Abstract
Background
The annual Hajj and Umrah are one of the largest recurring religious mass gatherings across the globe drawing pilgrims from more than 185 countries. The living circumstances and activities of the pilgrims may create an environment for the occurrence and spread of communicable diseases. Each year, the Health authority of the Kingdom of Saudi Arabia, in coordination with international health authorities, updates health requirements for pilgrims. The Hajj for 2017 took place from August 24 to September 5, 2017. Here, we review the expected obligations for immunizations for the 2018 Hajj and Umrah.
Results
The Hajj and Umrah vaccine requirements include mandatory vaccinations against yellow fever, quadrivalent meningococcal polysaccharide (every 3 years) or conjugated (every 5 years) vaccines and poliomyelitis vaccine. Influenza vaccine utilizing the 2016 (Southern Hemisphere vaccine to all pilgrims) was recommended but was not obligatory for pilgrims. Ciprofloxacin is required for individuals >12 years excluding pregnant women as chemoprophylaxis to be given at the port of entry for Pilgrims coming from the meningitis belt. With the ongoing outbreaks of measles in Europe, it is recommended that all pilgrims have an updated immunization against vaccine-preventable diseases (diphtheria, tetanus, pertussis, polio, measles and mumps).
Conclusion
The mandatory vaccines remain the same with continued vigilance for the development of any new or emerging infectious diseases. Continuing surveillance for Zika virus, cholera and MERS-CoV are ongoing.
Keywords: Hajj, Pilgrimage, Mass gathering, Vaccine requirements, Saudi Arabia
1. Introduction
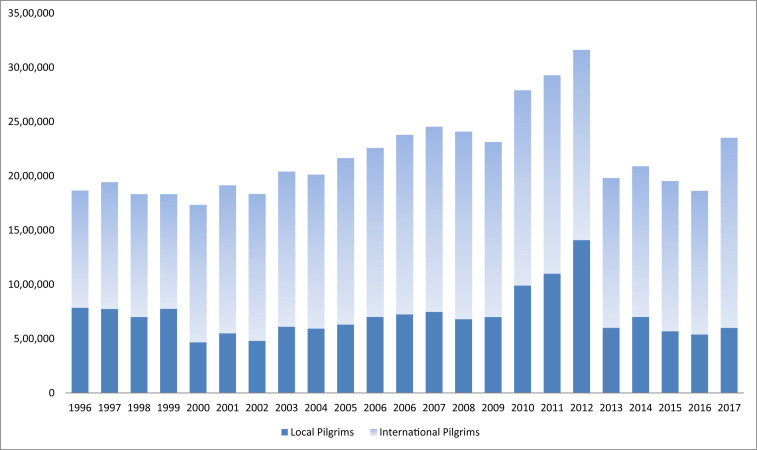
The annual Hajj and Umrah are one of the largest recurring religious mass gatherings across the globe drawing pilgrims from more than 185 countries. The number of pilgrims from each country is determined based on the number of Muslims in each country and is based on a ratio of one pilgrim per one thousand Muslims in that country [1]. The Hajj season occurs at a fixed time each year from the 8th to the 13th day of the 12th month (Dhu al-Hijjah) in the Islamic calendar which is 11 days shorter than the Gregorian calendar. Thus, the Hajj season occurs in different time of the Gregorgian calendar. On the other hand, the Umrah season is year round and is more intense during the month of Ramadhan (the month of fasting). The month of Ramadhan occurred May 27 to June 24, 2017 and will take place May 15 to June 14, 2018. Hajj is compulsory for all Muslims who have the resources once in a life time and the Umrah is not compulsory. The number of the annual Hajj pilgrims is about three million with two million non-Saudis pilgrims arriving from overseas countries and mainly arriving by air and others from neighboring countries may travel via land [2], [3], [4]. In 2016, the majority (94%) of pilgrims arrived by air, 5% arrived by land and only 1% arrived through the sea. The number of pilgrims per year is shown in Fig. 1 . The Kingdom of Saudi Arabia (KSA) provides healthcare free of charge to all pilgrims during the Hajj as done previously through 25 hospitals which have 5000 beds including 500 critical care beds and 550 emergency care beds and 155 healthcare centers staffed with 30,000 Ministry of Health staff [2], [3], [4]. In this year's Hajj more than 540,000 pilgrims were serviced in these healthcare facilities with emergency departments serving 23,000 pilgrims. The annual required vaccinations for the Hajj and Umrah seasons are issued by the Saudi Ministry of Health including the 2017 recommendations [5]. In this article we summarize the recommended vaccinations for the 2018 Hajj and Umrah season.
Fig. 1.
Annual Number of Pilgrims per year from 1996 to 2017.
1.1. Medical advice for Hajj and Umrah travelers
Each year the Saudi Ministry of Health publishes Hajj and Umrah requirements with emphasis on the required vaccinations. These guidelines are updated annually to reflect the changes in the epidemiology of important infectious diseases [1], [2], [6], [7]. The mandatory and recommended vaccines for the 2018 season are discussed further.
1.2. Vaccination during the Hajj and Umrah season
The vaccination requirements during the Hajj and Umrah are divided into: mandatory vaccinations (Meningococcal vaccination, Poliomyelitis vaccine, and Yellow Fever vaccine); recommended vaccination (Influenza), and other immunization against vaccine-preventable diseases (diphtheria, tetanus, pertussis, polio, measles and mumps).
