Summary
Since the initial description of the Middle East respiratory syndrome (MERS) in September 2012, a total of 1038 cases of MERS-CoV including 460 deaths have been reported from Saudi Arabia. From August 24, 2013 to September 3, 2013, a total of 397 patients and contacts were tested for MERS-CoV. Of those tested, there were 18 (4.5%) MERS-CoV cases reported in Al-Madinah al-Munawwarah with one large cluster. In this report, we describe the outcome, epidemiology and clinical characteristics of this cluster of which 4 cases involved healthcare workers. Fourteen cases appeared to be linked to one cluster involving healthcare workers (HCWs), family and patient contacts. Of the 18 cases, five (including 2 HCWs) were community acquired, two were household contacts, and 11 were healthcare associated (including 4 HCWs). All except 4 cases were symptomatic and the case fatality rate was 39% (7 of 18). The outbreak resulted in human to human transmission of an estimated 6 cases. Contact screening showed positive test in 1 of 56 (1.8%) household contacts, and 3 of 250 (1.2%) HCWs.
Keywords: Middle East, Clusters, MERS-CoV, RT-PCR, Coronavirus
1. Introduction
Since Middle East respiratory syndrome (MERS) was described in September 2012, a total of 1038 cases of MERS-CoV including 460 deaths have been reported from Saudi Arabia [1]. The current case fatality rate is lower than the initial rate of 65% [2]. MERS-CoV is known to cause three patterns of transmissions [2], [3], [4], [5], [6], [7], [8]: sporadic cases, community-transmission [9] and healthcare associated transmissions such as the case in the Zarqa, Jordan [10], [11], Al-Hasa, Saudi Arabia [12] and Jeddah, Saudi Arabia [13], [14]. The exact source of the infection for most patients remains unknown. In this report, we describe the outcome, epidemiology and clinical characteristics of this cluster of MERS-CoV in Al-Madinah al-Munawwarah of which 4 cases involved healthcare workers.
2. Methods
All samples were tested in Jeddah regional lab. We included all MERS-CoV cases reported from Al-Madinah al-Munawwarah between August 24, 2013 and September 3, 2013. A confirmed case of MERS CoV is defined as an isolation of MERS CoV from a nasopharyngeal or a respiratory sample by real time reverse transcriptase PCR, as described previously [12], [15]. Clinical information included demographic data, clinical symptoms and signs, co-morbidities, and contact with animals.
3. Results
3.1. MERS-CoV cases and clusters
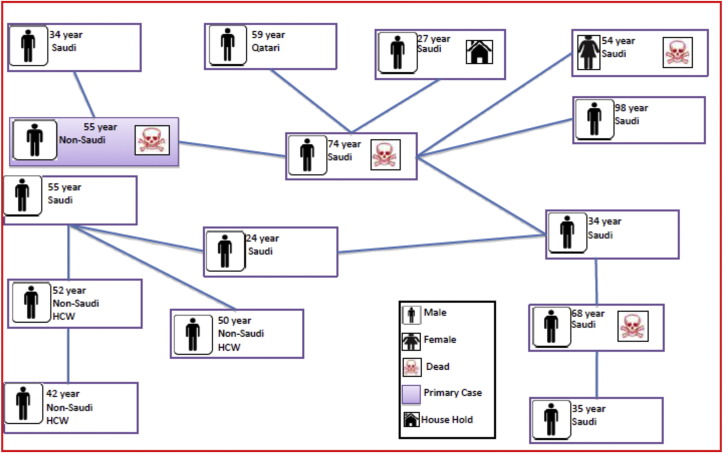
During the study period, a total of 397 patients and contacts were tested for MERS-CoV. There were 18 (4.5%) MERS-CoV positive cases reported in Al-Madinah al-Munawwarah with one large cluster. Of those cases, 15 (83%) were male and 3 (17%) were females. Twelve of the cases were Saudis (67%) and 6 were non-Saudis 33%. There were two possible clusters and two cases were sporadic in nature. The largest cluster included 15 cases and was thought to be initiated by a 55 year-old male resident. He was in the same hospital ward of a 74 year-old Saudi male who was thought to acquire the infection in the healthcare setting. Transmission then occurred in an additional 12 cases as illustrated in Fig. 1 . Another case was from Qatar, the son of a patient sharing a room with the second case although the father tested negative for MERS-CoV. The second cluster was from the city of Hanakia located 100 km from Madina, and involved a 56 year-old male healthcare worker (HCW), who then infected another 39 year-old HCW. There was one sporadic case, a 50 year-old HCW, who had no contacts with other cases. The majority of the cases (61.1%) were healthcare associated infections and primary cases constituted 27.8% and intra-familial transmission was only 11.1%.
