Short abstract
Objective
This study was performed to explore the effect of intra-articular injection of autologous platelet-rich plasma (PRP) on refractory pain after low-grade medial collateral ligament (MCL) injury.
Methods
In total, 52 patients with refractory pain after low-grade knee MCL injury were treated by intra-articular injection of autologous PRP. Every patient received a 5-mL intra-articular injection of autologous PRP once weekly for 3 weeks. All patients were evaluated by the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form score before treatment and 1, 3, and 6 months after treatment. Magnetic resonance imaging of the knee was performed to observe the healing of the MCL injury 6 months after treatment.
Results
After one injection, the patients’ pain was greatly decreased and they stopped taking nonsteroidal anti-inflammatory drugs. The IKDC Subjective Knee Evaluation Form scores were significantly better after than before treatment; however, there were no significant differences among the various post-treatment time points. Magnetic resonance imaging showed that the low-grade MCL injury had completely healed, and no edema was present around the MCL.
Conclusions
Intra-articular injection of autologous PRP is an effective treatment for refractory pain after low-grade MCL injury.
Keywords: Knee, pain, medial collateral ligament, injury, platelet-rich plasma, intra-articular injection
Introduction
Medial collateral ligament (MCL) injury, which is caused by valgus stress, is the most common knee ligament injury. According to the criteria established by Bergfeld,1 MCL injury can be classified into three grades of severity: grade I, tenderness over the MCL with no instability; grade II, tenderness over the MCL with valgus instability as indicated by a <10-mm opening at 25 to 30 degrees of flexion; and grade III, complete disruption of the ligament with resultant instability in full extension. Because the MCL has great potential to heal after injury, conservative therapy is recommended for most grade I and II MCL injuries and provides excellent outcomes.2,3 In a subgroup of patients, however, conservative measures are ineffective and medial knee pain persists, sometimes for even longer than 18 months. Tearing of the deep part of the MCL has been considered the cause of the refractory knee pain after low-grade MCL injury.4 Refractory pain after low-grade knee MCL injury seriously affects knee joint function and quality of daily life. Therefore, a new treatment is needed for this subgroup of patients.
Autologous platelet-rich plasma (PRP) is an autologous blood product containing highly concentrated platelets and multiple cell growth factors.5 PRP has been widely used in the treatment of orthopedic diseases such as osteoarthritis and musculature injury. Many of the growth factors found in PRP are involved in the tissue healing process by promoting cell recruitment, proliferation, and angiogenesis.6 Previous research has suggested that PRP increases the blood supply and nutrients required to regenerate the injured tissue, particularly in chronic tendinopathies in which the tissue healing processes are hampered by the local biologic microenvironment.7,8
In this study, intra-articular injections of autologous PRP were used to treat this subgroup of patients, and the effect of autologous PRP on refractory pain after low-grade MCL injury was explored.
Patients and methods
Patients
This study included consecutive patients with a ≥3-month history of chronic knee pain after knee injury who were diagnosed and treated at our hospital from October 2012 to December 2016. In all patients, injury of the deep portion of the MCL was identified by magnetic resonance imaging (MRI). All patients underwent failed conservative treatment involving either rest and physiotherapy or one or more corticosteroid injections. Each patient provided written informed consent, and the study was approved by the institutional review board. The inclusion criterion was a history of injury and chronic knee pain for >3 months associated with injury of the deep portion of the MCL as diagnosed by MRI and physical examination (marked knee tenderness on the medial side of the knee, especially on the tibial or femoral attachment of the MCL, with normal range of motion and knee stability confirmed by the anterior drawer test, posterior drawer test, varus stress test, and valgus stress test). The exclusion criteria were knee osteoarthritis with a history of either acute injury or no injury; grade III MCL injury or other combined injuries requiring surgical treatment; systemic conditions such as infection, rheumatoid arthritis, autoimmune diseases, or tumors; and contraindications for PRP, a hemoglobin concentration of <11 g/L, or a platelet count of <150 × 109/L.
