Short abstract
Objective
Several investigations have shown that the level of fibrinogen (Fg) is associated with the susceptibility to dementia and is usually affected by polymorphisms in its gene. Our study aimed to investigate the relationship between Fg level and the fibrinogen β (FGB) −148C/T gene polymorphism in patients with Alzheimer’s disease (AD) and vascular dementia (VaD).
Methods
The study included 64 AD patients, 72 VaD patients, and 56 healthy controls (HC). Plasma Fg level was detected by turbidimetry. Among the participants, 64 AD patients, 52 VaD patients, and 56 HC underwent FGB −148C/T polymorphism analysis using restriction fragment length polymorphism-PCR.
Results
Plasma Fg was significantly higher in AD and VaD groups than in HC. The AD and VaD patients with FGB −148 TT genotype had significantly higher plasma Fg than those with CC or CT genotypes. The distribution of CC and CT+TT genotypes differed in the three groups, with the frequency of CT+TT genotypes being higher in AD patients than in the HC group.
Conclusions
Plasma Fg level was significantly correlated with AD and VaD and related to the −148C/T polymorphism of FGB. The TT+CT genotypes and the distribution frequency of the T allele may be related to AD.
Keywords: β-Fibrinogen, Alzheimer’s disease, vascular dementia, −148C/T, gene polymorphism, FGB
Introduction
As the global population ages, the incidence of dementia is increasing each year.1 Dementia seriously affects patients’ quality of life and has become a focus of domestic and international research. Alzheimer’s disease (AD) and vascular dementia (VaD) are the two most common types of dementia.2 Previous epidemiological, molecular biology, pathology, and imaging studies have provided evidence indicating that vascular risk factors play an important role in the pathogenesis of AD and VaD. People with higher fibrinogen (Fg) levels often have an increased risk of cardiovascular disease and stroke. Fibrinogen, as a vascular risk factor, can be used as a biomarker for ischemic atherothrombotic stroke, coronary heart disease, peripheral arterial disease, and atherosclerosis.3–7 Evidence from a wide range of sources has suggested that people with higher Fg levels also have an increased risk of dementia,8,9 and Fg level is positively correlated with the risk of AD and VaD.8 Therefore, Fg, as a common vascular risk factor, may contribute to VaD and AD, and both forms of dementia seem to have similar pathogenesis.10,11 In addition, polymorphisms in the fibrinogen β-chain gene (FGB) are strongly associated with plasma Fg level.6,12 Thus, FGB gene polymorphisms might contribute to susceptibility of dementia by affecting plasma Fg level.
VaD is often characterized by vascular pathology, a procoagulant state, and chronic inflammation. The mechanisms underlying these abnormalities in AD are not clear.13 The level of Fg is significantly higher in AD patients compared with controls in experimental animal models.14 Depletion of factor XII (FXII) in AD mice inhibits the cleavage of high-molecular-weight kininogen in plasma, resulting in reduced neuroinflammation, fibrinogen deposition, and neurodegeneration in the brain. Moreover, FXII-depleted AD mice show better cognitive function than untreated AD mice, which indicates that Fg is involved in the occurrence of AD.15 A significant association between the level of Fg and VaD has been found.16 Besides its prothrombotic effect, Fg seems to have other destructive roles in developing microvascular dysfunctions, including changes in vascular reactivity and permeability. Increased permeability of brain microvessels has a profound effect because it may lead to cerebrovascular remodeling and result in memory reduction.17 Therefore, Fg may be a risk factor for both AD and VaD. The purpose of this study was to evaluate the relationship between Fg, and its regulatory gene, with AD and VaD.
Materials and methods
Patients
A total of 136 patients, including 64 AD patients and 72 VaD patients, were recruited from the Neurological Outpatient Department in our hospital from December 2005 to December 2007 and enrolled in the study. In addition, 56 healthy controls (HC) without cerebrovascular disease or cognitive dysfunction were randomly selected during the same period. Table 1 shows the basic information of the enrolled patients and HC. Among the participants, 172 (64 AD patients, 52 VaD patients, and 56 HC) underwent FGB −148C/T genetic polymorphism analysis using restriction fragment length polymorphism-polymerase chain reaction (RFLP-PCR) analysis. All patients were from Northern China.
Table 1.
