Abstract
Lymphadenopathy refers to any disease process involving lymph nodes that are abnormal in size and consistency. Lymphadenitis specifically refers to lymphadenopathies that are caused by inflammatory processes. Cervical lymphadenopathy is a common problem in the pediatric age group and is largely inflammatory and infectious in etiology. Although most patients are treated successfully by their primary care physician, surgical consultation is frequently required for patients who fail to respond to initial therapy or for those in whom there is an index of suspicion for a neoplastic process. This article addresses current approaches to the diagnosis and management of cervical lymphadenitis in children.
Index words: Cervical lymphadenitis, Acute viral lymphadenitis, Acute bacterial lymphadenitis, Mycobacterial lymphadenitis, Cat-scratch disease
Lymphadenopathy refers to any disease process involving lymph nodes that are abnormal in size and consistency. This condition has multiple etiologies, the most common of which are neoplasia, autoimmune diseases, and infection. Lymphadenitis refers to lymphadenopathies that are due to inflammatory processes. It is characterized not only by nodal swelling, but also by pain, skin changes, fever, edema, and/or purulent collections. In the pediatric age group, most lymphadenopathies are attributable to an infectious etiology.
Cervical lymphadenitis is a common pediatric problem, and most patients with this condition are treated successfully by their primary care physicians. Surgical consultation is, however, often required to assist in the diagnosis and treatment of patients who do not respond to initial therapy or in whom there is an index of suspicion for a neoplastic process. This article addresses contemporary approaches to the diagnosis and management of cervical lymphadenitis in the pediatric age group.
Anatomy and physiology
Although lymph nodes are located throughout the lymphatic system, they are concentrated in certain areas of the body, including the head and neck. Because infectious processes involving the oropharyngeal structures are common in children, cervical lymphadenitis is also common in this age group.
Lymphatic drainage follows well-defined patterns. As such, the location of the enlarged lymph node is a good indication of the likely site of entry of the inciting organism (Figure 1). Involvement of superficial or deep cervical lymph nodes is also frequently indicative of the site of entry since superficial nodal enlargement usually reflects invasion through an epithelial surface (eg, buccal mucosa, skin, scalp), whereas deep nodal enlargement results from an infectious process involving more central structures (eg, middle ear, posterior pharynx).
Figure 1.
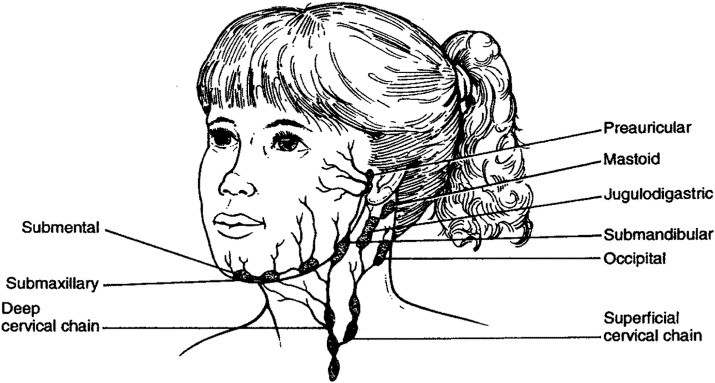
Lymphatic drainage and nodal regions in the head and neck. (Reprinted with permission.2)
Lymph nodes contain T- and B-lymphocytes as well as antigen-presenting macrophages (dendritic cells). Tissue lymph enters the lymph node via one or more afferent vessels and percolates through a series of reticuloendothelial-lined channels that coalesce and drain through an efferent lymphatic vessel. Particulate matter is phagocytosed by macrophages lining the lymphatic channels. Once phagocytized, foreign proteins become bound to major histocompatibility (MHC) antigens and are presented on the surface of macrophages. Foreign proteins bound to MHC class II molecules on the surface of dendritic cells, in combination with other cell surface receptors and secreted cellular signals (interleukins), are required for activation of T-helper lymphocytes. These lymphocytes can in turn activate naïve B-lymphocytes. Alternatively, memory B-lymphocytes may be directly activated by dendritic cells. Once activated, B- and T-lymphocytes proliferate to create a pool of lymphocytes that have the ability to recognize and bind the inciting foreign protein. In addition, activated T-lymphocytes and macrophages release cellular signals (cytokines) that induce leukocyte chemotaxis and increase vascular permeability.
The symptoms associated with acute cervical lymphadenitis reflect these pathophysiologic events. Nodal enlargement occurs as a result of cellular hyperplasia, leukocyte infiltration, and tissue edema. Vasodilation and capillary leak in response to locally released cytokines causes erythema and edema of the overlying skin, and tenderness results from distention of the nodal capsule.
