Abstract
The ongoing Ebola epidemic in West Africa has drawn attention to global health inequalities, in particular the inadequacies of health care systems in sub-Saharan African countries for appropriately managing and containing infectious diseases. The purpose of this article is to examine the sociopolitical and economic conditions that created the environment for the Ebola epidemic to occur, identify challenges to and opportunities for the prevention and control of Ebola and future outbreaks, and discuss policy recommendations and priority areas for addressing the Ebola epidemic and future outbreaks in West Africa. Articles in peer-reviewed journals on health system reforms in developing countries and periodicals of international organizations were used to gather the overview reported in this article. We identify individual, structural, and community challenges that must be addressed in an effort to reduce the spread of Ebola in West Africa. The Ebola epidemic in West Africa underscores the need for the overhaul and transformation of African health care systems to build the capacity in these countries to address infectious diseases. Public-private partnerships for investment in developing countries' health care systems that involve the international community are critical in addressing the current Ebola epidemic and future outbreaks.
Keywords: Ebola epidemic in West Africa, Health care systems in sub-Saharan Africa, Global health, Health systems improvement
Introduction
In December 2013, a reported unknown contagious and lethal illness started with a young boy in Guéckédou, Guinea—a town well-known for the presence of West African traders from Guinea, Sierra Leone, Liberia, and Côte d'Ivoire. The disease, which caught health officials in the region off guard, was soon identified as the Ebola virus disease (EVD), a disease with a case fatality rate of 90% (Heymann, 2015). The Ebola epidemic wreaking havoc in West Africa has led to a global ripple effect that has affected the United States and other Western countries. In the absence of a vaccine or treatment for Ebola, the disease has alarmed the global public health community and caused panic among some segments of the population. The fear associated with Ebola, a deadly disease that respects no borders or socioeconomic status, has captured the attention of the global health community (Baden et al., 2014). Although Ebola has been around since 1976 (Piot, 2012), with past outbreaks contained in Uganda and Congo, many people do not have the knowledge of how the disease is contracted and spread, and, thus, fears and myths continue unabated.
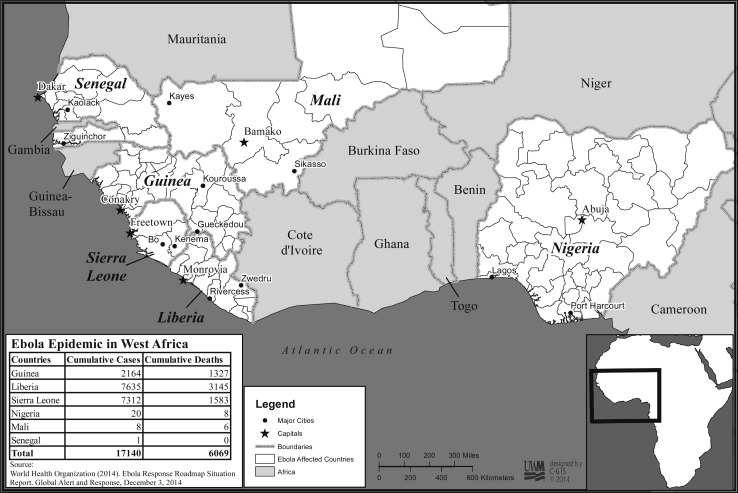
At the time of this writing, according to the World Health Organization (WHO), worldwide a total of 17,145 cases of EVD have been reported in five affected countries (Guinea, Liberia, Mali, Sierra Leone, and the United States) and three previously affected countries (Nigeria, Senegal, and Spain) up to November 30, 2014. Globally, there have been 6,070 reported deaths (WHO, 2014a). Liberia, Sierra Leone, and Guinea remain the epicenter of the disease. As of November 30, 2014, WHO reports 2,164 cumulative cases and 1,327 deaths in Guinea; 7,635 cumulative cases and 3,145 deaths in Liberia; and 7,312 cumulative cases and 1,583 cumulative deaths in Sierra Leone. Among the three countries at the epicenter of the disease, 17,111 cumulative cases and 6,055 cumulative deaths have been reported (WHO, 2014a). Although the number of new cases is reported to be stabilizing, the situation in these countries remains uncertain, with no treatment in sight. A map of countries at the epicenter of the Ebola epidemic in West Africa is displayed in Figure 1 .
Figure 1.
A Map of countries at the epicenter of the Ebola epidemic in West Africa.
Ebola has tested the readiness of health care systems around the world. The disease has especially drawn attention to the inadequacies of sub-Saharan African countries' health care systems and the lack of health care infrastructures to handle complex health emergencies in low-resourced, developing country settings. Because Ebola is an unprecedented disease that threatens the global community, international health agencies and the private sector are in a race with time to develop appropriate medications and potential vaccines to treat and prevent the disease. Although the advancement of such solutions is paramount, it is important to look beyond the current epidemic by examining factors that have led to such inefficiencies in the affected countries' health care systems.
All three affected countries are emerging from civil wars, which has resulted in low levels of the availability of health resources and dysfunctional health care systems, largely resulting from the lack of adequately trained and available health care workers. Sub-Saharan Africa accounts for 24% of the global burden of disease but with only 3% of the world's available health workforce (World Bank, 2013). Even before the Ebola outbreak, as democracy was being re-embraced in these countries, health care providers were overwhelmed with meeting system-wide needs and developing postwar capacities while economic growth and redevelopment were occurring. It is pertinent, then, to examine the challenges and opportunities for addressing the Ebola epidemic in the affected countries and propose strategies for strengthening these countries' health systems.
Although the governments of the affected countries have worked to improve the economy and health status of their populations, life expectancy across this region remains low. Physician and hospital bed capacities are dismally inadequate from a comparative global perspective, minimally meeting the basic health care needs of the general population. Infant and maternal death rates remain high. Because of high levels of illiteracy, it becomes difficult to disseminate uniform health messages. Economic and health-related information of the affected countries is displayed in Table 1 .
