Summary
Background
This study was conducted in Kunming, the capital of Yunnan, a poor province in south-west China experiencing rapid economic growth. The study examined the short-term trend in premature mortality burden from common causes of death in a suburban region between 1998 and 2003.
Methods
Years of life lost (YLL) per 1000 population and mortality rate per 100,000 population were calculated from medical death certificates, and broken down by cause of death, sex and year without age weighting but with a discounting rate of 3%.
Results
Non-communicable diseases contributed over 80% of all causes of YLL, with a slightly increasing trend. The combined rate for communicable, maternal, prenatal and nutritional deficiencies declined from 4.7 to 2.4 per 1000 population. Remarkably, declining trends in YLL were also seen for chronic obstructive pulmonary disease, drug use and road traffic accidents, whereas increasing trends were seen for ischaemic heart disease (IHD) and liver cancer (males). The YLL rate for stroke, self-inflicted injuries, lung cancer and stomach cancer fluctuated over time.
Conclusions
The region should focus on further control of IHD and liver cancer.
Keywords: Years of life lost, Premature mortality burden, Temporal trend, China
Introduction
While a descriptive study on disease burden at a single point of time in a given area is useful for planning, it would be more informative to see the dynamics. Few Western studies have reported the association between premature mortality burden and time.1, 2 Relatively little is known in developing countries due to the quality of the vital registration systems.
In China, along with rapid economic growth (per-capita gross domestic product increased at an average of 8.3% per year from 1979 to 2004) and an impressive increase in life expectancy at birth (average life expectancy at birth reached 71.8 years in 2004, compared with 35 years in 1949) over the past decades,3 epidemiological transition of the pattern of disease is well underway.4 However, to the authors’ knowledge, there have been no reports on the actual magnitude of the premature mortality burden since the introduction of a well-organized death registration system.
China has designated certain areas for surveillance of birth and death statistics, in which registration has been enhanced over the past decade. In south-west China, Guan Du district is one of these areas. Guan Du is a suburban region of Kunming, the capital of Yunnan province. China is a multi-ethnic country and has 56 ethnicities. Yunnan province is a multi-ethnic area with 52 ethnic groups, and is one of the poorest provinces in China. This study population is representative of the poor population in China. A computerized death registration system was established in 1998, which is validated for completeness every 3 years in this region. In 2003, Guan Du had a population of 335,622 (178,099 males and 157,523 females), with 17 townships and 157,604 families. The total area was 1025 km2. The major sources of income in this region are grain, vegetables and flowers. The per-capita income among peasants was USD$675.5 From 1998 to 2003, the proportion of the population who were illiterate or semi-literate declined from 15.3% to 6.7%,5, 6 and the per-capita income among peasants increased steadily at an average rate of 13% per year.5, 6 The local government has invested increasing public health expenditure on disease prevention and control, particularly for prevention and curative programmes for specific diseases (tuberculosis, endemic diseases, human immunodeficiency virus/acquired immunodeficiency syndrome, severe acute respiratory syndrome, etc.). Since 1984, an immunization system has been in place in Kunming to immunize and monitor diseases routinely. Kunming has engaged in health promotion through some educational programmes and by establishing smoking-free public areas.
This study was undertaken to examine the short-term trend in premature mortality burden from common causes of death in terms of years of life lost (YLL) in a suburban region of Kunming between 1998 and 2003. This may assist future decisions in health planning for this region.
Methods
Study population
In 1998, the total population in the study region was 307,778 (165,072 males, 142,707 females), and this increased to 335,622 (178,099 males, 157,523 females) by 2003. Migration rates were low; the immigration rate was 0.10 per 1000 population per year (range 0.08–0.11 per 1000), and the emigration rate was 0.11 per 1000 population per year (range 0.10–0.12 per 1000).
Data source
The mortality data for 1998–2003 were based on medical death certificate information, obtained from the Center for Disease Control in Guan Du. In order to avoid misclassification of cause of death, all death certificates were verified on the underlying cause of death by two independent physicians who had been working on death certification for over 20 years. Any discrepancies were reviewed to obtain consensus.
The age and gender breakdown of the population between 1998 and 2003 were obtained from Guan Du statistics office.
