Short abstract
Objective
To investigate the feasibility and efficacy of the Ambu® AuraOnce™ laryngeal mask (LMA) compared with endotracheal intubation (ETI) during supratentorial tumor resection in the right lateral decubitus position.
Methods
This was a randomized controlled trial of LMA compared with ETI in patients who were scheduled to undergo supratentorial tumor resection in the right lateral decubitus position. The patients were randomized to the LMA (n = 40) and ETI groups (n = 40). The hemodynamic parameters (primary outcome) and mechanical ventilation parameters, anesthetic dose, and complications as well as quality of anesthesia recovery (secondary outcomes) were compared.
Results
Patients in the LMA group exhibited lower mean arterial pressure (MAP) and heart rate (HR) compared with ETI. Nine and two patients received esmolol during intubation and extubation, respectively. The airway pressure (AP) in the LMA group was higher compared with the ETI group 60 minutes after the start of surgery. Compared with the ETI group, the sufentanil dose was lower by 24% and the anesthesia recovery rate was better in the LMA group.
Conclusions
LMA can improve hemodynamic stability in patients undergoing supratentorial tumor resection in the right lateral decubitus position. If there is a clinical need and no contraindication, LMA could replace ETI.
Keywords: Laryngeal mask, endotracheal intubation, neurosurgical anesthesia, airway management, comparative study, hemodynamic stability, supratentorial tumor resection
Introduction
Because there are potentially severe physiological changes in neurosurgical patients before surgery, reducing perioperative stress and maintaining hemodynamic stability in these patients is critical. Orotracheal intubation is a routine method in neurosurgical anesthesia to ensure safe and effective ventilation,1 but it may cause short but severe hemodynamic fluctuation during intubation and extubation.2,3 Studies have shown that as many as 50% of neurosurgical patients experienced varying types and degrees of adverse outcomes,4 which is not conducive to anesthesia management, and may lead to life-threatening conditions.5
Clinically, various methods have been used to control or reduce cardiovascular stress or airway response during peri-intubation and extubation, such as using vasoactive drugs (e.g. esmolol or labetalol), applying topical anesthesia to the throat and trachea, blocking the superior laryngeal nerve, increasing the amount of anesthetic, deepening anesthesia, or choosing a suitable airway management device (e.g. laryngeal mask; LMA).6 For neurosurgical patients, excessive drug dosage or drug type changes may be more likely to cause a wave impact on the patient’s circulation, or affect the accurate judgment of the depth of anesthesia, thereby increasing the risk of cardiovascular and cerebrovascular complications.
The LMA has been used widely to assist with anesthesia management. It has been shown to be safe and effective for both spontaneous and controlled ventilation and can be safely and effectively used in gynecological, endoscopic, orthopedic, and urological surgery, and in surgery lasting more than 2 hours.7,8 The use of the LMA in neurosurgical craniotomy surgeries is still limited, with only a few studies that were focused on special or short duration neurosurgeries such as awake craniotomy, interventional, stereotactic brain deep electrode implantation, and ventriculoperitoneal operations.9
Therefore, the aim of this clinical trial was to compare the feasibility and efficacy of the Ambu® AuraOnce™ (Ambu A/S) LMA with endotracheal intubation (ETI) during supratentorial tumor resections in the right lateral decubitus position.
Material and methods
Ethics approval
This study was approved by the Institutional Review Board and Ethics Committee of Sanbo Brain Hospital, Capital Medical University (approval number: SBNK-2018-022-01, 7 May, 2018). Written informed consent was obtained from all patients. The trial was registered at Chictr.org (ChiCTR1800015926).
Study participants
The inclusion criteria were as follows: 1) American Society of Anesthesiology (ASA) physical status I–II; 2) 18–65 years of age; 3) body mass index (BMI) 18–30 kg/m2; 4) scheduled for supratentorial tumor resection in the right lateral decubitus position between May 2018 and December 2018; and 5) under general anesthesia. Patients with heart disease and uncontrolled high blood pressure that was detected during preoperative assessment, predicted difficult airway (small mouth, big tongue, or tonsil abnormal enlargement; patients with infection or other pathological changes in the throat; patients with softened airway or airway mass), sleep apnea, obstructive pulmonary disease, gastroesophageal reflux disease, preoperative voice and swallowing problems, requiring emergency surgery, surgery requirement for high angles of the head and torso torsion (>30°), patients in whom the surgical approach or position had to be changed just before surgery, or pregnant or lactating women were excluded from the study. The patients were randomized to the LMA or ETI groups based on a random number table generated by a computer.
Study design and anesthetic management
This study used a randomized, single-blind, controlled trial design. Patients who underwent supratentorial tumor resection in the right lateral decubitus position by the same group of surgeons were enrolled in a blinded manner. Two senior anesthetists (attending physician and above, with experience in the insertion and management of LMA) and one highly-experienced resident performed all anesthesia operations. Postoperative data were collected by researchers who were also blinded to the patient’s study group.
