Abstract
An influenza pandemic is inevitable, and the H5N1 avian influenza outbreak in Southeast Asia has heightened concern that a disaster is imminent. Pandemic preparations are beginning around the world, and it is important for first responders, particularly disaster management personnel, to understand the difference between pandemic and epidemic influenza preparedness. This article will focus on distinguishing between an influenza epidemic and an influenza pandemic and, in light of these distinctions, how to manage the next pandemic with limited resources, particularly the absence of vaccine.
The presence of H5N1 influenza in Southeast Asia has reawakened fears of worldwide influenza pandemic of the sort that occurred in 1918.1 The “Spanish flu,” as it was known, raged through the world, killing 40 to 50 million people in less than 1 year.1 Very little is known about how the H1N1 virus of 1918 caused so much death, and only recently has it been suggested that this virus may have spread directly from birds to humans.2 (See Figure 1 for an explanation of influenza virus nomenclature.) Even less is known about the best way to respond to an inevitable influenza pandemic. This article features a discussion about how an influenza pandemic will differ from an annual influenza epidemic and how this difference will affect the public health response.
Figure 1.
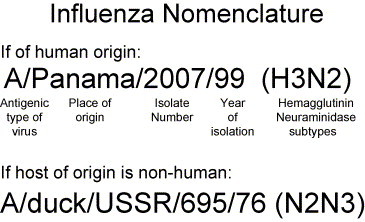
World Health Organization nomenclature for influenza viruses. Note that host of origin is indicated only if strain is isolated from nonhumans. (From the World Health Organization. A revision of the system of nomenclature for influenza viruses: a WHO memorandum. Bulletin of the World Health Organization, 1980;58:585-91.)
Pandemic Versus Epidemic Influenza: Definition
It is very important to distinguish an influenza pandemic from an influenza epidemic, because preparations and responses to each differ significantly. Influenza epidemics are events that occur yearly (or every few years) and are caused by a phenomenon known as antigenic drift. Antigenic drift refers to a minor change that occurs within the influenza virus (at the hemagglutinin or neuraminidase site).3 The resultant strain of influenza is different enough that a new vaccine must be developed to prevent people from getting sick. However, it is not so different that mortality or morbidity rates within a population change very much. Each year in the United States, approximately 36,000 people die from influenza-related illness. Mortality, very predictably, occurs among the very old and very young.4 In general, epidemic influenza strains are characterized early enough to develop adequate vaccine stocks to protect the population during the flu season.5 World Health Organization (WHO) collaborating influenza centers around the world detect new variants, and each year 2 influenza type-A strains and one influenza type-B strain are chosen for a trivalent vaccine.5
It is very important to distinguish an influenza pandemic from an influenza epidemic, because preparations and responses to each differ significantly.
Influenza pandemics, in contrast, occur every few decades and are the result of antigenic shift.3 Antigenic shift refers to the appearance of a completely new influenza virus to which the general population has no immunity.3 As a result, mortality rates are much higher than in epidemics and young healthy adults may have mortality rates as high or higher than those at the extremes of age.1 During the 1918 pandemic, the novel H1N1 influenza A virus killed 40 million people worldwide, and persons between the ages of 15 to 35 years had the highest mortality rates.1 A pandemic strain of influenza is likely to appear suddenly, without advanced warning, and it is unlikely that vaccine will be developed quickly enough to stop it. Production of vaccine takes 6 to 9 months, and in that time, the virus will have spread across the globe.6 Mass vaccination of the population will be required for a pandemic as opposed to the targeted vaccination required to control an epidemic.7
Pandemic Influenza and H5N1, Avian Influenza
The avian influenza (H5N1) outbreak in Southeast Asia, although not currently designated as a pandemic, has certainly increased fears that a worldwide infectious disease catastrophe is imminent. H5N1 first appeared in Hong Kong in 1997 when it infected 18 people and killed 6 people.8, 9 In addition, millions of chickens either died or were culled to prevent further spread.9 Since then, H5N1 has become endemic in wild fowl and poultry in Southeast Asia.10 Between January 28, 2004, and April 4, 2005, 79 people became infected in Thailand, Cambodia, and Vietnam, and 49 have died (a 62% mortality rate) (www.who.int/csr/don/2005_04_04/en/).11, 12 H5N1 has not achieved pandemic status because of its inefficient person-to-person spread.12, 13 However, the virus has changed significantly between 1997 and 2003,14 and human-to-human spread recently has been shown to occur, albeit at a low level.15 In addition, the virus has adapted to infect other animals, including cats, which typically are not susceptible to avian influenzas.16, 17 The looming fear is that H5N1 will genetically adapt into a human-tropic virus or mix with another human influenza virus to produce a novel pandemic strain.18
