Abstract
The collective impact of major shifts in public health infrastructure and numerous new chronic disease prevention (CDP) capacity-building initiatives that have taken place in Canada over the last decade is unknown. The objective of this study was to determine if CDP capacity (i.e., skills and resources) and involvement in CDP programming improved in public health organizations in Canada from 2004 to 2010. Data for this repeated cross-sectional study were drawn from two waves of a national census of organizations mandated to carry out primary prevention of chronic disease and/or promotion of healthy eating, physical activity and tobacco control. Medians for continuous variables and frequencies for categorical variables were compared across time. Neither resources nor level of priority for CDP increased over time. There was little difference in the proportion of organizations with high levels of skills and involvement in core CDP practices (i.e., needs assessment, identification of relevant practices, planning, evaluation). Skills and involvement in CDP risk factor programming showed some gains, some steady states and some losses. Specifically, skill and involvement in tobacco control programming declined markedly while the proportion of organizations involved in healthy eating and physical activity programming increased. Skills to address and involvement in programming related to social determinants of health remained low over time as did involvement in programming addressing multiple risk factors concurrently. The lack of marked improvement in CDP capacity between 2004 and 2010 against a backdrop of initiatives favourable to strengthening the preventive health system in Canada suggests that efforts may have fallen short.
Keywords: Chronic disease prevention, Public health services and systems, Organizational capacity, Survey, Follow-up study, Canada
Introduction
The first decade of the 21st century was historic for public health in Canada. On the one hand, failure to deal adequately with public health crises such as the contamination of drinking water in Walkerton, Ontario and the SARS (Severe Acute Respiratory Syndrome) outbreak, underscored serious deficiencies in the public health system. On the other hand, the role of public health expanded in health promotion and the primary prevention of chronic disease. Significant developments included, among others, the creation of the Institute for Public and Population Health as one of the Canadian Institutes for Health Research in 2000, and the Public Health Agency of Canada (PHAC) and the National Collaborating Centres for Public Health in 2004.1, 2 The Canadian Population Health Initiative, which has a particular focus on the social determinants of health,3 was launched in 1999 to provide information on the health status and the determinants of health among Canadians.4
Provincial changes in the public health infrastructure were also underway, beginning with the creation of the Institut national de santé publique du Québec in 1999, followed by restructuring of the health system in many provinces from 2000 to 2010.5 Initiatives to develop workforce capacity, define core public health competencies and support training programs were advanced,6, 7 and the number of Canadian universities offering a professional degree in public health (i.e., Masters of Public Health programs) more than tripled from five to over 15.8 Several universities across Canada began the process of building Schools of Public Health.
Initiatives were introduced at national and provincial levels addressing the prevention and control of chronic diseases using collaborative, comprehensive strategies that target populations in diverse settings and at multiple levels. These included, among others, the Pan-Canadian Healthy Living strategy,9 the Quebec Plan d'action gouvernemental de promotion des saines habitudes de vie,10 ActNow BC11 and Ontario's Action Plan for Healthy Eating and Active Living.12
Finally, large-scale chronic disease prevention (CDP) capacity-building initiatives were implemented in all provinces through the Canadian Heart Health Initiative. This multimillion dollar program spanning 15 years (mid-1980s to the late 1990s) comprised province-wide surveys of cardiovascular disease risk factors,13 demonstration projects aimed at developing and evaluating heart health promotion projects14 and dissemination projects to incorporate lessons learned into provincial public health systems.15 This initiative led to the involvement of the non-governmental organization (NGO) sector in public health programming, as well as the creation of multi-organization coalitions and alliances as new forms of public health organizations. An explicit goal was to increase capacity for health promotion and CDP in the public health system.
The collective impact of these changes on CDP capacity in Canada is unknown but, given the depth and breadth of change, a tenable hypothesis is that capacity in Canadian public health organizations increased considerably in the past decade. The objective of this study was to determine if CDP capacity (defined as skills and resources) in public health organizations in Canada, as well as involvement in CDP programming, improved from 2004 to 2010.
Methods
The Public Health Organizational Capacity Study (PHORCAST) is a repeated, cross-sectional survey of all CDP organizations at the regional, provincial and national levels in Canada. Data were drawn from two waves (2004 and 2010) of a national census of all organizations engaged in CDP at regional, provincial and national levels in Canada. Organizations included in the 2004 census were identified in an exhaustive internet search and through consultation with key contacts in all provinces. In addition to formal public health organizations (FPH), the census included NGOs and coalitions, partnerships, and alliances (termed herein as ‘grouped organizations’). ‘New’ organizations identified in 2010 included those created after 2004, existing organizations with ‘new’ CDP divisions or offering ‘new’ types of programming, and those formed by the amalgamation of two or more previously participating organizations. All organizations identified (n = 379 in 2004; n = 421 in 2010) were invited to participate and then screened for eligibility (Table 1 ). Appendix 1 (online file) describes the selection of eligible organizations. The response was high – 92% in 2004 and 89.5% in 2010.
