Summary
Background
The recent Ebola epidemic has increased public awareness of the risk of travel associated viral haemorrhagic fever (VHF). International preparedness to manage imported cases Ebola virus infection was inadequate, highlighted by cases of nosocomial transmission. Crimean-Congo haemorrhagic fever (CCHF) is a re-emerging tick-borne VHF centred in the Eurasian region, affecting a large geographical area and with human-to-human transmission reported, especially in the healthcare setting.
Objectives
To systematically review the characteristics of travel associated Crimean-Congo haemorrhagic fever.
Methods
A systematic review of travel-associated cases of CCHF was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement protocol. PubMed, SCOPUS, Science Citation Index (SCI) and ProMED databases were searched for reports published between January 1960 and January 2016. Three independent reviewers selected and reviewed studies and extracted data.
Results
21 cases of travel associated CCHF were identified, of which 12 died (3 outcome unknown) and 4 secondary (nosocomial) infections were reported. Risk occupations or activities for CCHF infection were reported in 8/12 cases when data were available. Travel from Asia to Asia occurred in 9 cases, Africa to Africa occurred in 5 cases, Africa to Europe in 3 cases, Asia to Europe in 2 cases and Europe to Europe in 2 cases.
Conclusion
CCHF related to travel is rare, is generally associated with at risk activities/occupation and is frequently fatal. Key to early diagnosis and prevention of nosocomial transmission is an understanding of CCHF risk factors and the geographical distribution of CCHF. International travel to CCHF endemic areas is increasing and clinicians and laboratory personnel managing returning travellers should maintain a high index of suspicion.
Keywords: Crimean-Congo haemorrhagic fever, Viral haemorrhagic fevers, Travel, Migration, Imported
1. Introduction
Increasing numbers of people travel each year and developing regions now represent half of all travel destinations. More than half of travellers to developing regions become ill during their journey and up to 8% attend medical facilities during or after their travel [1], [2]. Gastrointestinal illness, fever, and skin disorders remain the most common reasons for travellers seeking medical care [3], [4].
The causes of febrile illness imported by travellers vary with their travel destination and occupational and recreational exposures. Vector borne diseases are common, particularly malaria and tick typhus in travellers returning from Africa and dengue and chikungunya from South Asia [5]. Within this group of patients it is important to consider the rare possibility of a viral haemorrhagic fever (VHF) [6], [7]. These include a diverse group of viruses causing diseases ranging from asymptomatic infection to fatal syndromes and imported cases have significant public health implications. VHFs can be transmitted to humans by vectors such as mosquitoes and ticks or by contact with blood or other animal secretions. The majority also have potential for transmission from human to human.
The recent epidemic of Ebola virus disease (EVD) in West Africa has increased healthcare worker and public awareness of the risk of travel associated VHF. International preparedness to manage imported cases was inadequate, highlighted by onward transmission of EVD to healthcare workers in Europe and the USA [8], [9].
Crimean-Congo haemorrhagic fever (CCHF) is a re-emerging tick-borne VHF causing outbreaks in the Eurasian region, especially in Turkey, Russia, Iran, Pakistan, and Afghanistan in the last 15 years. It affects a large geographical area and human-to-human transmission is reported, especially in the healthcare setting [10]. It is a life threatening disease characterized by fever and haemorrhage, often with non-specific prodromal symptoms such as fatigue, myalgia and headache [11]. It has a case fatality rate of 5–80% [12] and as there is no FDA approved antiviral treatment [13], supportive treatment is essential [14].
Despite regular seasonal CCHF outbreaks [15], travel associated CCHF is rarely reported including in large surveillance studies of ill returning travellers [3]. In this study, we aimed to systematically review the characteristics of travel associated Crimean-Congo haemorrhagic fever and to provide practical advice for healthcare professionals.
2. Materials and methods
2.1. Search strategy
We planned and reported this systematic review in accordance with guidelines for performing and reporting systematic reviews and meta-analyses (PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
2.1.1. Data sources and searches
We searched for English and foreign language studies published between January 1960 and January 2016 in the following databases: PubMed (including MEDLINE), Science Citation Index (SCI) and Scopus. Broad search terms of “Crimean-Congo hemorrhagic fever” or “Crimean-Congo haemorrhagic fever” were utilised. The same search terms were also used to search the ProMED Mail database (http://www.promedmail.org/). We also searched for additional relevant studies by reviewing references from the included publications.