1.3. Meningococcal vaccination
Niesseria meningitides is associated with a high rate of carriage of 80% [8]. In a recent study, 3.4% of 1055 arriving pilgrims were classified as nasopharyngeal carriage of N. meningitides and of them 66.7% had serogroup B [9]. The requirement of the meningococcal vaccination for pilgrims came in effect in 1987 after the occurrence of meningococcal outbreaks [2].The vaccine initially was a bivalent A and C meningococcal vaccine and then was expanded to the quadrivalent vaccine (A,C,Y, W135) in May 2001 [10], [11]. This expansion of the vaccine resulted from the occurrence of two meningococcal outbreaks with serogroup W135 in 2000 and 2001 [12], [13], [14]. The mean numbers of Hajj-related invasive meningococcal disease cases decreased from 13 to 2 cases per year in 1995 compared to 2011 [11]. The requirement of the quadrivalent meningococcal vaccine includes all pilgrims from any country. Either polysaccharide or conjugated vaccine could be used with differing need for re-dosing according to ministry of health guidance (every 3 yrs for the polysaccharide vaccine while for the conjugated vaccine every 5 yrs). The advantages of the conjugated vaccine include the ability to eradicate carriage and prevent outbreaks among returning colonized pilgrims. Moreover, ciprofloxacin (500 mg tablets) is administered as an oral chemoprophylaxis to pilgrims arriving from the African meningitis belt [2], [6], [8], [15], [16]. In one study, the carriage rate of N. meningitides was 3.6% and 1.4% in a paired cohort of pilgrims from high endemic countries at arrival and departure, respectively [9]. In an earlier study, the carriage rate of N. meningitidis after a single dose of ciprofloxacin was 5.2% before and 4.6% after the Hajj (P = 0.65) [17]. The carriage rate of N. meningitides among returning pilgrims varies from 0% to 0.6% [17], [18], [19], [20] and thus ciprofloxacin was not adopted as a strategy post-Hajj. The compliance rate with the recommended meningococcal vaccination among arriving international pilgrims is 97–100% [9]. In one study 1055 arriving pilgrims at King Abdul Aziz International Airport, 98% of the pilgrims had the quadrivalent polysaccharide vaccine and 2% had the quadrivalent meningococcal conjugate vaccine (MCV4) [9]. Recently, N. meningitidis serogroup B is becoming an important cause of meningococcal meningitis in Europe, Australia, and north America and may cause outbreaks [21], [22], [23], [24]. Currently, a vaccine is available against N. meningitidis serogroup B [25] and there is no sufficient data to recommend the addition of this vaccine to the required Hajj vaccines [9]. An ideal meningococcal vaccine would contain the 4 currently available serogroups in addition to serogroup B.
1.4. Poliomyelitis
Poliomyelitis is a vaccine preventable disease; however, poliomyelitis eradication is hindered by the potential spread by international travelers [26]. There are reports of Hajj associated poliomyelitis cases. In a mathematical model, it was estimated that there is a potential of 21 importations of poliovirus into Saudi Arabia via Hajj pilgrims [27]. There are many countries which harbor patients infected with the Wild Polio Virus 1 or having a Vaccine Derived Polio Virus such as: Afghanistan, Nigeria and Pakistan. There are also countries which are prone to have re-infection of patients such as: Cameroon, Central African Republic, Chad, Guinea, Laos People's Democratic Republic, Madagascar, Myanmar, Niger, and Ukraine. And there are countries which are open to have Poliomyelitis: Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Iraq, Kenya, Liberia, Sierra Leone, Somalia, South Sudan, Syrian Arab Republic and Yemen. The Hajj requirement for those people coming from these three areas is summarized in Table 1 . In a recent study of vaccination compliance among pilgrims showed that 99.5% of pilgrims coming from at-risk countries: Pakistan, India, Nigeria, or Afghanistan had poliomyelitis vaccination [28].
Table 1.
Health Requirements and Recommendations for Entry Visas for the Hajj and Umrah.
