ABSTRACT
Background
Anterocollis posture is a relatively rare finding among patients with cervical dystonia and often the cause of treatment failure. The dystonic posture can be complex to analyze, and the deep flexor muscles of the neck, longus capiti, and longus coli can be challenging to access.
Methods
We present a modification of a previously described endoscopic technique that allows straightforward access to the longus capiti muscles in an outpatient setting under local anesthetic.
Results
We describe the technique based on our experience on 6 patients during a 2‐year period with a total of 22 injections, and we review the literature.
Conclusion
The injection is well tolerated and has led to significant improvement in the majority of patients.
Keywords: longus capiti, endoscopic injection longus capiti, anterocollis, anterocaput, botulinum toxin injection for cervical dystonia
Anterocollis is one of the most challenging dystonic postures to correct and is a common reason for treatment failure.1, 2 One of the main difficulties in the treatment is the injection of the deep muscles of the neck such as the longus colli and longus capiti.1, 2 We have previously published the technique of injection of the longus colli under electromyogram (EMG) guidance.3 In this article, we describe the technique of the endoscopic injection of the longus capiti and review the results of our current patient cohort.
The longus capiti arises in a series of thin tendons from the anterior tubercles of the transverse processes of C3 to C6; these unite to form a muscular band, which inserts superiorly on the occiput, anterior to the foramen magnum, and posterior to the pharyngeal tubercle. It is anterior and slightly lateral to the longus colli.4 It is responsible for head flexion on the cervical spine and therefore involved in the dystonic posture of flexion of the head on the neck. This was termed anterocaput posture in Reichel's classification.2, 5
As a result of its position deep in the neck and high up posterior to the pharynx, it has traditionally been thought to be inaccessible to botulinum toxin injections. Based on Reichel's work,6 we have developed a simplified technique that we have regularly used for the treatment of patients with anterocaput since 2017.
Methods
With the patient reclining at 45° on a couch ensuring the head is supported, the nose is prepared using cophenylcaine spray (lignocaine 5% with phenylephrine); 2 sprays are instilled in each nostril, and the patient is instructed to sniff to ensure the back of the nose and nasopharynx are covered. In addition, the spray is applied to cotton wool pledgets and inserted into the anterior nose. While the local anesthetic is taking effect, the rest of the injection is prepared.
The toxin is diluted and drawn into a 1 mL syringe attached to a spinal needle (18 g 12 mm × 90 mm). The cotton wool pledgets are removed. Using a 4 mm rigid Hopkins rod (Wolf 4 mm x 175 mm 0° sinus scope, Richard Wolf Medical instrument company, Vernon Hills, Illinois) attached to a camera stack, the spinal needle is advanced along the floor of the nose under direct vision (see video S1 in online version). In patients with dystonia affecting the longus capiti, it is possible to see lateral ridges in the postnasal space, which are the dystonic hypertrophic muscles under the pharyngeal mucosa (Fig. 1). Although it is easy to see the muscles, it is not always easy to target the exact spot because of anatomical variations such as deviation of the nasal septum and movement of the patient's head. For the majority of patients, the needle is advanced directly backward without difficulty; where there is a septal deviation, the needle may need to be passed above the inferior turbinate or more obliquely to reach the postnasal space. Once the postnasal space is identified, the needle is inserted into the visible ridge medial to the Eustachian tube orifice and the toxin is injected (Fig. 2).
Figure 1.
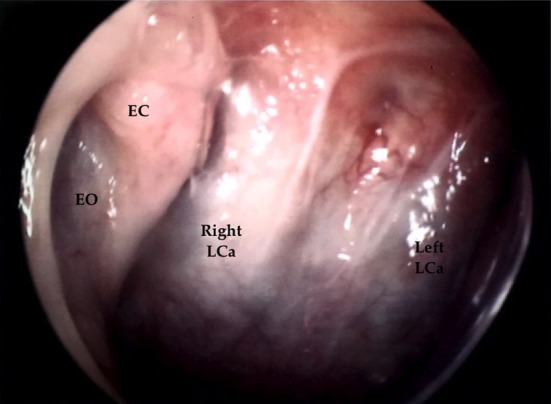
Endoscopic view of the postnasal space via right nostril using a 0‐degree telescope. Ridges of hypertrophic LCa muscles seen under the pharyngeal mucosa. EC, Eustacian cushion; EO, Eustacian tube orifice; LCa, longus capiti.
Figure 2.