Table 1.
Health, Economic, and Social Characteristics of West African Countries at the Epicenter of Ebola Epidemic
| Selected Indicators | Guinea | Sierra Leone | Liberia |
|---|---|---|---|
| Total population | 11,474,383 | 5,743,725 | 4,092,310 |
| Death rate (deaths per 1,000 population) | 9.69 | 11.03 | 9.9 |
| Maternal mortality rate (deaths per 100,000 live births) | 610 | 890 | 770 |
| Infant mortality rate (deaths per 1,000 live births) | 610 | 73.29 | 69.19 |
| Life expectancy at birth (in years) | 59.6 | 57.39 | 58.21 |
| GDP (purchasing power parity) | $12.56 billion | $9.16 billion | $2.89 billion |
| Health expenditures (% of GDP) | 6 | 18.8 | 19.5 |
| Physician density: number of physicians (per 1,000 population) | 0.1 | 0.02 | 0.01 |
| Number of hospital beds (per 1,000 population) | 0.3 | 0.4 | 0.8 |
| Percent of pop with access to clean drinking water | 73.6 | 57.5 | 74.4 |
| Percent of pop with access to sanitation facilities | 18.5 | 12.9 | 18.2 |
| HIV/AIDS: adult prevalence rate (%) | 1.7 | 1.5 | 0.9 |
| Education expenditures (% of GDP) | 2.5 | 2.9 | 2.8 |
| Literacy rate (for total population) (%) | 41 | 43.3 | 60.8 |
| Literacy rate (males) | 52 | 54.7 | 64.8 |
| Literacy rate (females) | 30 | 32.6 | 56.8 |
GDP, gross domestic product (spending purchasing power parity of a country).
Source: The World Fact Book (2014). Retrieved from: https://www.cia.gov/library/publications/the-world-factbook/.
Public health infrastructure in the region lacks even the rudimentary armaments to wage battle against an enemy such as Ebola (Forrester et al., 2014). Because the dire necessity in West Africa is so immense, opportunities to make a difference are many for American health care professionals, including nurses, individually and collectively. A critical factor lacking in the fight to address the current Ebola outbreak in West Africa is the absence of better delineation of contextual factors that serve as challenges to mitigating the spread of the disease. What are the individual, structural, and community factors that impede efforts to address Ebola in the West African countries at the epicenter of the epidemic? Also, despite the devastating effect of the disease on populations, the Ebola epidemic should be viewed as an opportunity for reorienting health care delivery systems and building countries' capacities at a level such that they are capable of addressing new and future outbreaks of Ebola-like infectious diseases in sub-Saharan Africa.
Purpose
The purpose of this article is to (a) critically examine the sociopolitical and economic conditions that created the environment for the Ebola epidemic to occur, (b) identify challenges to and opportunities for the prevention and control of Ebola and future outbreaks, and (c) discuss policy recommendations and priority areas for addressing the Ebola epidemic and future outbreaks in West Africa.
Methods
Our approach is guided by the use of literature in peer-reviewed journals on disease burden and health system reforms in developing countries, specifically in sub-Saharan West African countries. Periodicals released by international organizations, including the United Nations Development Program, WHO, United States Agency for International Development, and the World Bank, on global health challenges were also relied on to critically examine the health, sociopolitical, and economic conditions and to identify the priority and policy areas discussed in this article. Building on the policy analysis work of de-Graft Aikins, Boynton, and Atanga (2010), the structural psychology work of Hepworth (2004), and the antiretroviral adherence analysis work of Kagee et al. (2011), we extrapolated from these prior works to critically examine the challenges and opportunities that, if understood and addressed, can effectively contribute to halting the spread of Ebola and potential infectious diseases specific to the West African setting.
Findings
In this section, we organize and discuss findings from our analysis with a focus on personal-/individual-, structural-/organizational-, and community-level challenges that must be addressed in an effort to reduce the spread of the disease in West Africa. Although many view the disease primarily from a problem-based perspective, we contend that there are multiple opportunities for the prevention and control of Ebola and future infectious disease outbreaks in the West African setting. We maintain that, as with most controversial health and social issues, embracing a community-based, participatory approach in which key members of the public participate in decision making on how to mitigate the impact of Ebola on their communities would be a viable approach. Such approaches should also focus on the assets and resiliency of local health care workers and the affected populations.
To fully accomplish this participatory approach, trust by the local people of their government officials and health care workers will be pivotal. Therefore, a combination of centralized “top-down” and decentralized “bottom-up” approaches is proposed, as is the need to include trust-building capacities in order to work effectively (Chowdhury, 2012). In the case of the Ebola epidemic in West Africa, the use of the bottom-up approach (i.e., an empowerment model that creates opportunities for public health frontline workers to engage leaders and members of local communities to discuss factors surrounding the disease) is essential. Within the context of the bottom-up approach, community leaders are regarded as important stakeholders and knowledge reservoirs in contributing positively to programs that embrace and represent the values of their community members. The bottom-up approach has been used in several developing countries in designing effective primary health care programs (Chowdhury, July 2012, Magnussen et al., 2004). Thus, combining an array of individual-, structural-, and community-level factors directed at curtailing the Ebola epidemic in West Africa is essential.
Challenges to the Prevention and Control of Ebola in Affected West African Countries
Personal/Individual-Level Challenges
Entrenched Poverty and Food Insecurity
Barriers at the personal level affect individuals; people and their families may or may not be able to exercise control over their actions. For instance, the number of people in sub-Saharan Africa who live on incomes between $1.25 U.S. dollars to $2.00 U.S. dollars per day is disproportionately high compared with other regions of the world (World Bank, 2013). This extreme poverty causes individual resource scarcity, overcrowding, and rampant sharing of the basic amenities needed for survival. Many in the affected African countries go without bare necessities including food, water, sanitation, and shelter. Thus, Ebola is bound to adversely affect the poorest of individuals—those displaced during civil conflicts in these three countries and now living in urban slums.
