Abstract
Bacterial and parasitic diseases are not uncommon in domestic doves and pigeons. Many of the bacteria and parasites found in columbids do not cause disease unless the birds are immunocompromised. Often there are underlying viral infections that contribute to illness. This article focuses on some of the more common infections from a practical clinical point of view. Recent updates from the literature are included.
Keywords: Bacterial, Parasitic, Diseases, Columbiformes, Pigeons, Doves
Pigeons and doves have been associated with humans since 3000 to 5000 bc and make up an estimated 50% of all birds in captivity. Columbids are used for food, hobby, sport (racing homers), entertainment (rollers), display (exotic doves), shows and competitive exhibition (fancy breeds), research and communication (racing homers, tumblers and high fliers). All domestic pigeon breeds are derived from the common rock dove (Columba livia), and there are now more than 800 varieties. Common domesticated doves include the diamond dove (Geopelia cuneata) and European ringneck dove (Streptopelia risoria).
There are many excellent books, book chapters, journal articles, and conference proceedings manuscripts on the subject of pigeon medicine.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 This article focuses on bacterial and parasitic diseases of domestic columbiform birds, with special mention of several important underlying viral infections.
Preventive medicine
One of the most important factors in preventing infectious disease in columbid flocks is to incorporate a sound preventative medicine program. Medications are thus rarely necessary if these guidelines are followed by the pigeon fancier:
Buy quality stock from quality breeders. Do not introduce new birds into an existing flock until they have been quarantined and physically examined. The optimal length of quarantine is the time for a pair to raise two or three sets of babies. When quarantine is over, introduce one pair at a time to the existing flock. Allow each pair to establish territory before adding the next pair. This method minimizes the stress of pairs finding a place in the loft.
Examine all new birds for ectoparasites, such as lice, mites, and pigeon flies. Perform fecal floatation and direct smears to check for helminths and Coccidia sp. Examine throat aspirates for trichomonads and blood smears for Hemoproteus sp. If test results are negative, do not administer any medications, because evidence suggests that some drugs cause immunosuppression.
During quarantine, vaccinate all new acquisitions for paramyxovirus1 (PMV1). Salmonella vaccination is optional and is of questionable efficacy. Vaccination for pigeon pox is ideally done after other vaccines, because birds will have an active case of pox that can decrease the immune response to the other vaccines if these are given concurrently. Some practitioners administer all three vaccines at the same time, however, with no apparent ill effects.
Vaccinate all young birds at least 6 to 8 weeks before racing or show season. Do not add unvaccinated birds to the flock at this time because they could contract clinical poxvirus infection.
Keep pigeons in a clean, dry, well-ventilated loft. Do not overcrowd. Feed the birds according to their needs. If a problem arises, seek a diagnosis before administering medications.
Viral diseases
Viral infection is often an underlying cause of illness of bacterial and parasitic disease and viral disease is probably much more common than actually diagnosed in pigeons. Most infections cause only mild illness, but subclinical infections can complicate the disease processes caused by other pathogens. Because the presence of viruses is usually confirmed on necropsy, other pathogens (eg, protozoa, gram-negative bacteria) are more likely to be implicated as the meteoric agents. A brief description of some important viral diseases is provided here.
Excluding PMV1 and pigeon pox virus, herpes virus and adenovirus are the most notable pathogens; however, circovirus, rotavirus, parvovirus, and influenza virus infections have been suggested as causes of immune system compromise.
Pigeon Herpesvirus
Many pigeons are immune carriers of pigeon herpesvirus (PHV) and once infected are lifelong carriers, sometimes shedding without clinical signs. Young birds are most susceptible to clinical illness, but immunocompromised older birds can show symptoms.
A mild to necrotizing pharyngitis and esophagitis are the primary symptoms. Diphtheritic membranes and general signs of illness, including neurologic abnormalities, green droppings, and anorexia, can suggest PHV infection. Vomiting with no other symptoms and inclusion body hepatitis can occur.
Adenovirus
Adenovirus infection had been shown to cause primary illness in pigeons. Young birds are most susceptible and the symptoms are as would be expected with hepatic necrosis of any cause. Basophilic intranuclear inclusion bodies are strongly suggestive of adenovirus infection.15
Treatment is supportive. Antibiotics are indicated for prevention of secondary bacterial infection. Protozoal and helminth parasites should be eliminated and adequate hydration and nutrition provided.
Paramyxovirus-1
Although it has been a problem in Europe and many other parts of the world for a long time, PMV1 has been a problem in North America since 1984 and has spread over the whole continent since 1987 to 1989.
Fanciers with absolutely closed flocks are in the lowest risk. Those who race their pigeons frequently, or buy, sell, trade, or allow contact with feral pigeons are most likely to have infected flocks.
Primary signs of PMV-1 are polyuria (not diarrhea) and central nervous signs, ranging from incoordination, difficulty picking up grains, and mild head tilt, to severe ataxia and torticollis (Fig. 1 ). Surprisingly, affected pigeons do not seem to feel very ill and most eventually recover if given long-term supportive care. The most severely affected birds are unable to feed well enough to maintain body weight, and may need to be euthanized. Immune carriers are possible, and older and younger birds, especially, are most susceptible to infection. Viral shedding can precede clinical signs, and incubation has been suggested as lasting 1 week to as long as 6 weeks.
Fig. 1.

Neurologic signs of paramyxovirus 1. Pigeons are exhibiting stargazing, torticollis, and polyuria.
The author (R.H.) recommends expedient vaccination of all birds, including young birds, in the face of an outbreak. Devastation in outbreaks has been minimized by vaccination, suggesting that incubation is long (2–4 weeks) or that other factors cause a moderate to slow spread in a flock. Elimination of parasites, good nutrition, and loft cleanliness promote the strength of the pigeon's immune system.
Vaccination 1 to 2 months before breeding season and 6 to 8 weeks before racing or showing with oil emulsion vaccine SC has been recommended. The author (R.H.) vaccinates his young bird racing team on weaning and believes that lifelong immunity probably happens from that single immunization. The LaSota oral vaccine should not be depended on for adequate protection.
