Abstract
OBJECTIVES:
Previous research suggests black nursing home (NH) residents are more likely to receive inappropriate antipsychotics. Our aim was to examine how NH characteristics, particularly the racial and socioeconomic composition of residents, are associated with the inappropriate use of antipsychotics.
DESIGN:
This study used a longitudinal approach to examine national data from Long-Term Care: Facts on Care in the US (LTCFocUS.org) between 2000 and 2015. We used a multivariate linear regression model with year and state fixed effects to estimate the prevalence of inappropriate antipsychotic use at the NH level.
SETTING:
Free-standing NHs in the United States.
PARTICIPANTS:
The sample consisted of 12 964 NHs.
MEASUREMENTS:
The outcome variable was inappropriate antipsychotic use at the facility level. The primary indicator variables were whether a facility had high proportions of black residents and the percentage of residents with Medicaid as their primary payer.
RESULTS:
NHs with high and low proportions of blacks had similar rates of antipsychotic use in the unadjusted analyses. NHs with high proportions of black residents had significantly lower rates of inappropriate antipsychotic use (β = −2; P < .001) in the adjusted analyses. Facilities with high proportions of Medicaid-reliant residents had higher proportions of inappropriate use (β = .04; P < .001).
CONCLUSION:
Findings from this study indicate a decline in the use of antipsychotics. Although findings from this study indicated facilities with higher proportions of blacks had lower inappropriate antipsychotic use, facility-level socioeconomic disparities continued to persist among NHs. Policy interventions that focus on reimbursement need to be considered to promote reductions in antipsychotic use, specifically among Medicaid-reliant NHs.
Keywords: racial/ethnic disparities, medication restraint use, socioeconomic disparities, quality of care, nursing home
In 2014, approximately 16 000 nursing homes (NHs) provided care to an estimated 1.4 million residents who had cognitive and physical impairments.1 NHs provide care to some of the most vulnerable populations, and poor quality of care continues to be a concern for residents, families, and policymakers. Concerns with the inappropriate use of restraints, both physical and chemical, within NHs have plagued the industry for a number of years.2 Chemical restraints are psychotropic medications such as antipsychotics that are used inappropriately for so-called off-label management of dementia-related behaviors (eg, aggression and agitation), and they are an important measure of NH quality.3 A number of national initiatives have worked to decrease inappropriate antipsychotic use, specifically the 1987 Omnibus Budget Reconciliation Act’s Nursing Home Reform Act (OBRA’87), the 2005 and 2008 Food and Drug Administration (FDA) black box warnings, and the 2012 Centers for Medicare & Medicaid Services (CMS) National Partnership to Improve Dementia Care in Nursing Homes. Given the importance of reducing inappropriate antipsychotic use, CMS publicly reports the rates of residents who receive an antipsychotic medication.
The inappropriate use of antipsychotics among older adults often causes adverse outcomes such as memory loss, reductions in mobility and strength, depression, and mortality.4 As regulations concerning the use of physical restraints among NH residents became more stringent with the OBRA’87 legislation, some suggested that antipsychotics were being used as a substitute to control less desirable behaviors in residents.5,6 Research suggests that in recent years, inappropriate antipsychotic use decreased from 24% in 2011 to 20% in 2013.7 Nevertheless, reports show that the inappropriate use of antipsychotics in NHs, especially for residents with dementia, continues to be a widespread problem.3
Several facility-level characteristics were shown to be associated with NH antipsychotic use. NHs that are for profit, have a special care unit (SCU), and have increasing percentages of residents with dementia have been predictive of increased antipsychotic medication use, whereas larger NHs, those part of a chain, and those with higher occupancy were associated with decreasing use.8 Higher rates of antipsychotic drug use were also associated with NHs having higher proportions of African American residents.6 Although literature examining racial and ethnic disparities in NH care is expanding, literature is sparse on racial and ethnic disparities in inappropriate antipsychotic use, and especially limited at the facility level.
