Short abstract
Objective
The relationship between the use of screws and acetabular cup stability in total hip arthroplasty (THA) remains controversial. We evaluated cup stability in THA with and without the use of screws.
Methods
We performed a systematic literature search to identify studies on cup stability relative to the use of screws in patients undergoing THA before October 2018. Methodological quality assessment and data collection were performed by two individual reviewers. Meta-analysis was performed using Review Manager version 5.3.5.
Results
We included seven trials involving 1402 patients (1469 THAs): 767 patients (809 THAs) with screws and 635 patients (660 THAs) without screws. The findings of meta-analysis indicated that uncemented acetabular component fixation with the use of additional screws was not correlated with migration of the cup, migration on roentgen stereophotogrammetry, or reoperation after THA. Moreover, operation time was not significantly different according to whether screws were used. There was no relationship between use of additional screws and osteoporosis or Harris Hip Score; however, THA with or without the use of screws might be related to bone sclerosis in the C1 region.
Conclusion
Currently, limited evidence shows that the use of screws during THA may not improve cup stability.
Keywords: Total hip arthroplasty, cup stability, screws, meta-analysis, reoperation, uncemented acetabular component fixation
PROSPERO: CRD42019126410
Introduction
Total hip arthroplasty (THA) is among the most successful orthopedic procedures worldwide. For acute and chronic hip diseases, THA can relieve joint pain, correct deformities, and restore and improve hip function.1 Despite the initial use of cemented fixation, which remains satisfactory in many cases, uncemented fixation has gained popularity owing to improvements in metal implants and surface treatments. However, a variety of complications may lead to failure of THA.2
Loosening and migration of the acetabular cup are the main reasons for THA failure.3 Saito et al. reported cup loosening rates of 42% in the first 8 years after THA and 60% after 8 years.4 Recently, with the detailed design of acetabular cups and emergence of new materials,5 cups are widely used clinically, especially those with a porous coating and hemispherical design, which ensure good stability and durability of the press-fit cup.6,7 In a study of 4289 patients who underwent THA with uncemented acetabular cups, the results suggested that patients with the highest 15-year survival rate were those who used press-fit cups.8 Nevertheless, some studies have shown that press-fit cups made of new materials still have a possibility of aseptic loosening among less than 5% of patients in 10 years.9 Therefore, some scholars have proposed that uncemented acetabular component fixation can be supported by the use of screws, particularly in osteopenic bone.10,11 However, there are no data regarding significant advantages of the use of screws; thus, the usefulness of this approach remains uncertain.
We proposed the following hypothesis: additional screw fixation can improve initial stability of the acetabular cup and reduce the occurrence of cup migration. We examined the findings of evidence-based medicine to investigate the effect of uncemented acetabular component fixation with or without additional screw fixation on cup stability, to provide evidence for clinical applications.
Methods
Inclusion criteria
In this study, the inclusion criteria were as follows. 1) Research type: Randomized controlled trials (RCTs) or observational studies (OSs, including cohort studies and case-control studies). 2) Research participants: Adult patients (age > 18 years) with unilateral or bilateral osteoarthritis, traumatic arthritis, or avascular necrosis of the femoral head requiring initial THA; patients undergoing revision surgery were excluded. 3) Intervention measures: Patients with THA were divided into a screw-fixed group and a non-screw-fixed group; the former group included patients with screw-fixed press-fit cups whereas no screws were used in the latter group. 4) Measurement indexes: Migration of the cup, all-cause reoperation, operative time, postoperative bone changes, and Harris Hip Score (HHS) among patients with THA in both groups; short-term bone changes after surgery include osteosclerosis and decreased bone density.
Search strategy
According to the Cochrane Handbook for Systematic Reviews of Interventions, we searched PubMed, Embase, and the Cochrane Library using the following terms: “arthroplasty, replacement, hip”, “hip replacement”, “hip arthroplasty”, “screw”, “press-fit”, and “cup”. We also searched for “hip replacement, hip arthroplasty, screw, acetabulum cup” in SinoMed, China National Knowledge Infrastructure (CNKI), and Chongqing VIP Information Co., Ltd (CQVIP). The search timeline was from database inception to October 2018. There were no other restrictions on the search process, and we included studies published in English and Chinese language.