An arterial cannula was inserted into a peripheral vein under local anesthesia. Electrocardiography (ECG), oxygen saturation (SpO2), invasive arterial blood pressure (IBP), mean arterial pressure (MAP), heart rate (HR), and bispectral index (BIS) were monitored.
Anesthesia was induced by intravenous infusion (TCI-I, Guangxi Weili Ark Technology Co., Ltd., Nanning, China) of propofol (1%) and sufentanil (1 µg/mL) to maintain target plasma concentrations of 5 µg/mL (Marsh model10) and 0.3 ng/mL (Bovill model11), respectively. After loss of consciousness and when the BIS (BISx®, Aspect Medical Systems, Inc., Norwood, MA, USA) was ≤60, 0.6 mg/kg of rocuronium was given intravenously to facilitate tracheal intubation or LMA insertion. A LMA (size 3 for 30–50 kg, size 4 for 50–70 kg, and size 5 for >70 kg patients; Ambu A/S, Ballerup, Denmark) or ETI (size 7.5 for males and size 7 for females; Henan Tuoren Medical Equipment Group Co., Ltd., Xinxiang, China) was inserted 90 seconds after rocuronium administration. Size selection was guided by the manufacturer’s recommendations. The cuff of the LMA was inflated with the recommended volume of air (20, 30, and 40 mL for sizes 3, 4, and 5 LMAs, respectively). The parameters of mechanical ventilation were initially set to a tidal volume of 8 mL/kg, respiratory frequency of 12 times/minute, and gas flow at 1 L/minute. During surgery, the respiratory rate was adjusted to maintain the end-tidal carbon dioxide partial pressure (PetCO2) at 35 to 40 mmHg. Leaks were verified by auscultation at the following head positions to determine whether ventilation of LMA was successful: neutral, anterior flexion, and left and right rotation (≤30°). When the right lateral decubitus position was completed, auscultation was performed again. No audible leaking sound, good thoracic undulation, stable pulse oxygen saturation (>95%), and a typical CO2 waveform on the monitor screen were considered to indicate successful ventilation.
The plasma target concentration of propofol was kept stable at 3.5 µg/mL during surgery, and the sufentanil concentration was adjusted to maintain the MAP in the range of −20% to +10% from baseline.
Rocuronium was terminated 30 minutes before the end of surgery, and no antagonist was used. After surgery, the controlled infusion (TCI) of anesthetics was stopped. All patients were sent back to the intensive care unit (ICU) after surgery with their tubes for awakening and extubation. No analgesics and tranquilizers were allowed during recovery. To avoid the effect of postoperative analgesia on the accuracy of postoperative recovery assessment, all patients did not use a postoperative analgesia pump.
The airway devices were removed in the ICU when consciousness and airway protective reflexes were restored, muscle tension returned to normal, and spontaneous respiration was recovered (PetCO2 <45 mmHg, tidal volume >7 mL/kg).
Measurements
Clinical variables included the hemodynamic parameters (MAP was the primary outcome; the other variables were secondary outcomes), ventilation parameters, insertion parameters, surgical parameters, the quality of anesthesia, and postoperative recovery (secondary outcomes).
Hemodynamic parameters included HR and MAP, which were monitored continuously using an anesthesia monitor (Bene View T8, Shenzhen Mindray Biomedical Electronics Co., Ltd., Shenzhen, China). Both of these parameters were recorded before anesthesia induction (T0), before intubation (T1), at intubation (T2), at 1, 3, and 5 minutes after intubation (T3, T4, T5), spontaneous breathing recovery (T6), after extubation (T7), and at 10 minutes after extubation (T8). The numbers of patients who used vasoactive drugs perioperatively (especially during the induction or recovery of anesthesia) were recorded. Intravenous infusion of nicardipine 0.2 to 0.5 mg or/and esmolol 20 to 50 mg was used to treat persistent systemic hypertension (MAP 10% above preoperative base level) or/and tachycardia (HR faster than 100 beats/minute).
Ventilation parameters included minute ventilation (MV) and airway pressure (AP), and were recorded after successful intubation (t0), 60 minutes after the start of surgery (t1), and before surgery was completed (t2).
The insertion parameters included success rate (first success, first success following adjustment, second success), time of insertion, and the oropharyngeal leakage pressure (OLP) of the LMA.
Surgical parameters included the total sufentanil dose, anesthesia duration, total fluid input, urine output, and estimated blood loss.
The quality of anesthesia recovery was measured by the time of spontaneous respiratory recovery and extubation, the number of patients with cough, patients with sore throat at 24 hours after surgery, and the visual analog scale (VAS) scores for sore throat at 1, 2, and 3 days after surgery.
The quality of postoperative recovery was measured based on the number of patients with postoperative pyrexia, the duration of postoperative pyrexia, the recovery time in the ICU, the time until the patient had food and water intake, and the time until off-bed activity.