Death certificate data were grouped by underlying cause of death, as defined in the Global Burden of Disease (GBD) study.7 The underlying cause of death was coded using International Classification of Diseases (9th revision) codes. Overall mortality in the study region was divided into three broad groups of causes: Group I, communicable, maternal, prenatal and nutritional deficiencies; Group II, non-communicable diseases; and Group III, all injuries. These groups were then further subdivided into more than 100 specific causes of death.7
Calculation of years of life lost
Premature mortality was estimated in terms of YLL. This is one of the methods used to estimate the duration of time lost due to premature death; it is the mortality component of disability-adjusted life years.8
The formula for YLL is:
where K is the age-weighting modulation factor, C is the age-weighting correction constant, r is the discounting rate, a is the age at death, β is a parameter from the age-weighting function, and L is standard life expectancy at age a from the national life table.
In the GBD study, YLL incorporated an age-weighting factor that takes into account the higher social value given to young adults in most societies, and added a discounting factor (social time preference) to reflect the fact that most individuals prefer benefits now rather than in the future. YLL includes age weighting of the form: Cxe −βx, where C is a constant included so that the incorporation of unequal age weightings will not change the total estimated YLL burden, and β is a parameter that controls the shape of the age-weighting function, such that the maximum value of the function is reached at 1/β (for the GBD study, β was assigned a value of 0.04, so that the maximum value is at 25 years of age). When K is set equal to zero, the age weights are equivalent at all ages.
Consistent with the standard GBD approach,7 C was assigned a value of 0.1658 (this parameter controls the maximum height). This study calculated YLL with a 3% discounting rate per year. As China traditionally values living years in elderly and children, age weighting was not used in this study, so K was assigned a value of 0. To maintain comparability with other studies, YLL was calculated using the life tables provided in the GBD study, the model life table, West Level 26.9 In this table, life expectancy at birth is 82.5 years for females and 80 years for males.
Rate calculations
YLL rate per 1000 population and age-specific mortality rate per 100,000 population were calculated using the district population for the particular years. A direct standardization method was used to calculate both age-adjusted YLL and age-adjusted mortality rate to facilitate comparison of different years. The total population for the 6-year study was used as the standard population.
Statistical analysis
Descriptive statistics were used to analyse YLL by cause, sex and year, and to rank the top 10 causes of YLL for 1998–2003. Trend data were plotted on graphs to illustrate annual changes.
Results
In total, 11,533 deaths (6324 males, 5209 females) were registered in this region between 1998 and 2003.
Table 1 shows age-adjusted mortality rates and YLL in the study region for 1998–2003. Both mortality rate and YLL increased between 1998 and 2000, and decreased between 2001 and 2003. The rates were higher in males than females across these 6 years.
Table 1.
Age-adjusted mortality and years of life lost (YLL) by sex and year in a suburban region of Kunming.
| Year | Mortalitya |
YLLb |
||||
|---|---|---|---|---|---|---|
| Male | Female | All | Male | Female | All | |
| 1998 | 625.8 | 623.9 | 622.2 | 86.3 | 85.2 | 86.0 |
| 1999 | 635.8 | 612.6 | 625.0 | 89.9 | 81.6 | 86.2 |
| 2000 | 656.6 | 628.4 | 644.9 | 96.0 | 85.5 | 91.3 |
| 2001 | 590.3 | 579.3 | 585.7 | 84.2 | 81.9 | 83.5 |
| 2002 | 574.4 | 573.9 | 574.2 | 78.1 | 76.4 | 77.8 |
| 2003 | 566.1 | 558.2 | 563.8 | 76.7 | 75.9 | 76.5 |
Age-adjusted per 100,000 population.
Age-adjusted per 1000 population.
Table 2 compares YLL by broad-cause groups and by year. From 1998 to 2003, the rate of Group I conditions was reduced by a half (from 4.7 to 2.4 per 1000 population) and the rate of Group III conditions was reduced by 18.5%. On the other hand, Group II conditions, which accounted for over 80% of the total YLL throughout the observed period, increased by 2.7%.
Table 2.
Mortality burden by cause and year in a suburban region of Kunming.
| Year | Group Ia |
Group IIb |
Group IIIc |
||||||
|---|---|---|---|---|---|---|---|---|---|
| YLL | Age- and sex-adjusted YLL per 1000 population | % | YLL | Age- and sex-adjusted YLL per 1000 population | % | YLL | Age- and sex-adjusted YLL per 1000 population | % | |
| 1998 | 1501 | 4.7 | 5.4 | 22,131 | 66.4 | 80.3 | 3929 | 12.4 | 14.3 |
| 1999 | 1088 | 3.8 | 4.1 | 21,839 | 67.4 | 81.6 | 3871 | 12.3 | 14.3 |
| 2000 | 1052 | 3.6 | 3.9 | 22,103 | 67.5 | 81.9 | 3860 | 12.2 | 14.2 |
| 2001 | 1002 | 3.1 | 3.8 | 22,271 | 67.7 | 82.5 | 3743 | 12.1 | 13.7 |
| 2002 | 870 | 2.7 | 3.5 | 20,921 | 68.0 | 83.3 | 3323 | 10.2 | 13.2 |
| 2003 | 800 | 2.4 | 3.1 | 21,684 | 68.2 | 83.8 | 3424 | 10.1 | 13.1 |
Communicable, maternal, prenatal and nutritional deficiencies.
