats | Immunization showed reduced nasal viral shedding in cotton rats after hMPV challenge, while the lung pathology was comparable to that of control mice | 96 | ||
| Syrian golden hamsters | Immunization induced high virus neutralization titres against homologous virus. It also showed significantly reduced viral titres in nasal turbinates | 97 | ||
| Cynomolgus macaques | Immunization induced hMPV F specific antibody response, neutralizing antibody, and a robust cellular immune response. However, the induced humoral response waned rapidly over time | 98 | ||
| VLP | Virus-like particles (VLPs) | Mice | Immunization induced cross-protective immunity in mice against both homologous and heterologous strains, along with reduced viral titres in the lungs of immunized animals | 99 |
| Live attenuated vaccine | ΔM2-2 | Hamster | Attenuated and protective in hamsters against Wild type hMPV challenge | 18 |
| ΔG, ΔSH, ΔM2-2 | African green monkeys | ΔG and ΔM2-2 were sufficiently attenuated. After challenge with wild-type hMPV, virus shedding in the lower respiratory tract was undetectable | 101 | |
| ΔM2-2 | Mice | Immunization induced complete protection against challenge with a homologous strain and cross-protective immunity against a heterologous strain | 102 |
hRSV, human respiratory syncytial virus; SiRNA, small interfering RNA; IL, interleukin.
T cell epitope vaccines have been shown to reduce immunomodulation by hMPV challenge. Murine animals immunized with an hMPV cytotoxic T lymphocyte epitope vaccine produced less Th1 and Th2 type cytokines compared to non-immunized mice following hMPV challenge.93 A few studies have also evaluated immunization by chimeric vaccines against hMPV infection. When tested in hamsters and African green monkeys, chimeric vaccines for hMPV were shown to induce the production of neutralizing antibodies and confer immunity against a challenge with the wild-type.94 A subunit vaccine, using the fusion protein of hMPV, has been shown to induce cross-protective immunity against hMPV challenge in the hamster.95 Several hMPV F subunit vaccines have given strong levels of protection when tested in rodents, hamsters, and non-human primates.96, 97, 98 In a recent study, hMPV virus-like particles (VLPs) mimicking the properties of the viral surface of both subgroups A and B were tested as a vaccine candidate. When tested in mice, these VLPs were able to induce a strong humoral immune response against both heterologous and homologous strains.99 Although an hMPV-VLP vaccine seems to be a promising approach, more research is still warranted to develop a vaccine that will be effective against all of the subgroups of hMPV.
The emergence of plasmid-based reverse genetics systems has given a significant boost to efforts to develop a live vaccine against hMPV infection.100 Recombinant hMPVs with SH, G, or M2-2 gene deletions have been evaluated for virus replication levels and it has been shown that the deletion of these genes does not affect the immunogenicity or the antigenicity of the virus.18, 101 In a recent study, a live attenuated vaccine strain of hMPV was developed by changing the glycosylation site of the F protein. This vaccine was found to give complete protection against homologous virus challenge and some protection against heterologous viral challenge, even with a challenge at 56 days post-inoculation.102 All these findings suggest that before an effective vaccine against hMPV can be developed, more detailed knowledge of the molecular pathogenesis of hMPV is required.
8. Conclusions
Human metapneumovirus is a relatively recently described virus1 and hMPV appears to be as dangerous a pathogen as hRSV in terms of morbidity and mortality. As an important respiratory pathogen, understanding hMPV pathogenesis and molecular constraints for severe disease is essential for the treatment of infection and for the development of an effective vaccine against hMPV. Recent studies using animal models for hMPV infection and reverse genetics platforms have shed some light on hMPV pathogenesis and have allowed us to evaluate live vaccine candidates. Now we need to initiate the clinical trials to evaluate the different modalities of treatment available for hMPV infection.
Acknowledgements
The authors are grateful to Dr Nicole Edworthy for her contribution towards the correction of the English language in the manuscript.
Conflict of interest: The authors report no conflicts of interest and have not received any funds for this article.