Data extraction and quality assessment
Two trained professional reviewers independently read the full text of articles that met the inclusion criteria and extracted the specific details of study design and measurement index data. Quality of the included RCTs was assessed using the criteria provided in the Cochrane Handbook, including adequate random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting bias, and other bias. Assessment of the quality of OSs was done using the Newcastle–Ottawa Scale (NOS),12 including population selection, population comparability, exposure assessment, and outcome assessment.
All analyses in this work were based on previously published studies; therefore, no ethics approval or patient consent were required.
Statistical analysis
Statistical analysis was performed using Review Manager (RevMan) Version 5.3.5. We used the odds ratio (OR) and mean difference (MD) to indicate the effect size of count data and continuous variables, respectively, and calculated the 95% confidence interval (CI). Fixed-effects model analysis was used when the statistical heterogeneity among the studies was small (P > 0.1, I2 < 50%). When statistical heterogeneity among the studies was large (P < 0.1, I2 > 50%), then the possible sources of heterogeneity and possible interference factors were analyzed. If there was only statistical heterogeneity but no clinical heterogeneity, the random-effects model was used with pooled data.13 If there were small probability events or the data could not be analyzed, general description was used for qualitative evaluation. A P value < 0.05 was used to indicate statistical significance.
Results
Literature search and results
A total of 376 studies were identified in the database search. After excluding 104 duplicated studies, the reviewers read the titles and abstracts of the remaining studies, and then excluded 244 unrelated studies such as reviews, animal experiments, and biomechanical analyses, leaving 28 studies. After reading the full text and excluding 21 studies with no indicators of interest, seven studies were finally included.14–20
General information of the included studies
Among the seven included studies,14–20 one article was published in Chinese;20 three were RCTs16,17,19 and the remaining four were OSs.14,15,18,20 These studies were published from 2000 to 2012. The studies included 1402 patients (1469 THAs) with a baseline comparable between the groups in each study: 767 patients (809 THAs) in the screw-fixed group and 635 patients (660 THAs) in the non-screw-fixed group. The age range of patients was 32 to 89 years old. The number of screws (mostly one to three) used for fixing the cup varied between studies. Follow-up was from 2 to 9 years after THA. Specific baseline information for the included studies is shown in Table 1.
Table 1.
Specific baseline information for included studies.
| Study | Type | Number of hip joints | Age (years) | Inclusion criteria | Surgical approach | Composition of artificial hip joint | Screw usage | Follow-up time (years) |
|---|---|---|---|---|---|---|---|---|
| Thanner 2000 | ||||||||
| Screw-fixed group | RCT | 30 | 56 (32–75) | Patients requiring THA | Modified Hardinge approach | Trilogy cup; cemented and uncemented femoral stem | 1–3 screws | 2 |
| Non-screw-fixed group | 34 | 56 (32–75) | 0 | |||||
| Rohrl 2004 | ||||||||
| Screw-fixed group | RCT | 22 | 56 (40–65) | Primary or secondary osteoarthritis | Posterior approach | Polyethylene liner cup, 28-mm femoral head | – | 5 |
| Non-screw-fixed group | 21 | 56 (36–65) | 0 | |||||
| Pakvis 2012 | ||||||||
| Screw-fixed group | RCT | 18 | 64 ± 8 | Primary osteoarthritis | Posterolateral approach | RM Pressfit Cup (Switzerland); CLS femoral stem; 32-mm ceramic polyethylene articulation head | 2 screws | 2 |
| Non-screw-fixed group | 19 | 62 ± 6 | 0 | |||||
| Roth 2006 | ||||||||
| Screw-fixed group | OS | 110 | 61–72 | Patients requiring THA | Posterior approach | DURALOC cup | 1–3 screws | 5 |
| Non-screw-fixed group | 101 | 61–72 | 0 | |||||
| Iorio 2010 | ||||||||
| Screw-fixed group | OS | 509 | 67.16 (32–89) | Patients with osteoarthritis or traumatic arthritis | – | Press-Fit Condylar, DURALOC, Pinnacle cup; cemented and uncemented femoral stem; 28-mm and 32-mm femoral head | 109 hips using 1 screw; 335 hips using 2 screws; 59 hips using 3 screws; 6 hips using 4 or more screws | 6.32 |
| Non-screw-fixed group | 266 | 66.68 (39–88) | 0 | 6.9 | ||||
| Liang 2011 | ||||||||
| Screw-fixed group | OS | 32 | 50.25 ± 10.85 | Patients requiring THA | Anterolateral approach | DURALOC cup | 1–2 screws | 2 |
| Non-screw-fixed group | 30 | 50.06 ± 11.33 | 0 | |||||
| Garcia-Rey 2012 | ||||||||
| Screw-fixed group | OS | 88 | 47.9 ± 15.9 | Osteoarthrosis, developmental traumatic arthritis, inflammatory arthritis, avascular necrosis of the femoral head | Posterolateral approach | Cerafit Triradius press-fit cup (France); Cerafit Multicone femoral stem; 28-mm and 32-mm femoral head | 2 screws | 8.9 |
| Non-screw-fixed group | 189 | 51.9 ± 12.3 | 0 |
Abbreviations: RCT, randomized controlled trial; OS, observational study.