| Countries or areas at risk | Requirement | |
|---|---|---|
| Yellow fever |
Africa: Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Congo, Cote d’Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Gabon, Guinea, Guinea-Bissau, Gambia, Ghana, Kenya, Liberia, Mali, Mauritania, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, Sudan, South Sudan, Togo and Uganda. |
A valid yellow fever vaccination certificate (≥10 days after the date of vaccination). If no proof of vaccination, persons will be placed under strict surveillance for 6 days from the last date of potential exposure to infection. |
|
South and Central America: Argentina, Venezuela, Brazil, Colombia, Ecuador, French Guiana, Guyana, Panama, Paraguay, Peru, Bolivia, Suriname, and Trinidad and Tobago., | ||
| Meningococcal meningitis (Either polysaccharide or conjugate vaccines) | a) Any visitor | a) Certificate of vaccination with the quadrivalent (ACYW135) vaccine was not given > 3 years (for polysaccharide vaccines) and not > 5 years (for conjugate vaccines) and not < 10 days before arrival in Saudi Arabia. |
| b) Visitors from African meningitis belt: Benin, Burkina Faso, Cameroon, Chad, Central African Republic, Côte d’Ivoire, Eritrea, Ethiopia, Gambia, Guinea, Guinea-Bissau, Mali, Niger, Nigeria, Senegal and Sudan | b) ACYW135 vaccine (as above) AND ciprofloxacin 500 mg (for individuals ≥ 12 years excluding pregnant women) as chemoprophylaxis to be given at the port of entry. | |
| c) Interior pilgrims and the Hajj workers: | c) Vaccination with quadrivalent (ACYW135) vaccine is required if not vaccinated during the past 3 years with a polysaccharide vaccine or 5 years with a conjugate vaccine for: | |
| i) All citizens and residents of Medina and Mecca. | ||
| ii) All citizens and residents undertaking the Hajj. | ||
| iii) All Hajj workers. | ||
| -iv) Any individual working at entry points or in direct contact with pilgrims in Saudi Arabia. | ||
| Poliomyelitis |
a) Areas infected with Wild Polio Virus 1 or circulating Vaccine Derived Polio Virus: Afghanistan, Nigeria and Pakistan. |
|
| b) Areas vulnerable to re-infection: Cameroon, Central African Republic, Chad, Guinea, Laos People's Democratic Republic, Madagascar, Myanmar, Niger, and Ukraine. |
|
|
| c) States which remain vulnerable to Polio: Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Iraq, Kenya, Liberia, Sierra Leone, Somalia, South Sudan, Syrian Arab Republic and Yemen | ||
| Seasonal influenza | All pilgrims (internal and international) and all health-care workers in the Hajj area | It is recommends to have seasonal influenza vaccination |
| Cholera | No specific vaccine requirement |
1.5. Yellow fever vaccinations
The International Health Regulations (IHR) requires documentation of yellow fever vaccines for travelers from areas at risk of yellow fever transmission [29]. Although, yellow fever vaccination was considered valid for 10 years, the WHO World Health Assembly adopted an amended resolution that the yellow fever vaccination will be sufficient for the duration of the life of the vaccinated person starting July 11, 2017. This new guidelines apply to existing and new certificates and the validity begins 10 days after the date of vaccination [30]. The 2016 updated International travel and health lists the following countries as at risk of yellow fever [31]: Africa (Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Congo, Côte d’Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Liberia, Mali, Mauritania, Niger, Nigeria, Senegal, Sierra Leone, South Soudan, Sudan, Togo and Uganda), and Americas (Argentina, the Bolivarian Republic of Venezuela, Brazil, Colombia, Ecuador, French Guyana, Guyana, Panama, Paraguay, Peru, Plurinational State of Bolivia, Suriname and Trinidad and Tobago).
1.6. Influenza vaccinations
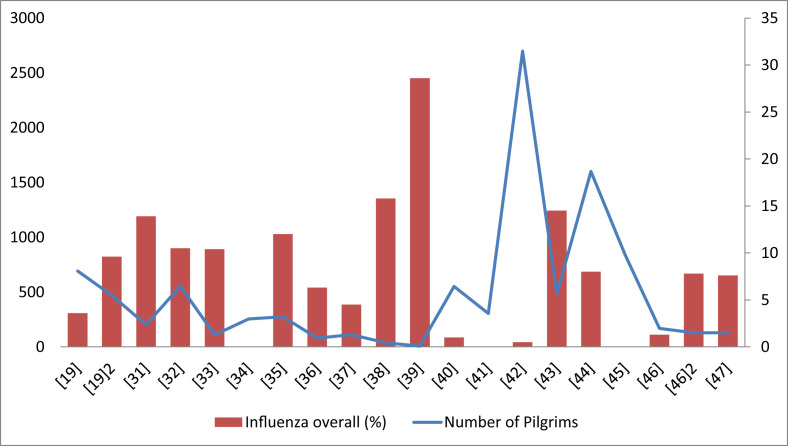
The prevalence of the occurrence of influenza virus by PCR among pilgrims varies depending on the study and ranges from 0-5%–28.6% (average of 9.2%) in various studies [20], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48] (Fig. 2 ). The impact of the pandemic H1N1 influenza was evaluated in five studies [36], [41], [42], [43], [45]. The largest study included 2699 departing pilgrims and 0.1% were positive for H1N1 virus [43] and other studies showed a prevalence of less than 2% [36], [42]. Influenza vaccine decreases development of influenza like-illness among pilgrims [49]. The compliance with influenza vaccination varies from 7.1% to 100% with an overall compliance of 96.3% [49], [50], [51]. The occurrence of the mismatch between vaccine and circulating influenza strains occur frequently and affect the Hajj pilgrims [52]. Currently, it is recommended that all pilgrims and Umrah visitors receive seasonal influenza vaccination [5]. However, influenza vaccine is currently not obligatory for pilgrims. The issue of influenza vaccine availability to match Southern and Northern hemispheres was discussed by the Saudi Ministry of Health in consultation with the World Health Organization and it was recommended to use the available hemisphere strain as long as there is a match in circulating strains.
Fig. 2.
Prevalence of Influenza (%) as detected by PCR among Pilgrims in Various Studies.
1.7. Middle East Respiratory Syndrome Coronavirus (MERS-CoV)
The initial description of the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) was few weeks before the 2012 Hajj season [34], [41], [53]. Subsequently, the following Hajj and Umrah seasons witnessed no transmission of MERS-CoV among pilgrims. Methodical screening of departing pilgrims was evaluated among a large number of visitors with no evidence of MERS-CoV transmission [20], [28], [38], [40], [44], [46], [47], [53], [54], [55], [56], [57], [58]. It is advisable that pilgrims adhere to hand hygiene and follow the cough etiquette and avoid contacts with camels [2].