Preparation of autologous PRP
A 5.0-mL sample of autologous leukocyte-reduced PRP was obtained from 20 mL of whole blood using a preparation kit (MyCells; Kaylight, Tel Aviv, Israel) according to the standard protocol. Whole blood obtained from the elbow vein was placed into two 15-mL conical tubes (BD Falcon; BD Biosciences, Franklin Lakes, NJ, USA); each tube contained 10 mL of blood with 1 mL of citrate phosphate dextrose adenine solution and was centrifuged for 10 minutes at 1000 × g. Next, 5 mL of the supernatant plasma above the red blood cell layer in each tube was aspirated, and the combined 10 mL of plasma supernatant from the two tubes was placed into another conical tube for centrifugation under the same conditions. Finally, 5 mL of non-activated PRP was obtained by aspiration from the layer above the white blood cells. All PRP was prepared by the same doctor.
Treatment of patients
The autologous PRP was injected into the knee joint using a 30-G needle after the skin had been sterilized with topical 10% povidone–iodine solution. Every patient received a 5-mL intra-articular injection of autologous PRP once weekly for a total of three injections. All intra-articular injections were performed by the same doctor. The knee was bandaged but not completely immobilized.
The patients were advised that their nonsteroidal anti-inflammatory drugs could be discontinued by themselves if the pain was relieved. Range-of-motion exercises were started, and weight bearing was gradually introduced. Total weight bearing was permitted if the patient was pain-free.
Clinical evaluation
The patients were examined clinically and evaluated with the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form by the same examiner before treatment and 1, 3, and 6 months after treatment. The IKDC Subjective Knee Evaluation Form is a knee-specific patient-reported outcome measure that is scored by summing the scores for the individual items and transforming them to a scale that ranges from 0 to 100. The transformed score is interpreted as a measure of function; higher scores represent higher levels of function and lower levels of symptoms. The MCL was observed by MRI scans before treatment and 6 months after treatment by an experienced radiologist using the same MRI monitor. Finally, the visual analog scale (VAS) score was applied to assess patients’ pain before treatment and at 1 week, 1 month, 3 months, and 6 months after treatment.
Statistical analysis
All data analyses were performed using SPSS version 21.0 software (IBM Corp., Armonk, NY, USA). The IKDC Subjective Knee Evaluation Form scores at the various time points are presented as mean and standard deviation and were compared by one-way analysis of variance using the Bonferroni test. A probability (P) value of <0.05 was considered statistically significant.
Results
General condition of the patients
In total, 52 patients were included in this study (22 men, 30 women; mean age, 36.5 ± 5.26 years; age range, (20 to 45 years). The mean time from the injury to PRP therapy was 6.5 ± 1.11 months (range, 3.5 to 12 months). The patients stated that the pain was relieved week after the first intra-articular injection of PRP. Physical examination showed a significant reduction in local tenderness. One week after treatment, all patients had autonomously discontinued nonsteroidal anti-inflammatory drugs, and two-thirds of patients were able to perform weight-bearing activities without pain. When the patients came to the hospital to receive the third intra-articular injection, they were able to walk with weight without pain, their gait had substantially improved, and their morning knee stiffness was obviously reduced.
IKDC Subjective Knee Evaluation Form scores
Significant improvements in the IKDC Subjective Knee Evaluation Form scores were observed between the pretreatment period (61.03 ± 5.07 points) and various post-treatment time points (86.63 ± 4.67 points at 1 month, 87.85 ± 4.43 points at 3 months, and 89.15 ± 4.08 points at 6 months; P < 0.05). However, there were no statistically significant differences among the various post-treatment time points (Table 1).
Table 1.