Non-communicable diseases.
Injuries.
Most of the top 10 causes of death were Group II and Group III conditions (Table 3 ). Chronic obstructive pulmonary disease (COPD), stroke and ischaemic heart disease (IHD) were the top three causes of death in each of the study years, while the ranking of the 10 leading causes of death varied slightly in the same period.
Table 3.
Top 10 causes of age-adjusted years of life lost (per 1000 population) in a suburban region of Kunming, 1998–2003.
| Cause of death | 1998 (rank) | 1999 (rank) | 2000 (rank) | 2001 (rank) | 2002 (rank) | 2003 (rank) |
|---|---|---|---|---|---|---|
| Chronic obstructive pulmonary disease | 17.6 (1) | 17.2 (1) | 16.8 (2) | 15.9 (2) | 15.1 (2) | 14.3 (2) |
| Stroke | 14.7 (2) | 17.1 (2) | 17.4 (1) | 16.7 (1) | 15.4 (1) | 15.4 (1) |
| Ischaemic heart disease | 4.3 (3) | 4.7 (3) | 4.9 (3) | 5.2 (3) | 6.0 (3) | 6.4 (3) |
| Self-inflicted injuries | 3.6 (4) | 4.5 (4) | 3.4 (5) | 4.5 (4) | 3.2 (4) | 3.0 (5) |
| Road traffic accidents | 3.3 (5) | 3.2 (5) | 3.0 (6) | 2.9 (5) | 2.7 (5) | 2.5 (7) |
| Lung cancer | 3.1 (6) | 3.2 (6) | 3.9 (4) | 2.4 (6) | 2.5 (7) | 3.6 (4) |
| Drug use | 2.9 (7) | 2.7 (9) | 2.6 (7) | 2.3 (8) | 1.7 (10) | 1.5 (10) |
| Stomach cancer | 2.4 (8) | 1.6 (8) | 2.1 (9) | 2.4 (7) | 2.4 (8) | 1.8 (8) |
| Liver cancer | 2.3 (9) | 2.2 (7) | 2.2 (8) | 1.8 (9) | 2.6 (6) | 2.6 (6) |
| Other malignant neoplasms | 2.1 (10) | 2.0 (10) | 1.9 (10) | 1.8 (10) | 2.0 (9) | 1.7 (9) |
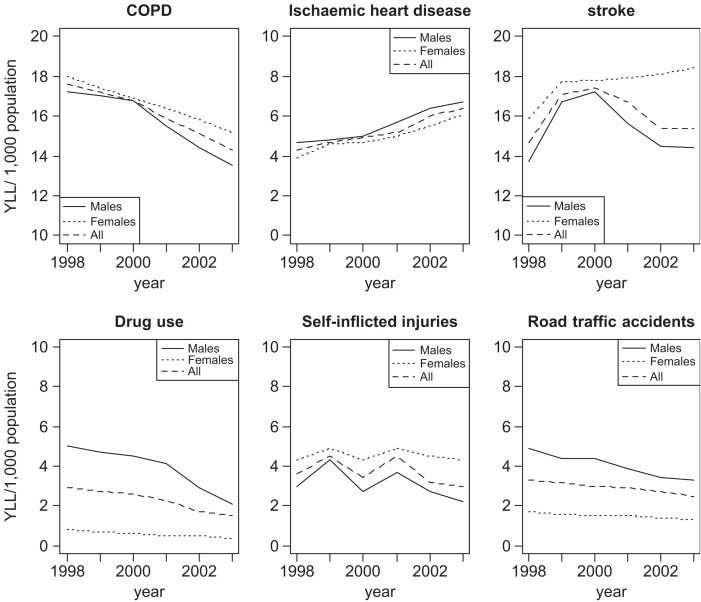
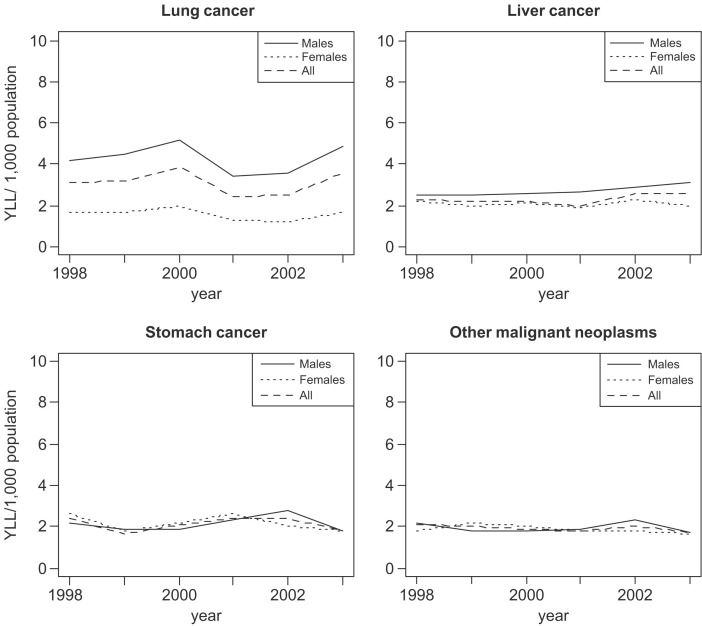