To our knowledge, only one study examines racial disparities in the use of antipsychotics and accounts for facility-level characteristics. Miller et al found that African Americans in New York NHs had a greater likelihood of receiving an antipsychotic as compared with their white counterparts, and residents in NHs with more African Americans had an increased risk for antipsychotic use.6 Although the Miller et al study provides the first insights into racial and ethnic disparities related to antipsychotic use in NHs, it lacks generalizability to the current national population of NHs, given that it focuses only on one state and uses data that are now almost 25 years old, well predating federal and state efforts to reduce antipsychotic use over the last 14 years.6
As the NH population continues to become more diverse, it is essential to understand mechanisms that may mitigate or enable disparities in long-term care and across facilities, creating a tiered NH system.9 Two primary contributors of NH racial and ethnic disparities are NH segregation and overrepresentation of minority residents in Medicaid-reliant NHs.9–13 Prior research indicates minority residents are disproportionately represented in lower tier facilities that rely heavily on Medicaid, a federal and state insurance program that helps people with limited income and resources access healthcare. Medicaid-reliant NHs are likely to have a lower availability of resources, lower staffing, and lower quality of care,9 as do NHs with higher proportions of black residents.14
The purpose of our study was to examine how NH characteristics, particularly facility racial composition and Medicaid reliance, may influence the inappropriate use of antipsychotics as chemical restraints in NHs. Building on previous literature linking racial composition and Medicaid reliance on quality, we hypothesized that (1) NHs with high proportions of black residents will be associated with increased inappropriate antipsychotic use; and (2) NHs with a higher proportion of Medicaid residents will be associated with an increased use of inappropriate antipsychotics. This study adds to the literature that commonly acknowledges that black residents disproportionately reside in lower quality NHs and experience disparate care and outcomes as a result.10,14–17
STUDY DATA AND METHODS
Data
Facility-level data were obtained from Brown University’s “Long-Term Care: Facts on Care in the US” project. The LTCFocUS data are composed of information from the annual NH survey, Online Survey, Certification and Reporting (OSCAR), and the resident assessment instrument, the Minimum Data Set (MDS). This study uses variables derived from the OSCAR/Certification and Survey Provider Enhanced Reports (CASPER) and MDS sets. These data are reported by state survey agencies and trained clinicians, respectively.
Sample
The sample consisted of 12 964 free-standing Medicare-and Medicaid-certified NHs operating in the United States between 2000 and 2015. All facilities had to be present in our data for at least 2 years to allow for within-facility changes in antipsychotic use over time.
Dependent Variables
The outcome variable was inappropriate antipsychotic use at the facility level, defined as the proportion of residents given an antipsychotic in the facility without a diagnosis of bipolar or schizophrenia on the first Thursday in April.
Independent Variables
Our primary indicator variables were whether a facility had high proportions of black residents and the percentage of residents with Medicaid as their primary payer at the time of the annual OSCAR survey. Consistent with prior literature,14,18 we categorized NHs as having high proportions of black residents if more than 36% (based on the top quintile of facilities) of the residents in the facility on the first Thursday in April were black. An average of 58% of the residents in NHs with a high percentage of black residents identify as black (≥36%). In NHs with a lower percentage of blacks, an average of 6% of the residents identify as black; these are NHs with less than 36% black residents.
Control Variables
We controlled for facility and resident characteristics that may influence antipsychotic use in NHs including (1) facility characteristics: percentage of residents who were physically restrained, percentage of residents with Medicare as the primary payer, staffing hours, the facility weighted inspection deficiency score, profit status, chain affiliation, the presence of an Alzheimer’s SCU; and (2) resident characteristics: percentage female, average age, average activities of daily living (ADLs) score within each facility, and percentage with severe cognitive impairment.
