Summary
Over the past decade, a number of unique zoonotic and non-zoonotic viruses have emerged in Malaysia. Several of these viruses have resulted in significant morbidity and mortality to those affected and they have imposed a tremendous public health and economic burden on the state. Amongst the most devastating was the outbreak of Nipah virus encephalitis in 1998, which resulted in 109 deaths. The culling of more than a million pigs, identified as the amplifying host, ultimately brought the outbreak under control. A year prior to this, and subsequently again in 2000 and 2003, large outbreaks of hand-foot-and-mouth disease due to enterovirus 71, with rare cases of fatal neurological complications, were reported in young children. Three other new viruses – Tioman virus (1999), Pulau virus (1999), and Melaka virus (2006) – whose origins have all been linked to bats, have been added to the growing list of novel viruses being discovered in Malaysia. The highly pathogenic H5N1 avian influenza has also been detected in Malaysia with outbreaks in poultry in 2004, 2006, and 2007. Fortunately, no human infections were reported. Finally, the HIV/AIDS epidemic has seen the emergence of an HIV-1 recombinant form (CRF33_01B) in HIV-infected individuals from various risk groups, with evidence of ongoing and rapid expansion.
Keywords: Enterovirus 71, Nipah virus, Tioman virus, Melaka virus, HIV-1 CRF33_01B, Highly pathogenic avian influenza H5N1
Introduction
Malaysia (2°30′N, 112°30′E) is located in the heart of Southeast Asia with a population of approximately 27 million as of 2007. It is made up of Peninsular Malaysia and the Malaysian Borneo, which are separated by the South China Sea, divided into a federation of 13 states and three federal territories including the Kuala Lumpur Federal Territory. The majority of the population is concentrated in Peninsular Malaysia with approximately 20 million people living in this more developed area of the country. The local climate is tropical and characterized by annual monsoons from October to January.
Progressive development over the last 50 years since independence in 1957 has meant that infectious diseases have gradually ceased to be the leading cause of death, with chronic diseases such as cardiovascular disease, cancer, chronic respiratory diseases, and diabetes mellitus becoming more commonplace amongst the increasingly more affluent Malaysians. However over the last decade attention has once again been drawn to infectious diseases, with the emergence of new infections and the re-emergence of diseases previously well-controlled in the Asian region in general, and in Malaysia in particular.1, 2 In Southeast Asia alone, the discovery of new human viruses that cause large and devastating epidemics, such as the severe acute respiratory syndrome (SARS) coronavirus and the highly pathogenic avian influenza (HPAI) H5N1 virus, have been reported. Unlike some countries in the region, Malaysia was spared from the outbreak of SARS coronavirus and has yet to identify the HPAI H5N1 infection in humans that adversely affected neighboring countries (although frequent outbreaks in poultry have been reported). Nevertheless, in the last decade, Malaysia has been battling different challenges caused by various known or novel zoonotic and non-zoonotic viruses identified for the first time in the country.
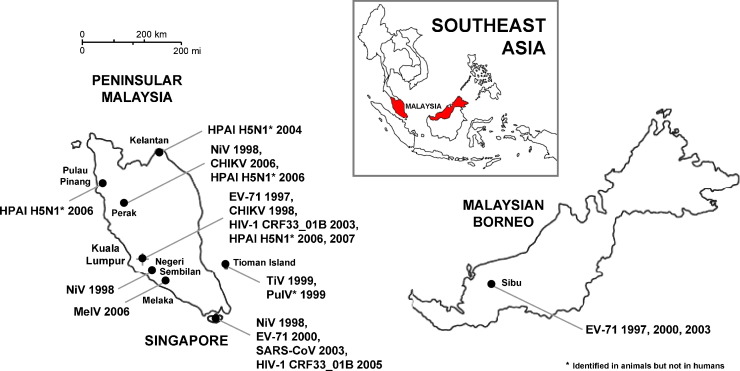
In this article we provide historical, epidemiological, clinical, and scientific insights into the emerging, re-emerging, and recombinant viruses identified in Malaysia between 1997 and 2007 (Figure 1 ). Although the discovery of novel viruses on some occasions may be explained partly as being an artifact of increased surveillance and reporting efforts in the country – the best example being the investigation of Nipah virus, which led to the incidental discovery of other novel zoonotic viruses – recent studies, taking into account various socio-economic, environmental, and ecological factors associated with the emergence of infectious diseases,3, 4, 5, 6 show that lower-latitude developing countries including Malaysia are particularly at risk of emerging infectious disease events due primarily to zoonotic pathogens of wildlife origin and vector-borne pathogens.2 Here, we discuss probable events that have been implicated in the appearance of these viruses, with the aim of strengthening the existing preventive measures and strategies for managing potentially new and unfamiliar diseases in the future.
Figure 1.
Zoonotic, non-zoonotic, and vector-borne viruses emerged in Malaysia between 1997 and 2007. The abbreviations for the viruses and their year(s) of emergence at various locations in Malaysia are shown. Viral outbreaks in Singapore during the same period are also indicated. HPAI H5N1, highly pathogenic avian influenza subtype H5N1; NiV, Nipah virus; CHIKV, chikungunya virus; EV-71, enterovirus 71; HIV-1 CRF33_01B, HIV type 1 circulating recombinant form (CRF33_01B); MelV, Melaka virus; TiV, Tioman virus; PulV, Pulau virus; SARS-CoV, severe acute respiratory syndrome coronavirus.
Enterovirus 71
Human enterovirus 71 (EV-71) and 11 other group A coxsackieviruses (CV-A) are members of the human enterovirus A (HEV-A) species from the Enterovirus genus of the Picornaviridae family. Enteroviruses are distributed worldwide and can be transmitted effectively through the fecal–oral route and to a lesser extent, by respiratory transmission. The great majority of enterovirus infections are asymptomatic, but some can lead to serious illnesses particularly in infants and the immunocompromised. Hand-foot-and-mouth disease (HFMD) in children is usually caused by enteroviruses such as CV-A10, CV-A16, and EV-71.
An epidemic of HFMD was first reported in Sibu, Sarawak (Malaysian Borneo) in April 1997,7, 8, 9, 10 followed by smaller outbreaks in Peninsular Malaysia in the same year (Figure 1).7, 8, 11 More than 2600 children were infected. Most presented with a febrile illness and characteristic lesions on the palms, soles, and oral mucosa, but a small proportion, mainly children <6 years of age, presented with severe neurological complications such as aseptic meningitis, poliomyelitis-like acute flaccid paralysis, or fatal encephalomyelitis. Cardiopulmonary symptoms such as neurogenic pulmonary edema with secondary myocardial dysfunction leading to rapid cardio-respiratory decompensation were also reported. Twenty-nine children eventually succumbed to the disease in Sarawak10 and 12 in Peninsular Malaysia.11
EV-71 was isolated from neuronal or non-neuronal samples from most of the infected children, including those who succumbed to the infection,7, 8, 9, 11 suggesting its role as the etiologic agent. Different lineages of EV-71 subgenotypes C1 and C2 and two previously undefined subgenotypes B3 and B4 were identified in these outbreaks, with novel subgenotype B3 being the most prevalent strain in Sarawak in 1997, particularly among patients with the milder form of HFMD.7, 12, 13, 14 Further outbreaks occurred in 2000 and 2003 in Sarawak where newly identified subgenotypes B4 and B5 were predominant.12, 15, 16 Interestingly, phylogenetic and recombination analyses revealed that some EV-71 strains isolated in the 1997 outbreak were intertypic recombinant involving EV-71 subgenotype B3, CV-A16, and various HEV-A species.17, 18 These recombinant strains were isolated from uncomplicated HFMD cases and were thought to have reduced viral fitness and adaptation to host immunity compared to the parental strains. The pathogenic potential and clinical attributes of these recombinants, however, are not well understood.
Subsequent to the first outbreaks in Malaysia, several large EV-71-associated HFMD outbreaks were also reported across the Asia Pacific region: in Taiwan in 1998;19 in Western Australia in 1999;20 in Singapore,21, 22 Japan,23 Korea,12 and Taiwan in 2000;24 in Vietnam in 2005;25 and in China in 2008.26 Despite the occurrence of numerous HFMD and EV-71 outbreaks worldwide since 1969, no outbreaks involving fatal cases of brainstem encephalitis and neurogenic pulmonary edema have been reported,27 except for those in Malaysia, Taiwan (which claimed 78 lives19), and recently in Vietnam and China. This shows that over the past decades EV-71 may have evolved to become more pathogenic than its ancestral strains. In the meantime, the synergistic potential exerted by other infectious agents in the pathogenesis of the disease cannot be ruled out. This includes the description of acute flaccid paralysis caused by adenoviruses9, 28 and echovirus 7-associated encephalomyelitis29 during these outbreaks. Furthermore, a prospective study conducted during the 2000 and 2003 HFMD outbreaks in Sarawak showed that co-infection with another enterovirus or adenovirus among children with EV-71 was common.16
Diverse EV-71 subgenotypes determined from different genomic regions indicate that multiple EV-71 lineages have been circulating in the Asia Pacific region since 1997, with each subgenotype causing distinct outbreaks of varying clinical manifestations and neurovirulence. Driven by such complexity, it has not been possible to identify a single neurovirulent genotype nor its pathogenic mechanisms associated with the severe neurological outcomes – although recent studies have suggested that subgenotype B516 and particular subgenotypes from the genogroup C14, 30 are linked with neurological complications. Continued molecular epidemiological surveillance is essential to delineate the temporal trends of EV-71 transmission, the neuropathogenic potential of its subgenotypes, and to plan for effective clinical interventions plus preventive measures.12, 15
Nipah virus
In September 1998, an outbreak of respiratory illness and encephalitis with low morbidity and mortality rates occurred among pigs in commercial farms (initially presumed as porcine respiratory and encephalitis syndrome) in the Kinta district of Ipoh, Perak state in Peninsular Malaysia.31 Later in the month, a group of workers linked with pig farming presented with acute febrile encephalitis that was associated with a high case fatality rate.32, 33, 34 The disease affecting humans was initially diagnosed as Japanese encephalitis (JE), which is endemic in Malaysia,35 prompting health authorities to attempt to contain the outbreak based on preventive measures against JE in the Kinta district and also throughout the country. The infected pigs in the Kinta district were presumed to be disease-free and eventually transported to pig farms and abattoirs in other states in Malaysia, and also to neighboring Singapore.
