Abstract
This study characterizes the prevalence of reverse-transcriptase polymerase chain reaction results positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) among patients presenting with influenzalike illness who underwent nasopharyngeal swab testing for influenza and respiratory syncytial virus over 4 days in March 2020.
Until recently, diagnostic testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), was only available through public health laboratories.1,2,3 This limited testing was prioritized for persons who had severe illness or identifiable risk factors, such as travel to an area with ongoing transmission. Thus, the incidence of community transmission by persons with mild illness and without risk factors remains ill-defined.
The current public health strategy of case containment is premised on the assumption of no or limited community transmission. Identifying a high rate of community transmission would indicate a need to shift the public health strategy from containment to mitigation of spread. Thus, determining the rate at which mild disease is spreading in the community, particularly among persons without risk factors for acquisition of the virus, is critically important.
We conducted a rapid sentinel surveillance study to determine what proportion of mild, outpatient influenzalike illnesses were caused by SARS-CoV-2.
Methods
Between March 12-13 and 15-16, 2020, the Los Angeles County + University of Southern California Medical Center conducted testing among patients presenting with mild influenzalike illness to the emergency department or urgent care. Patients who had nasopharyngeal swabs tested with polymerase chain reaction assays for influenza and respiratory syncytial virus (GeneXpert Flu, Cepheid) were automatically tested for SARS-CoV-2 (Quest Diagnostics).
Only the influenza tests conducted during the day shift were automatically tested for SARS-CoV-2 because the process was manual. Patients were excluded if they had specific risk factors for SARS-CoV-2 (eg, travel exposure or known contact with a traveler, severely ill patients admitted for respiratory tract infections). Positive test results were followed up by Department of Public Health experts to assess clinical factors and demographics.
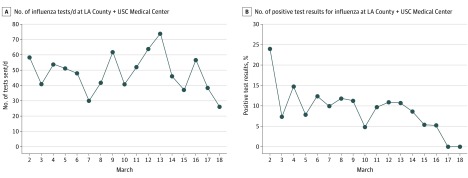
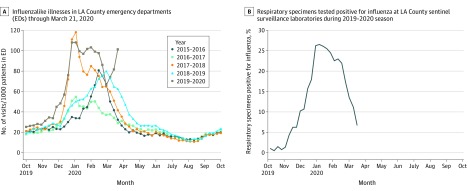
The number of influenza tests ordered by physicians at the Los Angeles County + University of Southern California Medical Center between March 2 and March 18, 2020, and the proportion testing positive for influenza were also assessed. In addition, the rate of influenzalike illnesses obtained from weekly surveys of emergency departments over the past 5 years were summarized, as well as the percentage of respiratory specimens testing positive for influenza from ongoing public health sentinel surveillance conducted at 7 clinical laboratories across Los Angeles County, California.
This study was approved as expedited with a waiver of informed consent by the University of Southern California health sciences campus institutional review board.
Results
One hundred thirty-one tests for SARS-CoV-2 were obtained and 7 were positive (5.3%; 95% CI, 2.2%-10.7%). The median age of patients who tested positive was 38 years (range, 34-44 years), 3 were male (43%), and the median duration of symptoms was 4 days (range, 2-4 days) at presentation. Six of 7 patients presented with fever, 5 with myalgias, and only 1 with cough. Only 1 patient had a travel history (returned from Miami, Florida). All patients had mild illnesses, and all tested negative for influenza and respiratory syncytial virus.
At the Los Angeles County + University of Southern California Medical Center, the number of influenza tests ordered by physicians was relatively stable, but the percentage of positive test results for influenza declined around the time of the study (Figure 1). Across the county, sentinel testing revealed a third seasonal spike in influenzalike illnesses during the weeks before the study; no third seasonal spike was seen during the prior 4 years, and the third spike occurred later than any spike during those years (Figure 2A). This late, third seasonal influenzalike illness spike occurred even as the percentage of respiratory specimens that tested positive for influenza steadily declined (Figure 2B).
Figure 1. Community Influenzalike Illnesses and Influenza Positivity at the LA County + USC Medical Center.
LA County + USC indicates Los Angeles County + University of Southern California.
Figure 2. Epidemiological Curve of Influenzalike Illnesses Through March 21, 2020, and Percentage of Positive Test Results for Influenza at Sentinel Surveillance Sites Across Los Angeles County, California.
Discussion
The 5% rate of SARS-CoV-2 among patients with mild influenzalike illness without risk factors is concerning. These patients had sufficiently mild illness to be active in the community throughout their illness, increasing the possibility of transmission. Such transmission is consistent with the unusual, third countywide influenzalike illness spike that occurred late in the season and with declining rates of influenza positivity.
The primary limitations of the study were the sampling for a brief period at 1 medical center and SARS-CoV-2 testing only being conducted during the day. Nevertheless, the results suggested that containment efforts were unlikely to succeed and helped inform the Los Angeles County Department of Public Health to adopt a more aggressive mitigation strategy to reduce COVID-19 morbidity and mortality. Similar efforts may be needed in other jurisdictions.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Del Rio C, Malani PN. 2019 novel coronavirus—important information for clinicians. JAMA. 2020;323(11):1039-1040. doi: 10.1001/jama.2020.1490 [DOI] [PubMed] [Google Scholar]
- 2.Del Rio C, Malani PN. COVID-19—new insights on a rapidly changing epidemic. JAMA. Published online February 28, 2020. doi: 10.1001/jama.2020.3072 [DOI] [PubMed] [Google Scholar]
- 3.Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA. 2020;323(8):707-708. doi: 10.1001/jama.2020.0757 [DOI] [PubMed] [Google Scholar]