Fear, Perceptions of Risk, and Social Stigma
Infectious diseases such as Ebola set in motion psychological responses including fear and stigma (Kinsman, 2012). Social stigma as a response to a disease is not a new phenomenon. Historically, the following infectious diseases are associated with a stigma: influenza, tuberculosis, HIV/AIDS, and severe acute respiratory syndrome (Barrett and Brown, 2008, Kinsman, 2012).
Limited Access to Modern Health Care
Limited access to modern health care services is an important challenge. Even before the Ebola outbreak, access to basic primary health care services was a major challenge to good health in the affected African countries. Access to early supportive care is pivotal for individuals suspected of being infected with Ebola. With interventions from the U.S. military and other international organizations, the number of Ebola treatment units has increased in Liberia. Unfortunately, because of the lack of transportation and limited ambulance services, individuals in some affected areas may not have access to needed supportive care—care that would increase their chance for survival.
Cultural Mores and African Traditional Belief Systems
Finally, how cultural practices and traditional African belief systems influence the prevention and control of Ebola must be considered in the fight against the Ebola epidemic in West Africa. Unlike the Western paradigm of disease, which is based on objectivity, the African concepts of disease are heavily influenced by mystical factors, the community, and the universe (Cheetham & Griffifths, 1982). Beliefs in witchcraft, religion, and ancestral spirits as reasons for being ill are common among many Africans (Chukwuneke, Ezenonu, Onyire, & Ezenonu, 2012). Western headlines have been filled with stories of sorcery, illusion, and curse as reasons for some families being decimated by Ebola.
Structural/Organizational Health System–level Challenges
Structural factors are those institutional and organizational health systems challenges that are caused in part by how health care in the countries are organized, financed, and delivered to the population. For instance, are the governments adequately funding health care in these countries? Although individual-level factors are essential for the prevention and containment of Ebola, structural-level factors are also critical.
Countries Emerging from Civil Conflicts
Structurally, all the countries at the epicenter of Ebola are emerging from civil conflicts with dysfunctional, fragile health systems. For instance, in Liberia, cultural, economic, educational, and health initiatives were all halted, with the exception of few international organizations providing health care to the general population (Buseh, 2008). Rebels went on a rampage, looting and destroying clinics and hospitals. Many trained health care workers were killed and/or fled the country and have not returned. Health care systems in these countries remain fragile, and government spending on health care remains low. Ebola has exacerbated the problems of these fragile systems.
Endemic Multimorbidities and Competing Health Priorities
All the countries affected by Ebola also experience endemic multimorbidities with competing health priorities. In sub-Saharan Africa, infectious and noninfectious diseases (both emergent and re-emerging) continue to affect a large proportion of the population (Boutayeb, 2006). The West African region is ripe for the coexistence of multiple health problems (e.g., very high infant and maternal mortality rates) as shown in Table 1. Diseases that affect mostly the poor in many sub-Saharan African countries—referred to as neglected tropical diseases (parasitic worm infestations, schistosomiasis, river blindness, and so on)—continue to persist (Boutayeb, 2006). The multimorbidity of diseases found in the region puts an extra strain on the health care systems of these countries with inadequate budgets.
Poor Public Health Infrastructure
Structurally, countries in the West African region lack the public health infrastructure for managing infectious disease outbreaks (Boozary et al., 2014). In the affected countries, there is limited disease surveillance in place, and almost all health centers constantly face logistical issues. Ebola warrants full occupational protection, with the use of special equipment and clothing when caring for patients. However, even before the Ebola outbreak, there was a dearth of medical equipment and supplies in the affected countries. The lack of supplies and the reuse of equipment serve to increase the risk for medical staff, thus the unprecedented high number of cases and deaths from Ebola among health care workers in the affected countries.
Community-level Challenges
Although individual- and structural-level factors are essential for the prevention and containment of the Ebola epidemic in West Africa, understanding the community-level factors is also essential. Individuals and institutions exist in communities. Many African societies and cultures pride themselves on a communal approach to health and survival. Thus, there is a synergistic effect between individuals and communities. When an increased number of individuals contract Ebola in a certain community, this can have an adverse effect on the well-being of that community at large. Several factors determined as pivotal community-level challenges to the prevention and control of Ebola are discussed later.
Porous Borders and Geographic Boundaries
In the West African region, borders are porous and contiguous, and, thus, conditions are ripe for the disease to spread rapidly from one country to another. For many West Africans, the border is just an imaginary boundary; movements between countries are fluid and constant. For instance, it is very common for individuals living in Guinea to have family members living in Liberia or Sierra Leone and for people across the region to speak similar languages and/or belong to the same tribe.
Mistrust of Government and Modern Health Care Services
Deep distrust of government and government health services exists in many sub-Saharan African countries. The mistrust of government in this region is especially pervasive in countries that have endured civil conflicts and for decades have suffered lies and deceit from their leaders. Trust is a critical component of public health because trust influences how people and a community respond to public health interventions and messages during complex emergencies (Meredith, Eisenman, Rhodes, Ryan, & Long, 2007).
Clash of Ethnomedicine with Biomedicine
The Ebola epidemic in West Africa has also revealed not only the inadequacies of modern health care systems in the affected countries but also the clash of biomedical systems with African traditional healing systems. In all sub-Saharan African countries, both systems exist in parallel and are not integrated. African traditional healing practices have existed for hundreds of years. For many individuals, especially in rural settings, their first line of health care is an African traditional healer. It is common for family members to seek health care from a traditional healer before finally seeking health care at a clinic or hospital. These ethnomedical practices are highly popular, have been used for centuries, and continue to be used in the treatment of both noninfectious and infectious diseases, including HIV/AIDS (Chinsembu, 2009). In the absence of treatment or an efficacious vaccine for Ebola, it is understandable that many individuals in the region have turned to African traditional healers for help.