Corresponding Editor: Eskild Petersen, Aarhus, Denmark
References
- 1.Williams B.G., Gouws E., Boschi-Pinto C., Bryce J., Dye C. Estimates of worldwide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25–32. doi: 10.1016/s1473-3099(01)00170-0. [DOI] [PubMed] [Google Scholar]
- 2.Shapiro E. Epidemiology of acute respiratory infections. Semin Pediatr Infect Dis. 1998;9:31–36. [Google Scholar]
- 3.Broor S., Bharaj P., Chahar H.S. Human metapneumovirus: a new respiratory pathogen. J Biosci. 2008;33:483–493. doi: 10.1007/s12038-008-0067-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weigl J.A., Puppe W., Grondahl B., Schmitt H.J. Epidemiological investigation of nine respiratory pathogens in hospitalized children in Germany using multiplex reverse transcriptase polymerase chain reaction. Eur J Clin Microbiol Infect Dis. 2000;19:336–343. doi: 10.1007/s100960050490. [DOI] [PubMed] [Google Scholar]
- 5.Van den Hoogen B.G., de Jong J.C., Groen J., Kuiken T., de Groot R., Fouchier R.A. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001;7:719–724. doi: 10.1038/89098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner P., Turner C., Watthanaworawit W., Carrara V., Cicelia N., Deglise C. Respiratory virus surveillance in hospitalised pneumonia patients on the Thailand–Myanmar border. BMC Infect Dis. 2013;13:434. doi: 10.1186/1471-2334-13-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu G., Li J., Xie Z., Liu C., Guo L., Vernet G. Human metapneumovirus associated with community-acquired pneumonia in children in Beijing, China. J Med Virol. 2013;85:138–143. doi: 10.1002/jmv.23438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López-Huertas M.R., Casas I., Acosta-Herrera B., García M.L., Coiras M.T., Pérez-Breña P. Two RT-PCR based assays to detect human metapneumovirus in nasopharyngeal aspirates. J Virol Methods. 2005;129:1–7. doi: 10.1016/j.jviromet.2005.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maggi F., Pifferi M., Vatteroni M., Fornai C., Tempestini E., Anzilotti S. Human metapneumovirus associated with respiratory tract infections in a 3-year study of nasal swabs from infants in Italy. J Clin Microbiol. 2003;41:2987–2991. doi: 10.1128/JCM.41.7.2987-2991.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams J.V., Harris P.A., Tollefson S.J., Halburnt R.L., Pingsterhaus J.M., Edwards K.M. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N Engl J Med. 2004;350:443–450. doi: 10.1056/NEJMoa025472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van den Hoogen B.G., Herfst S., Sprong L., Cane P.A., Forleo-Neto E., de Swart R.L. Antigenic and genetic variability of human metapneumoviruses. Emerg Infect Dis. 2004;10:658–666. doi: 10.3201/eid1004.030393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boivin G., Mackay I., Sllots T.P., Madhi S., Freymuth F., Wolf D. Global genetic diversity of human metapneumovirus fusion gene. Emerg Infect Dis. 2004;10:1154–1157. doi: 10.3201/eid1006.031097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo M.S., Brazas R.M., Holtzman M.J. Respiratory syncytial virus non-structural proteins NS1 and NS2 mediate inhibition of Stat2 expression and alpha/beta interferon responsiveness. J Virol. 2005;79:9315–9319. doi: 10.1128/JVI.79.14.9315-9319.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ditt V., Lusebrink J., Tillmann R.L., Schildgen V., Schildgen O. Respiratory infections by HMPV and RSV are clinically indistinguishable but induce different host response in aged individuals. PLoS One. 2011;6:e16314. doi: 10.1371/journal.pone.0016314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biacchesi S., Murphy B.R., Collins P.L., Buchholz U.J. Frequent frame shift and point mutation in the SH gene of human metapneumovirus passaged in vitro. J Virol. 2007;81:6057–6067. doi: 10.1128/JVI.00128-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feuillet F., Lina B., Rosa-Calatrava M., Boivin G. Ten years of human metapneumovirus research. J Clin Virol. 2012;53:97–105. doi: 10.1016/j.jcv.