Abstract
Biological attacks can cause both an epidemic of infectious disease and of fear and panic. Epidemiological triangle chain models can be used to present both these types of epidemic. By merging these two triangles we suggest a new four-sided pyramidal model of bioterrorism attack and appropriate levels of prevention. Primordial prevention of biological attacks should comprise the impeding of access of both terrorists and biological agents to the territory. The primary prevention level should comprise internal surveillance of potential sources of agents and terrorists. Secondary prevention activities should be directed toward breaking both the epidemic of infectious disease and that of fear and panic. Tertiary prevention should include measures for repair following the attack. This is a task mainly for mental health professionals, curing and rehabilitating those affected by the epidemic of fear and panic. The suggested epidemiological model can be implemented into training programmes for detecting and responding to bioterrorist attacks around the world.
Keywords: Bioterrorism, Epidemics, Paradigm, Prevention
Introduction
In 1998, the US Commission on National Security in the 21st Century concluded that biological agents were the most likely choice of weapons for disaffected states and groups.1 The Congressional Office of Technology Assessment estimated that the aerosolized release of 100 kg of anthrax spores upwind of Washington DC, could result in approximately 130 000 to 3 million deaths, a weapon as deadly as a hydrogen bomb.2 The World Health Organization (WHO) defines a biological agent as an agent that produces its effect through multiplication within a target host and is intended for use in war to cause disease or death in human beings, animals, or plants.3 Biological agents could also include protein biotoxins produced by microorganisms, poisonous animals and plants.4 Bioterrorism is defined as the release of biological agents or toxins that impact upon human beings, animals or plants with the intent to harm or intimidate.5
Unlike nuclear, chemical, and conventional weapons, the onset of a biological attack is insidious. Biological agents stimulate terror in the affected population because they cause injury and death in strange and prolonged ways. Biological weapons are nearly as easy to develop, far more lethal, and easier to deliver than chemical weapons and, unlike nuclear weapons, they are inexpensive to produce and the risk of detection is low. Progress in molecular biology has made fast and easy biotoxin production possible. Biological weapons may act on many different targets, can be disseminated by food and water, by insect vectors, or by aerosol, may have many means to penetrate targets and may be used by low-qualified terrorists. Considering these facts, it becomes obvious that it is practically impossible to make a unique doctrine for each possible threat. Improvement will not easily occur by investing money in established paradigms of public health; rather than that, a new, more effective, all-inclusive epidemiological model of bioterrorism attack must be introduced.
Since September 11th 2001, numerous papers have been published suggesting many antiterrorist measures. To simplify understanding of this abundance of measures we tried to categorize all preventive measures related to bioterrorism attack. To our knowledge, this is the first attempt to present an epidemiological model of the epidemic of fear and panic and possible means of its prevention.
Types of epidemics
Today, the main objective of bioterrorists is to spread fear, anxiety, uncertainty and depression within the population, arouse mistrust of authorities/government, inflict economic damage and disrupt travel and commerce, whereas the occurrence of physical disease remains in second place. If we carefully consider recent experiences from natural epidemics (severe acute respiratory syndrome [SARS], avian influenza) and biological attack (USA anthrax attack, 2001), two types of epidemic specific to biological attack can be recognized: the epidemic of infectious disease and the epidemic of fear and panic. The US anthrax bioterrorism attack in 2001, when letters containing Bacillus anthracis were sent within the country, showed the real dimensions of the epidemic of fear and panic. In total, 22 persons were diagnosed with B. anthracis infection of whom five died, over 32 000 people were treated with antibiotics and a tremendous epidemic of panic and fear overwhelmed the whole population. In the aftermath, a large number of letters, approximately 12 000, with suspect contents were discovered in the USA, as well as 7622 harmless letters across Europe, as imitations of the real attack.6, 7 They amplified and expanded the epidemic of panic and fear, giving it characteristics of pandemic.