General information of the enrolled subjects.
| Characteristics | AD (n = 64) | VaD (n = 72) | HC (n = 56) | χ2 | P-value |
|---|---|---|---|---|---|
| Age, years | 70.10 ± 9.75 | 68.41 ± 9.82 | 68.11 ± 9.94 | 0.644 | 0.527 |
| Education, years | 12.03 ± 3.75 | 11.65 ± 3.24 | 12.08 ± 3.36 | 2.472 | 0.085 |
| Male, n (%) | 30 (46.8) | 38 (52.8) | 32 (57.1) | 1.284 | 0.526 |
| MMSE (score) | 17.60 ± 7.93 | 17.60 ± 7.56 | 28.43 ± 1.72 | 33.678 | <0.001 |
| CDR (score) | 1.63 ± 0.80 | 1.68 ± 0.80 | 0.00 ± 0.00 | 50.238 | <0.001 |
| CDT (score) | 1.80 ± 1.20 | 1.67 ± 1.19 | 4.00 ± 0.00 | 55.814 | <0.001 |
AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls; MMSE, mini-mental state examination; CDR, Clinical Dementia Rating scale; CDT, clock drawing test.
The study was approved by the Ethics Committee for Medical Research at Tianjin Medical University General Hospital. All patients agreed to provide blood for genetic testing and signed written informed consent.
The inclusion criteria were as follows: (1) patients who completed a detailed clinical questionnaire on histories of cerebrovascular diseases, hypertension, diabetes, coronary heart disease, smoking, drinking, family history, eating habits; and (2) underwent a physical examination (comprehensive neurological examination) combined with clinical application to mini-mental state examination (MMSE) and clock drawing test (CDT) to screen those with cognitive dysfunction. Patients with dementia had an MMSE score between 4 and 24. Severity of dementia was determined by the Clinical Dementia Rating (CDR) scale. The diagnostic criteria for AD were in line with the NINCDS-ADRDA criteria and DSM-IV-R criteria. The diagnostic criteria for VaD5,18 included the State of California Alzheimer’s Disease Diagnostic and Treatment Centers criteria for probable and possible ischemic vascular dementia, the International Classification of Diseases, Tenth Edition (ICD-10) criteria for VaD, the National Institute of Neurological Disorders and Stroke, and the Association Internationale pour la Recherche et l’Enseignement en Neurosciences criteria for probable and possible VaD. All these criteria were in accordance with the VaD diagnostic criteria of the Chinese Medical Association Branch of Neurology.
Patients with cerebrovascular disease, other neurodegenerative dementia, normotensive hydrocephalus, epilepsy, infection, depression, systemic metabolic disease, family history of dementia, undernourished patients, and patients who did not cooperate with blood collection were excluded. All participants underwent brain examination and were excluded if they had history of head injury; tumor; liver or kidney dysfunction; thyroid deficiency; chronic malnutrition; recent use of folic acid and B vitamins; chronic alcoholism; substance abuse; disturbance of consciousness; mental disorders (Hamilton Depression Rating Scale ≥15); or other diseases that can cause dementia.
Methods
Plasma fibrinogen was measured using the Clauss fibrinogen assay. In brief, 2 mL of venous blood was withdrawn from the cubital vein of participants in the early morning. The blood was placed in a tube containing 0.2 mL of sodium citrate for 1 hour, centrifuged at 1006.2 × g for 10 minutes, and analyzed using an automatic blood coagulation analyzer.
For FGB genotyping, 2 mL of blood was mixed evenly in an EDTA anticoagulation tube and DNA was extracted using a genomic DNA extraction kit (SBS, Shanghai, China) as described by the manufacturer. Genotyping for FGB polymorphisms was performed by PCR amplification using primers 5′-CCTAACTTCCCATCATTTTGTC-3′ and 5′-ATGGTTTTAAGTTTGTGGAAGC-3′ and restriction enzyme analysis. The PCR reaction was performed in a 20-µL system containing 1 µL of genomic DNA template, 1 µL of each specific primer (TaKaRa, Dalian, China), 0.25 µL of Taq DNA polymerase (TaKaRa), 2 µL of 10× Mg2+-free PCR buffer (TaKaRa), and 1.5 µL of dNTP mixture (TaKaRa). The PCR reaction condition was 5 minutes of pre-denaturation at 95°C followed by 35 cycles of 30 s at 94°C, 30 s at 50°C, 45 s at 72°C, and a final 10 minutes at 72°C. The content and purity of PCR products were analyzed using absorption at 260 and 280 nm on an ultraviolet spectrophotometer (Bio-Rad, Hercules, CA, USA). The integrity of DNA was observed by 0.8% agarose gel electrophoresis (Sigma, Kanagawa, Japan). The amplified products were digested with HinfI (TaKaRa), electrophoresed on 3% agarose gels (Sigma), stained with DL2000 (TaKaRa), and visualized under ultraviolet light (Bio-Rad).