Table 1.
Criteria for inclusion and exclusion of CDP organizations.a
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Geographic area served | • region (i.e. sub-provincial) • province • territory (2010)b • Canada |
• local • territory (2004) |
| Mandate | • primary prevention of chronic disease (i.e., diabetes, cancer, cardiovascular diseases and chronic respiratory illness) • healthy lifestyle promotion • single-focus on healthy eating, tobacco control or physical activity |
• secondary or tertiary prevention of chronic diseasec |
| Primary focus of (prevention) activities | • delivers population-wide programs, campaigns, policies, AND/OR • develops and transfers prevention programs, practices, and policies (PPPs) to other organizations that deliver them to a specific population |
• advocacy • allocation of funds • fund-raising • facilitates joint efforts among organizations • research or knowledge transfer |
| Population served | • population-at-large • organizations (local, regional, provincial or national-level) |
• small groups, individuals • exclusively Aboriginal populations (due to major differences in mandates and resourcing) |
The term ‘organization’ refers to an entire organization (if the organization as a whole conducts CDP activities) or to a specific department, unit or division within an organization (if only a sub-unit of the organization undertakes CDP activities).
All CDP organizations located in the three territories were invited to participate in 2010 however these data were not analysed in this study.
Secondary prevention refers to early detection and prompt intervention to control disease and minimize disability; tertiary prevention refers to reducing the impact of long-term disease and disability by eliminating or reducing impairment, disability, and handicap; minimizing suffering; and maximizing potential years of useful life.
Organizations that delivered CDP programs in specific populations were labelled ‘user’ organizations. Those that developed and transferred programs to other organizations were labelled ‘resource’ organizations. Those with both a ‘user’ and ‘resource’ function were labelled ‘both’.
Data were collected in structured telephone interviews conducted by trained interviewers with one to two key informants per organization depending on whether the organization was ‘both’ user and resource (n = 35 in 2004; n = 81 in 2010). Key informants were identified by senior managers as persons most knowledgeable about implementation and delivery of CDP programs or transfer of CDP programs to other organizations. Interviews were conducted using separate questionnaires for ‘user’ and ‘resource’ organizations. Study variables are described in Appendix 2 (online file). Six organizations with more than one unit specializing in CDP programming in 2004, and 13 in 2010, provided more than one interview.