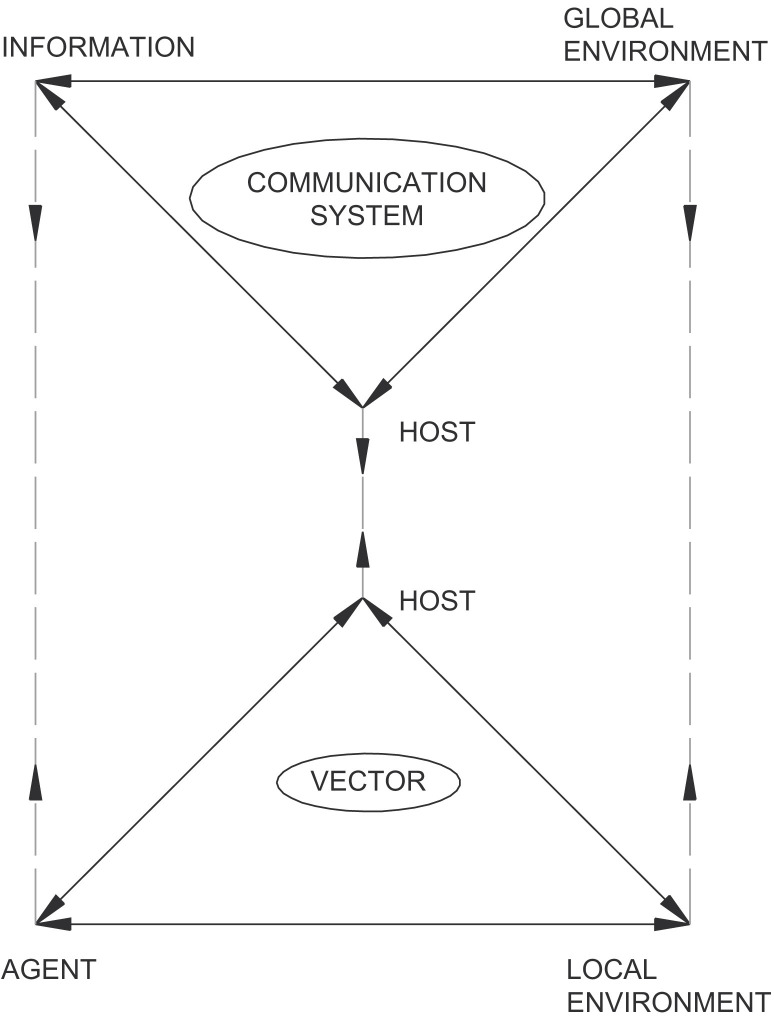
We used the old fashioned, simplest triangle chain model to present the epidemic of infectious disease. The epidemic of fear and panic is presented as a triangle chain model by analogy. In the new model, information is equivalent to the agent, global environment corresponds to the local environment, and the communication system is similar to the vector (Fig. 1 ). In reality, these two models are not separate.
Figure 1.
Model of the epidemic of fear and panic.
New epidemiological paradigm
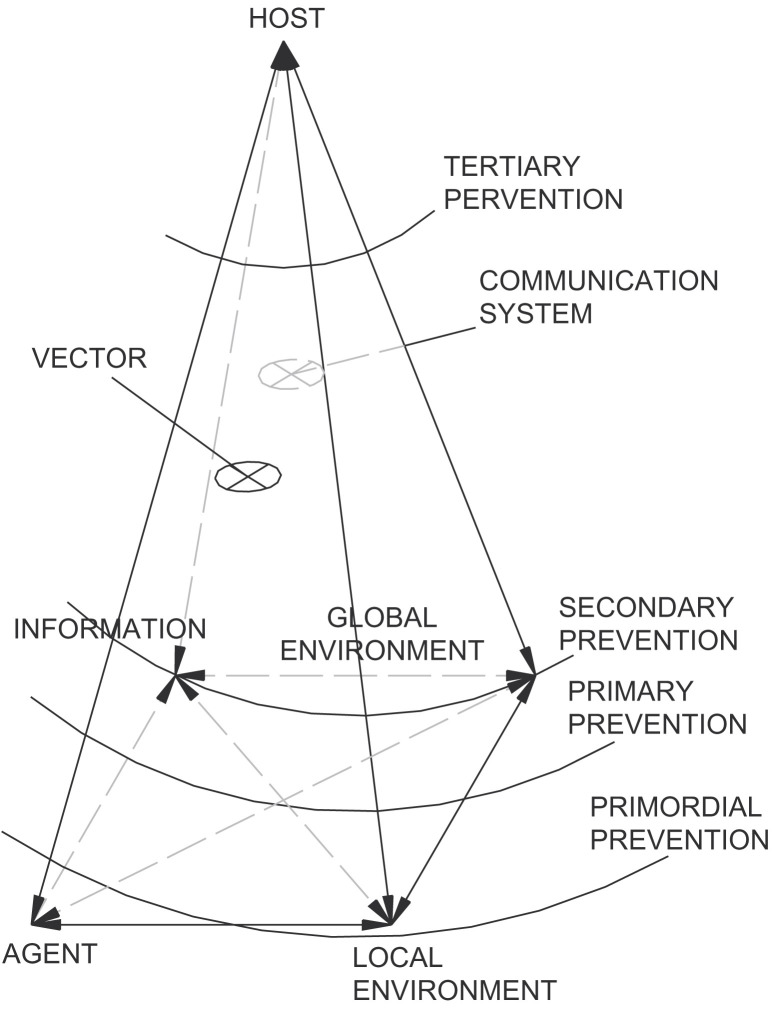
In the modern world, the ‘global environment’—political, social, economic and psychological environment—and the mass media, are of great importance, which adds a new dimension in the case of natural epidemics and biological attacks. In the light of the ‘global environment’, the new epidemiologic paradigm of bioterrorism attack is proposed. This model was created by merging two triangle chain models (epidemic of infectious disease and epidemic of fear and panic). The new model has the form of a four-sided pyramid. It shows the main components of these processes, their mutual relationships and possible inter-reactions. The cornerstones of that pyramid are: agent, information, local environment and global environment. They are in mutual inter-reactions and in inter-reaction with the host, which is on the top of the pyramid (Fig. 2 ). The new four-sided pyramidal epidemiological model should present perplexing events and relationships before, during and after biological attack. This epidemiologic pyramid could also serve as a practical model for the planning and implementation of intervention measures.