Two months later in December 1998, a similar outbreak was detected in Sikamat town, and then by February 1999 in Sungai Nipah village and the town of Bukit Pelandok, all within the city of Seremban in the state of Negeri Sembilan located in central Peninsular Malaysia.34 Approximately 70% of the infected patients were of Chinese ethnicity and were directly involved in pig farming activities (as pig farmers and workers). Those affected had had direct contact with pigs in the 2 weeks before the onset of illness, suggesting direct viral transmission from pigs to humans with a short incubation period. These patients presented with an acute illness with fever, headache, dizziness, vomiting, and reduced levels of consciousness, before rapidly progressing to severe encephalitis that was associated with a high mortality rate.36, 37 Up to 25% of cases had concomitant respiratory syndromes.34, 38 A similar outbreak was then reported in Singapore among abattoir workers who had handled infected pigs imported from Malaysia.39
In early March 1999, a novel paramyxovirus responsible for the outbreak was isolated from the cerebrospinal fluid of an encephalitic patient from Sungai Nipah village, and was later named the Nipah virus (NiV).34, 40 The discovery of NiV played a critical role and was an important turning point in controlling the outbreak. Strong evidence showed that transmission of NiV to humans was through close contact with infected pigs,41, 42 and affected those directly involved in pig farming activities such as assisting in pig breeding and birthing of piglets, those administering injections or medications to pigs, and those handling dead pigs. This led to an immediate halt in direct handling and transportation of pigs within the country and subsequently the culling of over a million pigs.40 Human-to-human transmission of NiV was also described among healthcare workers,43 although this was uncommon.44 The overall case fatality rate for the outbreak reported by the Ministry of Health was 38.5%; 109 fatalities from 283 cases of viral encephalitis.45
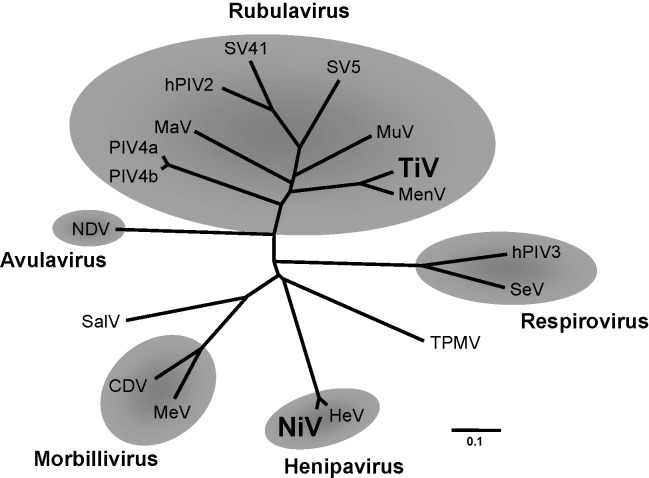
Genetic characterization revealed that NiV is closely related to the Hendra virus (HeV), a paramyxovirus species causing severe respiratory disease in horses and humans in Queensland, Australia, which first emerged in 1994.46 The full-length genome sequences of NiV and HeV are approximately 18 kb,47 significantly longer than the average size of 15.5 kb of other viral genomes from the Paramyxovirinae subfamily. NiV and HeV also share similar genomic organization, both having increased nucleotide length of the 3′ non-coding region in most of the genes. Taking together the close phylogenetic relationship of NiV and HeV40, 48 plus its distinct divergence and little immunological cross-reactivity with other established genera within the Paramyxoviridae, the two geographically remote viruses were classified as belonging to a new genus – Henipavirus 49, 50 (Figure 2 ). This unique relationship between NiV and HeV played an important role in identifying the natural reservoir for NiV in Malaysia. Based on findings that fruit bat species of the genus Pteropus are natural hosts of HeV,51, 52 extensive serological surveillance within and outside the outbreak epicenters was conducted involving various species of wild fruit bats plus other wildlife and domestic animals. Neutralizing antibodies against NiV were detected among the variable flying foxes (previously known as the Island flying foxes; Pteropus hypomelanus), Malayan flying foxes (Pteropus vampyrus), and other species of the order Chiroptera, suggesting widespread infection of NiV in the bat population in Peninsular Malaysia.53, 54 A novel method of collecting free-living fruit bat urine samples using plastic sheets was then adopted, and eventually NiV was isolated from urine samples and swabs from fruits partially eaten by the variable flying foxes,55 corroborating the serological evidence that fruit bats are the natural hosts of NiV.56 Following this feat, serological and/or genetic evidence of NiV circulating among the expansive species of flying foxes was also reported in Thailand,57 Indonesia,58 Cambodia,59, 60 Bangladesh,61, 62 and India63 indicating wide dissemination of NiV across Southeast and South Asia, especially in countries where populations of the Pteropus species are overlapping. Recent studies have also shown NiV circulating in Madagascar located in the southeastern part of Africa64 and Ghana in West Africa.65
Figure 2.
Phylogenetic reconstruction of the deduced amino acid sequence of the complete N gene of select Paramyxovirinae subfamily members. Nipah virus and Tioman virus, two newly emergent paramyxoviruses in Malaysia, are clustered within the Henipavirus and Rubulavirus genus, respectively. Rubulavirus genus: MuV, mumps virus; MenV, Menangle virus; TiV, Tioman virus; MaV, Mapuera virus; SV5, simian parainfluenza virus 5; SV41, simian parainfluenza virus 41; hPIV2, human parainfluenza virus 2; hPIV4a, human parainfluenza virus 4a; hPIV4b, human parainfluenza virus 4b. Respirovirus genus: SeV, Sendai virus; hPIV3, human parainfluenza virus 3. Henipavirus genus: NiV, Nipah virus; HeV, Hendra virus. Morbillivirus genus: MeV, measles virus; CDV, canine distemper virus. Avulavirus genus: NDV, Newcastle disease virus. Unclassified viruses: SalV, Salem virus; TPMV, Tupaia paramyxovirus.
The discovery of NiV as the causative agent of severe febrile encephalitis in humans and the identification of pteropid fruit bats as the natural hosts has helped regional as well as international scientific communities to be better prepared with management strategies for similar emerging zoonotic diseases, as witnessed in the recent NiV-associated encephalitis outbreaks in Bangladesh.61, 62, 66, 67 During the Bangladesh outbreaks between 2001 and 2005, the transmission pattern of NiV, however, seemed different from that in Malaysia because there was no involvement of pigs, and many of the patients who presented largely with neurological symptoms were young males who may have had direct contact with fruits eaten by bats or had consumed contaminated date palm sap.68 In addition, NiV spread occurred over a wide area in the country complicated by cases of human-to-human transmission.69 In some areas, the case fatality rate was as high as 75%.66 In India, a similar viral encephalitis outbreak was also reported in 2001 in the city of Siliguri, West Bengal not far from Bangladesh.70 Anthropogenic factors such as unrestrained deforestation and human population expansion in Bangladesh and India could possibly have been linked to these outbreaks. The high virulence of NiV and HeV and the wide range of susceptible hosts plus the absence of therapeutic and prophylactic interventions have led to the classification of these viruses as Biosafety Level 4 pathogens.71
Tioman virus
The pursuit of the natural host of NiV led to the unexpected discovery of another novel zoonotic virus in 1999. On an island about 25 km off the eastern coast of Peninsular Malaysia, a new virus of the Paramyxoviridae family called the Tioman virus (TiV) was identified.72, 73 TiV was isolated from pooled urine samples of free-living variable flying foxes (P. hypomelanus) roosting on tree branches along the coastal region of the island. TiV displayed characteristic microscopic features similar to those of other viruses in the Paramyxoviridae family: spherical, pleiomorphic, and enveloped viral particles with glycoprotein spikes.72 Serological tests revealed cross-reactivity with the Menangle virus (MenV), another newly described Paramyxoviridae member that caused infections among pigs and humans in New South Wales, Australia in 1997.74 Similar to NiV, evidence of TiV circulating among bats in wide geographical proximity has been reported.64
Phylogenetic analyses show that TiV and MenV are clustered in the Rubulavirus genus with up to 85% amino acid similarity in the nucleocapsid (N) gene between the two viruses (Figure 2). The N protein shows significant sequence homologies with other Rubulavirus members, including the mumps virus (approximately 50%). Human disease caused by TiV has not been documented thus far, although possible human infections, as determined by the presence of antibodies against TiV among the island inhabitants, have been observed.75 Animal experiments have demonstrated that TiV is neurotropic causing necrosis in the cerebrum and hypothalamus in intracerebrally-inoculated mice76 and is capable of causing mild disease in pigs, mainly by affecting the lymphoid tissues.77
Chikungunya virus
The first sporadic outbreak of chikungunya virus (CHIKV) infection occurred between late 1998 and early 1999 in Port Klang, Kuala Lumpur.78 Fifty-one patients living in low-cost and squatter estates presented with fever, polyarthritis of the small joints of the hands and feet, transient maculopapular rashes, myalgia, and arthralgia. The clinical symptoms resembled those of the more ubiquitous classical dengue fever; this posed an initial challenge in diagnosing the disease since dengue virus is endemic in the country.79
Chikungunya virus (chikungunya, from the root verb kungunyala that means ‘to dry up or become contorted’ in Makonde language in Tanzania80) is related to group A arboviruses. CHIKV is an Alphavirus from the Togaviridae family that shares the same vectors responsible for spreading dengue virus, namely Aedes aegypti and, to a lesser extent, Aedes albopictus, which are the common peridomestic mosquito species in the Southeast Asia region. Studies conducted in the 1970s detected antibody against CHIKV among the rural populations in Malaysia, indicating the presence of CHIKV infection.81, 82 However, until recently, outbreaks causing human diseases have not been reported.