Statistical analysis
The sample size was determined based on the sample size estimation method for a random comparison of two sample means. The calculation formula refers to the Chapman & Hall/CRC Biostatistics Series (Second Edition) published in 2003,12 as follows:
where α = 0.05, β = 0.20 for two-sample two-sided test, n represents the number of patients in each group, σ represents the standard deviation, µA and µB represent the mean of the two groups, α is Type I error, and β is Type II error. Based on the pre-experimental results, the mean MAP (µA) in the ETI group at extubation was 94.4 mmHg, while that in the LMA group was 87.5 mmHg, and the standard deviation (σ) was 8.0. The sample size calculated using this formula is 33. Because the expected dropout rate was 20%, the final sample size was 40 per group.
Statistical analysis was performed using SPSS version 22.0 (IBM, Armonk, NY, USA). The measurement data with normal distribution were presented as the mean ± standard deviation (SD) and were analyzed using a two-sample t-test (surgical time, insertion time, and postoperative recovery time). Discrete data were analyzed using the χ2 test or Fisher’s exact probability test (sex, tumor type, success rates, complications, and use of vasoactive drugs), as appropriate. Repeated measure analysis of variance (ANOVA) was used to compare the difference within the groups at different time points (for MAP, HR, MV, AP, and VAS scores). A p-value of <0.05 was considered to be statistically significant.
Results
Demographic and anesthesia data
Eighty patients were randomized to the LMA group (n = 40) or the ETI group (n = 40). Three patients in the ETI group had more than two intubation attempts, and three patients in the LMA group were converted to ETI because of failure to achieve satisfactory ventilation after two attempts. The demographic data (age, sex, and BMI) and the surgical details are shown in Table 1.
Table 1.
Demographic data and surgery details in the LMA and ETI groups.
| LMA group (n = 40) | ETI group (n = 40) | |
|---|---|---|
| Age (years) | 40.8 ± 10.6 | 44.4 ± 13.2 |
| Sex (M/F) | 17/23 | 18/22 |
| BMI (kg/m2) | 23.4 ± 3.1 | 24.4 ± 3.4 |
| Tumor types (glioma/meningioma/others) | 15/14/11 | 15/14/11 |
| Dose of sufentanil (µg) | 79.5 ± 20.8 | 105.3 ± 30.9 |
| Infusion amount (mL) | 3057.5 ± 756.3 | 3294.4 ± 610.1 |
| Urine amount (mL) | 1230.0 ± 530.7 | 1480.0 ± 737.4 |
| Blood loss (mL) | 326.3 ± 160.1 | 352.5 ± 141.9 |
| Application of vasoactive drug (cases) (esmolol/nicardipine) | 2/0 | 9/0 |
| Duration of anesthesia (minutes) | 247.9 ± 78.8 | 271.1 ± 43.5 |
| Duration of hospitalization (day) | 16.0 ± 6.4 | 17.9 ± 7.6 |
LMA, laryngeal mask; ETI, endotracheal intubation; BMI, body mass index.
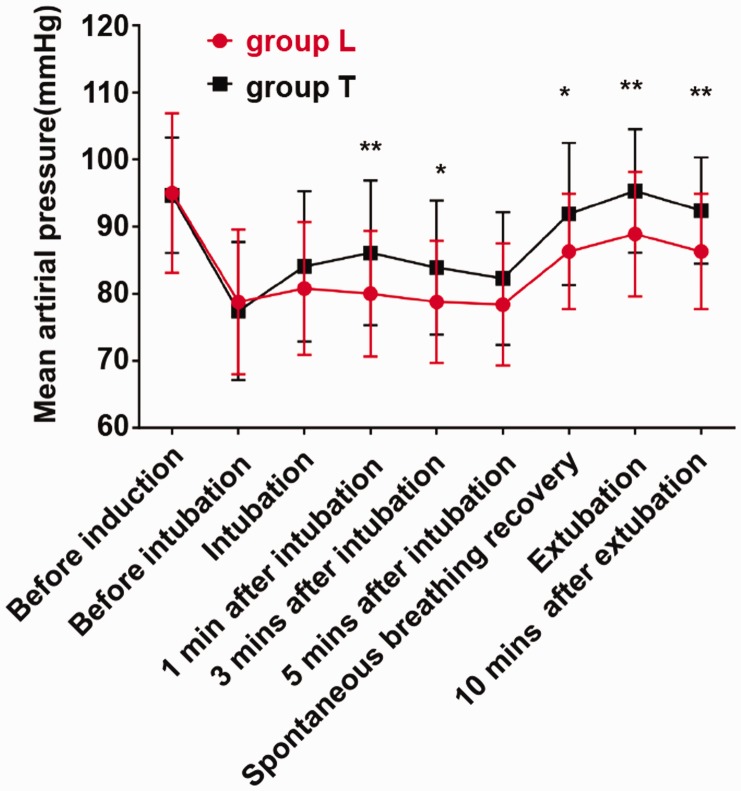
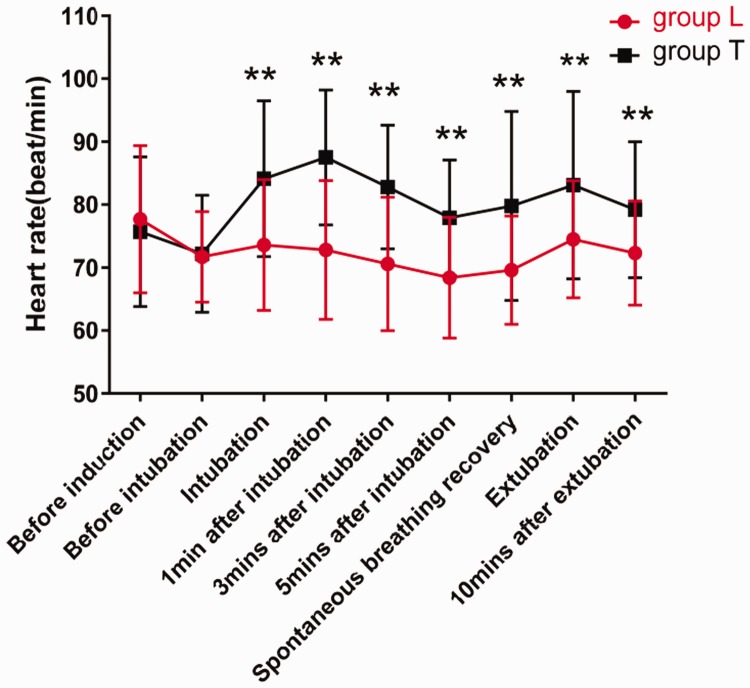
Intraoperative fluctuations of MAP and HR