Evaluation
History and physical examination
A thorough history and complete physical examination often suggests the probable cause of cervical lymphadenitis. Consideration of whether symptoms and presentation are acute, subacute, or chronic is often helpful in establishing a differential diagnosis. Clearly, the definitions of these categories are arbitrary, and many infectious processes are associated with symptom duration that fits into more than one category. In general, however, acute lymphadenitis, which can be 2 weeks in duration, is due to either a viral or bacterial invasion. Chronic lymphadenopathy is more likely to be due to a neoplastic process or invasion by an opportunistic organism. Subacute lymphadenitis, which is 2 and 6 weeks in duration, encompasses a much broader group of potential etiologies. In practice, surgeons seldom are involved in the care of patients with acute lymphadenitis unless the lymph nodes become suppurative. Most of these patients improve during a course of antibiotic therapy prescribed by their primary care physician.
Other important clinical information to obtain are the location (single or multiple sites) and progress of neck swelling (increasing, stable, or decreasing) and the presence of systemic symptoms (eg, fever, malaise, anorexia, weight loss, or arthralgias). More specific symptoms include skin changes and pain in the region of the nodal swelling, as well as at more distant sites. A history of recent upper respiratory tract symptoms, sore throat, ear pain, toothache, insect bites, superficial lacerations or rashes, and exposure to animals may suggest possible etiologies. In addition, a history of recent travel, exposure to individuals that are ill, and immunization status should be sought. Finally, patient age is another important consideration, since lymphadenopathy in young children is overwhelmingly due to infectious etiologies, whereas adenopathy due to neoplasia increases in the adolescent age group.
Findings on physical examination may also suggest an etiology. Cervical lymph nodes are frequently palpable in children; however, lymph nodes larger than 10 mm in diameter are considered abnormal. As noted previously, the location of involved nodes may indicate a potential site of entry and should prompt a detailed examination of that site. Erythema, tenderness, and fluctuance suggest an acute process, most likely attributable to a bacterial invasion. Involvement of bilateral cervical lymph nodes suggests a viral origin. The characteristics of the nodes are also important. Nodes involved in neoplastic processes frequently are firm and fixed, whereas those due to infectious agents tend to be softer in consistency and often slightly mobile. Other physical abnormalities, including respiratory findings, skin lesions, hepatosplenomegaly, and adenopathy in other parts of the body may also suggest an etiology.
Finally, it is important to keep in mind that not all swellings in the neck represent enlarged lymph nodes and that congenital and acquired cysts and soft tissue lesions also present as neck masses. Often the nonnodal nature of these masses is suggested by the history or by the findings on physical examination. In equivocal cases, however, diagnostic imaging almost always reveals whether a particular swelling is due to nodal enlargement or to a cyst or soft tissue mass.
Laboratory evaluation
Laboratory tests are seldom required as part of the workup for acute cervical lymphadenitis. Leukocyte counts and markers of inflammation (C-reactive protein and erythrocyte sedimentation rate) are usually abnormal but nonspecific. Although a left shift (ie, increased percentage of immature white cells) on the leukocyte differential count suggests a bacterial etiology, this etiology frequently is suggested by the clinical presentation alone. Any material that has been aspirated due to fluctuance should be sent for culture and sensitivity. These cultures may show an organism that is resistant to prior antibiotic therapy, but occasionally they are negative due to eradication of the infectious agent by a prior course of antibiotics. Blood cultures should be obtained in any patient that appears toxic. Cultures of other sites that appear to be the primary site of the infection (eg, pharynx) should also be obtained, although results from pharyngeal cultures may not correlate with organisms isolated from a nodal abscess.1
In contrast, laboratory evaluation plays a crucial role in determining the etiology of subacute, chronic, and generalized lymphadenopathy. Serologic tests for Bartonella henselae, syphilis (VDRL), toxoplasmosis, cytomegalovirus (CMV), Epstein-Barr virus (EBV), tularemia, brucellosis, histoplasmosis, and coccidiomycosis may suggest an infectious agent. A strongly positive intradermal tuberculin skin test is consistent with an infection due to Mycobacterium tuberculosis, whereas a lesser reaction to tuberculin skin testing is more consistent with a nontuberculous mycobacterial infection. Finally, serologic testing for human immunodeficiency virus (HIV) should be considered in any patient with at-risk behaviors, generalized lymphadenitis, and unusual or recurrent infections caused by opportunistic organisms. Figure 2 presents a suggested algorithm for the diagnostic evaluation of a child with cervical lymphadenitis.2
Figure 2.