Data analysis
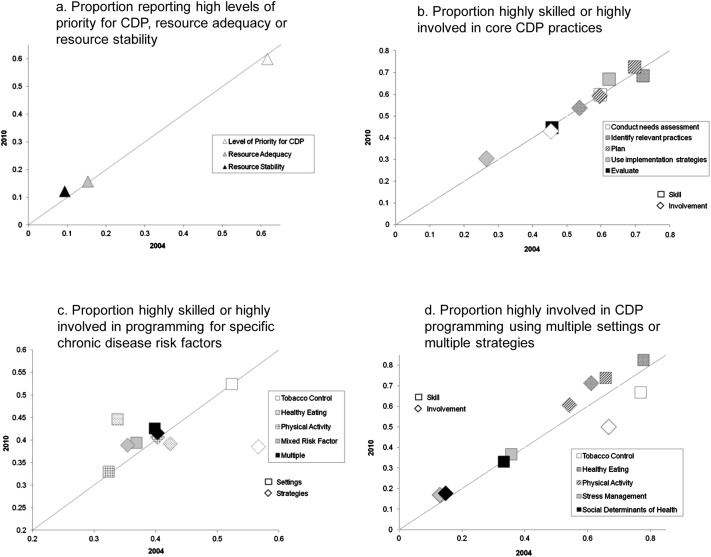
Data from organizations that participated in both surveys and from all new organizations in 2010 were included in the analytic database. Medians for continuous variables and frequencies for categorical variables were compared across time. To compare organizational capacity (i.e., skills and resources) for, and involvement in, core CDP practices and risk factor programming over time, the proportion of ‘user’ organizations that reported the highest levels (i.e., ‘4’ or ‘5’ on a 5-point Likert scale) of skill, involvement, and resources in 2004 was plotted on the x-axis against the proportion in 2010 on the y-axis. Points above the line emanating from the origin represent improvement from 2004 to 2010, those below represent a decrease, and points located on the line represent steady state. Data analyses were conducted using SAS software, version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
Number of organizations
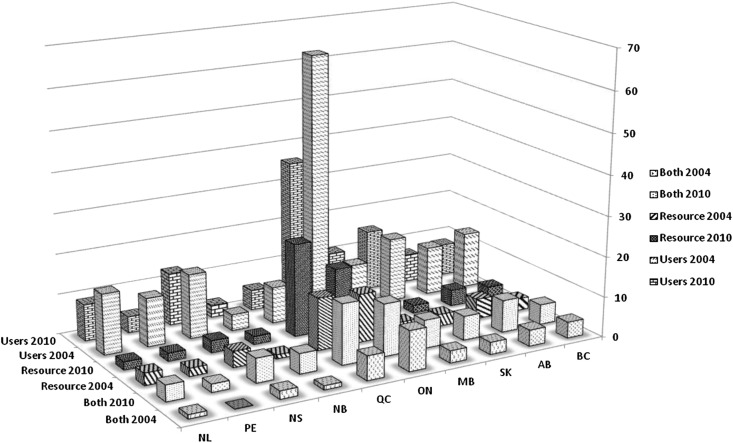
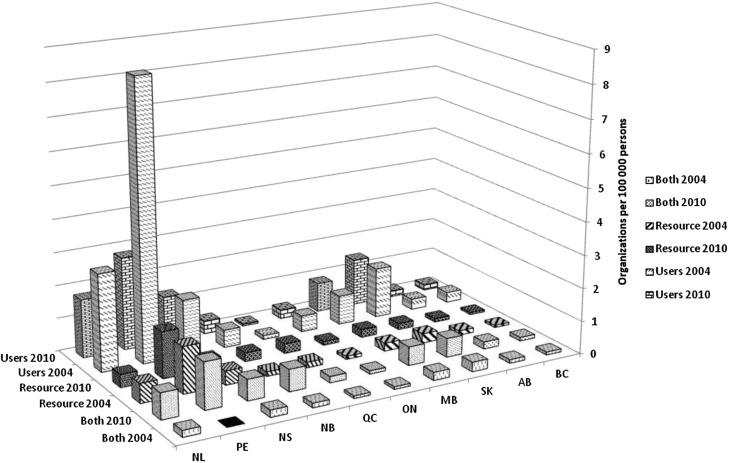
The number of organizations with a CDP mandate in Canada declined slightly over time (280 in 2004; 267 in 2010). Despite this relative stability nationally, there were notable differences within several provinces (Appendix 3 – online file), likely related to restructuring of the public health infrastructure. Also the number of ‘user’ organizations declined, and half of the 10 provinces experienced declines in the number of ‘resource’ organizations (Fig. 1 ). However, in every province, the number of organizations designated as ‘both’ increased. PE, NL and NS maintained the highest number of CDP organizations per 100,000 persons (Fig. 2 ).
Fig. 1.
Number of user and resource organizations in 2004 and 2010 in each of the 10 Canadian provinces.
Fig. 2.
Number of user and resource organizations per 100,000 population in 2004 and 2010 in each of the 10 Canadian provinces. Source Provincial Populations: National Health Expenditure Database (NHEX).
Type of organization
User organizations were older than resource organizations (29 vs 21 years) (Table 2 ). Several changes in the distribution of type of organization over time are notable. The proportion of grouped user organizations declined from 19% to 13%; and the proportion of formally mandated public health resource organizations declined from 31% to 25%. However, the proportion of NGOs increased from 34% to 38%.
Table 2.
Characteristics of CDP organizations in Canada, 2004 and 2010.
