Abstract
Objective:
To assess the interaction of chronotype with anxiety in patients with chronic primary insomnia.
Methods:
Sixty-four patients (50 women) with mean age 43.9±8.1 years were investigated with the Horne and Östberg Morningness-Eveningness Questionnaire (MEQ) and State-Trait Anxiety Inventory (STAI).
Results:
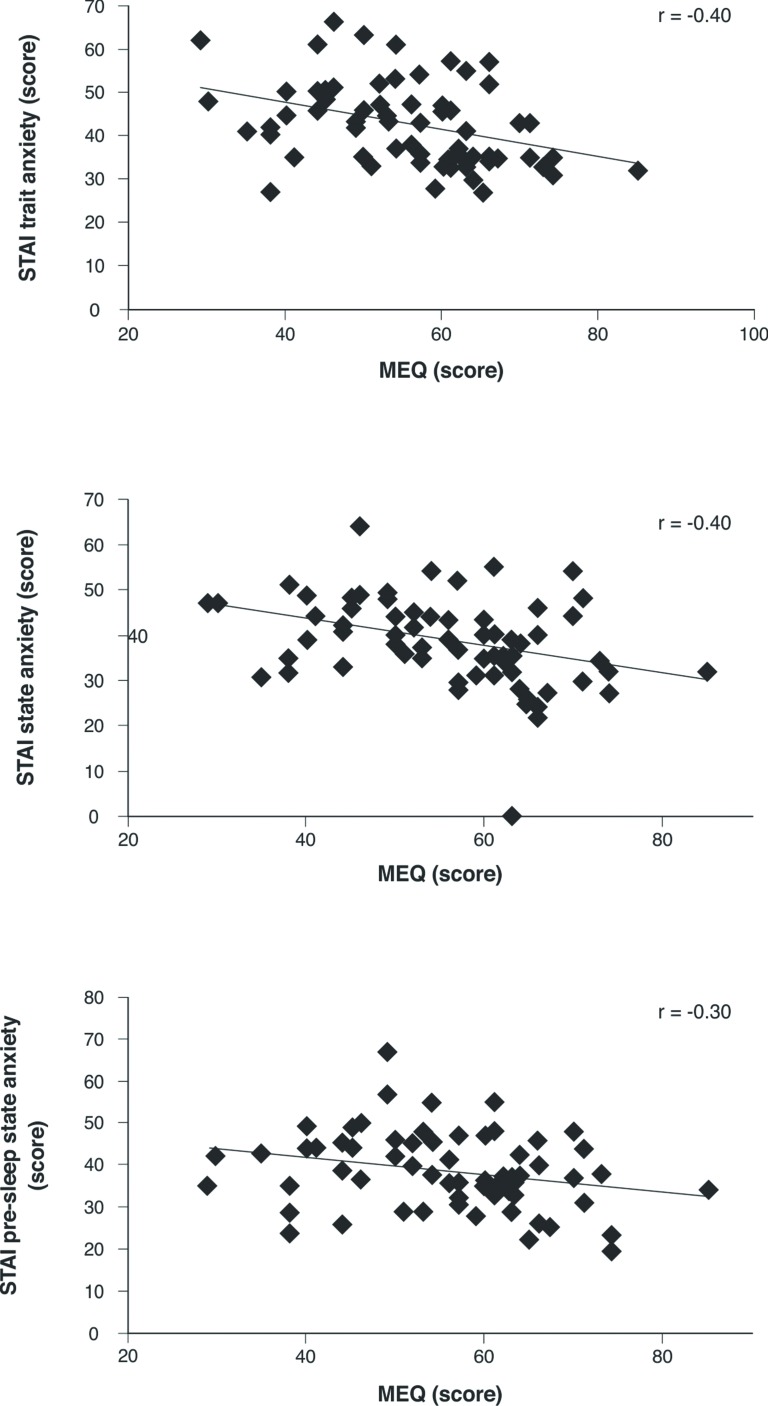
Significant negative correlations of chronotype-MEQ score with STAI state-anxiety (r = -0.40, p < 0.05), STAI trait-anxiety (r = -0.40, p < 0.05), and STAI pre-sleep state anxiety (r = -0.30, p < 0.05) were observed. Eveningness preference was associated with higher trait, state, and pre-sleep state anxiety.
Conclusions:
These results suggest that chronotype may be an important parameter to identifying the origin and significance of a vicious anxiety-insomnia-depression cycle in patients with chronic primary insomnia.