1.8. Pneumococcal disease
The available literature shows that 7–37% of pilgrims are older adults (≥65 years of age), and that the compliance with age specific pneumococcal vaccine among pilgrims is 5% [59]. In a recent review, the carriage of pneumococcal vaccine serotype was higher in the post-Hajj period compared to the pre-Hajj period [60]. However, the available data do not support a firm recommendation for the S. pneumoniae vaccination of all pilgrims.
1.9. Cholera and diarrheal diseases
Only few reports describe the specific incidence and etiology of diarrhea among pilgrims [61]. Cholera caused multiple outbreaks during the Hajj and the last ones were after the Hajj in 1984–86 and 1989 [62], [63]. Multiple factors contribute to diarrheal illness during the Hajj including inadequate food hygiene, presence asymptomatic carriers of bacteria, and mass food preparation. Cholera continues to cause outbreaks around the globe. World health Organization (WHO) recently reported an outbreak of cholera in Kenya and in Yemen, where the cases in the latter reached 500,000 [64], [65]. There are no recent cholera outbreaks among pilgrims. The Ministry of Health of Saudi Arabia takes active role in observing arriving pilgrims from areas with active cholera outbreaks and initiate quarantine and contact tracing once a case is suspected [2]. In addition, early detection of cases and timely treatment once the pilgrims are diagnosed. There had been extensive improvement and availability of water sources and good sewage systems. Currently, there is no mandatory cholera vaccine for pilgrims arriving from countries with cholera outbreaks.
1.10. Measles and rubella
There are multiple recent outbreaks of measles around the globe. However, to date no reported outbreaks of measles during the Hajj. Few studies confirmed the occurrence of measles in relation to other mass gatherings and had been reported and had been recently reviewed [66]. One measles outbreak took place in Pennsylvania, USA in an international youth sporting event [67]. The index case was a twelve year-old child, and seven (0.32%) of 1250 contacts in 8 states were diagnosed with measles [67]. Two other measles outbreaks occurred among attendees of a church gathering and in the 2010 Taizé festival in France [68], [69].
Most patients were young adults and were unvaccinated. Currently, the Saudi ministry of health as always makes a strong recommendation that all pilgrims are to update their immunization against vaccine-preventable diseases (diphtheria, tetanus, pertussis, polio, measles and mumps) before coming to Umrah or Hajj. Due to the occurrence of outbreaks of measles, there is a potential spread among susceptible populations. The European CDC strongly recommends measles immunization for non-immune pilgrims attending the Hajj [70].
1.11. Vector borne viruses (zika and dengue)
The concern of Zika, Dengue virus and other flaviviruses remain a valid point in the case of mass gatherings such as the Hajj and Umrah. Zika may produce asymptomatic infection in up to 80% of infected population [71]. The situation might be complicated by the presence of Aedes aegyptii in the surrounding cities of the Hajj and Umrah areas. The mosquito transmitting zika virus is the vector of the Yellow fever virus, Dengue Virus and chikungunya virus [72]. In a study of 159 cases of Dengue fever, only two patients were pilgrims [73]. Thus, despite the lack of large studies, it is thought that Dengue virus infection remains limited during the Hajj and Umrah. Thus, pilgrimages during the Hajj and Umrah are advised to take measures to avoid insect bite to reduce the risk of infection with Dengue and other mosquito borne diseases.
1.12. Antimicrobial resistance
A recent systematic review showed a high prevalence and/or a high risk of acquisition of MDR-bacteria in pilgrims during the Hajj [74]. Diarrhea and the use of antibiotics for upper respiratory tract infection were the strongest determinants of extended spectrum betalactamase producing Enterobacteriace acquisition in one study [75]. Overuse of antibiotics by Hajj pilgrims should be discouraged.
2. Conclusion and comments
Each year, the planning for the following Hajj and Umrah season take place with input from many players within the Kingdom of Saudi Arabia [6]. Additionally, the occurrence of outbreak and emerging diseases is received from World Health Organization (WHO), European Centre for Disease Prevention and Control (ECDC), Public Health England (PHE) and United States Centers for Disease Prevention and Control (CDC) through the Public Health Directorate of the Ministry of Health. These combined efforts are coordinated by 24 different committees [6]. The Saudi Ministry of Health then issues recommendations for the required vaccinations and other preventive measures. The ministry also ensures compliance with these required vaccines. Multiple studies showed excellent compliance rates with the recommended vaccinations for the pilgrimage and was 97–100% in case of meningococcal vaccination among arriving international pilgrims [9]. There is a concern that these verified numbers through vaccination cards might represent a false data. In order to verify the reported compliance rates, a serologic study of 796 pilgrims showed that the majority of pilgrims were vaccinated and protected against meningococcal serogroups ACWY [76]. The 2017 Hajj season ended with no reported outbreaks. The experience from each Hajj is growing each year and the planning for the 2018 Hajj had already began. The required vaccines will most likely remain the same with close monitoring for the development of any outbreaks internationally.
Conflict on interest
None.
Financial support
All authors have no funding.