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Chang A., Masante C., Buchholz U.J., Dutch R.E. Human metapneumovirus (HMPV) binding and infection are mediated by interactions between the HMPV fusion protein and heparan sulfate. J Virol. 2012;86:3230–3243. doi: 10.1128/JVI.06706-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schickli J.H., Kaur J., MacPhail M., Guzzetta J.M., Spaete R.R., Tang R.S. Deletion of human metapneumovirus M2-2 increases mutation frequency and attenuates growth in hamsters. Virol J. 2008;5:69. doi: 10.1186/1743-422X-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ren J., Wang Q., Kolli D., Prusak D.J., Tseng C.T., Chen Z.J. Human metapneumovirus M2-2 protein inhibits innate cellular signalling by targeting MAVS. J Virol. 2012;86:13049–13061. doi: 10.1128/JVI.01248-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kolli D., Bao X., Casola A. Human metapneumovirus antagonism of innate immune responses. Viruses. 2012;4:3551–3571. doi: 10.3390/v4123551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cespedes P.F., Gonzalez P.A., Kalergis A.M. Human metapneumovirus keeps dendritic cells from priming antigen-specific naive T cells. Immunology. 2013;139:366–376. doi: 10.1111/imm.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Piyaratna R., Tollefson S.J., Williams J.V. Genomic analysis of four human metapneumovirus prototypes. Virus Res. 2011;160:200–205. doi: 10.1016/j.virusres.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilger D.A., Cantarelli V.V., Amentea S.L., Leistner-Segal S. Detection of human bocavirus and human metapneumovirus by real-time PCR from patients with respiratory symptoms in Southern Brazil. Mem Inst Oswaldo Cruz. 2011;106:56–60. doi: 10.1590/s0074-02762011000100009. [DOI] [PubMed] [Google Scholar]
- 24.Choi E.H., Lee H.J., Kim S.J., Eun B.W., Kim N.H., Lee J.A. The association of newly identified respiratory viruses with lower respiratory tract infections in Korean children, 2000–2005. Clin Infect disease. 2006;43(5):585–592. doi: 10.1086/506350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mizuta K., Abiko C., Akoi Y., Ikeda T., Matsuza Y., Itagaki T. Seasonal patterns of respiratory syncytial virus, influenza A virus, human metapneumovirus and parainfluenza virus type 3 on the basis of virus isolation data between 2004 and 2011 in Yamagata, Japan. Jpn J Infect Dis. 2013;66:140–145. doi: 10.7883/yoken.66.140. [DOI] [PubMed] [Google Scholar]
- 26.Chan P.C., Wang C.Y., Wu P.S., Chang P.Y., Yang T.T., Chiang Y.P. Detection of human metapneumovirus in hospitalized children with acute respiratory tract infection using real-time RT-PCR in a hospital in northern Taiwan. J Formos Med Assoc. 2007;106:16–24. doi: 10.1016/S0929-6646(09)60211-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kahn J.S. Epidemiology of human metapneumovirus. Clin Microbiol Rev. 2006;19:546–557. doi: 10.1128/CMR.00014-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamelin M.E., Cote S., Laforge J., Lampron N., Bourbeau J., Weiss K. Human metapneumovirus infection in adults with community-acquired pneumonia and exacerbation of chronic obstructive pulmonary disease. Clin Infect Dis. 2005;41:498–502. doi: 10.1086/431981. [DOI] [PubMed] [Google Scholar]
- 29.Boivin G., Abed Y., Pelletier G., Ruel L., Moisan D., Cote S. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect Dis. 2002;186:1330–1334. doi: 10.1086/344319. [DOI] [PubMed] [Google Scholar]
- 30.Falsey A.R., Erdman D., Anderson L.J., Walsh E.E. Human metapneumovirus infections in young and elderly adults. J Infect Dis. 2003;187:785–790. doi: 10.1086/367901. [DOI] [PubMed] [Google Scholar]
- 31.Williams J.V., Martino R., Rabella N., Otegui M., Parody R., Heck J.M. A prospective study comparing human metapneumovirus with other respiratory viruses in adults with hematologic malignancies and respiratory tract infections. J Infect Dis. 2005;192:1061–1065. doi: 10.1086/432732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dokos C., Masjosthusmann K., Rellensmann G., Werner C., Schuler L.S., Muller K.M. Fatal human metapneumovirus infection following allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2013;15:97–101. doi: 10.1111/tid.12074. [DOI] [PubMed] [Google Scholar]