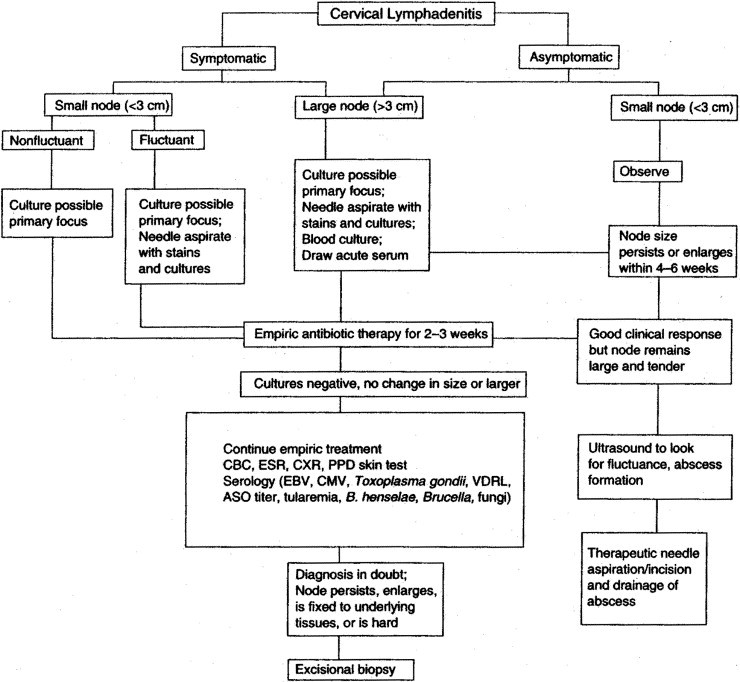
Evaluation and treatment algorithm for cervical lymphadenitis. (Reprinted with permission.2) (ASO, antistreptolysin titer; CXR, chest radiograph; CBC, complete blood count; CMV, cytomegalovirus; EBV, Epstein–Barr virus; ESR, erythrocyte sedimentation rate; HIV, human immunodeficiency virus; PPD, purified protein derivative; VDRL, Venereal Disease Research Laboratories.)
Diagnostic imaging
Plain radiographs are seldom necessary in patients with acute cervical lymphadenitis, but may occasionally document the primary site of an infection (eg, pneumonia, sinusitis, or dental caries). Plain radiographs are more valuable in the child with chronic or generalized adenopathy. Plain radiographs of the chest may suggest involvement of mediastinal lymph nodes or the lungs and are indicated in all patients with respiratory symptoms. Chest radiographs with two views should also be obtained in any patient with either symptomatic or asymptomatic cervical adenopathy. This is done to rule out critical airway compression if a biopsy under general anesthesia is planned. Other findings on plain radiographs may include bony lesions consistent with osteomyelitis or tumor involvement, evidence of hepatic and/or splenic enlargement, and/or calcifications involving the liver or spleen, suggesting a chronic granulomatous infection. In routine practice, however, plain radiographs of anatomic regions other than the chest are seldom required.
Ultrasonography (US) is the most frequently obtained and the most useful diagnostic imaging study. High-resolution US is used to assess nodal morphology, longitudinal and transverse diameter, and internal architecture. Doppler US is used to assess the presence of perfusion and its distribution, as well as to obtain measures of vascular resistance. Advantages of US are that it is noninvasive and avoids ionizing radiation and can be performed without sedation in almost every patient. Additionally, serial US can be performed to follow nodal diameters and architecture over time. One potential drawback of US, however, is its lack of absolute specificity and sensitivity in ruling out neoplastic processes as the cause of nodal enlargement. Thus, findings that are interpreted as being consistent with an infectious etiology might result in a false sense of security and delay diagnostic biopsy.
US in the acute setting is primarily of value in assessing whether a cervical swelling is nodal in origin or is attributable to an infected cyst or other soft tissue mass. Also, it may detect an abscess not already apparent on physical examination and that requires drainage.
In patients with subacute or chronic adenopathy, US is often used in an attempt to determine whether nodal enlargement is neoplastic or infectious in origin. Findings on gray-scale US shown to be consistent with reactive lymphadenopathy include a long- to short-axis ratio of greater than 2.0 (ie, oval shape), central irregular hyperechogenicity, blurred margins, and central necrosis.3 Findings on color Doppler examination reported to be consistent with a reactive lymphadenopathy include hilar vascularity4 and a low pulsatility index.5 However, neither of these features, alone or in combination, have been shown to consistently distinguish between benign and malignant etiologies.6, 7 Thus, although suspicious US findings may be useful in indicating the need for biopsy, US should not be considered as a definitive means to rule out neoplasia in patients with persistent lymphadenopathy.
