Short abstract
Background
A new plate for the treatment of Pauwels type III femoral neck fractures was developed, and its biomechanical stability was analyzed by the finite element method.
Method
Using 3-matic and UG-NX software, we constructed models of Pauwels type III femoral neck fractures with angles of 50°, 60°, and 70°. Moreover, a new femoral neck plate (NFNP) fixation model and a Pauwels screw fixation model were developed. Under axial loads of 1400 N and 2100 N, von Mises stress (VMS) distribution on the screws, peak VMS, displacement between fracture fragments, and model principal strains in cancellous bone were recorded.
Result
The peak VMS of internal fixation in the two models was mostly located near the fracture line, and the screw closest to the femoral calcar experienced maximum stress. With a Pauwels angle of 50°, 60°, and 70°, the peak VMS values of the new plates were lower than in the Pauwels screw. The displacement of fracture fragments in the NFNP was smaller than in the Pauwels screw, and peak VMS values of cancellous bone in the NFNP were lower than in the Pauwels screw.
Conclusion
The newly developed plate provided excellent biomechanical stability for Pauwels type III femoral neck fractures.
Keywords: Pauwels type III femoral neck fracture, new femoral neck plate, von Mises stress, displacement, peak VMS, finite element analysis
Introduction
Pauwels type III femoral neck fractures are often high-energy injuries that occur in young and middle-aged patients.1,2 Owing to the high shear stress of these fractures, the incidence of postoperative complications such as fracture displacement, bone nonunion, and avascular necrosis of the femoral head is relatively high; thus, their clinical treatment is difficult.3 Anatomic reduction and rigid internal fixation are important for successful fracture healing. However, the choice of optimal internal fixation technique for Pauwels type III femoral neck fractures is controversial. At present, the most common internal fixation methods are cancellous screw fixation and the dynamic hip screw. Cancellous lag screws remain the most common treatment for femoral neck fractures in young and middle-aged people.4–6 Cancellous lag screw fixation is mostly performed with parallel screws, which promote bone healing by sliding compression.7 When applying this fixation system for Pauwels type III femoral neck fractures, difficulties are often encountered in the resistance against shear stress. Therefore, postoperative internal fixation failure, fracture end displacement, femoral neck shortening, varus deformity, and bone nonunion occur relatively often.8–11 To reduce the shear stress in Pauwels type III femoral neck fractures, a large trochanteric transverse lag screw, known as a Pauwels cannulated screw (PCS), is often added in the application of cancellous lag screw fixation, exerting an anti-vertical shear force and an anti-slip effect.12,13 Although the PCS fixation method can resist partial shear stress, the PCS is still unable to provide effective angle support and is prone to varus deformity after surgery.9,13 One study1 has confirmed that the incidence of postoperative nonunion with nail-plate fixation (8%) is significantly lower than with traditional fixation using three cancellous screws (19%) for Pauwels type III femoral neck fractures.
In recent years, Mir and Collinge14 proposed the idea that medial support of the femoral neck, similar to the proximal humerus, is particularly important in the treatment of femoral neck fractures. Effective internal femoral neck support can effectively aid in the resistance against the strong shear stress generated by the vertical femoral neck fracture so that it can be maintained in the anatomical alignment until fracture healing after fixation. Some surgeons have applied a proximal femoral locking plate (PFLP) to femoral neck fractures.8,15 Its multiple locking screws can provide stable angular multi-point fixation for the femoral head, and stress is transferred to the plate through the bone during loading, thus preventing screw loosening.16 However, the plate itself cannot pressurize the fracture. Prior to the use of the locking screw, a lag screw is required to apply pressure to the fracture end. The clinical application has obvious limitations.17 Knobe et al.18 have shown that rotational stability is very important in the treatment and anchorage mechanism as well, and the new Screw-Anchor fixation is obviously better than Sliding Hip Screw-Blade in preventing rotation and shortening of the femoral neck.