The looming fear is that H5N1 will genetically adapt into a human-tropic virus or mix with another human influenza virus to produce a novel pandemic strain.18
Pandemic Versus Epidemic: Preparation
The traditional public health approach to yearly influenza epidemics has 3 components: (1) vaccination of high-risk populations, (2) chemoprophylaxis of exposed high-risk populations; and (3) treatment of populations at high risk for complications of influenza.11 However, the public health response to an influenza pandemic is very different. First, it is unlikely that enough (or any) vaccine will be available quickly enough to prevent significant morbidity and mortality. Second, the population at high risk for complications may expand tremendously. Finally, it is unlikely that an influenza pandemic will be contained among health care workers even if excellent infection control practices are followed. Therefore, the protection of health care workers will depend more on available antiviral drugs for chemoprophylaxis and treatment than on vaccination.
During a pandemic, vaccine will not be available. It should be assumed that at the beginning of a pandemic, little or no vaccine would be available.6, 7 Production of vaccine involves identification of strains, development of reassortment strains that will grow in eggs, collection of eggs, inoculation/incubation of eggs, virus extraction from eggs, potency testing, and clinical trials. Even under the most optimal conditions, and even if virus was grown in cell culture instead of eggs, this process requires 6 to 8 months.6 A pandemic influenza strain could spread around the world in half that time.19 It is unlikely that a more rapid vaccine production method (eg, reverse genetics) will be widely available before the next pandemic occurs.
The population at high risk for influenza complications will expand during a pandemic. During yearly influenza epidemics, the following groups are at increased risk of complications from influenza11:
-
•
Persons older than 65 years
-
•
Nursing home residents
-
•
Adults and children with chronic pulmonary and cardiovascular disorders
-
•
Adults and children with diabetes, renal dysfunction, hemoglobinopathies, or immunosuppression
-
•
Children and adolescents receiving long-term aspirin therapy because of the risk of Reye's Syndrome
-
•
Pregnant women
In 2000, approximately 73 million people in the United States were at increased risk of complications from influenza. During a pandemic influenza outbreak, the high-risk population might be 2 to 3 times greater. During the 1918 influenza pandemic, in addition to the high mortality rates in the very young and the elderly, especially high rates of death occurred among young adults between the ages of 15 and 35 years.1 This age group includes a large part of the health care workforce and first responders who would be asked to care for sick and dying influenza patients. Without vaccine to offer protection, health care workers would be left to rely on antiviral agents and infection control practices.
Without vaccine to offer protection, health care workers would be left to rely on antiviral agents and infection control practices.
Infection control practices will not contain an influenza pandemic. Although there is some evidence for aerosol transmission,20 influenza generally is spread through respiratory droplets, and droplet precautions are recommended to control spread of the virus in a health care setting.21 Unfortunately, health care worker attack rates during outbreaks are as high as 59%.21 Even with excellent infection control practices, in the absence of vaccine, attack rates of greater than 10% are likely to occur among health care workers.21 Viral shedding of influenza occurs 1 to 2 days before symptoms are noted and can continue for 7 days after symptoms begin. Infants and immunocompromised individuals may shed for weeks,21 which makes transmission of influenza even more difficult to control both in the hospital and the community. In contrast, the Severe Acute Respiratory Syndrome (SARS) coronavirus shedding peaks at 7 to 10 days after symptoms begin,22 making this disease more easily contained with current infection control practices.23
Strategies to Prepare for an Influenza Pandemic
The following are strategies for preparing for an inevitable influenza pandemic. The Table summarizes these strategies. The omission of vaccination as a strategy early in a pandemic is intentional.
