Short abstract
Objective
To evaluate the efficacy of intravenous iron sucrose (IS) in the perioperative period of a second thoracotomy after open-heart surgery.
Methods
This study enrolled patients that underwent a second thoracotomy after previous open-heart surgery. Propensity-score matching was used to match patients that received oral iron therapy with those that received IS after admission. The baseline demographic and clinical characteristics, perioperative data and adverse outcomes were compared between these two matched groups.
Results
The study enrolled 447 patients: of these, 148 received oral iron therapy and effective dietary guidance; and 299 patients received 300 mg IS per week. After matching the propensity scores, there were no significant differences between the two groups in terms of age, sex, smoking history, incidence of major cardiac adverse events, Euro-score, time between the two thoracotomies, application of recombinant erythropoietin, haemoglobin (Hb) on admission and red blood cell (RBC) count on admission. The differences between the two groups after propensity-score matching in terms of the amount of RBC input and Hb after the operation were significant.
Conclusion
The administration of IS might be useful for improving postoperative Hb levels and reducing intraoperative RBC input in patients undergoing a second thoracotomy.
Keywords: Iron sucrose, second thoracotomy, blood transfusion, postoperative anaemia
Introduction
In patients undergoing coronary artery bypass graft, heart valve replacement and major vascular surgery, a series of serious complications, such as bridge vascular restenosis and structural failure of biological valves are unavoidable problems for some patients.1 In these situations, reoperation is an important method used to solve these complications.2 With an increase in second thoracotomies following open-heart surgery, intraoperative bleeding and postoperative anaemia have become common factors affecting the prognosis of patients undergoing such operations.3 Routine surgical procedures can lead to tissue damage and blood loss; and fibrinolysis at the surgical site increases 4–8 times more than usual.4 The degree of fibrinolysis depends on the amount of damaged tissue and the type of surgery.5 Second thoracotomies are very traumatic and are currently recognized as one the cardiac surgical procedures that causes the greatest loss of blood.6 At present, allogeneic blood transfusions are the fastest and most effective treatments for anaemia after a second thoracotomy following open-heart surgery.7 However, in clinical practice, insufficient blood supply and blood transfusion risks are inevitable problems.8
Iron sucrose (IS) is a nano-scale colloidal solution in which a large amount of sucrose molecules are noncovalently bound to the surface of an iron hydroxide core.9 Intravenous IS has the advantage of having a more stable structure and lower toxicity than oral iron supplements.10 Intravenous IS can supplement iron to patients at a rate of 300 mg/30 min and few allergic reactions occur,11 but its application is limited because the maximum amount of iron supplementation per week should not exceed 600 mg.12
This current study investigated the role of intravenous IS during a secondary thoracotomy following open-heart surgery with a view to giving guidance to clinicians about how to deal with postoperative anaemia following these rare and complex operations.
Patients and methods
Study population
This retrospective study enrolled consecutive patients that underwent a second thoracotomy after open-heart surgery in the Department of Cardiovascular Surgery, Zhongshan Hospital, Fudan University, Shanghai, China between March 2013 and March 2018. The exclusion criteria were as follows: (i) haemoglobin (Hb) and red blood cell count (RBC) not available at admission; (ii) not iron sucrose treatment-naive; (iii) < 18 years; (iv) Hb depletion due to other diseases of the blood system. The inclusion criteria were as follows: (i) patients who had undergone open-heart surgery; (ii) no obvious blood transfusion reaction.
This study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University, Shanghai, China. Written informed consent was obtained from all study participants.
Study design
The patients were divided into two groups for analysis: patients that received 600 mg ferrous sulphate tablets orally per week and effective dietary guidance (iron-rich foods like meat, eggs, liver and a variety of seafood) after admission formed the control group; and patients that received 300 mg IS intravenously per week after admission formed the experimental group. Preoperative baseline demographic and clinical data were recorded for the two groups including age, sex, smoking history, percutaneous coronary intervention history, myocardial infarction history, presence or absence of congestive heart failure, left ventricular ejection fraction values, Euro score, whether or not recombinant erythropoietin (Rh-EPO) was used, the second thoracotomy method, time from first thoracotomy to second thoracotomy, admission Hb level and RBC count at admission. The perioperative outcomes of the two patient groups after surgery were recorded and compared.