Seven years after its first appearance, new CHIKV infections re-emerged in Bagan Panchor (about 50 km from Ipoh), Perak between March and April 2006.83, 84 More than 200 villagers in a fishing community were infected with CHIKV strains derived from a common ancestral lineage from the 1998/99 outbreak, but this recent outbreak had a notably higher number and rate of infections. This outbreak coincided with the largest ever CHIKV epidemics affecting the Indian Ocean territories between 2005 and 2006, where in Reunion alone more than 266 000 people, about a third of the total population, were infected. In India, an estimated 1.4 million human cases were reported during 2006. In these outbreaks, a substantial proportion of patients also showed unusual clinical manifestations, including severe neurological symptoms and fulminant hepatitis.85, 86 Although unclear, plausible explanations for the re-emergence of CHIKV in this region include tourism and migration labor (Malaysia is greatly dependent on migrant workers from neighboring countries where CHIKV is endemic78), viral mutation, and CHIKV introduction into a naïve population.87 Phylogenetic evidence has shown that the contemporary Malaysian strains isolated in 2006 were, however, distinct from the epidemic strains reported in the Indian subcontinent (2005–2006), suggesting that CHIKV is indeed endemic in Malaysia.83 Since the concurrent re-emergence of CHIKV in the Indian Ocean region and Malaysia seem to be unrelated, it is possible that other factors could have played an important role in driving these outbreaks. Climate anomalies, for instance, may have favored the mosquito vectors and consequently facilitated CHIKV emergence in these areas.88, 89
Pulau virus and Melaka virus
During the search for NiV in fruit bats on Tioman Island in 1999, another novel virus, initially thought to be a bat paramyxovirus, was identified. While serological tests excluded the presence of a paramyxovirus, further electron microscopic, serologic, and phylogenetic investigations established the fusogenic agent as a reovirus.90 Designated as Pulau virus (PulV) (pulau denotes ‘island’ in the Malay language), PulV is a dsRNA virus displaying the typical ultrastructural morphology of a reovirus. PulV formed large syncytium in Vero cells and showed serologic reactivity against Nelson Bay virus (NBV), another known bat Orthoreovirus isolated from the Australian flying foxes (Pteropus alecto).91 To date, PulV has not been associated with any human diseases, and very little is known about the host range, pathogenesis, and epidemiology of this newly recognized virus.
More recently in 2006, another novel Orthoreovirus named Melaka virus (MelV) associated with acute respiratory disease in the human was identified.92 MelV was isolated from an adult male who developed a high fever and acute respiratory symptoms. Icosahedral viruses similar to those of the Orthoreovirus genus were noted on microscopic examination of mammalian cell lines infected with MelV, and serological studies of the patient serum showed neutralization activity against PulV. Nucleotide analysis of the small (S) segments revealed a close genetic relationship of MelV to PulV and NBV, and clustering within the Orthoreovirus genus subgroup III of the Reoviridae family. In the meantime, two adolescent children of the index patient also developed fever (without respiratory symptoms) approximately 6 days after the onset of his illness. Interestingly, epidemiological investigations of the index case revealed that about one week before he developed the illness, he had a bizarre exposure to a bat that flew into his living room for a short period. Subsequently, antibodies against MelV were detected from the family members including his wife who was asymptomatic. Although direct evidence of bat-to-human transmission of MelV has not been documented, the role of the bat as a possible reservoir of MelV has not been ruled out. MelV is believed to be the first Orthoreovirus associated with acute respiratory disease in the human.92
HIV type 1 (clade CRF33_01B)
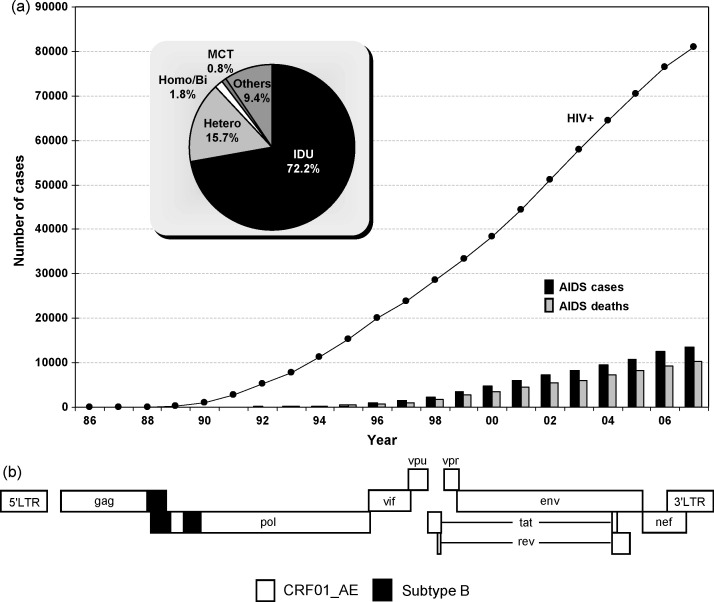
Since the first cases of AIDS reported in 1986,93 the rise in HIV/AIDS in Malaysia has continued unabated. As of December 2007, a total of 80 938 HIV type 1 (HIV-1) infections have been identified, while 10 334 people have died of AIDS-related illnesses nationwide. Of these, 72% were injecting drug users (IDUs), followed by 16% transmission via heterosexual route (Figure 3a). It has been suggested that the early epidemic was a spillover from Thailand, located at Malaysia's northern border. Malaysia is currently defined as a country with a ‘concentrated’ HIV-1 epidemic, based on relatively low rates of infection in the general population as measured by a prevalence of less than 0.1% among women attending government antenatal clinics, and seemingly isolated high prevalence rates among high-risk groups such as IDUs and female sex workers. In 2003 it was reported that Malaysia had the fifth fastest growing HIV infection rate in the Asia Pacific region, with the infection rate doubling every three years (http://www.unicef.org/aids/).
Figure 3.
(a) Cumulative numbers of HIV-1 infections, AIDS cases, and AIDS-related deaths reported by the Ministry of Health in Malaysia (1986–2007). Inset: Distribution of HIV-1 infections in different risk categories. Abbreviations: IDU, injecting drug user; Hetero, heterosexual; Homo/Bi, male homo-/bisexual; MCT, mother-to-child transmission. (b) Structural representation of the novel HIV-1 CRF33_01B identified in Malaysia. Full-length genetic sequence revealed short subtype B fragments are recombined into the gag and pol gene in the backbone of CRF01_AE. The recombinant structures of all HIV-1 CRFs are available at the HIV Sequence Database, Los Alamos National Library.98
HIV-1 exhibits tremendous genetic diversity that is driven by high rates of mutation and recombination, coupled with high viral turnover and the persistent nature of infection.94, 95, 96, 97 By these mechanisms, HIV-1 group M, which is largely responsible for the global pandemic, diversified into 11 subtypes and subsubtypes (A1, A2, B, C, D, F1, F2, G, H, J, and K) and various types of recombinants.98, 99 HIV-1 recombinants with epidemic spread are known as circulating recombinant forms (CRFs). Five strains of CRFs have been reported so far in Asia: CRF01_AE, CRF15_01B, and CRF34_01B in Thailand and CRF07_BC and CRF08_BC in China. In addition to CRFs, various types of unique recombinant forms (URFs) that are detected in a single individual or a single epidemiologically-linked cluster have been identified in the region, where multiple lineages of HIV-1 strains co-circulate in the same population.
The evolution of the HIV-1 epidemic in Malaysia produced a unique lineage when a distinctive recombinant strain emerged in 2003.100 Phylogenetic analyses of the HIV-1 protease and reverse transcriptase genes found 19% CRF01_AE/B intersubtype recombinants (a recombinant involving CRF01_AE and subtype B of Thai origin) amongst antiretroviral-naïve patients in Kuala Lumpur, all having a recombination profile different from other previously described CRFs. Designated as HIV-1 CRF33_01B from near full-length genome analyses (Figure 3b), this novel CRF was disseminating at a significant proportion among various high-risk populations, especially among the IDUs. Wide distribution of CRF33_01B involving all major ethnic and risk groups has provided evidence that extensive bridging of HIV-1 transmission between different risk groups has occurred in Malaysia.101, 102
We recently observed a unique parallelism of the transition in molecular epidemiological features of HIV-1 epidemics between Thailand and Malaysia.101 In the early phase of the Thai epidemic, two HIV-1 strains, CRF01_AE and subtype B, were circulating relatively independently among different risk populations. CRF01_AE was distributed among persons at risk of sexual exposure, while subtype B was distributed mainly among IDUs.103, 104 Co-circulation of CRF01_AE and subtype B in Thailand presented opportunities for inter-clade recombination to take place (a common feature for HIV-1), and has led to the generation of various forms of CRF01_AE/B recombinants.105, 106, 107 A similar molecular epidemiological trend has been observed in Malaysia. Studies conducted in 1992–1997 showed that CRF01_AE and subtype B were prevalent among 81% of heterosexuals and 55–92% of IDUs, respectively.108, 109, 110 However, recent studies have documented the gradual dilution of non-recombinant pure subtypes and the establishment of CRF33_01B as the emerging epidemic strain in Malaysia.101 Besides expanding rapidly within the country,111 further molecular epidemiological surveillance has shown that CRF33_01B spread across the border to Singapore in 2005 (Paton NI and Sun YJ, personal communication). Such genetic complexity and dynamicity of HIV-1 provides opportunities for new recombinants to develop and spread within Malaysia and also in the region, thus presenting new challenges to disease diagnosis and treatment, particularly in the development of antivirals and vaccine candidates.