Responders should assume that vaccine will not be available early in a pandemic. Of course, local and federal responders should prepare mass vaccination strategies to be implemented when vaccine is eventually available.
Surveillance
In August 2004, the US Department of Health and Human Services (DHHS) released a draft of a strategy for preparing for pandemic influenza in the United States (www.dhhs.gov/nvpo/pandemicplan/index.html). Although vaccination still is considered “the primary strategy to reduce the impact of a pandemic,” DHHS acknowledges that early in a pandemic, vaccine will not be available. DHHS suggests that only by improving worldwide surveillance can we hope to identify new influenza strains early enough to produce a vaccine. H5N1 avian influenza provides a good example. The virus was first identified in 1997 in Hong Kong,8, 9 and it has been monitored in animals and humans since that time.10, 11, 12, 17 An H5N1 vaccine already has been developed for chickens,24 and, recently, work has begun in earnest on developing a human H5N1 vaccine.25 If H5N1 does cause the next pandemic, this advanced surveillance might save many lives and prevent dissemination of the virus.
The downside to expansive influenza surveillance is the potential for mass production and inoculation of vaccine for a strain of influenza that ultimately does not cause a pandemic. This scenario occurred dramatically in the 1976 swine flu outbreak.26 In January 1976, an outbreak of influenza at Fort Dix, New Jersey, left 1 soldier dead, 4 ill, and 500 exposed. The influenza virus in the dead soldier was identified as H1N1, an antigenic shift from the H3N2 virus that had been circulating worldwide at that time. After confirming that person-to-person spread was probably occurring and surmising that a pandemic was imminent, a panel of experts from the Centers for Disease Control and Prevention (CDC), The Food and Drug Administration, and The National Institutes of Health recommended mass vaccination.26 Between October 1 and December 16, 1976, 45 million people in the United States were vaccinated against swine flu. As it turned out, a pandemic did not occur, and 532 people who received the influenza vaccine developed Guillain-Barre syndrome, a neurologic disease that causes paralysis.26 In retrospect, the fact that no other cases of swine flu occurred after the 5 cases at Fort Dix and the absence of cases in the southern hemisphere, where epidemics usually start, should have halted the vaccination campaign before it started.
To prevent such mistakes from occurring again, the WHO has developed a classification system that defines pandemic phases (http://www.who.int/csr/disease/avian_influenza/Public_health_interventions.pdf).
The inter-pandemic period includes phase 0.0a (no new influenza virus subtypes exist and there is no indication of highly pathogenic avian influenza activity in susceptible animal species) and phase 0.0b (no new influenza virus subtypes exist and evidence of highly pathogenic avian influenza activity in susceptible animal species is reported).
The pre-pandemic period is broken into phases 0.1, 0.2, and 0.3. At phase 0.1, a new influenza strain has been isolated from a single human case but no evidence exists of spread or outbreak activity. At phase 0.2, 2 or more human cases of the new strain have occurred but no evidence exists of human-to-human spread. At phase 0.3, human-to-human transmission is confirmed and a “pandemic alert” is issued by the WHO (see WHO document for details). The H5N1 outbreak currently is at phase 0.2, but if more evidence of person-to-person spread surfaces, it will rise to the level of a pandemic alert (phase 0.3). A pandemic alert results in increased surveillance, vaccine development and clinical testing, and education of health care providers and first responders.
The H5N1 outbreak currently is at phase 0.2, but if more evidence of person-to-person spread surfaces, it will rise to the level of a pandemic alert (phase 0.3).
Pandemic phase 1.0 is the onset of an influenza pandemic and indicates that the virus has spread to other countries and that serious morbidity and mortality are resulting from infection. Response activities during this phase are focused on minimizing spread until a vaccine is available and include isolation/quarantine, minimizing social contacts (travel restrictions), and dispensing antiviral medications for chemoprophylaxis and treatment. These activities will be discussed in more detail later in this article.