Treatment intervention
The control group received 600 mg ferrous sulphate tablets orally per week and effective dietary guidance (iron-rich foods like meat, eggs, liver and a variety of seafood) after admission. The experimental group, in strict accordance with the physician’s instructions, received 300 mg/week IS spread over two administrations intravenously after admission for 2 weeks.
Data collection
Changes in Hb, RBC and any adverse reactions in the two patient groups were recorded after admission and for 1 month postoperatively. RBC input during the operation was recorded at the same time as the intraoperative blood transfusion volume (units). The patient’s intraoperative blood loss volume was recorded (ml).
Propensity-score matching
A logistic regression model was established in which the dependent variables were Hb and RBC count after the operation. Independent variables were sex, smoking history, Hb on admission, RBC count on admission, major adverse heart events, left ventricular ejection fraction, time between thoracotomies, Euro-score and whether Rh-EPO was used in combination. The logistic regression model was used to calculate the postoperative Hb score of each patient and 1:1 matching was conducted between the experimental group and the control group. The matching ratio was first started with the highest accuracy of the propensity score of 0.0001 and then gradually decreased to 0.2.
Statistical analyses
All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY, USA). Continuous data that conformed to a normal distribution are expressed as the mean ± SD. Continuous data that did not conform to a normal distribution were expressed as median (interquartile range). After matching the patients, the comparison of the mean between the two groups was performed using a paired-samples t-test. Time between thoracotomies was not normally distributed, so statistical analysis was undertaken using Mann–Whitney U-test. Categorical data are expressed as percentages and comparison of the rates between the two groups was performed using χ2-test. A P-value < 0.05 was considered statistically significant.
Results
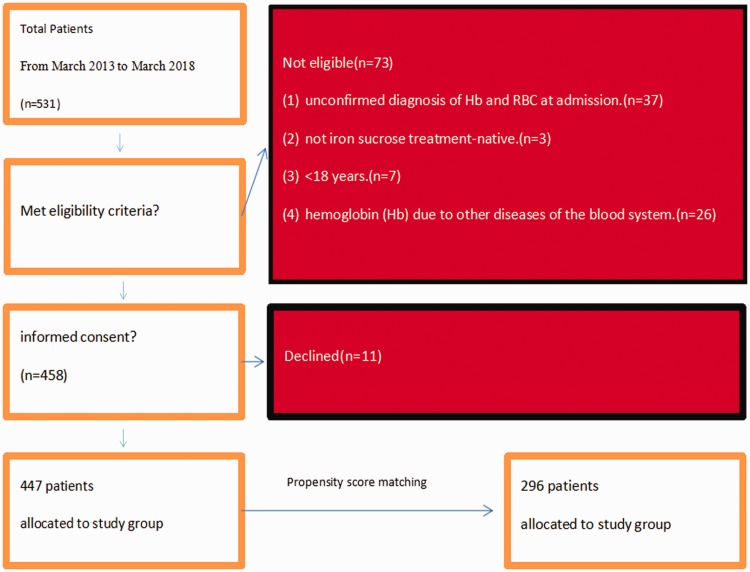
The study enrolled 447 patients that had valvular heart disease, coronary heart disease or macrovascular disease, all of which required surgery lasting more than 4 h. Of these, 148 patients (33.1%) received oral iron therapy and effective dietary guidance based on their Hb levels after admission; and the remaining 299 patients (66.9%) received 300 mg IS intravenously per week after admission. Figure 1 shows the patient selection process. A total of 241 of 447 patients had anaemia at admission. The surgical data for the entire study cohort are presented in Table 1.
Figure 1.
Flow chart showing patient selection during this study of the role of intravenous iron sucrose during a secondary thoracotomy following open-heart surgery.
Table 1.