IKDC Subjective Knee Evaluation Form scores at various time points.
| Time point | n | IKDC scores |
|---|---|---|
| Pretreatment | 52 | 61.03 ± 10.07 |
| 1 month post-treatment | 52 | 86.63 ± 7.67* |
| 3 months post-treatment | 52 | 87.85 ± 9.43* |
| 6 months post-treatment | 52 | 89.15 ± 7.08* |
| F | 126.00 | |
| P | 0.00 |
IKDC Subjective Knee Evaluation Form scores are presented as mean ± standard deviation.
IKDC, International Knee Documentation Committee.
*P < 0.05 vs. pretreatment.
VAS score
Significant decreases in the VAS score were observed between the pretreatment period (6.58 ± 0.82 points) and various post-treatment time points (2.67 ± 0.86 points at 1 week, 1.19 ± 0.79 points at 1 month, 1.02 ± 0.85 points at 3 months, and 1.00 ± 0.86 points at 6 months; P < 0.05). However, there were no significant differences among the scores at 1, 3, and 6 months post-treatment (Table 2).
Table 2.
VAS scores at various time points.
| Time point | n | VAS score |
|---|---|---|
| Pretreatment | 52 | 6.58 ± 0.82 |
| 1 week post-treatment | 52 | 2.67 ± 0.86* |
| 1 month post-treatment | 52 | 1.19 ± 0.79*,# |
| 3 months post-treatment | 52 | 1.02 ± 0.85*,# |
| 6 months post-treatment | 52 | 1.00 ± 0.86*,# |
| F | 421.86 | |
| P | 0.00 |
VAS scores are presented as mean ± standard deviation.
VAS, visual analog scale.
*P < 0.05 vs. pretreatment.
#P < 0.05 vs. 1 week.
MRI detection
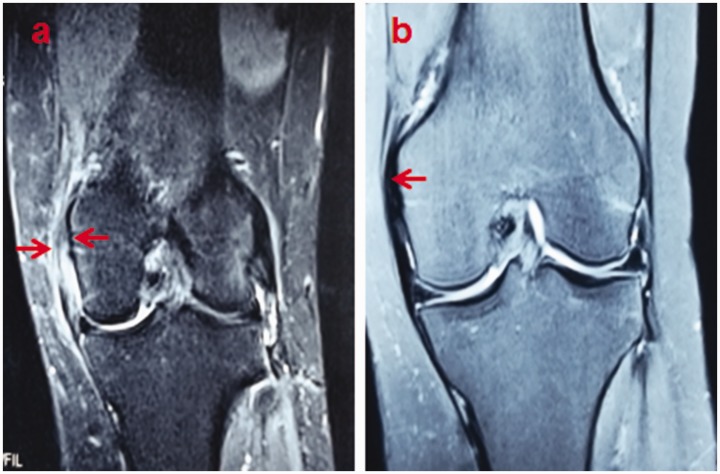
MRI was performed to examine the MCL before treatment and 6 months after treatment. Pretreatment MRI revealed loose structure of the deep layer of the MCL and edema around the injured ligament (Figure 1(a)). The damaged MCL completely healed and no edema around the MCL was observed at 6 months post-treatment (Figure 1(b)).
Figure 1.
Magnetic resonance images of the medial collateral ligament (MCL). (a) Coronal section, T2-weighted with selective fat-suppression image. Low-grade injury of the deep layer of the MCL and edema around the injured ligament were found before treatment (red arrows). (b) Coronal section, T2-weighted with selective fat-suppression image. The damaged MCL had completely healed and no edema was present around the MCL at 6 months post-treatment (red arrow).
Discussion
The effect of intra-articular injection of PRP in orthopedics is unclear, although the application of PRP is increasing rapidly. Many recent papers have reported that PRP is of benefit in the treatment of chronic tendon injuries, and many experimental studies have evaluated the effect of PRP on healing of MCL injury in animal models.9–11 Yoshioka et al.9 evaluated the effect of PRP on MCL healing in a rabbit model and found that PRP treatment promoted healing of the MCL. In a rat model of MCL injury, Amar et al.10 found no evidence to support a benefit of PRP for MCL healing in the acute stage. LaPrade et al.11 found that high doses of PRP decreased the quality of repair tissue in a rabbit model. A recent case report showed that PRP significantly shortened the healing time of a patient with an acute simple MCL injury (Grade 3).12 In another recent case report, three patients with a low-grade simple MCL injury of >8-month duration were treated by PRP.13 Three months later, all patients had returned to their sport activities without symptoms, and complete healing of the ligament was confirmed by MRI.