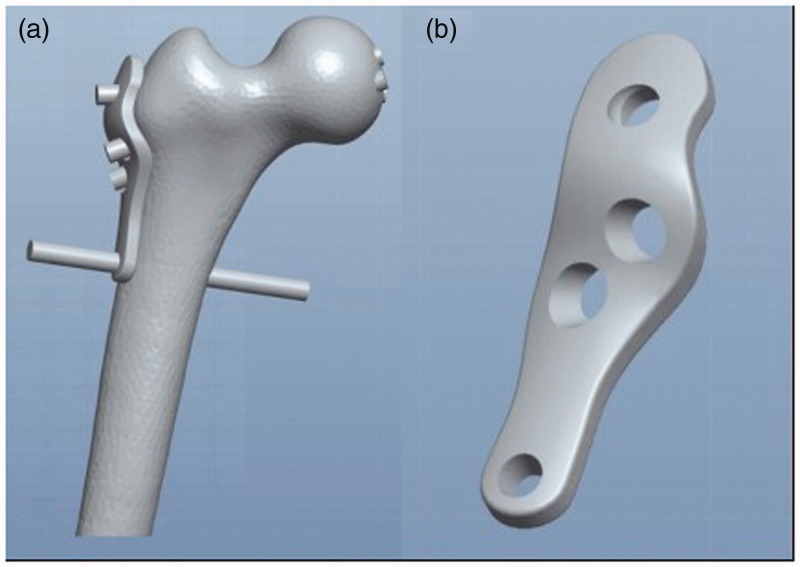
To solve this problem, we carried out anatomic studies of the femoral head, neck, and trochanter. On this basis, a new femoral neck plate (NFNP) was designed for the treatment of Pauwels type III femoral neck fractures (Figure 1). Through the first hole in the NFNP, a common cancellous screw is inserted into the trochanter, which crosses the fracture line perpendicularly. The screws through the second and third holes are placed at an angle of 135° to the vertical to fix the fracture (Figure 2). The fourth hole is designed at the farthest end to stably connect the femoral shaft with the entire construction (Figure 2–4). This system can provide not only immediate intraoperative pressure but also strong angle support. It also provides resistance against shear stress and fully integrates the advantages of cancellous nails and locking plates. In this study, the biomechanical properties of the NFNP and the PCS fixation techniques are compared by means of finite element analysis. Our aim was to prove its biomechanical stability and provide a theoretical basis for the application of the new plate in clinical practice.
Figure 1.
The plate was designed using 3-matic software. (a) 3D model of the plate and femur. (b) 3D model of the plate.
Figure 2.
The new plate and screws.
Figure 3.
Fixation model of the plate and screws. (a) The plate with screws inserted. (b) Orthotopic view of the plate on a femoral model. (c) Lateral view of the femoral model with plate and screws.
Figure 4.
Bone fracture model, with Pauwels angles of 50°, 60°, and 70°.
Materials and methods
The research was approved by the Ethics Committee of the First Affiliated Hospital of Suzhou University. The NFNP (Jiangsu Chuangsheng Medical Co., Ltd., Changzhou, China) was developed and designed by an orthopedic surgeon and a design engineer. The head of the plate is curved and wraps around the greater trochanter. At the proximal end, a hole for the insertion of a 7.3-mm partially threaded cancellous compression screw is located, in the middle are two holes for 7.3-mm half-screw locking compression screws, and at the distal end is a hole for a 5-mm locking screw. The three cancellous screws form a 3D cross-structure in the femoral head. This triangular structure not only prevents the collision of the three screws but also maintains stability (Figure 3).
This study was approved by the Institutional Review Board of Soochow University, and written informed consent from the subject was obtained prior to participation in the study. The NFNP was tested on one 25-year-old healthy male. A left lower limb computed tomography (CT) scan was performed preoperatively, and pelvic and lower limb fractures, osteoarthritis, and other bone diseases were excluded by plain films. All CT scans were performed using a 64-Slice CT Scanner (Philips, Amsterdam, Netherlands). The scanning layer was 0.7 mm thick, and a total of 651 layers of CT data (IM0-IM650) were obtained. The scanning results were stored in Digital Imaging and Communications in Medicine (DICOM) format, including information for the whole femur. Then, the Pauwels type III femoral neck fracture model was established by 3-matic software (Materialise, Leuven, Belgium), including Pauwels angles of 50°, 60°, and 70°. The osteotomy model was established by taking the osteotomy plane 10 cm above the femoral condyle as the distal osteotomy plane (Figure 4).