Table 4, Table 5 and Figure 1, Figure 2 should be considered together to determine the trends in these diseases by sex. Among the top three causes of death, COPD showed a steadily declining rate in both sexes (with a sharper decline in males); the steadily increasing trend in IHD was consistent in both sexes with a slightly higher rate in males; and stroke reached its peak in 1999/2000 followed by a decline in males and a slight increase in females. Two (male-dominant) causes of death, drug use and road traffic accidents (RTAs), had a steadily declining trend in males but a less marked decline in females. The mortality burden from self-inflicted injuries was higher among females, although the rates in both sexes fluctuated.
Table 4.
Age-adjusted years of life lost (per 1000 population) by cause of death in a suburban region of Kunming (males), 1998–2003.
| Cause of death | 1998 (rank) | 1999 (rank) | 2000 (rank) | 2001 (rank) | 2002 (rank) | 2003 (rank) |
|---|---|---|---|---|---|---|
| Chronic obstructive pulmonary disease | 17.2 (1) | 17.0 (1) | 16.8 (2) | 15.5 (2) | 14.4 (2) | 13.5 (2) |
| Stroke | 13.7 (2) | 16.7 (2) | 17.2 (1) | 15.6 (1) | 14.5 (1) | 14.4 (1) |
| Ischaemic heart disease | 4.7 (5) | 4.8 (3) | 5.0 (4) | 5.7 (3) | 6.4 (3) | 6.7 (3) |
| Self-inflicted injuries | 3.0 (7) | 4.3 (7) | 2.7 (7) | 3.7 (6) | 2.7 (6) | 2.2 (7) |
| Road traffic accidents | 4.9 (4) | 4.4 (6) | 4.4 (6) | 3.9 (5) | 3.4 (5) | 3.3 (5) |
| Lung cancer | 4.2 (6) | 4.5 (5) | 5.2 (3) | 3.4 (7) | 3.6 (4) | 4.9 (4) |
| Drug use | 5.0 (3) | 4.7 (4) | 4.5 (5) | 4.1 (4) | 2.9 (8) | 2.1 (8) |
| Stomach cancer | 2.2 (9) | 1.9 (9) | 1.9 (9) | 2.3 (9) | 2.8 (9) | 1.8 (9) |
| Liver cancer | 2.5 (8) | 2.5 (8) | 2.6 (8) | 2.7 (8) | 2.9 (7) | 3.1 (6) |
| Other malignant neoplasms | 2.2 (10) | 1.8 (10) | 1.8 (11) | 1.9 (11) | 2.3 (10) | 1.7 (10) |
Table 5.