Cross-sectional diagnostic imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) are of little value in managing most patients with cervical lymphadenitis, but may provide a useful roadmap in patients undergoing nodal excision with suspected atypical mycobacterial lymphadenitis. These studies certainly are indicated in patients with a biopsy-verified diagnosis of neoplasia.
Treatment
Treatment varies depending on the cause and presentation of cervical lymphadenitis. As such, treatment options will be considered within the framework of specific etiologic agents.
Acute viral lymphadenitis
Most cases of cervical adenitis in children are associated with viral infections.8 Acute viral associated cervical lymphadenitis typically develops following an upper respiratory tract infection. Involved nodes are usually bilateral, multiple, and relatively small, without warmth or erythema of the overlying skin. Virally induced adenopathy rarely suppurates and generally resolves spontaneously over a short period of time.
Many cases of cervical adenopathy associated with viral illnesses are due to reactive hyperplasia. Causes of the associated upper respiratory tract infection include rhinovirus, parainfluenza virus, influenza virus, respiratory syncytial virus, coronavirus, adenovirus, and reovirus.9 Other common viral etiologies include CMV and EBV. Less frequent etiologies include mumps, measles, rubella, varicella, herpes simplex, human herpesvirus 6 (roseola), and coxsackie viruses.10
Acute viral lymphadenitis is variably associated with fever, conjunctivitis, pharyngitis, and other upper respiratory tract symptoms. Rashes and hepatosplenomegaly may also be present, particularly when CMV is the causative organism. In some cases (eg, rubella), lymphadenopathy precedes the onset of a diagnostic rash. Both anterior and posterior cervical lymph nodes are frequently involved when associated with pharyngitis or tonsillitis, whereas preauricular adenitis occurs in 90% of patients with adenoviral-associated keratoconjunctivitis.11
Bilateral, acute cervical lymphadenitis associated with a viral upper respiratory tract infection rarely requires additional diagnostic testing or specific therapy. Adenopathy typically resolves spontaneously as the viral illness wanes. Treatment is directed at relieving symptoms associated with the viral illness. Specific antiviral therapy is seldom indicated except in the rare patient with severe respiratory tract or hepatic involvement, or in the immunocompromised patient.
Acute bacterial lymphadenitis
Large (>2-3 cm) solitary, tender, unilateral cervical lymph nodes that rapidly enlarge in the preschool age child are commonly due to bacterial infection. The most commonly involved lymph nodes in decreasing order of frequency are the submandibular, upper cervical, submental, occipital, and lower cervical nodes.10 Forty percent to 80% of cases of acute unilateral cervical lymphadenitis in the 1- to 4-year-old child are due to Staphylococcus aureus or Streptococcus pyogenes. 10 Group B streptococcal adenitis may present in the infant with unilateral facial or submandibular swelling, erythema, and tenderness, associated with fever, poor feeding, and irritability. Anaerobic bacteria occur in the older child with dental caries or periodontal disease. Isolated anaerobes include Bacteroides sp, Peptococcus sp, Peptostreptococcus sp, Propionibacterium acnes, and Fusobacterium nucleatum.12 Less frequent etiologies of acute bacterial lymphadenitis include Francisella tularensis, Pasteurella multocida, Yersinia pestis, and Haemophilus influenza type b, whereas other organisms, such as Gram-negative bacilli, Streptococcus pneumoniae, group C streptococci, Yersinia enterocolitica, Staphylococcus epidermidis, and α-hemolytic streptococci, are rarely encountered.11
Patients typically present with a history of fever, sore throat, earache, or cough, and physical findings include pharyngitis, tonsillitis, acute otitis media, or impetigo. Lymphadenitis due to S. pyogenes should be suspected if the patient presents with the typical vesicular, pustular, or crusted lesions of impetigo involving the face or scalp. As noted previously, cervical lymphadenitis due to anaerobic infections frequently is associated with dental caries or periodontal disease. Acute cervical adenitis due to Pasteurella multocida can occur following animal bites or scratches on the head, neck, or upper chest, whereas acute cervical lymphadenitis due to Yersinia pestis is associated with flea bites on the head and neck and is most commonly seen in the western United States.