References
- 1.Memish Z.A., Al-Tawfiq J.A. The Hajj in the time of an ebola outbreak in west Africa. Travel Med Infect Dis. 2014;12:415–417. doi: 10.1016/j.tmaid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tawfiq J.A., Memish Z.A. The Hajj: updated health hazards and current recommendations for 2012. Euro Surveill. 2012;17:20295. [PubMed] [Google Scholar]
- 3.Al-Tawfiq J.A., Memish Z.A. Mass gatherings and infectious diseases: prevention, detection, and control. Infect Dis Clin North Am. 2012:26. doi: 10.1016/j.idc.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Memish Z.A., Al-Tawfiq J.A., Al-Rabeeah A.A. Hajj: preparations underway. Lancet Glob Heal. 2013:1. doi: 10.1016/S2214-109X(13)70079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saudi Ministry of Health. Hajj 1438 Hijrah (2017) - Health Regulations 2017. http://www.moh.gov.sa/en/Hajj/Pages/HealthRegulations.aspx (accessed August 18, 2017).
- 6.Al-Tawfiq J.A., Memish Z.A. Mass gathering medicine: 2014 Hajj and Umra preparation as a leading example. Int J Infect Dis. 2014;27:26–31. doi: 10.1016/j.ijid.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Tawfiq J.A., Memish Z.A. Mass gatherings and infectious diseases. Prevention, detection, and control. Infect Dis Clin North Am. 2012:26. doi: 10.1016/j.idc.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 8.al-Gahtani Y.M., el Bushra H.E., al-Qarawi S.M., al-Zubaidi A.A., Fontaine R.E. Epidemiological investigation of an outbreak of meningococcal meningitis in Makkah (Mecca), Saudi Arabia. Epidemiol Infect. 1992;1995(115):399–409. doi: 10.1017/s0950268800058556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Memish Z.A., Al-Tawfiq J.A., Almasri M., Azhar E.I., Yasir M., Al-Saeed M.S. Neisseria meningitidis nasopharyngeal carriage during the Hajj: a cohort study evaluating the need for ciprofloxacin prophylaxis. Vaccine. 2017;35:2473–2478. doi: 10.1016/j.vaccine.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 10.Borrow R. Meningococcal disease and prevention at the Hajj. Travel Med Infect Dis. 2009;7:219–225. doi: 10.1016/j.tmaid.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Memish Z., Al Hakeem R., Al Neel O., Danis K., Jasir A., Eibach D. Laboratory-confirmed invasive meningococcal disease: effect of the Hajj vaccination policy, Saudi Arabia, 1995 to 2011. Euro Surveill. 2013;18 doi: 10.2807/1560-7917.es2013.18.37.20581. pii: 20581. [DOI] [PubMed] [Google Scholar]
- 12.Memish Z.A., Venkatesh S., Ahmed Q.A. Travel epidemiology: the Saudi perspective. Int J Antimicrob Agents. 2003;21:96–101. doi: 10.1016/s0924-8579(02)00364-3. [DOI] [PubMed] [Google Scholar]
- 13.Mayer L.W., Reeves M.W., Al-Hamdan N., Sacchi C.T., Taha M.-K., Ajello G.W. Outbreak of W135 meningococcal disease in 2000: not emergence of a new W135 strain but clonal expansion within the electrophoretic type-37 complex. J Infect Dis. 2002;185:1596–1605. doi: 10.1086/340414. [DOI] [PubMed] [Google Scholar]
- 14.Issack M.I., Ragavoodoo C. Hajj-related Neisseria meningitidis serogroup w135 in Mauritius. Emerg Infect Dis. 2002;8:332–334. doi: 10.3201/eid0803.010372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Memish Z.A. Meningococcal disease and travel. Clin Infect Dis. 2002;34:84–90. doi: 10.1086/323403. [DOI] [PubMed] [Google Scholar]
- 16.Shibl A., Tufenkeji H., Khalil M., Memish Z. Meningococcal Leadership Forum (MLF) Expert Group. Consensus recommendation for meningococcal disease prevention for Hajj and Umra pilgrimage/travel medicine. East Mediterr Health J. 2013;19:389–392. [PubMed] [Google Scholar]
- 17.Alborzi A, Oskoee S, Pourabbas B, Alborzi S, Astaneh B, Gooya MM, et al. Meningococcal carrier rate before and after Hajj pilgrimage: effect of single dose ciprofloxacin on carriage. East Mediterr Health J nd;14:277–282. [PubMed]
- 18.Wilder-Smith A., Barkham T.M.S., Chew S.K., Paton N.I. Absence of Neisseria meningitidis W-135 electrophoretic type 37 during the Hajj. Emerg Infect Dis. 2002;2003(9):734–737. doi: 10.3201/eid0906.020725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilder-Smith A., Barkham T.M.S., Earnest A., Paton N.I. Acquisition of W135 meningococcal carriage in Hajj pilgrims and transmission to household contacts: prospective study. BMJ. 2002;325:365–366. doi: 10.1136/bmj.325.7360.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Memish Z.A., Assiri A., Turkestani A., Yezli S., Al Masri M., Charrel R. Mass gathering and globalization of respiratory pathogens during the 2013 Hajj. Clin Microbiol Infect. 2015;21:571. doi: 10.1016/j.cmi.2015.02.008. e1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrison L.H., Trotter C.L., Ramsay M.E. Global epidemiology of meningococcal disease. Vaccine. 2009;27:B51–B63. doi: 10.1016/j.vaccine.2009.04.063. [DOI] [PubMed] [Google Scholar]