Figure 1.
Summary of Cluster of MERS-CoV cases.
3.2. Case fatality and comorbidity
The case fatality rate was 39% (7 of 18 cases). Of the 14 symptomatic cases, 11 (78.5%) had at least two of the following chronic diseases: diabetes mellitus, hypertension, end stage renal disease, cardiac disease, sickle cell anemia, obesity, or smoking. Only one patient had contact with animals, he was a healthcare worker and was asymptomatic.
3.3. Clinical symptoms
All of the 14 symptomatic cases had fever (100%), 64% had shortness of breath, 50% had cough, 35% had nausea, 35% headache, and 21% had sore throat.
3.4. Contacts screening
A total of 250 HCWs were screened and 4 (1.6%) were positive. In addition, 56 family contacts were screened and 1 (1.8%) was positive.
4. Discussion
The current report illustrates the pattern of transmission of MERS-CoV. Our data harmonizes with the previously described pattern of transmission of MERS-CoV [2], [3], [4], [5], [6], [7], [8]. The majority of the patients (61.1%) were healthcare associated infections and primary cases constituted 27.8% and intra-familial transmission was only 11.1%. The recent Jeddah outbreak in 2014 was documented to be secondary to intra-hospital and inter-hospital transmissions [13], [14]. Fig. 2 shows major MERS-CoV outbreaks in Kingdom of Saudi Arabia. The rate of community infections seem to be low with expansion of the infection in the healthcare setting [5]. Animal contact, especially with camels is uncommon among primary cases, and in our series only one patient had camel contact [3], [7]. The case fatality of these cases was 39%, compared to the overall case fatality in KSA of 44% [1] Of the 14 symptomatic cases, 78.5% had at least two of underlying chronic diseases. The presence of comorbidities predisposes to increased risk of MERS-CoV and was shown to also correlate with case fatality rates [16]. Screening of contacts yielded less than 2% positivity among HCWs and family contacts. In a large screening of contacts, MERS-CoV was detected in 1.12% of HCWs contacts and in 3.6% of family contacts [15]. However, the majority of the cases were acquired within healthcare facilities similar to the Al-Hasa and Jeddah outbreak [12], [13], [14]. An interesting observation in this report is the link of one of the MERS cases from Qatar to this healthcare associated cluster. Travel associated MERS cases were reported from: Turkey, Austria, United Kingdom, Germany, France, Greece, the Netherlands, Tunisia, Algeria, Malaysia, Philippines, China, and the United States of America [17]. The recent occurrence of an outbreak in the Republic of Korea was started with a returning traveler [17], [18], [19]. The patient traveled to Bahrain (18–29 April), the United Arab Emirates (29–30 April), Bahrain (30 April–1 May), Saudi Arabia (1–2 May), Bahrain (2 May) and Qatar (2–3 May) [17], [19]. The outbreak spanned 72 healthcare facilities which have treated patients and six healthcare facilities have documented nosocomial transmission [19]. As of June 24, 2015, this outbreak had caused 179 cases including 27 deaths [19]. The outbreak highlights the importance of infection control and early recognition and isolation of suspected cases [5]. The Kingdom of Saudi Arabia also hosts one of the largest mass gathering in the world hosting millions of pilgrims during the annual Hajj where pilgrims visit the holly cities of Makkah and Al-Madinah [7]. The occurrence of MERS-CoV transmission during the annual Hajj and subsequent development of a global epidemic is of a great concern. Respiratory samples were obtained from all MERS suspected cases during 2013 Hajj season and all samples tested negative for MERS-CoV [20]. A cohort of 129 French Hajj pilgrims were systematically sampled in 2013 with screened for MERS-CoV using nasal swabs prior to returning to France [21]. Although, the majority (90.7) had respiratory symptoms, none was tested positive for MERS-CoV [21]. In 2012 and 2013 Hajj season, a total of 5 million pilgrims from 184 countries visited Makkah and Al-Madinah and no cases of MERS-CoV were detected during or after the Hajj [22]. Screening of 5235 adult pilgrims from 22 countries in 2013 showed no positive MERS cases using nasopharyngeal swabs [23]. Although only rare cases have been associated with the Umrah pilgrimage so far, there is a need for continuing surveillance among travelers, pilgrims and HCW attending pilgrims [24].