Statistical methods
Statistical analysis was performed using SPSS version 11.5 (IBM Corp., Armonk, NY, USA). Genotype frequencies were estimated by gene counting. The genotype distributions in all groups were compatible with Hardy–Weinberg expectations. Measurement data were presented as mean ± standard deviations and compared using Student’s t-test. Comparison of mean values among multiple groups was performed using the least significant difference (LSD) t-test. Enumeration data were presented as rate (%) and compared using the χ2 test. Pearson correlation analysis was used to analyze correlations between single factors. Spearman correlation analysis was used for ranked data. The linear regression model was used to analyze the correlation between Fg levels and diseases. A P-value ≤ 0.05 was considered statistically significant.
Results
Compared with individuals in the HC group, AD and VaD patients showed significant differences in MMSE, CDR, and CDT scores (P < 0.05; Table 1), but not in average age, education, sex, coronary heart disease, diabetes, proportion of smokers, cholesterol, or diet structure.
The plasma Fg levels in AD, VaD, and HC groups were 298.82 ± 50.90, 317.97 ± 97.19, and 259.71 ± 48.20 mg/dL (Figure 1), respectively. Regression analysis showed that after controlling for age, sex, diabetes, hypertension, smoking, drinking, cholesterol, diet, coronary heart disease, gene, and other factors, plasma Fg levels were significantly different among the three groups (F = 3.939, P < 0.01). Among these factors, only disease (AD, VaD) (beta = −15.589, P = 0.020), genotype (beta = 25.966, P = 0.002), and hypertension (beta = −24.932, P = 0.026) had significant effects on plasma Fg level (Table 2). Statistical analysis showed that after controlling for the above baseline factors, plasma Fg level remained significantly higher in the AD and VaD groups compared with that in the HC group (P < 0.01) but was not significantly different between the AD and VaD groups (P = 0.062).
Figure 1.
Plasma Fg levels in AD, VaD, and HC groups. Fg, fibrinogen; AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls. The lower and upper ends of the box mark the 25th and 75th percentiles or the location of the first and third quartiles, and the solid band indicates the 50th percentile or the median. The whiskers represent the range of values.
Table 2.
Results of regression analysis.
| Variables |
Unstandardized Coefficients |
Standardized Coefficients Beta | t-test | P-value | |
|---|---|---|---|---|---|
| Beta | SE | ||||
| (Constant) | 299.943 | 62.945 | 4.765 | <0.001 | |
| Group (AD/VaD/HC) | −15.589 | 6.621 | −0.192 | −2.358 | 0.020 |
| TC | 6.938 | 4.567 | 0.110 | 1.519 | 0.131 |
| Age | −0.396 | 0.515 | −0.056 | −0.768 | 0.444 |
| Sex | 0.235 | 10.466 | 0.002 | 0.022 | 0.982 |
| Diabetes | −25.009 | 14.835 | −0.124 | −1.686 | 0.094 |
| Smoking | −2.954 | 14.190 | −0.018 | −0.208 | 0.835 |
| Drinking | 21.404 | 15.513 | 0.119 | 1.380 | 0.170 |
| CAD | 17.662 | 13.633 | 0.097 | 1.295 | 0.197 |
| FGB −148C/T | 25.966 | 8.228 | 0.236 | 3.156 | 0.002 |
| Hypertension | −24.932 | 11.106 | −0.179 | −2.245 | 0.026 |
| Diet | 1.435 | 6.621 | 0.016 | 0.217 | 0.829 |
AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls; TC, total cholesterol; CAD, coronary heart disease.
Analysis of CDR, MMSE, and Fg levels of patients showed no correlation in the dementia group (patients with AD and VaD) (Table 3).
Table 3.
