Feline coronavirus (FCoV) is a highly contagious virus that is ubiquitous in multicat environments. This virus commonly causes an asymptomatic infection, which can persist in certain individuals. Sporadically and unpredictably, FCoV infection leads to feline infectious peritonitis (FIP), a highly fatal systemic immune-mediated disease. The pathogenesis of FIP is not fully understood. Despite the low incidence of FIP among FCoV-infected cats, FIP is a major cause of mortality.1, 2 Since it can take weeks to months for FIP to develop after the initial infection with FCoV, the disease may only become apparent after a cat has been adopted or sold, resulting in devastating consequences for clients and adoption or breeding facilities. Currently, the development of FIP in a FCoV-infected cat is unpredictable, and once FIP develops, diagnosis confirmation is difficult. Historically, therapy has been limited to palliative treatment, although recent therapeutic protocols have improved survival time. This review provides interdisciplinary information about the virus, the pathophysiology of the disease, the available diagnostic methods, as well as the management and control of the virus and the disease in shelters and other multicat environments.
Etiology of Feline Coronaviruses
FCoVs belong to a family of considerable importance in veterinary medicine. Viruses within the Coronaviridae family infect and often cause enteric and respiratory disease, especially in young animals.3, 4, 5, 6, 7, 8, 9 In general, these viruses tend to be transmitted between and infectious for only closely related hosts.10 However, with the discovery of the severe acute respiratory syndrome coronavirus (SARSCoV) that commonly infects bats and apparently “jumped” from civets and raccoon dogs to humans, the broader range of transmission and zoonotic potential of animal coronaviruses is a reality.11
Group 1 Coronaviruses
The coronaviruses can be classified into at least 4, if not 5, groups.11, 12 The mammalian viruses are represented in 3 or 4 of these groups with the feline viruses residing in group 1, along with the porcine, canine, rabbit, and ferret coronaviruses, and a human coronavirus, that is distinct from the virus associated with severe acute respiratory syndrome (SARS).13, 14, 15 Within group 1 viruses, the feline, porcine, and canine members are closely related.14, 16, 17, 18 There are 2 distinct serotypes of FCoVs that are genetically related and, by definition, can be distinguished on the basis of specific antibodies.19, 20, 21, 22, 23, 24 Whereas serotype I FCoV shares genetics with the porcine virus, transmissible gastroenteritis virus (TGEV), type II FCoV shares homology with the canine coronavirus. The TGEV genomic sequences identified in the FCoV I and canine coronavirus sequences identified in FCoV II indicated these viruses likely originated in part by recombination events resulting in this exchange of genome regions.19, 25, 26, 27 Recombination is a common event for coronaviruses.19, 28, 29, 30, 31, 32, 33 The FCoV I isolates have repeatedly been shown to more commonly infect cats worldwide than FCoV serotype II viruses.34, 35, 36, 37, 38 However, the FCoV type II viruses are most commonly studied because of a greater propensity to replicate in vitro in cell culture. Unlike the type I FCoV, but similar to most of the group 1 coronaviruses, the FCoV type II viruses use their species-specific aminopeptidase N as the cell receptor for entry.39, 40, 41, 42
Of considerable clinical interest is the manifestation of 2 FCoV biotypes, which are associated with distinct diseases or pathologies.22, 38, 43 The feline enteric coronavirus (FECV) biotype is ubiquitous, commonly infecting the gut of cats and generally in the absence of disease, while the feline infectious peritonitis virus (FIPV) biotype is responsible for fatal, systemic disease. Because FECV and FIPV from the same cattery are nearly identical, both antigenically and genetically, while geographically separated isolates display greater sequence differences, it has been generally accepted that the FIPV arises from the FECV strains, within the same animal.38, 44, 45, 46, 47 It is important to understand how the 2 biotypes relate to FCoV serotypes. Both FIPV and FECV are represented within both FCoV serotypes I and II.37 Thus, the terms biotype and serotype are distinct and should not be confused.
Feline Coronavirus Genetics and Biotype Considerations
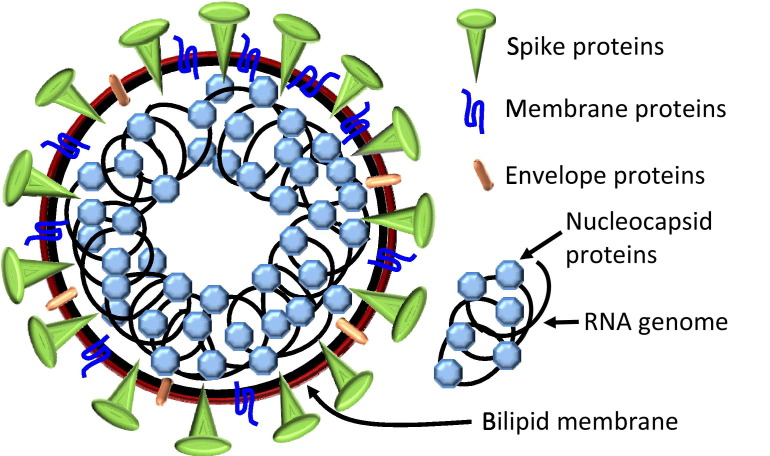
The infectious vehicle for transmission from cat to cat or from cell to cell is the coronavirus virion or viral particle (Fig. 1). The single-stranded RNA genome, lying within the core of the virion, is coated with nucleocapsid proteins.13, 24 A bilipid membrane, or envelope, originating from the host cell surrounds the nucleocapsid coated genome. Embedded within this membrane envelope are 3 major proteins that complete the repertoire of the virion particle. The membrane proteins are the glycosylated, envelope spike protein (S); the glycosylated, highly hydrophobic membrane protein (M); and a smaller hydrophobic envelope protein (E). The S protein can be cleaved into 2 parts resulting in the transmembrane S2, which anchors the protein in the cell derived envelope, and the more exterior S1. It is the S1 protein that houses the major determinants for virus attachment and thus antibody neutralization and serotype determination.48, 49
Fig. 1.
Schematic of the FCoV virion (viral particle). Nucleocapsid proteins coat the RNA genome. The spike, membrane, and envelope proteins are anchored in the bilipid membrane of cell origin.
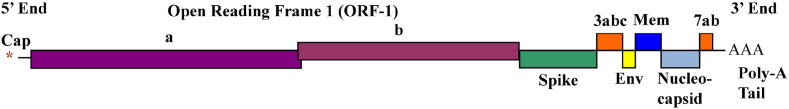
The order of the genes encoded on the FCoV genome is similar to that of other coronaviruses. The information encoding the polymerase activity required for making messenger RNA and genomic RNA is located in the 5′ two-thirds of the genome (Fig. 2). 24, 50, 51 The information encoded in the remaining third of the genome at the 3′ end encodes those proteins that make up the viral particle (see Fig. 1). These 3′ genes lie in an order of S, E, M, and N. Additional group I coronavirus ORFs encoding proteins of unknown function lie between the S and E genes (3a, 3b and 3c), and downstream of the N gene (7a, 7b).
Fig. 2.
Schematic of the gene organization on the FCoV genome. A cap structure at the 5′ end and the 3′ end poly-adenylated tail are typical structures on an RNA used as message for generating protein within a cell. The entire genome is approximately 29,000 nucleotide bases in length. The overlapping ORFs 1a and 1b encode proteins involved in RNA synthesis required for generating mRNA, the genome, and their negative sense templates. The spike refers to the gene encoding the highly glycosylated spike protein (S), Mem refers to the gene encoding the membrane protein (M), env refers to the gene encoding the envelope protein (E), and nucleocapsid refers to the gene encoding the nucleocapsid protein (N).
The potential for mutations in the RNA genome of coronaviruses provides the background for variations that may result in changes in the nature of the viral antigens or disease resulting from viral infection. Whereas antigenic changes are responsible for vaccine failures in the case of the avian coronaviruses, mutations in the FCoV may also be responsible for the metamorphosis of the fairly benign enteric virus to a highly pathogenic relative, responsible for FIP.28, 30, 44, 46, 52, 53, 54 The defining question is what mutations in the enteric virus lead to a pathogenic, fatal viral progeny. The large size of the coronavirus RNA genome presents difficulties in identifying single mutations that might be instrumental in defining virulence.51, 55 Although differences can also be identified within the extremely large ORF1 (at the beginning of the genome), the size of this region has been an obstacle to pinpointing mutations potentially involved in biotype determination. Thus, gene comparisons have concentrated on selected genes lying in the 3′ third of the genome.44, 46, 52, 53, 54
An intact 3c region between the S and M genes has been associated with FECV replicating in the gut while mutations that prevent expression of the protein have been identified in FIPV strains.44 The ORF 7b gene was also reported to be truncated in FECV but intact in FIPV strains.56, 57 However, such deletions may not be relevant to biotype since they also can occur with in vitro passage53 and Lin and colleagues58 found that small deletions in ORF7b could be found in both biotypes.
Epidemiology
FCoV Prevalence and Risk Factors
FCoV is distributed worldwide and is ubiquitous in virtually all cat populations. There is great variability in prevalence among different cat populations (Table 1). 59 The virus is transmitted via the fecal-oral route; therefore, the prevalence of FCoV infection is generally associated with the number and density of cats housed together. A serologic survey from Davis, California reported a seroprevalence of 20% in pet cats living in private households and 87% for purebred cats living in catteries.60 Among 2,214 relinquished cats at 14 British shelters, the risk of being seropositive was 2.3-fold higher for cats originating from multicat households than for cats from single-cat households.61 In other populations, more than 90% of the cats were seropositive, and certain cats could remain seropositive for 10 years or longer.62 The length of time in multicat environments also increases the risk of exposure, which was estimated to be 5 times higher for cats living in shelters for longer than 60 days.61 Although these environments are not the primary source of FCoV for many relinquished cats, factors intrinsic to the shelter environment amplify shedding and increase spread to susceptible individuals. One study demonstrated that FCoV-infected cats entering a shelter increased FECV shedding from 10- to 1 million-fold in 1 week.63 Housing and husbandry practices that reduce exposure to feces and contaminated environments have a tremendous influence on the number of cats exposed to the virus.62 As shown in Table 1, stray or feral cats generally have a lower prevalence of infection than pet cats, likely due to lower population densities and because burying feces outdoors results in less exposure to contaminated fecal material compared to pet cats.64
Table 1.
Frequency of cats exposed to or infected with FCoV in selected populations
| Sample Tested | Country | Population Type | Prevalence | No. Positive/Total | Diagnostic Method | Breed | Ref. |
|---|---|---|---|---|---|---|---|
| Serum | Australia | Multicat environment | 44% | 59/135 | ELISA | Many | 185 |
| Australia | Single cat household | 24% | 33/140 | ELISA | Many | 185 | |
| Australia | Stray | 0% | 0/49 | ELISA | Not disclosed | 185 | |
| Germany | Multicat environment | 69% | 29/42 | IFA | Mixed-breed | 68 | |
| Italy | Multicat environment | 82% | 98/120 | ELISA | Not disclosed | 155 | |
| Sweden | <5 cats in the environment | 29% | a/129 | IFA | Many | 186 | |
| Sweden | ≥5 cats in the environment | 71% | a/24 | IFA | Many | 186 | |
| Turkey | Multicat environment | 62% | 18/29 | VN | Not disclosed | 187 | |
| Turkey | Single cat households | 4% | 3/71 | VN | Not disclosed | 187 | |
| UK | Multicat environment | 28% | 28/100 | IFA | Many | 98 | |
| UK | Single cat household | 16% | 14/88 | IFA | Many | 98 | |
| UK | Multicat environment | 26% | 432/1654 | IFA | Many | 61 | |
| UK | Multicat environment | 84% | 110/131 | IFA | Many | 188 | |
| UK | Stray | 22% | 111/506 | IFA | Many | 189 | |
| USA, Florida | Stray | 18% | 101/553 | IFA | Many | 64 | |
| USA, California | Single cat households | 21% | 7/33 | IFA | Not disclosed | 60 | |
| USA, California | Multicat environment | 87% | 94/108 | IFA | Not disclosed | 60 | |
| Feces | Germany | Multicat environment | 38% | 16/42 | Nested RT-PCR | Mixed-breed | 68 |
| Malaysia | Multicat environment | 96% | 23/24 | RT-PCR | Persian | 190 | |
| Malaysia | Multicat environment | 70% | 14/20 | RT-PCR | Mixed-breed | 190 | |
| Sweden | Multicat environment | 80% | 12/15 | Nested PCR | Persian | 191 | |
| Sweden | Single cat household | 25% | 24/98 | Nested PCR | Many | 191 | |
| Blood | Netherlands | Multicat environment | 5% | 23/424 | mRNA RT-PCR | Many | 170 |
| Malaysia | Multicat environment | 15% | 6/40 | mRNA RT-PCR | Many | 169 | |
| Turkey | Stray | 45% | 10/22 | mRNA RT-PCR | Many | 168 | |
Abbreviations: ELISA, enzyme-linked immunosorbent assay; IFA, immunofluorescent antibody assay; mRNA, messenger RNA; RT-PCR, reverse transcriptase polymerase chain reaction; VN, virus neutralization assay.
Number of seropositives not provided.
FIP Incidence and Risk Factors
Despite the fact that FCoV is highly contagious and widely prevalent in multicat environments (Table 1), only 5% to 12 % of infected cats will ever develop FIP syndrome.60, 65, 66, 67, 68 However, depending on the population density, length of stay, and husbandry practices, the frequency rates in multicat environments can be as low as 0.6% to 0.8%.69, 70 The FIP incidence of 1 in every 200 new cases was determined based on 226,720 cats seen at 24 veterinary teaching hospitals in the United States over a period of 10 years (1986–1995).1 Several risk factors for the development of FIP have been identified. Sexually intact male and young cats have the highest risk of developing FIP.71 Over 40% of 1,182 cats with confirmed FIP seen in US teaching hospitals were from 6 months to 2 years of age.1 In one study in Taiwan, 88% of 51 FIP-confirmed cats were less than 2 years old.72 The risk decreases to 4% when cats reach 36 months of age.65 The disease is overrepresented in certain pure breeds, but the incidence of FIP can vary greatly between regions and countries. Abyssinian, Australian mist, Bengal, Birman, British shorthair, Burmese, Cornish rex, Himalayan, Persian, ragdoll, and rex breeds have been suggested as risk factors,71, 72, 73, 74 but FIP development is probably more related to bloodlines within a breed than to breeds themselves.59 It has been demonstrated that the development of FIP in certain lineages occurs at higher frequencies than other lineages, independently of environment, antibody titers, or viral shedding patterns.1, 75 Cats with high FCoV titers or continuous exposure to persistent shedders also have a greater risk of developing FIP.45, 59, 66
Cats with immunosuppressive conditions, such as advanced FeLV or FIV infections, are more susceptible for developing FIP when exposed to FCoV.66, 76, 77 It has been demonstrated that in FIV-infected cats the levels of FECV shedding are increased by 100-fold, with prolonged duration of fecal shedding.45 In this study, it was demonstrated that 2 cats in the FIV-infected group later developed FIP. It is theorized that the immunosuppression from the chronic FIV infection may have enhanced the evolution and selection of FIPV mutants because of the increased rate of FECV replication in the bowel and the affected individuals' decreased ability to fight off mutant viruses that may occur.45
Stress also plays a very large factor as to whether an FCoV-infected cat develops FIP.78 Stressors such as moving to a new environment, cat density, or surgery may increase the risk of an individual developing FIP. Virtually all cats in shelters and other multicat environments experience some level of stress and exposure to an array of pathogens; thus, higher incidence and outbreaks are expected in stressful environments.