The percentage of residents physically restrained is a quality indicator that may be inversely related to an NH’s use of antipsychotics and other chemical restraints.6,19,20 Medicare is another federal insurance program specifically for older adults and individuals with disabilities, but Medicare reimburses at a higher rate than Medicaid. The percentage of residents with Medicare as their primary payer in an NH offers some insight into the NH’s financial position, and prior work shows that greater numbers of Medicare residents is associated with decreased antipsychotic use.8 Staffing was defined as registered nurse, licensed practical nurse, and certified nursing assistant hours per resident day as separate variables, and increased staffing was shown to be associated with decreased antipsychotic use.6,21 The facility weighted deficiency score is a weighted sum that incorporates the scope and severity of each citation a facility receives during the required annual inspection (OSCAR). NH chain affiliation indicates if the facility is affiliated with a multifacility chain organization of NHs, and profit status indicates whether or not a facility is for profit. Both of these organizational characteristics were found to be associated with antipsychotic use.22 Lastly, we controlled for the presence of an Alzheimer’s SCU because antipsychotic use was reported at higher rates within SCUs.8,19
Average age is the average of all ages of every individual in the facility on the first Thursday in April. The ADL variable measures the proportion of residents with varying levels of dependence for seven ADLs. Dependence for each of the seven ADLs ranges from 0 to 4, where 0 indicates total independence in the task and 4 indicates total dependence. The average score for the facility is on a 0 to 28 scale where 28 indicates total dependence and is averaged across all of the residents present during the survey. Lastly, cognitive impairment was used as proxy for dementia and assessed as the proportion of residents with severe cognitive impairment on the Cognitive Performance Scale (CPS) or Cognitive Function Scale (CFS) on the first Thursday in April. We combined the use of the CPS and CFS because the CFS was unavailable throughout the entire time period. Therefore, we used the CPS score 5 to 6 for years 2000 to 2010 and the CFS score of 4 for 2011 to 2015. This method was validated in previous research.23
Statistical Analysis
Univariate analyses were conducted to provide descriptive statistics of the data. A linear regression model with year fixed effects was used to assess the association between NH characteristics and antipsychotic use among a panel of 12 964 NHs between 2000 and 2015. Our analysis was conducted at the facility-year level with multiple years of observations for each facility; we had a total of 208 418 facility-years in our sample. All analyses were conducted using Stata software v.14.24
RESULTS
Table 1 provides descriptive statistics for NHs during all years, 2000 and 2015. The average inappropriate antipsychotic and physical restraint use among NHs both decreased over this time period, from 17% and 11% in 2000 to 13% and 1% in 2015, respectively. Results not shown in the table indicate that among NHs with a high percentage of black residents (≥36%), 19.3% (standard deviation [SD] = 9.4) of residents inappropriately received an antipsychotic compared with 19.2% (SD = 9.3) among facilities with a low percentage of blacks (<36%). Within Medicaid-reliant NHs (≥85% residents on Medicaid), inappropriate antipsychotic use was an average of 21.8% (SD = 10.9), whereas in non-reliant Medicaid NHs, use was an average of 18.9% (SD = 9.1).
Table 1.
Descriptive Statistics of Nursing Homes, 2000-2015
| Variables | All yearsN = 208 418Facility-years | 2000n = 13 796NHs | 2015n = 13 736NHs |
|---|---|---|---|
| Restraint use, mean (SD) | |||
| Antipsychotic, % | 19.2 (9.4) | 17.4 (8.6) | 12.7 (7.4) |
| Physically restrained, % | 5.8 (8.8) | 10.7 (12) | 1.4 (4.3) |
| NH characteristics, n (%) | |||
| Racial composition | |||