Antiviral Medications
If the mortality rate for the next pandemic approaches that seen in the current avian influenza (H5N1) outbreak in Southeast Asia (62%)12, 27 it may be difficult to convince a frightened health care workforce to care for sick patients. Without a vaccine, and with imperfect protection afforded by sound infection control practices, the role of antiviral agents becomes paramount. The WHO has suggested that, in the absence of vaccine, advanced stockpiling of antiviral drugs may be an alternative tool to manage an influenza pandemic.7
Unfortunately, future pandemic influenza strains are likely to be resistant to the cheaper adamantanes, rimantadine and amantadine,28 and the use of these drugs in nursing home outbreaks has resulted in rapid development of resistance.29 The H5N1 avian influenza strain is resistant to the adamantanes.27 This leaves the neuraminidase inhibitors, oseltamivir and zanamivir, as the antiviral drugs of choice for stockpiling. Zanamivir is not widely available and it must be administered in an aerosolized form. Therefore, according to A. Fauci in the March 3, 2005 issue of The Washington Times, the CDC has begun to stockpile oseltamivir. Oseltamivir is expensive ($35 to $40 per 5-day treatment course) (hospital pharmacy data), and it is unlikely that enough medication can be stockpiled to protect all health care workers and patients in a timely fashion. Many hospitals have the resources to stockpile and efficiently disseminate antiviral drugs to health care workers and high-risk groups within the general population (from communications with hospital administrators).
Four potential strategies exist for using antiviral agents during an influenza outbreak7, 30: (1) chemoprophylaxis for the entire influenza outbreak/season (or until vaccine is available); (2) postexposure chemoprophylaxis; (3) treatment of ill patients; and (4) a combination of chemoprophylaxis and treatment.
Chemoprophylaxis is the best strategy to prevent the spread of influenza.30 Several nursing home studies of influenza prevention support the use of prophylactic antiviral agents.31, 32, 33, 34 In a model of the1957-1958 influenza pandemic (H2N2), targeted antiviral prophylaxis of close contacts of influenza cases for 8 weeks would have reduced the attack rate from 33% to 2%.35 However, this strategy is prohibitively expensive. During a pandemic, even targeted prophylaxis of health care workers would likely mean giving 6 to 8 weeks of prophylaxis (oseltamivir, 75 mg per day) to all or most of the persons working in hospitals and on the front lines of the outbreak. The cost to our hospital (the University of Michigan Medical Centers) would be $1 to $2 million to cover 5000 to 10,000 workers (pharmacy data). This cost would be incurred every 5 years as the medication expires.
Health Care Workers
A strategy that focuses primarily on treatment of ill health care workers with some targeted chemoprophylaxis of heavily exposed workers (eg, respiratory therapists and those intubating influenza patients) is financially feasible and offers adequate protection to health care workers caring for influenza-infected patients during a pandemic outbreak. Recent studies have demonstrated that neuraminidase inhibitors administered as treatment (75 mg twice a day for 5 days) within 48 hours of symptoms not only decrease the duration of illness but also decrease the incidence of hospitalization, antibiotic use, and mortality.34, 36, 37 Health care workers are a captive group and easily could be monitored for symptoms (eg, fevers and myalgias) of influenza. It seems feasible that such monitoring would identify most of the ill workers and, thus, allow timely administration of antiviral therapy. We estimate that, with excellent infection control practices, we could expect 10% to 15% of our hospital workers to become ill during an influenza pandemic. Thus, at our hospital, we would expect to treat approximately 1000 to 1500 people with a 5-day course of oseltamivir (10 pills). The total cost to stockpile enough Tamiflu for this strategy would be between $40,000 to $60,000 (pharmacy data). Smaller hospitals obviously would spend less.