Initial antibiotic therapy is directed at the most likely organisms. Because staphylococci and streptococci are the most common pathogens, initial therapy usually includes a β-lactamase resistant antibiotic; this agent is used because of the high incidence of penicillin resistance in isolated staphylococci. Very young patients or patients with severe symptoms (eg, cellulitis, high fever, or respiratory distress) may require hospitalization for initiation of parenteral antibiotic therapy and close observation. For older patients with dental or periodontal disease, the antibiotic regimen should include coverage for anaerobic oral flora (ie, penicillin V or clindamycin). Therapy is usually administered for 10 days and continued for at least 5 days beyond resolution of acute signs and symptoms. If a primary site is identified, cultures should be obtained and treatment is directed at that site as well. In most cases, symptomatic improvement should be noted after 2 to 3 days of therapy, although complete resolution of nodal enlargement may require several weeks.
Failure to improve, or worsening of the patient’s clinical condition, should prompt further diagnostic evaluation, including aspiration and culture, and consideration of an alternate antibiotic regimen. An etiologic agent can be recovered by needle aspiration of an affected node in 60% to 88% of cases.2 The largest node with the most direct access is typically the best target for aspiration. The node should be entered through an area of healthy skin. Aspirated material should be examined by Gram stain and acid-fast stain and cultured for aerobic, anaerobic bacteria, and mycobacteria. If no purulent material is aspirated, a small amount of nonbacteriostatic saline can be injected into the node and then aspirated to obtain material for culture.
Fluctuance develops in 25% of patients with acute bacterial adenitis. In many cases, it can be managed effectively with antibiotics and one or more needle aspirations under local anesthesia, with or without sedation. This approach is particularly attractive when treating fluctuant nodes in cosmetically important areas. However, adequate drainage by aspiration may be difficult, if not impossible, in the uncooperative child or when the abscess cavity is loculated. These patients often require operative drainage under general anesthesia. At the time of operative drainage, an attempt should be made to open and drain all loculations. Specimens should be sent for Gram stain and aerobic and anaerobic cultures and for acid-fast stains and mycobacterial culture. Material for KOH prep and fungal cultures should be sent if the patient is immunocompromised, and tissue should be sent for histologic examination if there is suspicion of neoplasia. Once drained, the abscess cavity is usually packed with a gauze strip to obtain hemostasis and to prevent early skin closure. The gauze packing can usually be removed over a period of several days on an outpatient basis.
Reports from multiple centers have documented an increasing frequency of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) skin and soft tissue infections, including lymphadenitis.13, 14, 15, 16 At present, the majority of isolates of Staphylococcus aureus associated with cervical lymphadenitis in most centers are methicillin-sensitive. However, given the documented increasing nasopharyngeal colonization by methicillin-resistant strains of Staphylococcus aureus in healthy children,17, 18 it is possible that the CA-MRSA will become the prevalent organism responsible for cervical lymphadenitis in the pediatric age group in the future. Certainly, failure to respond to appropriate first-line antibiotic therapy should prompt consideration of expanding coverage to include methicillin-resistant strains of Staphylococcus aureus.
Subacute and chronic lymphadenitis
Failure to resolve or improve despite a 2- to 4-week period of appropriate therapy, or the presence of generalized lymphadenopathy should prompt further diagnostic testing. A variety of organisms can result in generalized or persistent lymphadenopathy. A number of the more commonly encountered etiologies are described in the following sections.
Mycobacterial lymphadenitis
Chronic cervical lymphadenitis may be caused by Mycobacterium tuberculosis (“scrofula”) or by nontuberculous strains of mycobacteria. In the United States, 70% to 95% of cases of mycobacterial lymphadenitis are due to nontuberculous strains. The most commonly encountered strains of nontuberculous mycobacteria include Mycobacterium avium-intracellulare and Mycobacterium scrofulaceum. Less commonly encountered strains include M. kansasii, M. fortuitum, and M. hemophilum. Nontuberculous lymphadenitis is most commonly seen in Caucasians, whereas tuberculous lymphadenitis is more commonly encountered in Asians, Hispanics, and African-Americans. It also occurs in immigrants from endemic areas and likely represents reactivation of prior disease.
In general, the clinical presentation of tuberculous and nontuberculous lymphadenitis is similar. Patients usually present with rapid onset of nodal enlargement, followed by a gradual increase in nodal size over 2 to 3 weeks. Most nodes remain less than 3 cm in diameter. Constitutional signs are unusual. The skin overlying the node typically develops a pink to lilac-red hue and becomes thin and parchment-like. Approximately 50% of patients with nontuberculous lymphadenitis develop fluctuance and spontaneous drainage with sinus tract formation occurs in 10%.11 Epidemiologic and clinical features do not allow differentiation of tuberculous from nontuberculous lymphadenitis; however, fulfillment of two of three criteria has been shown to be associated with 92% sensitivity for the diagnosis of tuberculous lymphadenitis.19 These criteria include: (1) a positive tuberculin skin test reaction, (2) an abnormal chest radiograph, and (3) contact with a person with infectious tuberculosis. PPD skin tests may be positive in patients with nontuberculous infections, but are generally less reactive (<15 mm induration) as compared with the strongly positive reaction associated with M. tuberculosis infections.
