Abstract
Pneumonia is a leading killer of children in developing countries and results in significant morbidity worldwide. This article reviews the management of pneumonia and its complications from the perspective of both developed and resource-poor settings. In addition, evidence-based management of other respiratory infections, including tuberculosis, is discussed. Finally, the management of common complications of pneumonia is reviewed.
Keywords: Pneumonia, Tuberculosis, Respiratory infections, Treatment of pneumonia, Complications of community-acquired pneumonia
Epidemiology
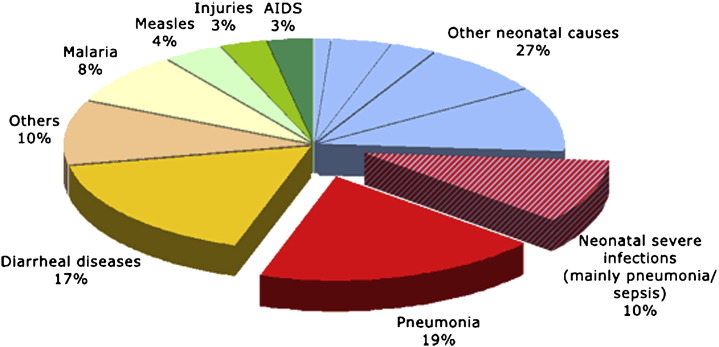
Pneumonia is a leading killer of children, causing an estimated 1.9 million deaths worldwide in children under the age of 5 years (Fig. 1 ).1, 2 The true mortality caused by pneumonia probably is underestimated, because most deaths in developing nations occur at home without a true medical diagnosis. Ninety percent of the deaths are thought to occur in the developing world, with 50% of these occurring in Africa.3 The incidence of pneumonia in North America and Europe is approximately 36 per 1000 per year.4, 5 Thus, although mortality is low, pneumonia causes significant morbidity even in developed countries.
Fig. 1.
Global distribution of cause-specific mortality among children under age 5 years in 2004. Pneumonia was the leading killer of children worldwide. (From UNICEF/WHO. Pneumonia: the forgotten killer of children. New York and Geneva: The United Nations Children's Fund (UNICEF)/World Health Organization (WHO); 2006; with permission.)
Definition
Pneumonia can be defined solely by clinical features6 or with the addition of radiologic findings. In part because of the considerable overlap between the diagnosis of bronchiolitis and pneumonia in young children,4 “lower respiratory illness” is a frequently used alternative term. Lower respiratory illness has been defined as fever, acute respiratory symptoms, and radiologic evidence of parenchymal infiltrates; the World Health Organization (WHO) guidelines use tachypnea as an important indicator of pneumonia when radiology facilities are unavailable.6 Tachypnea is defined as a respiratory rate greater than 60 breaths per minute in infants younger than 2 months, greater than 50 breaths per minute in children 2 to 12 months, and greater than 40 breaths per minute in children over 1 year of age. In children who have been symptomatic for more than 3 days, tachypnea has a sensitivity of 74% and a specificity of 67% for radiologically diagnosed pneumonia.7 In this study, sensitivity decreased when other clinical signs were included with tachypnea, but the addition of these other clinical signs increased specificity in relation to the reference standard of radiologically diagnosed pneumonia.
Etiology
Pneumonia usually begins as a colonization of the mucosa of the nasopharynx followed by spread into the lower respiratory tract. The infection can be community acquired or nosocomial. Bacteria, viruses, atypical organisms, and fungi are all known to cause pneumonia. In prospective research studies, a causative organism can be identified in nearly three quarters of cases of pneumonia. Respiratory viruses seem to be responsible for approximately 40% of cases of community-acquired pneumonia in children who are hospitalized, particularly in those under 2 years of age, whereas Streptococcus pneumoniae is responsible for 27% to 44% of the cases of community-acquired pneumonia.8, 9, 10, 11 Although infection with Mycoplasma pneumoniae and Chlamydia pneumoniae usually are considered to cause pneumonia in children of school age and in older patients, one study, in which preschool-aged children had as many episodes of atypical bacterial pneumonia episodes as older children, challenges this view.9 In this study a bacterial cause was identified in 60% of cases of pneumonia, with S. pneumoniae causing 73% of the cases in which a bacterial cause was identified. Other bacterial causes such as Staphylococcus aureus, Moraxhella catarrhalis, group A Streptococci, Streptococcus milleri, and Haemophilus species (non–type b) were identified infrequently. Mycoplasma pneumoniae and Chlamydia pneumoniae were responsible for 14% and 9% of cases of pneumonia, respectively. The most severe disease occurred in patients who had infection with a typical bacterial organism or in the 23% in whom mixed bacterial (usually S. pneumoniae) and viral coinfection were identified.9
Clinical features
-
•
Bacterial pneumonia is unlikely when wheeze is identified in young children (level of evidence: moderate).
Bacterial pneumonia should be considered in children if fever is higher than 38.5°C and is accompanied by tachypnea and recession.12, 13 Although auscultatory findings are not considered as reliable as other clinical signs in the diagnosis of pneumonia, crackles increase its likelihood. Wheeze in young children (preschool age and below) suggests a viral cause and in older subjects increases the possibility of infection by M pneumoniae. Fever, headache, and myalgia in older children are associated with M pneumoniae, whereas sticky eyes in a neonate are associated with Chlamydia trachomatis infection.12, 13
Management of a child who has community-acquired pneumonia at presentation
Assess for Contributing Etiology
History is important in the evaluation of community-acquired pneumonia, and the physician should inquire about contacts, travel, immunization history, the possibility of foreign body aspiration or primary aspiration, stools consistent with malabsorption, sinusitis, asthma, and environmental exposure. The examination should evaluate general features such as growth, upper airway anatomy, dysmorphism suggesting syndrome, neuromuscular weakness, and swallowing and gag reflexes. The pulmonary examination should assess oxygen saturation, respiratory rate, accessory muscle use, wheezes, and other auscultatory findings such as crackles. Cardiovascular examination also is important to rule out signs of cardiac failure.
Assess for Severity of Pneumonia
In terms of severity, the WHO recommends that children who have chest indrawing be admitted to hospital.13 The British Thoracic Society guidelines12, 14 regarding admission to hospital in the developed world are shown in Box 1 .
Box 1. British Thoracic Society guidelines: factors indicating need for admission of a child who has pneumonia.
-
•
Oxygen saturations ≤ 92%
-
•
Respiratory rate > 70 breaths per minute in infants or > 50 breaths per minute in older children
-
•
Intermittent apnea, grunting
-
•
Difficulty in breathing
-
•
Infant not feeding or signs of dehydration in older children
-
•
Family unable to provide appropriate observation or supervision
Data from British Thoracic Society. British Thoracic Society guidelines for the management of community acquired pneumonia in childhood. Thorax 2002;57(Suppl I):i1–24; and Kumar P, McKean MC. Evidence based paediatrics: review of BTS guidelines for the management of community acquired pneumonia in children. J Infect 2004;48(2):134–8.