Using the design drawings of the NFNP and the screw drawings provided by the manufacturer, the 3D models of the plate and screws were reconstructed by using computer-aided design (CAD) software. The distal threaded portion of the screw was replaced by smooth surfaces with diameters corresponding to the designed thread diameters. The number of nodes and elements of the three fixation models, and the elastic modulus of the bones and implants are listed in Tables 1 and 2. The combination of internal fixation and bone is done at the 3-matic site. For the three Pauwels angles, three new plate fixation models and three Pauwels screw fixation models were formed (Figure 5). All of the models were meshed using the software Hypermeshing 11.0 (Altair Engineering, Inc., Troy, MI, USA).
Table 1.
Material properties used in the current study (titanium alloy, cortical, and cancellous bone).
|
Titanium alloy |
Cortical bone |
Cancellous bone |
|||
|---|---|---|---|---|---|
| E (GPa) | Poisson’s ratio | E (GPa) | Poisson’s ratio | E (GPa) | Poisson’s ratio |
| 105 | 0.35 | 16.8 | 0.3 | 0.84 | 0.2 |
Table 2.
The details of the models in this study.
| Pauwels 50° | Pauwels 60° | Pauwels 70° | |
|---|---|---|---|
| Femur (NFNP) | |||
| Elements | 277024 | 286301 | 292052 |
| Nodes | 56789 | 58748 | 59899 |
| Mesh Size | Maximum: 3 mm; minimum: 0.5 mm | ||
| Femur (PCS) | |||
| Elements | 284595 | 271462 | 268143 |
| Nodes | 58341 | 55704 | 55049 |
| Mesh Size | Maximum: 3 mm; minimum: 0.5 mm | ||
| Plate with screws (NFNP) | |||
| Elements | 27135 | 26776 | 27254 |
| Nodes | 48571 | 48062 | 49002 |
| Mesh Size | Plate: 1.3 mm; Screw: 1 mm | ||
| Screws (PCS) | |||
| Elements | 18756 | 18397 | 18875 |
| Nodes | 33667 | 32985 | 33937 |
| Mesh Size | 1 mm | ||
Figure 5.
3D images of two internal fixation methods. (a) The newly developed plate system. (b) Fixation with three cancellous screws.
We imported the assembled 3D model into ABAQUS software (Simulia, France) and generated the finite element model as previously described.19 The plates and screws were composed of the titanium alloy Ti6Al4V. In the finite element models, loads of 1400 N and 2100 N, equivalent to double and triple body weight, respectively, were introduced to the center of the femoral head.20 The force vector pointed laterally at an angle of 13° with the axis of the femoral shaft on the coronal plane, posteriorly at an angle of 8° with the shaft in the sagittal plane. Effects of VMS distribution, peak VMS, and displacement on fixation stability and fracture healing of two internal fixation methods were recorded.
Results
The mesh convergence study showed that the increase in displacement was <4% when the number of femur elements increased from 134,000 to 268,143. Numbers of elements more than 268,000 were used as the optimal mesh size and resolution (Figure 6). The mesh distribution appearance diagram in the 70° PCS model is shown in Figure 7.
Figure 6.
Results of the mesh convergence study. Displacement at the point of load application in the 70° Pauwels cannulated screw (PCS) model as a function of the number of elements.
Figure 7.
The mesh distribution appearance diagram in the 70° Pauwels cannulated screw (PCS) model.
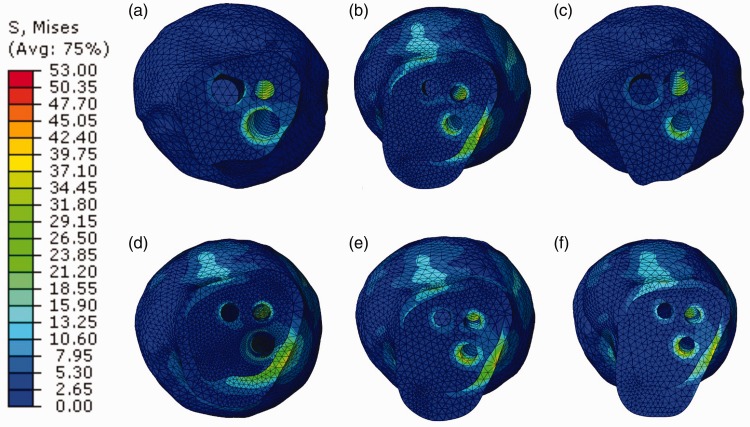
Von Mises stress (VMS) distribution and peak value of the two groups of internal fixation screws
VMS distributions were observed for the two types of internal fixation with Pauwels angles of 50°, 60°, and 70°. It was found that the stress was mainly concentrated on the screw surface close to the fracture line, and the screw closest to the femoral calcar bore the greatest stress (Figures 8, 9). The maximum stress of screws in the PCS group was higher than in the NFNP group. With increasing Pauwels angle, the maximum stress of screws in both groups increased significantly (Figure 10).