Opportunities for Prevention and Control of Ebola and Future Outbreaks in West Africa
Although much of the information seen in the media has centered on the lethal nature of Ebola and its potential for rapid spread to Western countries, this type of narrative only reinforces existing global health inequities. Instead of viewing the Ebola epidemic in West Africa only from a problem-based perspective, it should be viewed through another lens, as is the case with the HIV/AIDS epidemic, which is now viewed as an opportunity for addressing global public health threats. At a minimum, in the age of international travel and commerce, diseases can spread very easily from one setting to another. There are several essential areas that can serve as opportunities for addressing the Ebola epidemic and future infectious disease outbreaks in sub-Saharan Africa.
Creation of a Family-centered Response to Outbreaks
Ebola not only affects an individual, but it also affects the families of persons with the disease. Once a family member contracts Ebola, the chance of other family members contracting the disease increases. Thus, developing a family-centered approach to curtail the spread of the disease is essential. Lessons could be learned from the HIV/ADS epidemic in which embracing a family-centered approach to caring for individuals has been hailed as effective in the management and prevention of HIV infection (DeGennaro & Zeitz, 2009).
Community Engagement and Social Mobilization Around Infectious Diseases
It is particularly important to start the dialogue with community leaders and elders. African societies, especially in rural areas, are hierarchical in structure, and, thus, intervention aimed at finding lasting solutions to issues affecting communities at large must usually get the endorsement of the community leaders. In the prevention of Ebola, the use of good public health principles through incorporating community participation is essential. In a study exploring the value of community participation in disease surveillance in Niger, investigators found that the quality of surveillance on guinea worm control campaigns improved when community leaders were involved (Ndiaye, Quick, Sanda, & Niandou, 2003). Community leaders will be more effective in mobilizing their people around the efforts being promoted by the ministries of health and international organizations.
Development of Public-private Partnerships (Regional and International) for Infectious Disease Control
The Ebola epidemic is a public health problem that is difficult to address solely by one country. Governments in the affected countries do not have the capacity for delivering full and needed services to all people. Thus, the international community should assume some role in shoring up the affected countries' systems. Governments in the affected region constantly face competing needs and priorities and sometimes become easily distracted from daily governance and service provisions when large issues, such as an Ebola outbreak, can easily overwhelm the already fragile systems (Ross, 2013). However, the sovereignty of the affected countries must continue to be respected even as the international community partners address the Ebola epidemic. The international community will do harm if the public perceives that their governments are inefficient in providing basic health services.
Public-private Partnerships in the Area of Research and Development for Discovery of Vaccines and Drugs
Although the Ebola outbreak in West Africa is unprecedented, this outbreak gives the international community an opportunity to work together to figure out ways to address infectious diseases in resource-poor settings, such as researching, developing, and testing possible vaccines and treatment. Thus far, there is no known drug or vaccine that can be used safely in human populations for the prevention and treatment of Ebola. Some promising agents are being developed by several companies, including GlaxoSmithKline. The National Institutes of Health is also working on an Ebola vaccine. Although there is an urgency to develop treatment and vaccines, clinical trials must be designed and conducted under straight ethical guidelines, balancing any potential harm against potential benefits accrued by the affected populations.
Discussion
Several explanations are gleaned from the analyses of the Ebola epidemic in West Africa and reported in this article. First, Ebola is being presented as a fatal disease that spans global boundaries and has now spread to several Western countries, including the United States. Second, public health officials cannot afford to be complacent about the emerging and re-emerging infections. During the last 2 decades, the public health community has witnessed a series of emerging and re-emerging infections (e.g., subacute respiratory tract infection, avian flu, H1N1, the Middle East Respiratory Syndrome, and now Ebola in West Africa), all of which have put the global public health community on high alert. A third perspective is that when infectious disease outbreaks occur in developing countries, these countries are unlikely to have adequately resourced and staffed health care facilities capable of addressing the spread of the disease and managing those who are already infected. International agencies should review existing pandemic plans in an effort to increase their efforts to control outbreaks in the future. Could the Ebola outbreak in West Africa be a prelude to bigger outbreaks to come, potentially a different type of virus, maybe a more lethal virus and one spread via the airborne route?
Although we used a problem-based perspective in presenting the challenges of addressing the Ebola epidemic in West Africa, we are in no way neglecting the strengths and resilience of the affected countries. Health care professionals in the United States, including nurses who have returned from working in the West African region, could be excellent sources of ideas about how nurses and other health care professionals in the United States can become more engaged in addressing the epidemic in West Africa. A good place to start would be for health care workers to understand that although these populations in West Africa are vulnerable to disease, poverty, and other adversities, they are also very resilient. Thus, in the following section, we briefly discuss the strengths of the general population and health care workers in the West African setting.
Ebola and the Resiliency of Populations in the Affected West African Countries
Although Ebola has been raging since March 2014 in West Africa, it was not until mid-August that the disease began to make headline news in the United States when two Americans working at a hospital in Liberia contracted the virus and had to be flown back to the United States. Since then, the news coming out of West Africa has continued to be bleak, almost entirely focused on the Ebola epidemic, with the potential for spreading and more deaths to occur. Sometimes the news seems sensationalized, presenting a doomsday scenario that entire populations will be decimated if nothing is done to halt the disease. Yet, the countries at the epicenter of the disease (Liberia, Guinea, and Sierra Leone) are no strangers to tragedies. For instance, in the 1990s, civil conflicts erupted in both Liberia and Sierra Lone—senseless wars that led to hundreds of thousands of lives lost. Today the conflicts in these countries are over, and almost every Liberian, whether they were in Liberia during the active conflict or abroad, has some painful story to tell.