2.1.2. Study selection and data extraction
Three reviewers (HL, RO & TF) independently screened the titles and abstracts of all studies identified by the search strategy for their eligibility. For inclusion, each study had to meet the following criteria [1]: report a laboratory confirmed case of Crimean-Congo haemorrhagic fever and [2]; be associated with international travel. Foreign nationals residing in CCHF endemic countries, who were diagnosed and treated there were excluded. When the title and abstract did not clearly indicate whether the inclusion criteria were met, a full-text copy was retained and reviewed. Full-text copies of the potentially relevant studies were retrieved and evaluated for inclusion as described previously by two reviewers (HL & TF), who then independently extracted data from each study meeting the inclusion criteria. A standard table was utilised to ensure consistency of data extracted from each article. For cases, data were extracted on date, country of origin and final destination, age and gender, reported risk factors, secondary transmission and clinical outcome.
3. Results
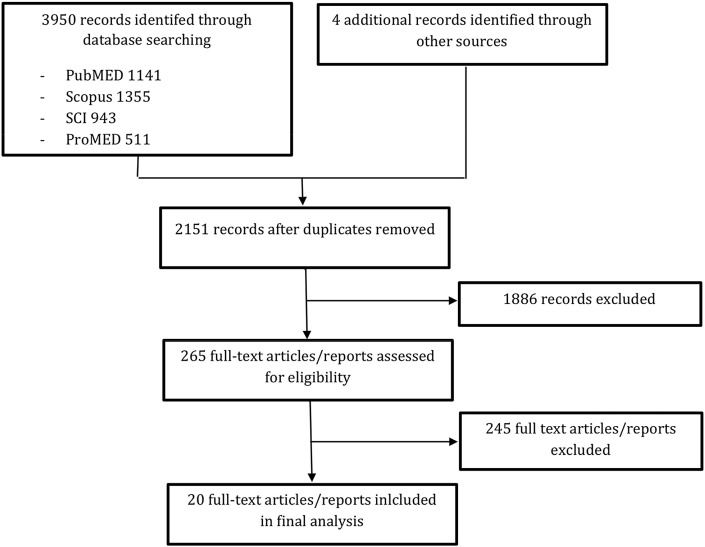
Our initial search identified 3950 records. After exclusion of duplicates, 2151 records were screened by title and abstract. Two hundred and sixty-five full-text articles/reports were retrieved and reviewed and cross-references yielded an additional 2 cases. The total number of travel-associated CCHF cases identified was 21 (Fig. 1 ).
Figure 1.
Flowchart of literature search.
We found two types of travel-related CCHF case: i) Those acquiring the disease during travel to CCHF endemic countries; ii) Residents in endemic countries acquiring the disease and then travelling and crossing borders to seek healthcare. The data on cases identified in these groups are summarized in Table 1 [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]. (Data on cases travelling from Afghanistan to Pakistan are reported separately in Table 2 due to limited detail reported on risk factors, outcome and method of laboratory confirmation) [29], [30], [31], [32], [33], [34], [35], [36].
Table 1.
Characteristics of cases with CCHF acquired abroad.
| Authors (reference) | Year | Source of infection | Country of importation | Route of transmission | Age (years)/sex | Diagnosis | Occupation/reason for travel | Secondary infection | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Swanepoel et al. [16] | 1985 | Zaire (DRC) | South Africa | Cattle-farm exposure | 48 M | Virus isolated | ND | ND | Died |
| 2 | Swanepoel et al. [16] | 1986 | Tanzania | South Africa | Possible tick bites | 26 M | Serology | ND | ND | Survived |
| 3 | Stuart [17] | 1997 | Zimbabwe | UK | Unknown | 78 F | Serology | Leisure | None | Died |
| 4 | ECDC [18] | 2001 | Bulgaria | Germany | Unknown | ND | Unknown | Leisure | ND | Survived |
| 5 | Jaureguiberry et al. [19] | 2004 | Senegal | France | Unknown | 60 F | Serology & PCR | Business (voluntary radiology technician) | None | Survived |
| 6 | Tall et al. [20], [21] | 2004 | Senegal | France | Possible tick bites | 72 F | Serology & PCR | Leisure | None | Died |
| 7 | Conger et al. [22], Olschläger et al. [23] | 2009 | Afghanistan | Germany | Frequent outdoor activities, tick bites, and exposure to undercooked goat meat and blood | 22 M | Serology & PCR | Soldier (US) | Nosocomial transmission to 2 persons: Both survived | Died |
| 8 | ProMED [24] | 2010 | Namibia | South Africa | Sheep and cattle famer | ND M | Unknown | Farmer | None | Survived |
| 9 | Barr et al. [25] | 2012 | Afghanistan | UK | Animal slaughtering, contact with blood and other tissues of infected animal | 38 M | PCR | Leisure | None | Died |
| 10 | ProMED [26] | 2013 | South Sudan | Uganda | Unknown | ND M | Unknown | Trader | None | Survived |
| 11 | ProMED [27] | 2014 | Namibia | South Africa | Farmer | 40 M | Unknown | Farmer | None | Died |
| 12 | Lumley et al. [28] | 2014 | Bulgaria | UK | Tick bite and tick crushing | 70 M | Serology & PCR | Leisure | None | Survived |
DRC: Democratic Republic of Congo, UK: United Kingdom, ND: not defined, M: Male, F: Female, PCR: Polymerase chain reaction.