Ambulatory care of a child who has community-acquired pneumonia
-
•
Investigations are not indicated routinely in mild childhood pneumonia.
-
•
The optimal duration of treatment is unknown, but most advocate treatment for 5 to 7 days (level of evidence: low).
-
•
Numerous adjunctive therapies in addition to antibiotics are prescribed frequently for the treatment of pneumonia (Table 1 ).
Table 1.
Adjunct therapies used in the treatment of childhood community-acquired pneumonia
| Medication/Intervention | Recommendation | Grading of Recommendation (Based on Evidence of Benefit) | Quality of Supporting Evidence |
|---|---|---|---|
| Antipyretics | Pain, fever, and irritability; no benefit on duration or severity of pneumonia | Low | No randomized, controlled trials |
| Cough suppressants | Not recommended as adjunct to treat cough in pneumonia | Moderate | Systematic review concluded insufficient evidence15 |
| Mucolytics | Not recommended in acute community-acquired pneumonia | Low | Systematic review concluded insufficient vidence15 |
| Chest physical therapy | Not indicated in acute community-acquired pneumonia | High | Randomized, controlled trial16 |
| Zinc supplementation | Zinc deficiency in high-mortality settings decreases prevalence and mortality of pneumonia | High | Meta-analysis of 17 randomized, controlled trials in children < 5 years17 |
Investigations of a child admitted with pneumonia
There are widespread variations in practice regarding the investigation of pneumonia in children who are admitted with this condition.
Chest Radiographs
-
•
Chest radiographs should not be performed routinely in children suspected of having pneumonia (level of evidence: high).
Radiologic findings are accepted as the reference standard for defining pneumonia, but it is not clear to what extent chest radiographs alter the outcome of childhood pneumonia even though they frequently are used to confirm the presence, site, and extent of pulmonary infiltrates. In one study in children between 2 months and 5 years of age, recovery occurred at a median of 7 days, whether or not a chest radiograph had been performed, and there was no difference in subsequent health care use. Having a chest radiograph significantly increased the likelihood of being prescribed antibiotics, however. Routine use of chest radiography was not beneficial in ambulatory children over the age of 2 months who had acute lower respiratory tract infection.18 The British Thoracic Society suggests that a chest radiograph be considered in a child younger than 5 years who has with a fever higher than 39°C of unknown origin and without features typical of bronchiolitis.12 Although lobar infiltrates, effusions, abscesses, and cavities on a chest radiograph are likely to be a consequence of bacterial rather than viral pneumonia,19 there are no other chest radiograph changes that are specific in differentiating bacterial from viral pneumonia and therefore indicating a need for treatment with antibiotics.
Blood Cultures
Blood cultures are positive in only 10% to 30% of children who have pneumonia and only in pneumonias where bacteremia occurs.20 In a study in The Gambia, clinical signs that predicted a positive blood culture were high fever (>38°C), dehydration, nasal flaring, grunting, bronchial breath sounds, and diminished air entry.21 Recent antibiotic use further reduces the chance of a positive blood culture, so in a developed country, where antibiotics are prescribed earlier in the course of lower respiratory illness, the clinical features that predict a positive blood culture are likely to be different. The British Thoracic Society guidelines recommend performing a blood culture in all children who are hospitalized and when bacterial pneumonia is suspected.12
Further Microbiology
-
•
Lung aspirates should be considered when peripheral consolidation is proven by chest radiograph (level of evidence: moderate).
-
•
Pleural aspiration is indicated when significant pleural effusion is identified (level of evidence: moderate).
Microbiologic investigations generally are not recommended for patients being managed in the community.12 Within the hospital setting, older children may be able to provide a sputum sample, but younger children usually cannot. When pulmonary tuberculosis (TB) is suspected, consecutive early morning, preprandial, preambulatory gastric washings are indicated and are more sensitive than bronchoalveolar lavage. Induction of sputum using hypertonic saline may also be useful when TB is suspected, but this technique increases the chances of a typically noninfectious patient being rendered temporarily infectious during the procedure.22 In hospitalized infants under 18 months of age a nasopharyngeal aspirate should be sent for viral antigen detection (such as immunofluorescence) with or without viral culture.12 When significant pleural fluid is present, it should be aspirated and sent for microscopic aspiration and culture as early as possible during the course of disease, and a specimen should be saved for bacterial antigen detection.12 If pleural fluid is associated with a complicated parapneumonic effusion, a sample of pleural fluid is likely to be obtained during the management of this complication, so in this circumstance an additional diagnostic pleural tap may not be in the best interest of the child. Lung aspirates are rarely performed, but the technique is safer than widely perceived and can provide a bacterial diagnosis in more than 50% of cases.23 Lung aspirates therefore are more sensitive than blood cultures, but the organisms identified by this technique frequently are different from those identified by blood cultures taken in the same children.24 The limitations of lung aspirates is that they are painful and result in a small (but usually clinically insignificant) pneumothorax, and the technique usually is limited to pneumonias associated with dense peripheral consolidations close to the chest wall. Lung aspiration in conjunction with use of nucleic amplification tests can potentially increase the yield further,25 and therefore lung aspiration should be considered if the benefits of identifying the causative agent outweigh the modest risk of the procedure and equipment for and expertise in the management of the potential complication of a pneumothorax are available.
Organisms causing pneumonia according to age
Neonates
Common organisms causing pneumonia in neonates are group B streptococci, gram-negative enteric bacteria, cytomegalovirus, Ureaplasma urealyticum, Listeria monocytogenes, and C trachomatis.
Less common organisms causing pneumonia in neonates are S pneumoniae, group D streptococcus, and anaerobes.
Infants
Common organisms causing pneumonia in infants are respiratory syncytial virus, parainfluenza viruses, influenza viruses, adenovirus, metapneumovirus, S pneumoniae, H influenzae, M pneumoniae, and Mycobacterium tuberculosis.
Less common organisms causing pneumonia in infants are Bordetella pertussis and Pneumocystis jiroveci.
Preschool Children
Common organisms causing pneumonia in preschool-age children are respiratory syncytial virus, parainfluenza viruses, influenza viruses, adenovirus, metapneumovirus, S pneumoniae, H influenzae, M pneumoniae, and M tuberculosis.
A less common organism causing pneumonia in preschool-age children is C pneumoniae
School-Age Children
Common organisms causing pneumonia in school-age children are M pneumoniae, C pneumoniae, S pneumonia, M tuberculosis, and respiratory viruses.
Organisms Rarely Causing Pneumonia
The following organisms rarely cause pneumonia:
Viruses: Coronavirus, Varicella-zoster, Epstein-Barr, Mumps
Atypical organisms: Chlamydia psittaci, Coxiella Burnetti
Bacteria: Klebsiella pneumoniae, Legionella, Streptococcus pyogenes, Brucella abortus
Fungi: Coccidioides immitis, Histoplasma capsulatum, Blastomyces dermatitidis
Treatment of children admitted with pneumonia
General
-
•
Hypoxia (oxygen saturation ≤ 92%) should be treated with supplemental oxygen (level of evidence: moderate).