Pox Virus
Pox virus is found in saliva and in nasal and lacrimal secretions. It enters the body through defects in the skin, especially on the wattle or cere. Direct contact, insect vectors, or airborne secretions can spread the disease. Birds develop scabs and proliferations of the cere, wattle, legs, feet, and commissures of the beak.
The first signs are usually conjunctivitis with excess lacrimation and swelling of the eye and cere. A diphtheroid form can occur, causing lesions on the mucosal surface inside the mouth. Secondary bacterial invasion can cause proliferative lesions, obstructing respiration and making eating difficult.
Treatment of infected birds is strictly supportive. Preventive measures (including practicing strict sanitation; providing proper nutrition; and using antibiotics, anthelminthics, and coccidiostats) should be taken in the event of an outbreak. Isolation of infected individual animals and insect control using screens or insecticides can slow the spread.
Birds develop immunity 3 to 4 weeks after administration of a commercially available vaccine. Feathers are pulled, and the vaccine is applied by a dropper or brush. The wing web is an acceptable site. An inflammatory reaction at the site suggests successful vaccination. Birds as young as 4 weeks of age can be vaccinated, and annual vaccination is recommended 4 weeks before mosquito season. Care should be taken not to introduce new birds into an already vaccinated loft. The incidence of pox varies greatly from year to year and by geographic area. Chances of outbreak increase in late summer and fall, especially in years when the first freeze comes late.
Circovirus
Circovirus, a relative to psittacine beak and feather disease virus and chicken anemia agent, has been recognized since 1986 and has been reported in the United States since 1990. The victims are usually young birds 2 months to 1 year of age. Clinical signs are anorexia, lethargy, diarrhea, rapid weight loss, inability to fly, sneezing, respiratory distress, and death in 3 to 5 days.16, 17, 18, 19, 20, 21
The incubation period is best estimated at about 2 weeks. Circovirus generally has an immunosuppressive effect, allowing concurrent infections to cause the demise of the bird. Among them are Pasteurella sp, herpes virus, Chlamydophila psittaci, Trichomonas gallinae, adenovirus, Aspergillus sp, and Escherichia coli.
It is the author's belief (R.H.) that the incidence of this viral illness is more common than reported. Often the concurrent agents previously mentioned are determined to be the cause of the illness, when they might have only been opportunistic. Recent research shows lesions and pathognomic botryoid inclusions in lymphoreticular tissues consistently in pigeons with “young bird sickness” (see later discussion). It is suggested that bursa be included with liver, spleen, and other tissue for histopathology in suspected viral illness.
Young bird sickness
In Europe, young bird sickness is a condition affecting pigeons in their first year of life.22 Birds exhibit slow crop emptying, regurgitation, diarrhea, weight loss, poor performance, and occasionally death. Lesions occur in the lymphoreticular system, alimentary tract, and respiratory system. Caused by underlying circovirus infection, birds exhibit protozoal, fungal, and mixed bacterial infections associated with ingluvitis and enteritis. Concurrent C psittaci pneumonitis is common.
Viral Hepatitis
Since 1992, an acute hepatic disease in pigeons has occurred in Europe. The syndrome is much like Pacheco disease in parrots, except that there are no inclusions in the hepatocytes and the agent has yet to be identified. Old and young birds are affected.
The birds are sick for 24 to 48 hours and they either die or recover without treatment. Some birds develop yellow, slimy droppings and foul-smelling vomitus. The symptoms can continue for a course of 3 to 4 weeks. The mortality rate is about 30%. Hepatomegaly with a pale-colored liver and complete destruction of all liver cells is found on postmortem examination and histopathology. Treatment is supportive only.
Bacterial infections
Paratyphoid (Salmonellosis)
The most important bacterial disease in pigeons and doves is paratyphoid, caused most often by Salmonella typhimurium var Copenhagen (less often by S arizonae, S pullorum). The best-known signs are swollen wing and leg joints (“boils”), which should be considered almost pathognomonic by the practitioner when observed. Most pigeons with paratyphoid present with an array of other signs, however, including anorexia; weight loss; ruffled feathers; dropped wings; refusal to fly; diarrhea; green droppings; reproductive problems, such as embryonic or early squab death; or death of older birds (Figs. 2 and 3 ) Although not always present and not the most common sign, elbow swelling (also seen in the canalis triosseus) may occur months or years after infection due to antibodies to Salmonella. Salmonella is the second most common agent after PMV-1 causing neurologic signs and can cause severe hepatomegaly and bony lesions that mimic infection with Mycobacterium sp.23
Fig. 2.

Articular form of salmonellosis. Swelling of the tibiotarsal tarsometatarsal joint and wing, causing lameness and inability to fly (wing droop).
Fig. 3.

Gazzi Modina breed pigeon with severe wing droop articular form of Salmonellosis.
Diagnosis is made by demonstration of the organism from the live bird or on necropsy. Selenite broth onto MacConkey or brilliant green agar is suitable for recovering the organism from intestinal or crop contents. Serology may also be useful.
Treatment should be determined by sensitivity testing, because many strains exist with variable drug susceptibility. Enrofloxacin has the most consistent efficacy record, although members of the penicillin, tetracycline, and aminoglycoside families sometimes can be suitable choices. Because Salmonella organisms are shed intermittently, pooling feces over 5 days may be useful. A recent study using 0.5 mg/mL florfenicol in drinking water reduced fecal excretion and clinical signs, but enhanced persistence of Salmonella in internal organs.24 In most outbreaks, there may also be concurrent infections with Klebsiella sp and E coli, so it is beneficial to treat all isolates. Be sure to check for concurrent circovirus infection, which causes immune suppression, therefore increasing susceptibility.
Prevention is far superior to treatment. Before introducing new stock into a disease-free loft, birds should be quarantined in individual cages until they have raised a nest of healthy young. Cleanliness, acidification of floor litter, and strict control of stray pigeons are also helpful measures. Vaccination with killed bacterin may be beneficial. Vaccine does not protect against infection but stimulates immunity.
Colibacillosis (Escherichia coli)
Colibacillosis is another important disease in pigeons. Disease syndromes previously attributed to paratyphoid recently have been shown to be caused by E coli when proper diagnostic tests were done. Excluding the swollen wing and limb joints, the symptoms of the two diseases are similar.