The correlation between CDR, MMSE, and Fg level in AD and VaD groups.
|
Fg level |
|||
|---|---|---|---|
| Group | Project | R value | P-value |
| AD group | CDR | 0.356 | 0.212 |
| MMSE | −0.081 | 0.743 | |
| Orientation | 0.114 | 0.685 | |
| Memory | −0.177 | 0.527 | |
| Recall | −0.001 | 0.998 | |
| Calculations | −0.080 | 0.768 | |
| Language | −0.049 | 0.862 | |
| VaD group | CDR | −0.154 | 0.583 |
| MMSE | −0.475 | 0.086 | |
| Orientation | −0.133 | 0.649 | |
| Memory | −0.370 | 0.193 | |
| Recall | −0.102 | 0.752 | |
| Calculations | −0.005 | 0.987 | |
| Language | −0.377 | 0.184 | |
CDR, Clinical Dementia Rating scale; MMSE, mini-mental state examination; AD, Alzheimer’s disease; VaD, vascular dementia; Fg, fibrinogen.
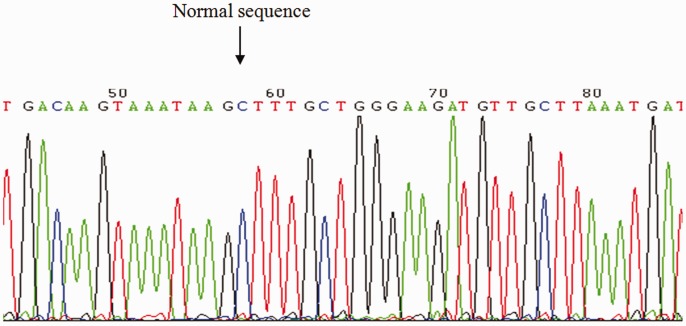
Amplification of the FGB −148C/T polymorphism resulted in a 300-bp fragment. The wild-type CC fragment can be digested with HindIII into two fragments of 202 and 98 bp, and the mutant heterozygote C/T can be digested into three fragments of 300, 202, and 98 bp. Because the homozygous mutant TT genotype had no HindIII restriction site, a 300-bp fragment is observed after digestion. Figure 2 shows the results of PCR amplification and endonuclease digestion, and Figures 3 and 4 show the sequencing results of the PCR product.
Figure 2.
Agarose gel analysis of amplification products of FGB −148 after digestion with HinfI. M, DL2000 Marker; TT/CT/CC, FGB −148C/T genotypes; PCR, amplification products of FGB −148.
Figure 3.
Sequence diagram of TT genotype of FGB −148C/T.
Figure 4.
Sequence diagram of CC genotype of FGB −148C/T.
Figure 5 shows the frequency distribution of FGB −148C/T in the AD, VaD, and HC groups. The frequency of the CT+TT genotypes was 56.2% in the AD group, 53.8% in the VaD group, and 33.9% in the HC group. The χ2 test was performed to explore the distribution of subjects with the CC genotype and the T allele (CT+TT). The results showed significant differences in the distribution of CC and CT+TT genotypes among the three groups (χ2 = 6.892, P = 0.032, df = 2). In addition, there was a significant difference in distribution of CC and CT+TT genotypes between the AD and HC groups (P = 0.014, df = 1) (Table 4). Moreover, we found significant differences in the distribution of T and C alleles among the three groups (χ2 = 7.832, P = 0.020, df = 2). The frequency of the T allele was 0.320 in the AD group, 0.298 in the VaD group, and 0.170 in the HC group, showing a significantly higher frequency of T allele carriers in the AD group than in the HC group (χ2 = 7.232, P = 0.007, df = 1) (Table 4). The genotype distributions in all groups were compatible with Hardy–Weinberg expectations.
Figure 5.
Distribution of FGB −148C/T polymorphism and T allele genotype frequencies in AD, VaD, and HC groups. AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls.
Table 4.
Comparison of frequencies of CC/CT+TT genotypes and C/T allele between different groups (χ2, P-value).
|
CC/CT+TT |
C/T |
Significant level | |||
|---|---|---|---|---|---|
| Groups | χ2 | P-value | χ2 | P-value | |
| AD/VaD | 0.067 | 0.796 | 0.133 | 0.716 | 0.0167 |
| AD/HC | 5.994 | 0.014 | 7.232 | 0.007 | 0.0167 |
| VaD/HC | 4.352 | 0.037 | 5.000 | 0.025 | 0.0167 |
AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls.