| Black residents, % | |||
| Low (<36%) | 187 148 (89.8) | 12 559 (91) | 12 247 (89.2) |
| High (>36%) | 21 270 (l0.2) | 1237(9) | 1489 (10.8) |
| Payer mix, mean (SD) | |||
| Medicaid residents, % | 63.2 (21.3) | 66.8 (21.7) | 60.2 (22.1) |
| Medicare residents, % | 12.67 (12) | 8.3 (11.1) | 14.3 (12.5) |
| Staffing, mean (SD) | |||
| LPN hours per resident day | .8 (.4) | .7 (.6) | .8 (.4) |
| RN hours per resident day | .4 (.4) | .3 (.4) | .5 (.4) |
| CNA hours per resident day | 2.2 (.9) | 2.1 (1.2) | 2.4 (.8) |
| Ownership, n (%) | |||
| Not for profit | 55 712 (26.7) | 3649 (26.5) | 3668 (26.7) |
| For profit | 152 706 (73.3) | 10 147(73.6) | 10 068 (73.3) |
| Chain affiliation, n (%) | |||
| No | 90 387 (43.4) | 5608 (40.7) | 5725 (41.7) |
| Yes | 118 031 (56.6) | 8188 (59.4) | 8011 (58.3) |
| Alzheimer’s SCU, n (%) | |||
| Not present | 170 219 (81.7) | 11 250 (81.6) | 11,570 (84.2) |
| Present | 38 199 (18.3) | 2546 (18.5) | 2166 (15.8) |
| Deficiency score, mean (SD) | 70.8 (80.2) | 62.1 (77.3) | 74.9 (75.1) |
| Resident characteristicsa | |||
| Demographics | |||
| Female, % | 70.1 (12.7) | 72.6 (12) | 66.6 (12.5) |
| Average age | 80.4 (7) | 81.3 (6.5) | 79.7 (7) |
| Functional and cognitive status, mean (SD) | |||
| Average ADL score | 15.8 (3.1) | 15.1 (3.2) | 16.4 (2.8) |
| Severe cognitive impairment, % | 18.3 (12.3) | 23.7 (12.8) | 13 (9.9) |
Abbreviations: ADL, activity of daily living; CNA, certified nursing assistant; LPN, licensed practical nurse; NH, nursing home; RN, registered nurse; SCU, special care unit.
Measured at the facility level.
Table 2 displays the associations between inappropriate antipsychotic use and the key independent variables: the proportion of black residents and percentage of Medicaid residents, while accounting for other control variables. NHs with high proportions of black residents were associated with a 2 percentage point average decrease (95% confidence interval [CI] = −2.3 to −1.7]) in inappropriate antipsychotic use. Additionally, a 1 percentage point increase of Medicaid residents is significantly associated with a .04 percentage point increase in inappropriate antipsychotic use. Alternatively, NHs with higher proportions of Medicare residents were significantly associated with a decreased use of inappropriate antipsychotics. Furthermore, findings from this study illustrate that physical restraints were significantly and positively associated with inappropriate antipsychotic use (β = .073; 95% CI = .06-.08).
Table 2.
Association Between Resident and Facility Characteristics and Proportion of Residents Inappropriately Given Antipsychotics within the Facility, 2000–2015, with Time and State Fixed Effects
| Nursing home characteristics | Coefficients | 95% CI |
|---|---|---|
| Racial composition | ||
| Black residents, %a | ||
| Low (<36%) | Ref. | Ref. |
| High (>36%) | −2.0** | −2.3 to −1.7 |
| Payer mix | ||
| Medicaid residents, % | .04** | .03 to .04 |
| Medicare residents, % | −.05** | −.06 to −.04 |
| Restraint use | ||
| Physically restrained, % | .07** | .06 to .08 |
| Staffing | ||
| LPN hours per resident day | −.6** | −.9 to −.4 |
| RN hours per resident day | −1.2** | −1.7 to −.9 |
| CNA hours per resident day | .4** | .3 to .5 |
| Ownership | ||
| Not-for-profit facility | Ref. | Ref. |
| For-profit facility | .9** | .7 to 1.1 |
| Chain affiliation | ||
| Non–chain facility | Ref. | Ref. |
| Chain facility | −.3** | −.5 to −.2 |
| Alzheimer’s SCU | ||
| Facility without Alzheimer’s SCU | Ref. | Ref. |
| Facility with Alzheimer’s SCU | 3.5** | 3.3 to 3.7 |
| Deficiency score | .002** | .002 to .003 |
| Resident characteristicsb | ||
| Demographics | ||
| Female, % | −.09** | −.1 to −.08 |
| Average age | .05* | .01 to .1 |
| Functional and cognitive status | ||
| Average ADL score | −.1** | −.2 to −.1 |
| Severe cognitive impairment, % | .08** | .07 to .09 |
Abbreviations: ADL, activity of daily living; CI, confidence interval; CNA, certified nursing assistant; LPN, licensed practical nurse; RN, registered nurse; SCU, special care unit.