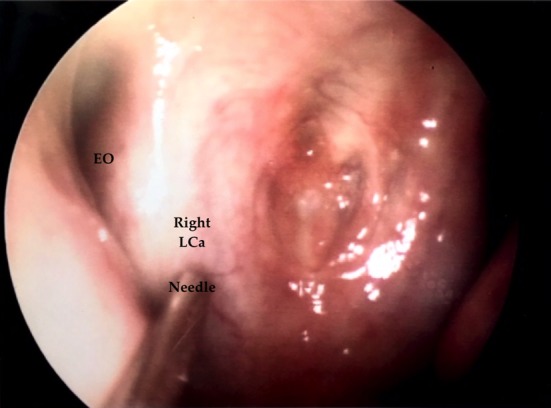
Endoscopic view of the postnasal space with injection needle in the right LCa muscle medial to the EO. EO, Eustacian tube orifice; LCa, longus capiti.
Results
The clinical characteristics of the patients and results are summarized in Table 1. Between March 2017 to April 2019, more than 2 years of experience using this technique, 22 injections have been performed in 6 patients with dystonic anterocollis posture.
Table 1.
Clinical characteristics and results of the 6 patients with CD having LCa injections between March 2017 and April 2019
| Sex/Age | Diagnosis | Age Onset, y | CD Type and Duration | Final Protocol in Units | Type of Toxin | Number Injections | Benefit Duration in Weeks | Side Effects | % Satisfaction | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| F/61 | CD + mouth dystonia | 55 | Antecaput, 4 years |
LCa 50 u × 2 SH 10 u × 2 SCM 60 u × 2 |
AboB | 7 | 14 | None | 95 |
Previous nasal regurgitation to fluids at higher dose Previous injection with LCo no benefit |
| F/79 | Meige | 73 | Antecaput + Antecollis, 4 years |
LCa 15 u × 2 LCo 15 u × 2 SH 5 u × 2 SCM 5 u × 2 |
IncoB | 4 | 16 | None | 70 | Previous severe dysphagia with AboBo changed to IncoBo and reduced dose |
| F/69 | Meige | 65 | Antecaput + left tilt, 2 years |
LCa 40 u × 2 SH 20 u × 2 SCM 20 u × 2 |
IncoB | 5 | 12 | None | 80 |
Initial dysphagia and nasal regurgitation changed to IncoBoNT Patient transferred to another clinic |
| F/53 | CD | 50 | Antecaput+ antecollis + right tilt, 3 years |
LCa 30 u × 2 LCo 30 u × 2 SH 10 u × 2 R SCM 80 u L SCM 120 u R Splenius 200 |
AboB | 4 | 12 | None | 70 | Severe CD much improved |
| F/85 | Meige + Kyphosis | 73 | Antecaput, 10 years |
SCM 80 u × 2 SH 10 u × 2 |
AboB | 1 | 12 | None | 20 | Fixed kyphosis limiting ROM; no clear benefit from addition of LCa |
| M/80 | Meige | 64 | Antecollis, 14 years |
LCo 60 u × 2 SH 10 u × 2 SM 80 u × 2 |
AboB | 1 | 16 | None | 90 | Patient did not feel additional benefit from LCa injection and declined further LCa injections; since then we have added SCM to protocol with significant additional benefit |
The final protocol is the optimal scheme of injections for the patient. % satisfaction is given by the patient at each visit.
F, female; M, male; u, units; R, right; L, left; ROM, range of movement; CD, cervical dystonia; Meige, cranio‐cervical dystonia; LCa, longus capiti; LCo, longus colli; SH, suprahyoids; SCM, sternocleidomastoid; AboB, abobotulinumtoxinA; IncoB, IncobotulinumtoxinA.
All of the patients who have received injections into the longus capiti were patients who experienced suboptimal results because they had failed the conventional approach with bilateral sternocleidomastoid muscles (SCMs), scalenius, or suprahyoid muscles alone or in combination. Patients were referred by expert neurological botulinum toxin injectors or were part of our cohort of anterocollis patients who did not get sufficient benefit from longus colli injections.
We report the subjective improvement in posture after adding the injection of the longus capiti expressed as a percentage of normal by the patient. The improvement ranged from 50% to 90%, except for 1 patient who only improved by 20% because of an additional skeletal deformity (kyphosis). The injections were well tolerated. For the patients with anatomical variation such as nasal septal deviation, the injections could be painful despite the local anesthesia. The injection was difficult for 1 recently seen patient with additional severe cervical myoclonus who has not been included in the study.
The main side effects were mild nasal regurgitation and mild transient dysphagia to solids lasting 2 weeks and requiring minor dietary modifications such as softer food or using a drink to wash down a solid bolus. None of our patients have had sufficient difficulty to require medical attention, and we are only aware of the issue because we specifically inquire about swallowing on each clinic visit.