The treatment of choice for lymphadenitis caused by M. tuberculosis is multi-agent antituberculous antibiotic therapy for 12 to 18 months. Nodal regression typically occurs within 3 months. Because of the effectiveness of antituberculous agents, the surgical excision of draining nodes and sinuses is infrequently required.
In contrast, most strains of nontuberculous mycobacteria respond poorly to antituberculous drugs, and the treatment of choice is surgical excision. In general, all clinically involved nodes, associated sinus tracts, and grossly involved overlying skin should be excised en masse. Care should be taken to avoid injury to adjacent structures. In patients in whom complete excision would result in unacceptable cosmetic outcomes or injury to adjacent nerves, thorough curettage may be effective. The role of multi-agent antituberculous drug therapy in patients with nontuberculous lymphadenitis is unclear. However, if chemotherapy is planned, appropriate samples should be sent to a qualified laboratory for drug susceptibility testing.
Cat scratch disease
Cat scratch disease is a lymphocutaneous syndrome characterized by regional lymphadenitis associated with a characteristic skin lesion at the site of inoculation. Cat scratch disease follows inoculation of Bartonella henselae through broken skin or mucous membranes. A skin papule typically develops at the site of inoculation, followed by regional adenopathy 5 days to 2 months later. Unfortunately, often the primary site of involvement has resolved by the time adenopathy is noted. The most common sites of lymphadenopathy are the axilla (52%) and the neck (28%). Patients typically present with a single large (>4 cm) tender node. Constitutional symptoms are usually mild and include low-grade fever, body aches, malaise, or anorexia. Suppuration occurs in 30% to 50% of cases. In most patients, the diagnosis can be confirmed by serologic testing.
Cat scratch disease is usually self-limited. In most cases, nodal enlargement resolves spontaneously after 1 to 3 months. As such, the benefit of antibiotic therapy is controversial. Azithromycin has, nevertheless, been shown to be associated with more rapid resolution of nodal enlargement.20 Aspiration of suppurative nodes may provide symptomatic relief. Rarely, systemic involvement develops and may include encephalitis, granulomatous hepatitis, hepatosplenic infection, endocarditis, and osteomyelitis. Effective antibiotic options for patients with systemic involvement may include rifampin, ciprofloxacin, gentamicin, trimethoprim and sulfamethoxazole, clarithromycin, or azithromycin.
Fungal, parasitic, and opportunistic infections
Infections caused by Nocardia sp. are infrequent in children and usually present as lung disease in immunocompromised hosts. These organisms are found in the soil or decaying vegetable matter, and infection in humans occurs via inhalation or direct skin inoculation. Skin inoculation usually results in an associated skin pustule, and the diagnosis can sometimes be established by culture of the pustule or an involved lymph node. Sulfonamides are the treatment of choice.
Actinomyces species are part of the normal oral flora in human beings. Local invasion results in cervicofacial actinomycosis, presenting as brawny induration with secondary nodal involvement. Diagnosis is usually made by biopsy. The organism may be difficult to isolate, though histologic examination may reveal “sulfur granules.” Treatment usually requires initial parenteral antibiotic therapy followed by a prolonged course of oral antibiotics for 3 to 12 months. Penicillin is the antibiotic of choice.
Approximately 10% of patients with acquired infections due to the intracellular protozoan Toxoplasma gondii (toxoplasmosis) present with cervical, suboccipital, supraclavicular, axillary, or inguinal adenopathy. Infections associated with cervical adenopathy are usually acquired via the oral route by consumption of meat- or milk-containing cysts or oocytes. Involved nodes are usually discrete and may be tender, but do not suppurate. The diagnosis can be made by isolation of the organism or by serologic testing. Patients with lymphadenopathy alone do not require antimicrobial therapy, but patients with severe or persistent symptoms are treated with a combination of pyrimethamine, sulfadiazine, and leucovorin for at least 4 to 6 weeks.
Histoplasmosis, blastomycosis, and coccidiomycosis are fungal infections caused by Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis, respectively. These organisms are soil saprophytes that have the ability to exist in a yeast form in human tissues. The diseases are endemic to certain geographic regions of the United States. Most patients present with pulmonary infections, and lymphadenopathy is usually secondary to the primary pulmonary involvement. The diagnosis can be established by serologic or skin testing. Most infections resolve spontaneously and do not require treatment. Patients with severe respiratory or systemic symptoms may, however, require prolonged courses of antifungal therapy.