- 33.Duchamp M.B., Lina B., Trompette A., Moret H., Motte J., Andreoletti L. Detection of human metapneumovirus RNA sequences in nasopharyngeal aspirates of young French children with acute bronchiolitis by real-time reverse transcriptase PCR and phylogenetic analysis. J Clin Microbiol. 2005;43:1411–1414. doi: 10.1128/JCM.43.3.1411-1414.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pelletier G., Dery P., Abed Y., Boivin G. Respiratory tract re-infections by the new human metapneumovirus in an immunocompromised child. Emerg Infect Dis. 2002;8:976–978. doi: 10.3201/eid0809.020238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Principi N., Esposito S. Paediatric human metapneumovirus infection: epidemiology, prevention and therapy. J Clin Virol. 2014;59:141–147. doi: 10.1016/j.jcv.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 36.Vicente D., Montes M., Cilla G., Perez-Yarza E.G., Perez-Trallero E. Differences in clinical severity between genotype A and genotype B human metapneumovirus infection in children. Clin Infect Dis. 2006;42:111–113. doi: 10.1086/504378. [DOI] [PubMed] [Google Scholar]
- 37.Papenburg J., Carbonneau J., Isabel S., Bergeron M.G., Williams J.V., De Serres G. Genetic diversity and molecular evolution of the major human metapneumovirus surface glycoproteins over a decade. J Clin Virol. 2013;58:541–547. doi: 10.1016/j.jcv.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 38.Edwards K.M., Zhu Y., Griffin M.R., Weinberg G.A., Hall C.B., Szilagyi P.G. New vaccine surveillance network burden of human metapneumovirus infection in young children. N Engl J Med. 2013;368:633–643. doi: 10.1056/NEJMoa1204630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim S., Sung H., Im H.J., Hong S.J., Kim M.N. Molecular epidemiological investigation of a nosocomial outbreak of human metapneumovirus infection in a pediatric hemato-oncology patient population. J Clin Microbiol. 2009;47:1221–1224. doi: 10.1128/JCM.01959-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tu C.C., Chen L.K., Lee Y.S., Ko C.F., Chen C.M., Yang H.H. An outbreak of human metapneumovirus infection in hospitalized psychiatric adult patients in Taiwan. Scand J Infect Dis. 2009;41:363–367. doi: 10.1080/00365540902849375. [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention (CDC) Outbreaks of human metapneumovirus in two skilled nursing facilities—West Virginia and Idaho, 2011–2012. MMWR Morb Mortal Wkly Rep. 2013;62:909–913. [PMC free article] [PubMed] [Google Scholar]
- 42.Greensill J., McNamara P.S., Dove W., Flanagan B., Smyth R.L., Hart C.A. Human metapneumovirus in severe respiratory syncytial virus bronchiolitis. Emerg Infect Dis. 2003;9:372–375. doi: 10.3201/eid0903.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fathima S., Lee B.E., May-Hadford J., Mukhi S., Drews S.J. Use of an innovative web-based laboratory surveillance platform to analyze mixed infections between human metapneumovirus (hMPV) and other respiratory viruses circulating in Alberta (AB), Canada (2009–2012) Viruses. 2012;4:2754–2765. doi: 10.3390/v4112754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Esposito S., Daleno C., Prunotto G., Scalla A. Impact of viral infections in children with community-acquired pneumonia: results of a study of 17 respiratory viruses. Influenza Other Respir Viruses. 2013;7:18–26. doi: 10.1111/j.1750-2659.2012.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin T.Y., Huang Y.C., Tsao K.C., Huang Y.L. Human metapneumovirus and community-acquired pneumonia in children. Chang Gung Med J. 2005;28:683–688. [PubMed] [Google Scholar]
- 46.Ghattas C., Mossad S.B. Fatal human metapneumovirus and influenza B virus coinfection in an allogeneic hematopoietic stem cell transplant recipient. Transpl Infect Dis. 2012;14:e41–e43. doi: 10.1111/j.1399-3062.2012.00766.x. [DOI] [PubMed] [Google Scholar]