Discussion
Dystonic anterocollis is a rare condition, but 1% to 24% of the cases of complex cervical dystonia present with an anterocollis component.2 It is a difficult entity to treat because of the involvement of the deep muscles of the neck. We found that the rating scales used in cervical dystonia are not helpful in assessing patients with anterocollis as the posture is very dependent on movements such as walking. We have used the subjective improvement reported by the patients as we feel this reflects the improvement in disability much more accurately. We acknowledge that a validated functional rating scale specifically designed for antecollis patients would be valuable.
Although the longus capiti is deeply placed in the neck, it lies under the mucosa of the posterior pharynx. In the 1990s, a per‐oral approach through the posterior pharyngeal wall was used but abandoned because of the unacceptable dysphagia as a result of diffusion into the pharyngeal constrictors (personal communication, M. H. Marion, 2010). In 2016, Reichel described a per‐nasal approach targeting the muscle above the pharyngeal constrictors. He reported 15 patients with anterocaput treated with an endoscopic approach under a short‐acting intravenous anesthetic (propofol).6 A recent update at 5 years of follow‐up showed a sustained clinical benefit.7
Another technique to inject the longus capiti has been recently reported by Michelis and colleagues8 that combined EMG and an endoscopic approach. They reported on 1 case with an EMG needle (Myoject, 75 mm; Natus Manufacturing Limited, Gort, Co Galway, Ireland) inserted under endoscopic control and EMG signal recorded during rest, phonation, and slight flexion of the head; it is not clear whether the approach was via the nose or mouth.
We feel that the procedure ideally should be performed in the clinic without the use of general anesthetic, hence avoiding repeated general anesthesia, approximately every 3 months. We therefore modified the Reichel's technique using the rigid endoscope under local anesthetic. In cases where there is severe head tremor or myoclonus, a short general anesthetic may be more appropriate.
The use of EMG as described by Michelis and colleagues8 could add precision to the procedure, but as we can visualize the bulk of the hypertrophic longus capiti (Fig. 1) with endoscopy, we think that this is not necessary. We have tried to use the EMG with the Myoject 75 mm through the endoscopic nasal approach, but the needle was not long enough to reach the muscle itself, and therefore we have continued using the spinal needle as described.
Rigid nasal endoscopy with a 0° Hopkins rod is a well‐established procedure in Otolaryngology (ENT), originally popularized by Stammberger and Posawetz.9 The procedure is often performed to treat epistaxis.10 The procedure is well tolerated, and although thinner endoscopes are available, patient tolerance of the 4 mm scope is similar.11 The equipment for performing the procedure is readily available in the ENT outpatient setting, and therefore this procedure is ideally performed in a joint neuro/ENT clinic.
Two of our patients had only 1 injection of longus capiti. We know that with further injections the results may have improved; however, in both instances the patients elected not to undergo further longus capiti injections as they did not feel the improvement in posture outweighed the discomfort of the procedure. On review of both patients, we concluded that they were not well suited to these injections because of the kyphosis and the limited range of active and passive movement of the neck in 1 patient and because of predominant antecollis posture in the other patient.
With increased experience with this group of patients it is clear that patients with a combination of anterocaput and antecollis need both the longus capiti and longus colli injected. In these patients, the total dose is the same (see Table 1). We also found that these patients require injections of other head flexor muscles such as suprahyoid and SCMs to gain full control of their neck posture (see Table 1). These injections are valuable in primary dystonic patients such isolated cervical dystonia or cranio‐cervical dystonia (Meige syndrome). The anterocollis posture in parkinsonism/multiple system atrophy is not solely a dystonic phenomenon, and we do not feel that this is a good indication for longus capiti injection.
The only complication we have regularly encountered is nasal regurgitation of fluids when drinking. In the majority of cases, this has been mild and short‐lived. We believe that this is the result of the leakage of toxin into the tensor veli palatine muscle, which helps to tense the palate and close off the postnasal space when swallowing. It is adjacent to the Eustachian tube orifice and in close proximity to the longus capiti. We have reduced the incidence of this side effect by trying to place the injection more medially and lower than the tubal orifice and also by reducing the dose of toxin injected. Initially our dose was 60 units abobotulinum toxin A on each side, based on the dose we use to inject longus colli as the size of the muscles are similar, but we have found the optimal dose is lower, between 30 to 50 units abobotulinum toxin A per side. Decreasing the dose was not associated with a decreased benefit from the injections. Our starter dose is now 30 units of Dysport (Ipsen Pharma, Boulogne‐Billancourt, France) in each longus capiti, and depending of the benefit, duration of effect, and side effects, we increase if necessary up to 50 units on each side.