Figure 6 shows that Fg levels of the three different genotype carriers had homogeneity of variance in the AD and VaD groups (F = 18.879 and P < 0.01 for the AD group; F = 12.194 and P < 0.01 the for VaD group) but not in the HC group (F = 0.486, P = 0.489). The results showed that plasma Fg level was higher for TT genotype carriers than for CC and CT genotype carriers in the AD and VaD groups (P < 0.01). No TT genotype carriers were found in the HC group. The level of plasma Fg was not significantly different between CT and CC genotype carriers in the AD and VaD groups.
Figure 6.
Comparison of gene polymorphism of FGB −148C/T and plasma Fg level in AD, VaD, and HC groups. Fg, fibrinogen; AD, Alzheimer’s disease; VaD, vascular dementia; HC, healthy controls.
Discussion
Evidence suggests that vascular risk factors play important roles in the development of dementia, and plasma fibrinogen is associated with VaD.16 AD is the most common form of dementia and there is no effective treatment for AD. In addition to pathologic characteristics, AD also has a vascular component. Substantial evidence has shown that thrombosis and fibrinogen play an important role in AD.19–21 Fourteen days after a stroke, the level of Fg gradually approaches that of healthy subjects.22 In all of the patients involved in this study, the time elapsed since stroke was more than 3 months. Therefore, the increase in Fg caused by stroke itself had little impact on results in this study.22 Our results showed that plasma Fg level was significantly higher in the AD and VaD groups than in the HC group. It was not significantly different between patients in the AD group and those in the VaD group. This finding indicated that a high plasma Fg level is strongly related to the onset of dementia.23 Chung et al.24 compared Fg levels in 86 patients diagnosed with stroke and their T2-weighted magnetic resonance images (MRI), and found that high Fg level was related to the severity of white matter damage. A study in Austria also suggested that high Fg level was independently associated with white matter density and lacunar infarcts in head MRI.25 We hypothesized that high plasma Fg level may play a common role in the occurrence of AD and VaD as a vascular risk factor.
The biosynthesis of Fg is influenced by genetic factors and various environmental factors.26,27 Humphries et al.28 first reported a correlation between Fg gene polymorphisms and Fg level in 1987. Schmidt et al.29 studied 399 individuals aged 45 to 75 years (Austrian Stroke Prevention Study) by computed tomography and showed that subjects with the TT genotype had a 6.17-fold higher risk of carotid artery atherosclerosis than subjects with the CC or CT genotype. They inferred that the FGB −148T/T genotype was related to asymptomatic carotid atherosclerosis. However, the relationship between Fg gene polymorphisms and dementia is rarely reported. We found significant differences among participants with the CC, CT, and TT genotypes. The frequency of the T allele was significantly higher in the AD group than in the HC group, suggesting that the T allele may be associated with AD. In addition, plasma Fg level was significantly higher in AD patients with FGB −148 TT than those with CC and CT genotypes, suggesting that plasma Fg level was closely related to FGB −148 TT genotype.30 Therefore, it is speculated that the FGB −148C/T polymorphism may affect the incidence of dementia by affecting plasma Fg level, and this effect is more obvious in patients with AD.