Table 2.
ProMED mail reports of confirmed CCHF cases travelling from Afghanistan to Pakistan.
| Authors (reference) | Year | Source of infection | Country of importation | Age (years)/sex | Outcome | |
|---|---|---|---|---|---|---|
| 1 | ProMED [29] | 2011 | Afghanistan | Pakistan (Quetta) | ND | ND – 2 HCWs infected |
| 2 | ProMED [30] | 2014 | Afghanistan | Pakistan (Islamabad) | ND M | Died |
| 3 | ProMED [31] | 2014 | Afghanistan | Pakistan Hayatabad | 15 M | ND |
| 4 | ProMED [32] | 2015 | Afghanistan | Pakistan (Islamabad) | 30 M | Died |
| 5 | ProMED [33] | 2015 | Afghanistan | Pakistan (Hayatabad) | 30 M | Died |
| 6 | ProMED [33] | 2015 | Afghanistan | Pakistan (Hayatabad) | 33 ND | Died |
| 7 | ProMED [34] | 2015 | Afghanistan | Pakistan (Islamabad) | 27 M | ND |
| 8 | ProMED [35] | 2015 | Afghanistan | Pakistan (Hayatabad) | 16 ND | Died |
| 9 | ProMED [36] | 2015 | Afghanistan | Pakistan (Hayatabad) | 26 F | Died |
ND: not defined, M: Male, F: Female.
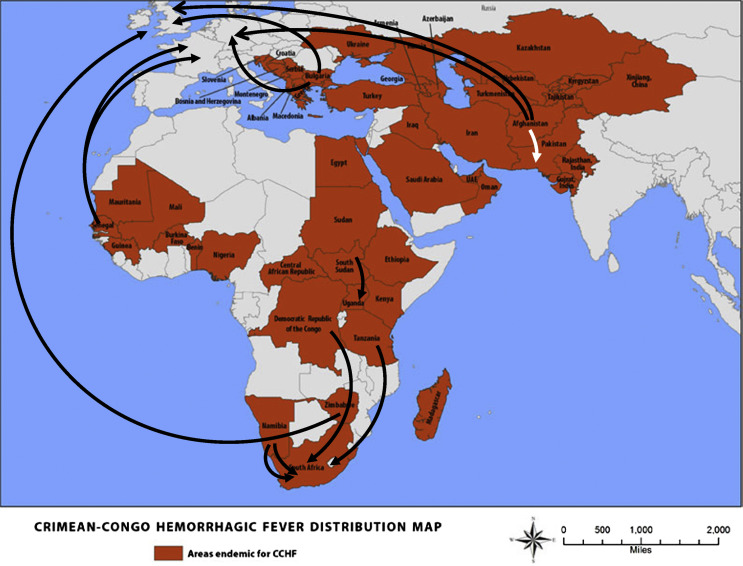
The source and importation country were as follows: Africa to Africa in 5 cases (Zaire to South Africa, Tanzania to South Africa, South Sudan to Uganda, and two cases from Namibia to South Africa) and Europe to Europe in 2 cases (Bulgaria to the UK and to Germany). In 3 cases, the disease was imported from Africa to Europe (Senegal to France [2], and Zimbabwe to the UK), and in 2 cases, Asia to Europe (Afghanistan to the UK and to Germany). In 9 cases (Table 2), the source of the infection was Asia to Asia from Afghanistan to Pakistan (Fig. 2 ).
Figure 2.
Map of imported CCHF cases (Updated from the Centers for Disease Control and Prevention. Each black arrow represents one infected traveller and the white arrow represents 9 infected cases travelling from Afghanistan to Pakistan. Coloured countries are endemic for CCHF.).
Risk occupations or activities for CCHF infection were reported in 7/21 cases. Although the occupation or reason for travel was not reported in some cases, tick bite, contact with wild life, animal exposure, animal handling and slaughtering were reported as risk factors for transmission of the virus. Among the 21 cases identified, 12 died, 7 survived and the outcome for 3 was not reported. Two cases resulted in secondary (nosocomial) infections to a total of 4 HCWS. Travel related cases only identified in ProMED mail include 1 from South Sudan to Uganda [26], two from Namibia to South Africa [27] and 9 from Afghanistan to Pakistan [29], [30], [31], [32], [33], [34], [35], [36].
4. Discussion
In this review of travel associated CCHF, we have identified 21 cases and highlighted the frequent cross border travel of CCHF cases in endemic regions. These figures undoubtedly underestimate the true situation, as CCHF is often a subclinical or mild clinical infection. Internet base reporting systems such as ProMED Mail are a valuable resource for highlighting current outbreaks of CCHF [37]. However, the number of diagnosed travel related infections is still under-reported in all systems.