Age-adjusted years of life lost (per 1000 population) by cause of death in a suburban region of Kunming (females), 1998–2003.
| Cause of death | 1998 (rank) | 1999 (rank) | 2000 (rank) | 2001 (rank) | 2002 (rank) | 2003 (rank) |
|---|---|---|---|---|---|---|
| Chronic obstructive pulmonary disease | 18.0 (1) | 17.4 (2) | 16.9 (2) | 16.4 (2) | 15.8 (2) | 15.2 (2) |
| Stroke | 15.9 (2) | 17.7 (1) | 17.8 (1) | 17.9 (1) | 18.1 (1) | 18.4 (1) |
| Ischaemic heart disease | 3.9 (4) | 4.6 (4) | 4.7 (3) | 5.0 (3) | 5.5 (3) | 6.1 (3) |
| Self-inflicted injuries | 4.3 (3) | 4.9 (3) | 4.3 (4) | 4.9 (4) | 4.5 (4) | 4.3 (4) |
| Road traffic accidents | 1.7 (12) | 1.6 (12) | 1.5 (14) | 1.5 (13) | 1.4 (13) | 1.3 (13) |
| Lung cancer | 1.7 (11) | 1.7 (11) | 2.0 (11) | 1.3 (15) | 1.2 (15) | 1.7 (11) |
| Drug use | 0.8 (27) | 0.7 (29) | 0.6 (28) | 0.5 (30) | 0.5 (31) | 0.4 (32) |
| Stomach cancer | 2.6 (6) | 1.8 (10) | 2.2 (9) | 2.6 (7) | 2.0 (7) | 1.8 (10) |
| Liver cancer | 2.2 (8) | 2.0 (9) | 2.1 (10) | 1.9 (10) | 2.3 (5) | 2.0 (8) |
| Other malignant neoplasms | 1.8 (10) | 2.2 (8) | 2.0 (12) | 1.8 (11) | 1.8 (12) | 1.6 (12) |
Figure 1.
Age-adjusted years of life lost (YLL) due to non-communicable diseases and injuries for 1998–2003. [COPD=chronic obstructive pulmonary disease.]
Figure 2.
Age-adjusted years of life lost (YLL) due to cancers for 1998–2003.
The 6-year study period was probably too short to show any trend in major cancers. Lung cancer and liver cancer were predominated by males. The rate fluctuated for lung cancer but showed a slight upward trend for males. Stomach cancer and other malignant neoplasms had relatively steady rates throughout the study period.
Discussion
Between 1998 and 2003, the mortality burden pattern in the study area did not change to any remarkable extent. This study found that non-communicable diseases have been the major cause of premature mortality in this region, and they have been increasing slowly but steadily. There was predominance of males in overall YLL throughout the study period, although the rates were higher among females for some diseases such as COPD, stroke and self-inflicted injuries. Declining trends in YLL were seen for COPD, drug use and RTAs, and increasing trends in YLL were seen for IHD and male liver cancer. YLL due to stroke, self-inflicted injuries, lung cancer and stomach cancer fluctuated over time.
The finding that non-communicable diseases have been the major cause of premature mortality is consistent with other studies in China,4, 10 as well as studies from other developed and developing countries.11, 12 However, among the communicable diseases, the trends are quite different.
COPD is a major cause of death in this suburban region. In most parts of the world, COPD mortality is still increasing in response to past increases in smoking. It has been estimated that COPD accounts for 35% of all smoking-related deaths.13 Passive exposure to cigarette smoke increases the frequency of respiratory symptoms in adults.14 In the USA, COPD is a leading cause of death,15 and the annual COPD death rate has been increasing over the past 20 years.16 In the UK, male mortality from COPD has been decreasing for 30 years, while female mortality has risen steadily during the same period.17 In Australia, the per-capita mortality burden of COPD has decreased in males but increased substantially in females. The increasing trend in mortality due to COPD in females found in most developed countries18 is partly explained by the increasing numbers of female smokers in the preceding few decades. However, in the present study, premature mortality due to COPD showed a steady decline over time in both males and females. The 1996 national survey in China indicated that the prevalence of smoking was 34.1% (63% in men, 3.8% in women).19 A recent Chinese study indicated that the smoking rate has reduced significantly but was still over 60% in men.20 Kunming has the largest consumption of tobacco in China.21 The decrease in YLL due to COPD indicates that there has been some success in smoking control during the period of economic growth. However, the present study found that females had a slightly higher premature mortality burden due to COPD than males throughout the study period, highlighting the importance of risk factors other than smoking for COPD in women. Cooking indoors with biomass fuel is common in the study region, and women are usually more exposed to this risk factor. The use of solid fuel has also been shown to be an important risk factor for COPD.22 The nature of this additional aetiologic factor needs to be explored further.