Quality assessment
Among RCT studies, Thanner 200019 used random grouping, but did not report the generation of sequences, allocation concealment, and blinding; Rohrl 200417 used sealed envelopes for allocation concealment, but did not mention blinding; Pakvis 201216 used a computer randomization sequence and sealed envelopes to conceal the allocation scheme, as well as blinding. The other bias in these RCTs was low risk. In quality assessment of OSs using the NOS, the scores for Roth 2006,18 Iorio 2010,15 Liang 2011,20 Garcia-Rey 201214 were 7, 6, 4, and 8, respectively.
Clinical efficacy
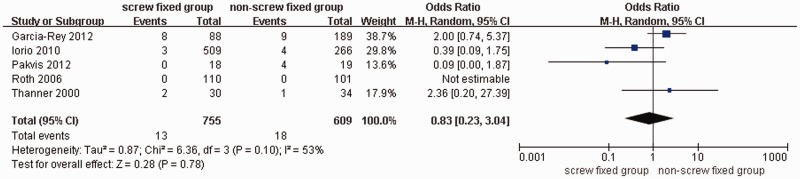
Cup migration
The overall heterogeneity of the included studies was high (I2 = 53%). After random-effects model analysis, we found no significant difference in the occurrence of acetabular cup migration between the screw-fixed and non-screw-fixed groups (OR = 0.83; 95% CI: 0.23–3.04). In other words, the use of screws may not influence cup migration (Figure 1). Similarly, the difference was not significant (OR = 1.19; 95% CI: 0.38–3.75), after removing Pakvis 2012,16 and the heterogeneity was low (I2 = 42%).
Figure 1.
Forest plot of cup migration in screw-fixed and non-screw-fixed groups.
M-H, Mantel–Haenszel.
Roentgen stereogrammetric analysis (RSA) evaluation
Three studies used RSA to measure the spatial position and rotation of the cup. The RSA evaluation system measures cup medial–lateral, distal–proximal, anterior–posterior displacements and rotation of the prosthesis according to the transverse, longitudinal, and sagittal axes; the heterogeneity was I2 = 0% for all measures. Fixed-effects model analysis indicated that the displacement and angle change of the cup in the above six directions or planes were as follows: (MD = −0.06; 95% CI: −0.31–0.19), (MD = −0.14; 95% CI: −0.27–0.00), (MD = 0.05; 95% CI: −0.22–0.32), (MD = 0.23; 95% CI: −0.20–0.66), (MD = 0.46; 95% CI: −0.27–1.18), and (MD = −0.06; 95% CI: −0.55–0.44), respectively. RSA measurement suggests that screw fixation may not be associated with displacement (Figure 2).
Figure 2.
Forest plot of roentgen stereogrammetric analysis between screw-fixed and non-screw-fixed groups.
IV, inverse variance.