The underreporting and underestimation of cases is especially true for the neighbouring countries Afghanistan, Iran and Pakistan where CCHF is endemic. As we have highlighted many patients with CCHF from Afghanistan travel to tertiary care hospitals in Pakistan [38], [39]. In their review of 2536 suspected cases of CCHF in Iran, Mostafavi et al. [40] also reported that 172 cases were from Afghanistan, and this was further supported by a large meta-analysis of major infectious diseases affecting the Afghan immigrant population in Iran [41]. Cases of CCHF have also been described in foreign workers who are resident in CCHF endemic countries. Schwarz et al. [42] reported a series of 10 expatriates from India (n = 6), Jordan (n = 1), Pakistan (n = 1), Sri Lanka (n = 1) and Oman (n = 1) who were infected with CCHF virus while working in the UAE. The majority had at risk occupations such as butchers or leather processing, or had been involved in high-risk activities such as animal slaughter. In Oman 39% (13/33) of the total number of cases reported have been in non-Omani nationals of which Bangledeshi residents (n = 8/13) were the largest group [43].
Occupations such as being in the military or specific leisure activities undertaken by travellers increase the likelihood of contact with CCHF. Rural activities such as camping or hiking increase the risk of exposure to tick bites and subsequent crushing of ticks with unprotected fingers is an especially high-risk behaviour, recently described in an imported case to the UK [28]. Exposure to infected animals is another important risk factor and travellers are at risk if they participate in animal slaughtering activities such as during Eid-al Adha [44] or at family celebrations [18].
Limitations of this review are the incomplete information in the case descriptions, particularly on risk factors and methods of laboratory confirmation in ProMED reports. As previously discussed the total numbers identified also represent a significant underestimate due to incomplete reporting of cases from endemic regions and the likelihood of undiagnosed mild CCHF cases. Clinically CCHF can be difficult to distinguish from other causes of undifferentiated febrile illness and other viral haemorrhagic fevers. This is mainly due to its non-specific clinical presentation and a lack of diagnostic laboratory capability in endemic regions. In combination with a lack of awareness of CCHF by clinicians many patients with mild disease may remain undiagnosed. The incubation period is variable (1–13 days) and initial signs and symptoms including fever and myalgia are easily misdiagnosed as influenza like illness. Haemorrhagic complications start around the fourth day of symptoms and it is at this stage that CCHF is often first considered. Malaria also shares epidemiological and clinical overlap and must be considered in any febrile traveller, particularly with thrombocytopenia, and co-infection with CCHF has been reported [45], [46].
Healthcare personnel may be exposed to infected patients and nosocomial transmission has been well reported [19], [22], [47], [48], [49]. In this series two imported cases led to subsequent healthcare related infections, and in endemic regions cases in healthcare workers are regularly reported. The main risks are through needle stick injuries, splashes to mucous membranes and the generation of aerosols, mainly associated with critical care interventions and severe disease. In a recent multicentre review of high-risk CCHF healthcare exposures in Turkey [10] CCHF was frequently not suspected at the time of exposure and mucous membrane ‘splash’ exposure highlighted inadequate use of personal protective equipment. CCHF was also initially not considered in a US soldier infected in Afghanistan, who was transferred to Germany, where nosocomial transmission to 2 HCWs occurred [22], [23]. Those at most risk are ‘frontline’ healthcare workers and often those in non-infection specialties such as Ear Nose and Throat surgeons who are asked to review cases with epistaxis [50].
Lessons can be learnt from imported cases of other viral haemorrhagic fevers and emerging infectious diseases. Amongst the 138 secondary and tertiary cases of SARS in Hong Kong, 85 (62%) occurred in HCWs [51] and in Toronto where SARS was first identified in 2003, 73/144 (51%) were HCWs [52]. More recently during the MERS-CoV outbreak in South Korea the index case, who had recently visited the Middle East and presented with respiratory symptoms, infected HCWs at 3 different hospitals or clinics before MERS-CoV was confirmed [53].
Prior to the West African Ebola epidemic, the most common VHF encountered in travellers was Lassa fever in returnees from West Africa, with occasional importations of filovirus infections such as Marburg and Ebola virus disease and newly recognized viruses, such as Alkhurma virus from Saudi Arabia [54]. During the West Africa outbreak many countries implemented travel restrictions [55], [56], and public health screening measures at airports. National and international recommendations for enhanced training and improved personal protection equipment have also been updated in light of recent experience [57]. The key to early diagnosis and prevention of nosocomial transmission is a detailed travel history that is often omitted in emergency room settings [58]. This needs to be combined with an understanding of CCHF risk factors/activities and the geographical distribution of CCHF.