Second thoracotomy data for patients (n = 447) enrolled in a study of the role of intravenous iron sucrose during a secondary thoracotomy following open-heart surgery.
| Operation | Frequency (n) | Percentage (%) |
|---|---|---|
| Aortic dissection | 24 | 5.4 |
| Aortic valve replacement | 84 | 18.8 |
| Bentall procedure | 48 | 10.7 |
| Coronary artery bypass graft | 16 | 3.6 |
| Cardiac tumour | 12 | 2.7 |
| Congenital heart disease | 8 | 1.8 |
| David procedure | 8 | 1.8 |
| Double-valve replacement | 70 | 15.7 |
| Double-valve replacement + tricuspid valvuloplasty | 4 | 0.9 |
| Ebstein anomaly | 8 | 1.8 |
| Mitral valvuloplasty | 12 | 2.7 |
| Mitral valve replacement | 72 | 16.1 |
| Mitral valve replacement + tricuspid valvuloplasty | 4 | 0.9 |
| Tricuspid valvuloplasty | 28 | 6.3 |
| Tricuspid valvuloplasty + aortic valve replacement | 4 | 0.9 |
| Tricuspid valvuloplasty + double-valve replacement | 8 | 1.8 |
| Tricuspid valvuloplasty + mitral valvuloplasty | 8 | 1.8 |
| Tricuspid valvuloplasty + mitral valve replacement | 8 | 1.8 |
| Tricuspid valve replacement | 10 | 2.2 |
| Ventricular septal defect repair | 11 | 2.5 |
| Total | 447 | 100.0 |
Out of the 299 patients that received IS after a second thoracotomy, 148 were selected to match those with similar propensity scores that did not receive IS (control group). The baseline demographic and clinical data for the two groups before and after matching are presented in Table 2. After propensity-score matching, there were no significant differences between the two groups in terms of age, sex, smoking history, incidence of major cardiac adverse events, Euro-score, time between the two thoracotomies, application of Rh-EPO, Hb on admission and RBC count on admission. There were significant differences between the two groups after propensity-score matching in terms of the proportion of patients with LVEF > 50% and 30% < LVEF < 50% (P < 0.05 for both comparisons).
Table 2.
Baseline demographic and clinical data for patients (n = 447) enrolled in a study of the role of intravenous iron sucrose during a secondary thoracotomy following open-heart surgery stratified according to their treatment (control group [CG] and experimental group [EG]) before and after propensity-score matching.
| Characteristic |
Before propensity-score matching |
After propensity-score matching |
||||
|---|---|---|---|---|---|---|
| CGn = 148 | EGn = 299 | Statistical analysisa | CGn = 148 | EGn = 148 | Statistical analysisa | |
| Age, years | 48 (36–57) | 46 (29–64) | P = 0.048 | 48 (36–57) | 46 (39–54) | NS |
| Sex, female/male | 70/78 | 108/191 | P = 0.023 | 70/78 | 59/89 | NS |
| Current smoker | 14 (9.5%) | 55 (18.4%) | P = 0.014 | 14 (9.5%) | 21 (14.2%) | NS |
| History of percutaneous coronary intervention | 17 (11.5%) | 38 (12.7%) | NS | 17 (11.5%) | 19 (12.8%) | NS |
| History of myocardial infarction | 55 (37.2%) | 106 (35.5%) | NS | 55 (37.2%) | 47 (31.8%) | NS |
| Congestive heart failure | 18 (12.2%) | 41 (13.7%) | NS | 18 (12.2%) | 22 (14.9%) | NS |
| LVEF > 50% | 138 (93.2%) | 257 (86.0%) | P = 0.024 | 138 (93.2%) | 126 (85.1%) | P = 0.025 |
| 30% < LVEF < 50% | 5 (3.4%) | 29 (9.7%) | P = 0.018 | 5 (3.4%) | 15 (10.1%) | P = 0.021 |
| LVEF < 30% | 5 (3.4%) | 13 (4.3%) | NS | 5 (3.4%) | 7 (4.7%) | NS |
| Euro-score | 4.6 ± 0.8 | 4.8 ± 0.8 | P = 0.027 | 4.6 ± 0.8 | 4.7 ± 0.9 | NS |
| Time between thoracotomies, years | 9 (3–12) | 9 (4–15) | P = 0.041 | 9 (3–12) | 11 (4–13) | NS |
| Application of Rh-EPO | 11 (7.4%) | 145 (48.5%) | P < 0.001 | 11 (7.4%) | 19 (12.8%) | NS |
| Hb on admission, g/l | 117.2 ± 12.6 | 115.6 ± 12.6 | NS | 117.2 ± 12.6 | 117.2 ± 12.4 | NS |
| RBC on admission, x 1012/l | 3.8 ± 0.5 | 3.8 ± 0.5 | NS | 3.8 ± 0.5 | 3.6 ± 0.6 | NS |
Data presented as mean ± SD, median (interquartile range) or n of patients (%).