Outbreaks
An outbreak is defined as a frequency of FIP-confirmed cases of greater than 10% in a multicat environment. However, rates lower than 10% may characterize an outbreak in shelters with low FIP prevalence. For example, in shelters with very low FIP frequency (<1%),69, 70 rates higher than 1% may be a cause of concern.79 Outbreaks with prevalences of 3% to 49% have been described.59, 80 Several factors have been associated with outbreaks, including (1) host-related factors: age at exposure, sex, and lineage susceptibility; (2) virus-related factors: strain virulence, high replication rate in the intestine, and a tendency to mutate to FIPV; and (3) environment-related factors: frequency of exposure to FECV, infective dose, exposure to chronic shedders, and length of exposure.79, 81
Pathology
FIP is classified as 2 forms: a noneffusive or dry and an effusive or wet form. Although the gross findings are different, the microscopic lesions are similar in both the dry and wet forms of FIP.82, 83 Furthermore, in most individual patients a mixture of both forms can be identified.
Gross Pathology
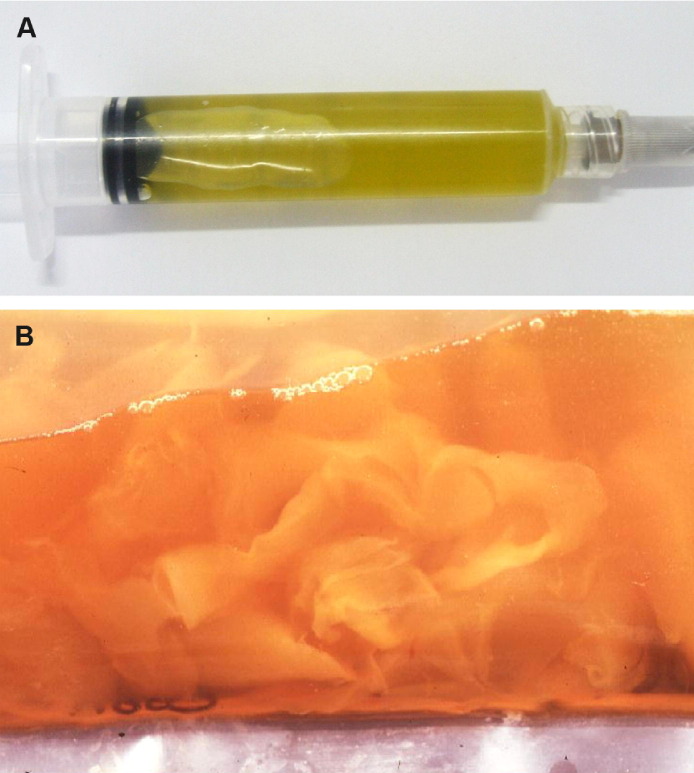
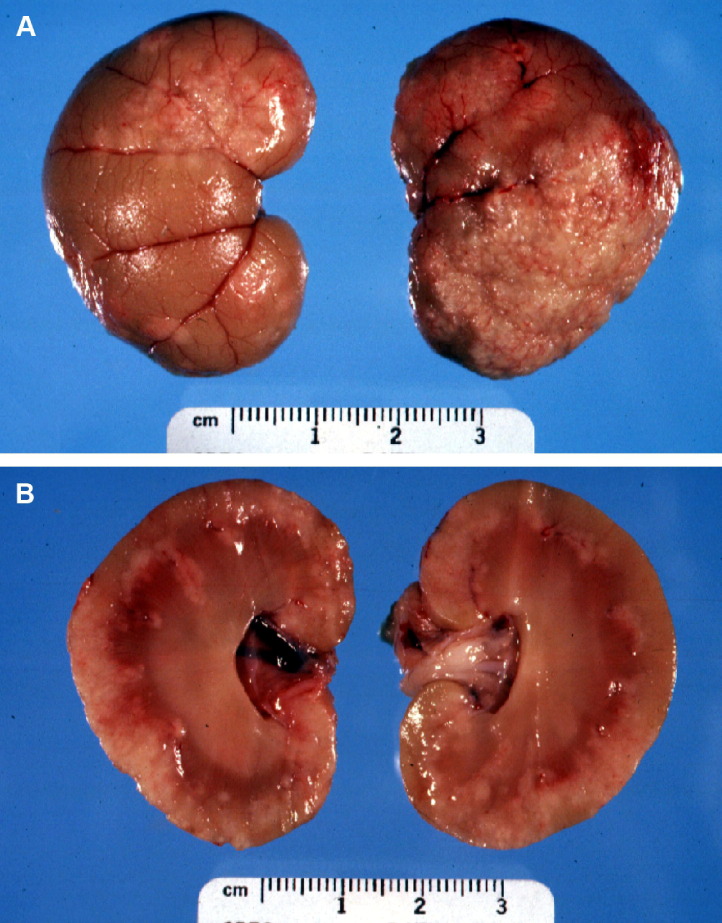
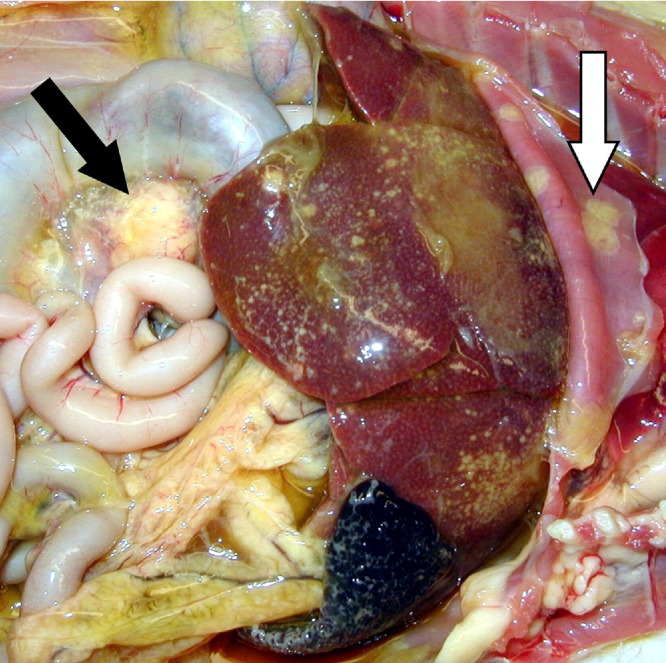
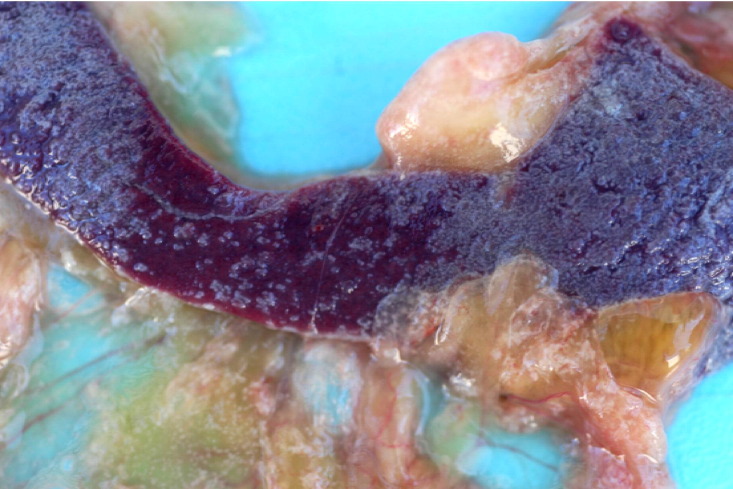
Both the wet and dry forms of FIP present with severe systemic disease and produce variable degrees of thoracic or abdominal effusions.59 The effusive or wet form produces abundant clear, proteinaceous, straw-colored peritoneal effusions (Fig. 3A). 84 Large amounts of thick exudative fluid containing copious amounts of fibrin (see Fig. 3B) severely distend the abdomen. However, this is not the only lesion, as the exudate is accompanied by a perivascular inflammatory reaction (Fig. 4). The distinctive characteristic of FIP is a whitish, slightly granular, inflammatory exudate observed in the kidneys and the omentum and covering the hepatic or splenic capsule and extending into the parenchyma (Fig. 5). The soft, thin, granular, whitish layer or thin plaques are found in the liver or on the splenic capsule (Fig. 6). Other abdominal organs, such as the intestines, lymph nodes, pancreas, or urinary bladder, may be affected to variable degrees. Inflammatory exudates can also be seen in the lungs and heart, which are frequently affected by similar, small, slightly granular nodules to plaquelike lesions with subtle vascular orientation.85
Fig. 3.
Peritoneal effusion from a cat with classic wet (or effusive) form of FIP. (A) Characteristic color of peritoneal effusion collected by abdominocentesis. (B) Close view of a plastic bag containing 350 ml of abdominal effusion and large clumps of fibrin. The high viscosity of the effusion due to high protein content can be seen in Video 1.
(A, courtesy of Daniel Gerardi, Universidade Federal do Rio Grande do Sul, Brazil.)
Fig. 4.
Cat kidneys. (A) Multifocal to coalescing granulomatous inflammation (white, rough appearance) following the superficial blood vessels. (B) Cut section also shows the vascular-oriented distribution.
(Courtesy of RN Fuji, VMD, Ithaca, NY.)
Fig. 5.
Peritoneal cavity of a cat: intestine, liver, lymph node, spleen, and diaphragm. White-to-yellow soft plaques covering the parietal and visceral peritoneal surfaces (white arrow). The lymph nodes associated with large intestine are enlarged and yellow (black arrow).
Fig. 6.
Spleen from a cat. The capsular surface shows severe fibrinous inflammatory reaction that extends to the omentum. The inflammatory reaction is admixed with copious amounts of fibrin.
In the noneffusive or dry form of FIP, where there is minimal to no effusion, the inflammatory reaction can be restricted to individual organs, such as kidneys, eyes, or brain. In these cases, the lesions still have the distinctive vascular orientation characteristic of the disease. The inflammatory response in the dry form is characterized by a perivascular oriented granulomatous to pyogranulomatous reaction with or without vasculitis.
FIPV and Hypersensitivity
The characteristic perivascular granulomatous lesions associated with FIPV infection have been attributed to type III and IV hypersensitivity reactions.86, 87, 88 Type III hypersensitivity occurs when soluble antigen binds to antibody, forming immune complexes that can be deposited into the vessel walls, also leading to vasculitis.89 Complement activation and deposition in tissues also occur during FIPV. This response triggers disseminated intravascular coagulation (DIC), vasculitis, and blood vessel necrosis. Type IV hypersensitivity is a delayed reaction due to excessive stimulation of T-cells and macrophages, which may also contribute to granuloma formation.90 On the other hand, the pathology findings associated with hypersensitivity reactions might be secondary to monocyte activation in the development of vasculitis.83 This is further supported by new findings that release of vascular endothelial growth factor (VEGF) by FIPV-infected monocytes induces vascular permeability and effusions.91
Shedding of FCoV
Following exposure to FCoV, the primary stage of infection lasts from 7 to 18 months, when the highest levels of viral shedding occur.92 A dramatic decrease in shedding over 2 years has been reported in naturally infected cats.68 Therefore, infected cats can be broadly divided into 3 categories: those that shed FECV relatively consistently over long periods of time (consistent shedders, about 10%–15%), intermittent shedders (about 70%–80%), and nonshedders (<5%).92, 93, 94 In one study, 27% of adults shed FECV virus 75% of the time.95 Apparently, these consistent shedders were persistently infected with the same strain of the virus,68, 96 but cats that recovered from the infection were susceptible to reinfection with the same strain or different strains of the virus.96 It has been demonstrated that the colon is the major site of FECV persistence and a probable source for recurrent shedding.97 It is presumed that stress factors may contribute to persistent or intermittent shedding, especially in kittens,59 where fecal shedding starts within in 1 week and remains at consistently high levels from 2 to 10 months after infection.92 In addition, kittens shed higher levels of FECV than adult cats.66, 92 In one study, one-third of older cats and 90% of kittens and juveniles presented to shelters in Sacramento, California, USA, were shedding FECV at the time of entry.63 Approximately one third of cats positive for antibodies specific for FCoV shed the virus in the feces.98 It is of particular interest that cats shedding virus tended to have higher antibody titers (immunofluorescence assay [IFA] titers ≥100) than cats no longer shedding virus (titers ≥25).92 Quantification of virus may not be an absolute indicator of the viral load, because of the presence of factors that inhibit reverse trasncription–polymerase chain reaction (RT-PCR) in feline feces.50, 92 Cats may be able to clear the infection within 6 to 8 months if there is no reinfection.92 Virus clearance has been correlated with humoral99 and cell-mediated immune responses to the virus.100
FIPV and Innate Immunity
Several studies have shown that FIPV replicates in monocytes/macrophages,20, 48, 101, 102 but there are few studies regarding the nature of the innate immune response to FIPV infection. Natural killer cells (NK) typically release type I interferons (IFNα and IFNβ) in response to viral infection inducing interferon-stimulated gene (ISG) transcription.103, 104, 105 These results in an antiviral state, which coronaviruses such as SARSCoV have been shown to suppress.106, 107 In addition, monocytes and macrophages release proinflammatory cytokines such as tumor necrosis factor TNFα, interleukin (IL)-1, IL-6, and IL-12 in response to viral pathogens but also antiinflammatory IL-10 as an immune regulator that increases TNFα, which in turn has implications for the mostly cell-mediated adaptive immune response. Cats with FIP have been shown to express increased levels of these cytokines and monocytes or macrophages are suspected to play a role.108, 109
FIPV and Humoral Immunity
In most viral infections, the humoral response results in the generation of viral neutralizing antibodies, which are pertinent in preventing infection. However, in the case of FIPV, there is evidence that the humoral antibody response contributes to pathogenesis by a mechanism called antibody-mediated enhancement.87, 110 Antibodies to the spike protein, which is responsible for viral attachment, facilitate the uptake of the virus through Fc receptors on macrophages.111 Macrophages from FIPV-infected cats release increased levels of B-cell differentiation and survival cytokines, suggesting that enhanced B-cell activation plays a role in antibody-mediated enhancement of infection.112 Vaccine development has been discouraged mainly because of concerns regarding vaccine-induced enhancement of infection.113 However, antibody-mediated enhancement of FCoV infection has only been experimentally demonstrated with laboratory strains, and not with field strains.65 In addition, clearance of FCoV infection in naturally infected cats was associated with the presence of antibodies against spike protein of FIPV.99 The overall conclusions from experimentally infected cats indicate that humoral immunity does not play a large role in preventing FIPV infection and spread but might rather contribute to pathogenesis, at least in the laboratory setting.
FIPV and Cell-Mediated Immunity
In contrast to humoral immunity, it appears that the cell-mediated immune response plays an important role in fighting FIPV infection and several studies support this assumption. Pedersen and colleagues59 hypothesized that differences in humoral and cellular immunity manifest in differences in pathogenesis in cats with FIP. They suggested that a strong humoral response and weak cellular immunity lead to the wet effusive form of FIP, while humoral immunity with an intermediate cellular immune response results in the dry form of FIP. It has been shown with other coronavirus infections that a strong cellular response will prevent the disease.114, 115 Additionally, infection with FeLV (feline leukemia virus), a strong suppressor of cellular immunity, is associated with a higher incidence of FIP.76, 77, 116, 117 FIP is characterized by depletion of T-lymphocytes,118, 119 with CD4+ and CD8+ T-lymphocyte counts remaining low.100 It is not clear how this depletion occurs, as T cells do not appear to be susceptible to FIPV infection.118 De Groot-Mijnes100 theorized that this depletion leads to an acute immunodeficiency and that virus-induced T-cell responses face an uphill battle fighting the infection.