5. Conclusion
The number of reported cases of CCHF in travellers is low, but international travel to CCHF endemic areas is increasing and the geographical range of CCHF is also enlarging, including within Europe. Clinicians and laboratory personnel managing returning travellers should maintain a high index of suspicion. A travel history should be taken from all patients with fever with or without bleeding, and a more detailed history of possible occupational, recreational or domestic exposure to animals and ticks should be obtained from those visiting at risk countries. Fever and thrombocytopenia is more often caused by malaria, dengue and other infections but can also be a clue to the diagnosis of CCHF. Undiagnosed cases present the highest risk of nosocomial transmission including to healthcare personnel and this can be prevented by early recognition and patient isolation. Travellers to endemic areas should be warned about the risks of tick bites and about safe removal of ticks (Box 1 ). The public health challenge for travel health professionals is how to raise awareness of the special risks among travellers attending family or religious events that include slaughtering of animals.
Box 1.
Recommendations for Travellers
-
•
Travellers should be made aware of the risk activities for CCHF and be given advice on appropriate protective measures when in rural endemic areas.
-
•
Light coloured clothing should be worn to increase the visibility of ticks including long trousers tucked into socks. Clothing can be treated with permethrin and a DEET solution applied to bare skin.
-
•
Travellers should check themselves regularly for attached ticks and if noticed these should not be removed with unprotected hands.
-
•
Travellers should avoid direct contact with animals and if involved in animal slaughtering practices, should wear appropriate personal protective equipment.
-
•
After travel to a CCHF endemic area travellers with a fever should immediately attend healthcare facilities and report possible CCHF exposure
Recommendations for Healthcare Personnel
-
•
A risk assessment for CCHF should be undertaken if there is history of fever and travel to an endemic country (e.g. detailed travel history, history of tick bites, animal contact, participation in animal slaughter)
-
•
Clinical presentation of CCHF is non-specific initially and laboratory abnormalities such as thrombocytopenia, leucopenia and raised liver enzymes (ALT/AST)/creatinine kinase may give a clue to the diagnosis.
-
•
The main risk of nosocomial transmission to HCWs is through needle stick injuries or splashes of blood/body fluids to mucous membranes
-
•
A suspect or confirmed CCHF case must be isolated and standard, contact and droplet precautions should be undertaken. Healthcare personnel must wear personal protective equipment including a medical mask, facial shield/goggles, gloves and a fluid repellant gown. An N95/FFP3 mask should be worn during aerosol generating procedures, e.g. endotracheal intubation
-
•
Healthcare personnel should not touch ticks directly with bare hands. Ticks should be removed by tweezers using gloves.
-
•
Laboratory workers should process samples in appropriate biosafety level laboratories. Laboratories should be fully informed before sending a clinical sample from a patient suspected of having CCHF.
Conflict of interest
There is no conflict of interest for any of the authors.
Funding source
No specific funding. NJB is partially supported by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emerging and Zoonotic Infections, a partnership between the University of Liverpool, Liverpool School of Tropical Medicine and Public Health England (PHE). The views expressed are those of the author(s) and not necessarily those of the Turkish Ministry of Health, the NHS, the NIHR, the Department of Health or Public Health England.
Authors contributions
HL initiated the review, the papers (abstracts and full papers) were independently evaluated and selected by HL, RO and TF. RO drafted the initial manuscript with TF; all co-authors reviewed and commented including approval of the final version.
References
- 1.Freedman D.O., Weld L.H., Kozarsky P.E., Fisk T., Robins R., von Sonnenburg F. Spectrum of disease and relation to place of exposure among ill returned travelers. N Engl J Med. 2006;354(2):119–130. doi: 10.1056/NEJMoa051331. [DOI] [PubMed] [Google Scholar]