aAfter matching the patients, the comparison of the means was performed using a paired-samples t-test; time between thoracotomies was not normally distributed, so statistical analysis was undertaken using Mann–Whitney U-test; categorical data were compared between the two groups using χ2-test; NS, no significant between-group difference (P ≥ 0.05).
LVEF, left ventricular ejection fraction; Rh-EPO, recombinant erythropoietin; Hb, haemoglobin; RBC, red blood cell.
The perioperative outcomes of the two patient groups were recorded (Table 3). After propensity-score matching, there were no significant differences in the volume of intraoperative blood loss and the RBC count after the operation in the experimental and control groups. The differences between the two groups after propensity-score matching in terms of the amount of RBC input and Hb after the operation were significant (P < 0.05 for both comparisons).
Table 3.
Perioperative data for patients (n = 447) enrolled in a study of the role of intravenous iron sucrose during a secondary thoracotomy following open-heart surgery stratified according to their treatment (control group [CG] and experimental group [EG]) before and after propensity-score matching.
|
Before propensity-score matching |
After propensity-score matching |
|||||
|---|---|---|---|---|---|---|
| CGn = 148 | EGn = 299 | Statistical analysisa | CGn = 148 | EGn = 148 | Statistical analysisa | |
| Intraoperative blood loss, ml | 781.8 ± 287.9 | 617.1 ± 105.6 | NS | 781.8 ± 287.9 | 718.9 ± 275.4 | NS |
| Quantity of red blood cell replacement, units | 4.3 ± 3.0 | 4.1 ±1.3 | NS | 4.3 ± 3.0 | 3.5 ± 2.4 | P = 0.013 |
| Hb after the operation, g/l | 90.5 ± 5.4 | 91.7 ± 7.2 | NS | 90.5 ± 5.4 | 92.3 ± 6.7 | P = 0.010 |
| RBC count after the operation, x 1012/l | 3.0 ± 0.4 | 3.4 ± 0.6 | NS | 3.0 ± 0.4 | 3.1 ± 0.4 | NS |
Data presented as mean ± SD.
aAfter matching the patients, the comparison of the means was performed using a paired-samples t-test; NS, no significant between-group difference (P ≥ 0.05).
Hb, haemoglobin; RBC, red blood cell.
The adverse reactions were recorded in the electronic medical records system. After propensity-score matching, there was a significant reduction in the overall incidence of adverse events in the experimental group compared with the control group (P = 0.001) (Table 4).
Table 4.
Adverse reactions for patients (n = 447) enrolled in a study of the role of intravenous iron sucrose during a secondary thoracotomy following open-heart surgery stratified according to their treatment (control group [CG] and experimental group [EG]) before and after propensity-score matching.