Initial management always should commence with an assessment of the airway, breathing, and circulation. Most children do not require admission to hospital. Children whose oxygen saturation is 92% or less in air should receive supplemental oxygen therapy.12 In a Zambian study, the mortality from pneumonia was increased when hypoxemia was present, a finding that highlights the importance of oxygen in treatment.26 Intravenous fluids rarely are indicated but may be required in the presence of severe dehydration, ongoing vomiting, severe electrolyte disturbances, or respiratory failure. In this context, inappropriate secretion of antidiuretic hormone may occur,27 and intravenous fluids may need to be administered at 80% of full maintenance.
Antibiotics
-
•
Children who have mild symptoms do not require treatment with antibiotics (level of evidence: moderate).
-
•
Amoxicillin or co-amoxyclavulanic acid is the antibiotic of choice in preschool children (level of evidence: moderate).
-
•
Children over 5 years of age also can be treated with amoxicillin or co-amoxyclavulanic acid or with a macrolide (or both) when atypical infection is suspected (level of evidence: moderate).
-
•
Antibiotics administered orally are safe and effective for most children (level of evidence: high).
-
•
The optimal duration of treatment for a child admitted with pneumonia is unknown, but most recommend 5 to 7 days of antibiotics (level of evidence: low).
When a decision has been made to treat with antibiotics, the oral route is the most appropriate for most children. Although co-trimoxazole is widely used as the first-choice antibiotic throughout the world, it is inferior to treatment with amoxicillin in severe pneumonia.28, 29 Amoxicillin is recommended as the first line of therapy for children under 5 years because it is relatively inexpensive, is well tolerated, and is effective against most of the pathogens in this age group. Co-amoxyclavulanic acid seems to be significantly more effective than oral amoxicillin alone but is more expensive.29 In children older than 5 years, amoxicillin again is an appropriate first-line agent unless mycoplasma or chlamydia pneumonia is suspected, in which case a macrolide antibiotic, either alone or in addition, is appropriate. Erythromycin is equally as effective as29 and is significantly cheaper than second-generation macrolides such as azithromycin, clarithromycin, or roxithromycin, but it has a shorter half-life and requires more frequent dosing. It also may be associated with more frequent adverse effects, especially involving the gastrointestinal tract.
There is no evidence that intravenous treatment is superior to oral treatment in community-acquired pneumonia. Intravenous antibiotics therefore are reserved for severe cases of pneumonia or for pneumonia in a child unable to tolerate oral antibiotics. Appropriate antibiotics to administer intravenously include benzyl penicillin, co-amoxyclavulanic acid, a second- or third-generation cephalosporin, and the addition of a macrolide if atypical infection is considered a possibility.
Antibiotic resistance
-
•
Antibiotic resistance is common and increasing, partly in response to inappropriate antibiotic prescribing (level of evidence: moderate).
Principles of good antibiotic prescribing (eg, using the appropriate antibiotic with the narrowest spectrum, aiming for high tissue or plasma concentrations, a short-half life, and administered as a short, intensive course) are important and are less likely to induce antibiotic resistance.30 Resistance to antibiotics usually is acquired through selective pressure on bacteria resulting from exposure to antibiotics and preferential survival of resistant organisms. Pneumococcal resistance has been documented in up to 40% of isolates,31and high rates have been reported in Spain, France, and the United States.31, 32 Mutations in genes coding for penicillin-binding proteins lead to decreased affinity for penicillin and consequently the failure of penicillin to inhibit the enzymes responsible for cell wall synthesis. Pneumococcal resistance to penicillin occurs when the mean inhibitory concentration is less than 2 μg/mL, but there is no evidence that treatment with high-dose penicillin or cephalosporins for pneumonia in which pneumococcal resistance is documented is associated with clinical failure.33, 34, 35 Most, however, would consider using a third-generation cephalosporin or vancomycin if clinical resistance is suspected or when resistance is identified in a child who is immunosuppressed.
Up to 34% of isolates of H influenzae (including nontypeable strains) are resistant to ampicillin because of the production of ß-lactamases by the organism that inhibit the antibiotic.36 Therefore, in areas of high endemic resistance, or when resistance is suspected clinically or is identified in an immunosuppressed individual, treatment with a third-generation cephalosporin is indicated.
Most strains of S aureus are penicillin resistant, because ß-lactamases are very prevalent. Methicillin/flucloxacillin resistance also is widespread now, particularly in hospital-acquired infection but also can be found in community-acquired infections.37 Vancomycin or teicoplanin are the antibiotics of choice to treat such infections, at least when vancomycin resistance is not suspected. The outcome may be better when rifampicin is added to treatment with vancomycin,38 but this benefit is not confirmed in community-acquired pneumonia. Apart from resistant S aureus, most other bacteria that cause hospital-acquired pneumonia are gram-negative organisms such as Pseudomonas species, Serratia species, Escherichia coli, and Enterobacter species. Multidrug resistance has been documented in each of these bacteria, so local guidelines are necessary for the appropriate selection of antibiotics.
Prevention
Vaccines
-
•
Vaccines against H influenzae and S pneumoniae are effective (level of evidence: high).
-
•
Vaccines are not currently available in populations where pneumonia has the highest mortality (level of evidence: high).
The recent development and introduction of conjugate vaccines for H. influenzae type b (Hib) and S pneumoniae has led to a degree of control of pneumonia caused by these two organisms in developed countries where they have been introduced into the immunization schedule. Hib vaccine was introduced in 1990. The first report from a bacterial pneumonia vaccine trial in the developing world was from The Gambia in 1997,39 where Hib vaccination reduced clinical pneumonia by 4% and radiologic pneumonia by 20%. No lung aspirates were identified as culture positive for Hib in children who received the vaccine in this study. A further study in Chile also confirmed the clinical efficacy of Hib vaccine.40 An Indonesian study, however, in which coverage with chest radiographs was much greater than in the other two studies, found no evidence for reduction of radiologic pneumonia as a result of the vaccine, even though a reduction in clinically diagnosed lower respiratory illness was confirmed.41
The first pneumococcal conjugate vaccine was introduced in 1990. Studies in the United States,42 South Africa,43 and The Gambia44 have demonstrated its efficacy against development of clinically diagnosed pneumonia, severe pneumonia, radiologically defined pneumonia, and vaccine serotype–specific bacteremia or lung aspirate culture.45 Newer vaccines that incorporate more serotypes than the nine included in the Gambian and South African studies are likely to offer improved efficacy when they are introduced. Because there are at least 90 pneumococcal serotypes, however, the risk is that serotype replacement eventually will result in diminished benefit from vaccination. The optimal schedule for administration of the seven-valent pneumococcal vaccine has not yet been determined.46
As antibiotics become less effective against common bacterial causes of childhood pneumonia, the role of primary vaccination will become increasingly important. Vaccination decreases the circulation of resistant organisms and, in the case of S pneumoniae, the current seven-valent vaccine is effective against the serotypes most commonly associated with antibiotic resistance.47
Other prevention measures
-
•
Environmental, nutritional, and socioeconomic factors affect mortality in childhood pneumonia and are preventable (level of evidence: high).