In the present study, the patients’ refractory pain was controlled, and all patients autonomously stopped their nonsteroidal anti-inflammatory drugs 1 week after intra-articular injection of PRP. Many studies have shown the benefit of PRP injections in eliminating chronic pain associated with other tendon injuries.14,15 In the present study, the MCL injury duration was >3 months and the patients had experienced chronic knee pain for >3 months. Jones et al.4 demonstrated that in patients with an incomplete MCL tear for which conservative treatment failed, refractory pain was caused by deep injury of the MCL. Narvani et al.16 also found that a small group of patients with MCL injury did not respond to nonoperative treatment and developed persistent symptoms. The surgical finding in this group of patients was non-healing of the deep MCL tear, allowing the synovial fluid to pass through the torn deep MCL and infiltrate the area surrounding the injury site. Large numbers of chronic inflammatory cytokines are present in the injured area and intra-articular fluid. The knee is slightly unstable in patients with injury of the deep portion of the MCL, and these patients cannot perform intense activities because of pain. Additionally, these patients walk with partial weight bearing, indicating that the pain is caused by chronic inflammation around the torn MCL rather than by instability of the knee. In the present study, the pain was quickly alleviated, possibly because of the anti-inflammatory effect of PRP. Huang et al.17 reported that the serum concentrations of inflammatory cytokines were greatly down-regulated after PRP treatment compared with placebo treatment in patients with knee osteoarthritis. PRP has anti-inflammatory properties through its effects on the canonical nuclear factor κB signaling pathway.18,19
In this study, the PRP was injected into the joint instead of the pain point. Intra-articular injection of PRP may be more effective than pain point injection because PRP acts directly on the injury site and more fully reaches the surrounding edematous tissue through the injury site. Pain point injection often requires multiple injections because several pain points are present; however, only one intra-articular injection is needed. Robinson et al.20 stated that the deep MCL is inseparable from the joint capsule. The synovial fluid passes through the torn deep MCL and infiltrates the area surrounding the injury site, thereby delaying or preventing healing. The most important finding in our study is the healing of the torn deep portion of the MCL and the elimination of edema of the surrounding soft tissue at 6 months after intra-articular injection of PRP. This finding indicates that PRP may accelerate the healing process of chronic MCL injury by eliminating the chronic inflammation around the damaged ligament. Intra-articular injection of PRP not only promoted healing by improving the microenvironment of the surrounding tissues but also affected the inflammatory cytokines in the joint. However, further studies with larger numbers of patients and both untreated and alternately treated groups are warranted to confirm the present results. The related mechanisms should also be further studied.