| Adverse event |
Before propensity-score matching |
After propensity-score matching |
||||
|---|---|---|---|---|---|---|
| CGn = 148 | EGn = 299 | Statistical analysisa | CGn = 148 | EGn = 148 | Statistical analysisa | |
| Allergy | 1 | 4 | 1 | 0 | ||
| Gastrointestinal dysfunction | 25 | 16 | 25 | 3 | ||
| Metallic odour | 2 | 5 | 2 | 2 | ||
| Low blood pressure | 1 | 4 | 1 | 0 | ||
| Respiratory adverse reaction | 0 | 1 | 0 | 0 | ||
| Parasympathetic symptoms | 2 | 2 | 2 | 0 | ||
| Fever | 0 | 3 | 0 | 1 | ||
| Gum changed colour | 0 | 0 | 0 | 0 | ||
| Overall incidence (%) | 31 (20.95) | 35 (11.71) | NS | 31 (20.95) | 6 (4.05) | P = 0.001 |
Data presented as n of patients (%).
aCategorical data were compared between the two groups using χ2-test; NS, no significant between-group difference (P ≥ 0.05).
Discussion
Second thoracotomy cases are rare and this type of difficult surgery often results in large amounts of blood loss. Excessive loss of Hb from the body leads to oxygenation disorders and a poor prognosis. Using extracorporeal circulation for too long and administering too many units of RBCs can readily cause coagulation dysfunction.13 This current study located every patient that had received a second thoracotomy between 2013 and 2018 in Zhongshan Hospital using the electronic case records. The aim of this current study was to investigate the relationship between iron supplementation and prognosis following a second thoracotomy procedure. Due to the different baseline conditions of the study cohort, such as age, sex, cardiac function, past history, intervals between thoracotomies, and Hb and RBC count on admission, there were many confounding factors when comparing the two groups. Therefore, propensity-score matching was undertaken to minimize the differences between the experimental and control groups as much as possible when comparing the baseline preoperative parameters.14
In this current study, there were no significant differences in the postoperative RBC count or the intraoperative blood loss volume between the two groups. However, there was a significant difference in the amount of RBC input, which was significantly lower in the experimental group compared with the control group. This may have resulted from the intravenous administration of IS in the perioperative period. In this current study, 241 of the 447 patients already had anaemia at admission. The underlying disease might have increased the amount of intraoperative blood transfusions and the severity of postoperative anaemia. Severe anaemia causes the blood to carry less oxygen.15 This may be one of the causes of organ dysfunction, pallor, dizziness and headache after the operation.16 In addition, it has been reported that the intraoperative transfusion of excessive RBCs might lead to the reduction of innate immune and cellular immune functions in patients.17 Compared with the control group, the amount of RBC input was significantly reduced in the experimental group in the current study. This allowed clinicians to cope with the severe situation of inadequate blood supply and the large amount of bleeding that can occur during second thoracotomies. An adequate blood reserve allows clinicians to deal with sudden situations during the operation.18 Changes in the amount of erythropoietin synthesis, RBCs in the circulation, iron balance, redox status and energy metabolism can all lead to anaemia.19 During a second thoracotomy following open-heart surgery, the sternal wounds are large and the whole body is heparinized. Compared with normal heart surgery, the number of blood transfusions and the degree of postoperative anaemia are significantly increased.20 Rh-EPO is used to treat the anaemia caused by renal insufficiency.21 EPO acts on erythroid progenitor cells to promote their survival and differentiation into mature RBCs.22 In recent years, erythrocyte mobilization has been widely used in the perioperative period to improve perioperative anaemia.23 The iron active ingredient in IS injections has a similar structure to serum ferritin, possessing low toxicity with fewer allergic reactions. It can also improve patients’ sensitivity to Rh-EPO.24 The volume of intraoperative blood loss depends on various factors, such as the number of fused levels, body mass index, age and duration of operation in adolescents with neuromuscular scoliosis.25 Following a massive perioperative haemorrhage, postoperative complications of respiratory, urinary, cardiovascular and wound infections in patients with long-term anaemia were significantly higher than in those without anaemia.26 Postoperative anaemia is a risk factor that threatens the survival rate and prognosis of patients, leading to an increased incidence of postoperative complications and increased mortality.27 The inevitable result of cardiopulmonary bypass is disordered coagulation mechanisms resulting from decreased platelet counts, weakened platelet function, decreased amounts of coagulation factors and hyperactivity of plasmin, which leads to postoperative anaemia.28
In another study of iron therapy for preoperative anaemia, the evaluation showed that preoperative treatment of anaemia increased Hb levels and reduced blood transfusion rates.29 In a randomized controlled trial of colorectal cancer patients, preoperative intravenous IS did not increase Hb levels, but it had a tendency to reduce the amount of RBCs administered after surgery.30 Although allogeneic blood transfusion techniques have recently been developed, there are additional issues such as the immune response, transfusion reactions and increased hospitalization costs for patients.31 At the same time, the current clinical demand for blood increases with an increase in the number of surgeries and the demand for blood is greater than the supply. As a multinuclear ferric hydroxide-sucrose complex solution with low toxicity and low allergic reactions, IS can effectively supplement serum iron concentrations and improve Rh-EPO efficacy, which helps to address the problems with the supply of blood.32 In order to reduce the amount of RBCs transfused during and after a second thoracotomy, clinicians routinely give IS for the first time after surgery. Or they might even give appropriate amounts of IS intravenously to patients in a poor physical condition before the operation to reduce the incidence and degree of anaemia after the operation.