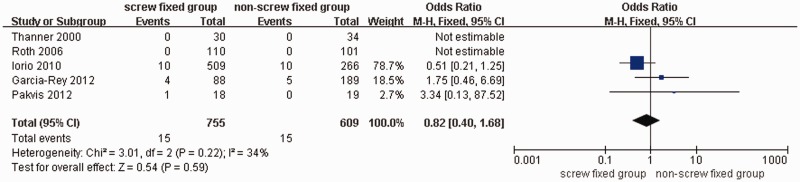
All-cause reoperation rate
Among five of the included studies, Roth 200618 and Thanner 200019 reported no reoperation during the follow-up period in either group. Owing to the low heterogeneity, meta-analysis using the fixed-effects model revealed that there was no significant difference (OR = 0.82; 95% CI: 0.40–1.68) in the occurrence of reoperation between the screw-fixed and non-screw-fixed groups (Figure 3). To verify stability of the results, we conducted a sensitivity analysis: after removing the most weighted study, that of Iorio 2010,15 the results showed no significant difference in the occurrence of reoperation between the screw-fixed and non-screw-fixed group (OR = 1.96; 95% CI: 0.57–6.66) and the heterogeneity was low (I2 = 0%).
Figure 3.
Forest plot of reoperation in screw-fixed and non-screw-fixed groups.
Operative time
Two studies compared operation time between the two groups, but the heterogeneity was high (I2 = 94%, P < 0.0001). After verification, no significant clinical heterogeneity was found between the two groups. The pooled results from the random-effects model suggested no significant difference in the length of operation time between the two groups (MD = 8.85; 95% CI: −7.85–25.56), as shown in Figure 4.
Figure 4.
Forest plot of operative time in screw-fixed and non-screw-fixed groups.
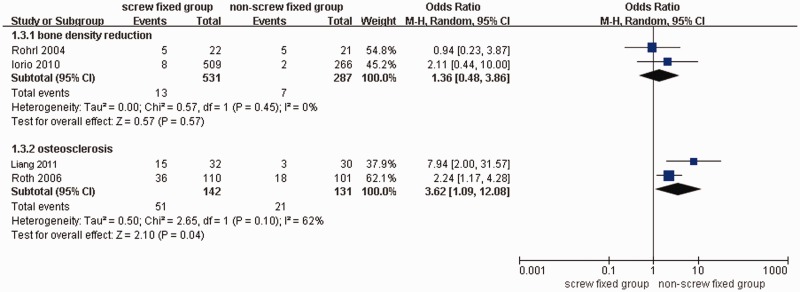
Postoperative bone change
Four studies reported postoperative hip bone changes in both groups. The heterogeneity of bone density reduction around the cup was low (I2 = 0%), and the results suggested that whether screws are used is not related to bone density reduction around the cup (OR = 1.36; 95% CI: 0.48–3.86). Additionally, heterogeneity of osteosclerosis in the C1 region of the DeLee and Charnley zone was high (I2 = 62%). Verification showed that Liang 201120 and Roth 200618 both reported that bone sclerosis in the C1 region occurred within 5 months after operation; the former study used one to two screws and the latter used one to three screws. The results of random-effects model analysis suggested that screw fixation may be related to bone sclerosis in the C1 region (OR = 3.62; 95% CI: 1.09–12.08; P = 0.04), as shown in Figure 5.
Figure 5.
Forest plot of bone changes in screw-fixed and non-screw-fixed groups.
HHS functional score
Three studies evaluated the HHS of hip function in the two groups. The heterogeneity was high (I2 = 57%), probably owing to differences in the time of postoperative evaluation. The results from the random-effects model suggested that screw fixation may not be related to the HHS (MD = −1.03; 95% CI: −3.58–1.53), as shown in Figure 6.
Figure 6.
Forest plot of Harris hip scores in screw-fixed and non-screw-fixed groups.
Discussion
In THA, doubts remain as to whether the press-fit acetabular component should be fixed with screws.18 Additional screws may damage important nerves and blood vessels,21 and wear of the screws may lead to osteolysis.22 To assess the relationship between the use of screws and cup stability, we conducted the present meta-analysis and found that additional screw fixation may not be associated with postoperative cup migration, RSA cup displacement or rotation, all-cause reoperation, length of operation, reduction of bone density around the cup, or HHS functional score, but use of additional screws may be associated with bone sclerosis in the C1 region of the hip.