Highly pathogenic avian influenza (H5N1)
The highly pathogenic avian influenza (HPAI) H5N1 virus that originated in southern China in the mid-1990s,112 was responsible for large disease outbreaks in poultry in China and other countries in the region in 2003–2004. Affected countries faced severe economic loss due to mortality in poultry and the loss of domestic and international trade of poultry and its products. Widespread circulation among avian populations and the significant number of human infections and deaths caused by HPAI H5N1 (as of June 19, 2008, 385 human cases including 243 deaths have been reported; www.who.int/csr/disease/avian_influenza/country/en) have raised concern over the plausible genetic mutation event (genetic reassortment) that could lead to the generation of an influenza strain with enhanced transmissibility among humans, possibly triggering a pandemic.113
In Malaysia, the first ever outbreak of HPAI caused by subtype H5N1 was reported in August 2004 in a village in the state of Kelantan located approximately 22 km from the Thai border in northeastern Peninsular Malaysia.114, 115 The virus, discovered in fighting cocks smuggled from a neighboring country, was transmitted mainly among the local village chickens. Molecular analysis showed that the H5N1 strain was highly homologous to the H5N1 strains previously isolated from Thailand and Vietnam. A few weeks following the first outbreak, eight other outbreaks were reported, largely affecting poultry in villages located around the index case. In these outbreaks, no human cases or deaths were reported and the disease was brought under control by depopulation and quarantine/clinical surveillance of poultry and birds within a 1-km and 10-km radius of the index case, respectively, coupled with restrictions on the movement of birds and their products to other states.115
In February 2006, fresh outbreaks of HPAI H5N1 emerged over a wider geographical area involving villages in Kuala Lumpur and the states of Perak and Pulau Pinang along the more industrialized western coast of Peninsular Malaysia.115 Phylogenetic analysis of the H5 and PB2 genes revealed that the H5N1 strain isolated from infected village chickens, ducks, and quails was different from that of the 2004 outbreak and was highly similar to the H5N1 isolates from Indonesia and China, suggesting different H5N1 lineages were introduced into the country, possibly by the poultry trade rather than through migratory birds.116 Although these outbreaks were brought under control through effective disease control and preventive efforts, including the culling of about 60 000 birds, a similar outbreak re-occurred in another village in Selangor state not far from Kuala Lumpur in June 2007.115 Through effective control measures, the 2007 outbreak was resolved several months later.
In Malaysia, cock fighting is a popular albeit illegal activity among village folks. Fighting cocks smuggled from neighboring countries (i.e., Thailand and Indonesia) have been implicated in the introduction and spread of HPAI H5N1 in Peninsular Malaysia. Such public health threats – that increase the risk of infection in humans – could be avoided by implementing a stricter ban by the authorities on cock fighting and smuggling activities in the country. In addition, continued surveillance of avian populations including domestic ducks (thought to be the potential reservoir and source of H5N1 persistence117) is important to counter possible re-occurrence or re-introduction of HPAI H5N1, a phenomenon that is not uncommon in the Southeast Asia region.118
Discussion
Over the last eleven years, between 1997 and 2007, Malaysia has witnessed the unprecedented appearance of eight novel viruses that have never been documented in the country before (Table 1 ). The majority of these viruses, such as EV-71, NiV, CHIKV, and HIV-1 recombinant, have caused serious human infections and/or deaths of varying magnitudes and are of epidemiological importance, whereas others have yet to be known to cause widespread human diseases (e.g., MelV and HPAI H5N1) or cross into a wider range of susceptible hosts (e.g., TiV and PulV). Factors leading to this emergence are not entirely understood but various features associated with such a trend – including socio-economic, environmental, and ecological factors3, 4, 5, 6 – have been hypothesized.
Table 1.
Emerging and re-emerging viruses in Malaysia, 1997–2007.
| Virus | Family | Genus | Properties | Year of emergence | Locations in Malaysia | Remarks |
|---|---|---|---|---|---|---|
| Enterovirus 71 | Picornaviridae | Enterovirus | +ssRNA, non-enveloped | 1997, 2000, 2003 | Sibu, Sarawak; Peninsular Malaysia | Fatal cases of brainstem encephalitis reported |
| Novel subgenotypes B3, B4, and B5 emerged | ||||||
| Recombinant involving coxsackievirus and other human enteroviruses identified | ||||||
| Chikungunya virus | Togaviridae | Alphavirus | +ssRNA, enveloped | 1998 | Port Klang, Kuala Lumpur | Sporadic outbreak causing febrile illness with polyarthritis |
| 2006 | Bagan Panchor, Perak | Endemic virus re-emerged 7 years later | ||||
| Aedes aegypti as vector | ||||||
| Nipah virus | Paramyxoviridae | Henipavirus | −ssRNA, enveloped | 1998 | Ipoh, Perak; Seremban, Negeri Sembilan | Novel bat paramyxovirus, closely related to Hendra virus |
| Febrile illness and encephalitis with high mortality rate | ||||||
| Acquired via close contact with infected pigs | ||||||
| Tioman virus | Paramyxoviridae | Rubulavirus | −ssRNA, enveloped | 1999 | Tioman Island | Novel bat paramyxovirus, closely related to Menangle virus |
| Human infections and diseases in experimentally infected animals have been reported | ||||||
| Pulau virus | Reoviridae | Orthoreovirus | dsRNA, non-enveloped | 1999 | Tioman Island | Novel bat Orthoreovirus |
| No human/animal disease reported | ||||||
| HIV type 1 (clade CRF33_01B) | Retroviridae | Lentivirus | Reverse-transcribing ssRNA, enveloped | 2003 | Kuala Lumpur | Novel recombinant descended from subtypes B and CRF01_AE |
| Widespread among all major risk groups | ||||||
| Highly pathogenic avian influenza H5N1 | Orthomyxoviridae | Influenzavirus A | −ssRNA, enveloped | 2004 | Kelantan | Outbreaks confined to poultry and have been linked to fighting cocks smuggled from neighboring countries |
| 2006 | Kuala Lumpur; Perak; Pulau Pinang | 60 000 birds culled to control outbreak | ||||
| 2007 | Kuala Lumpur | |||||
| Melaka virus | Reoviridae | Orthoreovirus | dsRNA, non-enveloped | 2006 | Melaka | Novel bat Orthoreovirus associated with acute respiratory disease in the human |
Unlike enterovirus infections that usually occur in densely populated areas, where hygiene levels are poor and food or water supplies may be contaminated, conditions that favor the fecal–oral route of transmission, more complex attributes, be it of the environment, viral hosts/vectors, or humans, have been associated with the emergence of the other novel viruses in Malaysia. For instance, early studies implicated the effects of the El Niño/Southern Oscillation (ENSO) phenomenon in 1997/98 in the emergence of NiV.119 Directly preceding these outbreaks, Malaysia experienced a severe drought resulting from the El Niño conditions (the largest and warmest to develop in the Pacific Ocean in the past century). The situation was aggravated by the excessive haze produced by the aggressive slash-and-burn deforestation activities in Indonesia. This series of environmental and human events may have affected the natural habitat of the pteropid bats, forcing their migration and subsequent encroachment into fruit orchards surrounding the pig-farming area, resulting in the unanticipated introduction of NiV from its natural host to pigs as the amplifying host. Recent investigations, however, refuted the effect of ENSO and showed evidence that NiV is frequently present in fruit bats in Malaysia, and that its spillover – from bats to pigs and subsequent transmission to human – was largely a chance event that might have occurred as a result of increased habitat encroachment and agricultural expansion by humans, confounded by the temporal and spatial dynamicity of both the virus and hosts, and the hosts (pigs) immunity against NiV infection.119, 120, 121 In fact, similar anthropogenic drivers have been linked to outbreaks in Malaysia, Bangladesh, and India, raising concerns that these countries, which are currently experiencing promising economic growth, are still at risk of NiV re-occurrence should unrestrained deforestation and agricultural intensification activities not be closely regulated.
Overlapping the NiV epidemic was the first sporadic outbreak of Aedes mosquito-borne CHIKV infections in Kuala Lumpur in 1998. The arbovirus then re-emerged seven years later in northern Malaysia, coinciding with the drought-associated CHIKV outbreaks affecting countries cresting the Indian Ocean,88 by far the largest CHIKV epidemic on record. The cause of the disease outbreaks remains multifactorial. Previous lessons have suggested that increased tourism, viral adaptation, and host immunity,87 plus importation of migrant workers from countries where CHIKV is endemic,78 may play a substantial role in the spread of the virus to humans, although the effect of a warmer climate has also been reported.88 As a whole, such a climate abnormality of prolonged drier-than-average conditions may be critical in introducing new viruses into the country, although more research is certainly needed to validate this relationship.122
The discovery of bat-associated NiV (a Henipavirus), TiV (Rubulavirus), and PulV and MelV (both within the Orthoreovirus genus) has highlighted the significant role that bats play as important reservoir hosts of emerging viruses.123, 124 Although yet to cause severe, widespread human outbreaks, medical and research institutions should adopt a proactive approach in understanding and managing the potential threats posed by these viruses. This includes conducting large-scale surveillance to determine the prevalence, both in bats and humans of these viruses (as in Bangladesh, for example, during the recent NiV outbreaks62, 68, 69), establishing diagnostic systems in public health laboratories that include the diagnosis of these viruses, and reviewing the traditional/medicinal practice of drinking fresh bat blood or eating improperly cooked bat products among certain rural communities.125
HIV is among the most genetically diverse human pathogens. In addition, co-circulation of two or more HIV-1 subtypes in any population can lead to co-infection in individuals and consequently generate recombinant strains,106, 107, 126 as occurred with clade CRF33_01B in Malaysia, a fact that further increases the genetic plasticity of HIV-1. The possible phenotypic advantage inherited from recombination among different HIV-1 clades remains uncertain. However, it has been reported that HIV recombinants may have enhanced replicative capacity and transmissibility or higher risk of disease progression compared to its parental strains,127, 128 as reflected by the high prevalence of such recombinants in particular populations with risk practices. Further genetic diversification of HIV-1, which will add further to the problems in the development of antivirals and vaccines, could be reduced by limiting the incidence of infections among the high-risk groups and among those who are already infected.