Figure 2.
Levels of prevention organized as spherical systems. (The pyramid does not have four equal sides; strictly mathematically, the pyramid is on an incline. However, for simplicity of understanding it is presented as a four-equal-sided pyramid.)
After the USA anthrax attack in 2001, medical and safety communities suggested numerous anti-attack measures and ideas. However, the question of how to solve and simplify so many suggested anti-attack measures remains. We have tried to define and classify them. The answer would be to apply several levels of prevention. Four levels of prevention were defined according to demands related to biological attack, and preventive measures were attributed to each of them. As presented in Fig. 2, the four levels of prevention are spherical systems. This shape was applied to ensure easier, apprehensible and simpler overviews both for health and safety professionals and for the public. Also, spherical systems indicate numerous prevention measures within each prevention level and at the same time reduce possible confusion and duplication of selection of preventive measures. Finally, spherical systems clearly indicate (1) which components (represented as cornerstones of the pyramid) should be protected at any phase of the biological attack (components inside of that sphere), and (2) which components (components outside of that sphere) should be addressed by intervention measures.
The primordial prevention level is a sphere that cuts the pyramid above the agent apex. In this phase, the biological agent is out of the target territory. The primary prevention level cuts the pyramid above both the agent apex and the local environment apex. The secondary prevention level cuts the pyramid through the information and global environment apexes. Secondary prevention activities should be addressed promptly, effectively, and should be directed to breaking both the epidemic of infectious disease and the epidemic of fear and panic. The tertiary prevention level is a sphere that cuts the pyramid below the top host apex. These four levels of prevention should not be strictly separated temporally and spatially. They should be developed and improved permanently, both in peacetime and in emergencies.
Characteristics of the epidemic of fear and panic
Attacks involving biological weapons may induce significant mental and social effects in a number of ways even when the agents induce low levels of mortality and physical morbidity. One of the first mental effects is intense social and psychological distress, especially fear of biological agents, even when they are not used. There are several reasons for this reaction: the invisibility of biological agents, the possibility that the agent can be spread by personal contact, the uncertainty of the extent of dangerousness of biological weapons, etc. On the other hand, the exposure to any severe stressor—whether natural or man-made—is a risk factor for a range of long-term social and mental problems. Social problems emerging after exposure to biological agents, including population displacement, breakdown of community support systems, and social stigma associated with contagion or contamination, may further contribute to the phenomenon of mass psychogenic illness.8, 9
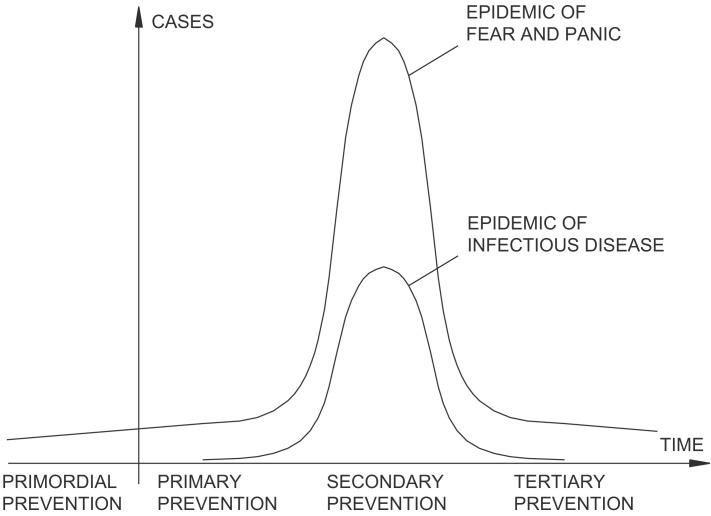
Fig. 3 clearly presents both the epidemic of infectious disease and the epidemic of fear and panic with their numerical (number of cases) and time dimensions and their zone of action for each prevention level, and emphasizes the significance of primordial and primary prevention. It helps us observe the differences between these two types of epidemics in order to prepare intervention measures. The epidemic of fear and panic can be divided into three phases (Fig. 3). The first is the anticipation phase that encounters fear, anxiety, and a possible lower level of panic and somatization at the individual and community level. The presence of these phenomena depends on the seriousness of the threat, any recent terrorist attack in the same or a close territory, awareness of community vulnerability, etc. Medical workers summoned in response teams and exposed to affected (or presumed affected) patients may become anxious, ambivalent and try to avoid contact with patients. Such patterns of behaviour may have a demoralizing effect, and should be treated by providing relevant information (contagiousness of agent) and by implementing appropriate means of protection (protective clothing, vaccinations). Primordial and primary levels of prevention should comprise activities designed to mitigate the anticipation phase of the epidemic of fear and panic.