The mechanism by which the FGB −148C/T polymorphism affects plasma Fg level and onset of dementia remains elusive. It is thought that gene polymorphisms affect the transcription of the FGB gene; synthesis of FGB mRNA is considered to be the rate-limiting step of Fg synthesis.31 Interleukin-6 (IL-6) is the main regulator of Fg biosynthesis.31 A region upstream of 5′ FGB gene contains three sites associated with IL-6.32 The polymorphic locus −148C/T is located in the 5′ promoter region of FGB and is one of more than a dozen Fg gene polymorphic loci close to the IL-6 effective site. Therefore, FGB −148C/T might influence Fg biosynthesis by affecting the interaction between nucleoprotein and IL-6RE. Verschuur et al.33 showed that the HNF3 locus in the Fg promoter region plays an important role in IL-6 expression. Polymorphisms in genes adjacent to the FGB −148C/T site could affect activity of FGB −148C/T. FGB −148C/T is the only genetic factor affecting the activity of IL-6 promoter in the six polymorphic sites of the β-Fg-activated zone. In contrast, the FGB −455G/A polymorphic site can affect both the HNF1 and FGB genes and promote secretion of more mature Fg by the liver. However, there is complete linkage imbalance between FGB −148C/T and FGB −455G/A polymorphic sites. Therefore, it is believed that the FGB −148C/T polymorphic site could increase plasma Fg level.34,35 Montgomery et al.36 confirmed that in the reaction of IL-6 to smoking, inflammation, and tissue damage, synthesis of β-Fg is affected by FGB −148C/T alone or in combination with FGB −455A. Furthermore, one study indicated that FGB −148C and FGB −455A are correlated in the Chinese population.37
In this study, the plasma Fg level was significantly higher in the AD and VaD groups than in the HC group. Within the dementia group (AD and VaD), patients with the TT genotype at FGB −148C/T had a higher Fg level than patients with CC and CT genotypes. TT+CT genotypes and T allele were only related to AD. Although the distribution frequency of the TT+CT genotype and T allele in the VaD group was higher than that in HC, the difference was not statistically significant. These discrepancies may be explained by a number of factors: (1) plasma Fg level is affected by many other factors besides gene polymorphisms, including interactions between environmental factors and genetic factors, and combined effects of FGB −148C and FGB −455A, which were not determined in this study; (2) ethnic and geographic differences also contribute to variability; and (3) the small sample size may have led to sampling error and therefore contributed to the discrepancy. Furthermore, our study was a cross-sectional study. Therefore, we cannot prove the sequence of increased Fg level and dementia. We will conduct a cohort study to further elucidate the relationship between Fg level and dementia.
This study showed that Fg, as a risk factor for dementia, may participate in the pathogenesis of dementia through its vascular mechanism. An increased level of circulating Fg indicates poorer subsequent cognitive ability and is associated with age-related cognitive decline in several domains, including general ability.38 The FGB −148C/T polymorphism is located in the regulatory gene for Fg and affects the incidence of dementia. A previous study indicated that changes in gene level result in changes in Fg level in plasma, which accounts for 51% of all influencing factors.31 Decreasing the Fg level not only lessens cerebral amyloid angiopathy and blood–brain barrier permeability, but also reduces microglial activity and improves cognitive performance in AD mouse models.39 The study underscores that reducing Fg level can control and prevent the development of dementia,21 although the curative effects need to be further studied. It should be noted that gene regulation can be used as a target and has potential for the prevention and treatment of dementia.
Conclusions
Plasma Fg level was significantly correlated with AD and VaD but not with the severity of dementia. Plasma Fg level was associated with the polymorphism of FGB −148C/T. The TT+CT genotypes of FGB −148C/T and the distribution frequency of T allele may be related to AD. Fg level is a vascular risk factor common to both AD and VaD.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The study was supported by the Special Research Fund for Central Universities, Peking Union Medical College (No. 3332018181), Tianjin Natural Science Foundation (No. 19JCYBJC26100); The Science &Technology Development Fund of Tianjin Education Commission for Higher Education (No. 2017ZD10).