Over the next decade, it is crucial that vaccines become available to children in the developing world, who are at greatest risk of dying from pneumonia. Failure to make these vaccines available would indicate that the motives behind vaccine development do not include a desire to affect significantly the global childhood mortality caused by pneumonia. Environmental, nutritional, and socioeconomic factors that affect equity of access are crucially important also.48 A concerted effort to address these factors in many developed nations at the beginning of the last century resulted in the large reduction in mortality from pneumonia that occurred before the availability of antibiotics49 and points out that mortality from pneumonia in childhood reflects socioeconomic disadvantage above all other factors.
Common respiratory issues in developing countries
The WHO estimates that nearly one fifth of childhood deaths are caused by pneumonia, which claims more than 2 million lives annually (see Fig. 1). Most of these deaths occur in Africa and Southeast Asia2, 50 and are caused either by community-acquired pneumonia or by infections secondary to measles, pertussis, or AIDS/HIV. Most of these deaths are preventable with available interventions.51 Although few of these episodes result in death, they produce significant morbidity and short-term sequelae, which may have a detrimental effect on the child's nutritional status and also may influence the risk of other childhood diseases. Effective strategies to combat this problem include the WHO Integrated Management of Childhood Illness (IMCI) program, nutritional interventions, and immunization. The use of case management guidelines recommended by IMCI for childhood pneumonia has reduced overall and pneumonia-specific mortality in children significantly.52, 53, 54
Integrated management of childhood illness
The generic IMCI guidelines are meant to target the leading causes of mortality and severe morbidity in children below 5 years of age, who are a particularly vulnerable age group. The IMCI strategy incorporates assessment of feeding, updating immunization status, and provision of vitamin A prophylaxis. The three components of the IMCI program are improving the skills of health workers, improving the health system, and improving household and community practices. IMCI is considered to be among the most cost-effective interventions in both low- and middle-income countries and to be the program most likely to have the greatest impact on the global burden of disease. As of December 2000, more than 81 countries around the world had adopted IMCI guidelines.
Management options for acute respiratory infection following the integrated management of childhood illness approach
-
•
Use oral co-trimoxazole rather than other oral/parenteral antibiotics in the treatment of nonsevere pneumonia (level of evidence: high).
-
•
Use ambulatory short-course amoxicillin for treatment of severe pneumonia (level of evidence: high).
-
•
Use parenteral chloramphenicol instead of ampicillin plus gentamicin for very severe pneumonia (level of evidence: high).
Community-based interventions to identify and treat pneumonia have a considerable effect on child mortality. The WHO guidelines for the case management of acute respiratory infections are based on simple signs such as fast breathing and indrawing of the chest and are designed for countries with an infant mortality rate higher than 40 per 1000 live births.55 The WHO defines cases of suspected pneumonia as children reported to have an illness associated with a cough accompanied by fast and/or difficult breathing. It is recommended that children who have cough without fast breathing be treated as outpatients without antibiotics; those who have fast breathing (nonsevere pneumonia) be treated at home with oral co-trimoxazole or amoxicillin for 5 days; and those who have lower chest indrawing (severe pneumonia) and general danger signs (very severe disease) be referred to hospital and treated with parenteral ampicillin/penicillin.
A recent meta-analysis assessing the effect of the pneumonia case-management approach on mortality identified a 24% reduction in total mortality and a 36% reduction in pneumonia mortality in children under 5 years of age.52 This analysis of nine studies53, 54, 56, 57, 58, 59, 60, 61, 62 concluded that community-based interventions to identify and treat pneumonia have reduced child mortality considerably, with consistent results, despite the diversity of pneumonia interventions and developing-country settings in which these trials took place. A potential limitation of this analysis is that all the studies were undertaken more than a decade ago, and with the increasing prevalence of antimicrobial resistance their implications for public health programs are unclear.
In the last decade, and more recently, studies have looked at the efficacy of various antibiotic regimens in developing country settings.28, 63, 64, 65, 66, 67, 68 All cases of suspected pneumonia in these settings should be treated with oral or parenteral antibiotics, depending on severity. The potential choice of antibiotics is wide but should be applicable for large-scale use in low-resource settings. Co-trimoxazole is a cheap and effective drug, and all the studies show that it compares favorably with other antibiotics for nonsevere pneumonia. A study comparing the efficacy of co-trimoxazole and that of amoxicillin for nonsevere pneumonia and examining the association with in vitro co-trimoxazole susceptibility found no difference in efficacy between co-trimoxazole and amoxicillin, despite high in vitro resistance to co-trimoxazole.28 Another study comparing the clinical efficacy of twice-daily oral co-trimoxazole and twice-daily oral amoxicillin found that both were equally effective for the treatment of nonsevere pneumonia.63 Three other studies comparing co-trimoxazole with chloramphenicol;64 with procaine penicillin on day 1 followed by 5 days of oral ampicillin;65 and with intramuscular procaine penicillin G or benzathine penicillin G in combination with procaine penicillin G66 did not indicate any difference in efficacy with alternative antibiotic regimens. Another double-blind, randomized, controlled trial comparing a course of the standard dose (45 mg/kg/d) of oral amoxicillin for the treatment of nonsevere pneumonia versus a course of a double dose (80–90 mg/kg/d) found no difference between the two doses.69 The only study assessing oral treatment for severe pneumonia concluded that home treatment with high-dose oral amoxicillin is equivalent to currently recommended hospitalization and parenteral ampicillin for treatment of severe pneumonia without underlying complications,67 but a recent Cochrane review suggested that amoxicillin is better than co-trimoxazole for severe pneumonia.29 Another study showed that the combination of parenteral ampicillin and gentamicin was more efficacious than parenteral chloramphenicol alone.68 Based on these findings, the WHO has revised the guidelines for the management of severe pneumonia to include home treatment with high-dose oral amoxicillin or a combination of parenteral ampicillin and gentamicin for hospitalized patients.