During the course of this current study, the following adverse reactions occasionally occurred in both groups: metallic odour, nausea, vomiting, diarrhoea, hypotension and dyspnoea. Comparing the two groups, the incidence of gastrointestinal dysfunction and allergy was lower in the experimental group. This indicated that IS was safe and effective compared with oral iron supplementation.
This current study had several limitations. Due to the rarity of these cases, it was difficult to obtain a large amount of data. At the same time, because of a variety of underlying diseases and the poor baseline condition of patients undergoing a second thoracotomy, the operations were often complicated, leading to difficulties in obtaining a control group. Since it was difficult to unify surgeons, the length of surgery and the operational plans, identifying and controlling these variables should be the aim of future research. However, despite these limitations, this current work provided significant data around feasibility, the best way of using IS and the perceived benefits during the second thoracotomy.
In conclusion, the results of this current study demonstrated that the routine use of IS was feasible and acceptable in patients undergoing a secondary thoracotomy. The findings of this current study suggest that the use of IS might be useful for improving postoperative Hb levels and reducing intraoperative RBC input. This has the potential to reduce the impact of administering a massive infusion of suspended RBCs on coagulation function. The improvement of postoperative Hb should improve oxygenation and prognosis. Hence, the use of IS in patients undergoing a secondary thoracotomy is worthy of consideration in clinical practice.
Supplemental Material
Supplemental material, IMR902912 Supplemental Material1 for Intravenous transfusion of iron sucrose reduces blood transfusions and improves postoperative anaemia after a second thoracotomy: a propensity-score matching study by Chentao Luo, Yunqing Shi, Yi Lin, Runhua Ma, Qi Xia and Wenjun Ding in Journal of International Medical Research
Supplemental material, IMR902912 Supplemental Material2 for Intravenous transfusion of iron sucrose reduces blood transfusions and improves postoperative anaemia after a second thoracotomy: a propensity-score matching study by Chentao Luo, Yunqing Shi, Yi Lin, Runhua Ma, Qi Xia and Wenjun Ding in Journal of International Medical Research
Acknowledgement
The authors give their thanks to Dr Xianglin Hu (Zhongshan Hospital, Fudan University) for providing expert suggestions on the article.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This research was supported by grants from the National Natural Science Foundation of China (no. 81570224, no. 81725002).