General Population
The strategy for use of antiviral medications in the general population is less clear. The guidelines for antiviral use during epidemics, which relies on identifying high-risk group treatment and prophylaxis,7 may be useless during a pandemic as the at-risk population increases or changes.1 If 15% to 30% of the nonimmune population gets infected with pandemic flu, approximately 45 to 90 million doses of oseltamivir will be required in the United States. Both financially and logistically, stockpiling and disseminating this amount of medication is not feasible. Neither the government nor hospitals can afford such a gargantuan expense. An alternative strategy might be to focus treatment and prophylaxis of the general population in the most heavily affected areas in an attempt to slow down transmission until vaccine is available. DHHS suggests that a strategy based on treatment is more cost-effective and efficient than one based on chemoprophylaxis (www.dhhs.gov/nvpo/pandemicplan/annex7.antiviral.pdf). However, treatment must be initiated within 48 hours of symptoms for therapy to be effective. Chemoprophylaxis, according to DHHS, should be used primarily to maintain adequate health care and safety services.
The strategy for use of antiviral medications in the general population is less clear.
Limiting Transmission: Infection Control, Quarantine, Modular Emergency Medical System
Once vaccine is available, limiting transmission will be based on a mass vaccination campaign. In the initial phases of a pandemic, influenza vaccine may not be available, and limiting transmission will be a huge challenge. Containment strategies are limited by influenza's short incubation period (3 days) and the fact that people infected with influenza can spread disease several days before symptoms appear.4, 7, 21 Thus, as previously described, infection control practices that are effective with other infections, such as SARS,22 will not work as well with pandemic flu. DHHS recommends that, early in a pandemic, patients should be placed in a negative pressure room (www.dhhs.gov/nvpo/pandemicplan/annex8.stratlimittrans.pdf). As cases mount, patients should be placed in private rooms, and, finally, cohorted on separate wards or in separate buildings. Health care workers caring for influenza patients should use droplet and contact precautions, including wearing a surgical mask, gloves, and gowns, using eye protection, and washing hands.21
Spread within the community will be more difficult to control than in health care facilities. For community containment, DHHS recommends travel limitations, screening of travelers for febrile or respiratory illness, canceling large group gatherings, closing schools, limiting public transportation, discouraging handshaking, encouraging hand hygiene, teaching respiratory hygiene/cough etiquette, and wearing masks in public (www.dhhs.gov/nvpo/pandemicplan/annex8.stratlimittrans.pdf). Even though large-scale quarantines have not traditionally been effective to limit the spread of influenza,38 home quarantine (or sheltering in place) might help to slow down a pandemic while vaccine is being developed. There are examples of quarantine/isolation being effective in slowing transmission of the 1918 Spanish flu in more remote populations in Somoa and Alaska (www.dhhs.gov/nvpo/pandemicplan/annex8.stratlimittrans.pdf). More recently, the quarantine of more than 150,000 people during the 2003 SARS outbreak in Taiwan contributed to shortening the onset-to-diagnosis time compared with those who were not quarantined.39
Any strategy that involves quarantine or limiting activity will rely heavily on existing public health laws. These laws vary widely from state to state, and many have not been updated in a quarter century or longer.40 Furthermore, these drastic measures, which are not commonplace, may foment panic and suspicion among an already edgy public. Public health, emergency management and law enforcement must establish quarantine/isolation strategies ahead of time and educate the public about the importance of these strategies in containing pandemic influenza.
Public health, emergency management and law enforcement must establish quarantine/isolation strategies ahead of time and educate the public about the importance of these strategies in containing pandemic influenza.
The Modular Emergency Medical System (MEMS) is another way of mobilizing the health care system to handle infectious disease outbreaks like pandemic influenza. Created in response to the Nunn-Lugar-Domenici Domestic Preparedness Program by the Department of Defense, MEMS is an attempt to expand the local health care structure in response to a mass casualty event (www.edgewood.army.mil/downloads/reports/mems_copper_book.pdf). To manage the huge patient burden of a mass casualty event like pandemic influenza, health care delivery will be moved away from hospitals except for the most seriously ill patients. Two patient care modules would be established within communities: The Neighborhood Emergency Help Center (NEHC) would be the primary triage point for symptomatic and asymptomatic exposed patients. From the NEHC, patients could be sent home, to a hospital, or to an Acute Care Center (ACC). ACCs would accommodate patients who require hospitalization but do not need ventilator support or ICU care. The ACC will be near a hospital and will be staffed by physicians and nurses who can provide intravenous fluids, intravenous and oral medications, oxygen, and other supportive care. Also, patients for whom survival is unlikely may be sent to an ACC for comfort care. Area hospitals will only take the sickest patients and all elective procedures will likely cease until the end of the outbreak. NEHCs and ACCs also might serve as distribution/administration points for antiviral medications and/or vaccine in the case of pandemic influenza. Although MEMS is not yet fully functional, states are beginning to implement plans for its creation, and exercises have been organized to test it. It is not yet clear what the trigger will be for activating MEMS, but it is likely to be different in each state/locality.