Tuberculosis in children and adolescents
The worsening TB pandemic remains a major threat to global health. TB kills nearly 2 million people every year (5000 per day).70 Precise estimates for the burden of childhood TB are not readily available, primarily reflecting the difficulty in diagnosing TB accurately in children. Children represent an increasing proportion of the total number of cases in TB-endemic areas, however, with almost 500,000 children succumbing to the disease each year. Although the overwhelming burden of disease is in developing countries, several developed countries also have reported a recent increase in the number of TB cases in children.71, 72 Although in most children the initial infection occurs in the lungs, TB in children and adolescents should be considered, at least potentially, to be a systemic disease. The primary complex comprising the site of infection and the involved regional lymph nodes may heal, or complications may develop from enlargement or rupture of the regional lymph nodes or from the spread of tubercle bacilli into the bloodstream, giving rise to disseminated disease. The risk of dissemination is greatest in the first 5 years of life and within the first 12 to 24 months after infection and is seen more commonly in children than in adults.
Recently, the Tuberculosis Coalition for Technical Assistance and its partners have published international standards of care for the management of TB.73 The reader is referred to this important document and its 17 standards relating to the diagnosis, treatment, and public health responsibilities of TB.
Diagnosis
Tuberculosis infection
Diagnosis of TB infection is based on tuberculin skin testing (TST) in the absence of signs or radiologic findings suggestive of TB disease. The interpretation of a positive test may be modified by the risk of infection, which is influenced by the contact history, duration of contact, medical history, and age of the individual and their Bacille Calmette-Guerin (BCG) vaccination status. The TST is an imperfect test. Its interpretation and subsequent clinical management depend on the prior probability of the test being positive and on the clinical circumstances of the individual or family.
Tuberculosis disease
Diagnosis of TB disease is based on clinical symptoms and signs, chest radiographs or other investigations, and smear and culture of infected body material. Although there are conflicting reports as to whether lateral chest radiographs increase the yield for detecting intrathoracic lymphadenopathy,74, 75 CT is considered an excellent tool for detecting mediastinal nodes. CT, however, requires a volumetric scanning protocol and should not be performed routinely because of the associated high radiation dose.
Even though the yield from cultures is low in children, microbiologic confirmation of TB should be sought. Treatment should be started as soon as samples have been obtained.
Microbiology
-
•
In patients unable to produce sputum, gastric aspirates are the investigation of choice for pulmonary TB in children (level of evidence: moderate).
In younger children, when it is not possible to obtain sputum, gastric aspirates should be collected on 3 consecutive days. About 50 mL of gastric contents should be aspirated via a nasogastric tube early in the morning after the child has fasted for 8 to 10 hours, preferably while the child is still recumbent. Both a smear and culture should be performed on the aspirate.
If there is radiologic evidence of focal disease, such as lobar, segmental, or subsegmental collapse, or clinical evidence of bronchial obstruction, a flexible fiberoptic bronchoscopy may be indicated to identify and biopsy endobronchial lesions, ideally, with bronchoalveolar lavage performed in addition to gastric aspiration. Otherwise, bronchoscopy with bronchoalveolar lavage offers no advantages over gastric aspiration.76
Inhalation of nebulized sterile hypertonic saline (3% to 6%) via an ultrasonic nebulizer can be used to induce sputum in patients unable to expectorate sputum. The cough produced by this technique may be of sufficient force to aerosolize tubercle bacilli and infect health care workers, however. Ideally, sputum should be induced in areas with high-efficiency particulate air filters, and qualified personnel should wear appropriate respiratory protection.
Role of interferon-gamma release assays in children
The sensitivity of the currently available interferon-gamma release assays for the diagnosis of culture-confirmed TB disease in children is not high enough for these assays to be used alone to rule out TB.77 In most studies interferon-gamma release assays and TST yield equivalent results for the detection of latent TB infection in children, once adjustment is made for interpretation of the TST based on differing cut-offs, and some evidence suggests these assays may be less sensitive than TST in children.78 Limited data suggest that in situations in which the value of TST is greatly reduced (eg, in patients infected with HIV), interferon-gamma release assays may prove useful when used as an adjunct to TST to increase sensitivity. Other specific situations in which the interferon-gamma release assays might be indicated are
-
•
To confirm infection in a child who has been vaccinated with BCG and the TST result is borderline positive/negative
-
•
As a replacement for TST when repeat testing with TST is likely to result in a booster phenomenon
-
•
If TST testing is considered likely to result in a blistering or a large painful response (eg, in a patient who has had a strong reaction to TST in the past)
-
•
For a child who is unable or unlikely to return at 48 to 72 hours for reading of the TST
Treatment
Latent Tuberculosis Infection
Treatment of children who have latent TB infection and no evidence of TB disease is indicated for two reasons: first, to reduce the risk of the patient's developing disease in the years immediately after acquiring the infection, particularly in children under the age of 5 years, when extrapulmonary disease is more common, and second, to reduce the lifelong risk of developing TB disease as a consequence of infection. These goals can be achieved by the use of isoniazid therapy for a minimum of 6 months. Although a dose of isoniazid, 5 to10 mg/kg once daily, is recommended, a dose of 10 mg/kg is optimal: children eliminate isoniazid faster than adults, and therefore relatively larger doses are required to achieve comparable serum concentrations.79
Treatment of latent TB infection is particularly important in HlV—positive children, children in whom corticosteroid or immunosuppressive therapy is contemplated, and in those who have diabetes or other chronic diseases associated with malnutrition (eg, celiac disease).
Treatment of latent TB infection in children and adolescents has few side effects. The incidence of liver toxicity in children is extremely low, and routine monitoring of liver function is not recommended.
Treatment of pulmonary tuberculosis disease
-
•
A rifampicin-containing regime is the backbone of antituberculosis treatment for drug-susceptible M tuberculosis (level of evidence: high).
-
•
At least 6 months' treatment is recommended using three or four drugs for 2 months with a further continuation phase of 4 months with isoniazid and rifampicin (level of evidence: high).
Children who have TB disease usually are treated with daily therapy with four drugs, isoniazid, rifampicin, pyrazinamide, and ethambutol, for 2 months, and then generally with two drugs, isoniazid and rifampicin, for a further 4 months. Normally these drugs are given daily, but supervised therapy given 3 days a week sometimes is necessary when adherence with daily therapy is considered to be poor.
Such short-course therapy (6 months) has been shown to be effective in children who have primary TB and complicated primary TB limited to the respiratory tract.
Infectivity
-
•Childhood TB is rarely contagious (level of evidence: high) because
-
•Children who have TB disease usually have a small bacterial load.
-
•Children are less able to generate the tussive forces needed to aerosolize bacilli.
-
•Children very rarely have cavitating disease.
-
•Young children swallow rather than expectorate sputum.
-
•Occasionally adolescents are seen with cavities caused by TB and then may be infectious.