HIV is a retrovirus that is transmitted by sexual contact, parenteral exposure to blood, or vertical transmission from mother to child. Initial symptoms may be subtle and may include lymphadenopathy, hepatosplenomegaly, failure to thrive, and chronic or recurrent diarrhea. The diagnosis is established by serologic testing.
Noninfectious etiologies
In some cases, cervical lymph node involvement is a manifestation of a systemic disease with an inflammatory component. The following is a brief description of several of these conditions, but is not inclusive:
Kikuchi–Fujimoto disease
Kikuchi-Fujimoto disease (histiocytic necrotizing lymphadenitis) is a rare entity of unknown etiology. It typically presents in older children with bilateral, enlarged, firm, painful, cervical lymph nodes (usually in the posterior cervical triangle). Associated findings include skin lesions, fever, nausea, weight loss, night sweats, and splenomegaly. Laboratory evaluation often reveals leukopenia with atypical lymphocytosis and an elevated erythrocyte sedimentation rate. Perinodal inflammation is common. Nodal histology is characteristic and most cases resolve spontaneously.
Kawasaki disease
Kawasaki disease is an acute febrile vasculitis of childhood of unknown etiology. Lymphadenitis is often one of the earliest manifestations of the disease. Involved nodes are usually unilateral, confined to the anterior triangle, greater than 1.5 cm in diameter, and only moderately tender and nonfluctuant. The diagnosis is made clinically based on the presence of a fever for at least 5 days, accompanying several other characteristic clinical features of the disease. Resolution of the cervical lymphadenopathy usually occurs early in the course of the disease.
Periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome (PFAPA syndrome)
PFAPA syndrome usually affects children younger than 5 years of age and is of unknown etiology. It is characterized by cyclic recurrences of the above symptom complex every 2 to 9 weeks, with spontaneous resolution after 4 to 5 days. Recurrences gradually abate with time; however, systemic corticosteroids may help relieve severe symptoms.
Rosai–Dorfman disease
Rosai–Dorfman disease (sinus histiocytosis with massive lymphadenopathy) is a rare disorder that typically manifests in the first decade of life, predominantly in African-Americans. Cervical lymph nodes are commonly the initial site of involvement and are usually mobile, discrete and asymmetric. Progression leads to massive bilateral cervical nodal enlargement and involvement of other nodal groups or extranodal sites. Laboratory evaluation reveals leukocytosis, neutrophilia, an elevated erythrocyte sedimentation rate, and hypergammaglobulinemia. Histopathologic analysis shows florid hyperplasia, marked histiocytosis and plasmacytosis. Resolution usually occurs after 6 to 9 months. Extensive or progressive disease may, however, require treatment with combination chemotherapy.21
Sarcoidosis
Sarcoidosis is a chronic granulomatous disease of unknown etiology. The disease may affect almost any organ in the body, but the lung is most frequently affected. The most common physical finding in children with this disease is peripheral lymphadenopathy. Involved cervical nodes are usually bilateral, discrete, firm, and rubbery. Supraclavicular nodes become involved in more than 80% of patients. Biopsy with histologic examination is the most valuable diagnostic test. Treatment is supportive. Corticosteroid therapy may suppress acute manifestations.
Conclusion
Cervical lymphadenopathy in the pediatric age group is largely inflammatory and infectious in etiology, although in some patients it may be related to neoplastic disease. It is important for the surgeon to be aware of the clinical manifestations and specific etiologies of this condition, as well as the diagnostic approaches and therapeutic options currently available. Close follow-up is required to monitor the need for either additional diagnostic tests or biopsy should a patient fail to respond to appropriate initial therapy.