ORCID iDs
Yanan Sun https://orcid.org/0000-0003-4127-7869
Benshu Zhang https://orcid.org/0000-0001-8702-5101
References
- 1.Sloane PD, Zimmerman S, Suchindran C, et al. The public health impact of Alzheimer’s disease, 2000-2050: potential implication of treatment advances. Annu Rev Public Health 2002; 23: 213–231. [DOI] [PubMed] [Google Scholar]
- 2.Kalaria RN, Maestre GE, Arizaga R, et al. Alzheimer’s disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol 2008; 7: 812–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilhelmsen L, Svardsudd K, Korsan-Bengtsen K, et al. Fibrinogen as a risk factor for stroke and myocardial infarction. N Engl J Med 1984; 311: 501–505. [DOI] [PubMed] [Google Scholar]
- 4.Howard SC, Algra A, Rothwell PM. Effect of age and glycaemic control on the association between fibrinogen and risk of acute coronary events after transient ischaemic attack or stroke. Cerebrovasc Dis 2008; 25: 136–143. [DOI] [PubMed] [Google Scholar]
- 5.Fukujima MM, Martinez TL, Pinto LE, et al. Fibrinogen as independent risk factor for ischemic stroke. Arq Neuropsiquiatr 1997; 55: 737. [DOI] [PubMed] [Google Scholar]
- 6.Wu G, Cai H, Cai H, et al. Effect of the -148C/T, 448G/A, and -854G/A polymorphisms of the β-fibrinogen gene on the risk of ischemic stroke in Chinese population. J Stroke Cerebrovasc Dis 2015; 24: 1577–1590. [DOI] [PubMed] [Google Scholar]
- 7.Li YY, Wu XY, Xu J, et al. Apo A5 -1131T/C, FgB-455G/A, -148C/T, and CETP TaqIB gene polymorphisms and coronary artery disease in the Chinese population: a meta-analysis of 15,055 subjects. Mol Biol Rep 2013; 40: 1997–2014. [DOI] [PubMed] [Google Scholar]
- 8.van Oijen M, Witteman JC, Hofman A, et al. Fibrinogen is associated with an increased risk of Alzheimer disease and vascular dementia. Stroke 2005; 36: 2637–2641. [DOI] [PubMed] [Google Scholar]
- 9.Xu G, Zhang H, Zhang S, et al. Plasma fibrinogen is associated with cognitive decline and risk for dementia in patients with mild cognitive impairment. Int J Clin Pract 2010; 62: 1070–1075. [DOI] [PubMed] [Google Scholar]
- 10.Breteler MM. Vascular risk factors for Alzheimer’s disease: an epidemiologic perspective. Neurobiol Aging 2000; 21: 153–160. [DOI] [PubMed] [Google Scholar]
- 11.Dede DS, Yavuz B, Yavuz BB, et al. Assessment of endothelial function in Alzheimer’s disease: is Alzheimer’s disease a vascular disease? Am Geriatr Soc 2007; 55: 1613–1617. [DOI] [PubMed] [Google Scholar]
- 12.Guo X, Zhang D, Zhang X. Fibrinogen gene polymorphism (Bbeta-148C/T) in Uygur patients with cerebral infarction. Neurol Res 2009; 31: 381–384. [DOI] [PubMed] [Google Scholar]
- 13.Zamolodchikov D, Strickland S. A possible new role for Aβ in vascular and inflammatory dysfunction in Alzheimer’s disease. Thromb Res 2016; 141: S59–S61. [DOI] [PubMed] [Google Scholar]
- 14.Narayan PJ, Kim SL, Lill C, et al. Assessing fibrinogen extravasation into Alzheimer’s disease brain using high-content screening of brain tissue microarrays. J Neurosci Methods 2015; 247: 41–49. [DOI] [PubMed] [Google Scholar]
- 15.Chen ZL, Revenko AS, Singh P, et al. Depletion of coagulation factor XII ameliorates brain pathology and cognitive impairment in Alzheimer’s disease mice. Blood 2017; 129: 2547–2556. doi: 10.1182/blood-2016-11-753202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vishnu VY, Modi M, Garg VK, et al. Role of inflammatory and hemostatic biomarkers in Alzheimer’s and vascular dementia - A pilot study from a tertiary center in Northern India. Asian J Psychiatr 2017; 29: 59–62. [DOI] [PubMed] [Google Scholar]
- 17.Muradashvili N, Tyagi R, Tyagi N, et al. Cerebrovascular disorders caused by hyperfibrinogenaemia. J Physiol 2016; 594: 5941–5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chui HC, Mack W, Jackson JE, et al. Clinical criteria for the diagnosis of vascular dementia. Arch Neurol 2000; 57: 191–196. [DOI] [PubMed] [Google Scholar]