MAP and HR were significantly different between the two groups and over time, and there was a significant interaction between group and time for the two parameters. Arterial pressure decreased to some extent after induction and before intubation but did not exceed 20% of the baseline value, and no drug treatment was needed. During intubation and extubation, the fluctuations of MAP and HR (i.e., the difference between the highest value and the baseline value) in the ETI group were 6 mmHg and 10 times/minute higher compared with those in the LMA group, respectively (p < 0.05, p < 0.01, Figures 1 and 2). The changes in HR were more intense and lasted longer in the ETI group compared with the LMA group. Nine patients in the ETI group and two patients in the LMA group were treated with esmolol during induction or recovery of anesthesia (p < 0.05, Table 1).
Figure 1.
MAP at different time points in the LMA and ETI groups. *p < 0.05 and **p < 0.01 versus ETI group, respectively. (Main effect: F, p = 6.103, 0.016, time effect: 51.541, <0.001, time-group interaction effect: 3.116, 0.048).
Figure 2.
HR at different time points in the LMA and ETI groups. **p < 0.01 versus ETI group. (Main effect: F, p = 18.839, <0.001, time effect: 10.699, <0.001, time-group interaction effect: 10.527, <0.001).
Insertion related parameters
There were no significant differences between the two groups in the success rate of the first insertion (92.5% vs. 92.5%), the first insertion following adjustment (7.5% vs. 0%), and secondary insertion (5.0% vs. 5.0%) (Table 2). Compared with the ETI group, the time of insertion was slightly longer in the LMA group, but there was no statistical difference (31.2±6.0 vs. 35.6±7.1 seconds, Table 2). The OLP in the LMA group was 22.2±1.5 cmH2O. One case of transient leak occurred in the LMA group, which was limited in time and did not cause other complications. The LMA was nudged in the oral cavity, and the air leak disappeared.
Table 2.
Comparison of insertion-related parameters between the LMA and ETI groups.
| LMA group (n = 40) | ETI group (n = 40) | T/χ2, p | |
|---|---|---|---|
| Insertion time (seconds) | 35.6 ± 7.1 | 31.2 ± 6.0 | 1.932, 0.057 |
| Ventilation achieved as planned [cases (%)] | 37 (92.5) | 37 (92.5) | 0.000, 1.000 |
| First success [cases (%)] | 32 (80.0) | 35 (87.5) | 1.420, 0.430 |
| First success by adjustment [cases (%)] | 3 (7.5) | 0 (0.0) | 3.117, 0.120 |
| Secondary success [cases (%)] | 2 (5.0) | 2 (5.0) | 2.636, 0.451 |
| OLP (cmH2O) | 22.2 ± 1.5 | none | – |
LMA, laryngeal mask; ETI, endotracheal intubation; OLP, oropharyngeal leakage pressure.
Intraoperative ventilation parameters
There was no significant difference in MV between the two groups regarding the ventilation parameters, while AP tended to increase from t0. The increase was not statistically significant in the ETI group at t1 compared with t0, but it was significant at t2 compared with t0 (p < 0.001, 95%CI: 0.270–0.680). The AP in the LMA group was significantly higher at t1 (p < 0.001, 95%CI: 1.308–2.342) and t2 (p < 0.001, 95%CI: 0.760–1.590) compared with t0. Compared with the LMA group, the AP in the ETI group was significantly decreased at t1 (p = 0.024, 95%CI: 0.153–2.097; Table 3).
Table 3.