Figure 3.
Phases and levels of prevention of the epidemic of infectious disease and the epidemic of fear and panic.
The second phase of the epidemic of fear and panic occurs simultaneously with the epidemic of infectious disease. People are faced with the real threat of infection and are involved in activities of rescuing and helping. Some people may exhibit maladaptive reactions, such as disorganized or apathetic behaviour, and may not be able to protect themselves appropriately. Also, the immediate attention of mental health workers should be paid to the possibility of direct consequences of the biological agents. Biological warfare agents may act directly on the central nervous system and produce a wide range of psychiatric symptoms.8, 10 Secondary prevention measures are recommended in this phase.
In the third phase, the level of fear and panic, disturbing mental health signs and symptoms as well as somatization and grief are significantly elevated long after the attack. It is a period of high vulnerability for the whole community. The threshold for somatization and triggering psychiatric and somatic diseases in the community is much lower than usual. Such a community is more susceptible and vulnerable to harmless threats and to the consecutive development of panic and chaos. This is a period for full tertiary prevention action. Actions should be two-dimensional, i.e., they should be handled in two directions: toward the reduction of fear and panic and toward shortening of this period (Fig. 3). Although in an acute attack biotoxins cannot multiply like living biological agents, the same model (Figure 1, Figure 2, Figure 3) can be applied both for the course of the attack and its prevention.
Finally, we would like to compare the epidemic of infectious disease with the epidemic of fear and panic caused by bioterrorism attack (Fig. 3). Due to the anticipation phase, the epidemic of fear and panic starts from a higher level than the epidemic of infectious disease, has a much higher amplitude and lasts much longer. While an epidemic of infectious disease can last several weeks or months, an epidemic of fear and panic could last for months, even years, acquiring characteristics of a pandemic. Furthermore, in an epidemic of infectious disease, the number of diseased (‘primary victims’) varies from several to several hundreds or thousands. On the other hand, in an epidemic of fear and panic the number of diseased (‘secondary’, ‘tertiary’ and ‘quaternary victims’) can reach hundreds of millions.10 According to this pattern, one can generally have more influence on the epidemic of infectious disease than on the epidemic of fear and panic.
The primordial level of prevention
The primordial prevention of biological attack should be addressed in two directions: impeding the access of bioterrorists and of the biological agents to the territory. These activities can be improved by better international cooperation and control, and by improving border control.
Progress in biotechnology has led to bioproduction capabilities being accessible to individuals with limited experience, allowing for illicit use, and making the identification of bioterrorists much more difficult. While certain countries are known or suspected to have biological weapons programmes, non-state actors or autonomic groups have become important as well.2, 5 Documents recovered in Afghanistan suggest that Al-Qaeda had conducted extensive research on weapons that can cause mass fatalities, including biological weapons.11 The role of intelligence services and their international cooperation is of prime importance in this phase. Suicide bio-bombers intentionally infected with biological agents are ‘nightmares’ for many countries. The mass movement of tourists, immigrants and refugees could result in the introduction and dissemination of emerging diseases into distant populations. In 1972, a Muslim pilgrim from Kosovo, who returned to Yugoslavia from Mecca, infected 175 people (35 of them died).12 In ‘virgin populations’ without hereditary immunity, the price would have been much worse. It was estimated that a single terrorist act that begins with just a few cases in April would end in the disease becoming endemic in 14 countries by the end of the same year.13
The USA has one of the best-controlled borders in the world. Enormous amounts of money have been spent on shoring up laboratory networks and communication systems in the inner USA. Nevertheless, the primary aim is to improve surveillance systems at borders and airports. The Central Intelligence Agency (CIA) has developed small, portable devices (PCR, biosensors) with high sensitivity and specificity for the rapid detection of environmental contamination with selected infectious agents.14 Other algorithms (e.g. LIDAR—Light Detection and Ranging System, BRACIS—Biological, Radiological and Chemical Information System, IBDS—Integrated Biological Detection System, etc.) have been developed for the detection of biological warfare.15
Primordial prevention should improve our ability to understand and control potential dynamics of disease transmission within human and animal populations, as well as plant diseases, in both industrialized and developing country settings. This should enhance our capacity to combat the effects of biological weapons and emerging diseases on biological communities and biodiversity.