Figure 8.
Von Mises stress (VMS) distribution of two internal fixation methods under an axial load of 1400 N. (a, b, c) New femoral neck plate (NFNP) method at Pauwels angles of (a) 50°, (b) 60°, and (c) 70°. (d, e, f) Pauwels cannulated screw (PCS) method at Pauwels angles of (d) 50°, (e) 60°, and (f) 70°.
Figure 9.
Von Mises stress (VMS) distribution of two internal fixation methods under an axial load of 2100 N. (a, b, c) New femoral neck plate (NFNP) method at Pauwels angles of (a) 50°, (b) 60°, and (c) 70°. (d, e, f) Pauwels cannulated screw (PCS) method at Pauwels angles of (d) 50°, (e) 60°, and (f) 70°.
Figure 10.
Graphic demonstration of the peak stress for two internal fixation methods at different Pauwels angles under axial loads of 1400 N and 2100 N.
The displacement between fracture fragments
Fracture displacements were observed for both internal fixation methods with Pauwels angles of 50°, 60°, and 70°. The motion of the fractured end was calculated by the displacement of the two proximal nodes of the gap on the coronal plane. The fracture fragment displacement was smaller in the NFNP group than in the PCS group. Moreover, with increasing Pauwels angle, the displacement of fracture fragments in both groups increased (Figure 11).
Figure 11.
Graphic demonstration of the displacement for two internal fixation methods at different Pauwels angles under axial loads of 1400 N and 2100 N.
Von Mises stress distribution and peak stress in the femoral neck cancellous bone model
The stress distribution nephogram of the proximal cancellous bone across the femoral neck is shown in Figures 12 and 13. The contour diagram of the maximum stress in both groups is shown in Figure 14. Under different Pauwels angles, the peak stress of cancellous bone near the femoral neck was modeled to be lower in the NFNP group than in the PCS group. Moreover, with increasing Pauwels angle, the stress of proximal cancellous bone increased in both groups.
Figure 12.
Von Mises stress (VMS) distribution of the proximal femoral neck under an axial load of 1400 N. (a, b, c) New femoral neck plate (NFNP) method at Pauwels angles of (a) 50°, (b) 60°, and (c) 70°. (d, e, f) Pauwels cannulated screw (PCS) method at Pauwels angles of (d) 50°, (e) 60°, and (f) 70°.
Figure 13.
Von Mises stress (VMS) distribution of the proximal femoral neck under an axial load of 2100 N. (a, b, c) New femoral neck plate (NFNP) method at Pauwels angles of (a) 50°, (b) 60°, and (c) 70°. (d, e, f) Pauwels cannulated screw (PCS) method at Pauwels angles of (d) 50°, (e) 60°, and (f) 70°.
Figure 14.
Graphic demonstration of the peak stress of the proximal femoral neck on different internal fixation methods under increasing Pauwels angles under axial loads of 1400 N and 2100 N.
Discussion
In this study, we compared the biomechanical stability of a newly developed plate to that of the PCS method in the fixation of Pauwels type III femoral neck fractures by finite element analysis. Compared with Pauwels screw fixation, the new plate showed lower peak stress of internal fixation, less fracture block displacement, and lower peak stress of proximal cancellous bone in Pauwels type III femoral neck fracture models at three different fracture angles. With increasing Pauwels angle, the stress of the internal fixation system, the displacement of the fracture block, and the stress of the proximal cancellous bone increased significantly. This indicates that the vertical femoral neck fracture requires a more stable internal fixation system. Compared with traditional Pauwels screw fixation, internal fixation with the newly developed plate showed improved biomechanical stability.
From the perspective of biomechanics based on fracture healing, the Pauwels classification is practical.21,22 For femoral neck fractures that are Pauwels type III, it is often difficult to achieve a stable state of abduction insertion due to strong shear stresses. Therefore, this type of femoral neck fracture is often classified as a Garden type III or IV unstable femoral neck fracture. Wang et al.23 found that the greater the Pauwels angle, the higher the risk of avascular necrosis of the femoral head, presumably due to the high shear stress and instability of the fracture.