In the past several years, the public health infrastructure has been bolstered to deal with an outbreak of pandemic influenza by the injection of funds for Weapons of Mass Destruction preparedness, particularly bioterrorism preparedness. Both the CDC and the Health Resources and Services Administration have provided funds for training, communication, public health preparedness and hospital preparedness (www.hhs.gov/news/press/2003pres/20030320.html). In 2003, Michigan received close to $41.5 million for bioterrorism preparedness. This money has been used to develop a regional structure that brings together public health, emergency management, law enforcement, and the hospitals in preparing for a biological event (www.2south.com/index.php).
Conclusion
Influenza pandemics are a real threat, based on previous history of genetic changes in the influenza virus. Influenza pandemics typically have caused significant morbidity and mortality, affecting all age groups, especially persons ages 15 to 35 years. A pandemic will require different strategies by health care providers, such as increased surveillance to recognize the emergence of novel strains, the use of antiviral agents to control symptoms, and increased public health and acute care efforts to contain the spread of the virus. Table 1
Table.
Summary of strategies for control of pandemic influenza
| Strategy | Control mechanisms |
| Surveillance | Worldwide surveillance to identify new strains of virus |
| Classify according to WHO's pandemic phases | |
| Antiviral medications | Vaccine is not likely to be available in sufficient time or quantities |
| Resistance to antivirals becoming more common | |
| Target heavily exposed health care workers | |
| Focus treatment on heavily exposed general population only | |
| Infection control practices | Containment efforts limited by influenza's short incubation period (3 days) |
| As pandemic unfolds and cases increase, isolate patients in negative pressure room, private rooms, and isolation wards | |
| Consider home quarantine, limit community gatherings | |
| Mobilize additional heath care services, eg, MEMS |
MEMS, Modular Emergency Medical System; WHO, World Health Organization.
References
- 1.Taubenberger J.K., Reid A.H., Fanning T.G. Capturing a killer flu virus. Sci Am. 2005(January):62–71. [PubMed] [Google Scholar]
- 2.Reid A.H., Fanning T.G., Janczewski T.A., Lourens R.M., Taubenberger J.K. Novel origin of the 1918 pandemic influenza virus nucleoprotein gene. J Virol. 2004;78:12462–12470. doi: 10.1128/JVI.78.22.12462-12470.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zambon M.C. Epidemiology and pathogenesis of influenza. J Antimicrob Chemother. 1999;44(suppl B):3–9. doi: 10.1093/jac/44.suppl_2.3. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2003;52(RR-08):1–50. [Google Scholar]
- 5.Stohr K. Overview of the WHO global influenza programme. Dev Biol. 2003;115:3–8. [PubMed] [Google Scholar]
- 6.Patriarca P.A., Cox N.J. Influenza pandemic preparedness plan for the United States. J Infect Dis. 1997;176(suppl 1):S4–S7. doi: 10.1086/514174. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . WHO; 2004. WHO guidelines on the use of vaccines and antivirals during influenza pandemics. Global health security: epidemic alert and response. p. 1-11. [Google Scholar]
- 8.Horimoto T., Kawaoka Y. Pandemic threat posed by avian influenza A viruses. Clin Microbiol Rev. 2001;14:129–149. doi: 10.1128/CMR.14.1.129-149.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan P.K. Outbreak of avian influenza A(H5N1) virus infection in Hong Kong in 1997. Clin Infect Dis. 2002;34(suppl 2):S58–S64. doi: 10.1086/338820. [DOI] [PubMed] [Google Scholar]