| Characteristic | User |
Resource |
||
|---|---|---|---|---|
| 2004 n = 216 |
2010 n = 197 |
2004 n = 77 |
2010 n = 121 |
|
| User and resource organizationsa | ||||
| Age (y), median (IQR)b | 28 (7–51) | 30 (12–57) | 20 (2–48) | 22 (12–50) |
| Type of organization, % | ||||
| Formal public health | 48 | 50 | 31 | 25 |
| NGO | 25 | 28 | 34 | 38 |
| Grouped organization | 19 | 13 | 12 | 15 |
| Other | 7 | 8 | 23 | 22 |
| Geographic area served, % | ||||
| Region | 71 | 58 | 38 | 39 |
| Province | 24 | 34 | 52 | 48 |
| Multiprovince/territory | 2 | 4 | 1 | 4 |
| Canada | 3 | 4 | 9 | 9 |
| Level of CDP activity, % | ||||
| Division/unit | 58 | 73 | 60 | 53 |
| Entire organization | 42 | 27 | 40 | 47 |
| No. Full Time Equivalents, median (IQR) | ||||
| Organizations housing CDP units | 150 (69–850) | 200 (52–1000) | 100 (43–1100) | 100 (30–300) |
| CDP units housed in larger organizations | 15 (7–35) | 17 (8.8–46) | 7 (4–22) | 12.5 (9–33) |
| Organizations entirely engaged in CDP | 3 (1–11) | 2.5 (1–7) | 2.5 (1–7) | 3.(1–7) |
| No. Volunteers, median (IQR) | 35 (12–200) | 31 (10–250) | 12 (0–33) | 13 (0–50) |
| Applied outside for funds, % | 77 | 81 | 69 | 66 |
| Source of outside funds, % | ||||
| Research funding organization | 10 | 17 | 17 | 11 |
| Health Canada | 68 | 39 | 68 | 38 |
| Other federal ministry | 11 | 13 | 21 | 13 |
| Public Health Agency of Canada | – | 39 | – | 49 |
| Provincial Ministry/Dept. of Health | 69 | 64 | 53 | 68 |
| Other provincial ministry | 22 | 33 | 23 | 31 |
| National NGO | 8 | 14 | 8 | 20 |
| Provincial NGO | 35 | 24 | 17 | 25 |
| Municipality | 16 | 19 | – | 13 |
| Major public charity | 13 | 19 | 19 | 16 |
| Private foundation | 18 | 21 | – | 18 |
| Private funding | 28 | 25 | 25 | 26 |
| Fund raising | 23 | 25 | 13 | 16 |
| Other | 2 | 18 | 6 | 15 |
| No. External sources of funding, median (IQR) | 3 (2–4) | 2 (0–3) | 1 (0–3) | 3 (2–5) |
| User organizations | ||||
| High/very high level of priority for CDP, %c | ||||
| All organizations | 62 | 60 | – | – |
| Organizations housing CDP units | 51 | 48 | – | – |
| Separate budget line for CDP, % | 55 | 62 | – | – |
| Entity responsible for CDP, % | ||||
| Specific unit | 51 | 37 | – | – |
| More than one unit | – | 46 | – | – |
| Groups within a unit | – | 74 | – | – |
| Specific manager | 62 | 76 | – | – |
| Part of all managers' jobs | 46 | 45 | – | – |
| Part of board's mandate | 82 | 85 | – | – |
| Primary target, % | ||||
| General | 91 | 85 | – | – |
| Specific health problem | 59 | 43 | – | – |
| Specific demographic group | 69 | 60 | – | – |
| Specific region | 51 | 33 | – | – |
| Size of population served, % | ||||
| <50,000 | 13 | 15 | – | – |
| 50,000–99,999 | 16 | 11 | – | – |
| 100,000–199.000 | 24 | 15 | – | – |
| 200,000–499,999 | 13 | 14 | – | – |
| >500,000 | 33 | 45 | – | – |
| Resource organizations | ||||
| Resources, % | ||||
| Adequacyd | – | – | 33 | 31 |
| Separate transfer budget, % | ||||
| Allocated for most recently transferred innovation | – | – | 61 | 59 |
| Target organizations, % | ||||
| Formal public healthe | – | – | 69 | 66 |
| Community health centre/CLSC | – | – | 47 | 41 |
| Centres de santé et services sociauxf | – | – | – | 71 |
| Family health team | – | – | – | 27 |
| Government | – | – | 65 | 53 |
| NGO | – | – | 51 | 69 |
| School board | – | – | 62 | 65 |
| Health professional assoc. | – | – | 42 | 43 |
| Branch/chapter of resource organization | – | – | 23 | 22 |
| Community group | – | – | 66 | 69 |
Number of organizations < number of interviews.
IQR = interquartile range.
Proportion indicating ‘high’ or ‘very high’ extent of support on a 5 point Likert scale where 1 = Not at all and 5 = Completely.
Proportion indicating ‘agree’ or ‘strongly agree’ on a 5-point Likert scale where 1 = Strongly disagree and 5 = Strongly agree.
Proportion indicating ‘yes’ to health authority/district/service or public health unit/agency.
CSSS exist in QC only. Therefore the proportion was calculated among QC resource organizations.
Organizational jurisdiction
The proportion of user organizations targeting regions declined from 71% in 2004 to 58% in 2010 (Table 2), while the proportion that served entire provinces increased (24% to 34%). Half of resource organizations targeted entire provinces; this did not change over time. A lower proportion of user organizations in 2010 than in 2004 reported that their main target was specific health issues (43% vs 59%) or specific regions (33% vs 51%). The distribution of the size of population served did not differ across years. The proportion of resource organizations targeting government entities declined from 65% to 53%, while the proportion that targeted NGOs increased from 51% to 69%.
Resources for CDP
Most CDP activity was carried out by units/divisions within organizations. The median number of full time equivalents (FTEs) increased in user organizations in which divisions or units undertook CDP activity (150 in 2004; 200 in 2010). There were no differences in FTEs in resource organizations. CDP units increased in size in both user and resource organizations, while the size of organizations entirely engaged in CDP remained stable. The number of volunteers in both user and resource organizations changed little over time.