- 22.Jafri R.Z., Ali A., Messonnier N.E., Tevi-Benissan C., Durrheim D., Eskola J. Global epidemiology of invasive meningococcal disease. Popul Health Metr. 2013;11:17. doi: 10.1186/1478-7954-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soeters H.M., McNamara L.A., Whaley M., Wang X., Alexander-Scott N., Kanadanian K.V. Serogroup B meningococcal disease outbreak and carriage evaluation at a college - Rhode Island. MMWR Morb Mortal Wkly Rep. 2015;2015(64):606–607. [PMC free article] [PubMed] [Google Scholar]
- 24.McNamara L.A., Shumate A.M., Johnsen P., MacNeil J.R., Patel M., Bhavsar T. First use of a serogroup B meningococcal vaccine in the US in response to a university outbreak. Pediatrics. 2015;135:798–804. doi: 10.1542/peds.2014-4015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Folaranmi T., Rubin L., Martin S.W., Patel M., MacNeil J.R. Centers for disease control (CDC). Use of serogroup B meningococcal vaccines in persons aged ≥10 Years at increased risk for serogroup B meningococcal disease: recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;2015(64):608–612. [PMC free article] [PubMed] [Google Scholar]
- 26.Mushtaq A., Mehmood S., Rehman M.A.U., Younas A., Rehman M.S.U., Malik M.F. Polio in Pakistan: social constraints and travel implications. Travel Med Infect Dis. 2015;13:360–366. doi: 10.1016/j.tmaid.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Wilder-Smith A., Leong W.-Y., Lopez L.F., Amaku M., Quam M., Khan K. Potential for international spread of wild poliovirus via travelers. BMC Med. 2015;13:133. doi: 10.1186/s12916-015-0363-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Memish Z.A., Assiri A., Almasri M., Alhakeem R.F., Turkestani A., Al Rabeeah A.A. Prevalence of MERS-CoV nasal carriage and compliance with the Saudi health recommendations among pilgrims attending the 2013 Hajj. J Infect Dis. 2014;210:1067–1072. doi: 10.1093/infdis/jiu150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO | International Health Regulations (IHR) n.d.
- 30.World Health Organization . WHO; 2016. New yellow fever vaccination requirements for travellers.http://www.who.int/ith/updates/20160727/en/ [Google Scholar]
- 31.World Health Organization . 2016. Countries with risk of yellow fever transmission and countries requiring yellow fever vaccination.http://www.who.int/ith/2016-ith-annex1.pdf?ua=1 [Google Scholar]
- 32.Rashid H., Shafi S., Booy R., El Bashir H., Ali K., Zambon M. Influenza and respiratory syncytial virus infections in British Hajj pilgrims. Emerg Health Threats J. 2008;1:e2. doi: 10.3134/ehtj.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rashid H., Shafi S., Haworth E., El Bashir H., Ali K.A., Memish Z.A. Value of rapid testing for influenza among Hajj pilgrims. Travel Med Infect Dis. 2007;5:310–313. doi: 10.1016/j.tmaid.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Rashid H., Shafi S., Haworth E., El Bashir H., Memish Z.A., Sudhanva M. Viral respiratory infections at the Hajj: comparison between UK and Saudi pilgrims. Clin Microbiol Infect. 2008;14:569–574. doi: 10.1111/j.1469-0691.2008.01987.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alborzi A., Aelami M.H., Ziyaeyan M., Jamalidoust M., Moeini M., Pourabbas B. Viral etiology of acute respiratory infections among iranian Hajj pilgrims. J Travel Med. 2006;2009(16):239–242. doi: 10.1111/j.1708-8305.2009.00301.x. [DOI] [PubMed] [Google Scholar]
- 36.Moattari A., Emami A., Moghadami M., Honarvar B. Influenza viral infections among the Iranian Hajj pilgrims returning to Shiraz, Fars province, Iran. Influenza Other Respi Viruses. 2012;6:e77–e79. doi: 10.1111/j.1750-2659.2012.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barasheed O., Almasri N., Badahdah A.-M., Heron L., Taylor J., McPhee K. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like illness transmission among australian Hajj pilgrims in 2011. Infect Disord Drug Targets. 2014;14:110–116. doi: 10.2174/1871526514666141021112855. [DOI] [PubMed] [Google Scholar]