Three parallel cancellous compression screws are often used to treat femoral neck fractures. However, the incidence of complications is very high when applied to Pauwels type III femoral neck fractures.24 Because the pressure generated by the screw is not perpendicular to the fracture line, the pressure generated at the fracture end actually exerts a pulling force on the screw. The other force acting on the screw is parallel to the fracture line, and there can be a landslide effect between the fracture ends, which is likely to cause complications such as loose internal fixation, fracture nonunion, and varus deformity of the hip. Therefore, Pauwels screws were used for fixation to resist shear stress, and the effect was better than that of three parallel cancellous screws. Hawks et al.12 pointed out in their biomechanical experiments that PCS of vertical femoral neck fractures increased the stiffness by 70% and the anti-displacement strength by 43% compared with traditional parallel screws, thus enhancing the mechanical stability of fixation. Dynamic hip screw with anti-rotation is a treatment option for vertical femoral neck fractures. However, a cross-sectional survey of Orthopaedic Trauma Association (OTA) specialists showed that there is still a wide variety of opinions on the best treatment options for vertical femoral neck fractures, and shows that further research in this area may lead to more appropriate internal fixation options. For vertical femoral neck fractures, the stability of single sliding hip screw fixation is low, and the fixation strength of inverted three parallel cancellous screws and a sliding hip screw combined with cancellous screw fixation is similar.25 For comminuted fractures affecting load transfer, a sliding hip screw combined with cancellous screw fixation is the best treatment.26 Compared with three parallel cancellous screws, PCS significantly improved the mechanical properties of vertical femoral neck fractures, and the improvements seemed to be consistent with the performance of dynamic hip screws.12 The models developed in this study fully support the improved biomechanical stability of the new plate fixation technique.
Some scholars have reported the mechanical strength of locking plates in the fixation of vertical femoral neck fractures. Aminian16 reported on the use of fresh cadaveric specimens with normal bone mineral density (BMD) to examine the fixation strength of vertical femoral neck fractures with cancellous screws, sliding hip screws, dynamic condylar screws, and proximal femoral locking plates. Their results showed that proximal femoral locking plates were the most rigid, followed by dynamic condylar screws and sliding hip screws, and the three cancellous screws were the weakest. The failure load and maximum sustainable energy were the highest for proximal femoral locking plates. Under the failure load, the cancellous screw was pulled out from the femoral head, resulting in fracture of the osteotomy site, and the other groups fractured at the junction of the screw and internal fixation. Basso et al.27 considered that the addition of one locking plate with three common cancellous screws could not only reduce the micromovement of the femoral neck but also prevent rotation in the proximal and lateral and anterior and posterior directions of the fracture. This immobilization can accelerate fracture end healing and effectively reduce the risk of femoral neck shortening. Ye et al.28 also combined three common cannulated nails with an internal femoral neck block plate for the treatment of vertical unstable femoral neck fractures, and their results showed that this surgical method improved the fracture healing rate. In addition, locking plates at angles such as 95° or 135° to fix vertical femoral neck fractures in a stable manner have also had good results.29 These studies indicate the importance of stable internal femoral support for fracture healing.
For Pauwels type III femoral neck fractures, the optimal internal fixation has not yet been determined. Nevertheless, irrespective of the internal fixator, stability is the cornerstone of fracture healing. Owing to the characteristics of Pauwels type III femoral neck fractures, the traditional “sliding compression theory” of three cancellous compression screws6 is not applicable in vertical femoral neck fractures. Because the pressure is applied in the direction of the screw, no effective pressure can be applied to the fractured end. The most effective way to resist shear stress is to stabilize the angle support; therefore, we designed this new plate.
Our new plate’s advantages are the following: (1) It provides resistance against shear stress. The first hole at the proximal end of the plate is designed as an ordinary cancellous pressure hole. The plate head is curved forward because there is sufficient bone mass above the anterior neck of the femur to allow nailing. The general cancellous nail is oriented in front of the femoral head and does not touch the second and third locking nails. (2) The second and third holes in the proximal end of the plate are locking holes. The locking screw is oriented at an angle of 135° to the nail fixation, providing strong angular support and effectively maintaining the fracture in position. (3) The locking screw is also a 7.3-mm cancellous partially threaded locking screw. The thread diameter of the locking screw tail increases, exerting a pressurizing effect in the process of locking. (4) A locking hole with a diameter of 5 mm is designed at the bottom end of the new plate. By locking screw fixation, the plate can be fixed to the femoral shaft so that the femoral shaft, the plate, and the femoral neck are connected and fixed. At the same time, the lateral wall of the femur is strengthened by the plate, which is a major advantage for osteoporosis patients. (5) One study30 has shown that if the femoral neck is shortened more than 5 mm, it has a large negative impact on the patient’s hip joint function. The new plate significantly reduces the risk of femoral neck shortening and improves postoperative hip joint function.