- 47.Leung J., Esper F., Weibel C., Kahn J.S. Sero-epidemiology of human metapneumovirus (hMPV) on the basis of a novel enzyme-linked immunosorbent assay utilizing hMPV fusion protein expressed in recombinant vesicular stomatitis virus. J Clin Microbiol. 2005;43:1213–1219. doi: 10.1128/JCM.43.3.1213-1219.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choi E.H., Lee H.J., Kim S.J., Eun B.W., Kim N.H., Lee J.A. The association of newly identified respiratory viruses with lower respiratory tract infections in Korean children, 2000–2005. Clin Infect Dis. 2006;43:585–592. doi: 10.1086/506350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Semple M.G., Cowell A., Dove W., Greensill J., McNamara P.S., Halfhide C. Dual infection of infants by human metapneumovirus and human respiratory syncytial virus is strongly associated with severe bronchiolitis. J Infect Dis. 2005;191:382–386. doi: 10.1086/426457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Foulongne V., Guyon G., Rodière M., Segondy M. Human metapneumovirus infection in young children hospitalized with respiratory tract disease. Pediatr Infect Dis J. 2006;25:354–359. doi: 10.1097/01.inf.0000207480.55201.f6. [DOI] [PubMed] [Google Scholar]
- 51.Van Woensel J.B., Bos A.P., Lutter R., Rossen J.W., Schuurman R. Absence of human metapneumovirus co-infection in cases of severe respiratory syncytial virus infection. Pediatr Pulmonol. 2006;41:872–874. doi: 10.1002/ppul.20459. [DOI] [PubMed] [Google Scholar]
- 52.Lazar I., Weibel C., Dziura J., Ferguson D., Landry M.L., Kahn J.S. Human metapneumovirus and severity of respiratory syncytial virus disease. Emerg Infect Dis. 2004;10:1318–1320. doi: 10.3201/eid1007.030983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boivin G., De Serres G., Cote S., Gilca R., Abed Y., Rochette L. Human metapneumovirus infections in hospitalized children. Emerg Infect Dis. 2003;9:634–640. doi: 10.3201/eid0906.030017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Matsuda S., Nakamura M., Hirano E., Kiyota N., Omura T., Suzuki Y. Characteristics of human metapneumovirus infection prevailing in hospital wards housing patients with severe disabilities. Jpn J Infect Dis. 2013;66:195–200. doi: 10.7883/yoken.66.195. [DOI] [PubMed] [Google Scholar]
- 55.Van den Hoogen B.G., van Doornum G.J., Fockens J.C., Cornelissen J.J., Beyer W.E., de Groot R. Prevalence and clinical symptoms of human metapneumovirus infection in hospitalized patients. J Infect Dis. 2003;188:1571–1577. doi: 10.1086/379200. [DOI] [PubMed] [Google Scholar]
- 56.Williams J.V., Tollefson S.J., Nair S., Chonmaitree T. Association of human metapneumovirus with acute otitis media. Int J Pediatr Otorhinolaryngol. 2006;70:1189–1193. doi: 10.1016/j.ijporl.2005.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jartti T., van den Hoogen B.G., Garofalo R.P., Osterhaus A.P., Ruuskanen O. Metapneumovirus and acute wheezing in children. Lancet. 2002;360:1393–1394. doi: 10.1016/S0140-6736(02)11391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Williams J.V., Crowe J.E., Jr., Enriquez R., Minton P., Peebles R.S., Jr., Hamilton R.G. Human metapneumovirus infection plays an etiologic role in acute asthma exacerbations requiring hospitalization in adults. J Infect. 2005;192:1149–1153. doi: 10.1086/444392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Perotin J.M., Dury S., Renois F., Deslee G., Wolak A., Duval V. Detection of multiple viral and bacterial infections in acute exacerbation of chronic obstructive pulmonary disease: a pilot prospective study. J Med Virol. 2013;85:866–873. doi: 10.1002/jmv.23495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ilvan A., Aslan G., Serin M.S., Calıkoglu M., Yılmaz F.M., Tezcan S. Investigation of the presence of human metapneumovirus in patients with chronic obstructive pulmonary disease and asthma and its relationship with the attacks. Mikrobiyol Bul. 2013;47:636–649. doi: 10.5578/mb.6041. [DOI] [PubMed] [Google Scholar]