Nevertheless, this level of prevention includes preparation of national and local plans for an adequate response in the case of biological attack, including risk analysis of weaknesses in the public mental health system during crisis and realistic training of relevant personnel in social and mental health interventions. Prioritizing the development of community mental health services, integrated with general health services, is thus essential to prepare for a mental health response during and after emergencies.8
The primary level of prevention
The primary prevention of biological attack should comprise monitoring and surveillance of potential internal sources of biological agents and bioterrorists. Several agents from category A (tularaemia, viral hemorrhagic fevers, botulism, anthrax, plague) are present in many countries. They are mainly sporadically present or currently absent as indigenous diseases. Also, the outbreak of the disease could occur due to accidental infection during the test and research of biological weapons. A smallpox outbreak involving a Soviet field test of weaponized smallpox killed three people (two of them children) and involved the disinfection of homes, quarantine of hundreds of people, and administration of 50 000 vaccine units.16 Early detection could save many lives by triggering an effective containment strategy such as vaccination, treatment, and, if necessary, isolation and quarantine.17 A developed network of data collecting, rapid data transmission to the relevant public health decision-makers and their careful analysis are the priorities. The aim is to notice subtle differences between usual and unusual occurrence of diseases.
Reforming state public health legislation can improve the infrastructure organized to respond to bioterrorism and other emerging threats. Laws often do not reflect contemporary scientific understanding of diseases (surveillance, prevention) or legal norms for protection of individual rights. When many of these statutes were written, public health sciences, such as epidemiology and biostatistics, were in their infancy and modern prevention and treatment methods were not scientifically established.17
Traditional surveillance systems are generally based on the recognition of a clear increase in diagnosed cases before an outbreak can be identified. For early detection of bioterrorist-initiated outbreaks the sensitivity of the systems need to be improved. This will probably lead to an increase in the number of false positive results; however, it is better to be more sensitive than specific when dealing with weapons of mass destruction. The false positive rate can be reduced by using certified training programmes and better devices.18 Surveillance systems with electronic reporting and internet connection are being developed.
Traditional ‘first responders’ such as the police, fire-fighters, and emergency personnel are not enough in the case of bioterrorism. Those reporting must include community physicians, public health laboratories, emergency departments, intensive care units, district health offices, and hospital admission and discharge systems. Considering the fact that terrorist attacks may occur in industrial facilities, even professionals in occupational health are in a position for early recognition, surveillance, and isolation, and should therefore be targeted for education.19
The recent intentional spread of anthrax in the USA has led to a surge in the development of new surveillance systems. The premises that should guide the design of such systems will have to be developed to integrate data from multiple sources into a single surveillance system. These surveillance systems should be oriented towards detection of unusual diseases, spread in unusual ways. It seems logical that specialists on bioterrorism surveillance should be involved in both developing and maintaining such systems. Innovative analytic procedures will be needed both for early detection and monitoring of the spread of the outbreak and for the identification of the source. Such analytical methods should be able to provide analyses and interpretations of the data that will serve the goals of the system.20
The secondary level of prevention
According to the pyramidal model (Fig. 2), measures of secondary prevention must be addressed to breaking both the epidemic of infectious disease and the epidemic of fear and panic. The emergency response has to take into account two different healthcare scenarios. The first relates to managing the disease caused directly by the attack. The second involves dealing with fear, panic, health concerns and other psychological reactions that normally arise in disasters. Because many people will feel at risk before the extent of exposure can be determined, these indirect consequences may pose the greater challenge to authority, acute healthcare and public confidence. After the emergency response, many of these initial health problems may have prolonged consequences.21
The infrastructure required to respond to an outbreak of infectious diseases is dilapidated in many industrialized countries, having suffered from decades of lack of investment. After the events of September 11th 2001, politicians have devoted enormous amounts of money to the strengthening of public health infrastructure. Thus, the US President has requested billions of dollars for bioterrorism-specific items, such as the manufacture of vaccines and drugs to provide a stockpile of doses sufficient to immunize and cure all US citizens.22 Other funds have been invested in the general infrastructure, in order to raise the essential public health services to a level of performance that matches the constantly evolving threats. Critical components of that infrastructure include a well-trained workforce, electronic information and communications systems, rapid disease diagnosis and reporting, laboratory capacity, and emergency capability.17 The law must provide authority, with fair safeguards, to manage property needed to contain a serious health threat. Stocks of medicines, hospital beds and facilities for disposal of corpses, vaccination, testing, physical examination, treatment, isolation, and quarantine may prevent the spread of infectious diseases. Although the vast majority of people probably will comply willingly (because it is in their interests and/or desirable for the common welfare), some compulsory powers are necessary for those who refuse to comply.17 Although these measures seem necessary, there are those of the opinion that these bioterrorism preparedness programmes have only contributed to a waste of public health resources without evidence of benefit.23
Of great concern in the halting of the epidemic of fear and panic is the variety of spoofing, hacking and malevolent cyberwar/infowar/psyop* activities.18 Bioterrorism and disaster-related information are likely to come to lay individuals from a variety of sources, from the mass media, public health, and government sources to informal workplace exchanges. The way people understand, remember and integrate the information from all these sources is of great importance, because it will serve as a basis for further decisions and actions.24 Information should be disseminated according to principles of risk communication, e.g., information should be timely (to avoid damaging rumours and magical thinking about microbes and viruses), uncomplicated (understandable to local 12-year-olds) and empathic (showing understanding of the situation of survivors).8 Therefore, accurate and transparent information is vital in order to diminish anxiety-provoking speculation and unrealistic fears. It may induce coping mechanisms and thus improve the overall management of bioterrorism.