E coli is found in 97% of all pigeon intestinal tracts (part of normal flora) and is not usually a primary problem. It may be involved in septicemia as a facultative pathogen, especially with concurrent adenovirus infection. Disease can occur solely in nestlings or in pigeons of all ages.
Base antibiotic therapy on culture sensitivity. Quinolone resistance is common but enrofloxacin and trimethoprim sulfa are generally successful. Rule out circovirus and other concurrent viruses.
Other Bacteria
Other bacteria, such as Streptococcus, Staphylococcus, Pasteurella, Haemophilus, and Pseudomonas, have been described as pathogens but are of lesser importance than Salmonella and E coli (Table 1 ).
Table 1.
Other bacterial diseases of columbiform birds
| Genus | Species | Comments |
|---|---|---|
| Pasteurella | P multocida | Unilateral (bilateral) epiphora, nasal discharge and swelling, otitis media/interna, arthritis, subcutaneous abscesses, septicemia |
| Mycoplasma | M columbinasale, M columborale, M columbinum | Persistent subclinical infections are common (resemble chlamydiosis and pasteurellosis). |
| Mycobacteria | M avium, M bovis | Pigeons and doves are susceptible to avian Mycobacteriosis. Host genetics (interspecies variations associated with color polymorphism) seem to play an important role in the susceptibility of doves to disease and immunity caused by this bacteria |
| Clostridium spp | C perfringens | Sometimes a cause of enteritis in individual birds |
Treatment of all bacterial diseases should involve culture and sensitivity testing. Often, fanciers and veterinarians “shotgun” flocks with antibiotics, resulting in many resistant strains of bacteria and many immunosuppressed pigeons. The author (R.H.) has noted several cases of peracute or at least acute death. Often they have full crops and no apparent lesions except what appear to be fluid-filled intestines. Clostridium perfringens is found on cultures. Possibly exotoxins damage the gut because of altered bacterial flora, much like hemorrhagic gastroenteritis syndrome in dogs.
Limb deformities caused by enrofloxacin
Krautwald and colleagues33 reported several problems with fluoroquinolone use in racing pigeons. Embryonic mortality was found with high parental doses and was due to streptococcal pneumonia, and secondary staphylococcal and candida infections. Young birds that survived often exhibited deformities, decreased food intake, delayed feather development, slow weight gain, and joint abnormalities, such as distal leg rotations, and intertarsal and stifle joint lesions. Thus far, the author (R.H.) has not appreciated these deformities.
Streptococcus
An acute or even peracute death in pigeons has been attributed to Streptococcus gallolyticus (previously known as S bovis).34 The primary sign in most birds is inability to fly (or deviant flying behavior) and dropped wings. Others have green, foamy droppings and sometimes loss of appetite, polyuria, polydipsia, and swollen abdomen. Birds that have acute disease presents with septicemia. Old and young birds are affected; young birds have pericarditis and old birds often have abnormal yellowing of the breast muscles. A chronic lameness has also been reported.
Nearly 40% of all pigeons carry streptococci in the gastrointestinal tract without clinical signs. It may be part of normal flora but can be a facultative pathogen. Clinical signs are usually not present if confined to the gastrointestinal tract. The disease can easily be mistaken for paramyxovirus and salmonellosis but is usually more acute. Amoxicillin is an effective treatment if instituted early enough. In the human literature, S gallolyticus is developing resistance to tetracyclines and erythromycin, so obtaining a culture before antibiotic administration is ideal.35
Ornithosis Complex
The ornithosis complex (known as “eye colds” or “one-eyed croup”) is common in domestic pigeons. Chlamydophila psittaci is the primary causal agent, but Mycoplasma spp and gram-negative bacteria are also involved. Many herpesvirus infections are also complicated with C psittaci so viral agents should be included in the complex. In addition, birds are often concurrently affected with Trichomonas gallinae. Frequently, the same eye of all the affected birds is in the windward side of wind currents (Fig. 4 ).
Fig. 4.
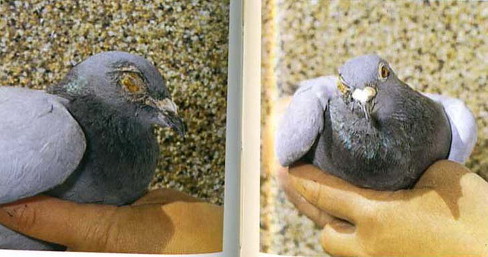
Ornithosis complex (one-eye cold) conjunctivitis. Underlying organisms may be Mycoplasma sp, Chlamydophila psittaci, or bacteria.
Treatment is usually successful with tylosin, but tetracyclines, lincomycin, or erythromycin are also effective. Intramuscular injection is irritating and should be avoided in racing birds. Oral administration and sinus flushing of antibiotics can be the best methods of treatment. Supportive therapy reduces stress and enhances immune response. Topical ophthalmic medications, such as tetracycline ointment, are also of benefit.
Chlamydophila Psittaci
It is estimated that 30% to 90% of pigeons are infected (feral pigeons are the most common carriers of C psittaci in the United States) and doves are also susceptible.36 Serotype B is most commonly isolated from pigeons. Usually considered part of the respiratory disease complex, C psittaci in columbiform birds exhibits low virulence and low zoonotic risk potential. Certain strains (ie, psittacine and turkey) are important causes of diarrhea and weight loss in young birds. Bacterial infections, especially salmonellosis, also complicate upper respiratory problems by pigeon strains leading to higher shedding and mortality. C psittaci may be accompanied by concurrent herpesvirus infections.
Polymerase chain reaction (PCR) testing can be performed and is best done by swabbing the superior conjunctiva and choana. If birds are PCR positive, this indicates active infection. Cloacal swabs are not recommended because a positive PCR means the bird has been exposed and the organism is passing through.37 Treatment with 0.5 mg/mL doxycycline in the drinking water for 45 days is safe and efficacious for doves.38
Parasitic diseases
Endoparasites
Gastrointestinal nematodes are the primary endoparasitic problem of pigeons (Table 2 ). Ascarids, Capillaria, Ornithostrongylus, and Dispharynx are of concern; geographic location determines the particular species that a clinician will encounter. Cestodes (Raillietina spp) are occasionally encountered, and trematodes (Echinostoma spp) are rarely, if ever, found in the United States. Although rare, ocular nematodes (Ceratospira inglisi) were found recently in a dove.39
Table 2.