- 61.Jain B., Singh A.K., Dangi T., Agarwal A., Verma A.K., Dwivedi M. High prevalence of human metapneumovirus subtype B in cases presenting as severe acute respiratory illness: an experience at tertiary care hospital. Clin Respir J. 2014;8(2):225–233. doi: 10.1111/crj.12064. [DOI] [PubMed] [Google Scholar]
- 62.Arnold J.C., Singh K.K., Milder E., Spector S.A., Sawyer M.H., Gavali S. Human metapneumovirus associated with central nervous system infection in children. Pediatr Infect Dis J. 2009;28:1057–1060. doi: 10.1097/INF.0b013e3181acd221. [DOI] [PubMed] [Google Scholar]
- 63.Bosis S., Esposito S., Osterhaus A.D., Tremolati E., Begliatti E., Tagliabue C. Association between high nasopharyngeal viral load and disease severity in children with human metapneumovirus infection. J Clin Virol. 2008;42:286–290. doi: 10.1016/j.jcv.2008.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Peng D., Zhao X., Liu E., Huang Y., Yang X., Zhao Y. Analysis of viral load in children infected with human metapneumovirus. Iran J Pediatr. 2010;20:393–400. [PMC free article] [PubMed] [Google Scholar]
- 65.Talaat K.R., Karron R.A., Thumar B., MacMohan B.A., Schmidt A.C., Collins P.L., Buchholz U.J. Experimental infection of adults with recombinant wild-type human metapneumovirus. J Infect Dis. 2013;208(10):1669–1678. doi: 10.1093/infdis/jit356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Englund J.A., Boeckh M., Kuypers J., Nichols W.G., Hackman R.C., Morrow R.A. Brief communication: fatal human metapneumovirus infection in stem-cell transplant recipients. Ann Intern Med. 2006;144:344–349. doi: 10.7326/0003-4819-144-5-200603070-00010. [DOI] [PubMed] [Google Scholar]
- 67.Sumino K.C., Agapov E., Pierce R.A., Trulock E.P., Pfeifer J.D., Ritter J.H. Detection of severe human metapneumovirus infection by real-time polymerase chain reaction and histopathological assessment. J Infect Dis. 2005;192:1052–1060. doi: 10.1086/432728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hopkins M.J., Redmond C., Shaw J.M., Hart I.J., Hart C.A., Smyth R.L. Detection and characterisation of human metapneumovirus from children with acute respiratory symptoms in north-west England. UK. J Clin Virol. 2008;42:273–279. doi: 10.1016/j.jcv.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 69.Wei Y.H., Tsao K.C., Huang C.G., Huang Y.C., Lin T.Y. Clinical feature of different genotypes/genogroups of human metapneumovirus in hospitalized children. J Microbiol Immunol Infection. 2013;46:352–357. doi: 10.1016/j.jmii.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 70.Alvarez R., Tripp R.A. The immune response to human metapneumovirus is associated with aberrant immunity and impaired virus clearance in BALB/c mice. J Virol. 2005;79:5971–5978. doi: 10.1128/JVI.79.10.5971-5978.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Laham F.R., Israele V., Casellas J.M., Garcia A.M., Lac Prugent C.M., Hoffman S.J. Differential production of inflammatory cytokines in primary infection with human metapneumovirus and with other common respiratory viruses of infancy. J Infect Dis. 2004;189:2047–2056. doi: 10.1086/383350. [DOI] [PubMed] [Google Scholar]
- 72.Lara M., Ghosh A., Plata A. Critical role of MDA5 in the interferon response induced by human metapneumovirus infection in dendritic cells and in vivo. J Virol. 2012;87:1242–1251. doi: 10.1128/JVI.01213-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ren J., Kolli D., Deng J., Fang R., Gong B., Xue M. MyD88 controls human metapneumovirus-induced pulmonary immune responses and disease pathogenesis. Virus Res. 2013;176:241–250. doi: 10.1016/j.virusres.2013.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schildgen O., Glatzel T., Geikowski T., Scheibner B., Matz B., Bindl L. Human metapneumovirus RNA in encephalitis patient. Emerg Infect Dis. 2005;11:467–470. doi: 10.3201/eid1103.040676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tollefson S.J., Cox R.G., Williams J.V. Studies of culture conditions and environmental stability of human metapneumovirus. Virus Res. 2010;151:54–59. doi: 10.1016/j.virusres.