ORCID iD
Chentao Luo https://orcid.org/0000-0002-9557-9988
References
- 1.Wang LJ, Qian XY, Wang Met al. Which factor is the most effective one in metabolic Sydrome on the outcomes after coronary artery bypass graft surgery? A cohort study of 5 Years. J Cardiothorac Surg 2018; 13: 1 doi.org/10.1186/s13019-017-0682-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta RH, Sheng S, O’Brien SMet al. Reoperation for bleeding in patients undergoing coronary artery bypass surgery: incidence, risk factors, time trends, and outcomes. Circ Cardiovasc Qual Outcomes 2009; 2: 583–590. [DOI] [PubMed] [Google Scholar]
- 3.Nwafor IA, Arua OA, Eze JCet al. Utilisation of blood and blood products during open heart surgery in a low-income country: our local experience in 3 years. Cardiology in the Young 2018; 28: 1289–1294. [DOI] [PubMed] [Google Scholar]
- 4.Zittermann A, Koster A, Faraoni Det al . The association between the transfusion of small volumes of leucocyte-depleted red blood cells and outcomes in patients undergoing open-heart valve surgery. Interact Cardiovasc Thorac Surg 2017; 24: 209–215. [DOI] [PubMed] [Google Scholar]
- 5.Mazur P, Myć J, Natorska Jet al . Impaired fibrinolysis in degenerative mitral and aortic valve stenosis. J Thromb Thrombolysis 2018; 46: 193–202. [DOI] [PubMed] [Google Scholar]
- 6.Mou Q, Zhou Q, and Liu S. Blood clot parameters: Prejudgment of fibrinolysis in thromboelastography. Clin Chim Acta 2018; 479: 94–97. [DOI] [PubMed] [Google Scholar]
- 7.Forbes S, Bond AR ,Thirlwell KLet al . Human umbilical cord perivascular cells improve human pancreatic islet transplant function by increasing vascularization. Sci Transl Med 2020; 12: pii: eaan5907. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Ou-Yang J, Xie Get al . Problems and challenges: development of blood transfusion services in Mainland China within the context of health-care system reform. Transfus Med 2019; 29: 253–261. [DOI] [PubMed] [Google Scholar]
- 9.Fu L, Zhang Y, Shao Bet al. Perioperative poor grip strength recovery is associated with 30-day complication rate after cardiac surgery discharge in middle-aged and older adults – a prospective observational study. BMC Cardiovasc Disord 2019; 19: 266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beguin Y, Jaspers A. Iron sucrose – characteristics, efficacy and regulatory aspects of an established treatment of iron deficiency and iron-deficiency anemia in a broad range of therapeutic areas. Expert Opin Pharmacother 2014; 15: 2087–2103. [DOI] [PubMed] [Google Scholar]
- 11.Winkelmayer WC, Goldstein BA, Mitani AAet al. Safety of Intravenous Iron in Hemodialysis: Longer-term Comparisons of Iron Sucrose Versus Sodium Ferric Gluconate Complex. Am J Kidney Dis 2017; 69: 771–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laso-Morales MJ, Vives R, Vallejo-Tarrat Aet al. Single dose of intravenous ferric carboxymaltose infusion versus multiple fractionated doses of intravenous iron sucrose in the treatment of postoperative anaemia in colorectal cancer patients: study protocol for a randomised controlled trial. Trials 2019; 20: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braga DV, Brandão MAG. Diagnostic evaluation of risk for bleeding in cardiac surgery with extracorporeal circulation. Rev Lat Am Enfermagem 2018; 26: e3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Austin PC, Fine JP. Propensity-score matching with competing risks in survival analysis. Stat Med 2019; 38: 751–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen X, Zhang X, Zhao Jet al. Split iron supplementation is beneficial for newborn piglets. Biomed Pharmacother 2019; 120: 109479. [DOI] [PubMed] [Google Scholar]
- 16.Maeda Y, Ogawa K, Morisaki Net al. Association between perinatal anemia and postpartum depression: a prospective cohort study of Japanese women. Int J Gynaecol Obstet 2019; 148: 48–52. [DOI] [PubMed] [Google Scholar]
- 17.Ba H, Xu L, Peng Het al. Amiodarone-related pure red cell aplastic anemia and hypothyroidism in a child with total anomalous pulmonary venous connection. Front Pediatr 2019; 7: 361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kobayashi K, Kokudo T, Yamaguchi Tet al. Hepatectomy in patients with inherited blood coagulation disorders can be safely performed with adequate coagulation factor replacement. Haemophilia 2019; 25: 463–467. [DOI] [PubMed] [Google Scholar]