As Malaysia progresses towards becoming a developed country in the new millennium, a number of zoonotic, non-zoonotic, and vector-borne viruses have been reported for the first time in the country. Although a decade has past, the potential health threats faced by the population are far from over. In fact, the momentum with which these diseases are spreading has intensified over time, as seen by the exponential increase in the annual HIV/AIDS incidence in Malaysia and elsewhere in the world, the temporal persistence of EV-71 infections, the sporadic expansion of CHIKV worldwide, the broad regional distribution and aggressive NiV outbreaks in Bangladesh and India, and the re-occurrence of highly pathogenic H5N1 avian influenza in poultry and humans. Taken together, indispensable lessons learnt from the past plus current understanding of the probable circumstances leading to disease emergence suggest calls for better preparedness to deal with impending infectious disease risks.
Acknowledgements
We would like to acknowledge Kaw Bing Chua, Sai Kit Lam, and colleagues for their inspiring work which led to the discovery and identification of many of the viruses reviewed in this article. We also thank Timothy D. Mastro for critical reading of the article and the anonymous reviewers for constructive comments and suggestions.
A.K. and Y.T. received financial support from the Ministry of Science, Technology and Innovation, Malaysia (eScienceFund 02-01-03-SF0379) and the Ministry of Health, Labour and Welfare, Japan (H18-AIDS-General-016), respectively.
Conflict of interest: No conflict of interest to declare.
Corresponding Editor: Jane Zuckerman, London, UK
References
- 1.Mackenzie J.S., Chua K.B., Daniels P.W., Eaton B.T., Field H.E., Hall R.A. Emerging viral diseases of Southeast Asia and the Western Pacific. Emerg Infect Dis. 2001;7:497–504. doi: 10.3201/eid0707.017703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D., Gittleman J.L. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daszak P., Cunningham A.A., Hyatt A.D. Anthropogenic environmental change and the emergence of infectious diseases in wildlife. Acta Trop. 2001;78:103–116. doi: 10.1016/s0001-706x(00)00179-0. [DOI] [PubMed] [Google Scholar]
- 4.Morens D.M., Folkers G.K., Fauci A.S. The challenge of emerging and re-emerging infectious diseases. Nature. 2004;430:242–249. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss R.A., McMichael A.J. Social and environmental risk factors in the emergence of infectious diseases. Nat Med. 2004;10:S70–S76. doi: 10.1038/nm1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woolhouse M.E., Gowtage-Sequeria S. Host range and emerging and reemerging pathogens. Emerg Infect Dis. 2005;11:1842–1847. doi: 10.3201/eid1112.050997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AbuBakar S., Chee H.Y., Al-Kobaisi M.F., Xiaoshan J., Chua K.B., Lam S.K. Identification of enterovirus 71 isolates from an outbreak of hand, foot and mouth disease (HFMD) with fatal cases of encephalomyelitis in Malaysia. Virus Res. 1999;61:1–9. doi: 10.1016/s0168-1702(99)00019-2. [DOI] [PubMed] [Google Scholar]
- 8.Abubakar S., Chee H.Y., Shafee N., Chua K.B., Lam S.K. Molecular detection of enteroviruses from an outbreak of hand, foot and mouth disease in Malaysia in 1997. Scand J Infect Dis. 1999;31:331–335. doi: 10.1080/00365549950163734. [DOI] [PubMed] [Google Scholar]
- 9.Cardosa M.J., Krishnan S., Tio P.H., Perera D., Wong S.C. Isolation of subgenus B adenovirus during a fatal outbreak of enterovirus 71-associated hand, foot, and mouth disease in Sibu, Sarawak. Lancet. 1999;354:987–991. doi: 10.1016/S0140-6736(98)11032-2. [DOI] [PubMed] [Google Scholar]
- 10.Chan L.G., Parashar U.D., Lye M.S., Ong F.G., Zaki S.R., Alexander J.P. Deaths of children during an outbreak of hand, foot, and mouth disease in Sarawak, Malaysia: clinical and pathological characteristics of the disease. For the Outbreak Study Group. Clin Infect Dis. 2000;31:678–683. doi: 10.1086/314032. [DOI] [PubMed] [Google Scholar]
- 11.Lum L.C., Wong K.T., Lam S.K., Chua K.B., Goh A.Y., Lim W.L. Fatal enterovirus 71 encephalomyelitis. J Pediatr. 1998;133:795–798. doi: 10.1016/s0022-3476(98)70155-6. [DOI] [PubMed] [Google Scholar]
- 12.Cardosa M.J., Perera D., Brown B.A., Cheon D., Chan H.M., Chan K.P. Molecular epidemiology of human enterovirus 71 strains and recent outbreaks in the Asia-Pacific region: comparative analysis of the VP1 and VP4 genes. Emerg Infect Dis. 2003;9:461–468. doi: 10.3201/eid0904.020395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herrero L.J., Lee C.S., Hurrelbrink R.J., Chua B.H., Chua K.B., McMinn P.C. Molecular epidemiology of enterovirus 71 in peninsular Malaysia, 1997–2000. Arch Virol. 2003;148:1369–1385. doi: 10.1007/s00705-003-0100-2. [DOI] [PubMed] [Google Scholar]
- 14.McMinn P., Lindsay K., Perera D., Chan H.M., Chan K.P., Cardosa M.J. Phylogenetic analysis of enterovirus 71 strains isolated during linked epidemics in Malaysia, Singapore, and Western Australia. J Virol. 2001;75:7732–7738. doi: 10.1128/JVI.75.16.7732-7738.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Podin Y., Gias E.L., Ong F., Leong Y.W., Yee S.F., Yusof M.A. Sentinel surveillance for human enterovirus 71 in Sarawak, Malaysia: lessons from the first 7 years. BMC Public Health. 2006;6:180. doi: 10.1186/1471-2458-6-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ooi M.H., Wong S.C., Podin Y., Akin W., del Sel S., Mohan A. Human enterovirus 71 disease in Sarawak, Malaysia: a prospective clinical, virological, and molecular epidemiological study. Clin Infect Dis. 2007;44:646–656. doi: 10.1086/511073. [DOI] [PubMed] [Google Scholar]
- 17.Chan Y.F., AbuBaker S. Recombinant human enterovirus 71 in hand, foot and mouth disease patients. Emerg Infect Dis. 2004;10:1468–1470. doi: 10.3201/eid1008.040059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoke-Fun C., AbuBakar S. Phylogenetic evidence for inter-typic recombination in the emergence of human enterovirus 71 subgenotypes. BMC Microbiol. 2006;6:74. doi: 10.1186/1471-2180-6-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ho M., Chen E.R., Hsu K.H., Twu S.J., Chen K.T., Tsai S.F. An epidemic of enterovirus 71 infection in Taiwan. Taiwan Enterovirus Epidemic Working Group. N Engl J Med. 1999;341:929–935. doi: 10.1056/NEJM199909233411301. [DOI] [PubMed] [Google Scholar]
- 20.McMinn P., Stratov I., Nagarajan L., Davis S. Neurological manifestations of enterovirus 71 infection in children during an outbreak of hand, foot, and mouth disease in Western Australia. Clin Infect Dis. 2001;32:236–242. doi: 10.1086/318454. [DOI] [PubMed] [Google Scholar]
- 21.Singh S., Chow V.T., Chan K.P., Ling A.E., Poh C.L. RT-PCR, nucleotide, amino acid and phylogenetic analyses of enterovirus type 71 strains from Asia. J Virol Methods. 2000;88:193–204. doi: 10.1016/s0166-0934(00)00185-3. [DOI] [PubMed] [Google Scholar]
- 22.Chan K.P., Goh K.T., Chong C.Y., Teo E.S., Lau G., Ling A.E. Epidemic hand, foot and mouth disease caused by human enterovirus 71, Singapore. Emerg Infect Dis. 2003;9:78–85. doi: 10.3201/eid1301.020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komatsu H., Shimizu Y., Takeuchi Y., Ishiko H., Takada H. Outbreak of severe neurologic involvement associated with enterovirus 71 infection. Pediatr Neurol. 1999;20:17–23. doi: 10.1016/s0887-8994(98)00087-3. [DOI] [PubMed] [Google Scholar]
- 24.Wang J.R., Tuan Y.C., Tsai H.P., Yan J.J., Liu C.C., Su I.J. Change of major genotype of enterovirus 71 in outbreaks of hand-foot-and-mouth disease in Taiwan between 1998 and 2000. J Clin Microbiol. 2002;40:10–15. doi: 10.1128/JCM.40.1.10-15.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tu P.V., Thao N.T., Perera D., Khanh T.H., Tien N.T., Thuong T.C. Epidemiologic and virologic investigation of hand, food, and mouth disease, southern Vietnam, 2005. Emerg Infect Dis. 2007;13:1733–1741. doi: 10.3201/eid1311.070632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chinese Center for Disease Control and Prevention, Office of the World Health Organization in China. Report on the hand, foot and mouth disease outbreak in Fuyang city, Anhui province and the prevention and control in China. China CDC/WHO; 2008.