The stability of the cup is an important index that reflects the outcome of THA. We analyzed the occurrence of cup migration and RSA evaluation and used OR, MD, and sensitivity analysis; we found that additional screw fixation had no significant effect on stability of the cup. The incidence of cup migration with screws was 1.72% (13/755) and that without screws was 2.96% (18/609). There are many factors affecting cup stability, including patient age, bone condition, cup surface coating, cup coverage rate, and cup placement.23 However, degenerative changes in the bone around the cup are the direct cause of cup loosening.24,25 Therefore, it is necessary to evaluate the patient’s characteristics before surgery. In addition, screw fixation had no effect on all-cause reoperation. In this meta-analysis, the main causes of all-cause reoperation were loosening of the acetabular cup or femoral stem prosthesis, followed by joint dislocation and local infection. The all-cause reoperation rate was 1.98% (15/755) in the screw-fixed group and 2.46% (15/609) in the non-screw-fixed group. Only two studies provided a comparison of operative time, with a high heterogeneity, which may be related to operations conducted by different surgeons. The Harris hip functional score, an important indicator of life quality, did not show that additional screw fixation can improve the clinical prognosis of patients.
A problem requiring attention is that additional screw fixation may cause sclerosis of the C1 region in the DeLee and Charnley zone of the hip.26 Roth et al. identified this phenomenon in the C1 region of the acetabulum after additional screw fixation. This phenomenon may be related to the unbalanced force exerted by the screws, as the fulcrum of acetabular prostheses,18 which may lead to the hypothesis that additional screws are not conducive to cup stability. Screws may not only promote peripheral bone changes22 but may also damage nerves and blood vessels;21 only a few of our included studies mentioned this complication. Particularly for patients in whom multiple screws are used for fixation, greater attention should be paid to this potential problem. Thus, there is no direct evidence that additional screw fixation can improve the initial stability of the cup and reduce the occurrence of cup loosening after THA.
Our study has some limitations. First, the timing of the RCT and OS studies included in this study is inconsistent, and the internal design of each study also has varying degrees of deficiency; these factors will affect the authenticity of our results. Second, the question remains as to whether using screws to fix the acetabular cup is related to the quality and coverage of the autologous bone, however, none of the seven studies considered this factor. Third, older cups used in long-term studies often had a relatively smooth surface whereas modern cups have a much higher coefficient of friction. These differences influence the need for screws, and opinions about the use of screws will likely change in the future. These limitations suggest that a prospective large-sample RCT is needed, to clarify the causal relationship between screw fixation, cup stability, and patient prognosis.
We can conclude that currently, limited evidence shows that the use of screws during THA may not improve stability of the cup.
Acknowledgement
We thank all the authors who contributed to this article.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was supported by the Social Development Foundation of Shaanxi Province (2017ZDXM-SF-009).
ORCID iDs
Chen Fei https://orcid.org/0000-0003-4390-1469
Yan Zhuang https://orcid.org/0000-0002-6816-3071
References
- 1.Jeldi A, Grant P, Granat Met al. Physical activity in hospital following total hip replacement: an objective analysis. Gait Posture 2014; 39: S96–S97. [Google Scholar]
- 2.Badarudeen S, Shu AC, Ong KLet al. Complications After Revision Total Hip Arthroplasty in the Medicare Population. J Arthroplasty 2017; 32: 1954–1958. DOI: 10.1016/j.arth.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 3.Zilkens C, Djalali S, Bittersohl Bet al. Migration pattern of cementless press fit cups in the presence of stabilizing screws in total hip arthroplasty. Eur J Med Res 2011; 16: 127–132. DOI: 10.1186/2047-783x-16-3-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saito S, Saito M, Nishina Tet al. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res 1989; 244: 198–207. [PubMed] [Google Scholar]