Most user (80%) and resource organizations (68%) applied to outside sources for additional funding to support CDP activities in 2004 and 2010. However, the sources of funding shifted over time. While the median number of external sources of funding declined in user organizations from three in 2004 to two in 2010, this number increased from one to three in resource organizations. There was no change in adequacy or stability of resources in user organizations (Fig. 3 a). One-third of resource organizations indicated that resources for transferring CDP programs were adequate and this proportion remained stable over time (Table 2).
Fig. 3.
Organizational capacity (skills and resources) for, and involvement in, CDP among public health organizations in 10 Canadian provinces.
CDP priority and accountability
Two-thirds of user organizations indicated that CDP was a high priority in both 2004 and 2010 (Table 2). However among CDP units situated within larger organizations, only 50% indicated that CDP was a high priority for the organization as a whole. Sixty-two per cent of user organizations had a separate budget line for CDP in 2010, compared to 55% in 2004. The responsibility for CDP became more dispersed within organizations over time, shifting from specific units in 2004, to more than one unit or groups within units in 2010.
Skills for and involvement in CDP programming
Both surveys measured skills and involvement in core CDP practices and in programming related to smoking, nutrition, and physical activity. There was little difference across years in skill level or involvement in core practices (Fig. 3b). Two-thirds (67%) of organizations reported high skill levels in needs assessment, identification of best practices, planning, and use of implementation strategies, although less than half (46%) rated evaluation skills as strong. Across years, 56% indicated high involvement in identification of relevant practices and planning. Only 37% reported high involvement in needs assessment and evaluation.
Skill and involvement in tobacco control programming declined markedly over time (Fig. 3c). The proportion of user organizations heavily involved in healthy eating and physical activity programming increased, but involvement in the social determinants of health remained low. Involvement in programs targeting single risk factors across multiple settings or using multiple strategies was higher in both 2004 and 2010 than involvement in activities that targeted multiple risk factors concurrently (Fig. 3d).
Discussion
With the many new initiatives in CDP over the last decade, positive changes to the CDP landscape may have occurred. However, our data suggest that the CDP landscape remained relatively stable in Canada, with few notable improvements across time.
The geographic area targeted by user organizations remained predominantly regional, although the number of organizations with provincial mandates increased. In addition, public health organization housing divisions or units dedicated to CDP activities became larger. These findings may reflect the changeability that characterizes the regionalized healthcare systems implemented in nine of the ten provinces during the 1990s.16 Changes to the regional model since 2004 ranged from consolidation of two or more health regions as in Ontario, Newfoundland and Labrador (2005), and New Brunswick (2008), to complete abolition of regional health authorities as in Prince Edward Island (2005) and Alberta (2008). Such structural transformation creates disruption in CDP programming through, and not limited to, loss of trained personnel, change and/or increase in workloads, increased uncertainty among public health practitioners (regarding differences in cultures between merging organizations) and the public (regarding level of community involvement in decision-making and planning).17, 18, 19 Further, there is evidence20 that sectors similar to CDP, which rely more on people than technology to deliver programs, do not achieve anticipated economies of scale following amalgamations. Most CDP activity is carried out by units within larger structures which focus primarily on health care services. As these structures expand, existing priority attributed to health promotion and disease prevention may erode and the resources for CDP prevention diverted to curative or treatment activities. Macro-level organizational theories21 postulate that the ability to obtain a stable flow of resources from the environment is a core determinant of the maintenance of infrastructure and the development of services within22, 23, 24 and outside competitive markets.25 Within the context of the preventive health system, these theories would imply that long-term stability in infrastructure is critical for the preventive health system to building capacity or even maintaining current levels.
In organizations with CDP mandates, neither the resources nor level of priority increased. Further, skills and involvement in core CDP practices did not change. In 2004 the authors reported that skills and involvement in evaluation were lower than all other practices26 and in 2010, evaluation remained the weakest core CDP practice. Skills and involvement in CDP risk factor programming showed some gains, some steady states and some losses. Tobacco-related skills and involvement decreased, corresponding to decreases in funding for tobacco control in Canada.27, 28 Skills to address the social determinants of health and involvement in social determinants of health-specific programming remained low over time. Although others29 have documented a paucity of public health interventions that address CDP through action on the social determinants of health, the lack of improvement in skills is surprising given increasing recognition of the importance of the social gradient in chronic disease.30, 31 The growing pressure to tackle these ‘upstream’ causes may be tempered by major challenges including: current Canadian political and economic policies;32 lack of evidence of effective interventions;33 lack of clarity as to where on the pathway from determinants to outcomes public health would be expected to have impact;34 significant barriers in partnering with sectors for collaborative cross-sectoral action;35 and absence of systems to support the application of such programming so that health equity is built into planning and performance indicators.36 On the plus side, new public policies to prevent overweight37, 38 seem to have translated into increased skills and involvement in healthy eating and, to some extent, physical activity.