Comparison of the ventilation parameters between the LMA and ETI groups.
|
MV (L/minute) |
AP (cmH2O) |
|||
|---|---|---|---|---|
| Time point | LMA group (n = 40) | ETI group (n = 40) | LMA group (n = 40) | ETI group (n = 40) |
| Completion of intubation (t0) | 5.5 ± 0.8 | 5.6 ± 1.1 | 14.1 ± 2.0 | 14.6 ± 1.5 |
| 60 minutes after the start of surgery (t1) | 5.5 ± 1.0 | 5.6 ± 1.0 | 15.9 ± 2.7**,# | 14.8 ± 1.4 |
| At the end of surgery (t2) | 5.5 ± 1.0 | 5.6 ± 1.0 | 15.2 ± 2.4** | 15.1 ± 1.3** |
| Integral analysis: Two-wayrepeated measures ANOVA: F, p | ||||
| Comparison between groups | 0.060, 0.808 | 0.375, 0.542 | ||
| Time point comparison | 2.367, 0.111 | 43.979, <0.001 | ||
| Time-group interaction effect | 0.938, 0.373 | 26.439, <0.001 | ||
**p < 0.01 versus t0 (completion of intubation), #p < 0.05 versus group ETI.
LMA, laryngeal mask; ETI, endotracheal intubation; ANOVA, analysis of variance; AP, airway pressure; MV, minute ventilation.
Anesthesia and postoperative recovery
The time for spontaneous respiratory recovery, extubation, ICU stay, feeding, and off-bed activity in the LMA group was significantly earlier or shorter compared with that of the ETI group (p < 0.05 for all results). The VAS score for sore throat was significantly higher in the ETI group compared with the LMA group at days 1 and 2 (p < 0.013; p < 0.001, respectively), while for the duration of postoperative pyrexia, there were no significant differences in the number of sore throats or the number of patients with post-operative pyrexia between the two groups at 24 hours after surgery (Table 4). The number of patients with cough (n = 37) was significantly higher in the ETI group (p < 0.01, Table 4) compared with the LMA group (n = 7).
Table 4.
Comparison of the quality of anesthesia and postoperative recovery between the LMA and ETI groups.
| LMA group (n = 40) | ETI group (n = 40) | T/χ2, p | |
|---|---|---|---|
| Number of patients with cough (cases) | 7 | 37 | 45.455, <0.001 |
| Number of cases of sore throat 24 hours after surgery (cases) | 20 | 23 | 0.453, 0.654 |
| VAS of postoperative sore throat | |||
| Day 1 | 2.9±1.2 | 3.6±1.1 | −2.538, 0.013 |
| Day 2 | 2.1±1.4 | 3.1±1.1 | −3.347, 0.001 |
| Day 3 | 0.7±1.2 | 1.1±1.3 | −1.238, 0.220 |
| Time for spontaneous respiratory recovery (minutes) | 39.5±34.1 | 71.4±34.9 | −3.856, <0.001 |
| Time from the end of surgery to extubation (minutes) | 76.1±37.1 | 104.1±41.5 | −3.509, 0.001 |
| Duration of stay in ICU (hour) | 4.9±1.8 | 8.8±3.2 | −6.673, <0.001 |
| Time from the end of the surgery to food and water intake (hour) | 6.9±2.2 | 12.0±5.0 | −5.812, <0.001 |
| Time from the end of the surgery to off-bed activity (day) | 3.6±1.5 | 5.2±3.6 | −2.337, 0.023 |
| Number of cases of postoperative pyrexia (cases) | 10 | 17 | 2.739, 0.155 |
| Duration of postoperative pyrexia (day) | 0.4±0.9 | 1.2±2.0 | −2.346, 0.023 |
LMA, laryngeal mask; ETI, endotracheal intubation; VAS, visual analog scale, ICU, intensive care unit.
Discussion
Although ETI remains the most common method for airway management, there are many disadvantages such as abnormality in hemodynamic and respiratory parameters, airway obstruction, difficult extubation, cuff-related problems, sore throat, laryngeal edema, hoarseness of voice, tension pneumothorax, and nerve injury. For patients undergoing neurosurgery, intracranial pressure may increase because of the stimulation during ETI and extubation, which may lead to intracranial hemorrhage, encephaledema, and even life-threatening cerebral hernia.5
The main factors that may affect the respiratory parameters during surgery include age, BMI, respiratory system diseases, surgical method, surgical position (which can lead to airway compression), and ventilation method (depending upon the ventilator settings).13–17 To minimize the confounding factors, we only used data from patients who were undergoing supratentorial craniotomy in the right lateral decubitus position, between 18 and 65 years of age, with a BMI of 18 to 30 kg/m2, and whose surgical duration was < 6 hours. The patients enrolled did not have respiratory system-related complications or excessive twisting of the head or neck.
Many complications that are associated with tracheal intubation can be avoided using an LMA, which does not cause stress from the laryngoscope and tracheal tube and allows a faster recovery.18,19 LMA has become an important choice, particularly in outpatient surgeries.18,19 Many short-duration surgery studies have demonstrated the device’s safety and effectiveness,20–22 but reports on the use of LMA in neurosurgical anesthesia are limited. Therefore, our study focused on comparing the effectiveness and feasibility of the Ambu® AuraOnce™ LMA and tracheal intubation during supratentorial craniotomy.