Another important issue in the management of bioterrorism is preservation of the basic communal and social structure. The social atmosphere in the case of bioterrorism may be charged with uncertainties, prejudice and fear. In such instances, the importance of unchanging communal and social structures cannot be overemphasized.10 Moreover, disasters may leave some communities with increased social coherence. Community members often show great altruism and cooperation, and people may experience pride about coping and resilience and great satisfaction from helping others.8 Laws that complicate or hinder data communication among states and responsible agencies would obstruct a thorough investigation and response to such a public health emergency.17
The tertiary level of prevention
The tertiary level of prevention comprises measures of repair after biological attack (Figure 2, Figure 3). This is mainly a task for mental health professionals, curing and rehabilitating those affected by the epidemic of fear and panic and its consequences. Along with efforts to prevent acts of biological attack, a comprehensive strategy needs to be developed that includes potential for a response against indirect and long-term consequences. Indirect effects comprise medical, social, economic and legal consequences that follow months to years afterwards. The long-term effects can be substantial in the case of biological attack. Experience indicates that following a biological attack there would be three major health concerns: (1) chronic harm and diseases directly caused by the agent, (2) psychological effects, and (3) increased levels of somatic symptoms.21 A population exposed to biological attack experiences direct chronic disease/harm depending on the nature of the agent. The psychological casualties of a bioterrorism event will likely far outnumber all other medical casualties.25 Anticipated psychological consequences include distress responses, such as insomnia, phobias, fear, and the feeling of vulnerability.26, 27, 28, 29, 30, 31 Furthermore, behavioural changes—social withdrawal, acting out, and increased consumption of nicotine, alcohol or drugs—can be one of the responses to the attack.28, 29 Finally, psychiatric/psychological symptoms, such as sadness, irritability, dissociation, the occurrence of psychosomatic symptoms, and psychiatric illnesses such as depression and post-traumatic stress disorder (PTSD) are expected.30, 31, 32
Mental health elements should be included in all disaster response plans. Many people will not develop post-traumatic stress disorder, but a minority will develop the emotional upset reaching the diagnostic threshold for PTSD. The general level of fear can remain high for years, exacerbating pre-existing psychiatric disorders and posing a challenge to the entire public mental health system. The nature of the particular biological weapon will also have a consequential impact on recovery efforts. For example, anthrax spores can persist in the environment for decades; this would make decontamination efforts problematic and lead to persistent health concerns.21 If attack destroys a community, with dislocation and relocation of its members, additional stresses result from the loss of dignity as residents are forced into public shelters and experience the anxiety/fear of strange environments and the disruption of their social networks.33, 34
Many people, whether exposed or not, will exhibit numerous physical symptoms due to prolonged stress. These symptoms include muscular tension, headaches, palpitations, sleep deprivation, hypertension, tachycardia, increased respiratory rate, tremors, and other non-specific signs and symptoms.35 Fear of exposure to biological agents may lead to episodes of medically unexplained epidemic illness (also known as mass sociogenic illness, mass psychogenic illness, or mass hysteria), involving the rapid spread of medically unexplained signs and symptoms, which are misinterpreted by affected persons as signs of serious physical illness.8
From a social psychology point of view, general social interventions are recommended in order to diminish the development of psychopathological consequences. They include re-establishment of normal cultural and religious, and other common interest activities, assuming these activities are safe.8
The potential for new, larger, and more sophisticated attacks has created a sense of vulnerability. According to the role delineation model there are several types of victims: primary victims are people directly exposed to the disaster; secondary victims are people with close family and personal ties to primary victims; tertiary victims are people whose occupations require them to respond to the disaster; and quaternary victims are concerned and caring members of communities beyond the impact area. As a result, these groups should be considered separately in mental health interventions in emergency situations.10 Normative post-disaster reactions of individuals and communities form a relatively predictable pattern from the onset of the disaster through the subsequent 18–36 months.36
Biological weapons induce loss of confidence in the authorities. People have to learn to live with the threat of biological terrorism. Once they lose their novelty, biological weapons will lose their primary potency—the capacity to cause fear. Respecting the applied epidemiology and training programmes already existing in some countries,37 the suggested epidemiological model can be implemented into training programmes for detecting and responding to bioterrorist attacks around the world.