Columbid helminths
| Name | Species | Comments |
|---|---|---|
| Ascarids | Ascaridia columbae | Most common nematodes (common in feral pigeons, rare in racing pigeons); direct intestinal life cycle, larvae may encyst in lung and liver |
| Capillaria | C caudinflata, C obsignata, C columbae | Direct intestinal lifestyle; may cause vomiting, diarrhea, anemia |
| Roundworms | Dispharynx (previously Acuaria) spiralis (proventriculus) and Ornithostrongylus spp (intestine) | Most serious roundworms; cause severe hemorrhage. Dispharynx requires an intermediate host (pill bug). |
| Globular stomach worm | Tetrameres spp, T columbicola | Require an intermediate host (pill bug). Proventriculus has raspberry-like appearance on necropsy. Not as pathogenic, but causes poor condition |
Diagnosis is made by fecal flotation, direct smear, or intestinal or proventricular scrapings on necropsy. Cestode proglottids can be shed after food deprivation. Because cestodes and some nematodes (eg, Tetrameres) require intermediate hosts (eg, pill bugs), care should be taken to prevent pigeons from foraging where organisms are found. Raised lofts are the most common sites where pigeons are infected.
Deworm birds before the racing and breeding season (Table 3 ). Piperazine is effective only for ascarids. Fenbendazole and mebendazole are effective for ascarids, Capillaria, and probably other parasites that feed on blood or body tissue, but must be used for 3 days. Levamisole is effective against ascarids and has some value against Capillaria sp. Ivermectin is most effective against all nematodes, but other drugs, such as pyrantel pamoate, are better for ascarids. Praziquantel is the drug of choice for cestodes and trematodes.
Table 3.
Some common helminth treatment doses
| Drug | Effective | Dose |
|---|---|---|
| Fenbendazole | Nematodes, including Capillaria, ascarids, strongyles, Tetrameres | 10–12 mg/kg po q 24 h × 3 d |
| Pyrantel pamoate | Nematodes, including ascarids | 20–25 mg/kg po |
| Ivermectin | Best for all nematodes, excellent for Capillaria and Tetrameres but less effective for Ascaridia spp | 0.2 mg/kg po >sq >im, repeat 10–14 d |
| Praziquantel | Cestodes, trematodes | 10–20 mg/kg po repeat in 10–14 d |
Benzimidazole toxicosis
Most reported cases of benzimidazole toxicosis in birds are Columbiformes. Fenbendazole and albendazole cause bone marrow suppression and direct intestinal tract cell damage.41, 42 Use of fenbendazole at reported literature dose of 50 mg/kg by mouth every 24 hours for 5 days caused death in doves.41 Avoid the use of fenbendazole in birds with developing primaries because it will cause weakness and breakage of growing remiges.
Protozoa
Coccidia
The role of coccidian parasites as primary pathogens remains controversial because oocysts are commonly found in healthy birds. Often, pigeons are afflicted with other diseases or under stress shed large numbers of oocysts, particularly young birds. The physical examination should not end when a fecal flotation reveals oocysts but should be thorough in eliminating bacterial infections, trichomoniasis, nutritional deficiencies, husbandry errors, and helminths.
Infections in domestic pigeons are typically mixed and commonly include Eimeria columbarum and Eimeria labbaena. The estimated prevalence of infection is 5.1% to 71.9% and mortality in juvenile pigeons ranges from 5% to 70% worldwide. Most deaths occur in juveniles 3 to 4 months old.43
Evidence indicates that low-level exposure to mildly virulent strains of coccidia can help to produce immunity to more pathogenic strains. Immunity is species-specific and disappears if birds are not reinfected. Coccidiostatic drugs should be administered to poorly performing birds or when experiencing mortalities.
When a disease situation involving coccidia occurs and drugs must be used, sanitation and good husbandry to prevent fecal–oral contact should be the first therapy instituted. Heavily bred, heavily raced older birds, and young birds kept under less than optimal conditions are the most susceptible to disease.
Clazuril, amprolium, sulfachlorpyridazine, and other sulfas (eg, sulfadimethoxine and sulfamethazine) are effective coccidiostats (Table 4 ). There is evidence of growing resistance against sulfonamides and amprolium.43 Because the sulfas reduce thiamine absorption, vitamin B supplementation after therapy is beneficial.
Table 4.
Some common coccidiostats
| Drug | Dose | Comments |
|---|---|---|
| Amprolium | 0.2% solution (200 mg/L) for 5 d, 25 mg/kg/d po | — |
| Clazuril | 2.5 mg per pigeon once | Suppresses oocyst excretion for up to 2 wk |
| Toltrazuril | 20 mg/kg drinking water 2 d42 | Effective for refractory coccidiosis |
| Sulfamethazine | 50–65 mg/pigeon orally × 5 d; 400 mg/L day 1 followed by 200–270 mg/L for 4 d | Supplement B vitamins for 5 d |
| Sulfadimethoxine | 25 mg/kg po q 12 h × 5 d; 330–400 mg/L day 1 followed by 200 mg/L for 4 d | Supplement B vitamins for 5 d |
Nitrofurazone can help with secondary bacterial enteric infections but is not recommended for treatment of coccidiosis in pigeons. Three to 5 days are required for the oocyst to sporulate and become infective, so frequent cleaning is the best preventative measure.
Trichomoniasis
Primarily a columbid disease, most pigeons and doves carry Trichomonas gallinae. The parasite can be a primary pathogen or cause disease secondary to other illnesses or stressful conditions. The severity of trichomoniasis depends on the virulence of the strain and the magnitude of debility from concurrent diseases. The common name “canker” refers to the cheesy, white caseous deposits in the throats of birds that have advanced disease (Fig. 5 ). Mentioned by John Moore as far back as 1735, trichomoniasis is certainly not a new disease.
Fig. 5.

Pigeon with caseous trichomoniasis lesion. This advanced form is canker complicated with secondary bacterial infection.