Historically, although much research has stressed the emotional deficits and vulnerabilities of populations in sub-Saharan Africa, less research has illustrated their strengths, resources, and resilience (Almedom, 2009). Black people around the world and as a racial group have thrived in the wake of traumatic experiences (Bryant-Davis, 2005). Although the media in the United States is fraught with news about Ebola coming to the United States and the panic calls from some politicians to close the borders and not allow West Africans from the three most affected countries to enter the United States, Africans in the affected countries continued to scramble for resources in an effort to survive daily. Generally speaking, Africans are a resilient people. As the international community continues to work on addressing the Ebola epidemic in West Africa, we must not lose sight of the strength and will of the affected populations to survive in these countries despite the meager economic and health resources available, in particular considering their histories of suffering colonial injustices and their experiences of racial bias.
Even when access to modern health care may be impossible, African communities use communal approaches in devising ways to address their own problems when tragedies emerge in their communities instead of waiting for people from the outside to rescue them. Although many Africans increasingly embrace the Western way of life, they are also highly spiritual, relying heavily on traditions, rituals, and the spiritual guidance of their ancestral spirits for day-to-day survival (Some, 1999). Their ability to navigate both Western and African traditional healing systems is an asset that should be embraced.
Like most of sub-Saharan Africa, in the West African Ebola-affected countries, there are many factors that increase the population's vulnerabilities to disease, not the least of which is poverty. In a review of the literature on the construct of vulnerability, poverty, and health in sub-Saharan African populations, many of the studies focused mostly on the deficits of the populations, with limited or no attention paid to the assets and resiliency of local populations that have sustained them for centuries (Almedom, 2009). However, in an issues brief examining health and social systems, Almedom (2009) argues that focusing on the observed weaknesses of systems of African countries overshadows the real and potential strengths that need to be harnessed for the development of community discourse around critical health and social issues. Because resilience is a dynamic process, it will be important to explore factors that lead to the endurance and resiliency of West Africans during complex emergencies, as is the case now of the Ebola epidemic. As Almedom (2009) sums up, “Focusing on the strengths of formal and informal African institutions so far has served to understand the dynamics of adaptive processes that sustained lives and livelihoods” (p. 6).
Still, the pestilence of Ebola, which has killed thousands, destroyed families, and created orphans, has crippled not only the health care systems of these countries but also their economies, in particular the educational and agricultural sectors. Schools remained closed, many marketplaces are closed, and farming activities have decreased or halted in some regions. Many are confused and fearful about what is happening. Some are angry that the international community was painfully slow to respond to the epidemic. Many people, however, are enduring the disease with the same resignation as they did when faced with challenges during the civil war and other adversities. Ebola too will end regardless of how long it takes to mitigate the spread of the disease. Populations in the affected countries are coming to terms with the Ebola epidemic and increasingly learning about its seriousness; they are doing everything they can to protect themselves and their families from contracting the disease. Although the epidemic is reported to be stabilizing, the disease is far from over.
Liberian Head of State and Nobel Peace Prize winner President Ellen Johnson Sirleaf explained the situation on October 19, 2014, in a “letter to the world” broadcast on the British Broadcasting Corporation News Hour.
Dear World,
… Ebola has managed to bring my country to a standstill… . There is no coincidence Ebola has taken hold in three fragile states – Liberia, Sierra Leone and Guinea – all battling to overcome the effects of interconnected wars … the war destroyed our public infrastructure, crushed our economy and led to an exodus of educated professionals. A country that had some 3,000 qualified doctors at the start of the war was dependent by its end on barely three dozen … Ebola is not just a health crisis—across West Africa, a generation of young people risk being lost to an economic catastrophe as harvests are missed, markets are shut and borders are closed … The time for talking or theorizing is over (Sirleaf, 2014).
Impact of Ebola on Health Care Workers and the Resiliency of Health Care Workers
From the onset of the Ebola epidemic in West Africa, health care workers, including physicians and nurses struggling to defeat the epidemic have in many cases, also became frontline victims of the disease. In many ways, the advent of the Ebola epidemic in West Africa has intensified and broadened the challenges faced by health care professionals, including nurses, working on the frontlines in developing countries. The situation in West Africa is compounded by the lack of health care workers skilled in the prevention and treatment of infectious diseases. Despite the bravery and resilience of the nurses and the efforts of other health care workers in the affected countries, Ebola has threatened the productivity of nurses and led to increased attrition and lower morale. If these structural factors are not addressed, the quality of care for Ebola patients and patients suffering from other conditions could be even further threatened.
According to reports from WHO, the initial infection rates showed how health care workers at the very heart of West Africa's fight against Ebola were adversely affected, many of whom were poorly equipped, poorly paid, and insufficiently prepared and became some of Ebola's immediate causalities (WHO, 2014b). Although the exact numbers of health care workers who have contracted Ebola and who have died from the disease is unknown and inaccurate, Ebola has taken the lives of prominent doctors and nurses in Sierra Leone, Liberia, and Guinea, depriving these countries not only of experienced and dedicated medical care but also of inspirational national heroes (WHO, 2014b). According to WHO, as of the end of November 2014, in countries at the epicenter of the disease, a total of 622 health care workers are known to have been infected with Ebola; 346 of them have died (WHO, 2014a).
Health care workers in the affected countries have cared for patients and their families in difficult health care environments, which in some cases increased their risk of contracting Ebola. These are courageous health care workers; despite not knowing what they were dealing with, most did not run from the challenges. Rather, they faced the EVD head on with bravery and resilience. Despite working in areas with severe workforce shortages, inadequate and dysfunctional facilities, and the propensity to be at increased personal risk for contracting Ebola, health care workers in the affected countries are working tirelessly to save the lives of their people while helping to reduce the spread of the disease.