This study found an increasing trend in YLL due to IHD, whereas YLL due to stroke fluctuated over time. Deaths due to stroke and IHD have been declining in most developed countries.23, 24, 25, 26 Stroke mortality has been declining in mainland China, Singapore, Hong Kong, Cuba and Japan.27, 28, 29, 30 IHD mortality has declined in Japan but is increasing in China and shows a plateau in Hong Kong.31, 32, 33 The contrast between these two diseases suggests that they have different aetiologies and that the control measures will require different approaches.
This study found that the premature mortality burden due to major cancers (stomach cancer, lung cancer and other malignant neoplasms) fluctuated over time. Liver cancer is one of the leading causes of cancer deaths in Asia. Its mortality had been decreasing in Korea and Japan34, 35 before introduction of mass vaccination against hepatitis B.36 Unfortunately, this study and a previous Chinese study37 found that deaths due to liver cancer had not decreased in China. Similarly, the declining trend in stomach cancer mortality found in most Asian countries between 1950 and 199938 was not seen in this region. Thus, to date, improvements in the Chinese economy have not been followed by an improvement in these two poverty-associated cancers. China may require a longer interval between economic growth and hygienic life style to reduce the transmission of carcinogenic organisms such as hepatitis viruses that cause cancer and helicobacter that leads to stomach cancer.39
RTAs and self-inflicted injuries are important causes of YLL in the study region. In this study, self-inflicted injuries led to more premature deaths in females than males, whereas deaths due to RTAs were more common in males. Most developed countries, such as Sweden40 and Spain,41 exhibit a decreasing trend in RTA mortality, but the trend is increasing in developing countries, such as Thailand42 and China.43 Increased number of motor vehicles, speed, alcohol and a mixture of road users are known risk factors for RTAs in developing countries.44 In China, approximately 70% of RTAs are related to bicycles, and prehospital emergency treatment is an effective method to reduce RTA deaths.45 Despite the fact that economic growth has resulted in more high speed vehicles in China, the reduction in YLL due to RTAs indicates a positive trend in this context.
The trends in premature mortality burden observed in this study only cover a 6-year period. When more data become available, it will be important to see whether the trends persist over a longer period. Migration is a very important factor in determining mortality in some regions of the world.46, 47 The rate was low in this study but may increase in the future and lead to changes in the mortality burden pattern.
In conclusion, while the mortality burden of COPD, drug use and RTAs has decreased in the study region, the burden of IHD is increasing, and the burden of liver and stomach cancer has not decreased in the same way as in more developed Asian countries. As such, these diseases need better control.
Acknowledgements
This study is part of the first author's thesis to fulfill the requirement for a PhD in Epidemiology at Prince of Songkla University. This research was greatly supported by Guan Du Center for Disease Control (CDC). The authors would like to thank Lu Yichun, Head of Guan Du CDC, who helped with the mortality data.
Ethical approval
None sought.
Funding
Yunnan Provincial Natural Science Funds (Grant Number: 2003C0022Q).
Competing interests
None declared.
References
- 1.Gold J., Li Y., Kaldor J.M. Premature mortality in Australia 1983–1992: the first decade of the AIDS epidemic. Med J Aust. 1994;161:652–656. [PubMed] [Google Scholar]
- 2.Nielsen L.C., Hansen K.S., Nielsen U.R. Burden of mortality in Greenland—today and tomorrow. Int J Circumpolar Health. 2004;63(Suppl 2):86–92. doi: 10.3402/ijch.v63i0.17822. [DOI] [PubMed] [Google Scholar]
- 3.National Bureau of Statistics. China statistical yearbook. Beijing: China Statistical Publishing House; 2004.
- 4.Liu D.W., Mou L.H., Tang X.J., Xu H. Analysis on causes of death of townspeople in Chongqin in 1990s. China Public Health. 2002;18:956–957. [Google Scholar]
- 5.Yunnan Province Statistical Bureau. Yunnan statistical yearbook: 2004. Beijing: China Statistics Press; 2005.
- 6.Yunnan Province Statistical Bureau. Yunnan statistical yearbook: 1998. Beijing: China Statistics Press; 1999.
- 7.Murray CJL, Lopez AD. The global burden of disease. Global Burden of Disease and Injury Series. vol. 1. Cambridge, MA: Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996.