Recently, TNFα and interferon IFNγ have been shown to play a significant role in immunity and pathogenesis associated with FIPV infection. T-cells, B-cells, NK cells, and professional antigen-presenting cells (APCs) such as macrophages and dendritic cells secrete IFNγ,120 which is important in further activation of immune cells, especially macrophages,121, 122 and is likely to be important in early host defenses.121, 123 Macrophage recognition of PAMPs (pathogen-associated molecular patterns) induces the release of IL-12 and chemokines, which attract NK cells to the site of inflammation, promoting IFNγ synthesis.124, 125 Negative regulators of IFNγ production include anti-inflammatory cytokines, as well as glucocorticoids.126 IFNγ therefore, is crucial for the early innate response, as well as linking the innate to the adaptive immune response, especially cell-mediated adaptive immunity. Interestingly, clinically normal FCoV-infected cats living in catteries had higher serum IFNγ levels than cats with fulminant FIPV infection, suggesting it has an important role in suppressing the development of FIP.127 The IFNγ response can be compromised by several factors, in FIPV-infected cats, including stress.
Elevated TNFα release are linked to apoptosis of CD4+ and CD8+ T-lymphocytes, as well as macrophage upregulation of the aminopeptidase N receptor (APN),109, 128 the receptor for FIPV type II. Significant changes were observed in cats after immunization with FIPV and subsequent challenge, regarding proinflammatory cytokine messenger RNA (mRNA) levels in blood leukocytes. Specifically, cats developing the disease expressed high levels of TNFα and low levels of IFNγ. In contrast, in cats that were immune and did not develop FIP, TNFα levels were low with IFNγ levels being elevated. In summary, these studies suggest that FIPV infection leads to reduced cell-mediated immunity, possibly through compromising IFNγ release from blood leukocytes, increased TNFα release from infected monocytes/macrophages, and subsequent T-cell depletion.
Immunity and Stress in Shelter Cats
Shelter cats live in environments that predispose them to increased chronic stress. Stress leads to elevated glucocorticoid release, which in turn negatively regulated IFNγ production, and impaired T-cell function129, 130 with negative effects on cell-mediated immunity. Considering that cell-mediated immunity is most likely responsible for clearance of FIPV infection, it becomes obvious that reducing stress in shelter cats potentially improves their odds of successfully combating infection. Additionally, the close contact of cats in shelters facilitates transmission of any virus, enabling an RNA virus such as FCoV to proliferate and evolve, eventually, to a virulent virus. To address the problem of widespread FECV infection in shelter cats, as well as their increased risk of FIPV infection and consequent disease, it is critical to increase efforts to elucidate the role of the host immune response to FCoV.
Disease Presentation
Common Historical Findings
When cats are initially exposed to FCoV, they may be asymptomatic or have diarrhea and/or upper respiratory signs.82 Cats with coronavirus-associated enteritis can have mild signs of vomiting and/or diarrhea, which can be of short duration or last for weeks or even months.131 Gastrointestinal signs are generally mild or subclinical, and therapy is not required in most of the cases.
Physical Examination Findings
Although there is often a distinction made between the wet and dry forms of FIP, they are not mutually exclusive, and the progression of the disease may change from one form to the other. With both forms, an array of multiple clinical signs many be present, but none of them is pathognomonic for the disease. Patients may be asymptomatic or present with different levels of depression and anorexia. Other common findings include weight loss, pale mucous membranes, fever of unknown origin, and uveitis.73, 81
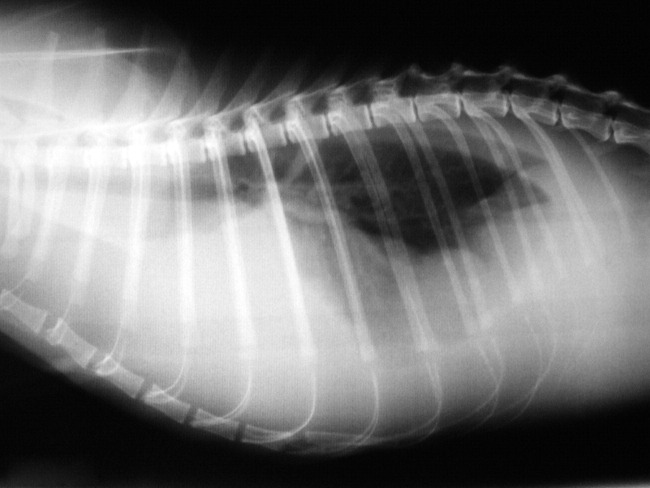
In the wet (effusive) form (see Video 1 online [within this article at www.vetsmall.theclinics.com, November 2011 issue]), ascites with abdominal distention is the most common presentation (Fig. 7). A fluid wave on physical examination may be evident, but some cats will have less fluid accumulation, only detectable by abdominal ultrasound. Pleural effusion with secondary dyspnea, tachypnea, and muffled heart sounds may present (Fig. 8), whereas pericardial effusion is uncommon.59, 131 The wet form can also be associated with several clinical signs identified in the dry form, described later.
Fig. 7.
Cat with wet (effusive) form of FIP presenting moderate abdominal distention due to peritoneal effusion. The abdominal distention is generally not evident in early stages, and may require imaging techniques to be confirmed.
Fig. 8.
Lateral thoracic radiograph image of a cat with pleural effusion due to FIP.
(Courtesy of Daniel Gerardi, Universidade Federal do Rio Grande do Sul, Brazil.)
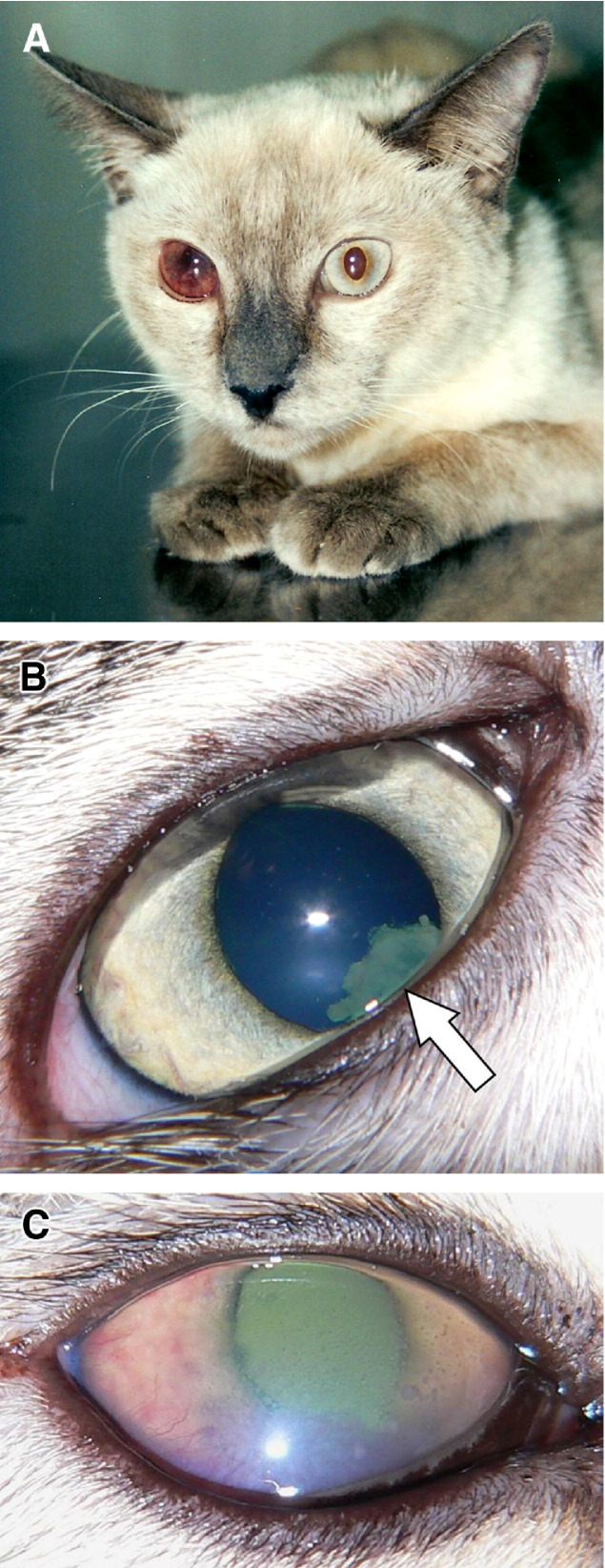
Common signs of the dry or noneffusive form are mild and intermittent fever, decreased appetite, weight loss, stunted growth, depression, pale or yellow mucous membranes, and palpable abdominal organ enlargement.73, 131 Pyogranulomatous lesions develop in one or more abdominal organ, and the clinical signs will be associated with the affected organ, mimicking hepatic or kidney insufficiency, or intestinal tumors.81 The pyogranulomatous lesions are detected on abdominal palpation as enlarged mesenteric lymph nodes and palpable nodular irregularities on the surface of kidneys and liver.73, 131 If granulomas form on the intestine, constipation, diarrhea, and/or vomiting may be the major clinical signs observed. Uveitis is the most common ocular abnormality documented in FIP cases, but other ocular lesions may be present, such as iritis, cuffing of the retinal vasculature, and keratic precipitates on the cornea (Fig. 9). 78, 81, 132 Neurologic signs can also be seen with FIP, the most common being abnormal mental status, ataxia, central vestibular signs, hyperesthesia, nystagmus, and seizures,133, 134, 135, 136 demonstrating that any part of the central nervous system can become affected in this disease.137
Fig. 9.
(A) Anterior uveitis typically seen in noneffusive cases of FIP. Mild iridal neovascularization (rubeosis iridis) and hyphema are evident in the anterior chamber of the right eye (OD). (B) Fibrin formation, hypopyon, and evidence of mild diapedesis are suggestive of blood–ocular barrier breakdown associated with mild anterior uveitis. (C) Severe iritis, with rubeosis iridis, aqueous flare, hypopyon, and keratitic precipitates. These precipitates, known as “mutton-fat” precipitates, are suggestive of a chronic granulomatous disease process.
(A, courtesy of Daniel Gerardi, Universidade Federal do Rio Grande do Sul, Brazil.)
Diagnosis
Almost half a century has passed since the first description of FIP in cats; nonetheless, the diagnosis of this syndrome remains one of the greatest challenges for veterinarians. Despite great advances in laboratory diagnostic techniques in the past decades, the diagnosis of FIP is still based on the combination of history of risk factors, signalment, clinical abnormalities, and laboratory findings.81 With exception of histopathology and immunostaining, no single laboratory test can definitely diagnose the FIP syndrome. Likewise, no diagnostic procedure can identify which FCoV-infected cats will go on to develop FIP. The diagnostic process starts with a good history and comprehensive physical examination.
Complete Blood Cell Count and Biochemical Profile
The complete blood cell count (CBC) and biochemical profile can be helpful in expanding the clinical picture of FIP. Often, as with most chronic illnesses in the feline patient, a nonregenerative anemia may be present. Other abnormalities may include but are not limited to lymphopenia, neutrophilia, thrombocytopenia, hyperbilirubinemia, and elevated aspartate aminotransferase (AST).72, 78, 138, 139, 140
Serum Proteins
Hyperproteinemia (>8.0 mg/dl) is a consistent finding, present in approximately 60% of the cats with FIP.73 This is mainly because of elevated serum globulin levels, caused by a specific antibody response, presence of complement, and immune complexes in the bloodstream.73, 141, 142 Hypoalbuminemia can be present associated with hepatic insufficiency or increased loss from endothelial leakage,141 resulting in decrease in the albumin:globulin (A:G) ratio (Table 2). Low A:G ratios are strongly associated with FIP, but other causes of hyperglobulinemia should always be ruled out.141, 143
Table 2.
Accuracy of various diagnostic tests for FIP
| Category | Test Type | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Prevalence (%) | Ref. |
|---|---|---|---|---|---|---|---|
| Protein analysis | Total protein ≥8 g/dl | 57 | 64 | 76 | 43 | 67 | 138, 143a |
| Gamma-globulin ≥2.5 g/dl | 70 | 86 | 90 | 61 | 65 | 143 | |
| A:G ratio | |||||||
| ≤0.8 | 80 | 82 | 92 | 61 | 72 | 143 | |
| <0.45 | 25 | 98 | 64 | 90 | 13 | 139 | |
| Protein electrophoresis | 38 | 50 | 60 | 29 | 67 | 144 | |
| α1-Acid glycoprotein levels >1.5 | 85 | 100 | 100 | 75 | 70 | 192 | |
| Effusion analysis | Total protein >3.5 g/dl | 87 | 60 | 77 | 71 | 72 | 142 |
| Gamma-globulin ≥1.0 g/dl | 82 | 83 | 84 | 80 | 53 | 143 | |
| A:G ratio | |||||||
| ≤0.9 | 86 | 74 | 79 | 82 | 53 | 143 | |
| ≤0.5 | 62 | 89 | 86 | 68 | 53 | 143 | |
| Rivalta test | 98 | 80 | 84 | 97 | 51 | 143 | |
| Presence of antibodies | 86 | 85 | 86 | 85 | 51 | 143 | |
| Cytology suggestive of FIP | 90 | 71 | 89 | 73 | 72 | 142 | |
| Antigen staining in macrophages | 72 | 100 | 100 | 68 | 62 | 142, 143, 193a | |
| Serology | IFA (any titer) | 85 | 57 | 44 | 90 | 28 | 143 |
| IFA (titer >1,600) | 67 | 98 | 94 | 88 | 28 | 143 | |
| ELISA | 100 | 93 | 94 | 100 | 53 | 155, 187,a | |
| Antigen–antibody complex | 48 | 91 | 67 | 84 | 26 | 143 | |
| Viral nucleic acid detection | Nested RT-PCR | ||||||
| Serum | 55 | 88 | 90 | 48 | 67 | 143, 163,a | |
| Effusion | 96 | 92 | 96 | 92 | 63 | 143, 162, 163,a | |
| mRNA RT-PCR | |||||||
| Blood | 94 | 92 | 67 | 92 | 15 | 168, 169, 170,a | |
Abbreviations: A:G ratio, albumin to globulin ratio; ELISA, enzyme-linked immunosorbent assay; IFA, immunofluorescent antibody assay; mRNA, messenger RNA; NPV, negative predictive value; PPV, positive predictive value; RT-PCR, reverse transcriptase polymerase chain reaction.
Calculated based on concatenated data from original studies.