Keywords: Chronotype, insomnia, anxiety, eveningness, State-Trait Anxiety Inventory
Introduction
Chronic primary insomnia is a sleep disorder characterized by long-term difficulty initiating and maintaining sleep, early waking or non-restorative sleep, and daytime impairment (including fatigue, mood disorders, impaired concentration, and poor quality of life).1,2
Some evidence suggests that circadian rhythm factors may be involved in the development of psychophysiological insomnia,3 defined as a form of primary insomnia that is associated with physiological/psychological hyperarousal and a negative conditioning to sleep, resulting in pre-sleep anxiety.4
Chronotype has also been associated with higher risk of mood disorders; evening types are more likely to report severe depressive symptoms compared to morning or intermediate types.5 Chronotype-dependent individual differences in both circadian clock and homeostatic sleep drive can be observed. Eveningness has been associated with negative consequences on sleep, including insomnia.6 Consistent with the foregoing, evening-type insomniacs have been found to report greater depressive symptoms than morning or intermediate types.7
In addition, a recent study8 assessing diurnal variation in brain activity among insomnia patients suggested that positive affect-related neural structures may underlie differences in the phase and amplitude of self-reported positive affect between morning and evening types.
It seems clear that eveningness is associated with mood disorders, including depression. However, there is no published evidence to support other impairments of evening-type insomnia on other domains of mood, such as anxiety.
Anxiety can be defined as a disorder in its own right or as a symptom associated with other disorders (e.g., insomnia).9 We hypothesized that evening chronotypes would exhibit higher rates of anxiety complaints than subjects of other chronotypes. Thus, the aim of this study was to assess the interaction of chronotype with anxiety in patients with chronic primary insomnia.
Methods
Study participants
Sixty-four patients with a recent diagnosis of chronic primary insomnia (DSM-IV)2 were recruited from a sleep clinic in São Paulo, Brazil. The inclusion criteria were as follows: 1) age 30-60 years; 2) having complaints of insomnia lasting longer than 6 months; 3) no evidence insomnia was directly related to medical conditions or to side effects of medications; 4) not using medications (including psychopharmaceuticals) for insomnia or other psychiatric disorders; 5) no diagnosis of depression; 6) apnea-hypopnea index (AHI) < 15, evaluated by polysomnography; and 7) periodic leg movement index (PLMI) < 15, evaluated by polysomnography. Shift workers or those working a night shift were excluded. Approval for the study was obtained from the local Ethics Committee (protocol no. 1404/05), and all participants signed an informed consent form.
One hundred fifty-six subjects were evaluated between March 2007 and June 2010; of these, 64 (50 women) participated of the present study. Twenty-three were excluded due to high scores (> 20) on the Beck Depression Inventory, 22 for other major psychiatric disorders (such as severe anxiety disorders), 14 for shift work, and 33 for pharmacologic treatment.
Study design
Data were collected using self-administered questionnaires at two time points. First, participants answered the Horne and Östberg Morningness-Eveningness Questionnaire (MEQ) and State-Trait Anxiety Inventory (STAI) between 8 a.m. and 10 a.m.; then, they were instructed to answer the pre-sleep STAI state questionnaire at night, before sleep.
Instruments
Horne and Östberg Morningness-Eveningness Questionnaire
This scale, developed in 1976, evaluates chronotypes on a single scale from 16 to 86. Higher scores (≥ 59) suggest greater morningness preference, while lower scores (≤ 41) indicate greater eveningness.10,11
State-Trait Anxiety Inventory
The STAI scales encompass 20 items and provide a one-dimensional measurement of trait and state anxiety.12,13 Volunteers were instructed to complete the instrument in the morning and retake the state anxiety scale 30 minutes before going to sleep. The range of scores for each subtest is 20-80, with higher scores indicating greater anxiety.
Statistical analyses
Statistical analyses were performed using Statistic 7.0 software (Statsoft, Tulsa, OK, USA). Kolmogorov-Smirnov’s normality tests were performed for all variables. Spearman’s correlation test was used to assess the interaction of chronotype with anxiety. The subjects’ characteristics are presented as means and standard deviations (SD). The significance level for the analyses was p < 0.05.
Results
The characteristics of the sample are presented in Table 1. Regarding chronotype, 42% of participants were classified as morning types, 44% as intermediate types, and 14% as evening types.
Table 1. Physical, clinical, and behavioral characteristics of patients with chronic primary insomnia.
| Variable | Female (n=50) | Male (n=14) | Total (n=64) |
|---|---|---|---|
| Age (years) | 43.3±7.9 | 46.0±8.6 | 43.9±8.1 |
| Duration of insomnia (years) | 7.7±7.6 | 7.6±7.3 | 7.6±7.5 |
| MEQ questionnaire (score) | 55.9±11.9 | 54.6±10.5 | 55.7±11.6 |
| STAI | |||
| Trait (score) | 41.6±9.2 | 47.1±9.9 | 42.8±9.6 |
| State (score) | 39.9±8.9 | 37.5±7.1 | 39.4±8.6 |
| State, pre-sleep (score) | 38.6±9.7 | 38.8±8.2 | 38.6±9.3 |
Data presented as mean ± standard deviation.
MEQ = Horne and Östberg Morningness-Eveningness Questionnaire; STAI = State-Trait Anxiety Inventory.
Significant negative correlations of MEQ chronotype score with trait anxiety (r = -0.40, p < 0.05), state anxiety, and pre-sleep state-anxiety (r = -0.30, p < 0.05) were observed (Figure 1).