More often the condition is confused with respiratory diseases because the oculonasal and oral discharges are clear. The organism can easily be demonstrated by suctioning the mucus from the throat with a 1-mL needleless syringe and immediately observing the sample with immersion microscopy. There is no cyst stage, only the trophozoite, which moves in an undulate on wet mounts.
Trichomonas often accompanies the ornithosis complex, viral illnesses, parasitic diseases, and noninfectious stressful situations. Successful therapy involves resolving the other diseases and treatment of the trichomonads. The immune status of the bird is important to consider if recovery is to be expected. Exposure to strains of low virulence in an immunocompetent bird can produce resistance against more pathogenic strains. Trichomoniasis causes caseous masses that are easily removed without bleeding, whereas poxvirus typically creates more voluminous masses localized to the front of the mouth, and the mucosa bleeds when removed.
Although trichomoniasis is primarily a disease of the upper alimentary tract, local lesions, including omphalitis, can occur, along with infection of the liver, lung, and other organs (Figs. 6 and 7 ) Erosion of the palatal flaps indicates previous or current infection. Tiny, pinpoint abscesses in the choanal region may be seen in chronic infections. Signs of infection depend on immunocompetency, previous exposure, and virulence of the infective strain. Most strains are low virulence and most affected pigeons do not show macroscopic lesions. Any debilitated, juvenile, or immunocompromised birds, especially squabs or circovirus-infected birds, are high-risk. A novel respiratory tract presentation has recently been reported.44
Fig. 6.

Squab with omphalitis (right chick). This is an atypical presentation of trichomoniasis complicated with secondary bacteria. The squab on the left is normal for comparison.
Fig. 7.

Crop abscess secondary to trichomoniasis, readily corrected with surgery.
Trichomonas is transmitted via crop secretions from parent to squab or during courtship and through drinking water. Passive immunity is acquired from crop milk and resistance develops from previous exposure.
Effective treatment involves proper use of the 5-nitroimidazole derivatives, including ronidazole, carnidazole, dimetridazole, and metronidazole (Table 5 ). Carnidazole is the drug of choice. Dimetriazole is quite toxic and doses should be reduced in hot weather. Licensed for treatment of blackhead in turkeys, dimetriazole has been discontinued in US because the FDA found traces of the drug in pork. Prevention depends on reducing stress and controlling other diseases. Total eradication of the organism is not practical or desirable. Certain strains may have increased resistance and dosages may need to be adjusted.45
Table 5.
Some common antiprotozoal medications
| Drug | Dose | Comments |
|---|---|---|
| Carnidazole | 20 mg/kg once | Only drug labeled for use in pigeons in United States |
| Ronidazole | 2.5 mg/kg po × 6 d, 100–600 mg/L drinking water for 3–5 d | Flock treatment: lower end of dose range for preventative, higher dose range for treatment |
| Metronidazole | 25–50 mg/kg po q 12–24 h × 5 d; 1057 mg/L drinking water | Lower dose if twice daily |
Hexamita
Hexamitiasis occurs primarily in young pigeons. Host-specific, Hexamita columbae (previously Spironucleus columbae), can be primary or secondary (ie, complication of adenovirus 1 infection). Carriers harbor organisms in cecal tonsils. Symptoms include weight loss, diarrhea, and general unthriftiness. Demonstration of the organism on fresh direct fecal smears is diagnostic.
Important differential diagnoses include: Salmonella, E coli, adenovirus, and PMV. Treat with ronidazole or metronidazole for 7 days. Use caution because pigeons that have polyuria may develop acute toxicosis. Severe infections may need secondary bacterial coverage; trimethoprim or enrofloxacin are good choices. Preventing fecal–oral contact is helpful in controlling hexamitiasis.
Other enteric protozoa
Giardia is seldom a problem in captive columbids. Clinical toxoplasmosis and sarcocystosis are rarely reported in pigeons; however, there have been several reports in the last few years.46, 47, 48, 49, 50 Enclosure contamination with cat (toxoplasma) and opossum (sarcocystis) feces should be considered. Intestinal cryptosporidiosis was reported in pigeons in that had diarrhea and weight loss.51 Feral pigeons have recently been found to shed microsporidia (Enterocytozoon and Encephalitozoon spp), which could spread to domestic birds that come into contact with them.52, 53 There is little information on disease from microsporidia in pigeons at this time, however.
Hemoprotozoa
“Pigeon malaria” is the name frequently given to hemoproteus infection (H columbae, H sacharovi, H maccallumi). Hemoproteus is usually nonpathogenic in domestic pigeons but disease is possible and is a sign of an overcrowded pigeon aviary. Plasmodium spp are rarely reported in pigeons, but can cause disease in young or debilitated birds. Leukocytozoon spp have caused deaths in some Columbids.
Hemoproteus is much more common in performing breeds than in fancy and utility pigeons, possibly because of stresses and exposure to insect vectors in racing situations that make the disease more apparent in racing pigeons then in sedentary exhibition pigeons. The disease is transmitted by the pigeon louse (hippoboscid) fly. Hemoproteus infection is diagnosed by demonstration of the organism in the red blood cell's cytoplasm without nuclear displacement (as apposed to Plasmodium sp), as shown on stained blood smears.
Control of insect vectors is the best prevention. Dusting or dipping with pyrethrin every 2 weeks can be effective in controlling pigeon flies in endemic areas. The disease has been effectively treated with quinacrine. Primaquine has been successfully used as a preventative.
Ectoparasites
Pigeon flies (hippoboscids), lice, and mites are the most significant ectoparasites of pigeons. Pseudolynchia canariensis, the pigeon louse fly, seldom flies. It spends most of its time feeding on birds' blood, causing anemia and transmission of Hemoproteus (and also possibly pox, PMV-1). Louse flies cause considerable discomfort to the bird and can be devastating to the general health of the flock. Louse flies have also been found to transport skin mites (Myialges sp) from one bird to another.54
Columbicola columbae, the slender pigeon louse, is the most common mallophagian parasite. It does not take blood but feeds on feathers, causing tiny pinpoint holes. When lice are found by the clinician, other diseases should be considered. Heavy louse infestations usually indicate a debilitated bird that might not feel well enough to groom properly. Dermanyssus gallinae and Ornithonyssus sylviarum cause skin irritation and feed on blood. They are called red mites or roost mites and are found on the bird at night. Knemidokoptes mutans, the scaly leg mite, causes considerable skin damage. K laevis, the depluming mite, is rare.