Acknowledgement
This work was supported by the Ministry of Science and Ecology of Serbia, contract no. 145037 and 145013, 2006–2010.
Footnotes
Cyberwar — refers to hostile attacks and illegal invasions of computer systems and networks. Information warfare — also called “cyberterrorism”, it refers to creating havoc by disrupting the computers that manage stock exchanges, power grids, air traffic control and telecommunications. For example, devastating viruses may be considered information warfare. PSYOPS or Psychological Operations: Planned operations to convey selected information and indicators to foreign audiences to influence their emotions, motives, objective reasoning, and ultimately the behavior of foreign governments, organizations, groups, and individuals.
References
- 1.US Commission on National Security in the 21st Century. New world coming: American security in the 21st century, supporting research and analysis. September 15, 1999. Available at: 〈http://govinfo.library.unt.edu/nssg/NWR_Apdf〉 (accessed 31 May 2002).
- 2.Inglesby T.V., Henderson D.A., Bartlett J.G., Ascher M.S., Eitzen E., Friedlander A.M. Anthrax as a biological weapon: medical and public health management. Working group on civilian biodefense. JAMA. 1999;281:1735–1745. doi: 10.1001/jama.281.18.1735. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva: 2002. Health aspects of chemical and biological weapons. [Google Scholar]
- 4.Patocka J., Streda L. Protein biotoxins of military significance. Acta Med (Hradec Kralove) 2006;49:3–11. [PubMed] [Google Scholar]
- 5.Venkatesh S., Memish Z.A. Bioterrorism—a new challenge for public health. Int J Antimicrob Agents. 2003;21:200–206. doi: 10.1016/s0924-8579(02)00366-7. [DOI] [PubMed] [Google Scholar]
- 6.Ashraf H. Europe's response to bioterrorism starts slowly but gathers pace. Lancet. 2002;360:733–734. doi: 10.1016/S0140-6736(02)09943-9. [DOI] [PubMed] [Google Scholar]
- 7.Roffey R., Lantorp K., Tegnell A., Elgh F. Biological weapons and bioterrorism preparedness: importance of public-health awareness and international cooperation. Clin Microbiol Infect. 2002;8:522–528. doi: 10.1046/j.1469-0691.2002.00497.x. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva: 2005. Mental health of populations exposed to biological and chemical weapons. [Google Scholar]
- 9.Durodie B. Facing the possibility of bioterrorism. Curr Opin Biotechnol. 2004;15:264–268. doi: 10.1016/j.copbio.2004.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kron S., Mendlovic S. Mental health consequences of bioterrorism. Isr Med Assoc J. 2002;4:524–527. [PubMed] [Google Scholar]
- 11.Cottrell R, Wolffe R. Safe houses yielding documents on weapons of mass destruction. The Financial Times Limited; November 23, 2001.
- 12.Kuljic-Kapulica N. Smallpox—in the past or not? Srp Arh Celok Lek. 2004;132:272–276. doi: 10.2298/sarh0408272k. [DOI] [PubMed] [Google Scholar]
- 13.O’Toole T. Smallpox: an attack scenario. Emerg Infect Dis. 1999;5:540–546. doi: 10.3201/eid0504.990416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Griffiths P.D. Benefits of bioterrorism. Rev Med Virol. 2002;12:131–132. doi: 10.1002/rmv.358. [DOI] [PubMed] [Google Scholar]
- 15.Spencer R.C., Lightfoot N.F. Preparedness and response to bioterrorism. J Infect. 2001;43:104–110. doi: 10.1053/jinf.2001.0906. [DOI] [PubMed] [Google Scholar]
- 16.Smallpox outbreak, 1971—Soviet Union: revealed. Available at: 〈http://www.nytimes.com/2002/06/15/health/15SMAL.html〉 (accessed 31 May 2002).