- 38.Barasheed O., Rashid H., Alfelali M., Tashani M., Azeem M., Bokhary H. Viral respiratory infections among Hajj pilgrims in 2013. Virol Sin. 2014;29:364–371. doi: 10.1007/s12250-014-3507-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Memish Z.A., Almasri M., Turkestani A., Al-Shangiti A.M., Yezli S. Etiology of severe community-acquired pneumonia during the 2013 Hajj-part of the MERS-CoV surveillance program. Int J Infect Dis. 2014;25:186–190. doi: 10.1016/j.ijid.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aberle J.H., Popow-Kraupp T., Kreidl P., Laferl H., Heinz F.X., Aberle S.W. Influenza A and B Viruses but not MERS-CoV in Hajj pilgrims, Austria. Emerg Infect Dis. 2014;2015(21):726–727. doi: 10.3201/eid2104.141745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kandeel A., Deming M., Elkreem E.A., El-Refay S., Afifi S., Abukela M. Pandemic (H1N1) 2009 and Hajj pilgrims who received predeparture vaccination, Egypt. Emerg Infect Dis. 2011;17:1266–1268. doi: 10.3201/eid1707.101484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ziyaeyan M., Alborzi A., Jamalidoust M., Moeini M., Pouladfar G.R., Pourabbas B. Pandemic 2009 influenza A (H1N1) infection among 2009 Hajj Pilgrims from Southern Iran: a real-time RT-PCR-based study. Influenza Other Respi Viruses. 2012;6:e80–e84. doi: 10.1111/j.1750-2659.2012.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Memish ZA, Assiri AM, Hussain R, Alomar I, Stephens G. Detection of respiratory viruses among pilgrims in Saudi Arabia during the time of a declared influenza A(H1N1) pandemic. J Travel Med 19:15–21. doi:10.1111/j.1708-8305.2011.00575.x. [DOI] [PMC free article] [PubMed]
- 44.Refaey S., Amin M.M., Roguski K., Azziz-Baumgartner E., Uyeki T.M., Labib M. Cross-Sectional survey and surveillance for influenza viruses and MERS-CoV among egyptian pilgrims returning from Hajj during 2012-2015. Influenza Other Respi Viruses. 2016 doi: 10.1111/irv.12429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ashshi A., Azhar E., Johargy A., Asghar A., Momenah A., Turkestani A. Demographic distribution and transmission potential of influenza A and 2009 pandemic influenza A H1N1 in pilgrims. J Infect Dev Ctries. 2014;8:1169–1175. doi: 10.3855/jidc.4204. [DOI] [PubMed] [Google Scholar]
- 46.Annan A., Owusu M., Marfo K.S., Larbi R., Sarpong F.N., Adu-Sarkodie Y. High prevalence of common respiratory viruses and no evidence of Middle East respiratory syndrome coronavirus in Hajj pilgrims returning to Ghana. Trop Med Int Health. 2013;2015(20):807–812. doi: 10.1111/tmi.12482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benkouiten S., Charrel R., Belhouchat K., Drali T., Nougairede A., Salez N. Respiratory viruses and bacteria among pilgrims during the 2013 Hajj. Emerg Infect Dis. 2014;20:1821–1827. doi: 10.3201/eid2011.140600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gautret P., Charrel R., Benkouiten S., Belhouchat K., Nougairede A., Drali T. Lack of MERS coronavirus but prevalence of influenza virus in French pilgrims after 2013 Hajj. Emerg Infect Dis. 2014;20:728–730. doi: 10.3201/eid2004.131708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aleflali M., Khandaker G., Booy R., Rashid H. Mismatching between circulating strains and vaccine strains of influenza: effect on Hajj pilgrims from both hemispheres. Hum Vaccin Immunother. 2015 doi: 10.1080/21645515.2015.1085144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alfelali M., Barasheed O., Tashani M., Azeem M.I., El Bashir H., Memish Z.A. Changes in the prevalence of influenza-like illness and influenza vaccine uptake among Hajj pilgrims: a 10-year retrospective analysis of data. Vaccine. 2015;33:2562–2569. doi: 10.1016/j.vaccine.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 51.Al-Tawfiq J.A., Benkouiten S., Memishc Z.A. Systematic review of emerging respiratory viruses at the Hajj and possible coinfection with Streptococcus pneumoniae. Vaccine. 2017 doi: 10.1016/j.tmaid.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gautret P, Vu Hai V, Sani S, Doutchi M, Parola P, Brouqui P. Protective measures against acute respiratory symptoms in French pilgrims participating in the Hajj of 2009. J Travel Med 18:53–55. doi:10.1111/j.1708-8305.2010.00480.x. [DOI] [PubMed]
- 53.Al-Tawfiq J.A., Smallwood C.A.H., Arbuthnott K.G., Malik M.S.K., Barbeschi M., Memish Z.A. Emerging respiratory and novel coronavirus 2012 infections and mass gatherings. East Mediterr Heal J = La Rev Santé La Méditerranée Orient = Al-Majallah Al-Ṣiḥḥīyah Li-Sharq Al-Mutawassiṭ. 2013;19(Suppl 1):S48–S54. [PubMed] [Google Scholar]
- 54.Gautret P., Charrel R., Belhouchat K., Drali T., Benkouiten S., Nougairede A. Lack of nasal carriage of novel corona virus (HCoV-EMC) in French Hajj pilgrims returning from the Hajj 2012, despite a high rate of respiratory symptoms. Clin Microbiol Infect. 2013;19:E315–E317. doi: 10.1111/1469-0691.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baharoon S., Al-Jahdali H., Al Hashmi J., Memish Z.A., Ahmed Q.A. Severe sepsis and septic shock at the Hajj: etiologies and outcomes. Travel Med Infect Dis. 2009;7:247–252. doi: 10.1016/j.tmaid.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 56.Atabani S.F., Wilson S., Overton-Lewis C., Workman J., Kidd I.M., Petersen E. Active screening and surveillance in the United Kingdom for Middle East respiratory syndrome coronavirus in returning travellers and pilgrims from the Middle East: a prospective descriptive study for the period 2013–2015. Int J Infect Dis. 2016;47:10–14. doi: 10.1016/j.ijid.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.ProMed . 2013. Novel coronavirus – eastern mediterranean (03): Saudi comment 12 February 2013.http://promedmail.org/post/20130326.1603038 [Google Scholar]