- 5.Valle AG, Zoppi A, Peterson MGet al. Clinical and radiographic results associated with a modern, cementless modular cup design in total hip arthroplasty. J Bone Joint Surg Am 2004; 86: 1998–2004. DOI: 10.2106/00004623-200409000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Fehring KA, Owen JR, Kurdin AAet al. Initial stability of press-fit acetabular components under rotational forces. J Arthroplasty 2014; 29: 1038–1042. DOI: 10.1016/j.arth.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Streit MR, Weiss S, Andreas Fet al. 10-year results of the uncemented Allofit press-fit cup in young patients. Acta Orthop 2014; 85: 368–374. DOI: 10.3109/17453674.2014.925351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engh CA Hopper RH JrandEngh CA Jr.. Long-term porous-coated cup survivorship using spikes, screws, and press-fitting for initial fixation. J Arthroplasty 2004; 19: 54–60. DOI: 10.1016/j.arth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Rey E, Garcia-Cimbrelo E, Cordero-Ampuero J. Outcome of a hemispherical porous-coated acetabular component with a proximally hydroxyapatite-coated anatomical femoral component: a 12- to 15-year follow-up study. J Bone Joint Surg Br 2009; 91: 327–332. DOI: 10.1302/0301-620X.91B3.20947. [DOI] [PubMed] [Google Scholar]
- 10.Parvizi J, Sullivan T, Duffy Get al. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty 2004; 19: 672–677. DOI: 10.1016/j.arth.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Utting MR, Raghuvanshi M, Amirfeyz Ret al. The Harris-Galante porous-coated, hemispherical, polyethylene-lined acetabular component in patients under 50 years of age: a 12- to 16-year review. J Bone Joint Surg Br 2008; 90: 1422–1427. DOI: 10.1302/0301-620X.90B11.20892. [DOI] [PubMed] [Google Scholar]
- 12.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603–605. DOI: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJet al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. DOI: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia-Rey E, Garcia-Cimbrelo E, Cruz-Pardos A. Cup press fit in uncemented THA depends on sex, acetabular shape, and surgical technique. Clin Orthop Relat Res 2012; 470: 3014–3023. DOI: 10.1007/s11999-012-2381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iorio R, Puskas B, Healy WLet al. Cementless acetabular fixation with and without screws: analysis of stability and migration. J Arthroplasty 2010; 25: 309–313. DOI: 10.1016/j.arth.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Pakvis D, Luites J, van Hellemondt Get al. A cementless, elastic press-fit socket with and without screws. Acta Orthop 2012; 83: 481–487. DOI: 10.3109/17453674.2012.720116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rohrl SM, Nivbrant B, Strom Het al. Effect of augmented cup fixation on stability, wear, and osteolysis: a 5-year follow-up of total hip arthroplasty with RSA. J Arthroplasty 2004; 19: 962–971. DOI: 10.1016/j.arth.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 18.Roth A, Winzer T, Sander Ket al. Press fit fixation of cementless cups: how much stability do we need indeed? Arch Orthop Trauma Surg 2006; 126: 77–81. DOI: 10.1007/s00402-005-0001-9. [DOI] [PubMed] [Google Scholar]
- 19.Thanner J, Karrholm J, Herberts Pet al. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation: a randomized study of 64 hips. J Arthroplasty 2000; 15: 405–412. DOI: 10.1054/arth.2000.2963. [DOI] [PubMed] [Google Scholar]
- 20.Liang WB. Effect of technique with and without screw on stability of cup in total hip arthroplasty. 2011. Retrieved from https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2011&filename=1011088800.nh&v=MTI2MTViUElSOGVYMUx1eFlTN0RoMVQzcVRyV00xRnJDVVI3cWZadVJtRkNubVc3L05WRjI2SDdPd0Z0bk1yNUU=.
- 21.Barrack RL. Neurovascular injury: avoiding catastrophe. J Arthroplasty 2004; 19: 104–107. DOI: 10.1016/j.arth.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Rohrl SM, Nivbrant B, Snorrason Fet al. Porous-coated cups fixed with screws: a 12-year clinical and radiostereometric follow-up study of 50 hips. Acta Orthop 2006; 77: 393–401. DOI: 10.1080/17453670610046316. [DOI] [PubMed] [Google Scholar]
- 23.Lu Z, Ebramzadeh E. Origins of material loss in highly worn acetabular cups of metal-on-metal total hip replacements. J Orthop Res 2019; 37: 143–150. DOI: 10.1002/jor.24139. [DOI] [PubMed] [Google Scholar]
- 24.Alshuhri AA, Holsgrove TP, Miles AWet al. Non-invasive vibrometry-based diagnostic detection of acetabular cup loosening in total hip replacement (THR). Med Eng Phys 2017; 48: 188–195. DOI: 10.1016/j.medengphy.2017.06.037. [DOI] [PubMed] [Google Scholar]
- 25.Dorr LD, Bechtol CO, Watkins RGet al. Radiographic anatomic structure of the arthritic acetabulum and its influence on total hip arthroplasty. J Arthroplasty 2000; 15: 890–900. DOI: 10.1054/arth.2000.8323. [DOI] [PubMed] [Google Scholar]
- 26.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976; 121: 20–32. [PubMed] [Google Scholar]