To understand dysphagia in this cohort of patients, it is important to take into account the fact that they also have injections in other muscles that are known to be associated with dysphagia such as the suprahyoid muscles (anterior part of the digastric muscle) and the bilateral SCMs. In addition, most patients with anterocaput posture have mild to moderate dystonic swallowing difficulties present before treatment. In our protocol of treating antecaput posture, we have tried different combinations of injections either including or excluding these 3 groups of muscles (longus capiti, suprahyoids, SCMs) to minimize side effects but have found that optimal results required the injection of these 3 muscle groups.
Although the longus capiti is deeply placed in the neck, it is easily accessible in the postnasal space in most patients and can be safely injected with botulinum toxin under local anesthetic in the outpatient setting.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
L.A.H.: 1A, 1B, 1C, 2A
M.H.M.: 1A, 1B, 1C, 2B
Disclosures
Ethical Compliance Statement
We performed a retrospective case note study. The treatment that the patients received was according to our normal protocols and consents procedures and followed the trust's ethical guidelines. Informed written patient consent was obtained from every patient prior to the procedure. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflicts of Interest
The authors declare that there is no funding source for this study, and there are no conflicts of interest relevant to this work.
Financial Disclosures for the Previous 12 Months
L.A.H. declares that there are no additional disclosures to report. M.H.M. has received travel grants and honoraria from Merz Ltd.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Papapetropoulos S, Tuchman A, Sengun C, Russell A, Mitsi G, Singer C. Anterocollis: clinical features and treatment options. Med Sci Monit 2008;14:427–430. [PubMed] [Google Scholar]
- 2. Finsterer J, Maetzu C, Revuelta GJ, Reichel G, Truong D. Collum‐caput (COL‐CAP) concept for conceptual anterocollis, anterocaput and forward sagittal shift. J Neurosci 2015;355:37–43. [DOI] [PubMed] [Google Scholar]
- 3. Flowers J, Hicklin L, Marion MH. Anterior and posterior sagittal shift in cervical dystonia: a clinical and electromyographic study, including a new EMG approach of the longus colli muscle. Mov Disord 2011;13:2411–2114. [DOI] [PubMed] [Google Scholar]
- 4. Bakkum BW, Cramer GD. Muscles that influence the spine In: Cramer GD, Darby SA, eds. Clinical Anatomy of the Spine, Spinal Cord and ANS. 3rd ed. Amsterdam, The Netherlands: Elsevier; 2014:98–134. [Google Scholar]
- 5. Reichel G. The COL CAP Concept. 3rd ed. Self‐Publishing Company; 2014. [Google Scholar]
- 6. Reichel G, Stenner A, von Sanden H, et al. Endoscopic‐guided injection of botulinum toxin into the longus capitis muscle and into the obliquus superior part of the longus colli muscle in dystonic antecaput: our experience. Basal Ganglia 2016;6:97–100. [Google Scholar]
- 7. Reichel G, Glaess S, Stenner A. Endoscopic treatment of dystonic antecaput—5 years experience. Poster presented at: TOXINS, Basic Science and Clinical Aspects of Botulinum and Other Neurotoxins— 16–19 January, 2019, Copenhagen, Denmark.
- 8. Michelis J, Schuler F, Debove I, Müllner J, Lachenmayer L, Seifert E. Combined EMG and endoscopy guided botulinum toxin injection of the longus capitis muscle in cervical dystonia with anterocaput [abstract]. Mov Disord 2018;33(suppl 2). https://www.mdsabstracts.org/abstract/combined-emg-and-endoscopy-guided-botulinum-toxin-injection-of-the-longus-capitis-muscle-in-cervical-dystonia-with-anterocaput/. Accessed June 30, 2019. [Google Scholar]
- 9. Stammberger H, Posawetz W. Functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol 1990;247:63–76. [DOI] [PubMed] [Google Scholar]
- 10. Kumar MVV, Prasad K, Gowda PRB, Manohar SR, Chennaveerappa PK. Rigid nasal endoscopy in the diagnosis and treatment of epistaxis. J Clin Diagn Res 2013;7:831–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Neel GS, Kau RL, Bansberg SF, Lal D. Comparison of 3 mm versus 4 mm rigid endoscope in diagnostic nasal endoscopy. World J Otorhinolaryngol Head Neck Surg 2017;3:32–36. [DOI] [PMC free article] [PubMed] [Google Scholar]