- 58.Griffiths K., Charrel R., Lagier J.-C., Nougairede A., Simon F., Parola P. Infections in symptomatic travelers returning from the Arabian peninsula to France: a retrospective cross-sectional study. Travel Med Infect Dis. 2016;14:414–416. doi: 10.1016/j.tmaid.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Al-Tawfiq J.A., Memish Z.A. Prevention of pneumococcal infections during mass gathering. Hum Vaccin Immunother. 2016;12:326–330. doi: 10.1080/21645515.2015.1058456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Edouard S., Al-Tawfiq J.A., Memish Z.A., Yezli S., Gautret P. Impact of the Hajj on pneumococcal carriage and the effect of various pneumococcal vaccines. Vaccine. 2017 doi: 10.1016/j.vaccine.2017.03.109. [DOI] [PubMed] [Google Scholar]
- 61.Memish Z.A., Zumla A., Alhakeem R.F., Assiri A., Turkestani A., Al Harby K.D. Hajj: infectious disease surveillance and control. Lancet. 2014;383:2073–2082. doi: 10.1016/S0140-6736(14)60381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gautret P., Benkouiten S., Sridhar S., Al-Tawfiq J.A., Memish Z.A. Diarrhea at the Hajj and Umrah. Travel Med Infect Dis. 2015;13:159–166. doi: 10.1016/j.tmaid.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 63.Ahmed Q.A., Arabi Y.M., Memish Z.A. Health risks at the Hajj. Lancet (London, Engl. 2006;367:1008–1015. doi: 10.1016/S0140-6736(06)68429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization Cholera – Kenya WHO 2017. http://www.who.int/csr/don/21-july-2017-cholera-kenya/en/(accessed August 21, 2017).
- 65.World Health Organization . WHO; 2017. Cholera count reaches 500 000 in Yemen.http://www.who.int/mediacentre/news/releases/2017/cholera-yemen-mark/en/ [Google Scholar]
- 66.Gautret P., Steffen R. Communicable diseases as health risks at mass gatherings other than Hajj: what is the evidence? Int J Infect Dis. 2016;47:46–52. doi: 10.1016/j.ijid.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 67.Chen T.-H., Kutty P., Lowe L.E., Hunt E.A., Blostein J., Espinoza R. Measles outbreak associated with an international youth sporting event in the United States. Pediatr Infect Dis J. 2007;2010(29):794–800. doi: 10.1097/INF.0b013e3181dbaacf. [DOI] [PubMed] [Google Scholar]
- 68.Parker A.A., Staggs W., Dayan G.H., Ortega-Sánchez I.R., Rota P.A., Lowe L. Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355:447–455. doi: 10.1056/NEJMoa060775. [DOI] [PubMed] [Google Scholar]
- 69.Pfaff G., Lohr D., Santibanez S., Mankertz A., van Treeck U., Schonberger K. Spotlight on measles 2010: measles outbreak among travellers returning from a mass gathering, Germany, September to October. Euro Surveill. 2010;2010:15. pii: 19750. [PubMed] [Google Scholar]
- 70.Ecdc . 2017. Public health risks related to communicable diseases during the Hajj 2017, Saudi Arabia 30 August – 4 September 2017.https://ecdc.europa.eu/sites/portal/files/documents/RRA-Mass-gathering-Saudi-Arabia-Hajj-10-Aug-2017.pdf [Google Scholar]
- 71.Ahmed Q.A., Memish Z.A. Yellow fever and Hajj: with all eyes on Zika, a familiar flavivirus remains a threat. Front Med. 2016;10:527–530. doi: 10.1007/s11684-016-0487-2. [DOI] [PubMed] [Google Scholar]
- 72.Elachola H., Sow S., Al-Tawfiq J., Memish Z. Better than before and yet no quick fix: zika virus outbreak and its containment efforts. J Heal Spec. 2016;4:87. doi: 10.4103/1658-600X.179824. [DOI] [Google Scholar]
- 73.Shahin W., Nassar A., Kalkattawi M., Bokhari H. Dengue fever in a tertiary hospital in Makkah, Saudi Arabia. Dengue Bull. 2009:33. [Google Scholar]
- 74.Leangapichart T., Rolain J.-M., Memish Z.A., Al-Tawfiq J.A., Gautret P. Emergence of drug resistant bacteria at the Hajj: a systematic review. Travel Med Infect Dis. 2017;18:3–17. doi: 10.1016/j.tmaid.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 75.Leangapichart T., Tissot-Dupont H., Raoult D., Memish Z.A., Rolain J.-M., Gautret P. Risk factors for acquisition of CTX-M genes in pilgrims during Hajj 2013 and 2014. J Antimicrob Chemother. 2017;72:2627–2635. doi: 10.1093/jac/dkx155. [DOI] [PubMed] [Google Scholar]
- 76.Memish Z.A., Yezli S., Almasri M., Assiri A., Turkestani A., Findlow H. Meningococcal serogroup A, C, W, and Y serum bactericidal antibody profiles in Hajj pilgrims. Int J Infect Dis. 2014;28:171–175. doi: 10.1016/j.ijid.2014.09.005. [DOI] [PubMed] [Google Scholar]