In Liberia, Dr. Samuel Brisbane, director of the emergency department at Monrovia's John F. Kennedy Memorial Medical Center, was the first Liberian doctor to die in the country's Ebola outbreak. Dr. Brisbane's colleagues, Dr. Josh Mugele from Indiana School of Medicine and Chad Priest from Indiana School of Nursing, paid tribute to him in an essay in the September 2014 edition of The New England Journal of Medicine and in an interview on National Public Radio, saying that Brisbane's death was a “selfless act” because he did not have to treat those patients (Mugele & Priest, 2014).
We believe our friend (Dr. Brisbane) died a good death — as did all the nurses and doctors who have sacrificed themselves caring for patients with this awful disease … He didn't have to be a doctor at that stage of his life. But he kept doing it even though he knew [Ebola] was very contagious and he had a high likelihood of getting it. Dying was a selfless act on his part … I think a good death is not about how you die. It's about the quality of the life you left behind. And that's not an end-of-life discussion. It's a beginning-of-life discussion. (Mugele & Priest, 2014).
In all three countries seriously affected by Ebola, there are many nurses and doctors who have done similar great work and would be considered heroes and heroines in sacrificing their lives in caring for patients with a highly infectious disease—many of whose stories have not been told. We highly applaud all the doctors and nurses in the affected countries who have been working and continue to deal with patient needs that so vastly exceed the resources available in these low-resourced countries. Whether or not we would consider the loss of the lives of hundreds of nurses and doctors fighting the Ebola disease in West Africa a “good death,” probably more relevant questions for nurses and other health care workers in the United States to ponder as we push for global health equity are the following: Why has it taken so long to discover a treatment and/or vaccine for Ebola even after it has been around for over three decades? Are the deaths of health care workers and the general populations in West Africa from Ebola preventable ones? Would a treatment and/or vaccine for Ebola have been discovered a long time ago if wealthy Western populations were affected with such a deadly pestilence?
Policy Recommendations and Priority Areas
As for long-term prospects, Farmer (2014) insists that the formula for success against Ebola and threats like it is to “invest in a comprehensive model of prevention and care for the poor” (p. 38). Without intact public health and health care delivery systems in all countries, little can be done to control outbreaks or offer the chance of recovery to those stricken. Improved clinical care across the world is necessary. Facilities and personnel capable of offering early diagnosis and aggressive supportive care, including fluid resuscitation, electrolyte replacement, and blood products, may be able to increase the survival rate of those with the EVD to 90% (Farmer, 2014).
We provide some of these policy areas that will require efforts from the affected countries, regional West African organizations, and the international community.
Addressing the Socioeconomic Issues of Poverty, Food Security, and Livelihoods Including Improving Access to Clean Water and Sanitation Facilities
People living in poverty are at an increased risk of experiencing deleterious effects from Ebola. Entrenched poverty makes it impractical for families to purchase their food and other supplies in advance and stockpile when quarantine orders are issued by the government. In rural settings, it is reported that famers are no longer engaged in communal farming on as large a scale as before. Without large farms, segments of the population are likely to experience hunger even when Ebola is halted. Providing seeds during the next farming season may be an important policy issue to consider helping address future hunger in the populations of affected countries. The United States Agency for International Development and the World Food Program are scaling up efforts in providing support for individuals receiving treatment in Ebola treatment units, Ebola survivors who are discharged from treatment centers, the families of people infected with Ebola, and communities with widespread transmission (United States Agency for International Development, 2014).
Reorganizing Sub-Saharan African Health Systems
Ebola is a disease that calls for the complete overhaul and transformation of African health systems. The countries affected by the epidemic are all emerging from civil conflicts that had an effect on their health care delivery systems. Although much effort has been made during last 2 decades to build the health care systems in sub-Saharan African countries, the Ebola epidemic in West Africa underscores the need for developed countries and international organizations to provide foreign aid support repairing and building the capacity of nonfunctioning health care systems. As these systems are restructured, they should include resources to strengthen both the provision of basic primary health care as well as to be able to handle infectious disease outbreaks.
Strengthening Transboundary Collaboration and Partnerships Aimed at Addressing Infectious Disease Outbreaks
Viewed within a global context, the current Ebola outbreak in West Africa and future outbreaks will require coordination among the affected countries, governments, and health agencies as well as a myriad of partners dedicated to international health. In addressing this type of epidemic, there are many stakeholders and actors. Thus, coordination may not be clear, and it could be a logistical nightmare to unify resources in the fight against the disease. Addressing Ebola in the affected countries not only includes the involvement of doctors and nurses but also involves issues of transportation, food, medical supplies, and the development of telecommunications networks as well as addressing other logistics.
Application of Information Technology Systems for Identification and Management of Cases
The health care systems in sub-Saharan African countries face serious challenges, including the lack of the technologies seen in the developed countries to aid in the diagnosis and management of diseases. Information technology systems are purported to improve access to care, lower costs, and create efficiencies in the overall system (Cline & Luiz, 2013). In all the countries affected by Ebola, road networks are poor, electricity is limited, and medical records are still kept in the old-fashioned way with papers and folders. As part of the scaling-up process in the fight against Ebola, we propose the development and integration of information technology systems in the affected countries' health systems. Technology can also be used to enhance communication between the central unit of command in charge of coordinating Ebola in capital cities and outlying health care centers in rural villages and towns.