- 27.Pallansch M.A., Roos R.P. Enteroviruses: polioviruses, coxsackieviruses, echoviruses, and newer enteroviruses. In: Knipe D.M., Howley P.M., Griffin D.E., Lamb R.A., Martin M.A., Roizman B., editors. Fields virology. 4th ed. Lippincott Williams and Wilkins; Philadelphia: 2001. pp. 723–776. [Google Scholar]
- 28.Ooi M.H., Wong S.C., Clear D., Perera D., Krishnan S., Preston T. Adenovirus type 21-associated acute flaccid paralysis during an outbreak of hand-foot-and-mouth disease in Sarawak, Malaysia. Clin Infect Dis. 2003;36:550–559. doi: 10.1086/367648. [DOI] [PubMed] [Google Scholar]
- 29.Lum L.C., Chua K.B., McMinn P.C., Goh A.Y., Muridan R., Sarji S.A. Echovirus 7 associated encephalomyelitis. J Clin Virol. 2002;23:153–160. doi: 10.1016/s1386-6532(01)00214-1. [DOI] [PubMed] [Google Scholar]
- 30.Shimizu H., Utama A., Onnimala N., Li C., Li-Bi Z., Yu-Jie M. Molecular epidemiology of enterovirus 71 infection in the Western Pacific Region. Pediatr Int. 2004;46:231–235. doi: 10.1046/j.1442-200x.2004.01868.x. [DOI] [PubMed] [Google Scholar]
- 31.Mohd Nor M.N., Gan C.H., Ong B.L. Nipah virus infection of pigs in peninsular Malaysia. Rev Sci Tech. 2000;19:160–165. doi: 10.20506/rst.19.1.1202. [DOI] [PubMed] [Google Scholar]
- 32.Anonymous Outbreak of Hendra-like virus—Malaysia and Singapore, 1998–1999. MMWR Morb Mortal Wkly Rep. 1999;48:265–269. [PubMed] [Google Scholar]
- 33.Anonymous Update: outbreak of Nipah virus—Malaysia and Singapore, 1999. MMWR Morb Mortal Wkly Rep. 1999;48:335–337. [PubMed] [Google Scholar]
- 34.Chua K.B., Goh K.J., Wong K.T., Kamarulzaman A., Tan P.S., Ksiazek T.G. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet. 1999;354:1257–1259. doi: 10.1016/S0140-6736(99)04299-3. [DOI] [PubMed] [Google Scholar]
- 35.Cardosa M.J., Hooi T.P., Kaur P. Japanese encephalitis virus is an important cause of encephalitis among children in Penang. Southeast Asian J Trop Med Public Health. 1995;26:272–275. [PubMed] [Google Scholar]
- 36.Chong H.T., Kunjapan S.R., Thayaparan T., Tong J., Petharunam V., Jusoh M.R. Nipah encephalitis outbreak in Malaysia, clinical features in patients from Seremban. Can J Neurol Sci. 2002;29:83–87. doi: 10.1017/s0317167100001785. [DOI] [PubMed] [Google Scholar]
- 37.Goh K.J., Tan C.T., Chew N.K., Tan P.S., Kamarulzaman A., Sarji S.A. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med. 2000;342:1229–1235. doi: 10.1056/NEJM200004273421701. [DOI] [PubMed] [Google Scholar]
- 38.Wong K.T., Shieh W.J., Zaki S.R., Tan C.T. Nipah virus infection, an emerging paramyxoviral zoonosis. Springer Semin Immunopathol. 2002;24:215–228. doi: 10.1007/s00281-002-0106-y. [DOI] [PubMed] [Google Scholar]
- 39.Paton N.I., Leo Y.S., Zaki S.R., Auchus A.P., Lee K.E., Ling A.E. Outbreak of Nipah-virus infection among abattoir workers in Singapore. Lancet. 1999;354:1253–1256. doi: 10.1016/S0140-6736(99)04379-2. [DOI] [PubMed] [Google Scholar]
- 40.Chua K.B., Bellini W.J., Rota P.A., Harcourt B.H., Tamin A., Lam S.K. Nipah virus: a recently emergent deadly paramyxovirus. Science. 2000;288:1432–1435. doi: 10.1126/science.288.5470.1432. [DOI] [PubMed] [Google Scholar]
- 41.Chew M.H., Arguin P.M., Shay D.K., Goh K.T., Rollin P.E., Shieh W.J. Risk factors for Nipah virus infection among abattoir workers in Singapore. J Infect Dis. 2000;181:1760–1763. doi: 10.1086/315443. [DOI] [PubMed] [Google Scholar]
- 42.Parashar U.D., Sunn L.M., Ong F., Mounts A.W., Arif M.T., Ksiazek T.G. Case–control study of risk factors for human infection with a new zoonotic paramyxovirus, Nipah virus, during a 1998–1999 outbreak of severe encephalitis in Malaysia. J Infect Dis. 2000;181:1755–1759. doi: 10.1086/315457. [DOI] [PubMed] [Google Scholar]
- 43.Tan C.T., Tan K.S. Nosocomial transmissibility of Nipah virus. J Infect Dis. 2001;184:1367. doi: 10.1086/323996. [DOI] [PubMed] [Google Scholar]
- 44.Mounts A.W., Kaur H., Parashar U.D., Ksiazek T.G., Cannon D., Arokiasamy J.T. A cohort study of health care workers to assess nosocomial transmissibility of Nipah virus, Malaysia, 1999. J Infect Dis. 2001;183:810–813. doi: 10.1086/318822. [DOI] [PubMed] [Google Scholar]
- 45.Chua K.B. Nipah virus outbreak in Malaysia. J Clin Virol. 2003;26:265–275. doi: 10.1016/s1386-6532(02)00268-8. [DOI] [PubMed] [Google Scholar]
- 46.Murray K., Selleck P., Hooper P., Hyatt A., Gould A., Gleeson L. A morbillivirus that caused fatal disease in horses and humans. Science. 1995;268:94–97. doi: 10.1126/science.7701348. [DOI] [PubMed] [Google Scholar]
- 47.Chan Y.P., Chua K.B., Koh C.L., Lim M.E., Lam S.K. Complete nucleotide sequences of Nipah virus isolates from Malaysia. J Gen Virol. 2001;82:2151–2155. doi: 10.1099/0022-1317-82-9-2151. [DOI] [PubMed] [Google Scholar]
- 48.Harcourt B.H., Tamin A., Ksiazek T.G., Rollin P.E., Anderson L.J., Bellini W.J. Molecular characterization of Nipah virus, a newly emergent paramyxovirus. Virology. 2000;271:334–349. doi: 10.1006/viro.2000.0340. [DOI] [PubMed] [Google Scholar]
- 49.Wang L., Harcourt B.H., Yu M., Tamin A., Rota P.A., Bellini W.J. Molecular biology of Hendra and Nipah viruses. Microbes Infect. 2001;3:279–287. doi: 10.1016/s1286-4579(01)01381-8. [DOI] [PubMed] [Google Scholar]
- 50.Wang L.F., Yu M., Hansson E., Pritchard L.I., Shiell B., Michalski W.P. The exceptionally large genome of Hendra virus: support for creation of a new genus within the family Paramyxoviridae. J Virol. 2000;74:9972–9979. doi: 10.1128/jvi.74.21.9972-9979.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Halpin K., Young P.L., Field H.E., Mackenzie J.S. Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. J Gen Virol. 2000;81:1927–1932. doi: 10.1099/0022-1317-81-8-1927. [DOI] [PubMed] [Google Scholar]
- 52.Young P.L., Halpin K., Selleck P.W., Field H., Gravel J.L., Kelly M.A. Serologic evidence for the presence in Pteropus bats of a paramyxovirus related to equine morbillivirus. Emerg Infect Dis. 1996;2:239–240. doi: 10.3201/eid0203.960315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yob J.M., Field H., Rashdi A.M., Morrissy C., van der Heide B., Rota P. Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg Infect Dis. 2001;7:439–441. doi: 10.3201/eid0703.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shirai J., Sohayati A.L., Daszak P., Epstein J.H., Field H.E., Abdul Aziz J. Nipah virus survey of flying foxes in Malaysia. JARQ-Jpn Agr Res Q. 2007;41:69–78. [Google Scholar]
- 55.Chua K.B. A novel approach for collecting samples from fruit bats for isolation of infectious agents. Microbes Infect. 2003;5:487–490. doi: 10.1016/s1286-4579(03)00067-4. [DOI] [PubMed] [Google Scholar]
- 56.Chua K.B., Koh C.L., Hooi P.S., Wee K.F., Khong J.H., Chua B.H. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect. 2002;4:145–151. doi: 10.1016/s1286-4579(01)01522-2. [DOI] [PubMed] [Google Scholar]
- 57.Wacharapluesadee S., Lumlertdacha B., Boongird K., Wanghongsa S., Chanhome L., Rollin P. Bat Nipah virus, Thailand. Emerg Infect Dis. 2005;11:1949–1951. doi: 10.3201/eid1112.050613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sendow I., Field H.E., Curran J., Darminto, Morrissy C., Meehan G. Henipavirus in Pteropus vampyrus bats, Indonesia. Emerg Infect Dis. 2006;12:711–712. doi: 10.3201/eid1204.051181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Olson J.G., Rupprecht C., Rollin P.E., An U.S., Niezgoda M., Clemins T. Antibodies to Nipah-like virus in bats (Pteropus lylei), Cambodia. Emerg Infect Dis. 2002;8:987–988. doi: 10.3201/eid0809.010515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reynes J.M., Counor D., Ong S., Faure C., Seng V., Molia S. Nipah virus in Lyle's flying foxes, Cambodia. Emerg Infect Dis. 2005;11:1042–1047. doi: 10.3201/eid1107.041350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anonymous Outbreaks of viral encephalitis due to Nipah/Hendra-like viruses, Western Bangladesh. Health Sci Bull. 2003;1:1–6. [Google Scholar]