- 19.Madeddu C, Gramignano G, Astara Get al. Pathogenesis and treatment options of cancer related anemia: perspective for a targeted mechanism-based approach. Front Physiol 2018; 9: 1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma JG, An JX. Deep sternal wound infection after cardiac surgery: a comparison of three different wound infection types and an analysis of antibiotic resistance. J Thorac Dis 2018; 10: 377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Köhler M, Mörsdorf S, Jung Fet al. Recombinant human erythropoietin (rh-EPO) in chronic, dialysis-dependent renal failure: effects on macro- and microcirculation and hematologic parameters. Beitr Infusionsther 1990; 26: 89–95 [Article in German, English abstract]. [PubMed] [Google Scholar]
- 22.Coffey R, Sardo U, Kautz Let al. Erythroferrone is not required for the glucoregulatory and hematologic effects of chronic erythropoietin treatment in mice. Physiol Rep 2018; 6: e13890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sabbah M, Trad D, Jouini Ret al. Gastric ulcerated stromal tumor revealed by anemia. Presse Med 2019; 48: 1005–1006. [DOI] [PubMed] [Google Scholar]
- 24.Wang K, Wu J, Xu Jet al. Correction of anemia in chronic kidney disease with Angelica sinensis polysaccharide via restoring EPO production and improving iron availability. Front Pharmacol 2018; 9: 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jia R, Li N, Xu BYet al. Incidence, influencing factors, and prognostic impact of intraoperative massive blood loss in adolescents with neuromuscular scoliosis: A STROBE-compliant retrospective observational analysis. Medicine (Baltimore) 2017; 96: e6292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eghbal MH, Samadi K, Khosravi MBet al . The Impact of Preoperative Variables on Intraoperative Blood Loss and Transfusion Requirements During Orthotopic Liver Transplant. Exp Clin Transplant 2019; 17: 507–512. [DOI] [PubMed] [Google Scholar]
- 27.Ferraris VA, Davenport DL, Saha SPet al. Surgical outcomes and transfusion of minimal amounts of blood in the operating room. Arch Surg 2012; 147: 49–55. [DOI] [PubMed] [Google Scholar]
- 28.Kertai MD, Zhou S, Karhausen JAet al. Platelet counts, acute kidney injury, and mortality after coronary artery bypass grafting surgery. Anesthesiology 2016; 124: 339–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ng O, Keeler BD, Mishra Aet al. Iron therapy for pre-operative anaemia. Cochrane Database Syst Rev 2015; 12: CD011588. [DOI] [PubMed] [Google Scholar]
- 30.Keeler BD, Dickson EA, Simpson JAet al. The impact of pre-operative intravenous iron on quality of life after colorectal cancer surgery: outcomes from the intravenous iron in colorectal cancer-associated anaemia (IVICA) trial. Anaesthesia 2019; 74: 714–725. [DOI] [PubMed] [Google Scholar]
- 31.Kim JL, Park JH, Han SBet al. Allogeneic Blood Transfusion Is a Significant Risk Factor for Surgical-Site Infection Following Total Hip and Knee Arthroplasty: A Meta-Analysis. J Arthroplasty 2017, 32: 320–325. [DOI] [PubMed] [Google Scholar]
- 32.Kaneva K, Chow E, Rosenfield CGet al. Intravenous Iron Sucrose for Children With Iron Deficiency Anemia. J Pediatr Hematol Oncol 2017; 39: e259–e262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, IMR902912 Supplemental Material1 for Intravenous transfusion of iron sucrose reduces blood transfusions and improves postoperative anaemia after a second thoracotomy: a propensity-score matching study by Chentao Luo, Yunqing Shi, Yi Lin, Runhua Ma, Qi Xia and Wenjun Ding in Journal of International Medical Research
Supplemental material, IMR902912 Supplemental Material2 for Intravenous transfusion of iron sucrose reduces blood transfusions and improves postoperative anaemia after a second thoracotomy: a propensity-score matching study by Chentao Luo, Yunqing Shi, Yi Lin, Runhua Ma, Qi Xia and Wenjun Ding in Journal of International Medical Research