- 10.Ellis T.M., Bousfield R.B., Bissett L.A., Dyrting K.C., Luk G.S., Tsim S.T. Investigation of outbreaks of highly pathogenic H5N1 avian influenza in waterfowl and wild birds in Hong Kong in late 2002. Avian Pathol. 2004;33:492–505. doi: 10.1080/03079450400003601. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Cases of influenza A (H5N1)—Thailand, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:100–103. [PubMed] [Google Scholar]
- 12.Chotpitayasunondh T., Ungchusak K., Hanshaoworakul W., Chunsuthiwat S., Sawanpanyalert P., Kijphati R. Human disease from influenza A (H5N1), Thailand, 2004. Emerg Infect Dis. 2005;11:201–209. doi: 10.3201/eid1102.041061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liem N.T., Lim W. Lack of H5N1 avian influenza transmission to hospital employees, Hanoi, 2004. Emerg Infect Dis. 2005;11:210–215. doi: 10.3201/eid1102.041075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horimoto T., Fukuda N., Iwatsuki-Horimoto K., Guan Y., Lim W., Peiris M. Antigenic differences between H5N1 human influenza viruses isolated in 1997 and 2003. J Vet Med Sci. 2004;66:303–305. doi: 10.1292/jvms.66.303. [DOI] [PubMed] [Google Scholar]
- 15.Ungchusak K., Auewarakul P., Dowell S.F., Kitphati R., Auwanit W., Puthavathana P. Probable person-to-person transmission of avian influenza A (H5N1) N Engl J Med. 2005;352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 16.Keawcharoen J., Oraveerakul K., Kuiken T., Fouchier R.A., Amonsin A., Payungporn S. Avian influenza H5N1 in tigers and leopards. Emerg Infect Dis. 2004;10:2189–2191. doi: 10.3201/eid1012.040759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuiken T., Rimmelzwaan G., van Riel D., van Amerongen G., Baars M., Fouchier R. Avian H5N1 influenza in cats. Science. 2004;306:241. doi: 10.1126/science.1102287. [DOI] [PubMed] [Google Scholar]
- 18.Guan Y., Poon L.L., Cheung C.Y., Ellis T.M., Lim W., Lipatov A.S. H5N1 influenza: a protean pandemic threat. Proc Natl Acad Sci U S A. 2004;101:8156–8161. doi: 10.1073/pnas.0402443101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stohr K., Esveld M. Public health. Will vaccines be available for the next influenza pandemic? Science. 2004;306:2195–2196. doi: 10.1126/science.1108165. [DOI] [PubMed] [Google Scholar]
- 20.Moser M.R., Bender T.R., Margolis H.S., Nable G.R., Kendal A.P., Ritter D.G. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 21.Algado C.D., Farr B.M., Hall K.K., Hayden F.G. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 22.Peiris J.S.M., Chu C.M., Cheng V.C.C., Chan K.S., Hung I.F.N., Poon L.L.M. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gopalakrishna G., Choo P., Leo Y.S., Tay B.K., Lim Y.T., Khan A.S. SARS transmission and hospital containment. Emerg Infect Dis. 2004;10:395–400. doi: 10.3201/eid1003.030650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ellis T.M., Leung C.Y., Chow M.K., Bissett L.A., Wong W., Guan Y. Vaccination of chickens against H5N1 avian influenza in the face of an outbreak interrupts virus transmission. Avian Pathol. 2004;33:405–412. doi: 10.1080/03079450410001724012. [DOI] [PubMed] [Google Scholar]
- 25.Subbarao K., Chen H., Swayne D., Mingay L., Fodor E., Brownlee G. Evaluation of a genetically modified reassortant H5N1 influenza A virus vaccine candidate generated by plasmid-based reverse genetics. Virology. 2003;305:192–200. doi: 10.1006/viro.2002.1742. [DOI] [PubMed] [Google Scholar]