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schildgen V., Lusebrink J., Ditt V., Tillmann R., Simon A., Muller A. Human HepG2 cells support respiratory syncytial virus and human metapneumovirus replication. J Virol Methods. 2010;163:74–81. doi: 10.1016/j.jviromet.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 77.Isaeva E.I., Kozulina I.S., Podcherniaeva R.I., Grinkevich O.M. Reproduction of the metapneumovirus in different cell lines. Vopr Virusol. 2012;57:19–23. [PubMed] [Google Scholar]
- 78.Matsuzaki Y., Mizuta K., Takashita E., Okamoto M., Itagaki T., Katsushima F. Comparison of virus isolation using the Vero E6 cell line with rt RT-PCR assay for detection of hMPV. BMC Infect Dis. 2010;10:170. doi: 10.1186/1471-2334-10-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pujol B.S., Vabret A., Legrand L., Dina J., Gouarin S., Lecherbonnier J.P. Development of three multiplex RT-PCR assays for the detection of 12 respiratory RNA viruses. J Virol Methods. 2005;126:53–63. doi: 10.1016/j.jviromet.2005.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Litwin C.M., Bosley J.G. Seasonality and prevalence of respiratory pathogens detected by multiplex PCR at a tertiary care medical centre. Arch Virol. 2014;159(1):65–72. doi: 10.1007/s00705-013-1794-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bharaj P., Sullender W.M., Kabra S.K., Mani K., Cherian J., Tyagi V. Respiratory viral infections detected by multiplex PCR among pediatric patients with lower respiratory tract infections seen at an urban hospital in Delhi from 2005 to 2007. Virol J. 2009;6:89. doi: 10.1186/1743-422X-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Choudhury M.L., Anand S.P., Heydari M., Rane G., Potdar V.A., Chandha M.S. Development of a multiplex one step RT PCR that detects eighteen respiratory viruses in clinical specimens in comparison with real time RT-PCR. J Virol Methods. 2013;189:15–19. doi: 10.1016/j.jviromet.2012.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jokela P., Piiparinen H., Luiro K., Lappalainen M. Detection of hMPV and RSV by duplex real time PCR assay in comparison with DFA. Clin Microbiol Infect. 2012;16:1568–1573. doi: 10.1111/j.1469-0691.2010.03191.x. [DOI] [PubMed] [Google Scholar]
- 84.Wyde P.R., Chetty S.N., Jewell A.M., Boivin G., Piedra P.A. Comparison of the inhibition of human metapneumovirus and respiratory syncytial virus by ribavirin and immune serum globulin in vitro. Antiviral Res. 2003;60:51–59. doi: 10.1016/s0166-3542(03)00153-0. [DOI] [PubMed] [Google Scholar]
- 85.Kitanovski L., Kopriva S., Pokorn M., Dolnicar M.B., Rajic V., Stefanovic M. Treatment of severe human metapneumovirus pneumonia in an immunocompromised child with oral ribavirin and IVIG. J Pediatr Hematol Oncol. 2013;35:e311–e313. doi: 10.1097/MPH.0b013e3182915d2d. [DOI] [PubMed] [Google Scholar]
- 86.Hamelin M.E., Gagnon C., Prince G.A., Kiener P., Suzich J., Ulbrandt N. Prophylactic and therapeutic benefits of a monoclonal antibody against the fusion protein of human metapneumovirus in a mouse model. Antiviral Res. 2010;88:31–37. doi: 10.1016/j.antiviral.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 87.Ulbrandt N.D., Ji H., Patel N.K., Riggs J.M., Brewah Y.A., Ready S. Isolation and characterization of monoclonal antibodies which neutralize human metapneumovirus in vitro and in vivo. J Virol. 2006;80:7799–7806. doi: 10.1128/JVI.00318-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Corti D., Bianchi S., Vanzetta F., Minola A., Perez L., Agatic G. Cross-neutralization of four paramyxoviruses by a human monoclonal antibody. Nature. 2013;501:439–443. doi: 10.1038/nature12442. [DOI] [PubMed] [Google Scholar]