Acute-Phase Proteins
Acute-phase proteins are a class of proteins whose plasma concentrations increase or decrease in response to inflammatory disorders. α1-acid glycoprotein levels greater than 1.5 g/L in plasma or effusions are suggestive of FIP,144 with diagnostic accuracy provided in Table 2. However, risk factors and clinical signs should be taken into account for the appropriate interpretation, since other inflammatory conditions can also cause increase in this protein.145 Therefore, in cats with clinical signs and supporting risk factors, a α1-acid glycoprotein value above 1.5 g/L is consistent with FIP, whereas in asymptomatic cats, α1-acid glycoprotein values equal to or above 3 g/L are needed to support the diagnosis of FIP.145
Effusion Fluid
In cats with the wet form of FIP, effusions from the abdomen or pleural space are typically clear, straw-colored, or viscous due to the high protein content (see Video 1 online [within this article at www.vetsmall.theclinics.com, November 2011 issue]). Sometimes the effusion can be red, pink, almost colorless, or even chylus.82 It is characterized as nonseptic, modified transudate or pyogranulomateous exudate. Cytology generally documents low cell count (<5,000 nucleated cells/ml) consisting of neutrophils and macrophages, but with a high protein content (>3.5 g/dl).82, 131 A high A:G ratio in the effusion (>0.8) is unlikely to be seen in FIP syndrome, whereas a A:G ratio less than 0.45 is highly suggestive of effusive FIP.131, 146
The Rivalta test, originally designed one century ago to differentiate transudates from exudates, provides good predictive values when compared to more expensive techniques (Table 2).82, 143 Detailed descriptions of how to perform this test are provided in written78, 81, 131 and video resources elsewhere.147 Due to its simplicity and low cost, the Rivalta test should be performed in any case of effusion in cats.143 IFA can be used to detect macrophages infected with FCoV in effusions. Positive staining of macrophages is 100% predictive of FIP, but false-negative results can occur with low levels of infection.142, 143
Serology
In the multicat environment, the quantification of FCoV antibodies is valuable for the following70, 82, 98:
-
•
Identifying cats exposed to FCoV prior to their introduction into a FCoV-free cattery
-
•
Screening a cattery for infection
-
•
Testing a cat that has been in contact with a suspected FCoV shedder
-
•
Establishing breeding programs based on FCoV status
-
•
Classifying cats based on shedding level for the purpose of isolation in FCoV-eradication programs.
Although there are several assays currently available that detect antibodies to FCoV, there is no serologic test capable of diagnosing the FIP syndrome, and serology cannot be used to differentiate between FECV and FIPV infections. A positive titer only indicates that a given cat has been exposed to FCoV and cannot predict if the cat will ever develop FIP. Conversely, a negative titer is a good predictor of the absence of infection (90% negative predictive value).143 Because the disease is caused by the FIPV, which arises from a mutant of the common FECV, control and prevention of the FIP syndrome must be directed first at control of its parent virus.94 Therefore, knowledge of antibodies titers to FCoV can be helpful in controlling and eradicating the virus from multicat environments. Approximately one third of cats presenting with antibodies to FCoV shed FECV in the feces.98 Cats with titers of 25 or less are often shedding low levels of FECV.93 These cats frequently stop shedding when isolated from other cats.94 Cats with titers of 400 or greater are frequently shedding high levels of FECV. When isolated, some of these cats will stop shedding, with concurrent decrease in titers. Cat with persistently high antibody titers generally are consistently shedding.81, 94 If isolation and stress reduction do not promote a decrease in shedding, removal of these consistently shedders from multicat environments should be taken into consideration.
It has been suggested that very high antibody titers (≥1,600) are good predictors of the development of FIP (94% positive predictive value, Table 2).143 However, several studies have described cats with confirmed FIP in which no serologic response to FCoV was detected.145, 148, 149 This is particularly true in cats with the wet form of FIP. It is suggested that large amounts of virus are present that can bind to antibodies, making them unavailable for the antibody test in these cases. An alternative explanation is that antibodies against FCoV are lost in the effusion when protein is translocated due to vasculitis.82 The quantification of antibodies in effusions correlates with the presence of antibodies in blood,150 suggesting effusions may be a more useful than testing sera.141 However, other studies have shown no correlation between magnitudes of antibody titers with the occurrence of FIP.82, 143, 151 Specific antibodies against FCoV may also be detected in CSF of cats with the neurologic form of FIP,136 but the diagnostic value of their presence is limited because anti-FCoV antibodies were also detected in cats with brain tumors.133 In addition, vaccination can also result in a positive titer and cannot be differentiated from natural exposure.152
The expression of the 7b gene was reported to be associated with FIPV infection.153 Consequently, cats with clinical signs of FIP would have titers against 7b protein higher than cats infected only with FECV. Unfortunately, other studies suggest these findings may be artifactually related to the specific isolate tested. Furthermore, intact 7b genes were described in other field strains of FECV.52, 58 Testing for antibodies directed against the 7b protein was compared against the IFA in one study. The authors showed that the 7b protein assay had high sensitivity but poor specificity, with many false-positive results occurring in uninfected animals.154 Therefore, this test should not be used alone for the diagnosis of FIP. Regardless of these findings, the 7b protein test has been advertised as “FIP Specific ELISA” by a commercial laboratory in the United States.
Several protocols, including enzyme-linked immunosorbent assay (ELISA),155 kinetics-based ELISA,156 virus neutralization assays,157 and indirect IFA, have been developed to detect antibodies specific for FCoV.67, 92 The choice of the laboratory is important, since methodologies and antibody titer results can vary significantly among laboratories.82 Clinicians should be encouraged to select a diagnostic service for which the methodology in use is supported by peer-reviewed publications. In addition, results should be provided as endpoint titers.82, 158 One should also understand that false-positive results can occur, for example due to antinuclear antibodies (ANA), which can be caused by concurrent infections (FIV, Ehrlichia canis), autoimmune disease, recent vaccination, or certain drugs, including thiamazole and methimazole.158, 159, 160
RT-PCR
The RT-PCR assay can detect FCoV in a variety of samples (feces, blood, effusion, cerebrospinal fluid, tissue, and saliva) with high sensitivity (Table 2).93, 161, 162, 163 In multicat environments, RT-PCR can be a valuable tool to identify continuous shedders as part of an FCoV management plan. However, repeated fecal RT-PCR tests are generally necessary to accurately document if a cat is shedding FCoV. In order to demonstrate that a cat has stopped shedding the virus, at least 5 consecutive monthly negative fecal tests should be obtained, or the cat should become seronegative by IFA. Due to the inherit risk of false-negative and false-positive results, RT-PCR results are best interpreted in conjunction with serology results.93
RT-PCR cannot discriminate between FECV and FIPV due to the various single nucleotide polymorphisms (SNPs) and deletion mutations present in both biotypes, sometimes even identified from the same cat.46, 164, 165 At the time of writing, no specific genetic determinants that trigger the evolution of FECV to FIPV or otherwise distinguish the 2 biotypes have been confirmed. Due to these particularities of FCoV, a specific RT-PCR for FIPV cannot, as yet, be designed.
Despite the FECV tropism for feline enterocytes, the enteric virus can be detected by RT-PCR in the bloodstream of healthy cats.161 Therefore, the detection of FCoV in blood does not indicate the presence of FIPV and cannot solely support the diagnosis of the FIP syndrome. In addition, the presence of viremia does not appear to predispose the cats to the development of FIP.161
The presence of FCoV in effusions by as detected by RT-PCR is associated with the FIP syndrome, but reports of false-positive results indicate that the specificity is limited. The combined data from three initial studies indicated sensitivity of 96% and specificity of 92% for the diagnosis of FIP using RT-PCR to detect FCoV RNA in effusions from 23 FIP-confirmed cats and 13 cats with effusions due to other causes (Table 2). The detection of FCoV by RT-PCR in biopsy samples or fine needle aspirates of affected organs is considered suggestive of the systemic disease, if blood contamination of samples can be ruled out.81 However, it is suggested that histopathologic examination and immunohistochemistry should be performed to confirm the diagnosis, since in one study, 51 of 84 (60.7%) cats without clinical signs of FIP were positive for FCoV in tissue samples by RT-PCR.166
mRNA RT-PCR
In 2005, a PCR procedure targeting the mRNA of the highly conserved M gene of FCoV was described with potential for detecting only replicating virus.167 The concept was based on the assumption that during the pathogenesis of FIPV, the mutant virus replicates in peripheral blood monocytes and tissue macrophages. Therefore, detection of FCoV mRNA in blood samples would correlate with replication of FIPV and the development of FIP. Two studies in Europe and one in Malaysia have used this technique, with sensitivity ranging from 93% to 100%. However, the percentage of false negatives varied from 5% to 52%.168, 169, 170 These variations may be associated with population selection, criteria used for diagnosis of FIP, and different RNA extraction procedures that may affect the quality of RNA template and downstream assays. The College of Veterinary Medicine at Auburn provides this PCR test for blood, effusion, and tissue, and results are provided in a semiquantitative scale. Unfortunately, at the time of writing, no epidemiologic data from the United States are available using the mRNA RT-PCR assay. Longitudinal studies are needed to determine if cats with replicating FCoV in the bloodstream have a higher risk for developing FIP in the future.
Histopathology
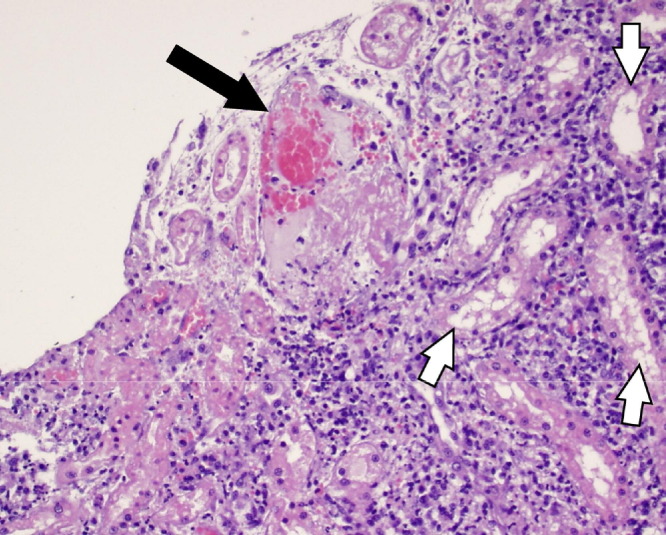
The gold standard and definitive diagnostic test available for FIP is provided by histopathologic examination. In the majority of cases, FIP can be diagnosed by gross and histopathologic lesions alone. The distinctive inflammatory infiltrates are characterized by varying degrees of severity and present with a combination of macrophages, lymphocytes, and plasma cells, mixed with lesser numbers of neutrophils.82, 83 The hallmark of the lesion is a perivascular granulomatous to pyogranulomatous inflammation and vasculitis. The vessels primarily affected are small to medium-size veins (Fig. 10). 83 The perivascular macrophage-dominated infiltrate occasionally extends into the vessel wall, producing focal areas of necrosis and sporadic smooth muscle hyperplasia (Fig. 11). Vasculitis is one of the microscopic lesions that distinguishes the disease from other inflammatory infectious diseases.
Fig. 10.
Kidney. Superficial renal venules. Necrotic tubular epithelial cells (white arrows) with severe interstitial pyogranulomatous inflammation. The small venule (black arrow) contains an intravascular fibrin thrombus and with moderate mural vascular necrosis (hematoxylin-eosin, original magnification ×20).
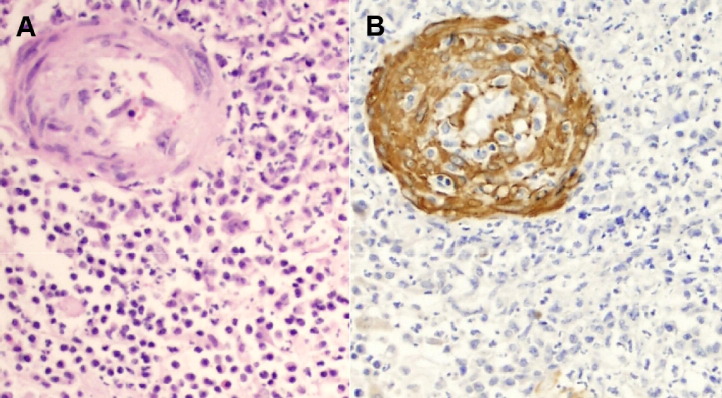
Fig. 11.
Spinal cord. (A) There is severe pyogranulomatous inflammation that is most intense around the blood (hematoxylin-eosin, original magnification ×60). (B) The vessel wall is stained in brown and shows thickening of the wall by moderate to severe smooth muscle hyperplasia (smooth muscle actin with peroxidase stain, original magnification ×60).
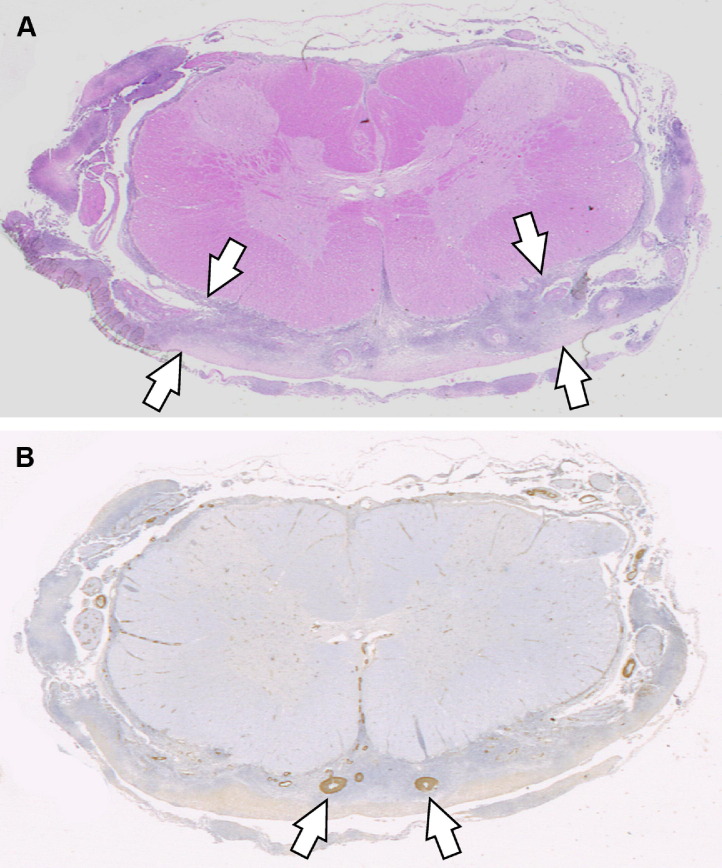
In cases of the noneffusive or dry form, brain, spinal cord, or eyes might be the only sites affected. Histopathologic lesions in the brain could include periventriculitis, ventriculitis, ependymitis, and/or leptomeningitis with vascular-oriented inflammatory reaction with or without vasculitis as the distinctive inflammatory lesion (Fig. 12). Lesions affecting the eyes have been reported as bilateral granulomatous anterior uveitis often accompanied by chorioretinitis.171
Fig. 12.
Spinal cord. (A) Subgross cross-section with marked thickening of the meninges due to pyogranulomatous inflammation (between white arrows). (B) Immunohistochemistry for smooth muscle actin indicates marked medial thickening of the small or medium-size vessels due to smooth muscle hyperplasia (white arrows).
Recently, a nonpruritic intradermal cutaneous form of FIP has been described.172, 173 The skin lesions are described as slightly raised intradermal papules over the dorsal neck and on both lateral thoracic walls. In one of the cases reported, the patient was also infected with FIV.172
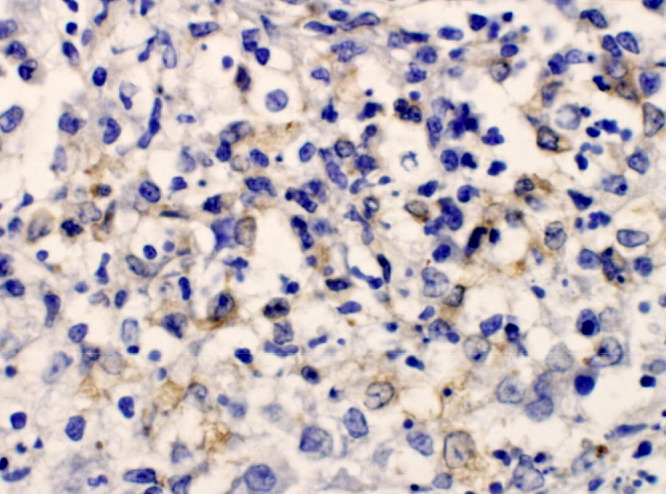
Immunostaining
When pathognomonic lesions are not present in histopathology, the detection of intracellular FCoV antigen in macrophages in effusions by immunofluorescence or in tissue by immunohistochemistry is the alternative diagnostic procedure (Fig. 13). 82 Unfortunately, these procedures cannot differentiate between FIPV and FECV, but positive antigen staining of macrophages in effusions or granulomatous lesions confirms the diagnosis for FIP.81, 143 In some instances, lesions can resemble systemic fungal infection, and it may be pertinent to rule this out with special histochemical stains. In the immunostaining of the effusion, false-negative results may occur and are explained by the possibility of an insufficient number of macrophages on the effusion smear or the presence of high quantity of host anti-FCoV antibodies in the effusion competing with the assay.59, 82
Fig. 13.