The ratio of user to resource organizations declined from 3.2 in 2004 to 1.8 in 2010, suggesting a shift from a predominantly user to a more resource orientation within the public health system. Additionally, in every province, the proportion of organizations designated as ‘both’ user and resource increased, which may indicate a reduced focus on implementation of programs if organizations are now involved in both activities. Although the most effective mix of user to resource organizations is not known, this trend raises questions about if and how CDP programs, policies and services reach the populations targeted. The decline in the proportion of formal public health resource organizations funded by governments and the increase in the proportion of resource NGOs suggests a shift from the public to the private and not-for-profit sector in CDP innovation and leadership.
The lack of marked improvement in CDP priority, resources, skills and involvement over time against a backdrop of initiatives favourable to strengthening the preventive health system in Canada, suggests that efforts may have fallen short. The reasons for this are likely complex and may relate at least in part to changes in economic conditions and governmental priorities over this period. Our findings are, however, consistent with other studies of change efforts in health systems, which document weak linkages between intentions and results, and high levels of status quo preserving resilience.39, 40, 41 Resilience can be explained by many factors but two may be particularly salient. First, to ensure survival, organizations in highly institutionalized environments generally seek to conform to norms in their fields.41 Although they may slowly evolve, norms are rarely revolutionized, providing a strong foundation for immovability. An example in our context is evaluation capacity. Despite momentum toward evidence-based medical practice, evaluation is still not part of normative organizational capacity in Canadian public health organizations. Second, when there are barriers to workforce renewal, workers in the system remain to all intents and purposes the same. Barriers in the period studied may have included a limited supply of well-trained public health professionals coupled with a growing need for specialized public health expertise in CDP.
Limitations of this research include that data were collected from only one key informant per organization. Ideally organizational-level constructs should be assessed using objective measures, but because few objective measures of organizational attributes exist, informant ‘self-report’ is commonly used to collect data in organizational research.42 The fact that the key informant in most organizations that participated in both surveys differed across time was unavoidable. However, the methodology used to select the individual was consistent across surveys. The follow-up survey data reported herein provide unique longitudinal empirical insight into Canada's preventive health system and contribute to better understanding of the system, identifying areas needing improvement; and provide empirical support for developing OC through human resource planning, development and training, and help monitor changes in OC over time. The current state of knowledge on OC for CDP and the system-level focus taken in our analyses preclude making recommendations that can be turned into specific action points. Future research aimed at understanding causal mechanisms for capacity improvement is needed to complement and extend this work.
As in most developed countries, the chronic disease burden is increasing in Canada and, given the aging of the population, this is unlikely to change. Prevention and public health intervention are generally viewed as having a major role to play in limiting this burden. That this study did not detect marked improvement in CDP skills, resources and involvement over six years against a backdrop of major shifts in infrastructure and numerous initiatives favourable to strengthening CDP should raise concerns about the approaches currently taken to increase public health capacity in Canada to address complex, multidetermined chronic diseases and reduce health inequities.
Author statements
The authors acknowledge the contribution made by Marie-Pierre Sylvestre, PhD and thank all the organizations that participated in this research. Damien Contandriopoulos is the recipient of an FRSQ Research Scholar, Junior 2 career award. Jennifer O'Loughlin holds a Canada Research Chair in the Early Determinants of Adult Chronic Disease. Gilles Paradis holds a CIHR Applied Public Health Research Chair.
Ethical approval
Ethics approval was provided by the Institutional Review Board of the Faculty of Medicine, McGill University and the Comité d'éthique de la recherche du Centre hospitalier de l'Université de Montréal (CRCHUM).
Funding
This study was funded by the Partnerships for Health System Improvement program of the Canadian Institutes of Health Research (CIHR): PHE – 85197.
Competing interests
None declared.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.puhe.2014.05.016.