Ivermectin is effective for ectoparasites that feed on blood and body tissues and is recommended with dusting or preferably dipping with 0.15% pyrethrin or 5% carbaryl products. Ivermectin and pyrethrin are effective against lice when used properly. The author (L.W.) reports that fipronil (Frontline; Merial, Athens, Georgia) 0.29% spray has been used off-label successfully by wildlife rehabilitators on pigeons and raptor veterinarians to remove hippoboscids and also reduce black flies and mosquitoes. The suggested dose is two to three squirts under each wing and tail every 30 days. One of the metabolites of fipronil has higher toxicity to birds than the parent compound; use the product carefully because it shows variable toxicity in different avian families.55
Summary
Treatment of infectious diseases in columbiform birds typically involves consideration for both individual birds and the flock. An awareness of the pathogens involved, including underlying viruses and bacterial sensitivity patterns, greatly improves the successful treatment of ill pigeons and doves. Considering organ systems involved and possible differential diagnoses is also useful (Boxes 1 and 2 ).
Box 1. Possible pigeon diseases based on common clinical signs.
Central nervous system
Trauma
Salmonella
Streptococcus gallolyticus
Paramyxovirus
Herpesvirus
West Nile Virus
Eastern Equine Encephalities (EEE)
St. Louis Encephalitis
Rabies
Toxoplasma
Lead
Zinc
Sodium chloride
Pesticides (especially OP)
Mycotoxins
Benzimidazoles
Nitrofurazone
Ivermectin
Alphachloralose
Avitrol
Clostridium botulinum (exotoxin)
Neoplasia
Diarrhea (with blood)
Salmonella (B)
Escherichia coli
S gallolyticus
Chlamydia psittaci
Mycobacteria
Clostridia (B)
Herpesvirus
Adenovirus
Parvovirus
Reovirus
Rotavirus
Influenza A
EEE
Trichomoniasis (severe)
Hexamita (B)
Coccidia
Cestodes (B) (squabs)
Trematodes (B)
Asper (late)
Mycotoxins (B)
Insecticides
Rodenticides (cholecalciferol)
Lead
Zinc
Copper
Neoplasia
Vomiting
E coli
Adenovirus
Capillaria
Lead
Zinc
Copper
Rodenticides (cholecalciferol)
Levamisole
Foreign body
Neoplasia
Respiratory
Trauma
Salmonella
C psittaci
E coli
Streptococcus intermedius
Pelistega europaea
Pasteurella
Mycoplasma
Herpesvirus
Influenza A (acute)
Adenovirus (some)
Coronavirus
Aspergillus
Rodenticides (anticoagulants)
Pesticides
Neoplasia
Polyuria (PU)/polydipsia (PD)
Salmonella (PU)
S gallolyticus (PU)
Paramyxovirus
Herpes (PD)
Ethylene glycol (PU)
Rodenticides (cholecalciferol)
Sodium chloride
Avicides (2-chloro-4-acetotoliudine, 3-chloro-4-methybenzenamine)
Lameness
Trauma
Salmonella
S gallolyticus
Mycobacteria
Staphylococci
Pasteurella
Herpesvirus
Enrofloxacin
Neoplasia
Box 2. Possible pigeon diseases associated with poor management, infectious/zoonotic risk, and circovirus infection.
Poor management
Salmonella
Chlamydophila
Paramyxovirus
Pox
Aspergillus
Ascarids
Coccidia
Hemoproteus
Hippoboscids
Lice
Infectious/zoonotic (at-risk species)
Salmonella (all)
Chlamydophila (humans, birds)
E coli (all)
Clostridium (all)
Pasteurella (birds)
Adenovirus (galliforms)
Herpes (psittacines, raptors?)
Influenza A (humans, birds)
Paramyxovirus (poultry, raptors, psittacines, passerines)
Hippoboscids (birds)
Pigeon circovirus-associated
Salmonella
E coli
C psittaci
Pasteurella
Pseudomonas
Paramyxovirus
Poxvirus
Adenovirus
Herpesvirus
Candida
Aspergillus
Trichomonas
Hemoproteus
Tetrameres
Acknowledgement
The authors thank Jamie Gorman (Southside Dog, Cat and Bird Hospital, Oklahoma City, OK) for help with this manuscript.