- 8.Murray C.J.L. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ. 1994;72:429–445. [PMC free article] [PubMed] [Google Scholar]
- 9.Coale A., Guo G. Revised regional model life tables at very low levels of mortality. Popul Index. 1989;55:613–643. [PubMed] [Google Scholar]
- 10.Xia Y., Gong Y.L., Gu X.Y., Shu B.G. The burden of disease study in Shanghai city. Chin J Health Stat. 2000;17:211–214. [Google Scholar]
- 11.Hyder A.A., Morrow R.H. Applying burden of disease methods in developing countries: a case study from Pakistan. Am J Public Health. 2000;90:1235–1240. doi: 10.2105/ajph.90.8.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mariotti S., D’Errigo P., Mastroeni S., Freeman K. Years of life lost due to premature mortality in Italy. Eur J Epidemiol. 2003;18:513–521. doi: 10.1023/a:1024635401206. [DOI] [PubMed] [Google Scholar]
- 13.Ezzati M., Lopez A.D. Regional, disease specific patterns of smoking-attributable mortality in 2000. Tobacco Control. 2004;13:388–395. doi: 10.1136/tc.2003.005215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaridze D, Peto R, editors. Tobacco: a major international health hazard. IARC Scientific Publication No. 74. Lyon: International Agency for Research on Cancer; 1986.
- 15.Michaud C.M., Murray C.J., Bloom B.R. Burden of disease—implications for future research. J Am Med Assoc. 2001;285:535–539. doi: 10.1001/jama.285.5.535. [DOI] [PubMed] [Google Scholar]
- 16.Wei M., Valdez R.A., Mitchell B.D., Haffner S.M., Stern M.P., Hazuda H.P. Migration status, socioeconomic status, and mortality rates in Mexican Americans and non-Hispanic whites: the San Antonio Heart Study. Ann Epidemiol. 1996;6:307–313. doi: 10.1016/s1047-2797(96)00026-9. [DOI] [PubMed] [Google Scholar]
- 17.Pride N.B., Soriano J.B. Chronic obstructive pulmonary disease in the United Kingdom: trends in mortality, morbidity, and smoking. Curr Opin Pulmon Med. 2002;8:95–101. doi: 10.1097/00063198-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Varkey A.B. Chronic obstructive pulmonary disease in women: exploring gender differences. Curr Opin Pulmon Med. 2004;10:98–103. doi: 10.1097/00063198-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Yang G., Fan L., Tan J., Qi G., Zhang Y., Samet J.M. Smoking in China Findings of the 1996 national prevalence survey. J Am Med A. 1999;282:1247–1253. doi: 10.1001/jama.282.13.1247. [DOI] [PubMed] [Google Scholar]
- 20.Wu Y.F. Current status of major cardiovascular risk factors in Chinese populations and their trends in the past two decades. Chin J Cardiol. 2001;29:74–79. [Google Scholar]
- 21.Rossel S. Marketplace China: Kunming 2004. Tobacco J Int. 2004;5:24–26. [Google Scholar]
- 22.Desai MA, Mehta S, Smith KR. Indoor smoke from solid fuels: assessing the environmental burden of disease at national and local levels. WHO Environmental Burden of Disease Series, vol. 4. Geneva: World Health Organization; 2004.
- 23.Sarti C., Rastenyte D., Cepaitis Z., Tuomilehto J. International trends in mortality from stroke, 1968–1994. Stroke. 2000;31:1588–1601. doi: 10.1161/01.str.31.7.1588. [DOI] [PubMed] [Google Scholar]
- 24.Howard G., Howard V.J., Katholi C., Oli M.K., Huston S. Decline in US stroke mortality: an analysis of temporal patterns by sex, race, and geographic region. Stroke. 2001;32:2213–2220. doi: 10.1161/hs1001.096047. [DOI] [PubMed] [Google Scholar]
- 25.Tobias M., Sexton K., Mann S., Sharpe N. How low can it go? Projecting ischaemic heart disease mortality in New Zealand to 2015. N Z Med J. 2006;119:U1932. [PubMed] [Google Scholar]
- 26.Hu J., Waters C., Ugnat A.M., Horne J., Szuto I., Desmeules M. Trends in mortality from ischemic heart disease in Canada, 1986–2000. Chron Dis Can. 2006;27:89–95. [PubMed] [Google Scholar]
- 27.Venketasubramanian N. Trends in cerebrovascular disease mortality in Singapore: 1970–1994. Int J Epidemiol. 1998;27:15–19. doi: 10.1093/ije/27.1.15. [DOI] [PubMed] [Google Scholar]