The Role of Nurses in Educating Patients and the Public While Advocating for Relevant Evidenced-based Policies
In many of the affected countries, nurses are frontline workers. Many are trusted and respected members of local communities and thus are considered reliable resources for health management in both formal and informal settings. West African nurses speak the local languages and, thus, can be tasked with providing factual and relevant information inside and outside of their communities about this alarming and disturbing disease. Nurses can help inform the public about what information is necessary for individuals suspected of being exposed to Ebola so they can receive the most prompt and appropriate health care. In the case of the affected countries, nurses can take to the lead to help dispel rumors and address social stigma and common misconceptions that a frightened population may be hearing through news outlets. Community forums can be held in which nurses could provide real-time information and hand out resources.
Development of Multipronged Clinical and Social Sciences Research
Developing multipronged research agendas aimed at addressing Ebola in the region is important. First, scientists' quests to increase our understanding of the epidemiology and pathogenesis of the Ebola virus will help us prevent and manage the disease. Along with such epidemiological research, policy makers should also conduct research aimed at understanding the barriers to addressing Ebola. Whether the current efforts being mounted to address the Ebola outbreak in West African are successful will depend heavily on engagement and collaboration with the people in the affected communities. As far as we know, there are no reports about local populations' beliefs and attitudes about Ebola and what they think about the response efforts from their national governments and international organizations relative to the Ebola outbreak. This is an opportunity to assess the perceptions of those who have the disease as well as those at risk of contracting it, including family members.
This is especially important in the rush to develop effective treatment and a vaccine. In one of the few studies exploring the cultural contexts of a past Ebola outbreak in Northern Uganda, investigators found that indigenous epidemic control measures and some cultural practices (e.g., burial practices) amplified the outbreak (Hewlett & Amola, 2003). Hewlett and Amola conclude that consideration must be given to the narratives of local populations relative to the Ebola outbreak. The population's cultural beliefs and local population characteristics must be taken into account in developing appropriate and accurate targeted messages in conjunction with local community leaders.
Sustained Funding for the Prevention and Management of Infectious Diseases
We have discussed at length the need for the international community to increase investment in strengthening the health care systems of sub-Saharan African countries. This is especially important in countries that are emerging from civil conflicts. Without sustained funding, it will be difficult to bring Ebola under control in the West African region. Globally, much progress has been made by countries around the world in improving the health and well-being of their people in the 20th century. However, disparities continue to persist in the developing countries in sub-Saharan Africa. Ultimately, when viewed from a global health perspective, Ebola is suggestive of the increasing disparity in global health care between developed and developing countries. Only when we are able to have honest conversations and hold our leaders and policy makers accountable will global health issues be made a priority agenda.
Conclusion
In this article, we identified and discussed some critical challenges and opportunities related to the current Ebola epidemic in West Africa. We also proposed specific policy agendas that should be undertaken by the affected countries and the international community. Among the lay public in West Africa and abroad as well as among scientists, uncertainties also persist, and myths about the disease continue to be widespread. It is evident that there are numerous issues to unravel about this disease. The fight to contain this virulent disease has taken on global urgency and is now being viewed through the lens of global public health. Absolute human power is what it will take to control this epidemic. How scientists, policy makers, and health care workers, including nurses, work at disentangling the multicomplex and unknown factors surrounding Ebola will be important in containing this disease as well as future outbreaks.
Scientific advances are being made in the quest for treatment and vaccines. However, in pursuing these advances, it is important to encourage global public health research efforts that combine integrative, top-down and bottom-up approaches to disease prevention and care with consideration of the knowledge and cultural sensitivity of local populations. An integrative approach will go a long way in gaining the trust of those afflicted by Ebola. An integrative approach will also have greater potential for preventing the spread of Ebola to other sub-Saharan African countries. If policy makers become complacent and ignore the interconnected challenges and opportunities outlined and described in this article, they run the risk of seeing current efforts aimed at addressing the spread of the disease reversed. Today, it is Ebola in West Africa; tomorrow it could be another disease in another sub-Saharan African country, Latin America, Asia, or even the United States. How can we risk not preparing and developing measures aimed at addressing these emergencies in advance? More important, do wealthy countries with health resources and public health expertise have any obligation to help stem the tide of this pestilence that is ravaging poor and vulnerable populations in West Africa? Readers can ask these questions, but failure of the global community to jointly and vigorously address the current Ebola epidemic in West Africa by assisting the affected countries to rebuild their health care systems will only serve to contribute to the spread of emerging and re-emerging infectious diseases globally.
References
- Almedom, A. M. (2009). A call for resilience index for health and social systems in Africa. The Frederick S. Pardee Center for the Study of the Longer Range Future, Issues in Brief, No. 10. Retrieved from http://www.bu.edu/pardee/policy-010-resilience-index/
- Baden L.R., Kanapathipillai R., Campion E.W., Morrissey S., Rubin E.J., Drazen J.M. Ebola—An ongoing crisis. The New England Journal of Medicine. 2014;371(15):1458–1459. doi: 10.1056/NEJMe1411378. [DOI] [PubMed] [Google Scholar]
- Barrett R., Brown P.J. Stigma and the time of influenza: Social and institutional responses to pandemic emergencies. Journal of Infectious Diseases. 2008;197(Suppl 1):S34–S37. doi: 10.1086/524986. [DOI] [PubMed] [Google Scholar]
- Boozary A.S., Farmer P.E., Jha A.K. The Ebola outbreak, fragile health systems, and quality as a cure. Journal of American Medical Association. 2014;312:1859–1860. doi: 10.1001/jama.2014.14387. [DOI] [PubMed] [Google Scholar]
- Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Transaction of Royal Society of Tropical Medicine Hygiene. 2006;100(3):191–199. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T. Rowman & Littlefield Publishers, Inc; Lanham, MD: 2005. Thriving in the wake of trauma: A multicultural guide. [Google Scholar]
- Buseh A. University Press of America; Lanham, MD: 2008. Empowering resilience: Improving health care delivery in war-impacted African Countries—A case study of Liberia. [Google Scholar]
- Cheetham R.W.S., Griffifths J.A. Sickness and medicine—An African paradigm. South African Medical Journal. 1982;62(11):954–965. [PubMed] [Google Scholar]
- Chinsembu K.C. Model and experiences of initiating collaboration with traditional healers in validation of ethnomedicines for HIV/AIDS in Namibia. Journal of Ethnobiology and Ethnomedicine. 2009;30(5):1–13. doi: 10.1186/1746-4269-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury, J. (2012). Hacking Health: Bottom-up Innovation for Healthcare. Technology Innovation Management Review, 2(7), 31-35.