- 26.Dowdle W.R. Pandemic influenza: confronting a re-emergent threat. The 1976 experience. J Infect Dis. 1997;176(suppl 1):S69–S72. doi: 10.1086/514180. [DOI] [PubMed] [Google Scholar]
- 27.Hien T.T., Liem N.T., Dung N.T., San L.T., Horby P. Avian influenza A (H5N1) in 10 patients in Vietnam. N Eng J Med. 2004;350:1179–1188. doi: 10.1056/NEJMoa040419. [DOI] [PubMed] [Google Scholar]
- 28.Wainright P.O., Perdue M.L., Brugh M. Amantadine resistance among hemagglutinin subtype 5 strains of avian influenza virus. Avian Dis. 1991;35:31–39. [PubMed] [Google Scholar]
- 29.Saito R., Oshitani H., Masuda H., Suzuki H. Detection of amantadine-resistant influenza A virus strains in nursing homes by PCR-restriction fragment length polymorphism analysis with nasopharyngeal swabs. J Clin Micro. 2002;40:84–88. doi: 10.1128/JCM.40.1.84-88.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ward P., Smith I., Small J., Suter P., Dutkowski R. Oseltamivir (Tamiflu®) and its potential for use in the event of an influenza pandemic. J Antimicrob Chemo. 2005;55(suppl S1):i5–i21. doi: 10.1093/jac/dki018. [DOI] [PubMed] [Google Scholar]
- 31.Brady M.T., Sears S.D., Pacini D.L., Samorodin R., DePamphilis J., Oakes M. Safety and prophylactic efficacy of low-dose rimantidine in adults during an influenza A epidemic. Antimicrob Agents Chemo. 1990;34:1633–1636. doi: 10.1128/aac.34.9.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shilling M., Povinelli L., Krause P., Gravenstein M., Ambrozaitis A., Jones H.H. Efficacy of zanamivir for chemoprophylaxis of nursing home influenza outbreaks. Vaccine. 1998;16:1771–1774. doi: 10.1016/s0264-410x(98)00141-8. [DOI] [PubMed] [Google Scholar]
- 33.Hayden F.G., Altmar R.L., Schilling M., Johnson C., Poretz D., Paar D. Use of the selective neuraminidase inhibitor oseltamivir to prevent influenza. New Engl J Med. 1999;341:1336–1343. doi: 10.1056/NEJM199910283411802. [DOI] [PubMed] [Google Scholar]
- 34.Bowles S.K., Lee W., Simor A.E., Vearncombe M., Loeb M., Tamblyn S. Use of oseltamivir during influenza outbreaks in Ontario nursing homes, 1999-2000. J Am Geriatr Soc. 2002;50:608–616. doi: 10.1046/j.1532-5415.2002.50153.x. [DOI] [PubMed] [Google Scholar]
- 35.Longini I.M., Halloran M.E., Nizam A. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159:623–633. doi: 10.1093/aje/kwh092. [DOI] [PubMed] [Google Scholar]
- 36.Kaiser L., Wat C., Mills T., Mahoney P., Ward P., Hayden F. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med. 2003;163:1667–1672. doi: 10.1001/archinte.163.14.1667. [DOI] [PubMed] [Google Scholar]
- 37.Whitley R.J., Hayden F.G., Reisinger K.S., Young N., Dutkowski R., Ipe D. Oral oseltamivir treatment of influenza in children. Pediatr Infect Dis J. 2001;20:127–133. doi: 10.1097/00006454-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Sattenspiel L., Herring D.A. Simulating the effect of quarantine on the spread of the 1918-19 flu in central Canada. Bull Math Biol. 2003;65:1–26. doi: 10.1006/bulm.2002.0317. [DOI] [PubMed] [Google Scholar]
- 39.Hsieh Y.H., King C.C., Chen C.W., Ho M.S., Lee J.Y., Liu F.C. Quarantine for SARS, Taiwan. Emerg Infect Dis. 2005;11:278–282. doi: 10.3201/eid1102.040190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gostin L.O. Pandemic Influenza: public health preparedness for the next global health emergency. J Law Med Ethics. 2004;32:565–573. doi: 10.1111/j.1748-720x.2004.tb01962.x. [DOI] [PubMed] [Google Scholar]