- 2.Steffen R., Rickenbach M., Wilhelm U., Helminger A., Schar M. Health problems after travel to developing countries. J Infect Dis. 1987;156(1):84–91. doi: 10.1093/infdis/156.1.84. [DOI] [PubMed] [Google Scholar]
- 3.Leder K., Torresi J., Libman M.D., Cramer J.P., Castelli F., Schlagenhauf P. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–468. doi: 10.7326/0003-4819-158-6-201303190-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlagenhauf P., Weld L., Goorhuis A., Gautret P., Weber R., von Sonnenburg F. Travel-associated infection presenting in Europe (2008–12): an analysis of EuroTravNet longitudinal, surveillance data, and evaluation of the effect of the pre-travel consultation. Lancet Infect Dis. 2015;15(1):55–64. doi: 10.1016/S1473-3099(14)71000-X. [DOI] [PubMed] [Google Scholar]
- 5.Gautret P., Schlagenhauf P., Gaudart J., Castelli F., Brouqui P., von Sonnenburg F. Multicenter EuroTravNet/GeoSentinel study of travel-related infectious diseases in Europe. Emerg Infect Dis. 2009;15(11):1783–1790. doi: 10.3201/eid1511.091147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beeching N.J., Fletcher T.E., Hill D.R., Thomson G.L. Travellers and viral haemorrhagic fevers: what are the risks? Int J Antimicrob Agents. 2010;36(Suppl. 1):S26–S35. doi: 10.1016/j.ijantimicag.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher T.E., Brooks T.J., Beeching N.J. Ebola and other viral haemorrhagic fevers. BMJ. 2014;349:g5079. doi: 10.1136/bmj.g5079. [DOI] [PubMed] [Google Scholar]
- 8.Liddell A.M., Davey R.T., Jr., Mehta A.K., Varkey J.B., Kraft C.S., Tseggay G.K. Characteristics and clinical management of a cluster of 3 patients with Ebola virus disease, including the first domestically acquired cases in the United States. Ann Intern Med. 2015;163(2):81–90. doi: 10.7326/M15-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopaz M.A., Amela C., Ordobas M., Dominguez-Berjon M.F., Alvarez C., Martinez M. First secondary case of Ebola outside Africa: epidemiological characteristics and contact monitoring, Spain, September to November 2014. Euro Surveill. 2015;20(1) doi: 10.2807/1560-7917.es2015.20.1.21003. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=21003 pii=21003. Available online: [DOI] [PubMed] [Google Scholar]
- 10.Leblebicioglu H., Sunbul M., Guner R., Bodur H., Bulut C., Duygu F. Healthcare associated Crimean-Congo haemorrhagic fever in Turkey 2002–2014 – a multi-centre retrospective cross-sectional study. Clin Microbiol Infect. 2016 doi: 10.1016/j.cmi.2015.11.024. http://www.sciencedirect.com/science/article/pii/S1198743X16000057 Published on line 20 Jan 2016: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yilmaz G.R., Buzgan T., Irmak H., Safran A., Uzun R., Cevik M.A. The epidemiology of Crimean-Congo hemorrhagic fever in Turkey, 2002–2007. Int J Infect Dis. 2009;13(3):380–386. doi: 10.1016/j.ijid.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 12.Leblebicioglu H. Crimean-Congo haemorrhagic fever in Eurasia. Int J Antimicrob Agents. 2010;36(Suppl. 1):S43–S46. doi: 10.1016/j.ijantimicag.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 13.Ascioglu S., Leblebicioglu H., Vahaboglu H., Chan K.A. Ribavirin for patients with Crimean-Congo haemorrhagic fever: a systematic review and meta-analysis. J Antimicrob Chemother. 2011;66(6):1215–1222. doi: 10.1093/jac/dkr136. [DOI] [PubMed] [Google Scholar]
- 14.Leblebicioglu H., Bodur H., Dokuzoguz B., Elaldi N., Guner R., Koksal I. Case management and supportive treatment for patients with Crimean-Congo hemorrhagic fever. Vector Borne Zoonotic Dis. 2012;12(9):805–811. doi: 10.1089/vbz.2011.0896. [DOI] [PubMed] [Google Scholar]
- 15.Leblebicioglu H., Ozaras R., Irmak H., Sencan I. Crimean-Congo hemorrhagic fever in Turkey: current status and future challenges. Antivir Res. 2016;126:21–34. doi: 10.1016/j.antiviral.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Swanepoel R., Shepherd A.J., Leman P.A., Shepherd S.P., McGillivray G.M., Erasmus M.J. Epidemiologic and clinical features of Crimean-Congo hemorrhagic fever in southern Africa. Am J Trop Med Hyg. 1987;36(1):120–132. doi: 10.4269/ajtmh.1987.36.120. [DOI] [PubMed] [Google Scholar]
- 17.Stuart J. Suspected case of Crimean/Congo haemorrhagic fever in British traveller returning from Zimbabwe. Euro Surveill. 1998;2(8) http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=1256 pii=1256. Available online: [Google Scholar]