- 89.Deffrasness C., Hamelin M.E., Prince G.A., Boivin G. Identification and evaluation of a highly effective fusion inhibitor for human metapneumovirus. Antimicrob Agents Chemother. 2008;52:279–287. doi: 10.1128/AAC.00793-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Deffrasnes C., Cavanagh M.H., Goyette N., Cui K., Ge Q., Seth S. Inhibition of human metapneumovirus replication by small interfering RNA. Antivir Ther. 2008;13:821–832. [PubMed] [Google Scholar]
- 91.Darniot M., Schildgen V., Schildgen O., Sproat B., Kleines M., Ditt V. RNA interference in vitro and in vivo using Dsi RNA targeting the nucleocapsid N mRNA of human metapneumovirus. Antiviral Res. 2012;93:364–373. doi: 10.1016/j.antiviral.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 92.Hamelin M.E., Couture C., Sackett M.K., Boivin G. Enhanced lung disease and Th2 response following human metapneumovirus infection in mice immunized with the inactivated virus. J Gen Virol. 2007;88:3391–3400. doi: 10.1099/vir.0.83250-0. [DOI] [PubMed] [Google Scholar]
- 93.Herd K.A., Mahalingam S., Mackay I.M., Nissen M., Sloots T.P., Tindle R.W. Cytotoxic T-lymphocyte epitope vaccination protects against human metapneumovirus infection and disease in mice. J Virol. 2006;80:2034–2044. doi: 10.1128/JVI.80.4.2034-2044.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tang R.S., Schickli J.H., MacPhail M., Fernandes F., Bicha L., Spaete J. Effects of human metapneumovirus and respiratory syncytial virus antigen insertion in two 3′ proximal genome positions of bovine/human parainfluenza virus type 3 on virus replication and immunogenicity. J Virol. 2003;77:10819–10828. doi: 10.1128/JVI.77.20.10819-10828.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Skiadopolous M.H., Biacchesi S., Buchholz U.J., Amaro-Carambot E., Surman S.R., Collins P.L. Individual contributions of the human metapneumovirus F, G, and SH surface glycoproteins to the induction of neutralizing antibodies and protective immunity. Virology. 2006;345:492–501. doi: 10.1016/j.virol.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 96.Cseke G., Wright D.W., Tollefson S.J., Johnson J.E., Crowe J.E., Jr., Williams J.V. Human metapneumovirus fusion protein vaccines that are immunogenic and protective in cotton rats. J Virol. 2007;81:698–707. doi: 10.1128/JVI.00844-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Herfst S., de Graaf M., Schrauwen E.J., Ulbrandt N.D., Barnes A.S., Senthil K. Immunization of Syrian golden hamsters with F subunit vaccine of human metapneumovirus induces protection against challenge with homologous or heterologous strains. J Gen Virol. 2007;88:2702–2709. doi: 10.1099/vir.0.83084-0. [DOI] [PubMed] [Google Scholar]
- 98.Herfst S., Schrauwen E.J., de Graaf M., van Amerongen G., van den Hoogen B.G., de Swart R.L. Immunogenicity and efficacy of two candidate human metapneumovirus vaccines in cynomolgus macaques. Vaccine. 2008;26:4224–4230. doi: 10.1016/j.vaccine.2008.05.052. [DOI] [PubMed] [Google Scholar]
- 99.Levy C., Aerts L., Hamelin M.E., Granier C., Szecsi J., Lavillette D. Virus like particle vaccine induces cross protection against human metapneumovirus infection in mice. Vaccine. 2013;31:2778–2785. doi: 10.1016/j.vaccine.2013.03.051. [DOI] [PubMed] [Google Scholar]
- 100.Smith K. The use of plasmid-based reverse genetics to generate influenza virus strains for improved vaccine production. MMG 445 Basic Biotechnology eJournal. 2007;3:123–130. [Google Scholar]
- 101.Biacchesi S., Pham Q.N., Skiadopoulos M.H., Murphy B.R., Collins P.L., Buchholz U.J. Infection of nonhuman primates with recombinant human metapneumovirus lacking the SH, G, or M2-2 protein categorizes each as a nonessential accessory protein and identifies vaccine candidates. J Virol. 2005;79:12608–12613. doi: 10.1128/JVI.79.19.12608-12613.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu P., Shu Z., Qin X., Dou Y., Zhao Y., Zhao X. A live attenuated human metapneumovirus vaccine strain provides complete protection against homologous viral infection and cross-protection against heterologous viral infection in BALB/c Mice. Clin Vaccine Immunol. 2013;20:1246–1254. doi: 10.1128/CVI.00145-13. [DOI] [PMC free article] [PubMed] [Google Scholar]