- 62.Hsu V.P., Hossain M.J., Parashar U.D., Ali M.M., Ksiazek T.G., Kuzmin I. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Epstein J.H., Prakash V., Smith C.S., Daszak P., McLaughlin A.B., Meehan G. Henipavirus infection in fruit bats (Pteropus giganteus), India. Emerg Infect Dis. 2008;14:1309–1311. doi: 10.3201/eid1408.071492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lehle C., Razafitrimo G., Razainirina J., Andriaholinirina N., Goodman S.M., Faure C. Henipavirus and Tioman virus antibodies in pteropodid bats, Madagascar. Emerg Infect Dis. 2007;13:159–161. doi: 10.3201/eid1301.060791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hayman D.T., Suu-Ire R., Breed A.C., McEachern J.A., Wang L., Wood J.L. Evidence of Henipavirus infection in West African fruit bats. PLoS ONE. 2008;3:e2739. doi: 10.1371/journal.pone.0002739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Anonymous Person-to-person transmission of Nipah virus during outbreak in Faridpur District, 2004. Health Sci Bull. 2004;2:5–9. [Google Scholar]
- 67.Anonymous Nipah virus encephalitis outbreak over wide area of Western Bangladesh, 2004. Health Sci Bull. 2004;2:7–11. [Google Scholar]
- 68.Luby S.P., Rahman M., Hossain M.J., Blum L.S., Husain M.M., Gurley E. Foodborne transmission of Nipah virus, Bangladesh. Emerg Infect Dis. 2006;12:1888–1894. doi: 10.3201/eid1212.060732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gurley E.S., Montgomery J.M., Hossain M.J., Bell M., Azad A.K., Islam M.R. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg Infect Dis. 2007;13:1031–1037. doi: 10.3201/eid1307.061128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chadha M.S., Comer J.A., Lowe L., Rota P.A., Rollin P.E., Bellini W.J. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12:235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Daniels P., Ksiazek T., Eaton B.T. Laboratory diagnosis of Nipah and Hendra virus infections. Microbes Infect. 2001;3:289–295. doi: 10.1016/s1286-4579(01)01382-x. [DOI] [PubMed] [Google Scholar]
- 72.Chua K.B., Wang L.F., Lam S.K., Crameri G., Yu M., Wise T. Tioman virus, a novel paramyxovirus isolated from fruit bats in Malaysia. Virology. 2001;283:215–229. doi: 10.1006/viro.2000.0882. [DOI] [PubMed] [Google Scholar]
- 73.Chua K.B., Wang L.F., Lam S.K., Eaton B.T. Full length genome sequence of Tioman virus, a novel paramyxovirus in the genus Rubulavirus isolated from fruit bats in Malaysia. Arch Virol. 2002;147:1323–1348. doi: 10.1007/s00705-002-0815-5. [DOI] [PubMed] [Google Scholar]
- 74.Philbey A.W., Kirkland P.D., Ross A.D., Davis R.J., Gleeson A.B., Love R.J. An apparently new virus (family Paramyxoviridae) infectious for pigs, humans, and fruit bats. Emerg Infect Dis. 1998;4:269–271. doi: 10.3201/eid0402.980214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yaiw K.C., Crameri G., Wang L., Chong H.T., Chua K.B., Tan C.T. Serological evidence of possible human infection with Tioman virus, a newly described paramyxovirus of bat origin. J Infect Dis. 2007;196:884–886. doi: 10.1086/520817. [DOI] [PubMed] [Google Scholar]
- 76.Yaiw K.C., Ong K.C., Chua K.B., Bingham J., Wang L., Shamala D. Tioman virus infection in experimentally infected mouse brain and its association with apoptosis. J Virol Methods. 2007;143:140–146. doi: 10.1016/j.jviromet.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 77.Yaiw K.C., Bingham J., Crameri G., Mungall B., Hyatt A., Yu M. Tioman virus, a paramyxovirus of bat origin, causes mild disease in pigs and has a predilection for lymphoid tissues. J Virol. 2008;82:565–568. doi: 10.1128/JVI.01660-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lam S.K., Chua K.B., Hooi P.S., Rahimah M.A., Kumari S., Tharmaratnam M. Chikungunya infection—an emerging disease in Malaysia. Southeast Asian J Trop Med Public Health. 2001;32:447–451. [PubMed] [Google Scholar]
- 79.Hammon W.M., Rudnick A., Sather G.E. Viruses associated with epidemic hemorrhagic fevers of the Philippines and Thailand. Science. 1960;131:1102–1103. doi: 10.1126/science.131.3407.1102. [DOI] [PubMed] [Google Scholar]
- 80.Lumsden W.H. An epidemic of virus disease in Southern Province, Tanganyika Territory, in 1952–53. II. General description and epidemiology. Trans R Soc Trop Med Hyg. 1955;49:33–57. doi: 10.1016/0035-9203(55)90081-x. [DOI] [PubMed] [Google Scholar]
- 81.Bowen E.T., Simpson D.I., Platt G.S., Way H.J., Bright W.F., Day J. Arbovirus infections in Sarawak, October 1968–February 1970: human serological studies in a land Dyak village. Trans R Soc Trop Med Hyg. 1975;69:182–186. doi: 10.1016/0035-9203(75)90151-0. [DOI] [PubMed] [Google Scholar]
- 82.Marchette N.J., Rudnick A., Garcia R. Alphaviruses in Peninsular Malaysia: II. Serological evidence of human infection. Southeast Asian J Trop Med Public Health. 1980;11:14–23. [PubMed] [Google Scholar]
- 83.AbuBakar S., Sam I.C., Wong P.F., MatRahim N., Hooi P.S., Roslan N. Reemergence of endemic chikungunya, Malaysia. Emerg Infect Dis. 2007;13:147–149. doi: 10.3201/eid1301.060617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kumarasamy V., Prathapa S., Zuridah H., Chem Y.K., Norizah I., Chua K.B. Re-emergence of chikungunya virus in Malaysia. Med J Malaysia. 2006;61:221–225. [PubMed] [Google Scholar]
- 85.Paquet C., Quatresous I., Solet J.L., Sissoko D., Renault P., Pierre V. Chikungunya outbreak in Reunion: epidemiology and surveillance, 2005 to early January 2006. Euro Surveill. 2006;11:E060202.3. doi: 10.2807/esw.11.05.02891-en. [DOI] [PubMed] [Google Scholar]
- 86.Schuffenecker I., Iteman I., Michault A., Murri S., Frangeul L., Vaney M.C. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 2006;3:e263. doi: 10.1371/journal.pmed.0030263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pialoux G., Gauzere B.A., Jaureguiberry S., Strobel M. Chikungunya, an epidemic arbovirosis. Lancet Infect Dis. 2007;7:319–327. doi: 10.1016/S1473-3099(07)70107-X. [DOI] [PubMed] [Google Scholar]
- 88.Chretien J.P., Anyamba A., Bedno S.A., Breiman R.F., Sang R., Sergon K. Drought-associated chikungunya emergence along coastal East Africa. Am J Trop Med Hyg. 2007;76:405–407. [PubMed] [Google Scholar]
- 89.Patz J.A., Campbell-Lendrum D., Holloway T., Foley J.A. Impact of regional climate change on human health. Nature. 2005;438:310–317. doi: 10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- 90.Pritchard L.I., Chua K.B., Cummins D., Hyatt A., Crameri G., Eaton B.T. Pulau virus; a new member of the Nelson Bay Orthoreovirus species isolated from fruit bats in Malaysia. Arch Virol. 2006;151:229–239. doi: 10.1007/s00705-005-0644-4. [DOI] [PubMed] [Google Scholar]
- 91.Gard G., Compans R.W. Structure and cytopathic effects of Nelson Bay virus. J Virol. 1970;6:100–106. doi: 10.1128/jvi.6.1.100-106.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chua K.B., Crameri G., Hyatt A., Yu M., Tompang M.R., Rosli J. A previously unknown reovirus of bat origin is associated with an acute respiratory disease in humans. Proc Natl Acad Sci USA. 2007;104:11424–11429. doi: 10.1073/pnas.0701372104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Goh K.L., Chua C.T., Chiew I.S., Soo-Hoo T.S. The acquired immune deficiency syndrome: a report of the first case in Malaysia. Med J Malaysia. 1987;42:58–60. [PubMed] [Google Scholar]
- 94.Ho D.D., Neumann A.U., Perelson A.S., Chen W., Leonard J.M., Markowitz M. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. 1995;373:123–126. doi: 10.1038/373123a0. [DOI] [PubMed] [Google Scholar]
- 95.Mansky L.M. Forward mutation rate of human immunodeficiency virus type 1 in a T lymphoid cell line. AIDS Res Hum Retroviruses. 1996;12:307–314. doi: 10.1089/aid.1996.12.307. [DOI] [PubMed] [Google Scholar]
- 96.Perelson A.S., Neumann A.U., Markowitz M., Leonard J.M., Ho D.D. HIV-1 dynamics in vivo: virion clearance rate, infected cell life-span, and viral generation time. Science. 1996;271:1582–1586. doi: 10.1126/science.271.5255.1582. [DOI] [PubMed] [Google Scholar]
- 97.Robertson D.L., Sharp P.M., McCutchan F.E., Hahn B.H. Recombination in HIV-1. Nature. 1995;374:124–126. doi: 10.1038/374124b0. [DOI] [PubMed] [Google Scholar]
- 98.Los Alamos National Library. Los Alamos HIV Sequence Database. Available at: http://www.hiv.lanl.gov (accessed October 2008).