The major limitation of our study is that our results have not been verified by animal experiments or clinical experiments. However, our aim was to explore possibilities to improve treatment. In the future, more realistic biomechanical experiments and clinical trials will need to be conducted.
Conclusions
In this study, a new plate was designed to treat Pauwels type III femoral neck fractures. Through finite element model analysis, we proved that the new plate is superior to the Pauwels screw with regard to biomechanical stability, so this plate provides a new option for the treatment of vertical femoral neck fractures.
List of abbreviations
NFNP: new femoral neck plate
VMS: von Mises stress
PCS: Pauwels cannulated screw
CAD: computer-aided design
BMD: bone mineral density.
Acknowledgements
We thank LetPub (www.letpub.com) for linguistic assistance during the preparation of this manuscript.
Authors' contributions
G.W. and Y.T. conceived and designed the study, analyzed the data, and wrote the manuscript. G.W. collected data. Y.T. and X.H.W. contributed to the data curation and preparation of the original draft. H.L.Y. supervised the study, analyzed the data, and revised the manuscript. All authors read and approved the final manuscript.
Availability of data and material
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Written informed consent for publication of their clinical details and clinical images was obtained from the patients.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval and consent to participate
This research was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University.
Funding
This publication was partially funded by the Zhejiang Medical Science Foundation of China (2019KY682).
ORCID iD
Huilin Yang https://orcid.org/0000-0001-9679-2759
References
- 1.Liporace F, Gaines R, Collinge Cet al. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am 2008; 90: 1654–1659. [DOI] [PubMed] [Google Scholar]
- 2.Marsh JL, Slongo TF, Agel Jet al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007; 21: S1–S133. [DOI] [PubMed] [Google Scholar]
- 3.Kunapuli SC, Schramski MJ, Lee ASet al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma 2015; 29: 144–150. [DOI] [PubMed] [Google Scholar]
- 4.Huang HK, Su YP, Chen CMet al. Displaced femoral neck fractures in young adults treated with closed reduction and internal fixation. Orthopedics 2010; 33: 873. [DOI] [PubMed] [Google Scholar]
- 5.Haidukewych GJ, Rothwell WS, Jacofsky DJet al. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am 2004; 86-A: 1711–1716. [DOI] [PubMed] [Google Scholar]
- 6.Yang JJ, Lin LC, Chao KHet al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am 2013; 95: 61–69. [DOI] [PubMed] [Google Scholar]
- 7.Parker MJ, Porter KM, Eastwood DMet al. Intracapsular fractures of the neck of femur. Parallel or crossed garden screws? J Bone Joint Surg Br 1991; 73: 826–827. [DOI] [PubMed] [Google Scholar]
- 8.Wang Z, Yin Y, Li Qet al. Comparison of early complications between the use of a cannulated screw locking plate and multiple cancellous screws in the treatment of displaced intracapsular hip fractures in young adults: a randomized controlled clinical trial. J Orthop Surg Res 2018; 13: 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson JP, Borenstein TR, Waryasz GRet al. Vertically oriented femoral neck fractures: a biomechanical comparison of 3 fixation constructs. J Orthop Trauma 2017; 31: 363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker MJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am 2009; 91: 490–491; author reply 1. [PubMed] [Google Scholar]
- 11.Gumustas SA, Tosun HB, Agir Iet al. Influence of number and orientation of screws on stability in the internal fixation of unstable femoral neck fractures. Acta Orthop Traumatol Turc 2014; 48: 673–678. [DOI] [PubMed] [Google Scholar]
- 12.Hawks MA, Kim H, Strauss JEet al. Does a trochanteric lag screw improve fixation of vertically oriented femoral neck fractures? A biomechanical analysis in cadaveric bone. Clin Biomech (Bristol, Avon) 2013; 28: 886–891. [DOI] [PubMed] [Google Scholar]