Figure 1. Correlation of MEQ score with STAI trait anxiety, STAI state anxiety, and STAI pre-sleep state anxiety in patients with chronic primary insomnia. MEQ = Horne and Östberg Morningness-Eveningness Questionnaire; STAI = State-Trait Anxiety Inventory.
Discussion
In the present study, the evening chronotype was associated with higher trait, state, and pre-sleep state anxiety. In general, anxiety and cognitive impairments are among the most common symptoms of chronic primary insomnia.1 According to our results, we can hypothesize that these symptoms may be more evident in evening types.
Among other mood disorders, some studies have identified an association between evening typology and depressive symptoms in healthy subjects5 and patients with major depressive disorder.14 In our sample of patients with chronic primary insomnia, we also found an association of evening chronotype with anxiety.
Ong et al.6 assessed diurnal variation in brain activity of insomnia patients via fluorodeoxyglucose-positron emission tomography (FDG-PET) analysis of the relative regional cerebral metabolic rate of glucose uptake during morning and evening wakefulness. The authors suggest that alterations in the diurnal activity of positive affect-related neural structures may underlie differences in the phase and amplitude of self-reported positive affect between morning and evening types, and may constitute one mechanism for increased risk of mood disorders among evening-type insomniacs.
In addition, Hidalgo et al.5 suggest that chronotype is a biological characteristic that itself constitutes a trait or behavioral symptom related to affective disorders. The findings of our study confirm this hypothesis in patients with chronic primary insomnia, and thus provides important evidence considering the established vicious cycle of anxiety-insomnia-depression.4
The limitations of this study are inherent to self-reported data. However, the questionnaires used in this study are reliable instruments. Although the initial sample was large, the number of participants was reduced substantially after initial screening. However, our strict inclusion criteria were important to ensure sample homogeneity and exclude the possibility of chronotype alterations due to medication use, psychiatric conditions, or shift work.
In conclusion, eveningness preference was associated with higher trait, state, and pre-sleep state anxiety in our sample. These results suggest that chronotype may be an important marker of the origin and significance of the vicious cycle in chronic primary insomnia.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
This study received financial support from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; protocol no. 98/14303-3; 2008/02862-1), Associação Fundo de Incentivo à Pesquisa (AFIP), and Centro de Estudos em Psicobiologia e Exercício (CEPE). The authors are grateful to all the patients who volunteered their time to participate in the study.
References
- 1.American Academy of Sleep Medicine (AASM). The international classification of sleep disorders: diagnostic and coding manual. Westchester: Diagnostic Classification Steering Committee; 2005. [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Arlington: American Psychiatric Publishing; 1994. [Google Scholar]
- 3.Lack LC, Bootzin RR. Circadian rhythm factors in insomnia and their treatment. In: Perlis ML, Lichstein KL, editors. Treating sleep disorders: principles and practice of behavioral sleep medicine. Hoboken: John Wiley & Sons; 2003. [Google Scholar]
- 4.American Academy of Sleep Medicine (AASM). International Classification of Sleep Disorders. 3rd ed. Darien: AASM; 2014. [Google Scholar]
- 5.Hidalgo MP, Caumo W, Posser M, Coccaro SB, Camozzato AL, Chaves ML. Relationship between depressive mood and chronotype in healthy subjects. Psychiatry Clin Neurosci. 2009;63:283–90. doi: 10.1111/j.1440-1819.2009.01965.x. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez-Mendoza J, Vela-Bueno A, Vgontzas AN, Olavarrieta-Bernardino S, Ramos-Platón MJ, Bixler EO, et al. Nighttime sleep and daytime functioning correlates of the insomnia complaint in young adults. J Adolesc. 2009;32:1059–74. doi: 10.1016/j.adolescence.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 2007;3:289–94. [PMC free article] [PubMed] [Google Scholar]
- 8.Hasler BP, Germain A, Nofzinger EA, Kupfer DJ, Krafty RT, Rothenberger SD, et al. Chronotype and diurnal patterns of positive affect and affective neural circuitry in primary insomnia. J Sleep Res. 2012;21:515–26. doi: 10.1111/j.1365-2869.2012.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Benedito-Silva AA, Menna-Barreto L, Marques N, Tenreiro S. A self-assessment questionnaire for the determination of morningness-eveningness types in Brazil. Prog Clin Biol Res. 1990;341B:89–98. [PubMed] [Google Scholar]
- 11.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 12.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–7. [PubMed] [Google Scholar]
- 13.Spielberger CD, Gorshusch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory ("Self-Evaluation Questionaire"). Palo Alto: Consulting Psychologist Press; 1970. [Google Scholar]
- 14.Gaspar-Barba E, Calati R, Cruz-Fuentes CS, Ontiveros-Uribe MP, Natale V, De Ronchi D, et al. Depressive symptomatology is influenced by chronotypes. J Affect Disord. 2009;119:100–6. doi: 10.1016/j.jad.2009.02.021. [DOI] [PubMed] [Google Scholar]