Conclusion
Intra-articular injection of autologous PRP is an effective treatment for refractory pain after low-grade MCL injury. Intra-articular injection of PRP may serve as a treatment option for chronic MCL injury.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Guoyou Zou https://orcid.org/0000-0002-9099-6168
References
- 1.Bergfeld J. Symposium: functional rehabilitation of isolated medial collateral ligament sprains. First-, second-, and third-degree sprains. Am J Sports Med 1979; 7: 207–209. [DOI] [PubMed] [Google Scholar]
- 2.Varelas AN, Erickson BJ, Cvetanovich GL, et al. Medial collateral ligament reconstruction in patients with medial knee instability: a systematic review. Orthop J Sports Med 2017; 5: 2325967117703920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Indelicato PA. Isolated medial collateral ligament injuries in the knee. J Am Acad Orthop Surg 1995; 3: 9–14. [DOI] [PubMed] [Google Scholar]
- 4.Jones L, Bismil Q, Alyas F, et al. Persistent symptoms following non operative management in low grade MCL injury of the knee - The role of the deep MCL. Knee 2009; 16: 64–68. [DOI] [PubMed] [Google Scholar]
- 5.Galatz LM, Gerstenfeld L, Heber-Katz E, et al. Tendon regeneration and scar formation: the concept of scarless healing. J Orthop Res 2015; 33: 823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andia I, Rubio-Azpeitia E, Maffulli N. Platelet-rich plasma modulates the secretion of inflammatory/angiogenic proteins by inflamed tenocytes. Clin Orthop Relat Res 2015; 473: 1624–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Vos RJ, Weir A, van Schie HT, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA 2010; 303: 144–149. [DOI] [PubMed] [Google Scholar]
- 8.Smith RW, Papadopolous E, Mani R, et al. Abnormal microvascular responses in a lateral epicondylitis. Br J Rheumatol 1994; 33: 1166–1168. [DOI] [PubMed] [Google Scholar]
- 9.Yoshioka T, Kanamori A, Washio T, et al. The effects of plasma rich in growth factors (PRGF-Endoret) on healing of medial collateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1763–1769. [DOI] [PubMed] [Google Scholar]
- 10.Amar E, Snir N, Sher O, et al. Platelet-rich plasma did not improve early healing of medial collateral ligament in rats. Arch Orthop Trauma Surg 2015; 135: 1571–1577. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade RF, Goodrich LR, Phillips J, et al. Use of platelet-rich plasma immediately after an injury did not improve ligament healing, and increasing platelet concentrations was detrimental in an in vivo animal model. Am J Sports Med 2018; 46: 702–712. [DOI] [PubMed] [Google Scholar]
- 12.Bagwell MS, Wilk KE, Colberg RE, et al. The use of serial platelet rich plasma injections with early rehabilitation to expedite grade iii medial collateral ligament injury in a professional athlete: a case report. Int J Sports Phys Ther 2018; 13: 520–525. [PMC free article] [PubMed] [Google Scholar]
- 13.Yoshida M, Marumo K. An autologous leukocyte-reduced platelet-rich plasma therapy for chronic injury of the medial collateral ligament in the knee: a report of 3 successful cases. Clin J Sport Med 2019; 29: e4–e6. [DOI] [PubMed] [Google Scholar]
- 14.Rha DW, Park GY, Kim YK, et al. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil 2013; 27: 113–122. [DOI] [PubMed] [Google Scholar]
- 15.Houck DA, Kraeutler MJ, Thornton LB, et al. Treatment of lateral epicondylitis with autologous blood, platelet-rich plasma, or corticosteroid injections: a systematic review of overlapping meta-analyses. Orthop J Sports Med 2019; 7: 2325967119831052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Narvani A, Mahmud T, Lavelle J, et al. Injury to the proximal deep medial collateral ligament: a problematical subgroup of injuries. J Bone Joint Surg Br 2010; 92: 949–953. [DOI] [PubMed] [Google Scholar]
- 17.Huang G, Hua S, Yang T, et al. Platelet-rich plasma shows beneficial effects for patients with knee osteoarthritis by suppressing inflammatory factors. Exp Ther Med 2018; 15: 3096–3102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bendinelli P, Matteucci E, Dogliotti G, et al. Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: mechanisms of NF-kappaB inhibition via HGF. J Cell Physiol 2010; 225: 757–766. [DOI] [PubMed] [Google Scholar]
- 19.Anitua E, Sanchez M, Nurden AT, et al. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford) 2007; 46: 1769–1772. [DOI] [PubMed] [Google Scholar]
- 20.Robinson JR, Bull AM, Amis AA. Structural properties of the medial collateral ligament complex of the human knee. J Biomech 2005; 38: 1067–1074. [DOI] [PubMed] [Google Scholar]