P <.05;
P <.001.
High and low categories were created using the quintile for each group; the top 10% of nursing homes with the most minorities were coded as high (36% for blacks).
Measured at the facility level.
Not only was there a difference by racial composition, but there were also notable and statistically significant year effects (Figure 1). Figure 1A and B show lower rates of inappropriate antipsychotic use for NHs with higher percentages of black residents and facilities with lower Medicaid reliance (<85% residents using Medicaid). The figures also highlight the major time points of interest. With each 1-year increase, there was an increase in the percentage of residents experiencing inappropriate antipsychotic use, of 2 to 6 percentage points each yearly until 2006. Between 2006 and 2012, the proportion of residents receiving inappropriate antipsychotic medications decreased for all NHs, possibly due to the national initiatives implemented during this time frame.
Figure 1.
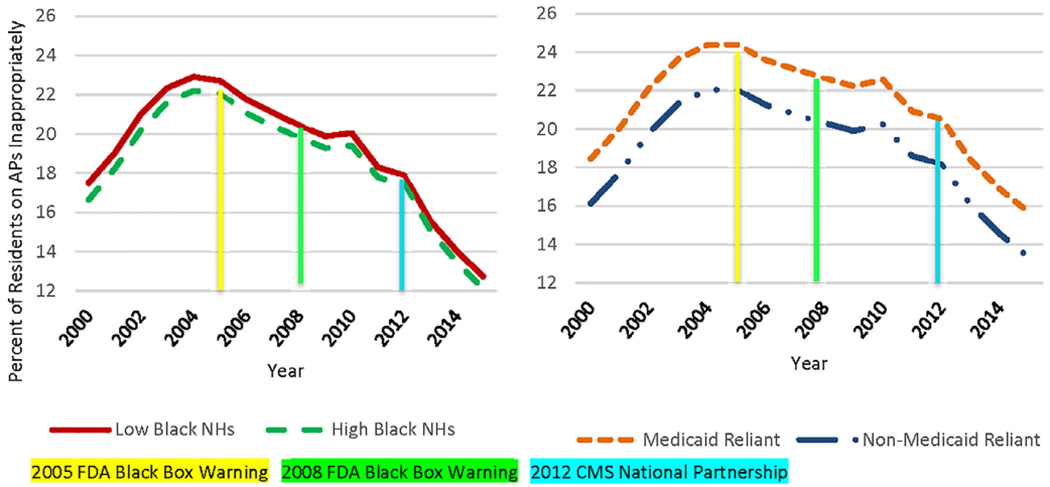
(A, B) Predicted percentage of residents given antipsychotics inappropriately, by year, nursing home (NH) racial composition, and Medicaid reliance between 2000 and 2015 for all NHs. Note: Predicted proportion of residents inappropriately administered antipsychotics was calculated using the adjusted model (Table 2). For panel B (Medicaid reliance), another adjusted model, not shown in Table 2, was used to calcuate the predicted percentage of inappropriate antipsychotic use. Medicaid reliance is based on a binary variable (Medicaid reliant vs non-Medicaid reliant) that indicates if 85% or greater of a NH’s residents have Medicaid as their priamary payer. This measure was developed empircally.9 APs, antipsychotics; CMS, Centers for Medicare & Medicaid Services; FDA, Food and Drug Administration.
DISCUSSION
The findings from this study do not support the existence of facility-level racial disparities in antipsychotic use during this time period. Specifically, facilities with high proportions of black residents have lower rates of inappropriate antipsychotic use. However, facility-level socioeconomic disparities were identified: NHs with higher proportions of Medicaid residents had higher rates of inappropriate antipsychotic use, whereas NHs with higher proportions of Medicare residents had lower rates of inappropriate antipsychotic use. Additionally, physical restraints were found to be positively correlated with inappropriate antipsychotics, suggesting that antipsychotics may not be used as a substitute for physical restraints; rather, inappropriate antipsychotics and physical restraints may be used concurrently. The use of either of these restraint methods is a sign of poor quality. From the facility-level perspective, we can conclude that poor quality facilities, as measured by antipsychotics, are also poor quality facilities, as measured by physical restraints.