- 28.Yu T.S., Tse L.A., Wong T.W., Wong S.I. Recent trends of stroke mortality in Hong Kong: age, period, cohort analyses and the implications. Neuroepidemiology. 2000;19:265–274. doi: 10.1159/000026264. [DOI] [PubMed] [Google Scholar]
- 29.Liu L., Ikeda K., Yamori Y. Changes in stroke mortality rates for 1950 to 1997: a great slowdown of decline trend in Japan. Stroke. 2001;32:1745–1749. doi: 10.1161/01.str.32.8.1745. [DOI] [PubMed] [Google Scholar]
- 30.Cooper R.S., Ordunez P., Iraola Ferrer M.D., Munoz J.L., Espinosa-Brito A. Cardiovascular disease and associated risk factors in Cuba: prospects for prevention and control. Am J Public Health. 2006;96:94–101. doi: 10.2105/AJPH.2004.051417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okayama A., Ueshima H., Marmot M., Elliott P., Choudhury S.R., Kita Y. Generational and regional differences in trends of mortality from ischemic heart disease in Japan from 1969 to 1992. Am J Epidemiol. 2001;153:1191–1198. doi: 10.1093/aje/153.12.1191. [DOI] [PubMed] [Google Scholar]
- 32.Yu T.S., Wong S.L., Lloyd O.L., Wong T.W. Ischaemic heart disease: trends in mortality in Hong Kong, 1970–89. J Epidemiol Community Health. 1995;49:16–21. doi: 10.1136/jech.49.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu X.G. Current prevalent situation and trend on coronary heart disease in Chinese population. Chin J Chron Dis Prevent Control. 2003;4:15–17. [Google Scholar]
- 34.Bae J.M., Jung K.W., Won Y.J. Estimation of cancer deaths in Korea for the upcoming years. J Korean Med Sci. 2002;17:611–615. doi: 10.3346/jkms.2002.17.5.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoshimi I., Sobue T. Mortality trend of liver cancer in Japan: 1960–2000. Jpn J Clin Oncol. 2003;33:202–203. [PubMed] [Google Scholar]
- 36.Zuckerman J.N. Vaccination against hepatitis A and B: developments, deployment and delusions. Curr Opin Infect Dis. 2006;19:456–459. doi: 10.1097/01.qco.0000244051.23511.09. [DOI] [PubMed] [Google Scholar]
- 37.Yang G.H., Wang J.F., Wan X., Wang L.J., Chen A.P. Quantitative analysis of factors affected mortality trend in Chinese, 2002. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:934–938. [PubMed] [Google Scholar]
- 38.Ngoan L.T., Yoshimura T. Pattern and time trends of stomach cancer in Asia from 1950–99. Asian Pac J Cancer Prev. 2002;3:47–54. [PubMed] [Google Scholar]
- 39.Maeda H. Carcinogenesis via microbial infection. Gan To Kagaku Ryoho. 1998;25:1474–1485. [PubMed] [Google Scholar]
- 40.Ekman R., Svanstrom L., Langberg B. Temporal trends, gender, and geographic distributions in child and youth injury rates in Sweden. Inj Prev. 2005;11:29–32. doi: 10.1136/ip.2003.005074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Redondo Calderon J., Luna Del Castillo J.D., Jimenez Moleon J.J., Lardelli Claret P., Galvez Vargas R. Trends in traffic accident mortality in Spain, 1962–1994. Gac Sanit. 2000;14:7–15. doi: 10.1016/s0213-9111(00)71423-3. [DOI] [PubMed] [Google Scholar]
- 42.Sintuvanich A. The impact of industrialization on road traffic accidents in Thailand. J Med Assoc Thai. 1997;80:631–635. [PubMed] [Google Scholar]
- 43.Yang G.H., Zhou M.G., Huang Z.J., Wang L.J. Study on the trend and disease burden of injury deaths in Chinese population, 1991–2000. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:193–198. [PubMed] [Google Scholar]
- 44.Hazen A., Ehiri J.E. Road traffic injuries: hidden epidemic in less developed countries. J Natl Med Assoc. 2006;98:73–83. [PMC free article] [PubMed] [Google Scholar]
- 45.Wang Z., Jiang J. An overview of research advances in road traffic trauma in China. Traffic Inj Prev. 2003;4:9–16. doi: 10.1080/15389580309860. [DOI] [PubMed] [Google Scholar]
- 46.Drumond J.A., Marcopito L.F. Internal migration and distribution of Chagas disease mortality, Brazil, 1981–1998. Cad Saude Publica. 2006;22:2131–2140. doi: 10.1590/s0102-311x2006001000019. [DOI] [PubMed] [Google Scholar]
- 47.Markides K.S., Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]