Appendix 1–3. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Bill C-5: Public Health Agency of Canada Act . 2006. Legislative summary.http://www.parl.gc.ca/Content/LOP/LegislativeSummaries/39/1/c5-e.pdf [Google Scholar]
- 2.Medlar B., Mowat D., Di Ruggiero E., Frank J. Introducing the National Collaborating Centres for Public Health. CMAJ. 2006;175(5):493–494. doi: 10.1503/cmaj.060850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health Disparities Task Group of the Federal/Provincial/Territorial Advisory Committee on Population Health and Health Security . December 2004. Reducing health disparities – roles of the health sector: discussion paper.http://www.phac-aspc.gc.ca/ph-sp/disparities/pdf06/disparities_discussion_paper_e.pdf [Google Scholar]
- 4.Canadian Population Health Initiative . 2004. Improving the health of Canadians, CIHI.https://secure.cihi.ca/free_products/IHC2004rev_e.pdf [Google Scholar]
- 5.O'Connor P., Sanmartin C., Williams-Jones B., Wright C.J., for the Canadian Health Services Research Foundation . April 2012. Harkness Canadian Health Policy Briefing Tour Backgrounder.http://www.chsrf.ca/Librairies/Harkness/2012Harknessbackgrounder-ENsflb.ashx (accessed 19 Jul 2012) [Google Scholar]
- 6.Joint Task Group on Public Health Human Resources . 2005. Building the public health workforce for the 21st century: a Pan-Canadian Framework for Public Health Human Resources planning.http://www.phac-aspc.gc.ca/php-psp//pdf/building_the_public_health_workforce_fo_%20the-21stc_e.pdf Ottawa. [Google Scholar]
- 7.Federal/Provincial/Territorial Joint Task Group on Public Health Human Resources . January 2005. The development of a draft set of public health workforce core competencies.http://www.ciphi.ca/files/documents/cpc/ccemerson.pdf Summary report. [Google Scholar]
- 8.Massé R., Moloughney B. New era for schools of public health in Canada. Public Health Rev. 2011;33:277–288. [Google Scholar]
- 9.Public consultation to inform the Integrated Pan-Canadian Healthy Living Strategy Roundtable: summary report. May, 2003. http://www.phac-aspc.gc.ca/hl-vs-strat/pdf/html/rt_summary-eng.php [Google Scholar]
- 10.Ministère de la Santé et des Services sociaux . Investir pour l'avenir; Québec: 2006–2012. Investir pour l'avenir: Plan d'action gouvernemental de promotion des saines habitudes de vie et de prévention des problèmes reliés au poids.http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2006/06-289-01.pdf [Google Scholar]
- 11.BC Ministry of Health . March 2006. ACTNOWBC: backgrounder. http://www2.news.gov.bc.ca/news_releases_2005-2009/2006HEALTH0017-000253-Attachment1.pdf. [Google Scholar]
- 12.Ministry of Health Promotion . 2006. Ontario's action plan for healthy eating and active living.http://www.mhp.gov.on.ca/en/heal/actionplan-EN.pdf [Google Scholar]
- 13.MacDonald S., Joffres M.R., Stachenko S., Horlick L., Fodor G., for the Canadian Heart Health Surveys Research Group Multiple cardiovascular disease risk factors in Canadian adults. CMAJ. 1992;146:2021–2029. [PMC free article] [PubMed] [Google Scholar]
- 14.Conference of Principal Investigators (COPI) of Heart Health . Health Canada; Ottawa, ON: 2001. Canadian Heart Health initiative: process evaluation of the demonstration phase.http://www.med.mun.ca/chhdbc/pdf/Cvd%20Heart%20Health.pdf Available at: (accessed 19 Jul 2012) [Google Scholar]
- 15.O'Loughlin J., Elliott S.J., Cameron R., Eyles J., Harvey D., Robinson K., Hanusaik N. From diversity comes understanding: health promotion capacity-building and dissemination research in Canada. Promot Educ. 2001;(Suppl. 1):4–8. [PubMed] [Google Scholar]
- 16.Lewis S., Kouri D. Regionalization: making sense of the Canadian experience. Healthc Pap. 2004;5(1):12–31. doi: 10.12927/hcpap.2004.16847. [DOI] [PubMed] [Google Scholar]
- 17.Shortell S.M., Gillies R.R., Anderson D.A., Mitchell J.B., Morgan K.L. Creating organized delivery systems: the barriers and facilitators. Hosp Health Serv Adm. 1993;38:447–466. [PubMed] [Google Scholar]
- 18.Fulop N., Protopsaltis G., Hutchings A., King A., Allen P., Normand C., Walters R. Process and impact of mergers of NHS trusts: multicentre case study and management cost analysis. BMJ. 2002;325:246–249. doi: 10.1136/bmj.325.7358.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Philippon D.J., Braithwaite J. Health system organization and governance in Canada and Australia: a comparison of historical developments, recent policy changes and future implications. Healthc Policy. 2008;4(1):e169–e186. [PMC free article] [PubMed] [Google Scholar]
- 20.Church J., Barker P. Regionalization of health services in Canada: a critical perspective. Int J Health Serv. 1998;28(3):467–486. doi: 10.2190/UFPT-7XPW-794C-VJ52. [DOI] [PubMed] [Google Scholar]