References
- 1.Tudor D.C. Iowa State University Press; Ames (IA): 1991. Pigeon health and disease. [Google Scholar]
- 2.Marx D.A. Racing Pigeon Digest Co; Lake Charles (LA): 1997. Veterinary approach to pigeon health. [Google Scholar]
- 3.Hooimeijer J. Management of racing pigeons. In: Harrison G.J., Lightfoot T.L., Flinchum G.B., editors. Clinical avian medicine. Spix Pub; Palm Beach (FL): 2006. pp. 849–860. [Google Scholar]
- 4.Rupiper D.J. Diseases that affect race performance of homing pigeons. Part I: husbandry, diagnostic strategies and viral diseases. J Avian Med Surg. 1998;12(2):70–77. [Google Scholar]
- 5.Rupiper D.J. Diseases that affect race performance of homing pigeons. Part II: bacterial, fungal and parasitic diseases. J Avian Med Surg. 1998;12(3):138–148. [Google Scholar]
- 6.De Herdt P., Devriese L. Pigeons. In: Tully T.N., Lawton M.P.C., Dorrestein G.M., editors. Avian medicine. Butterworth Heinemann; Oxford: 2000. pp. 312–338. [Google Scholar]
- 7.Hooimeijer J., Dorrestein G.M. Pigeons and doves. In: Altman R.B., Clubb S.L., Dorrestein G.M., editors. Avian medicine and surgery. WB Saunders; Philadelphia: 1997. pp. 886–909. [Google Scholar]
- 8.Vogel C., Gerlach H., Loffler M. Columbiformes. In: Ritchie B.W., Harrison G.J., Harrison L.R., editors. Avian medicine principles and application. Wingers Publishing; Lake Worth (FL): 1994. pp. 1201–1217. [Google Scholar]
- 9.Beynon P.H., Forbes N.A., Harcourt-Brown N.H., editors. BSAVA manual of raptors, pigeons and waterfowl. Iowa State University Press; Ames (IA): 1996. [Google Scholar]
- 10.Harlin R.W. Practical pigeon medicine. Proc Annu Conf Assoc Avian Vet. 2006:249–262. [Google Scholar]
- 11.Powers L.V. Veterinary care of columbiformes. Proc Annu Conf Assoc Avian Vet. 2005:171–183. [Google Scholar]
- 12.Rupiper D., Ehrenberg M. Practical pigeon medicine. Proc Annu Conf Assoc Avian Vet. 1997:479–497. [Google Scholar]
- 13.Harlin R.W. Pigeon therapeutics. Veterinary Clin North Am Exot Anim Pract. 2000;3(1):19–34. doi: 10.1016/s1094-9194(17)30093-2. [DOI] [PubMed] [Google Scholar]
- 14.Ritchie B.W. Winger's Publishing; Lake Worth (FL): 1995. Avian viruses: function and control. [Google Scholar]
- 15.Takase K., Yoshinaga N., Egashira T. Avian adenovirus isolated from pigeons affected with inclusion body hepatitis. Nippon Juigaku Zasshi. 1990;52(2):207–215. doi: 10.1292/jvms1939.52.207. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt V., Schlomer J., Luken C. Experimental infection of domestic pigeons with pigeon circovirus. Avian Dis. 2008;52(3):380–386. doi: 10.1637/8188-120407-Reg. [DOI] [PubMed] [Google Scholar]
- 17.Duchatel J.P., Todd D., Smyth J.A. Observations on detection, excretion and transmission of pigeon circovirus in adult, young and embryonic pigeons. Avian Pathol. 2006;35(1):30–34. doi: 10.1080/03079450500465692. [DOI] [PubMed] [Google Scholar]
- 18.Abadie J., Nguyen F., Groizeleau C. Pigeon circovirus infection: pathological observations and suggested pathogenesis. Avian Pathol. 2001;30:149–158. doi: 10.1080/03079450124811. [DOI] [PubMed] [Google Scholar]
- 19.Lester V.K., Wilson G.H., Gregory C.R. Testing parameters for the control of pigeon circovirus. Proc Annu Conf Assoc Avian Vet. 2003:11–12. [Google Scholar]
- 20.Woods L.W., Latimer K.S. Circovirus infection of nonpsittacine birds. J Avian Med Surg. 2000;14(3):154–163. [Google Scholar]
- 21.Woods L.W., Latimer K.S., Niagro F.D. A retrospective study of circovirus infection in pigeons: 9 cases (1986–1993). J Vet Diagn Invest 1996;6:156–64. http://jvdi.org/cgi/reprint/6/2/156.pdf Available at: Accessed June 24, 2009. [DOI] [PubMed]
- 22.Scullion F.T., Scullion M.G. Pathologic findings in racing pigeons (Columba livia domestica) with “young bird sickness.”. J Avian Med Surg. 2007;21(1):1–7. doi: 10.1647/1082-6742(2007)21[1:PFIRPC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Suedmeyer W.K., Bermudez A., Shaiken L. Osteolysis and hepatomegaly caused by Salmonella typhimurium in a Temminck's fruit dove (Ptilinopus porphyrea) J Avian Med Surg. 1998;12(3):184–189. [Google Scholar]
- 24.Martel A., Baert K., Lanckreit R. The use of an oral formulation of florfenicol to control Salmonellosis in pigeons. Proc Annu Conf Assoc Avian Vet. 2005:19–21. [Google Scholar]
- 25.Esposito J.F. Respiratory medicine in pigeons. Veterinary Clin North Am Exot Anim Pract. 2000;3(2):395–402. doi: 10.1016/s1094-9194(17)30078-6. [DOI] [PubMed] [Google Scholar]
- 26.Loria G.R., Tamburello A., Liga F. Isolation of mycoplasmas from pigeons suffering eye lesions and respiratory disease. Vet Rec. 2005;157(21):664–665. doi: 10.1136/vr.157.21.664. [DOI] [PubMed] [Google Scholar]
- 27.Nagatomo H., Kato H., Shimizu T. Isolation of mycoplasmas from fantail pigeons. J Vet Med Sci. 1997;59(6):461–462. doi: 10.1292/jvms.59.461. [DOI] [PubMed] [Google Scholar]
- 28.Saggese M.D., Phalen D.N. Serological and histological findings in doves with Mycobacteriosis. Proc Annu Conf Assoc Avian Vet. 2005:71–73. [Google Scholar]
- 29.Bougiouklis P., Brellou G., Fragkiadaki E. Outbreak of avian mycobacteriosis in a flock of 2 year old domestic pigeons (Columba livia f domestica) Avian Dis. 2003;49(3):442–445. doi: 10.1637/7325-011005R.1. [DOI] [PubMed] [Google Scholar]
- 30.Pond C.L., Rush H.C. Infection of white carneaux pigeons (Columba livia) with Mycobacterium avium. Lab Anim Sci. 1981;31(2):196–199. [PubMed] [Google Scholar]