- 19.Cortes-Canteli M, Mattei L, Richards AT, et al. Fibrin deposited in the Alzheimer’s disease brain promotes neuronal degeneration. Neurobiol Aging 2015; 36: 608–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahn HJ, Zamolodchikov D, Cortescanteli M, et al. Alzheimer’s disease peptide beta-amyloid interacts with fibrinogen and induces its oligomerization. Proc Natl Acad Sci U S A 2010; 107: 21812–21817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortescanteli M, Paul J, Norris EH, et al. Fibrinogen and β-amyloid association alters thrombosis and fibrinolysis: a possible contributing factor to Alzheimer’s disease. Neuron 2010; 66: 695–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zang RS, Zhang H, Xu Y, et al. Serum C-reactive protein, fibrinogen and D-dimer in patients with progressive cerebral infarction. Transl Neurosci 2016; 7: 84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hainsworth AH, Minett T, Andoh J, et al. Neuropathology of white matter lesions, blood-brain barrier dysfunction, and dementia. Stroke 2017; 48: 2799–2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung CS, Caplan LR, Van Swieten J, et al. White matter changes in stroke and fibrinogen levels. Ann Neurol 1993; 34: 260. [Google Scholar]
- 25.Schmidt R, Fazekas F, Hayn M, et al. Risk factors for microangiopathy-related cerebral damage in the Austrian Stroke Prevention Study. J Neurol Sci 1997; 152: 15–21. [DOI] [PubMed] [Google Scholar]
- 26.Humphries SE, Luong LA, Montgomery HE, et al. Gene environment interaction in the determination of levels of plasma fibrinogen. Thromb Haemost 1999; 82: 818. [PubMed] [Google Scholar]
- 27.Zhang X, Li Y, Guo X, et al. Relationship between the -455G/A and -148C/T polymorphisms in the beta-fibrinogen gene and cerebral infarction in the Xinjiang Uygur and Han Chinese populations. Neural Regen Res 2012; 7: 546–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Humphries SE, Cook M, Dubowitz M, et al. Role of genetic variation at the fibrinogen locus in determination of plasma fibrinogen concentrations. Lancet 1987; 1: 1452. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt H, Schmidt R, Niederkorn K, et al. Beta-fibrinogen gene polymorphism (C148-T) is associated with carotid atherosclerosis: results of the Austrian Stroke Prevention Study. Arterioscler Thromb Vasc Biol 1998; 18: 487–492. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Xu G, Zhao X, et al. Relationship between fibrinogen beta 148C/T gene polymorphism and cardio-cerebral thrombosis disease. Chin J Emergency Med 2003; 2: 6832684. [Google Scholar]
- 31.Cronjé HT, Nienaber-Rousseau C, Zandberg L, et al. Fibrinogen and clot-related phenotypes determined by fibrinogen polymorphisms: independent and IL-6-interactive associations. Plos One 2017; 12: e0187712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roy SN, Mukhopadhyay G, Redman CM. Regulation of fibrinogen assembly. Transfection of Hep G cells with B beta cDNA specifically enhances synthesis of the three component chains of fibrinogen. J Biol Chem 1990; 265: 6389. [PubMed] [Google Scholar]
- 33.Verschuur M, de Jong M, Felida L, et al. A hepatocyte nuclear factor-3 site in the fibrinogen β promoter is important for interleukin 6-induced expression, and its activity is influenced by the adjacent-148C/T polymorphism. J Biol Chem 2005; 280: 16763–16771. [DOI] [PubMed] [Google Scholar]
- 34.Anderson GM, Shaw AR, Shafer JA. Functional characterization of promoter elements involved in regulation of human B beta-fibrinogen expression. Evidence for binding of novel activator and repressor proteins. J Biol Chem 1993; 268: 22650. [PubMed] [Google Scholar]
- 35.Morozumi T, Sharma A, De NE. The functional effects of the -455G/A polymorphism on the IL-6-induced expression of the beta-fibrinogen gene may be due to linkage disequilibrium with other functional polymorphisms. Immunol Invest 2009; 38: 311–323. [DOI] [PubMed] [Google Scholar]
- 36.Montgomery HE, Clarkson P, Nwose OM, et al. The acute rise in plasma fibrinogen concentration with exercise is influenced by the G-453-A polymorphism of the beta-fibrinogen gene. Arterioscler Thromb Vase Biol 1996; 16: 386–391. [DOI] [PubMed] [Google Scholar]
- 37.Liu C, Qian J, Zhao K. Study on the polymorphism of beta fibrinogen 455G/A and 148C/T genes in patients with cerebral infarction. Chin J Neurol 2004; 1: 94. [Google Scholar]
- 38.Marioni RE, Stewart MC, Murray GD, et al. Peripheral levels of fibrinogen, C-reactive protein, and plasma viscosity predict future cognitive decline in individuals without dementia. Psychosom Med 2009; 71: 901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cortes-Canteli M, Zamolodchikov D, Ahn HJ, et al. Fibrinogen and altered hemostasis in Alzheimer’s disease. J Alzheimers Dis 2012; 32: 599–608. [DOI] [PMC free article] [PubMed] [Google Scholar]