- 18.ECDC . 2008. Meeting report. Consultation on Crimean-Congo haemorrhagic fever prevention and control. Stockholm. [Google Scholar]
- 19.Jaureguiberry S., Tattevin P., Tarantola A., Legay F., Tall A., Nabeth P. Imported Crimean-Congo hemorrhagic fever. J Clin Microbiol. 2005;43(9):4905–4907. doi: 10.1128/JCM.43.9.4905-4907.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tall A., Diallo M., Faye O., Diab H., Diatta B., Sall A.A. Crimean-Congo hemorrhagic fever in Senegal. Med Trop (Mars) 2009;69(1):18. [PubMed] [Google Scholar]
- 21.Tall A., Sall A.A., Faye O., Diatta B., Sylla R., Faye J. Two cases of Crimean-Congo haemorrhagic fever (CCHF) in two tourists in Senegal in 2004. Bull Soc Pathol Exot. 2009;102(3):159–161. [PubMed] [Google Scholar]
- 22.Conger N.G., Paolino K.M., Osborn E.C., Rusnak J.M., Gunther S., Pool J. Health care response to CCHF in US soldier and nosocomial transmission to health care providers, Germany, 2009. Emerg Infect Dis. 2015;21(1):23–31. doi: 10.3201/eid2101.141413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olschläger S., Gabriel M., Schmidt-Chanasit J., Meyer M., Osborn E., Conger N.G. Complete sequence and phylogenetic characterisation of Crimean-Congo hemorrhagic fever virus from Afghanistan. J Clin Virol. 2011;50(1):90–92. doi: 10.1016/j.jcv.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 24.ProMED-mail. Crimean-Congo hem. fever – Namibia: (KA) 2010. ProMED mail 201008102732. [16 February 2016] [Google Scholar]
- 25.Barr D.A., Aitken C., Bell D.J., Brown C.S., Cropley I., Dawood N. First confirmed case of Crimean-Congo haemorrhagic fever in the UK. Lancet. 2013;382(9902):1458. doi: 10.1016/S0140-6736(13)61718-3. [DOI] [PubMed] [Google Scholar]
- 26.ProMED-mail. Crimean-Congo hem. fever – Uganda (04): clarification. 2013. ProMED-mail 201308261903826. [updated 26 August 2003, 17 August 2015] [Google Scholar]
- 27.ProMED-mail. Crimean-Congo hem. fever – South Africa ex Namibia. 2014. ProMED-mail 201409192788764. [updated 19 September 2014, 17 August 2015] [Google Scholar]
- 28.Lumley S., Atkinson B., Dowall S., Pitman J., Staplehurst S., Busuttil J. Non-fatal case of Crimean-Congo haemorrhagic fever imported into the United Kingdom (ex Bulgaria), June 2014. Euro Surveill. 2014;19(30) doi: 10.2807/1560-7917.es2014.19.30.20864. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20864 pii=20864. Available from: [DOI] [PubMed] [Google Scholar]
- 29.ProMED-mail. Crimean-Congo hem. fever – Pakistan ex Afghanistan, nosocomial. 2011. ProMED-mail 201109172833. [17 August 2015] [Google Scholar]
- 30.ProMED-mail. Crimean-Congo hem. fever – Pakistan. 2014. ProMED-mail 201405242496690. [16 February 2016] [Google Scholar]
- 31.ProMED-mail. Crimean-Congo hem. fever – Pakistan (05) 2014. ProMED-mail 201407222628425. [16 February 2016] [Google Scholar]
- 32.ProMED-mail. Crimean-Congo hem. fever – Pakistan (02): ex Afghanistan, additional information. 2015. ProMED-mail 201505153365765. [16 February 2016] [Google Scholar]
- 33.ProMED-mail. Crimean-Congo hem. fever – Pakistan (05): ex Afghanistan, Iran. 2015. ProMED-mail 201506253465423. [16 February 2016] [Google Scholar]
- 34.ProMED-mail. Crimean-Congo hem. fever – Pakistan (07): ex Afghanistan. 2015. ProMED-mail 201507053485737. [updated 5 July 201517 August 2015] [Google Scholar]
- 35.ProMED-mail. Crimean-Congo hem. fever – Pakistan (08): ex Afghanistan suspected. 2015. ProMED-mail 201508033555191. [16 February 2015] [Google Scholar]
- 36.ProMED-mail. Crimean-Congo hem. fever – Pakistan (19) 2015. ProMED-mail Crimean-Congo hem fever - Pakistan (19) [16 February 2015] [Google Scholar]
- 37.Ince Y., Yasa C., Metin M., Sonmez M., Meram E., Benkli B. Crimean-Congo hemorrhagic fever infections reported by ProMED. Int J Infect Dis. 2014;26:44–46. doi: 10.1016/j.ijid.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 38.Abbas T., Younus M., Muhammad S.A. Spatial cluster analysis of human cases of Crimean Congo hemorrhagic fever reported in Pakistan. Infect Dis Poverty. 2015;4:9. doi: 10.1186/2049-9957-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alam M.M., Khurshid A., Sharif S., Shaukat S., Rana M.S., Angez M. Genetic analysis and epidemiology of Crimean Congo Hemorrhagic fever viruses in Baluchistan province of Pakistan. BMC Infect Dis. 2013;13:201. doi: 10.1186/1471-2334-13-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mostafavi E., Pourhossein B., Chinikar S. Clinical symptoms and laboratory findings supporting early diagnosis of Crimean-Congo hemorrhagic fever in Iran. J Med Virol. 2014;86(7):1188–1192. doi: 10.1002/jmv.23922. [DOI] [PubMed] [Google Scholar]