- 21.Astley W.G., Van de Ven A.H. Central perspectives and debates in organization theory. Adm Sci Q. 1983;28(2):245–273. [Google Scholar]
- 22.DiMaggio P.J., Powell W.W., editors. The new institutionalism in organizational analysis. The University of Chicago Press; Chicago, IL: 1991. [Google Scholar]
- 23.Hasenfeld Y., editor. Human services as complex organizations. Sage; Newbury Park, CA: 1992. [Google Scholar]
- 24.Perrow C. Goals and power structures: a historical case study. In: Freidson E., editor. The hospital in modern society. The Free Press; NewYork, NY: 1963. pp. 112–146. [Google Scholar]
- 25.Meyer M.W. Chapter 3: performance and persistence in Organizational Theory. In: Meyer M.W., Zucker L.G., editors. Permanently failing organizations. Sage; Newbury Park, CA: 1989. pp. 45–61. [Google Scholar]
- 26.Hanusaik N., O'Loughlin J., Kishchuk N., Paradis G., Cameron R. Organizational capacity for chronic disease prevention: a survey of Canadian public health organizations. Eur J Public Health. 2010;20(2):195–201. doi: 10.1093/eurpub/ckp140. [DOI] [PubMed] [Google Scholar]
- 27.Picard A. May 25, 2011. Is tobacco control no longer a federal priority? The globe and mail.http://www.theglobeandmail.com/life/health/new-health/andre-picard/is-tobacco-control-no-longer-a-federal-priority/article2034642/ (accessed 21 Sep 2011) [Google Scholar]
- 28.Physicians for a Smoke-Free Canada . April 6, 2004. News releases: Health Groups to Prime Minister: cuts to tobacco control programme threaten public health.http://www.smoke-free.ca/eng_home/news_press_April6-04.htm (accessed 18 Oct 2011) [Google Scholar]
- 29.Gore D., Kothari A. Social determinants of health in Canada: are healthy living initiatives there yet? A policy analysis. Int J Equity Health. 2012;11:41. doi: 10.1186/1475-9276-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Chief Public Health Officer's report on the state of public health in Canada. 2008. http://www.phac-aspc.gc.ca/cphorsphc-respcacsp/2008/cpho-aspc01-eng.php [Google Scholar]
- 31.Strategic review of health inequalities in England Post-2010 (The Marmot Review). http://www.instituteofhealthequity.org/.
- 32.Raphael D., Curry-Stevens A., Bryant T. Barriers to addressing the social determinants of health: insights from the Canadian experience. Health Policy. 2008;88:222–235. doi: 10.1016/j.healthpol.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 33.Bambra C., Gibson M., Sowden A., Wright K., Whitehead M., Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. JECH. 2010;64:284–291. doi: 10.1136/jech.2008.082743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Collaborating Centre for Determinants of Health . National Collaborating Centre for Determinants of Health, St. Francis Xavier University; Antigonish, NS: 2010. Integrating social determinants of health and health equity into Canadian Public Health Practice: environmental scan 2010. [Google Scholar]
- 35.Alvaro C., Jackson L.A., Kirk S., McHugh T.L., Hughes J., Chirop A. Moving governmental policies beyond a focus on individual lifestyle: some insights from complexity and critical theories. Health Promot Int. 2011;26(1):91–99. doi: 10.1093/heapro/daq052. (Epub 2010 Aug 13) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Collaborating Centre for Determinants of Health . National Collaborating Centre for Determinants of Health, St. Francis Xavier University; Antigonish, NS: 2012. Bridging the gap between research and practice: building leadership competencey in public health – taking advantage of changes in health delivery in Québec. [Google Scholar]
- 37.Health Canada . Health Canada; Ottawa, ON: 2002. Canada's physical activity guide for children. Publication H39-611/2002-2E; 4. [Google Scholar]
- 38.Health Canada . Health Canada; Ottawa, ON: 2002. Canada's physical activity guide for youth. Publication H39-611/2002-1E. [Google Scholar]
- 39.Contandriopoulos D., Brousselle A. Reliable in their failure: an analysis of healthcare reform policies in public systems. Health Policy. 2010;95(2–3):144–152. doi: 10.1016/j.healthpol.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 40.Evans R.G. Fellow travelers on a contested path: power, purpose, and the evolution of European health care systems. J Health Polit Policy Law. 2005;30(1–2):277–293. doi: 10.1215/03616878-30-1-2-277. [DOI] [PubMed] [Google Scholar]
- 41.Meyer M.W., Zucker L.G., editors. Permanently failing organizations. Sage; Newbury Park, CA: 1989. [Google Scholar]
- 42.Podsakoff P.M., Organ D.W. Self-reports in organizational research: problems and prospects. J Manag. 1986;12(4):531–544. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.