Our hypothesis that NHs with high proportions of black residents would have higher antipsychotic use was not confirmed; rather, our results suggest that higher percentages of black residents are associated with lower inappropriate antipsychotic use. It may be the case that higher proportions of black residents may be a protective factor against inappropriate antipsychotic use for NHs. We propose two reasons that may explain why high black NHs have lower rates of inappropriate antipsychotic use among residents. First, findings from this study indicate NHs with Alzheimer’s SCUs have significantly higher odds of inappropriate antipsychotic use among residents. This finding may suggest that NHs with SCUs attract residents with more advanced dementia and greater behavioral and psychological problems that may increase the risk of inappropriate antipsychotic medication use.25 However, blacks are less likely to reside in facilities with Alzheimer’s SCUs.19
Second, NHs with high percentages of black residents may have more residents with cardiovascular comorbid diseases such as diabetes and hypertension.26 The use of certain antipsychotics may be associated with metabolic disturbances for residents with these comorbidities, and high black facilities may use fewer antipsychotics to reduce the increased adverse risks.27,28 This theory could not be examined at the facility level using our data but may be possible using other sources.
As hypothesized, Medicaid-reliant NHs have a higher use of antipsychotic medications. This finding is also consistent with past findings about antipsychotic use.8 Although the magnitude of our percentage Medicaid coefficient is small, the numbers are clinically meaningful. Medicaid-reliant NHs have a 10% to 15% relative increased use of inappropriate antipsychotics as compared with non-Medicaid-reliant facilities. In 2015 this was almost 20% above the national average. NHs with higher proportions of Medicaid residents were found to have lower staffing levels and fewer resources that can lead to poorer quality of care.9 Although state and federal policies have been implemented to decrease inappropriate antipsychotic use, NHs with high proportions of Medicaid residents may still lack the resources to change their organization and implement better quality-of-care practices. Consequently, all residents in Medicaid-reliant NHs have a greater risk of inappropriate use of antipsychotic medications, specifically minority residents who are typically overrepresented in these facilities.9
Results from this study indicate that inappropriate antipsychotic use has decreased over time among NHs. The proportion of residents receiving inappropriate antipsychotics increased steadily until 2005, when the rates of residents receiving antipsychotics then began to decrease. This drop in the rate of inappropriate use is most likely a reflection of the FDA’s black box warning issued in 2005, indicating the risk for increased mortality for so-called off-label use of antipsychotics.3 Additionally, between 2012 and 2013 we saw another sharp decrease in the rate of antipsychotics, most likely due to the CMS National Partnership to lower the use of antipsychotics and improve the care provided to dementia residents.3 As a part of this National Partnership, CMS also added two quality measures to the NH Compare website focused on antipsychotic use in NH long-stay residents.3 Given our findings, research to understand if differences in the impact of these initiatives to reduce antipsychotic use exist across facility types is warranted.