Brain, lateral ventricle from a cat with FIP (FCoV immunohistochemistry stain). Macrophages within the lesion have intense cytoplasmic staining (gold-brownish color), confirming the presence of viral antigen (monoclonal antibody 1:400, original magnification ×60).
Prognosis
With the development of FIP, prognosis is poor to grave, with a reported survival time between 3 and 200 days.174 All of these animals eventually die from the disease. Euthanasia is recommended when quality of life becomes poor.
Treatment of FIP
Although treatment is focused on reducing the inflammatory and hyperimmune response, no studies have been published to prove any beneficial effects of corticosteroids. There have been several antivirals and immunosuppressants considered for use in FIP cases, and a review of the evidence-based data about therapy is provided elsewhere.78 Of the antivirals, ribavirin and vidarabine, which are effective in inhibiting virus in cell culture, are toxic in cats. Human IFNα is contraindicated orally and is ineffective with subcutaneous administration.78 Currently, feline interferon treatment is one of the options to treat FIPV-infected cats, although studies show differences in efficacy.175 Of the immunosuppressants, prednisone/dexamethasone at immunosuppressive doses is the treatment of choice but such treatment is not curative and may only slow the progression of the disease.78, 176 Recently, a new immunostimulant named polyprenyl improved survival in 3 cats with the dry form of FIP, with 2 of them still alive 2 years after the diagnosis. Polyprenyl enhances cell-medicated immunity by upregulating biosynthesis of mRNA of Th-1 cytokines,177 which is believed to be required to eliminate the FIP virus. Further studies with a larger number of cats are currently under way.
Prevention
Vaccination
A modified-live, nonadjuvanted, intranasal coronavirus vaccine is available that may provide some protection to cats that have not been previously exposed to FCoV. Preventable fractions between 0% and 75% have been reported.178, 179, 180, 181 Vaccination could be advantageous for cats with a negative FCoV titer, if they are entering a multicat environment known to be endemic for FCoV or to have been exposed to FCoV. However, its effectiveness is questionable in situations when cats have already been exposed, which frequently occurs in multicat environments. The vaccination is currently not recommended as a core vaccine in the feline patient.182, 183
Co-infections
Since immunocompromised cats shed much more viruses45 and perhaps have less ability to fight off mutant strains, screening and control of other infectious organisms, such as FeLV and FIV, in multicat environments are recommended for the management of FIP. It is a current practice in some shelters to keep FeLV- and FIV-infected individuals for “special needs adoptions.” It is important for shelter managers and staff to understand the additional risks such a population poses to the rest of the feline residents and to ensure that measures are taken to minimize these risks. One might reconsider maintaining such populations in the shelter environment. A better option may be to house FeLV- and/or FIV-positive cats with an appropriate rescue organization, to separate them from the rest of the shelter population. Depopulation of FeLV- and/or FIV-positive cats is also an alternative.
Stress
Noise, overcrowding, and inefficient ventilation are a few of the many stress factors, especially in a shelter or cattery environments, that may contribute to the development of FIP in a given population. In the design and management of facilities that house cats, these issues should be addressed. To establish consistency and to introduce new approaches to infection control measures throughout a facility, having accessible “policies and procedures” may prove helpful in keeping compliance among the staff in instituting and maintaining appropriate protocols.184
Disinfection
FCoV can survive for 7 weeks in a dry environment and can be transmitted via feces and fomites, so proper cleaning and disinfection are essential in the management of the infection in feline populations. The majority of organic debris should be removed prior to use of disinfectants. A simple 1:32 dilution of sodium hypochlorite (equivalent to 1:10 dilution of the commercially available bleach) is an option but should be protected from light and should be prepared at the time of use. The majority of disinfectants effectively inactivates FCoV81; however, it has been suggested that some disinfects may be a more appropriate. Oxidizing agents (eg, Trifectant, Virkon-S, Oxy-Sept 333) are considered effective, whereas some of the quaternary ammonium compounds (eg, Roccal, Parvosol, DiQuat), biguanides (chlorhexidine), and phenolic compounds (eg, Lysol, TekTrol, Amphyl) have limited activity against enveloped viruses.184 The virus is rarely found in saliva of healthy cats so contact with feeding bowls probably plays a minor role in transmission compared to the sharing of litter boxes among individuals.93 Nonetheless, proper disinfection of all potentially contaminated surfaces is warranted.
Management
Cat Management After Exposure
If a single cat is diagnosed with FIP, it is recommended to wait at least 2 months before a new cat is introduced into the household so that FCoV infection is likely to be minimal or absent from the environment.78 If FIP is diagnosed in a multicat household, there is no need to isolate the other cats as they have most likely already been exposed to FECV. If the other cats in the environment are genetically related, the risk of FIP to occur may be higher due to lineage predisposition.75, 78, 79
Multicat Environments
The key to control FCoV in a shelter/foster home is to minimize the viral load in the environment. Reducing the number of cats per room/cage; grouping high FCoV shedders, low shedders, and negative cats separately; decreasing stress; controlling concurrent illness; keeping surfaces and litter trays clean; and providing sufficient litter trays are the best methods to achieve this goal (Table 3). 70, 78, 81, 176 Despite these precautions, the evaluation of the infection status of the population is still warranted for successful control of FCoV in a multicat environment.
Table 3.
Common methods to prevent FCoV infection and control feline infectious peritonitis outbreaks in multicat environments
| Method | Effectiveness | Advantages | Disadvantages | Comments |
|---|---|---|---|---|
| Individual cages | Effective | Decreases exposure to FCoV | Requires bigger infrastructure and personnel Decreases socialization of cats |
If not an option consider monitoring potential shedders in group facilities. |
| In-cage spot cleaning | Effective | Decreases stress by preventing frequent rehousing of cats | Requires more frequent staff monitoring of litter trays | Not only may decrease the viral load in the environment but presents a more appealing environment for potential adopters. |
| Isolation or quarantine of cats exposed to FIP cases | Inefficient | None | True quarantine is hard to be performed Decreases socialization of cats |
The majority of cats in the same environment are already infected with FCoV when FIP arises. It can take months for FIP to develop, and it occurs in a small percentage of the population |
| Staff workflow from new cats to longer term residents | Effective | Reduces exposure of more vulnerable population to shedders among longer term residents | Staff compliance with protocol may present a challenge | Fomites can easily transmit FCoV between different areas. This method will not eliminate but may reduce fomite transmission between populations. |
| Segregation by length of time | Partially effective | Limits exposure between populations Increases socialization | May be difficult to arrange distribution of populations within physical plant limitations | As younger cats are at an increase risk of infection, segregating the younger cats and kittens from adults helps limit their exposure to FCoV |
| Segregation by antibody status | Effective | Prevents exposure of naïve cats Increases socialization | Requires isolation of new cats until serology results are available | Expense of serology may be a limiting factor. |
| Grouping by shedding status | Effective | Prevents reinfection of cats Increases socialization | Requires frequent serology or fecal PCR testing to determine shedding status | Only 1/3 of the seropositive cats shed the virus. Repeated fecal PCR test are required to document shedding. Expenses of lab tests may be a limiting factor. |
| Isolation and removal of chronic shedders from facility | Partially effective | Decreases risk of FIP by reducing frequent re-exposure to FCoV | May require depopulation if chronic shedders are not adoptable. May increase risk of FIP in other cats at the adopters environment |
Shedding decreases once the cat is isolated. Chronic shedders should be adopted only to single-cat households. |
| Visitor's flow from new cats to longer term residents | Partially effective | Reduces exposure of more vulnerable population to shedders among longer term residents | Keeping visitors consistent with protocol may present a challenge Predisposes new cats in the shelter to be adopted more frequently than long term residents |
Visitors should be encouraged to adopt long term residents. |
| Vaccination | Partially effective | May decrease incidence of FIP in the long term | At the age of vaccination (16 weeks) the majority of cats in a shelter have already been exposed to FCoV | The vaccine is ineffective when cats have already had contact with FCoV. Not currently recommended for shelters. |
| Depopulation | Ineffective | Decreases amount of FCoV present in the environment Decreases the risk of exposure of new intakes to FCoV Prevents adoption of FCoV-infected cats |
It must be followed by extensive disinfection of facility and introduction of strict biosecurity protocols. Poor shelter reputation regarding euthanasia of “healthy cats”. Decrease moral of shelter staff attached to resident cats. |
Depopulating only certain “sick” individuals is not effective as an apparently healthy cat may be chronic or intermittent shedder. Depopulating seropositive cats is not recommended due to the small number that may ever develop FIP. FCoV can easily become endemic again if other strict measures are not implemented. |
In catteries, several methods have been attempted to minimize FIP outbreaks. Kittens are removed from the cattery (and from the mother if she has a positive titer for FCoV) and isolated at 3 to 4 weeks of age to prevent exposure to FCoV. This method may prove effective as kittens are protected from FCoV via maternal antibodies until about 4 to 6 weeks of age.67, 70 Although a genetic component for predisposition is not well established,75 the removal of cats that has produced 2 or more litters affected by the disease from a breeding program is recommended.82 Because the virus is very easily transmitted via fomites, isolation is not a particularly effective method of control.78 Depopulation of shedders is generally not effective and requires specific diagnostic tests to identify shedders, which may not be cost effective for some catteries and shelters. Currently, complete elimination of FCoV in these multicat environments would seem to be virtually impossible.176
Outbreak Management
When an outbreak of FIP occurs in a shelter setting, several options should be considered, such as increased sanitation, isolation (segregation of infected and uninfected animals), depopulation, and adopters/community education. The characteristics of common methods for prevention and control of FIP outbreaks in multicat environments are presented at Table 3.
Even in shelters that follow strict sanitation or biosecurity guidelines, periodic reviewing and updating cleaning practices (especially in the event of an outbreak) are recommended. Good protocols that reduce stress and the amount of fomite transmission of FCoV are (1) to keep cats in the cage while cleaning, (2) daily “in-cage spot cleaning,” and (3) deep cleaning of cages when the individual resident has changed. A detailed approach for FIP outbreaks in shelters and foster homes has been published elsewhere.81
Isolation is inefficient when an outbreak occurs. As incoming kittens are at the greatest risk, the physical separation between exposed/at-risk cats and newly acquired ones is recommended. This separation should not only create a physical barrier but also involve client and staff flow within a facility (handling of new population first and then exposed cats last). These procedure may not eliminate infection with FCoV, but it will at least reduce exposure to the virus.79
Depopulation may be used to control FIP outbreaks, but it requires the removal of the exposed population, comprehensive disinfection of the facility and equipments, and adoption of strict biosecurity methods, which are unfeasible for most of the shelters. Depopulation of cats seroreactive to FCoV is not recommended, since most cats will have antibodies against the virus, but very few will ever develop FIP.81 In addition, depopulation poses ethical, as well as public relation issues for any shelter.
Client Education
Although the incidence of FIP is fairly low, when outbreaks do occur, the impact on a facility can be profoundly damaging. When a cat adopted from a shelter develops FIP, it causes an emotionally and financially traumatic experience for the adopter, which can damage the reputation for the shelter. Ultimately, these cases can result in a lower adoption and higher euthanasia rates for the facility. Educating adopters about FCoV and FIP and the unfortunate consequences of infection in a multicat facility, prior to adopting a cat, is crucial in maintaining a good relationship with the public. Information regarding signs and symptoms is helpful in making a quicker diagnosis for the patient/client when such unfortunate scenarios arise.79, 81, 82
Summary
An interdisciplinary approach is needed to better understand the relationship of FCoV and FIP. The epizoology and diagnostics assist in providing the stated management protocols aimed to decrease the risks of cats in shelters for developing FIP. Although FIP has been undeniably linked to FCoV infection, the mechanisms that permit the rather benign FECV to evolve into the FIPV are still unknown. As FIP is intimately connected to the immune responses of affected animals, the details of this interaction and the pathogenesis of FIPV will be valuable in designing therapeutic and prophylactic prevention, as will our understanding of prophylactic immunization. Currently, the best weapon for diminishing the occurrences of FIP in multicat environments is to use appropriate biosecurity protocols. Unfortunately, the highly infectious nature of the FECV and our lack of understanding of its evolution to FIPV causing either the dry or wet form of FIP make elimination of risk virtually impossible.
Acknowledgments
The authors thank Drs Elizabeth Boynton and Linda Kidd for their review of this manuscript, Dr Christine Tindal Green for the description of the eye figures, and John Greenwood for his assistance.
Footnotes
Disclosure: Pedro Diniz has received speaker honoraria from Boehringer Ingelheim Pharmaceuticals, Inc.