-
•
Strategies to Improve Adherence
Adherence is a multidimensional phenomenon determined by the interplay of socioeconomic, health system, disease-related, patient-related, and therapy-related factors.73 A few pragmatic strategies to enhance treatment adherence include
-
•
Emphasizing the importance of adherence at outset of treatment to child and family
-
•
Assigning a key worker to each family with information on how to contact the worker
-
•
Using professional interpreters to communicate if necessary, rather than family members
-
•
Giving information about potential side effects to the child and the family
-
•
Providing pill organizers for multidrug regimes
-
•
Using combination antibiotic preparations when available and if tolerated
-
•
Providing written information in appropriate languages
-
•
Maintaining close liaison with the dispensing pharmacy regarding collection of scripts
-
•
Having liquid preparations readily available for preschool children
-
•
Providing easy access to follow-up
Respiratory infections in HIV-infected children
-
•
Parenteral benzyl penicillin or ampicillin should be used in combination with gentamicin (level of evidence: high).
The clinical expression of HIV disease in children is highly variable. HIV-related lower respiratory infections account for 30% to 40% of pediatric admissions and have a case fatality rate of up to 35%, much higher than the 10% for children not infected with HIV. In addition to S pneumoniae and S aureus, P jiroveci, gram-negative bacteria, and cytomegalovirus are important opportunistic infections in this group of children.80 The WHO developed revised guidelines for presumptive treatment of pneumonia in young children in regions where the prevalence of HIV is high. It is recommended that children admitted with severe pneumonia in HIV-endemic areas receive benzyl penicillin or ampicillin in combination with gentamicin, irrespective of age, and that all infants receive high-dose co-trimoxazole because of the high prevalence of P jiroveci. 81 There are no reported studies assessing the efficacy of these treatment guidelines since publication. A study conducted before the publication of the guidelines used the same recommendations and concluded that in children older than 1 year the WHO guidelines were effective, irrespective of HIV status. For those aged younger than 1 year, however, the guidelines were found to be inadequate, because nearly half of the infants did not respond to therapy. This failure was attributed to polymicrobial disease.82
Common tropical respiratory infections
Pulmonary Hydatid Cyst (Echinococcosis)
-
•
Surgical excision of the cyst in conjunction with benzimidazoles is recommended (level of evidence: moderate).
-
•
Exclusive medical therapy is reserved for patients who are poor candidates for surgery (level of evidence: moderate).
Echinococcosis or hydatid disease is caused by the cystic larval stage of the tapeworm Echinococcus. The liver is the most common site of cyst formation, followed by the lung in 10% to 30% of cases. Pulmonary disease seems to be more common in children and younger individuals. Although most patients are asymptomatic, some may expectorate the contents of the cyst or develop symptoms related to compression of the surrounding structures. Surgical excision of the cyst is the treatment of choice whenever feasible, because the parasite can be removed completely and the patient cured.83 The surgical options for lung cysts include lobectomy, wedge resection, pericystectomy, intact endocystectomy, and capitonnage. Medical therapy with benzimidazoles is valuable in disseminated disease, including secondary lung or pleural hydatidosis, in patients who are poor surgical risks, and when there is intraoperative spillage of hydatid fluid.84
Pulmonary amebiasis
-
•
Tissue amebicides are effective treatment (level of evidence: moderate).
-
•
Surgical management is reserved for patients who have advanced disease (level of evidence: moderate).
Amebiasis caused by Entameba histolytica is endemic in the tropical countries. The lungs are the second most common extraintestinal site after amebic liver abscess. Pleuropulmonary amebiasis most often is a consequence of the direct extension of an amebic liver abscess manifested by consolidation, lung abscess, pleural effusion/empyema or hepato-bronchial fistula. Tissue amebicides such as metronidazole, chloroquine, and dehydroemetine are effective in most patients who have pulmonary disease.85, 86 Percutaneous pleural drainage and surgical decortication have a role in patients who have advanced disease.87, 88
Tropical eosinophilia
-
•
A 3-week course of diethylcarbamazine is recommended (level of evidence: moderate).
Tropical eosinophilia is a syndrome characterized by a generalized tissue reaction in which pulmonary manifestations predominate. An underlying hypersensitivity reaction to the filarial parasites Wuchereria bancrofti or Brugia malayi results in cough, breathlessness, wheeze, marked increase in peripheral eosinophilia, and eosinophilic pulmonary infiltrates.89, 90 Treatment is with a 3-week course of diethylcarbamazine.91, 92
Management of complications of respiratory infections
Empyema
-
•
Use a chest drain with intrapleural fibrinolytics (level of evidence: high).
-
•
Use video-assisted thoracoscopic surgery (level of evidence: high).
A number of treatment options currently are available for empyema, including systemic antibiotics alone or in combination with thoracocentesis; chest drain insertion, with or without intrapleural fibrinolytics; and surgical techniques such as video-assisted thoracoscopic surgery (VATS), mini-thoracotomy, and standard thoracotomy with decortication. All these treatment options are safe and effective. Chest drain with intrapleural fibrinolytics, particularly urokinase,93, 94 and VATS94, 95 have been shown to be effective primary approaches in the treatment of empyema, with a shorter duration of hospital stay, which is used consistently as an outcome measure. The failure rates are similar with both modalities of treatment. The cost of treatment with intrapleural urokinase is around 25% cheaper than VATS, and, because the expertise to perform VATS may not be universally available, intrapleural urokinase is advocated as first-line management.94
A meta-analysis comparing the results of nonoperative and primary operative therapy for the treatment of pediatric empyema reviewed 67 studies.96 Data were aggregated from reports of children treated nonoperatively (3418 cases from 54 studies) and from children treated with a primary operative approach (363 cases from 25 studies). Data analysis showed that primary operative therapy was associated with a lower mortality rate, lower re-intervention rate, shorter length of hospitalization, decreased time with a thoracostomy tube, and shorter course of antibiotic therapy, compared with nonoperative therapy. The limitations of this analysis are that most of the studies included were observational or retrospective case note reviews. The observational data from the analysis show that the length of stay is similar for primary fibrinolytic therapy (10.7 days), thoracotomy (10.6 days), and VATS (11.2 days). The analysis also suggests that current surgical options for childhood empyema seem safe, with no reported mortality and little morbidity, and that there is complete resolution of the disease, whatever the treatment.
Pneumatoceles
-
•
Pneumatoceles resolve without treatment (level of evidence: moderate).
-
•
Refractory cases require surgery (level of evidence: moderate).
Pneumatoceles are associated most frequently with staphylococcal pneumonia but also are seen in pneumonias caused by S pneumoniae, H influenzae, E coli, and Klebsiella. They usually do not produce any additional symptoms to the underlying infective process and regress spontaneously.97, 98 Surgical management, including drainage, resection, or decortication, is required only in refractory cases or those that are symptomatic.98
Lung Abscess
-
•
Lung abscess resolves with a prolonged course of antibiotics (level of evidence: moderate).
-
•
Abscess drainage hastens recovery (level of evidence: moderate).
Lung abscesses coexisting with necrotizing pneumonia or empyema usually do not require surgical drainage and resolve with a prolonged course of antibiotics administered for the pneumonic process.99 In the last decade, however, there has been increasing interest in the early use of interventional radiology for the aspiration of lung abscesses, with or without placement of an external drain, as a way of hastening recovery and decreasing hospital stay. Surgical resection of the affected lobe is associated with significant morbidity and is very rarely advocated.100, 101, 102
Bronchopleural Fistulae and Pyopneumothorax
-
•
Bronchopleural fistula resolves with continued drainage (level of evidence: moderate).