Perelló-Cerdà et al.1 reported that before the end of neurosurgery, replacing the endotracheal tube with a LMA can avoid severe fluctuations of hemodynamic parameters during extubation. In our study, the MAP and HR in the ETI group were 5 to 6 mmHg and 11 to 15 bpm higher compared with the LMA group, respectively. The HR response was more intense, and the duration was longer in the ETI group. These differences might be small, but they could be clinically important because minute variations in hemodynamic parameters might be clinically significant in patients undergoing intracranial surgery, especially for patients who have concomitant cardiovascular or cerebrovascular diseases.2 Although this study does not involve such a population, the results can still provide a reference value for the choice of anesthesia ventilation in such patients in the future. Additionally, esmolol was used in nine patients in the ETI group and two patients in the LMA group to control HR resulting from tachycardia during the induction or recovery of anesthesia. No vasoactive drugs were used in the two groups during surgery. Esmolol combined with propofol or sevoflurane can inhibit the intubation reaction and reduce the amount of propofol or sevoflurane administered, which is conducive to smooth and rapid recovery after surgery.23 However, there is still a risk of bradycardia; about 30% of patients may have transient bradycardia24 or the depth of anesthesia may be affected, resulting in shallow anesthesia. The above-mentioned adverse conditions did not occur in this study, but this may be because of the small sample size or the good heart function in the patients. Overall, non-pharmacological interventions to reduce or avoid fluctuations in hemodynamic parameters caused by ETI or endotracheal extubation are likely a result of the advantages and effectiveness of the LMA.
The insertion time and success rate of the first and final LMA insertion attempts were reported to be between 11.2±2.7 and 27.0±10.0 seconds in previous studies.25–27 Studies showed that the success rate of the first insertion attempt ranged from 83% to 92.5%25–27 in adults and 93% to 100%7,25,27,28 in children, while the success rate of final insertion was an average of 98%.26,29 In the present study, the LMA insertion time was 35.6 ± 7.1 seconds, which is slightly longer than that of the ETI (31.2 ± 6.0 seconds). The success rate of the first insertion attempt was 80% and the final success rate was 92.5%, which is slightly different from previous reports, and this might be because of differences in the anesthetists’ experience or the small number of patients who were included, but it would not have a clinical impact (in our study, pulse oximetry was 100% during intubation in all patients).
An OLP of LMA ≥20 cmH2O is considered to be safe and effective for mechanical ventilation in most patients.30 In the present study, the mean OLP in the LMA group was >20 cmH2O. The stability of the LMA position is very important for safe ventilation. The following two moments in the perioperative period can easily lead to change in the LMA position: when the patient is positioned from the supine position into the correct position, and when the cranium is drilled to mill the bone flap, which requires effective and timely communication among all staff to avoid any movement of the head and head frame that could compress the airway. The AP of the Proseal and the I-gel increases, decreases, or maintains the original level in the case of maximal flexion, extension, and leftward rotation of the neck, while the OLP changes to a corresponding degree of consistency.31 In the present study, after the successful placement of the ventilation device, preventive testing of the oropharyngeal leak at different head and neck angles was performed immediately. The AP in the LMA group was significantly higher at 60 minutes after the start of surgery compared with the ETI group, which might be attributed to the swing of the head that results from skull drilling, which could cause shifting of the LMA. However, the changes in AP in both groups did not affect normal ventilation. It is likely that the OLP also increased simultaneously to a certain extent, thus leading to safe ventilation. One case of transient leak occurred in the LMA group, which was limited in time and did not cause other complications.
Little has been reported on the comparison of ventilation parameters between the Ambu LMA and ETI. In our study, there was no significant difference in MV between the two groups during the perioperative period, which is consistent with earlier results.32,33
Compared with the ETI group, the LMA group had a lower incidence of cough and a lower VAS score for postoperative sore throat, and a shorter time for postoperative spontaneous breathing recovery, extubation, ICU stay, eating and drinking, off-bed activity, and duration of postoperative pyrexia, but their occurrence was too low and the total sample size was too small to draw any conclusions. Postoperative sore throat is listed as the eighth most serious adverse reaction after general anesthesia,34 which is a factor that affects the quality of postoperative recovery, overall postoperative satisfaction, and medical disputes. Postoperative sore throat may be an inflammatory response35 and it is closely related to pyrexia. Previous studies on LMA and ETI for sore throat after general anesthesia airway management had different conclusions.36–40 In the present study, there was no significant difference in the number of patients with postoperative sore throat and pyrexia between the two groups. LMA caused fewer complications during anesthesia convalescence, resulting in faster patient postoperative rehabilitation.
This study was a single-blind randomized trial, and only the Ambu® AuraOnce™ LMA was compared with ETI in patients undergoing supratentorial tumor resection in the right lateral decubitus position. An additional limitation is the absence of postoperative analgesia. This could be harmful to the patient and exaggerate the hypertensive effects of extubation. The effect of other types of LMAs on neurosurgery under different postures needs further investigation.