Our study had some limitations. First, our analyses were conducted at the facility level, inevitably limiting the ability to understand the within-facility resident-level disparities that may exist. All implications of this research apply to all residents in the facility. Although the study did not find a facility-level racial disparity in inappropriate antipsychotic use, results indicate facility-level socioeconomic disparities. In future studies, using resident-level data will help parse out possible within-facility resident-level racial disparities in inappropriate antipsychotic use and the interactions and variations within high/low Medicaid and high/low black facilities. Additionally, this study only examined antipsychotics. Future studies should consider other psychotropic medications29 and account for the underreporting of antipsychotics by utilizing drug claims data.30 Furthermore, there is a significant concern that NHs are diagnosing residents with schizophrenia to reduce rates of inappropriate antipsychotic use,7 which may be happening disproportionately by race; however, we are unable to account for this in our work. Moreover, the data used were cross-sectional, so causality cannot be inferred. However, we used multiple years of cross-sectional data that allowed us to track facilities over time. Last, measurement error is always a threat to observational studies, particularly those that rely on selfreport. Our construction of inappropriate antipsychotics differs from the quality measure of the CMS because we do not account for other appropriate antipsychotic medication uses such as for patients with Huntington’s disease or Tourette’s syndrome. However, rates of these conditions in NHs are low.7
In conclusion, our findings indicate there are disparities in high-quality NH care, as measured by inappropriate antipsychotic use, for older adults in NHs with higher proportions of Medicaid beneficiaries. However, facilities having higher proportions of blacks does not seem to be a predictor of poor quality antipsychotic use. Facilities with higher proportions of Medicaid residents may lack the resources to change their organization and implement better quality-of-care practices despite quality initiatives to improve care in these facilities. As such, Medicaid-reliant NHs may benefit from additional resources to facilitate changes needed to improve care for residents. One potential mechanism to reduce facility-level socioeconomic disparities of care in Medicaid-reliant NHs would be to increase Medicaid reimbursements because studies have shown that increased Medicaid payments are associated with higher quality of care in NHs.16 Additionally, our findings illustrate that the National Partnership and public reporting influence antipsychotic use among NHs. Nevertheless, all facilities or residents may not benefit from these initiatives. Finally, we showed that many structural characteristics have an impact on antipsychotic use; as such, interventions at the organizational-level may also be appropriate to mitigate the inappropriate use of antipsychotic medications. In addition, training for NH staff and providers on approaches to manage behaviors associated with dementia may reduce inappropriate use of antipsychotics in NHs.
ACKNOWLEDGMENTS
Financial Disclosure: Research reported in this publication was supported by grants from the National Institute on Aging (P01 AG027296), the Agency for Healthcare Research and Quality (4T32 HS000011), and the Veterans Affairs Health Services Research and Development Service (CDA 14–422).
Footnotes
Conflict of Interest: Much of Vincent Mor’s research focuses on NH care and, specifically, policy issues related to the quality of NH care. His three significant financial interests broadly related to his area of research are HCR Manor Care, Inc (chair, Independent Quality Committee), NaviHealth, Inc (chair of Scientific Advisory Board), and PointRight (former director; holds less than 1% equity). The other authors have declared no conflicts of interest for this article.
REFERENCES
- 1.Nursing Home Care. FastStats - Nursing Home Care. https://www.cdc.gov/nchs/fastats/nursing-home-care.htm. 2016. Accessed December 18, 2018.
- 2.Fashaw SA, Thomas KS, McCreedy E, Mor V. Thirty-year trends in nursing home composition and quality since the passage of the omnibus reconciliation act. J Am Med Dir Assoc. 2019. 10.1016/j.jamda.2019.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cioltan H, Alshehri S, Howe C, et al. Variation in use of antipsychotic medications in nursing homes in the United States: a systematic review. BMC Geriatr. 2017;17(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tampi R, Tampi D, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta-analyses. Ther Adv Chronic Dis. 2016;7(5):229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid. Nursing Home Data Compendium 2013 Edition. 2013. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/nursinghomedatacompendium_508.pdf. Accessed December 18, 2018.