-
•
Surgical management is useful in protracted cases (level of evidence: moderate).
Bronchopleural fistulae associated with necrotizing pneumonias and empyema usually are peripheral and resolve with continued chest drainage.103 Sometimes, however, they are slow to resolve, and surgical management must be considered. Talc pleurodesis and limited decortication with muscle flap around the bronchopleural fistula have been used successfully in protracted cases.104, 105
References
- 1.Wardlaw T., Salama P., Johansson E.W. Pneumonia: the leading killer of children. Lancet. 2006;368(9541):1048–1050. doi: 10.1016/S0140-6736(06)69334-3. [DOI] [PubMed] [Google Scholar]
- 2.Williams B.G., Gouws E., Boschi-Pinto C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2(1):25–32. doi: 10.1016/s1473-3099(01)00170-0. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. The World Health Organization report 2005. 2005. http://www.who.int/whr/en Available at: Accessed July 2008.
- 4.Jokinen C., Heiskanen L., Juvonen H. Incidence of community-acquired pneumonia in the population of four municipalities in eastern Finland. Am J Epidemiol. 1993;137(9):977–988. doi: 10.1093/oxfordjournals.aje.a116770. [DOI] [PubMed] [Google Scholar]
- 5.McCracken G.H., Jr. Etiology and treatment of pneumonia. Pediatr Infect Dis J. 2000;19(4):373–377. doi: 10.1097/00006454-200004000-00032. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation . WHO; Geneva: 1995. The management of acute respiratory infections in children. practical guidelines for outpatient care. [Google Scholar]
- 7.Palafox M., Guiscafre H., Reyes H. Diagnostic value of tachypnoea in pneumonia defined radiologically. Arch Dis Child. 2000;82(1):41–45. doi: 10.1136/adc.82.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heiskanen-Kosma T., Korppi M., Jokinen C. Etiology of childhood pneumonia: serologic results of a prospective, population-based study. Pediatr Infect Dis J. 1998;17(11):986–991. doi: 10.1097/00006454-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Michelow I.C., Olsen K., Lozano J. Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics. 2004;113(4):701–707. doi: 10.1542/peds.113.4.701. [DOI] [PubMed] [Google Scholar]
- 10.Wubbel L., Muniz L., Ahmed A. Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J. 1999;18(2):98–104. doi: 10.1097/00006454-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Juven T., Mertsola J., Waris M. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19(4):293–298. doi: 10.1097/00006454-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 12.British Thoracic Society British Thoracic Society guidelines for the management of community acquired pneumonia in childhood. Thorax. 2002;57(Suppl I) doi: 10.1136/thorax.57.90001.i1. i1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pio A. Standard case management of pneumonia in children in developing countries: the cornerstone of the Acute Respiratory Infection Programme. Bull World Health Organ. 2003;81(4):298–300. [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar P., McKean M.C. Evidence based paediatrics: review of BTS guidelines for the management of community acquired pneumonia in children. J Infect. 2004;48(2):134–138. doi: 10.1016/j.jinf.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Chang C.C., Cheng A.C., Chang A.B. Over-the-counter (OTC) medications to reduce cough as an adjunct to antibiotics for acute pneumonia in children and adults. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD006088.pub2. CD006088. [DOI] [PubMed] [Google Scholar]
- 16.Paludo C., Zhang L., Lincho C.S. Chest physical therapy for children hospitalized with acute pneumonia: a randomized controlled trial. Thorax. 2008;63(9):791–794. doi: 10.1136/thx.2007.088195. [DOI] [PubMed] [Google Scholar]
- 17.Aggarwal R., Sentz J., Miller M.A. Role of zinc administration in prevention of childhood diarrhea and respiratory illnesses: a meta-analysis. Pediatrics. 2007;119(6):1120–1130. doi: 10.1542/peds.2006-3481. [DOI] [PubMed] [Google Scholar]
- 18.Swingler G.H., Hussey G.D., Zwarenstein M. Randomised controlled trial of clinical outcome after chest radiograph in ambulatory acute lower-respiratory infection in children. Lancet. 1998;351(9100):404–408. doi: 10.1016/S0140-6736(97)07013-X. [DOI] [PubMed] [Google Scholar]
- 19.Davies H.D., Wang E.E., Manson D. Reliability of the chest radiograph in the diagnosis of lower respiratory infections in young children. Pediatr Infect Dis J. 1996;15(7):600–604. doi: 10.1097/00006454-199607000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Anonymous Pneumonia in childhood. Lancet. 1988;1(8588):741–743. [PubMed] [Google Scholar]
- 21.Banya W.A., O'Dempsey T.J., McArdle T. Predictors for a positive blood culture in African children with pneumonia. Pediatr Infect Dis J. 1996;15(4):292–297. doi: 10.1097/00006454-199604000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Zar H.J., Hanslo D., Apolles P. Induced sputum versus gastric lavage for microbiological confirmation of pulmonary tuberculosis in infants and young children: a prospective study. Lancet. 2005;365(9454):130–134. doi: 10.1016/S0140-6736(05)17702-2. [DOI] [PubMed] [Google Scholar]
- 23.Vuori-Holopainen E., Peltola H. Reappraisal of lung tap: review of an old method for better etiologic diagnosis of childhood pneumonia. Clin Infect Dis. 2001;32(5):715–726. doi: 10.1086/319213. [DOI] [PubMed] [Google Scholar]
- 24.Falade A.G., Mulholland E.K., Adegbola R.A. Bacterial isolates from blood and lung aspirate cultures in Gambian children with lobar pneumonia. Ann Trop Paediatr. 1997;17(4):315–319. doi: 10.1080/02724936.1997.11747904. [DOI] [PubMed] [Google Scholar]
- 25.Vuori-Holopainen E., Salo E., Saxen H. Etiological diagnosis of childhood pneumonia by use of transthoracic needle aspiration and modern microbiological methods. Clin Infect Dis. 2002;34(5):583–590. doi: 10.1086/338642. [DOI] [PubMed] [Google Scholar]
- 26.Smyth A., Carty H., Hart C.A. Clinical predictors of hypoxaemia in children with pneumonia. Ann Trop Paediatr. 1998;18(1):31–40. doi: 10.1080/02724936.1998.11747923. [DOI] [PubMed] [Google Scholar]
- 27.Dhawan A., Narang A., Singhi S. Hyponatraemia and the inappropriate ADH syndrome in pneumonia. Ann Trop Paediatr. 1992;12(4):455–462. doi: 10.1080/02724936.1992.11747614. [DOI] [PubMed] [Google Scholar]