References
- 1.Cengiz A.B., Kara A., Kanra G. Acute neck infections in children. Turk J Pediatr. 2004;46:153–158. [PubMed] [Google Scholar]
- 2.Darville T., Jacobs R.F. Lymphadenopathy, lymphadenitis and lymphangitis. In: Jenson H.B., Baltimore R.S., editors. Pediatric Infectious Diseases: Principles and Practice, 2nd edition, chap 51. Saunders; Philadelphia, PA: 2002. pp. 610–629. [Google Scholar]
- 3.Papakonstantinou O., Bakantaki A., Paspalaki P. High-resolution and color Doppler ultrasonography of cervical lymphadenopathy in children. Acta Radiol. 2001;42:470–476. doi: 10.1080/028418501127347197. [DOI] [PubMed] [Google Scholar]
- 4.Ahuja A., Ying M. An overview of neck sonography. Invest Radiol. 2002;37:333–342. doi: 10.1097/00004424-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Ying M., Ahuja A., Brook F. Accuracy of sonographic vascular features in differentiating different causes of cervical lymphadenopathy. Ultrasound Med Biol. 2004;30:441–447. doi: 10.1016/j.ultrasmedbio.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Ahuja A., Ying M., King A. Lymph node hilus: Gray scale and power Doppler sonography of cervical nodes. J Ultrasound Med. 2001;20:987–992. doi: 10.7863/jum.2001.20.9.987. [DOI] [PubMed] [Google Scholar]
- 7.Asai S., Miyachi H., Oshima S. A scoring system for ultrasonographic differentiation between cervical malignant lymphoma and benign lymphadenitis. Rinsho Biyori. 2001;49:613–619. [PubMed] [Google Scholar]
- 8.Peters T., Edwards K. Cervical lymphadenopathy and adenitis. Pediatr Rev. 2000;21:399–404. [PubMed] [Google Scholar]
- 9.Leung A., Robson W. Childhood cervical lymphadenopathy. J Pediatr Health Care. 2004;18:3–7. doi: 10.1016/j.pedhc.2003.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly C., Kelly R. Lymphadenopathy in children. Pediatr Clin North Am. 1998;45:875–888. doi: 10.1016/s0031-3955(05)70051-1. [DOI] [PubMed] [Google Scholar]
- 11.Chesney P. Cervical lymphadenitis and neck infections. In: Long S., Pickering L., Prober C., editors. Principles and Practice of Pediatric Infectious Diseases, 2nd edition, chap 23. Churchill Livingstone; Philadelphia, PA: 2003. pp. 165–176. [Google Scholar]
- 12.Bodenstein L., Altman R. Cervical lymphadenitis in infants and children. Sem Pediatr Surg. 1994;3:134–141. [PubMed] [Google Scholar]
- 13.Purcell K., Fergie J. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections: a 14-year study at Driscoll Children’s Hospital. Arch Pediatr Adolesc Med. 2005;159:980–985. doi: 10.1001/archpedi.159.10.980. [DOI] [PubMed] [Google Scholar]
- 14.Mongkolrattanothai K., Daum R. Impact of community-associated, methicillin-resistant Staphyloccous aureus on management of skin and soft tissue infections in children. Curr Infect Dis Rep. 2005;7:381–389. doi: 10.1007/s11908-005-0013-1. [DOI] [PubMed] [Google Scholar]
- 15.Ochoa T., Mohr J., Wanger A. Community-associated methicillin-resistant Staphylococcus aureus in pediatric patients. Emerg Inf Dis. 2005;11:966–968. doi: 10.3201/eid1106.050142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez-Aguilar G., Hammerman W.A., Mason E.O., Jr Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus in children. Pediatric Infect Dis J. 2003;22:593–598. doi: 10.1097/01.inf.0000073163.37519.ee. [DOI] [PubMed] [Google Scholar]
- 17.Anwar M., Jaffery G., Rehman B. Staphylococcus aureus and MRSA nasal carriage in general population. J Coll Physicians Surg Pak. 2004;14:661–664. [PubMed] [Google Scholar]
- 18.Creech C., Kernodle D., Alsentzer A. Increasing rates of nasal carriage of methicillin-resistant Staphylococcus aureus in healthy children. Pediatr Infect Dis J. 2005;24:617–621. doi: 10.1097/01.inf.0000168746.62226.a4. [DOI] [PubMed] [Google Scholar]
- 19.Spyridis P., Maltezou H., Hantzakos A. Mycobacterial cervical lymadenitis in children: Clinical and laboratory factors of importance for differential diagnosis. Scand J Infect Dis. 2001;33:362–366. doi: 10.1080/003655401750174002. [DOI] [PubMed] [Google Scholar]
- 20.Bass J., Freitas B., Freitas A. Prospective randomized double blind placebo-controlled evaluation of azithromycin for treatment of cat-scratch disease. Pediatr Infect Dis J. 1998;17:1059–1061. doi: 10.1097/00006454-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Jabali Y., Smrcka V., Pradna J. Rosai-Dorfman disease: successful long-term results by combination chemotherapy with prednisone, 6-mercaptopurine, methotrexate and visblastine: a case report. Int J Surg Pathol. 2005;13:285–289. doi: 10.1177/106689690501300311. [DOI] [PubMed] [Google Scholar]