Supplementary data
References
- 1.Rohrbach B.W., Legendre A.M., Baldwin C.A., et al. Epidemiology of feline infectious peritonitis among cats examined at veterinary medical teaching hospitals. J Am Vet Med Assoc. 2001;218(7):1111–1115. doi: 10.2460/javma.2001.218.1111. [DOI] [PubMed] [Google Scholar]
- 2.Cave T.A., Thompson H., Reid S.W., et al. Kitten mortality in the United Kingdom: a retrospective analysis of 274 histopathological examinations (1986 to 2000) Vet Rec. 2002;151(17):497–501. doi: 10.1136/vr.151.17.497. [DOI] [PubMed] [Google Scholar]
- 3.Decaro N., Buonavoglia C. An update on canine coronaviruses: viral evolution and pathobiology. Vet Microbiol. 2008;132(3-4):221–234. doi: 10.1016/j.vetmic.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garwes D.J. Transmissible gastroenteritis. Vet Rec. 1988;122(19):462–463. doi: 10.1136/vr.122.19.462. [DOI] [PubMed] [Google Scholar]
- 5.Perlman S., Dandekar A.A. Immunopathogenesis of coronavirus infections: implications for SARS. Nat Rev Immunol. 2005;5(12):917–927. doi: 10.1038/nri1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharpee R.L., Mebus C.A., Bass E.P. Characterization of a calf diarrheal coronavirus. Am J Vet Res. 1976;37(9):1031–1041. [PubMed] [Google Scholar]
- 7.Ward J.M. Morphogenesis of a virus in cats with experimental feline infectious peritonitis. Virology. 1970;41(1):191–194. doi: 10.1016/0042-6822(70)90070-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pedersen N.C., Boyle J.F., Floyd K. Infection studies in kittens, using feline infectious peritonitis virus propagated in cell culture. Am J Vet Res. 1981;42(3):363–367. [PubMed] [Google Scholar]
- 9.Collisson E.W., Pei J., Dzielawa J., et al. Cytotoxic T lymphocytes are critical in the control of infectious bronchitis virus in poultry. Dev Comp Immunol. 2000;24(2-3):187–200. doi: 10.1016/s0145-305x(99)00072-5. [DOI] [PubMed] [Google Scholar]
- 10.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson L.J., Tong S. Update on SARS research and other possibly zoonotic coronaviruses. Int J Antimicrob Agents. 2010;36(Suppl 1):S21–S25. doi: 10.1016/j.ijantimicag.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorbalenya A.E., Snijder E.J., Spaan W.J. Severe acute respiratory syndrome coronavirus phylogeny: toward consensus. J Virol. 2004;78(15):7863–7866. doi: 10.1128/JVI.78.15.7863-7866.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai M.M.C., Perlman S., Anderson L.J. In: Knipe D.M., Howley P.M., editors. vol 1. Lippincott William & Wilkins; Philadelphia: 2007. Coronaviridae; pp. 1305–1335. (Fields virology). [Google Scholar]
- 14.Pedersen N.C., Ward J., Mengeling W.L. Antigenic relationship of the feline infections peritonitis virus to coronaviruses of other species. Arch Virol. 1978;58(1):45–53. doi: 10.1007/BF01315534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wise A.G., Kiupel M., Maes R.K. Molecular characterization of a novel coronavirus associated with epizootic catarrhal enteritis (ECE) in ferrets. Virology. 2006;349(1):164–174. doi: 10.1016/j.virol.2006.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonzalez J.M., Gomez-Puertas P., Cavanagh D., et al. A comparative sequence analysis to revise the current taxonomy of the family Coronaviridae. Arch Virol. 2003;148(11):2207–2235. doi: 10.1007/s00705-003-0162-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gorbalenya A.E., Enjuanes L., Ziebuhr J., et al. Nidovirales: evolving the largest RNA virus genome. Virus Res. 2006;117(1):17–37. doi: 10.1016/j.virusres.2006.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobs L., de Groot R., van der Zeijst B.A., et al. The nucleotide sequence of the peplomer gene of porcine transmissible gastroenteritis virus (TGEV): comparison with the sequence of the peplomer protein of feline infectious peritonitis virus (FIPV) Virus Res. 1987;8(4):363–371. doi: 10.1016/0168-1702(87)90008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrewegh A.A., Smeenk I., Horzinek M.C., et al. Feline coronavirus type II strains 79-1683 and 79-1146 originate from a double recombination between feline coronavirus type I and canine coronavirus. J Virol. 1998;72(5):4508–4514. doi: 10.1128/jvi.72.5.4508-4514.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hohdatsu T., Nakamura M., Ishizuka Y., et al. A study on the mechanism of antibody-dependent enhancement of feline infectious peritonitis virus infection in feline macrophages by monoclonal antibodies. Arch Virol. 1991;120(3-4):207–217. doi: 10.1007/BF01310476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hohdatsu T., Okada S., Ishizuka Y., et al. The prevalence of types I and II feline coronavirus infections in cats. J Vet Med Sci. 1992;54(3):557–562. doi: 10.1292/jvms.54.557. [DOI] [PubMed] [Google Scholar]
- 22.Pedersen N.C., Evermann J.F., McKeirnan A.J., et al. Pathogenicity studies of feline coronavirus isolates 79-1146 and 79-1683. Am J Vet Res. 1984;45(12):2580–2585. [PubMed] [Google Scholar]
- 23.Shiba N., Maeda K., Kato H., et al. Differentiation of feline coronavirus type I and II infections by virus neutralization test. Vet Microbiol. 2007;124(3-4):348–352. doi: 10.1016/j.vetmic.2007.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rottier P.J. The molecular dynamics of feline coronaviruses. Vet Microbiol. 1999;69(1-2):117–125. doi: 10.1016/S0378-1135(99)00099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horsburgh B.C., Brierley I., Brown T.D. Analysis of a 9.6 kb sequence from the 3' end of canine coronavirus genomic RNA. J Gen Virol. 1992;73(Pt 11):2849–2862. doi: 10.1099/0022-1317-73-11-2849. [DOI] [PubMed] [Google Scholar]
- 26.Motokawa K., Hohdatsu T., Hashimoto H., et al. Comparison of the amino acid sequence and phylogenetic analysis of the peplomer, integral membrane and nucleocapsid proteins of feline, canine and porcine coronaviruses. Microbiol Immunol. 1996;40(6):425–433. doi: 10.1111/j.1348-0421.1996.tb01089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wesley R.D. The S gene of canine coronavirus, strain UCD-1, is more closely related to the S gene of transmissible gastroenteritis virus than to that of feline infectious peritonitis virus. Virus Res. 1999;61(2):145–152. doi: 10.1016/S0168-1702(99)00032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L., Junker D., Collisson E.W. Evidence of natural recombination within the S1 gene of infectious bronchitis virus. Virology. 1993;192(2):710–716. doi: 10.1006/viro.1993.1093. [DOI] [PubMed] [Google Scholar]
- 29.Wang L., Junker D., Hock L., et al. Evolutionary implications of genetic variations in the S1 gene of infectious bronchitis virus. Virus Res. 1994;34(3):327–338. doi: 10.1016/0168-1702(94)90132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang L., Xu Y., Collisson E.W. Experimental confirmation of recombination upstream of the S1 hypervariable region of infectious bronchitis virus. Virus Res. 1997;49(2):139–145. doi: 10.1016/S0168-1702(97)01466-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang X.W., Yap Y.L., Danchin A. Testing the hypothesis of a recombinant origin of the SARS-associated coronavirus. Arch Virol. 2005;150(1):1–20. doi: 10.1007/s00705-004-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Groot R.J., Andeweg A.C., Horzinek M.C., et al. Sequence analysis of the 3'-end of the feline coronavirus FIPV 79-1146 genome: comparison with the genome of porcine coronavirus TGEV reveals large insertions. Virology. 1988;167(2):370–376. doi: 10.1016/0042-6822(88)90097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Banner L.R., Lai M.M. Random nature of coronavirus RNA recombination in the absence of selection pressure. Virology. 1991;185(1):441–445. doi: 10.1016/0042-6822(91)90795-D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benetka V., Kubber-Heiss A., Kolodziejek J., et al. Prevalence of feline coronavirus types I and II in cats with histopathologically verified feline infectious peritonitis. Vet Microbiol. 2004;99(1):31–42. doi: 10.1016/j.vetmic.2003.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duarte A., Veiga I., Tavares L. Genetic diversity and phylogenetic analysis of Feline Coronavirus sequences from Portugal. Vet Microbiol. 2009;138(1-2):163–168. doi: 10.1016/j.vetmic.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kummrow M., Meli M.L., Haessig M., et al. Feline coronavirus serotypes 1 and 2: seroprevalence and association with disease in Switzerland. Clin Diagn Lab Immunol. 2005;12(10):1209–1215. doi: 10.1128/CDLI.12.10.1209-1215.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pedersen N.C., Allen C.E., Lyons L.A. Pathogenesis of feline enteric coronavirus infection. J Feline Med Surg. 2008;10(6):529–541. doi: 10.1016/j.jfms.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pedersen N.C., Black J.W., Boyle J.F., et al. Pathogenic differences between various feline coronavirus isolates. Adv Exp Med Biol. 1984;173:365–380. doi: 10.1007/978-1-4615-9373-7_36. [DOI] [PubMed] [Google Scholar]
- 39.Tusell S.M., Schittone S.A., Holmes K.V. Mutational analysis of aminopeptidase N, a receptor for several group 1 coronaviruses, identifies key determinants of viral host range. J Virol. 2007;81(3):1261–1273. doi: 10.1128/JVI.01510-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tresnan D.B., Holmes K.V. Feline aminopeptidase N is a receptor for all group I coronaviruses. Adv Exp Med Biol. 1998;440:69–75. doi: 10.1007/978-1-4615-5331-1_9. [DOI] [PubMed] [Google Scholar]
- 41.Benbacer L., Kut E., Besnardeau L., et al. Interspecies aminopeptidase-N chimeras reveal species-specific receptor recognition by canine coronavirus, feline infectious peritonitis virus, and transmissible gastroenteritis virus. J Virol. 1997;71(1):734–737. doi: 10.1128/jvi.71.1.734-737.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kolb A.F., Hegyi A., Maile J., et al. Molecular analysis of the coronavirus-receptor function of aminopeptidase N. Adv Exp Med Biol. 1998;440:61–67. doi: 10.1007/978-1-4615-5331-1_8. [DOI] [PubMed] [Google Scholar]
- 43.Pedersen N.C. Virologic and immunologic aspects of feline infectious peritonitis virus infection. Adv Exp Med Biol. 1987;218:529–550. doi: 10.1007/978-1-4684-1280-2_69. [DOI] [PubMed] [Google Scholar]
- 44.Chang H.W., de Groot R.J., Egberink H.F., et al. Feline infectious peritonitis: insights into feline coronavirus pathobiogenesis and epidemiology based on genetic analysis of the viral 3c gene. J Gen Virol. 2010;91(Pt 2):415–420. doi: 10.1099/vir.0.016485-0. [DOI] [PubMed] [Google Scholar]
- 45.Poland A.M., Vennema H., Foley J.E., et al. Two related strains of feline infectious peritonitis virus isolated from immunocompromised cats infected with a feline enteric coronavirus. J Clin Microbiol. 1996;34(12):3180–3184. doi: 10.1128/jcm.34.12.3180-3184.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vennema H., Poland A., Foley J., et al. Feline infectious peritonitis viruses arise by mutation from endemic feline enteric coronaviruses. Virology. 1998;243(1):150–157. doi: 10.1006/viro.1998.9045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pedersen N.C., Floyd K. Experimental studies with three new strains of feline infectious peritonitis virus FIPV-UCD2, FIPV-UCD3, and FIPV-UCD4. Compendium Continuing Education Practicing Veterinarians. 1985;7:1001–1011. [Google Scholar]
- 48.Rottier P.J., Nakamura K., Schellen P., et al. Acquisition of macrophage tropism during the pathogenesis of feline infectious peritonitis is determined by mutations in the feline coronavirus spike protein. J Virol. 2005;79(22):14122–14130. doi: 10.1128/JVI.79.22.14122-14130.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tekes G., Hofmann-Lehmann R., Bank-Wolf B., et al. Chimeric feline coronaviruses that encode type II spike protein on type I genetic background display accelerated viral growth and altered receptor usage. J Virol. 2010;84(3):1326–1333. doi: 10.1128/JVI.01568-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dye C., Helps C.R., Siddell S.G. Evaluation of real-time RT-PCR for the quantification of FCoV shedding in the faeces of domestic cats. J Feline Med Surg. 2008;10(2):167–174. doi: 10.1016/j.jfms.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tekes G., Hofmann-Lehmann R., Stallkamp I., et al. Genome organization and reverse genetic analysis of a type I feline coronavirus. J Virol. 2008;82(4):1851–1859. doi: 10.1128/JVI.02339-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brown M.A., Troyer J.L., Pecon-Slattery J., et al. Genetics and pathogenesis of feline infectious peritonitis virus. Emerg Infect Dis. 2009;15(9):1445–1452. doi: 10.3201/eid1509.081573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Herrewegh A.A.P.M., Vennema H., Horzinek M.C., et al. The molecular genetics of feline coronaviruses: comparative sequence analysis of the ORF7a/7b transcription unit of different biotypes. Virology. 1995;212(2):622–631. doi: 10.1006/viro.1995.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vennema H., Heijnen L., Rottier P.J., et al. A novel glycoprotein of feline infectious peritonitis coronavirus contains a KDEL-like endoplasmic reticulum retention signal. J Virol. 1992;66(8):4951–4956. doi: 10.1128/jvi.66.8.4951-4956.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dye C., Siddell S.G. Genomic RNA sequence of Feline coronavirus strain FIPV WSU-79/1146. J Gen Virol. 2005;86(Pt 8):2249–2253. doi: 10.1099/vir.0.80985-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kennedy M., Boedeker N., Gibbs P., et al. Deletions in the 7a ORF of feline coronavirus associated with an epidemic of feline infectious peritonitis. Vet Microbiol. 2001;81(3):227–234. doi: 10.1016/S0378-1135(01)00354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kennedy M.A., Moore E., Wilkes R.P., et al. Analysis of genetic mutations in the 7a7b open reading frame of coronavirus of cheetahs (Acinonyx jubatus) Am J Vet Res. 2006;67(4):627–632. doi: 10.2460/ajvr.67.4.627. [DOI] [PubMed] [Google Scholar]
- 58.Lin C.N., Su B.L., Huang H.P., et al. Field strain feline coronaviruses with small deletions in ORF7b associated with both enteric infection and feline infectious peritonitis. J Feline Med Surg. 2009;11(6):413–419. doi: 10.1016/j.jfms.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pedersen N.C. A review of feline infectious peritonitis virus infection: 1963–2008. J Feline Med Surg. 2009;11(4):225–258. doi: 10.1016/j.jfms.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pedersen N.C. Serologic studies of naturally occurring feline infectious peritonitis. Am J Vet Res. 1976;37(12):1449–1453. [PubMed] [Google Scholar]
- 61.Cave T.A., Golder M.C., Simpson J., et al. Risk factors for feline coronavirus seropositivity in cats relinquished to a UK rescue charity. J Feline Med Surg. 2004;6(2):53–58. doi: 10.1016/j.jfms.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Addie D.D., Dennis J.M., Toth S., et al. Long-term impact on a closed household of pet cats of natural infection with feline coronavirus, feline leukaemia virus and feline immunodeficiency virus. Vet Rec. 2000;146(15):419–424. doi: 10.1136/vr.146.15.419. [DOI] [PubMed] [Google Scholar]
- 63.Pedersen N.C., Sato R., Foley J.E., et al. Common virus infections in cats, before and after being placed in shelters, with emphasis on feline enteric coronavirus. J Feline Med Surg. 2004;6(2):83–88. doi: 10.1016/j.jfms.2003.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Luria B.J., Levy J.K., Lappin M.R., et al. Prevalence of infectious diseases in feral cats in Northern Florida. J Feline Med Surg. 2004;6(5):287–296. doi: 10.1016/j.jfms.2003.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Addie D.D., Toth S., Murray G.D., et al. Risk of feline infectious peritonitis in cats naturally infected with feline coronavirus. Am J Vet Res. 1995;56(4):429–434. [PubMed] [Google Scholar]
- 66.Foley J.E., Poland A., Carlson J., et al. Risk factors for feline infectious peritonitis among cats in multiple-cat environments with endemic feline enteric coronavirus. J Am Vet Med Assoc. 1997;210(9):1313–1318. [PubMed] [Google Scholar]
- 67.Addie D.D., Jarrett O. A study of naturally occurring feline coronavirus infections in kittens. Vet Rec. 1992;130(7):133–137. doi: 10.1136/vr.130.7.133. [DOI] [PubMed] [Google Scholar]
- 68.Herrewegh A.A., Mahler M., Hedrich H.J., et al. Persistence and evolution of feline coronavirus in a closed cat-breeding colony. Virology. 1997;234(2):349–363. doi: 10.1006/viro.1997.8663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Spain C.V., Scarlett J.M., Houpt K.A. Long-term risks and benefits of early-age gonadectomy in cats. J Am Vet Med Assoc. 2004;224(3):372–379. doi: 10.2460/javma.2004.224.372. [DOI] [PubMed] [Google Scholar]
- 70.Hickman M.A., Morris J.G., Rogers Q.R. Elimination of feline coronavirus infection from a large experimental specific pathogen-free cat breeding colony by serologic testing and isolation. Feline practice. 1995;23(3):96–102. [Google Scholar]
- 71.Pesteanu-Somogyi L.D., Radzai C., Pressler B.M. Prevalence of feline infectious peritonitis in specific cat breeds. J Feline Med Surg. 2006;8(1):1–5. doi: 10.1016/j.jfms.2005.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tsai H.Y., Chueh L.L., Lin C.N., et al. Clinicopathological findings and disease staging of feline infectious peritonitis: 51 cases from 2003 to 2009 in Taiwan. J Feline Med Surg. 2011;13(2):74–80. doi: 10.1016/j.jfms.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Norris J.M., Bosward K.L., White J.D., et al. Clinicopathological findings associated with feline infectious peritonitis in Sydney, Australia: 42 cases (1990–2002) Aust Vet J. 2005;83(11):666–673. doi: 10.1111/j.1751-0813.2005.tb13044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bell E.T., Malik R., Norris J.M. The relationship between the feline coronavirus antibody titre and the age, breed, gender and health status of Australian cats. Aust Vet J. 2006;84(1-2):2–7. doi: 10.1111/j.1751-0813.2006.tb13114.x. [DOI] [PubMed] [Google Scholar]
- 75.Foley J.E., Pedersen N.C. The inheritance of susceptibility to feline infectious peritonitis in purebreed catteries. Vet Pract. 1996;24(1):14–22. [Google Scholar]
- 76.Hardy W.D., Jr. Immunopathology induced by the feline leukemia virus. Springer Semin Immunopathol. 1982;5(1):75–106. doi: 10.1007/BF00201958. [DOI] [PubMed] [Google Scholar]
- 77.Cotter S.M., Hardy W.D., Jr, Essex M. Association of feline leukemia virus with lymphosarcoma and other disorders in the cat. J Am Vet Med Assoc. 1975;166(5):449–454. [PubMed] [Google Scholar]
- 78.Addie D., Belak S., Boucraut-Baralon C., et al. Feline infectious peritonitis: ABCD guidelines on prevention and management. J Feline Med Surg. 2009;11(7):594–604. doi: 10.1016/j.jfms.2009.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hurley K.F. Feline Infectious Peritonitis/Feline Enteric Coronavirus (FIP/FECV) 2011. http://www.sheltermedicine.com/shelter-health-portal/information-sheets/feline-infectious-peritonitisfeline-enteric-coronavirus-fip Accessed May 8, 2001.