- 13.Hoshino CM, Christian MW, O'Toole RVet al. Fixation of displaced femoral neck fractures in young adults: fixed-angle devices or Pauwel screws? Injury 2016; 47: 1676–1684. [DOI] [PubMed] [Google Scholar]
- 14.Mir H, Collinge C. Application of a medial buttress plate may prevent many treatment failures seen after fixation of vertical femoral neck fractures in young adults. Med Hypotheses 2015; 84: 429–433. [DOI] [PubMed] [Google Scholar]
- 15.Wang G, Tang Y, Wang Bet al. Minimally invasive open reduction combined with proximal femoral hollow locking plate in the treatment of Pauwels type III femoral neck fracture. J Int Med Res 2019; 47: 3050–3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aminian A, Gao F, Fedoriw WWet al. Vertically oriented femoral neck fractures: mechanical analysis of four fixation techniques. J Orthop Trauma 2007; 21: 544–548. [DOI] [PubMed] [Google Scholar]
- 17.Berkes MB, Little MT, Lazaro LEet al. Catastrophic failure after open reduction internal fixation of femoral neck fractures with a novel locking plate implant. J Orthop Trauma 2012; 26: e170–e176. [DOI] [PubMed] [Google Scholar]
- 18.Knobe M, Altgassen S, Maier KJet al. Screw-blade fixation systems in Pauwels three femoral neck fractures: a biomechanical evaluation. Int Orthop 2018; 42: 409–418. [DOI] [PubMed] [Google Scholar]
- 19.Li J, Wang M, Li Let al. Finite element analysis of different configurations of fully threaded cannulated screw in the treatment of unstable femoral neck fractures. J Orthop Surg Res 2018; 13: 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergmann G, Deuretzbacher G, Heller Met al. Hip contact forces and gait patterns from routine activities. J Biomech 2001; 34: 859–871. [DOI] [PubMed] [Google Scholar]
- 21.Collinge CA, Mir H, Reddix R. Fracture morphology of high shear angle “vertical” femoral neck fractures in young adult patients. J Orthop Trauma 2014; 28: 270–275. [DOI] [PubMed] [Google Scholar]
- 22.Luttrell K, Beltran M, Collinge CA. Preoperative decision making in the treatment of high-angle “vertical” femoral neck fractures in young adult patients. An expert opinion survey of the Orthopaedic Trauma Association's (OTA) membership. J Orthop Trauma 2014; 28: e221–e225. [DOI] [PubMed] [Google Scholar]
- 23.Wang SH, Yang JJ, Shen HCet al. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury 2015; 46: 1969–1974. [DOI] [PubMed] [Google Scholar]
- 24.Goffin JM, Pankaj P, Simpson AH. The importance of lag screw position for the stabilization of trochanteric fractures with a sliding hip screw: a subject-specific finite element study. J Orthop Res 2013; 31: 596–600. [DOI] [PubMed] [Google Scholar]
- 25.Luttrell K, Beltran M, Collinge CA. Preoperative decision making in the treatment of high-angle “vertical” femoral neck fractures in young adult patients an expert opinion survey of the Orthopaedic Trauma Association's (OTA) membership. J Orthop Trauma 2014; 28: E221–E225. [DOI] [PubMed] [Google Scholar]
- 26.Kemker B, Magone K, Owen Jet al. A sliding hip screw augmented with 2 screws is biomechanically similar to an inverted triad of cannulated screws in repair of a Pauwels type-III fracture. Injury 2017; 48: 1743–1748. [DOI] [PubMed] [Google Scholar]
- 27.Basso T, Klaksvik J, Foss OA. Locking plates and their effects on healing conditions and stress distribution: a femoral neck fracture study in cadavers. Clin Biomech (Bristol, Avon) 2014; 29: 595–598. [DOI] [PubMed] [Google Scholar]
- 28.Ye Y, Chen K, Tian KWet al. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: surgical technique and preliminary results. Injury 2017; 48: 2189–2193. [DOI] [PubMed] [Google Scholar]
- 29.Zhu F, Liu G, Shao HGet al. Treatment of femoral neck fracture with percutaneous compression plate: preliminary results in 74 patients. Orthop Surg 2015; 7: 132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zlowodzki M, Ayieni O, Petrisor BAet al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma 2008; 64: 163–169. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.