- 17.Gostin L.O., Sapsin J.W., Teret S.P., Burris S., Mair J.S., Hodge J.G., Jr The Model State Emergency Health Powers Act: planning for and response to bioterrorism and naturally occurring infectious diseases. JAMA. 2002;288:622–628. doi: 10.1001/jama.288.5.622. [DOI] [PubMed] [Google Scholar]
- 18.LaPorte R.E., Sauer F., Dearwater S., Sekikawa A., Sa E.R., Aaron D. Towards an internet civil defence against bioterrorism. Lancet Infect Dis. 2001;1:125–127. doi: 10.1016/S1473-3099(01)00068-8. [DOI] [PubMed] [Google Scholar]
- 19.Sterling D.A., Clements B., Rebmann T., Shadel B.N., Stewart L.M., Thomas R., Evans R.G. Occupational physician perceptions of bioterrorism. Int J Hyg Environ Health. 2005;208:127–134. doi: 10.1016/j.ijheh.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Green M.S., Kaufman Z. Surveillance for early detection and monitoring of infectious disease outbreaks associated with bioterrorism. Isr Med Assoc J. 2002;4:503–506. [PubMed] [Google Scholar]
- 21.Hyams K., Murphy F., Wessely S. Responding to chemical, biological, or nuclear terrorism: the indirect and long-term health effects may present the greatest challenge. J Health Polit Policy Law. 2002;27:273–291. doi: 10.1215/03616878-27-2-273. [DOI] [PubMed] [Google Scholar]
- 22.Protecting the Homeland: the President's budget for 2003. Available at: 〈http://www.whitehouse.gov/omb/budget/fy2003/pdf/bud05.pdf〉 (accessed 4 April 2002).
- 23.Cohen H.W., Gould R.M., Sidel V.W. The pitfalls of bioterrorism preparedness: the anthrax and smallpox experiences. Am J Public Health. 2004;94:1667–1671. doi: 10.2105/ajph.94.10.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keselman A., Slaughter L., Patel V.L. Toward a framework for understanding lay public's comprehension of disaster and bioterrorism information. J Biomed Inform. 2005;38:331–344. doi: 10.1016/j.jbi.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Compton M.T., Kotwicki R.J., Kaslow N.J., Reissman D.B., Wetterhall S.F. Incorporating mental health into bioterrorism response planning. Public Health Rep. 2005;120(Suppl 1):16–19. doi: 10.1177/00333549051200S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Butler AS, Panzer AM, Goldfrank LR. Preparing for the psychological consequences of terrorism: a public health strategy. Committee on Responding to the Psychological Consequences of Terrorism, Board on Neuroscience and Behavioral Health, Institute of Medicine of the National Academies. Washington: The National Academies Press; 2003. [PubMed]
- 27.Flynn B.W., Norwood A.E. Defining normal psychological reactions to disaster. Psych Annals. 2004;34:597–603. [Google Scholar]
- 28.Vlahov D., Galea S., Resnick H., Ahern J., Boscarino J.A. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. Am J Epidemiol. 2002;155:988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- 29.Grieger T.A., Fullerton C.S., Ursano R.J. Posttraumatic stress disorder, alcohol use, and perceived safety after the terrorist attack on the Pentagon. Psychiatr Serv. 2003;54:1380–1382. doi: 10.1176/appi.ps.54.10.1380. [DOI] [PubMed] [Google Scholar]
- 30.Silver R.C., Holman E.A., McIntosh D.N., Poulin M., Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11th. JAMA. 2002;288:1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- 31.Schlenger W.E., Caddell J.M., Ebert L., Jordan B.K., Rourke K.M., Wilson D. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288:581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 32.Engel C.C. Outbreaks of medically unexplained physical symptoms after military action, terrorist threat, or technological disaster. Mil Med. 2001;166(12 Suppl):47–48. [PubMed] [Google Scholar]
- 33.Raphael B. Basic Books; New York: 1986. When disaster strikes: how individuals and communities cope with catastrophe. [Google Scholar]
- 34.Ramalingaswami V. Psychosocial effects of the 1994 plague outbreak in Surat, India. Mil Med. 2001;166(12 Suppl):29–30. [PubMed] [Google Scholar]
- 35.DiGiovanni C. Domestic terrorism with chemical or biological agents: psychiatric aspects. Am J Psychiatry. 1999;156:1500–1505. doi: 10.1176/ajp.156.10.1500. [DOI] [PubMed] [Google Scholar]
- 36.Green B.L., Lindy J.D., Grace M.C. Psychological effects of toxic contamination. In: Ursano R.J., McCaughey B.G., Fullerton C.S., editors. Individual and community response to trauma and disaster. Cambridge University Press; Cambridge: 1994. pp. 154–176. [Google Scholar]
- 37.Sandhu H.S., Thomas C., Nsubuga P., White M.E. A global network for early warning and response to infectious diseases and bioterrorism: applied epidemiology and training programs, 2001. Am J Public Health. 2003;93:1640–1642. doi: 10.2105/ajph.93.10.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]