- 80.Potkay S., Bacher J.D., Pitts T.W. Feline infectious peritonitis in a closed breeding colony. Lab Anim Sci. 1974;24(2):279–289. [PubMed] [Google Scholar]
- 81.Mullin C.H. Feline Infectious Peritonitis. Infectious disease management in animal shelters. 2009;(20):319–330. [Google Scholar]
- 82.Hartmann K. Feline infectious peritonitis. Vet Clin North Am Small Anim Pract. 2005;35(1):39–79. doi: 10.1016/j.cvsm.2004.10.011. vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kipar A., May H., Menger S., et al. Morphologic features and development of granulomatous vasculitis in feline infectious peritonitis. Vet Pathol. 2005;42(3):321–330. doi: 10.1354/vp.42-3-321. [DOI] [PubMed] [Google Scholar]
- 84.Andrew S.E. Feline infectious peritonitis. Vet Clin North Am Small Anim Pract. 2000;30(5):987–1000. doi: 10.1016/S0195-5616(00)05002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hagan W.A., Bruner D.W., Timoney J.F. Comstock Publishing Assoc; Ithaca (NY): 1992. Hagan and Bruner's microbiology and infectious diseases of domestic animals. [Google Scholar]
- 86.Jacobse-Geels H.E., Daha M.R., Horzinek M.C. Antibody, immune complexes, and complement activity fluctuations in kittens with experimentally induced feline infectious peritonitis. Am J Vet Res. 1982;43(4):666–670. [PubMed] [Google Scholar]
- 87.Petersen N.C., Boyle J.F. Immunologic phenomena in the effusive form of feline infectious peritonitis. Am J Vet Res. 1980;41(6):868–876. [PubMed] [Google Scholar]
- 88.Paltrinieri S., Cammarata Parodi M., Cammarata G., et al. Type IV hypersensitivity in the pathogenesis of FIPV-induced lesions. Zentralbl Veterinarmed B. 1998;45(3):151–159. doi: 10.1111/j.1439-0450.1998.tb00778.x. [DOI] [PubMed] [Google Scholar]
- 89.Wills-Karp M. In: Fundamental immunology. 6th edition. Paul W.E., editor. Lippincott Williams & Wilkins; Philadelphia: 2008. Immunological mechanisms of allergic diseases; pp. 1375–1425. [Google Scholar]
- 90.Benacerraf B., Levine B.B. Immunological specificity of delayed and immediate hypersensitivity reactions. J Exp Med. 1962;115:1023–1036. doi: 10.1084/jem.115.5.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Takano T., Ohyama T., Kokumoto A., et al. Vascular endothelial growth factor (VEGF), produced by feline infectious peritonitis (FIP) virus-infected monocytes and macrophages, induces vascular permeability and effusion in cats with FIP. Virus Res. 2011;158(1-2):161–168. doi: 10.1016/j.virusres.2011.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pedersen N.C., Allen C.E., Lyons L.A. Pathogenesis of feline enteric coronavirus infection. J Feline Med Surg. 2008;10(6):529–541. doi: 10.1016/j.jfms.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Addie D.D., Jarrett O. Use of a reverse-transcriptase polymerase chain reaction for monitoring the shedding of feline coronavirus by healthy cats. Vet Rec. 2001;148(21):649–653. doi: 10.1136/vr.148.21.649. [DOI] [PubMed] [Google Scholar]
- 94.Addie D.D., Paltrinieri S., Pedersen N.C. Recommendations from workshops of the second international feline coronavirus/feline infectious peritonitis symposium. J Feline Med Surg. 2004;6(2):125–130. doi: 10.1016/j.jfms.2003.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Harpold L.M., Legendre A.M., Kennedy M.A., et al. Fecal shedding of feline coronavirus in adult cats and kittens in an Abyssinian cattery. J Am Vet Med Assoc. 1999;215(7):948–951. [PubMed] [Google Scholar]
- 96.Addie D.D., Schaap I.A., Nicolson L., et al. Persistence and transmission of natural type I feline coronavirus infection. J Gen Virol. 2003;84(Pt 10):2735–2744. doi: 10.1099/vir.0.19129-0. [DOI] [PubMed] [Google Scholar]
- 97.Kipar A., Meli M.L., Baptiste K.E., et al. Sites of feline coronavirus persistence in healthy cats. J Gen Virol. 2010;91(Pt 7):1698–1707. doi: 10.1099/vir.0.020214-0. [DOI] [PubMed] [Google Scholar]
- 98.Addie D.D., Jarrett O. Feline coronavirus antibodies in cats. Vet Rec. 1992;131(9):202–203. doi: 10.1136/vr.131.9.202-a. [DOI] [PubMed] [Google Scholar]
- 99.Gonon V., Duquesne V., Klonjkowski B., et al. Clearance of infection in cats naturally infected with feline coronaviruses is associated with an anti-S glycoprotein antibody response. J Gen Virol. 1999;80(Pt 9):2315–2317. doi: 10.1099/0022-1317-80-9-2315. [DOI] [PubMed] [Google Scholar]
- 100.de Groot-Mijnes J.D., van Dun J.M., van der Most R.G., et al. Natural history of a recurrent feline coronavirus infection and the role of cellular immunity in survival and disease. J Virol. 2005;79(2):1036–1044. doi: 10.1128/JVI.79.2.1036-1044.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hohdatsu T., Yamada H., Ishizuka Y., et al. Enhancement and neutralization of feline infectious peritonitis virus infection in feline macrophages by neutralizing monoclonal antibodies recognizing different epitopes. Microbiol Immunol. 1993;37(6):499–504. doi: 10.1111/j.1348-0421.1993.tb03242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dewerchin H.L., Cornelissen E., Nauwynck H.J. Replication of feline coronaviruses in peripheral blood monocytes. Arch Virol. 2005;150(12):2483–2500. doi: 10.1007/s00705-005-0598-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Samuel C.E. Antiviral actions of interferons. Clin Microbiol Rev. 2001;14(4):778–809. doi: 10.1128/CMR.14.4.778-809.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kawai T., Akira S. Innate immune recognition of viral infection. Nat Immunol. 2006;7(2):131–137. doi: 10.1038/ni1303. [DOI] [PubMed] [Google Scholar]
- 105.Pichlmair A., Reis e Sousa C. Innate recognition of viruses. Immunity. 2007;27(3):370–383. doi: 10.1016/j.immuni.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 106.Spiegel M., Pichlmair A., Martinez-Sobrido L., et al. Inhibition of Beta interferon induction by severe acute respiratory syndrome coronavirus suggests a two-step model for activation of interferon regulatory factor 3. J Virol. 2005;79(4):2079–2086. doi: 10.1128/JVI.79.4.2079-2086.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Versteeg G.A., Bredenbeek P.J., van den Worm S.H., et al. Group 2 coronaviruses prevent immediate early interferon induction by protection of viral RNA from host cell recognition. Virology. 2007;361(1):18–26. doi: 10.1016/j.virol.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kiss I., Poland A.M., Pedersen N.C. Disease outcome and cytokine responses in cats immunized with an avirulent feline infectious peritonitis virus (FIPV)-UCD1 and challenge-exposed with virulent FIPV-UCD8. J Feline Med Surg. 2004;6(2):89–97. doi: 10.1016/j.jfms.2003.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Takano T., Hohdatsu T., Hashida Y., et al. A “possible” involvement of TNF-alpha in apoptosis induction in peripheral blood lymphocytes of cats with feline infectious peritonitis. Vet Microbiol. 2007;119(2-4):121–131. doi: 10.1016/j.vetmic.2006.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Weiss R.C., Scott F.W. Antibody-mediated enhancement of disease in feline infectious peritonitis: comparisons with dengue hemorrhagic fever. Comp Immunol Microbiol Infect Dis. 1981;4(2):175–189. doi: 10.1016/0147-9571(81)90003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Olsen C.W., Corapi W.V., Ngichabe C.K., et al. Monoclonal antibodies to the spike protein of feline infectious peritonitis virus mediate antibody-dependent enhancement of infection of feline macrophages. J Virol. 1992;66(2):956–965. doi: 10.1128/jvi.66.2.956-965.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Takano T., Azuma N., Hashida Y., et al. B-cell activation in cats with feline infectious peritonitis (FIP) by FIP-virus-induced B-cell differentiation/survival factors. Arch Virol. 2009;154(1):27–35. doi: 10.1007/s00705-008-0265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Huisman W., Martina B.E., Rimmelzwaan G.F., et al. Vaccine-induced enhancement of viral infections. Vaccine. 2009;27(4):505–512. doi: 10.1016/j.vaccine.2008.10.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Seo S.H., Wang L., Smith R., et al. The carboxyl-terminal 120-residue polypeptide of infectious bronchitis virus nucleocapsid induces cytotoxic T lymphocytes and protects chickens from acute infection. J Virol. 1997;71(10):7889–7894. doi: 10.1128/jvi.71.10.7889-7894.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Seo S.H., Collisson E.W. Specific cytotoxic T lymphocytes are involved in in vivo clearance of infectious bronchitis virus. J Virol. 1997;71(7):5173–5177. doi: 10.1128/jvi.71.7.5173-5177.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pedersen N.C., Theilen G., Keane M.A., et al. Studies of naturally transmitted feline leukemia virus infection. Am J Vet Res. 1977;38(10):1523–1531. [PubMed] [Google Scholar]
- 117.Cotter S.M., Gilmore C.E., Rollins C. Multiple cases of feline leukemia and feline infectious peritonitis in a household. J Am Vet Med Assoc. 1973;162(12):1054–1058. [PubMed] [Google Scholar]
- 118.Haagmans B.L., Egberink H.F., Horzinek M.C. Apoptosis and T-cell depletion during feline infectious peritonitis. J Virol. 1996;70(12):8977–8983. doi: 10.1128/jvi.70.12.8977-8983.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kipar A., Kohler K., Leukert W., et al. A comparison of lymphatic tissues from cats with spontaneous feline infectious peritonitis (FIP), cats with FIP virus infection but no FIP, and cats with no infection. J Comp Pathol. 2001;125(2-3):182–191. doi: 10.1053/jcpa.2001.0501. [DOI] [PubMed] [Google Scholar]
- 120.Munder M., Mallo M., Eichmann K., et al. Murine macrophages secrete interferon gamma upon combined stimulation with interleukin (IL)-12 and IL-18: A novel pathway of autocrine macrophage activation. J Exp Med. 1998;187(12):2103–2108. doi: 10.1084/jem.187.12.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Frucht D.M., Fukao T., Bogdan C., et al. IFN-gamma production by antigen-presenting cells: mechanisms emerge. Trends Immunol. 2001;22(10):556–560. doi: 10.1016/s1471-4906(01)02005-1. [DOI] [PubMed] [Google Scholar]
- 122.Gessani S., Belardelli F. IFN-gamma expression in macrophages and its possible biological significance. Cytokine Growth Factor Rev. 1998;9(2):117–123. doi: 10.1016/s1359-6101(98)00007-0. [DOI] [PubMed] [Google Scholar]
- 123.Sen E., Chattopadhyay S., Bandopadhyay S., et al. Macrophage heterogeneity, antigen presentation, and membrane fluidity: implications in visceral Leishmaniasis. Scand J Immunol. 2001;53(2):111–120. doi: 10.1046/j.1365-3083.2001.00856.x. [DOI] [PubMed] [Google Scholar]
- 124.Salazar-Mather T.P., Hamilton T.A., Biron C.A. A chemokine-to-cytokine-to-chemokine cascade critical in antiviral defense. J Clin Invest. 2000;105(7):985–993. doi: 10.1172/JCI9232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Pien G.C., Satoskar A.R., Takeda K., et al. Cutting edge: selective IL-18 requirements for induction of compartmental IFN-gamma responses during viral infection. J Immunol. 2000;165(9):4787–4791. doi: 10.4049/jimmunol.165.9.4787. [DOI] [PubMed] [Google Scholar]
- 126.Krukowski K., Eddy J., Kosik K.L., et al. Glucocorticoid dysregulation of natural killer cell function through epigenetic modification. Brain Behav Immun. 2011;25(2):239–249. doi: 10.1016/j.bbi.2010.07.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Giordano A., Paltrinieri S. Interferon-gamma in the serum and effusions of cats with feline coronavirus infection. Vet J. 2009;180(3):396–398. doi: 10.1016/j.tvjl.2008.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Takano T., Hohdatsu T., Toda A., et al. TNF-alpha, produced by feline infectious peritonitis virus (FIPV)-infected macrophages, upregulates expression of type II FIPV receptor feline aminopeptidase N in feline macrophages. Virology. 2007;364(1):64–72. doi: 10.1016/j.virol.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Han S., Choi H., Ko M.G., et al. Peripheral T cells become sensitive to glucocorticoid- and stress-induced apoptosis in transgenic mice overexpressing SRG3. J Immunol. 2001;167(2):805–810. doi: 10.4049/jimmunol.167.2.805. [DOI] [PubMed] [Google Scholar]
- 130.Dhabhar F.S. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16(5):300–317. doi: 10.1159/000216188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Addie D.D. In: Greene C.E., editor. vol 3rd. Saunders Elsevier; St. Louis: 2006. Feline coronavirus infection; pp. 88–102. (Infectious diseases of the dog and cat). [Google Scholar]
- 132.Doherty M.J. Ocular manifestations of feline infectious peritonitis. J Am Vet Med Assoc. 1971;159(4):417–424. [PubMed] [Google Scholar]
- 133.Boettcher I.C., Steinberg T., Matiasek K., et al. Use of anti-coronavirus antibody testing of cerebrospinal fluid for diagnosis of feline infectious peritonitis involving the central nervous system in cats. J Am Vet Med Assoc. 2007;230(2):199–205. doi: 10.2460/javma.230.2.199. [DOI] [PubMed] [Google Scholar]
- 134.Marioni-Henry K., Vite C.H., Newton A.L., et al. Prevalence of diseases of the spinal cord of cats. J Vet Intern Med. 2004;18(6):851–858. doi: 10.1892/0891-6640(2004)18<851:podots>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 135.Timmann D., Cizinauskas S., Tomek A., et al. Retrospective analysis of seizures associated with feline infectious peritonitis in cats. J Feline Med Surg. 2008;10(1):9–15. doi: 10.1016/j.jfms.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Foley J.E., Lapointe J.M., Koblik P., et al. Diagnostic features of clinical neurologic feline infectious peritonitis. J Vet Intern Med. 1998;12(6):415–423. doi: 10.1111/j.1939-1676.1998.tb02144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Diaz J.V., Poma R. Diagnosis and clinical signs of feline infectious peritonitis in the central nervous system. Can Vet J. 2009;50(10):1091–1093. [PMC free article] [PubMed] [Google Scholar]
- 138.Sparkes A.H., Gruffydd-Jones T., Harbour D.A. Feline infectious peritonitis: a review of clinico-pathological changes in 65 cases, and critical assessment of their diagnostic value. Vet Rec. 1991;129:209–212. doi: 10.1136/vr.129.10.209. [DOI] [PubMed] [Google Scholar]
- 139.Sparkes A.H., Gruffydd-Jones T.J., Harbour D.A. An appraisal of the value of laboratory tests in the diagnosis of feline infectious peritonitis. J Am Anim Hosp Assoc. 1994;30:345–350. [Google Scholar]
- 140.Norsworthy G.D. In: Norsworthy G.D., Crystal M.A., Grace S.F., et al., editors. vol 3rd. Wiley-Blackwell Publishing; Iowa: 2006. Feline infectious peritonitis; pp. 97–98. (The feline patient). [Google Scholar]
- 141.Goodson T., Randell S., Moore L. Feline infectious peritonitis. Compend Contin Educ Vet. 2009;31(10):E1–E9. [PubMed] [Google Scholar]
- 142.Paltrinieri S., Parodi M.C., Cammarata G. In vivo diagnosis of feline infectious peritonitis by comparison of protein content, cytology, and direct immunofluorescence test on peritoneal and pleural effusions. J Vet Diagn Invest. 1999;11(4):358–361. doi: 10.1177/104063879901100411. [DOI] [PubMed] [Google Scholar]
- 143.Hartmann K., Binder C., Hirschberger J., et al. Comparison of different tests to diagnose feline infectious peritonitis. J Vet Intern Med. 2003;17(6):781–790. doi: 10.1111/j.1939-1676.2003.tb02515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Giori L., Giordano A., Giudice C., et al. Performances of different diagnostic tests for feline infectious peritonitis in challenging clinical cases. J Small Anim Pract. 2011;52(3):152–157. doi: 10.1111/j.1748-5827.2011.01042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Paltrinieri S., Giordano A., Tranquillo V., et al. Critical assessment of the diagnostic value of feline alpha1-acid glycoprotein for feline infectious peritonitis using the likelihood ratios approach. J Vet Diagn Invest. 2007;19(3):266–272. doi: 10.1177/104063870701900306. [DOI] [PubMed] [Google Scholar]
- 146.Shelly S.M., Scarlett-Kranz J., Blue J.T. Protein electrophoresis on effusions from cats as a diagnostic test for feline infectious peritonitis. Journal of the American Animal Hospital Association. 1988;24:495–500. [Google Scholar]
- 147.Addie D.D. The Rivalta Test in diagnosis of effusive Feline Infectious Peritonitis (FIP) 2010. http://www.youtube.com/user/DrDianeDAddie#p/u/4/XmOk2veunqA [Online video] Accessed May 12th, 2011.