Figure 2.
A map of the Kingdom of Saudi Arabia showing main clusters: Riyadh (The Capital); Hofof (Al-Hasa 2013 outbreak); Jeddah (2014 outbreak); and the holy Cities Makkah and Al-Madinah (the described outbreak in this report).
Conflict of interest
None.
Acknowledgments
We are grateful to the staff of the Ministry of Health in Al-Madinah area and the staff of the regional laboratory, Kingdom of Saudi Arabia.
Contributor Information
Ziad A. Memish, Email: zmemish@yahoo.com.
Jaffar A. Al-Tawfiq, Email: jaltawfi@yahoo.com.
References
- 1.Saudi Ministry of Health. Available at: http://www.moh.gov.sa/en/CCC/PressReleases/Pages/default.aspx [accessed 02.06.15].
- 2.Al-Tawfiq J.A., Memish Z.A. Middle East respiratory syndrome coronavirus: epidemiology and disease control measures. Infect Drug Resist. 2014 Nov 3;7:281–287. doi: 10.2147/IDR.S51283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Tawfiq J.A., Zumla A., Memish Z.A. Coronaviruses: severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus in travelers. Curr Opin Infect Dis. 2014 Oct;27(5):411–417. doi: 10.1097/QCO.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 4.Al-Tawfiq J.A., Memish Z.A. An update on Middle East respiratory syndrome: 2 years later. Expert Rev Respir Med. 2015 Mar 19:1–9. doi: 10.1586/17476348.2015.1027689. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Memish Z.A., Al-Tawfiq J.A. Middle East respiratory syndrome coronavirus infection control: the missing piece? Am J Infect Control. 2014 Dec;42(12):1258–1260. doi: 10.1016/j.ajic.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Tawfiq J.A., Memish Z.A. Middle East respiratory syndrome coronavirus: transmission and phylogenetic evolution. Trends Microbiol. 2014 Oct;22(10):573–579. doi: 10.1016/j.tim.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Tawfiq J.A., Zumla A., Memish Z.A. Travel implications of emerging coronaviruses: SARS and MERS-CoV. Travel Med Infect Dis. 2014 Sep-Oct;12(5):422–428. doi: 10.1016/j.tmaid.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Tawfiq J.A., Perl T.M. Middle east respiratory syndrome coronavirus (MERS-CoV) in healthcare setting. Curr Opin Infect Dis. 2015 doi: 10.1097/QCO.0000000000000178. [in press] [DOI] [PubMed] [Google Scholar]
- 9.Memish Z.A., Zumla A.I., Al-Hakeem R.F., Al-Rabeeah A.A., Stephens G.M. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013 Jun 27;368(26):2487–2494. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 10.Hijawi B., Abdallat M., Sayaydeh A., Alqasrawi S., Haddadin A., Jaarour N. Novel coronavirus infections in Jordan, April 2012: epidemiological findings from a retrospective investigation. East Mediterr Health J. 2013;19(Suppl. 1):S12–S18. [PubMed] [Google Scholar]
- 11.Al-Abdallat M.M., Payne D.C., Alqasrawi S., Rha B., Tohme R.A., Abedi G.R. Hospital-associated outbreak of Middle East respiratory syndrome coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014 Nov;59(9):1225–1233. doi: 10.1093/cid/ciu359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assiri A., McGeer A., Perl T.M., Price C.S., Al Rabeeah A.A., Cummings D.A. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013 Aug 1;369(5):407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drosten C., Muth D., Corman V.M., Hussain R., Al Masri M., HajOmar W. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, kingdom of Saudi Arabia. Clin Infect Dis. 2015 Feb 1;60(3):369–377. doi: 10.1093/cid/ciu812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oboho I.K., Tomczyk S.M., Al-Asmari A.M., Banjar A.A., Al-Mugti H., Aloraini M.S. 2014 MERS-CoV outbreak in Jeddah–a link to health care facilities. N Engl J Med. 2015 Feb 26;372(9):846–854. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Memish Z.A., Al-Tawfiq J.A., Makhdoom H.Q., Al-Rabeeah A.A., Assiri A., Alhakeem R.F. Screening for Middle East respiratory syndrome coronavirus infection in hospital patients and their healthcare worker and family contacts: a prospective descriptive study. Clin Microbiol Infect. 2014 May;20(5):469–474. doi: 10.1111/1469-0691.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assiri A., Al-Tawfiq J.A., Al-Rabeeah A.A., Al-Rabiah F.A., Al-Hajjar S., Al-Barrak A. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013 Sep;13(9):752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Europenan CDC . 11 June 2015. Rapid risk assessment. Middle East respiratory syndrome coronavirus (MERS-CoV)- 17th update.http://ecdc.europa.eu/en/publications/Publications/middle-east-respiratory-syndrome-coronavirus-rapid-risk-assessment-11-June-2015.pdf Available at: [Google Scholar]
- 18.ProMed. http://www.promedmail.org/direct.php?id=3402059 [accessed 02.06.15].
- 19.World Health Organization . 19 June 2015. Middle East respiratory syndrome coronavirus (MERS-CoV): summary and risk assessment of current situation in the Republic of Korea and China.http://www.who.int/emergencies/mers-cov/mers-cov-republic-of-korea-and-china-risk-assessment-19-june-2015.pdf?ua=1 Available at: [Google Scholar]
- 20.Memish Z.A., Almasri M., Turkestani A., Al-Shangiti A.M., Yezli S. Etiology of severe community-acquired pneumonia during Hajj—part of the MERS-CoV surveillance program. Int J Infect Dis. 2014;25:186–190. doi: 10.1016/j.ijid.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gautret P., Charrel R., Belhouchat K., Drali T., Benkouiten S., Nougairede A. Lack of nasal carriage of novel corona virus (HCoV-EMC) in French Hajj pilgrims returning from the Hajj 2012, despite a high rate of respiratory symptoms. Clin Microbiol Infect. 2013;19:E315–E317. doi: 10.1111/1469-0691.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zumla A., Mwaba P., Bates M., Al-Tawfiq J.A., Maeurer M., Memish Z.A. The Hajj pilgrimage and surveillance for Middle East respiratory syndrome coronavirus in pilgrims from African countries. Trop Med Int Health. 2014 Jul;19(7):838–840. doi: 10.1111/tmi.12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Memish Z.A., Assiri A., Almasri M., Alhakeem R.F., Turkestani A., Al Rabeeah A.A. Prevalence of MERS-CoV nasal carriage and compliance with the Saudi health recommendations among pilgrims attending the 2013 Hajj. J Infect Dis. 2014 Oct 1;210(7):1067–1072. doi: 10.1093/infdis/jiu150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sridhar S., Brouqui P., Parola P., Gautret P. Imported cases of Middle East respiratory syndrome: an update. Travel Med Infect Dis. 2015 Jan-Feb;13(1):106–109. doi: 10.1016/j.tmaid.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]