- 99.Taylor B.S., Sobieszczyk M.E., McCutchan F.E., Hammer S.M. The challenge of HIV-1 subtype diversity. N Engl J Med. 2008;358:1590–1602. doi: 10.1056/NEJMra0706737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tee K.K., Pon C.K., Kamarulzaman A., Ng K.P. Emergence of HIV-1 CRF01_AE/B unique recombinant forms in Kuala Lumpur, Malaysia. AIDS. 2005;19:119–126. doi: 10.1097/00002030-200501280-00003. [DOI] [PubMed] [Google Scholar]
- 101.Tee K.K., Li X.J., Nohtomi K., Ng K.P., Kamarulzaman A., Takebe Y. Identification of a novel circulating recombinant form (CRF33_01B) disseminating widely among various risk populations in Kuala Lumpur, Malaysia. J Acquir Immune Defic Syndr. 2006;43:523–529. doi: 10.1097/01.qai.0000242451.74779.a7. [DOI] [PubMed] [Google Scholar]
- 102.Tee K.K., Saw T.L., Pon C.K., Kamarulzaman A., Ng K.P. The evolving molecular epidemiology of HIV type 1 among injecting drug users (IDUs) in Malaysia. AIDS Res Hum Retroviruses. 2005;21:1046–1050. doi: 10.1089/aid.2005.21.1046. [DOI] [PubMed] [Google Scholar]
- 103.Ou C.Y., Takebe Y., Weniger B.G., Luo C.C., Kalish M.L., Auwanit W. Independent introduction of two major HIV-1 genotypes into distinct high-risk populations in Thailand. Lancet. 1993;341:1171–1174. doi: 10.1016/0140-6736(93)91001-3. [DOI] [PubMed] [Google Scholar]
- 104.Weniger B.G., Takebe Y., Ou C.Y., Yamazaki S. The molecular epidemiology of HIV in Asia. AIDS. 1994;8(Suppl 2):S13–S28. [PubMed] [Google Scholar]
- 105.Tovanabutra S., Kijak G.H., Beyrer C., Gammon-Richardson C., Sakkhachornphop S., Vongchak T. Identification of CRF34_01B, a second circulating recombinant form unrelated to and more complex than CRF15_01B, among injecting drug users in northern Thailand. AIDS Res Hum Retroviruses. 2007;23:829–833. doi: 10.1089/aid.2006.0300. [DOI] [PubMed] [Google Scholar]
- 106.Tovanabutra S., Beyrer C., Sakkhachornphop S., Razak M.H., Ramos G.L., Vongchak T. The changing molecular epidemiology of HIV type 1 among northern Thai drug users, 1999 to 2002. AIDS Res Hum Retroviruses. 2004;20:465–475. doi: 10.1089/088922204323087705. [DOI] [PubMed] [Google Scholar]
- 107.Tovanabutra S., Watanaveeradej V., Viputtikul K., De Souza M., Razak M.H., Suriyanon V. A new circulating recombinant form, CRF15_01B, reinforces the linkage between IDU and heterosexual epidemics in Thailand. AIDS Res Hum Retroviruses. 2003;19:561–567. doi: 10.1089/088922203322230923. [DOI] [PubMed] [Google Scholar]
- 108.Beyrer C., Vancott T.C., Peng N.K., Artenstein A., Duriasamy G., Nagaratnam M. HIV type 1 subtypes in Malaysia, determined with serologic assays: 1992–1996. AIDS Res Hum Retroviruses. 1998;14:1687–1691. doi: 10.1089/aid.1998.14.1687. [DOI] [PubMed] [Google Scholar]
- 109.Brown T.M., Robbins K.E., Sinniah M., Saraswathy T.S., Lee V., Hooi L.S. HIV type 1 subtypes in Malaysia include B, C, and E. AIDS Res Hum Retroviruses. 1996;12:1655–1657. doi: 10.1089/aid.1996.12.1655. [DOI] [PubMed] [Google Scholar]
- 110.Saraswathy T.S., Ng K.P., Sinniah M. Human immunodeficiency virus type 1 subtypes among Malaysian intravenous drug users. Southeast Asian J Trop Med Public Health. 2000;31:283–286. [PubMed] [Google Scholar]
- 111.Wang B., Lau K.A., Ong L.Y., Shah M., Steain M.C., Foley B. Complex patterns of the HIV-1 epidemic in Kuala Lumpur, Malaysia: evidence for expansion of circulating recombinant form CRF33_01B and detection of multiple other recombinants. Virology. 2007;367:288–297. doi: 10.1016/j.virol.2007.05.033. [DOI] [PubMed] [Google Scholar]
- 112.Li K.S., Guan Y., Wang J., Smith G.J., Xu K.M., Duan L. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430:209–213. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- 113.Webster R.G. The importance of animal influenza for human disease. Vaccine. 2002;20(Suppl 2):S16–S20. doi: 10.1016/s0264-410x(02)00123-8. [DOI] [PubMed] [Google Scholar]
- 114.Alexander D.J. Summary of avian influenza activity in Europe, Asia, Africa, and Australasia, 2002–2006. Avian Dis. 2007;51:161–166. doi: 10.1637/7602-041306R.1. [DOI] [PubMed] [Google Scholar]
- 115.World Organisation for Animal Health. Update on highly pathogenic avian influenza in animals (type H5 and H7). Paris: World Organisation for Animal Health; 2008.
- 116.Kilpatrick A.M., Chmura A.A., Gibbons D.W., Fleischer R.C., Marra P.P., Daszak P. Predicting the global spread of H5N1 avian influenza. Proc Natl Acad Sci USA. 2006;103:19368–19373. doi: 10.1073/pnas.0609227103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hulse-Post D.J., Sturm-Ramirez K.M., Humberd J., Seiler P., Govorkova E.A., Krauss S. Role of domestic ducks in the propagation and biological evolution of highly pathogenic H5N1 influenza viruses in Asia. Proc Natl Acad Sci USA. 2005;102:10682–10687. doi: 10.1073/pnas.0504662102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wallace R.G., Hodac H., Lathrop R.H., Fitch W.M. A statistical phylogeography of influenza A H5N1. Proc Natl Acad Sci USA. 2007;104:4473–4478. doi: 10.1073/pnas.0700435104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chua K.B., Chua B.H., Wang C.W. Anthropogenic deforestation, El Niño and the emergence of Nipah virus in Malaysia. Malays J Pathol. 2002;24:15–21. [PubMed] [Google Scholar]
- 120.Daszak P., Plowright R.K., Epstein J.H., Pulliam J., Abdul Rahman S., Field H.E., the Henipavirus Ecology Research Group (HERG) The emergence of Nipah and Hendra virus: pathogen dynamics across a wildlife-livestock-human continuum. In: Collinge S.K., Ray C., editors. Disease ecology: community structure and pathogen dynamics. Oxford University Press; Oxford: 2006. pp. 186–201. [Google Scholar]
- 121.Epstein J.H., Field H.E., Luby S., Pulliam J.R., Daszak P. Nipah virus: impact, origins, and causes of emergence. Curr Infect Dis Rep. 2006;8:59–65. doi: 10.1007/s11908-006-0036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rogers D.J., Randolph S.E. Studying the global distribution of infectious diseases using GIS and RS. Nat Rev Microbiol. 2003;1:231–237. doi: 10.1038/nrmicro776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Calisher C.H., Childs J.E., Field H.E., Holmes K.V., Schountz T. Bats: important reservoir hosts of emerging viruses. Clin Microbiol Rev. 2006;19:531–545. doi: 10.1128/CMR.00017-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Halpin K., Hyatt A.D., Plowright R.K., Epstein J.H., Daszak P., Field H.E. Emerging viruses: coming in on a wrinkled wing and a prayer. Clin Infect Dis. 2007;44:711–717. doi: 10.1086/511078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wacharapluesadee S., Boongird K., Wanghongsa S., Phumesin P., Hemachudha T. Drinking bat blood may be hazardous to your health. Clin Infect Dis. 2006;43:269. doi: 10.1086/505311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Takebe Y., Motomura K., Tatsumi M., Lwin H.H., Zaw M., Kusagawa S. High prevalence of diverse forms of HIV-1 intersubtype recombinants in Central Myanmar: geographical hot spot of extensive recombination. AIDS. 2003;17:2077–2087. doi: 10.1097/00002030-200309260-00009. [DOI] [PubMed] [Google Scholar]
- 127.Konings F.A., Burda S.T., Urbanski M.M., Zhong P., Nadas A., Nyambi P.N. Human immunodeficiency virus type 1 (HIV-1) circulating recombinant form 02_AG (CRF02_AG) has a higher in vitro replicative capacity than its parental subtypes A and G. J Med Virol. 2006;78:523–534. doi: 10.1002/jmv.20572. [DOI] [PubMed] [Google Scholar]
- 128.Kiwanuka N., Laeyendecker O., Robb M., Kigozi G., Arroyo M., McCutchan F. Effect of human immunodeficiency virus type 1 (HIV-1) subtype on disease progression in persons from Rakai, Uganda, with incident HIV-1 infection. J Infect Dis. 2008;197:707–713. doi: 10.1086/527416. [DOI] [PubMed] [Google Scholar]