- 148.Pedersen N. The history and interpretation of feline coronavirus serology. Feline Practice. 1995;23:46–51. [Google Scholar]
- 149.Richards J.R. Problems in the interpretation of feline coronavirus serology (specificity vs. sensitivity of test procedures) Feline Practice. 1995;23:52–55. [Google Scholar]
- 150.Soma T., Ishii H. Detection of feline coronavirus antibody, feline immunodeficiency virus antibody, and feline leukemia virus antigen in ascites from cats with effusive feline infectious peritonitis. J Vet Med Sci. 2004;66(1):89–90. doi: 10.1292/jvms.66.89. [DOI] [PubMed] [Google Scholar]
- 151.Kennedy M.A., Brenneman K., Millsaps R.K., et al. Correlation of genomic detection of feline coronavirus with various diagnostic assays for feline infectious peritonitis. J Vet Diagn Invest. 1998;10(1):93–97. doi: 10.1177/104063879801000119. [DOI] [PubMed] [Google Scholar]
- 152.Lappin M.R., Turnwald G.H. In: Small animal clinical diagnosis by laboratory methods. 4th edition. Willard M.D., Tvedten H., editors. Elsevier; St. Louis: 2004. Microbiology and infectious diseases; pp. 350–351. [Google Scholar]
- 153.Vennema H., Rossen J.W., Wesseling J., et al. Genomic organization and expression of the 3' end of the canine and feline enteric coronaviruses. Virology. 1992;191(1):134–140. doi: 10.1016/0042-6822(92)90174-N. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kennedy M.A., Abd-Eldaim M., Zika S.E., et al. Evaluation of antibodies against feline coronavirus 7b protein for diagnosis of feline infectious peritonitis in cats. Am J Vet Res. 2008;69(9):1179–1182. doi: 10.2460/ajvr.69.9.1179. [DOI] [PubMed] [Google Scholar]
- 155.Pratelli A. Comparison of serologic techniques for the detection of antibodies against feline coronaviruses. J Vet Diagn Invest. 2008;20(1):45–50. doi: 10.1177/104063870802000108. [DOI] [PubMed] [Google Scholar]
- 156.Barlough J.E., Jacobson R.H., Sorresso G.P., et al. Coronavirus antibody detection in cats by computer-assisted kinetics-based enzyme-linked immunosorbent assay (KELA): field studies. Cornell Vet. 1986;76(3):227–235. [PubMed] [Google Scholar]
- 157.Shiba N., Maeda K., Kato H., et al. Differentiation of feline coronavirus type I and II infections by virus neutralization test. Vet Microbiol. 2007;124(3-4):348–352. doi: 10.1016/j.vetmic.2007.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Addie D. Feline Coronavirus (Feline Infectious Peritonitis) Antibody tests. 2009. http://www.dr-addie.com/FCoVantibody.htm Accessed 4/26/2011, 2011.
- 159.Peterson M.E., Kintzer P.P., Hurvitz A.I. Methimazole treatment of 262 cats with hyperthyroidism. J Vet Intern Med. 1988;2(3):150–157. doi: 10.1111/j.1939-1676.1988.tb02812.x. [DOI] [PubMed] [Google Scholar]
- 160.Breitschwerdt E.B., Abrams-Ogg A.C., Lappin M.R., et al. Molecular evidence supporting Ehrlichia canis-like infection in cats. J Vet Intern Med. 2002;16(6):642–649. doi: 10.1111/j.1939-1676.2002.tb02402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Gunn-Moore D.A., Gruffydd-Jones T.J., Harbour D.A. Detection of feline coronaviruses by culture and reverse transcriptase-polymerase chain reaction of blood samples from healthy cats and cats with clinical feline infectious peritonitis. Vet Microbiol. 1998;62(3):193–205. doi: 10.1016/S0378-1135(98)00210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gamble D.A., Lobbiani A., Gramegna M., et al. Development of a nested PCR assay for detection of feline infectious peritonitis virus in clinical specimens. J Clin Microbiol. 1997;35(3):673–675. doi: 10.1128/jcm.35.3.673-675.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Herrewegh A.A., de Groot R.J., Cepica A., et al. Detection of feline coronavirus RNA in feces, tissues, and body fluids of naturally infected cats by reverse transcriptase PCR. J Clin Microbiol. 1995;33(3):684–689. doi: 10.1128/jcm.33.3.684-689.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Takano T., Tomiyama Y., Katoh Y., et al. Mutation of neutralizing/antibody-dependent enhancing epitope on spike protein and 7b gene of feline infectious peritonitis virus: influences of viral replication in monocytes/macrophages and virulence in cats. Virus Res. 2011;156(1-2):72–80. doi: 10.1016/j.virusres.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Pedersen N., Liu H., Dodd K., et al. Significance of Coronavirus Mutants in Feces and Diseased Tissues of Cats Suffering from Feline Infectious Peritonitis. Viruses. 2009;1(2):166–184. doi: 10.3390/v1020166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Li X., Scott F.W. Detection of feline coronaviruses in cell cultures and in fresh and fixed feline tissues using polymerase chain reaction. Vet Microbiol. 1994;42(1):65–77. doi: 10.1016/0378-1135(94)90078-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Simons F.A., Vennema H., Rofina J.E., et al. A mRNA PCR for the diagnosis of feline infectious peritonitis. J Virol Methods. 2005;124(1-2):111–116. doi: 10.1016/j.jviromet.2004.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Can-Sahna K., Soydal Ataseven V., Pinar D., et al. The detection of feline coronaviruses in blood samples from cats by mRNA RT-PCR. J Feline Med Surg. 2007;9(5):369–372. doi: 10.1016/j.jfms.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sharif S., Arshad S.S., Hair-Bejo M., et al. Evaluation of Feline Coronavirus Viraemia in Clinically Healthy and Ill Cats with Feline Infectious Peritonitis. Journal of Animal and Veterinary Advances. 2011;10(1):18–22. [Google Scholar]
- 170.Simons F.A., Vennema H., Rofina J.E., et al. A mRNA PCR for the diagnosis of feline infectious peritonitis. J Virol Methods. 2005;124(1-2):111–116. doi: 10.1016/j.jviromet.2004.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Foley J.E., Leutenegger C. A review of coronavirus infection in the central nervous system of cats and mice. J Vet Intern Med. 2001;15(5):438–444. doi: 10.1111/j.1939-1676.2001.tb01572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Cannon M.J., Silkstone M.A., Kipar A.M. Cutaneous lesions associated with coronavirus-induced vasculitis in a cat with feline infectious peritonitis and concurrent feline immunodeficiency virus infection. J Feline Med Surg. 2005;7(4):233–236. doi: 10.1016/j.jfms.2004.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Declercq J., De Bosschere H., Schwarzkopf I., et al. Papular cutaneous lesions in a cat associated with feline infectious peritonitis. Vet Dermatol. 2008;19(5):255–258. doi: 10.1111/j.1365-3164.2008.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ritz S., Egberink H., Hartmann K. Effect of feline interferon-omega on the survival time and quality of life of cats with feline infectious peritonitis. J Vet Intern Med. 2007;21(6):1193–1197. doi: 10.1111/j.1939-1676.2007.tb01937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ishida T., Shibanai A., Tanaka S., et al. Use of recombinant feline interferon and glucocorticoid in the treatment of feline infectious peritonitis. J Feline Med Surg. 2004;6(2):107–109. doi: 10.1016/j.jfms.2003.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Hartmann K. In: Ettinger S.J., Feldman E.C., editors. vol 1. Saunders Elsevier; St. Louis: 2010. Feline infectious peritonitis and feline coronavirus infection; pp. 940–945. (Textbook of veterinary internal medicine: diseases of the dog and the cat). [Google Scholar]
- 177.Legendre A.M., Bartges J.W. Effect of Polyprenyl Immunostimulant on the survival times of three cats with the dry form of feline infectious peritonitis. J Feline Med Surg. 2009;11(8):624–626. doi: 10.1016/j.jfms.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hoskins J., Taylor H., Lomax T. Independent evaluation of a modified live feline infectious peritonitis virus vaccine under experimental conditions (Louisiana experience) Feline Practice. 1995;23(3):72–73. [Google Scholar]
- 179.McArdle F., Bennett M., Gaskell R.M., et al. Independent evaluation of a modified live FIPV vaccine under experimental conditions (University of Liverpool experience) Feline Practice. 1995;23(3):67–71. [Google Scholar]
- 180.Scott F., Corapi W., Olsen C. Independent evaluation of a modified live FIPV vaccine under experimental conditions (Cornell experience) Feline Practice. 1995;23(3):74–76. [Google Scholar]
- 181.Gerber J. Overview of the development of a modified live temperature-sensitive FIP virus vaccine. Feline Practice. 1995;23(3):62–66. [Google Scholar]
- 182.Richards J.R., Elston T.H., Ford R.B., et al. The 2006 American Association of Feline Practitioners Feline Vaccine Advisory Panel report. J Am Vet Med Assoc. 2006;229(9):1405–1441. doi: 10.2460/javma.229.9.1405. [DOI] [PubMed] [Google Scholar]
- 183.Day M.J., Horzinek M.C., Schultz R.D. WSAVA guidelines for the vaccination of dogs and cats. J Small Anim Pract. 2010;51(6):1–32. doi: 10.1111/j.1748-5827.2010.00959a.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Peterson C.A., Dvorak G., Spickler A.R. 1st edition. Iowa State University, Center for Food Security and Public Health; Ames (IA): 2008. Maddie's infection control manual for animal shelters for veterinary personnel. [Google Scholar]
- 185.Bell E.T., Toribio J.A., White J.D., et al. Seroprevalence study of feline coronavirus in owned and feral cats in Sydney, Australia. Aust Vet J. 2006;84(3):74–81. doi: 10.1111/j.1751-0813.2006.tb12231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Holst B.S., Englund L., Palacios S., et al. Prevalence of antibodies against feline coronavirus and Chlamydophila felis in Swedish cats. J Feline Med Surg. 2006;8(3):207–211. doi: 10.1016/j.jfms.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Pratelli A., Yesilbag K., Siniscalchi M., et al. Prevalence of feline coronavirus antibodies in cats in Bursa province, Turkey, by an enzyme-linked immunosorbent assay. J Feline Med Surg. 2009;11(10):881–884. doi: 10.1016/j.jfms.2009.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Sparkes A.H., Gruffydd-Jones T.J., Harbour D.A. Feline coronavirus antibodies in UK cats. Vet Rec. 1992;131(10):223–224. doi: 10.1136/vr.131.10.223-a. [DOI] [PubMed] [Google Scholar]
- 189.Muirden A. Prevalence of feline leukaemia virus and antibodies to feline immunodeficiency virus and feline coronavirus in stray cats sent to an RSPCA hospital. Vet Rec. 2002;150(20):621–625. doi: 10.1136/vr.150.20.621. [DOI] [PubMed] [Google Scholar]
- 190.Sharif S., Arshad S.S., Hair-Bejo M., et al. Prevalence of feline coronavirus in two cat populations in Malaysia. J Feline Med Surg. 2009;11(12):1031–1034. doi: 10.1016/j.jfms.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kiss I., Kecskemeti S., Tanyi J., et al. Prevalence and genetic pattern of feline coronaviruses in urban cat populations. Vet J. 2000;159(1):64–70. doi: 10.1053/tvjl.1999.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Duthie S., Eckersall P.D., Addie D.D., et al. Value of alpha 1-acid glycoprotein in the diagnosis of feline infectious peritonitis. Vet Rec. 1997;141(12):299–303. doi: 10.1136/vr.141.12.299. [DOI] [PubMed] [Google Scholar]
- 193.Hirschberger J., Hartmann K., Wilhelm N., et al. [Clinical symptoms and diagnosis of feline infectious peritonitis] Tierarztl Prax. 1995;23(1):92–99. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.