In conclusion, the results suggest that LMA could be used and could improve hemodynamic stability in patients who are undergoing supratentorial tumor resection in the right lateral decubitus position. Therefore, if there is a clinical need and no contraindication, after obtaining patient consent and in consultation with the surgeon, consideration may be given to replacing ETI with a laryngeal mask.
Acknowledgement
None.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The study was supported by the National Key Basic Research Development Programme (973 programme No. 2013CB531901).
ORCID iD
Baoguo Wang https://orcid.org/0000-0001-6879-8491
References
- 1.Perello-Cerda L, Fabregas N, Lopez AMet al. ProSeal laryngeal mask airway attenuates systemic and cerebral hemodynamic response during awakening of neurosurgical patients: A randomized clinical trial. J Neurosurg Anesthesiol 2015; 27: 194–202. [DOI] [PubMed] [Google Scholar]
- 2.Russo SG, Goetze B, Troche Set al. LMA-ProSeal for elective postoperative care on the intensive care unit: A prospective, randomized trial. Anesthesiology 2009; 111: 116–121. [DOI] [PubMed] [Google Scholar]
- 3.Carron M, Veronese S, Gomiero Wet al. Hemodynamic and hormonal stress responses to endotracheal tube and ProSeal laryngeal mask airway for laparoscopic gastric banding. Anesthesiology 2012; 117: 309–320. [DOI] [PubMed] [Google Scholar]
- 4.Wong AY, O’Regan AM, Irwin MG. Total intravenous anaesthesia with propofol and remifentanil for elective neurosurgical procedures: an audit of early postoperative complications. Eur J Anaesthesiol 2006; 23: 586–590. [DOI] [PubMed] [Google Scholar]
- 5.Bruder N, Pellissier D, Grillot Pet al. Cerebral hyperemia during recovery from general anesthesia in neurosurgical patients. Anesth Analg 2002; 94: 650–654; table of contents. [DOI] [PubMed] [Google Scholar]
- 6.Bruder N, Ortega D, Granthil C. [Consequences and prevention methods of hemodynamic changes during laryngoscopy and intratracheal intubation]. Ann Fr Anesth Reanim 1992; 11: 57–71. [DOI] [PubMed] [Google Scholar]
- 7.Sudhir G, Redfern D, Hall JEet al. A comparison of the disposable Ambu AuraOnce laryngeal mask with the reusable LMA Classic laryngeal mask airway. Anaesthesia 2007; 62: 719–722. [DOI] [PubMed] [Google Scholar]
- 8.Shah K. ProSeal laryngeal mask airway as an alternative to standard endotracheal tube in securing upper airway in the patients undergoing beating-heart coronary artery bypass grafting. Ann Card Anaesth 2017; 20: 61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atef HM, Fattah SA, Gaffer MEet al. Perfusion index versus non-invasive hemodynamic parameters during insertion of i-gel, classic laryngeal mask airway and endotracheal tube. Indian J Anaesth 2013; 57: 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marsh B, White M, Morton Net al. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth 1991; 67: 41–48. [DOI] [PubMed] [Google Scholar]
- 11.Bovill JG, Sebel PS, Blackburn CLet al. The pharmacokinetics of sufentanil in surgical patients. Anesthesiology 1984; 61: 502–506. [DOI] [PubMed] [Google Scholar]
- 12.Chow SC, Wang H and Shao J. Sample Size Calculations in Clinical Research. 2nd Ed. Florida: Chapman and Hall/CRC, 2007, p.58.
- 13.Salihoglu T, Salihoglu Z, Zengin AKet al. The impacts of super obesity versus morbid obesity on respiratory mechanics and simple hemodynamic parameters during bariatric surgery. Obes Surg 2013; 23: 379–383. [DOI] [PubMed] [Google Scholar]
- 14.Klasen J, Junger A, Hartmann Bet al. Increased body mass index and peri-operative risk in patients undergoing non-cardiac surgery. Obes Surg 2004; 14: 275–281. [DOI] [PubMed] [Google Scholar]
- 15.Nam Y, Yoon AM, Kim YHet al. The effect on respiratory mechanics when using a Jackson surgical table in the prone position during spinal surgery. Korean J Anesthesiol 2010; 59: 323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi SJ, Gwak MS, Ko JSet al. The effects of the exaggerated lithotomy position for radical perineal prostatectomy on respiratory mechanics. Anaesthesia 2006; 61: 439–443. [DOI] [PubMed] [Google Scholar]
- 17.Suh MK, Seong KW, Jung SHet al. The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol 2010; 59: 329–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hernandez MR Klock PA JrandOvassapian A.. Evolution of the extraglottic airway: A review of its history, applications, and practical tips for success. Anesth Analg 2012; 114: 349–368. [DOI] [PubMed] [Google Scholar]
- 19.van Zundert TC, Brimacombe JR, Ferson DZet al. Archie Brain: Celebrating 30 years of development in laryngeal mask airways. Anaesthesia 2012; 67: 1375–1385. [DOI] [PubMed] [Google Scholar]