- 41.Pourhossein B., Irani A.D., Mostafavi E. Major infectious diseases affecting the Afghan immigrant population of Iran: a systematic review and meta-analysis. Epidemiol Health. 2015;37:e2015002. doi: 10.4178/epih/e2015002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwarz T.F., Nsanze H., Ameen A.M. Clinical features of Crimean-Congo haemorrhagic fever in the United Arab Emirates. Infection. 1997;25(6):364–367. doi: 10.1007/BF01740819. [DOI] [PubMed] [Google Scholar]
- 43.ProMED-mail. Crimean-Congo hem. fever – Oman (02) 2014. ProMED-mail 201411082939718. [16 February 2016] [Google Scholar]
- 44.Leblebicioglu H., Sunbul M., Memish Z.A., Al-Tawfiq J.A., Bodur H., Ozkul A. Consensus report: preventive measures for Crimean-Congo hemorrhagic fever during Eid-al-Adha festival. Int J Infect Dis. 2015;38:9–15. doi: 10.1016/j.ijid.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 45.Christova I., Petrov A., Papa A., Vutchev D., Kalvatchev N., Vatev N. Fatal outcome of coinfection of Crimean-Congo hemorrhagic fever and malaria. Jpn J Infect Dis. 2015;68(2):131–134. doi: 10.7883/yoken.JJID.2014.106. [DOI] [PubMed] [Google Scholar]
- 46.Sharifi-Mood B., Metanat M., Rakhshani F., Shakeri A. Co-infection of malaria and Crimean-Congo hemorrhagic fever. Iran J Parasitol. 2011;6(3):113–115. [PMC free article] [PubMed] [Google Scholar]
- 47.Burney M.I., Ghafoor A., Saleen M., Webb P.A., Casals J. Nosocomial outbreak of viral hemorrhagic fever caused by Crimean Hemorrhagic fever-Congo virus in Pakistan, January 1976. Am J Trop Med Hyg. 1980;29(5):941–947. doi: 10.4269/ajtmh.1980.29.941. [DOI] [PubMed] [Google Scholar]
- 48.Pshenichnaya N.Y., Nenadskaya S.A. Probable Crimean-Congo hemorrhagic fever virus transmission occurred after aerosol-generating medical procedures in Russia: nosocomial cluster. Int J Infect Dis. 2015;33C:120–122. doi: 10.1016/j.ijid.2014.12.047. [DOI] [PubMed] [Google Scholar]
- 49.van Eeden P.J., Joubert J.R., van de Wal B.W., King J.B., de Kock A., Groenewald J.H. A nosocomial outbreak of Crimean-Congo haemorrhagic fever at Tygerberg Hospital. Part I. Clinical features. S Afr Med J. 1985;68(10):711–717. [PubMed] [Google Scholar]
- 50.Bosan A.H., Asghar H., Dil A.S., Kakar F., Ahmad I., Sadaruddin A. Nomad index case responsible for crimean congo hemorrhagic fever (CCHF) outbreak in Pishin. Pak J Med Res. 2003;42(4):200–201. [Google Scholar]
- 51.Lee N., Hui D., Wu A., Chan P., Cameron P., Joynt G.M. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 52.Booth C.M., Matukas L.M., Tomlinson G.A., Rachlis A.R., Rose D.B., Dwosh H.A. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289(21):2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 53.Lee J. Better understanding on MERS Corona virus outbreak in Korea. J Korean Med Sci. 2015;30(7):835–836. doi: 10.3346/jkms.2015.30.7.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Madani T.A., Azhar E.I., Abuelzein el T.M., Kao M., Al-Bar H.M., Abu-Araki H. Alkhumra (Alkhurma) virus outbreak in Najran, Saudi Arabia: epidemiological, clinical, and laboratory characteristics. J Infect. 2011;62(1):67–76. doi: 10.1016/j.jinf.2010.09.032. [DOI] [PubMed] [Google Scholar]
- 55.Bogoch, Creatore M.I., Cetron M.S., Brownstein J.S., Pesik N., Miniota J. Assessment of the potential for international dissemination of Ebola virus via commercial air travel during the 2014 west African outbreak. Lancet. 2015;385(9962):29–35. doi: 10.1016/S0140-6736(14)61828-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Poletto C., Gomes M.F., Pastore y Piontti A., Rossi L., Bioglio L., Chao D.L. Assessing the impact of travel restrictions on international spread of the 2014 West African Ebola epidemic. Euro Surveill. 2014;19(42) doi: 10.2807/1560-7917.es2014.19.42.20936. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20936 pii=20936. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beeching N.J., Fenech M., Houlihan C.F. Ebola virus disease. BMJ. 2014;349:g7348. doi: 10.1136/bmj.g7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Price V.A., Smith R.A., Douthwaite S., Thomas S., Almond D.S., Miller A.R. General physicians do not take adequate travel histories. J Travel Med. 2011;18(4):271–274. doi: 10.1111/j.1708-8305.2011.00521.x. [DOI] [PubMed] [Google Scholar]