- Chukwuneke F.N., Ezenonu C.T., Onyire B.N., Ezenonu P.O. Culture and biomedical care in Africa: The influence of culture on biomedical care in a traditional African society, Nigeria, West Africa. Nigerian Journal of Medicine. 2012;21(2):331–333. [PubMed] [Google Scholar]
- Cline G.B., Luiz J.M. Information technology systems in public sector health facilities in developing countries: The case of South Africa. BMC Medical Informatics and Decision Making. 2013;13:13. doi: 10.1186/1472-6947-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de-Graft Aikins A., Boynton P., Atanga L.L. Developing effective chronic disease interventions in Africa: Insights from Ghana and Cameroon. Globalization and Health. 2010;6:6. doi: 10.1186/1744-8603-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGennaro V., Zeitz P. Embracing a family-centered response to the HIV/AIDS epidemic for the elimination of pediatric AIDS. Global Public Health. 2009;4(4):386–401. doi: 10.1080/17441690802638725. [DOI] [PubMed] [Google Scholar]
- Farmer P. Diary. London Review of Books. 2014;36(20):38–39. [Google Scholar]
- Forrester J.D., Pillai S.K., Beer K.D., Bjork A., Neatherlin J., Massaquoi M., de Cock K. Assessment of Ebola virus disease, health care infrastructure, and preparedness—Four counties, southeastern Liberia. Morbidity and Mortality Weekly Report. 2014;63:1–3. [PMC free article] [PubMed] [Google Scholar]
- Hepworth J. Public health psychology: A conceptual and practical framework. Journal of Health Psychology. 2004;9(1):41–54. doi: 10.1177/1359105304036101. [DOI] [PubMed] [Google Scholar]
- Hewlett B.S., Amola R. Cultural context of Ebola in Northern Uganda. Emerging Infectious Diseases. 2003;9(10):1242–1248. doi: 10.3201/eid0910.020493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann D.L. 20th ed. American Public Health Association; Washington, D.C: 2015. Control of communicable diseases manual. [Google Scholar]
- Kagee A., Remien R.H., Berkman A., Hoffman S., Campos L., Swartz L. Structural barriers to ART adherence in South Africa: Challenges and potential ways forward. Global Public Health. 2011;6(1):83–97. doi: 10.1080/17441691003796387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsman J. “A time of fear”: Local, national and international responses to a large Ebola outbreak in Uganda. Globalization and Health. 2012;8(15):1–12. doi: 10.1186/1744-8603-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnussen L., Ehiri J., Jolly P. Comprehensive versus selective primary health care: Lessons for global health policy. Health Affairs. 2004;23(3):167–176. doi: 10.1377/hlthaff.23.3.167. [DOI] [PubMed] [Google Scholar]
- Meredith L.S., Eisenman D.P., Rhodes H., Ryan G., Long A. Trust influences response to public health messages during bioterrorist event. Journal of Health Communication. 2007;12:217–232. doi: 10.1080/10810730701265978. [DOI] [PubMed] [Google Scholar]
- Mugele J., Priest C. A good death: Ebola and sacrifice. The New England Journal of Medicine. 2014;371:1185–1187. doi: 10.1056/NEJMp1410301. [DOI] [PubMed] [Google Scholar]
- Ndiaye S.M., Quick L., Sanda O., Niandou S. The value of community-participation in disease surveillance: A case study of Niger. Health Promotion International. 2003;18(2):89–98. doi: 10.1093/heapro/18.2.89. [DOI] [PubMed] [Google Scholar]
- Piot Peter. W.W. Norton & Company, Inc.; New York, N.Y: 2012. No time to lose: A life in pursuit of deadly viruses. [Google Scholar]
- Ross J. Ebola outbreak strains West Africa's health workers, systems. Mod Healthcare. 2014, August 7 http://www.modernhealthcare.com/article/20140807/NEWS/308079940 Retrieved from. [Google Scholar]
- Sirleaf, E. J. (2014, October). Liberia: President Sirleaf's letter to the world delivered via the BBC World Service. Retrieved from http://allafrica.com/stories/201410171772.html
- Some M.P. Penguin Putman Press; New York: NY: 1999. The healing wisdom of Africa: Finding life purpose through nature, ritual and community. [Google Scholar]
- The World Bank (2013). The global burden of disease: Main findings for Sub-saharan Africa. Retrieved from http://www.worldbank.org/en/news/feature/2013/09/09/global-burden-of-disease-findings-for-sub-saharan-africa
- The World Fact Book (2014). Retrieved from https://www.cia.gov/library/publications/the-world-factbook/
- United States Agency for International Development. (2014, November). West Africa-Ebola outbreak-fact sheet #8 (FY 15). Retrieved from http://www.usaid.gov/ebola/fy15/fs08
- World Health Organization (2014a). Ebola response roadmap situation report. Global alert and response. Retrieved from http://www.who.int/csr/disease/ebola/situation-reports/en/?m=20141203#
- World Health Organization (2014b). Unprecedented number of medical staff infected with Ebola. Retrieved from http://www.who.int/mediacentre/news/ebola/25-august-2014/en/