- 20.Hagberg CA, Jensen FS, Genzwuerker HVet al. A multicenter study of the Ambu laryngeal mask in nonparalyzed, anesthetized patients. Anesth Analg 2005; 101: 1862–1866. [DOI] [PubMed] [Google Scholar]
- 21.Shariffuddin II, Wang CY. Randomised crossover comparison of the Ambu AuraOnce laryngeal mask with the LMA Classic laryngeal mask airway in paralysed anaesthetised patients. Anaesthesia 2008; 63: 82–85. [DOI] [PubMed] [Google Scholar]
- 22.Lopez AM, Valero R, Bovaira Pet al. A clinical evaluation of four disposable laryngeal masks in adult patients. J Clin Anesth 2008; 20: 514–520. [DOI] [PubMed] [Google Scholar]
- 23.Asouhidou I, Trikoupi A. Esmolol reduces anesthetic requirements thereby facilitating early extubation: A prospective controlled study in patients undergoing intracranial surgery. BMC Anesthesiol 2015; 15: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu SK, Tait G, Karkouti Ket al. The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg 2011; 112: 267–281. [DOI] [PubMed] [Google Scholar]
- 25.Williams DL, Zeng JM, Alexander KDet al. Randomised comparison of the AMBU AuraOnce laryngeal mask and the LMA unique laryngeal mask airway in spontaneously breathing adults. Anesthesiol Res Pract 2012; 2012: 405812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Theiler LG, Kleine-Brueggeney M, Luepold Bet al. Performance of the pediatric-sized i-gel compared with the Ambu AuraOnce laryngeal mask in anesthetized and ventilated children. Anesthesiology 2011; 115: 102–110. [DOI] [PubMed] [Google Scholar]
- 27.Heuer JF, Stiller M, Rathgeber Jet al. [Evaluation of the new supraglottic airway devices Ambu AuraOnce and Intersurgical i-gel. Positioning, sealing, patient comfort and airway morbidity]. Anaesthesist 2009; 58: 813–820. [DOI] [PubMed] [Google Scholar]
- 28.Suzanna AB, Liu CY, Rozaidi SWet al. Comparison between LMA-Classic and AMBU AuraOnce laryngeal mask airway in patients undergoing elective general anaesthesia with positive pressure ventilation. Med J Malaysia 2011; 66: 304–307. [PubMed] [Google Scholar]
- 29.Alzahem AM, Aqil M, Alzahrani TAet al. Ambu AuraOnce versus i-gel laryngeal mask airway in infants and children undergoing surgical procedures. A randomized controlled trial. Saudi Med J 2017; 38: 482–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keller C, Brimacombe JR, Keller Ket al. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 1999; 82: 286–287. [DOI] [PubMed] [Google Scholar]
- 31.Mishra SK, Nawaz M, Satyapraksh MVet al. Influence of head and neck position on oropharyngeal leak pressure and cuff position with the ProSeal laryngeal mask airway and the I-Gel: A randomized clinical trial. Anesthesiol Res Pract 2015; 2015: 705869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang C, Chai X, Kang Fet al. I-gel laryngeal mask airway combined with tracheal intubation attenuate systemic stress response in patients undergoing posterior fossa surgery. Mediators Inflamm 2015; 2015: 965925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai CJ, Liu CM, Wu CYet al. I-Gel is a suitable alternative to endotracheal tubes in the laparoscopic pneumoperitoneum and Trendelenburg position. BMC Anesthesiol 2017; 17: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Venugopal A, Jacob RM, Koshy RC. A randomized control study comparing the pharyngolaryngeal morbidity of laryngeal mask airway versus endotracheal tube. Anesth Essays Res 2016; 10: 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Puyo CA, Peruzzi D, Earhart Aet al. Endotracheal tube-induced sore throat pain and inflammation is coupled to the release of mitochondrial DNA. Mol Pain 2017; 13: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joshi GP, Inagaki Y, White PFet al. Use of the laryngeal mask airway as an alternative to the tracheal tube during ambulatory anesthesia. Anesth Analg 1997; 85: 573–577. [DOI] [PubMed] [Google Scholar]
- 37.Fujii Y, Tanaka H, Toyooka H. [Effects of laryngeal mask airway on circulation and on incidence of postoperative sore throat and hoarseness]. Masui 1993; 42: 1659–1662. [PubMed] [Google Scholar]
- 38.Rieger A, Brunne B, Hass Iet al. Laryngo-pharyngeal complaints following laryngeal mask airway and endotracheal intubation. J Clin Anesth 1997; 9: 42–47. [DOI] [PubMed] [Google Scholar]
- 39.Splinter WM, Smallman B, Rhine EJet al. Postoperative sore throat in children and the laryngeal mask airway. Can J Anaesth 1994; 41: 1081–1083. [DOI] [PubMed] [Google Scholar]
- 40.Mizutamari E, Yano T, Ushijima Ket al. A comparison of postoperative sore throat after use of laryngeal mask airway and tracheal tube. J Anesth 2004; 18: 151–157. [DOI] [PubMed] [Google Scholar]