- 31.Fitzgerald S.D., Zwick L.S., Berry D.E. Experimental inoculation of pigeons (Columba livia) with Mycobacterium bovis. Avian Dis. 2003;47(2):470–475. doi: 10.1637/0005-2086(2003)047[0470:EIOPCL]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Hejlicek K., Treml F. Epizoology and pathology of avian mycobacteriosis in domestic pigeons (Columba livia f domestica) Vet Med (Praha) 1994;39(10):615–624. [PubMed] [Google Scholar]
- 33.Krautwald M.E., Pieper K., Rullof R. Further experience with the use of Baytril in pet birds. Proc Annu Conf Assoc Avian Vet. 1990:226–236. [Google Scholar]
- 34.Chadfield M.S., Christensen J.P., Decastere A. Geno-and phenotypic diversity of avian isolates of Streptococcus gallolyticus subsp. gallolyticus (Streptococcus bovis) and associated diagnostic problems. J Clin Microbiol. 2007;54(3):822–827. doi: 10.1128/JCM.00922-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leclercq R., Huet R., Picherot M. Genetic basis of antibiotic resistance in clinical isolates of Streptococcus gallolyticus (Streptococcus bovis) Antimicrobial Agents Chemother. 2005;49(4):1646–1648. doi: 10.1128/AAC.49.4.1646-1648.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grimes J.E., Small M.F., French L.L. Chlamydiosis in captive white-winged doves (Zenaida asiatica) Avian Dis. 1997;41(2):505–508. [PubMed] [Google Scholar]
- 37.Phalen D.N., Hofle M., Dahlhausen B. Diagnosis of Chalmydia psittaci infections in cockatiels and columbiformes. Proc Annu Conf Assoc Avian Vet. 1999:13–17. [Google Scholar]
- 38.Padilla L.R., Flammer K., Miller R.E. Doxycycline-medicated drinking water for treatment of Chlamydophila psittaci in exotic doves. J Avian Med Surg. 2005;19(2):88–91. [Google Scholar]
- 39.Suedmeyer W.K., Smith T., Moore C. Ceratospira inglisi ocular infestation in a wompoo fruit-dove (Ptilinopus magnificus) J Avian Med Surg. 1999;13(4):261–264. [Google Scholar]
- 40.Carpenter J.W. 3rd edition. Elsevier Saunders; St. Louis (MO): 1991. Exotic animal formulary. p. 135–344. [Google Scholar]
- 41.Howard L.L., Papendick R., Stalis I.H. Fenbendazole and albendazole toxicity in pigeons and doves. J Avian Med Surg. 2002;16(3):203–210. [Google Scholar]
- 42.Rivera S.R., McClearen J., Reavill D. Suspected fenbendazole toxicity in pigeons (Columba livia) Proc Annu Conf Assoc Avian Vet. 2000:207–209. [Google Scholar]
- 43.Krautwald-Junghanns M.E., Zebisch R., Schmidt V. Relevance and treatment of coccidiosis in domestic pigeons (Columba livia forma domestica) with particular emphasis on toltrazuril. J Avian Med Surg. 2009;23(1):1–5. doi: 10.1647/2007-049R.1. [DOI] [PubMed] [Google Scholar]
- 44.Stoute S.T., Charlton B.R., Bickford A.A. Respiratory tract trichomoniasis in breeder squab candidates in Northern California. Avian Dis. 2009;53(1):139–142. doi: 10.1637/8389-070108-Case.1. [DOI] [PubMed] [Google Scholar]
- 45.Franssen F.F., Lumeij J.T. In vitro nitroimidazole resistance of Trichomonas gallinae and successful therapy with an increased dosage of ronidazole in racing pigeons (Columba livia domestica) J Vet Pharmacol Ther. 1992;15(4):409–415. doi: 10.1111/j.1365-2885.1992.tb01032.x. [DOI] [PubMed] [Google Scholar]
- 46.Mushi E.Z., Binta M.G., Chabo R.G. Seroprevalence of T. gondii and C. psittaci in domestic pigeons (Columa livia domestica) at Sebele, Gabarone, Botswana. Onderstepoort J Vet Res. 2001;68(1):159–161. [PubMed] [Google Scholar]
- 47.Las R.D., Shivaprasad H.L. An outbreak of toxoplasmosis in an aviary collection of Nicobar pigeons (Caloenus nicobara) J S Afr Vet Assoc. 2008;79(3):149–152. [PubMed] [Google Scholar]
- 48.Suedmeyer W.K., Bermudez A.J., Barr B.C. Acute pulmonary Sarcocystis faculata-like infection in three Victoria crowned pigeons (Goura Victoria) housed indoors. J Zoo Wildl Med. 2001;32(2):252–256. doi: 10.1638/1042-7260(2001)032[0252:APSFLI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 49.Olias P., Gruber A.D., Heydorn A.O. A novel sarcocystis-associated encephalitis and myositis in racing pigeons. Avian Pathol. 2009;38(2):121–128. doi: 10.1080/03079450902737847. [DOI] [PubMed] [Google Scholar]
- 50.Ecco R., Luppi M.M., Malta M.C. An outbreak of sarcocystosis in psittacines and a pigeon in a zoological collection in Brazil. Avian Dis. 2008;52(4):706–710. doi: 10.1637/8303-040408-Case.1. [DOI] [PubMed] [Google Scholar]
- 51.Rodriguez F., Oros J., Rodriguez J.L. Intestinal cryptosporidiosis in pigeons (Columba livia) Avian Dis. 1997;41(3):748–750. [PubMed] [Google Scholar]
- 52.Haro M., Henriques-Gil N., Fennoy S. Detection and genotyping of Enterocytozoon bieneusi in pigeons. J Eukaryot Microbiol. 2006;53(1):S58–S60. doi: 10.1111/j.1550-7408.2006.00173.x. [DOI] [PubMed] [Google Scholar]
- 53.Graczyk T.K., Sunderland D., Rule A.M. Urban feral pigeons (Columba livia) as a source for air-and waterborne contamination with Enterocytozoon bieneusi spores. Appl Environ Microbiol. 2007;73(13):4357–4358. doi: 10.1128/AEM.00202-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Macchioni F., Magi M., Mancianti F. Phoretic association of mites and mallophaga with the pigeon fly Pseudolynchia canariensis. Parasite. 2005;12(3):277–279. doi: 10.1051/parasite/2005123277. [DOI] [PubMed] [Google Scholar]
- 55.National pesticide telecommunications network fact sheet on fipronil. http://npic.orst.edu/factsheets/fipronil.pdf Available at: Accessed June 24, 2009.
- 56.Wade L. Pigeon medicine. Proc Mid-Atlantic States Assoc Av Vet. 2007:137–157. [Google Scholar]
- 57.Vandamme P., Segers P., Ryll M. Pelistega europaea gen.nov., sp. nov., a bacterium associated with respiratory disease in pigeons:taxonomic structure and phylogenetic allocation. Int J Syst Bacteriol. 2002;48(2):431–440. doi: 10.1099/00207713-48-2-431. [DOI] [PubMed] [Google Scholar]