- 6.Miller SC, Papandonatos G, Fennell M, Mor V. Facility and county effects on racial differences in nursing home quality indicators. Soc Sci Med. 2006; 63(12):3046–3059. [DOI] [PubMed] [Google Scholar]
- 7.Winter JD, Kerns JW, Winter KM, Sabo RT. Increased reporting of exclusionary diagnoses inflate apparent reductions in long-stay antipsychotic prescribing. Clin Gerontol. 2019;42(3):297–301. [DOI] [PubMed] [Google Scholar]
- 8.Hughes CM, Lapane KL, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing. Med Care. 2000;38(12):1164–1173. [DOI] [PubMed] [Google Scholar]
- 9.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff. 2007;26(5):1448–1458. [DOI] [PubMed] [Google Scholar]
- 11.Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Aff. 2011;30(7):1358–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Konetzka RT, Werner RM. Disparities in long-term care building equity into market-based reforms. Med Care Res Rev. 2009;66(5):491–521. [DOI] [PubMed] [Google Scholar]
- 13.Davis JA, Weech-Maldonado R, Lapane KL, Laberge A. Contextual determinants ofUS nursing home racial/ethnic diversity. Soc Sci Med. 2014;104:142–147. [DOI] [PubMed] [Google Scholar]
- 14.Chisholm L, Weech-Maldonado R, Laberge A, Lin F- C, Hyer K. Nursing home quality and financial performance: does the racial composition of residents matter? Health Serv Res. 2013;48(6 Pt 1):2060–2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gruneir A, Miller SC, Feng Z, Intrator O, Mor V. Relationship between state Medicaid policies, nursing home racial composition, and the risk of hospitalization for black and white residents. Health Serv Res. 2007;43(3): 869–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grabowski DC. The admission of blacks to high-deficiency nursing homes. Med Care. 2004;42(5):456–464. [DOI] [PubMed] [Google Scholar]
- 17.Smith DB, Feng Z, Fennell ML, Zinn J, Mor V. Racial disparities in access to long-term care: the illusive pursuit of equity. J Health Polit Policy Law. 2008;33(5):861–881. [DOI] [PubMed] [Google Scholar]
- 18.Rivera-Hernandez M, Kumar A, Epstein-Lubow G, Thomas KS. Disparities in nursing home use and quality among African American, Hispanic, and white Medicare residents with Alzheimer’s disease and related dementias. J Aging Health. 2018;31:1259–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sloane PD, Mathew LJ, Scarborough M, Desai JR, Koch GG, Tangen C. Physical and pharmacologic restraint of nursing home patients with dementia. Impact of specialized units. JAMA. 1991;265(10):1278–1282. [PubMed] [Google Scholar]
- 20.Konetzka RT, Brauner DJ, Shega J, Werner RM. The effects of public reporting on physical restraints and antipsychotic use in nursing home residents with severe cognitive impairment. J Am Geriatr Soc. 2014;62(3): 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mattingly TJ. A review exploring the relationship between nursing home staffing and antipsychotic medication use. Neurol Ther. 2015;4(2):169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castle NG, Hanlon JT, Handler SM. Results of a longitudinal analysis of national data to examine relationships between organizational and market characteristics and changes in antipsychotic prescribing in US nursing homes from 1996 through 2006. Am J Geriatr Pharmacother. 2009;7(3):143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas KS, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function Scale. Med Care. 2017;55(9):e68–e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; https://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/. 2015. Accessed November 30, 2018. [Google Scholar]
- 25.Chatterjee S, Mehta S, Sherer JT, Aparasu RR. Prevalence and predictors of anticholinergic medication use in elderly nursing home residents with dementia. Drugs Aging. 2010;27(12):987–997. [DOI] [PubMed] [Google Scholar]
- 26.Dagogo-Jack S Ethnic disparities in type 2 diabetes: pathophysiology and implications for prevention and management. J Natl Med Assoc. 2003;95(9): 774, 779–789. [PMC free article] [PubMed] [Google Scholar]
- 27.Hudson TJ, Cody M, Armitage TL, Curtis MA, Sullivan G. Disparities in use of antipsychotic medications among nursing home residents in Arkansas. Psychiatr Serv. 2005;56(6):749–751.15939955 [Google Scholar]
- 28.Cook TB, Reeves GM, Teufel J, Postolache TT. Persistence of racial disparities in prescription of first-generation antipsychotics in the USA. Pharmacoepidemiol Drug Saf. 2015;24(11):1197–1206. [DOI] [PubMed] [Google Scholar]
- 29.Maust DT, Kim HM, Chiang C, Kales HC. Association of the Centers for Medicare & Medicaid Services’ national partnership to improve dementia care with the use of antipsychotics and other psychotropics in long-term care in the United States from 2009 to 2014. JAMA Intern Med. 2018;178(5): 640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Briesacher BA, Mui B, Devlin JW, Koethe B. Nursing homes underreport antipsychotic prescribing. Aging Ment Health. 2019. 10.1080/13607863.2019.1571015. [DOI] [PMC free article] [PubMed] [Google Scholar]