- 28.Straus W.L., Qazi S.A., Kundi Z. Antimicrobial resistance and clinical effectiveness of co-trimoxazole versus amoxycillin for pneumonia among children in Pakistan: randomised controlled trial. Pakistan Co-trimoxazole Study Group. Lancet. 1998;352(9124):270–274. doi: 10.1016/s0140-6736(97)10294-x. [DOI] [PubMed] [Google Scholar]
- 29.Kabra S.K., Lodha R., Pandey R.M. Antibiotics for community acquired pneumonia in children. Cochrane Database Syst Rev. 2006;3 doi: 10.1002/14651858.CD004874.pub2. CD004874. [DOI] [PubMed] [Google Scholar]
- 30.Schrag S.J., McGee L., Whitney C.G. Emergence of Streptococcus pneumoniae with very-high-level resistance to penicillin. Antimicrobial Agents Chemother. 2004;48(8):3016–3023. doi: 10.1128/AAC.48.8.3016-3023.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Low D.E., Pichichero M.E., Schaad U.B. Optimizing antibacterial therapy for community-acquired respiratory tract infections in children in an era of bacterial resistance. Clin Pediatr (Phila) 2004;43(2):135–151. doi: 10.1177/000992280404300203. [DOI] [PubMed] [Google Scholar]
- 32.Whitney C.G., Farley M.M., Hadler J. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343(26):1917–1924. doi: 10.1056/NEJM200012283432603. [DOI] [PubMed] [Google Scholar]
- 33.Deeks S.L., Palacio R., Ruvinsky R. Risk factors and course of illness among children with invasive penicillin-resistant Streptococcus pneumoniae. The Streptococcus pneumoniae Working Group. Pediatrics. 1999;103(2):409–413. doi: 10.1542/peds.103.2.409. [DOI] [PubMed] [Google Scholar]
- 34.Friedland I.R. Comparison of the response to antimicrobial therapy of penicillin-resistant and penicillin-susceptible pneumococcal disease. Pediatr Infect Dis J. 1995;14(10):885–890. doi: 10.1097/00006454-199510000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Tan T.Q., Mason E.O., Jr., Barson W.J. Clinical characteristics and outcome of children with pneumonia attributable to penicillin-susceptible and penicillin-nonsusceptible Streptococcus pneumoniae. Pediatrics. 1998;102(6):1369–1375. doi: 10.1542/peds.102.6.1369. [DOI] [PubMed] [Google Scholar]
- 36.Doern G.V., Jones R.N., Pfaller M.A. Haemophilus influenzae and Moraxella catarrhalis from patients with community-acquired respiratory tract infections: antimicrobial susceptibility patterns from the SENTRY Antimicrobial Surveillance Program (United States and Canada, 1997) Antimicrob Agents Chemother. 1999;43(2):385–389. doi: 10.1128/aac.43.2.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gorak E.J., Yamada S.M., Brown J.D. Community-acquired methicillin-resistant Staphylococcus aureus in hospitalized adults and children without known risk factors. Clin Infect Dis. 1999;29(4):797–800. doi: 10.1086/520437. [DOI] [PubMed] [Google Scholar]
- 38.Gang R.K., Sanyal S.C., Mokaddas E. Rifampicin as an adjunct to vancomycin therapy in MRSA septicaemia in burns. Bur. 1999;25(7):640–644. doi: 10.1016/s0305-4179(99)00045-5. [DOI] [PubMed] [Google Scholar]
- 39.Mulholland K., Hilton S., Adegbola R. Randomised trial of Haemophilus influenzae type-b tetanus protein conjugate vaccine [corrected] for prevention of pneumonia and meningitis in Gambian infants. Lancet. 1997;349(9060):1191–1197. doi: 10.1016/s0140-6736(96)09267-7. [DOI] [PubMed] [Google Scholar]
- 40.Levine O.S., Lagos R., Munoz A. Defining the burden of pneumonia in children preventable by vaccination against Haemophilus influenzae type b. Pediatr Infect Dis J. 1999;18(12):1060–1064. doi: 10.1097/00006454-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Gessner B.D., Sutanto A., Linehan M. Incidences of vaccine-preventable Haemophilus influenzae type b pneumonia and meningitis in Indonesian children: hamlet-randomised vaccine-probe trial. Lancet. 2005;365(9453):43–52. doi: 10.1016/s0140-6736(04)17664-2. [DOI] [PubMed] [Google Scholar]
- 42.Black S., Shinefield H., Fireman B. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J. 2000;19(3):187–195. doi: 10.1097/00006454-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Klugman K.P., Madhi S.A., Huebner R.E. A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med. 2003;349(14):1341–1348. doi: 10.1056/NEJMoa035060. [DOI] [PubMed] [Google Scholar]
- 44.Cutts F.T., Zaman S.M., Enwere G. Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: randomised, double-blind, placebo-controlled trial. Lancet. 2005;365(9465):1139–1146. doi: 10.1016/S0140-6736(05)71876-6. [DOI] [PubMed] [Google Scholar]
- 45.Obaro S.K., Madhi S.A. Bacterial pneumonia vaccines and childhood pneumonia: are we winning, refining, or redefining? Lancet Infect Dis. 2006;6(3):150–161. doi: 10.1016/S1473-3099(06)70411-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whitney C.G., Pilishvili T., Farley M.M. Effectiveness of seven-valent pneumococcal conjugate vaccine against invasive pneumococcal disease: a matched case-control study. Lancet. 2006;368(9546):1495–1502. doi: 10.1016/S0140-6736(06)69637-2. [DOI] [PubMed] [Google Scholar]
- 47.Cohen R., Levy C., de La R.F. Impact of pneumococcal conjugate vaccine and of reduction of antibiotic use on nasopharyngeal carriage of nonsusceptible pneumococci in children with acute otitis media. Pediatr Infect Dis J. 2006;25(11):1001–1007. doi: 10.1097/01.inf.0000243163.85163.a8. [DOI] [PubMed] [Google Scholar]
- 48.Mulholland K. Childhood pneumonia mortality—a permanent global emergency. Lancet. 2007;370(9583):285–289. doi: 10.1016/S0140-6736(07)61130-1. [DOI] [PubMed] [Google Scholar]
- 49.Grove R.D., Hetzel A.M. US National Center for Health Statistics; Washington DC: 1968. Vital statistics rates in the United States 1940–1960. 2008. [Google Scholar]
- 50.Bryce J., Boschi-Pinto C., Shibuya K. WHO estimates of the causes of death in children. Lancet. 2005;365(9465):1147–1152. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 51.Jones G., Steketee R.W., Black R.E. How many child deaths can we prevent this year? Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 52.Sazawal S., Black R.E. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: a meta-analysis of community-based trials. Lancet Infect Dis. 2003;3(9):547–556. doi: 10.1016/s1473-3099(03)00737-0. [DOI] [PubMed] [Google Scholar]
- 53.Pandey M.R., Sharma P.R., Gubhaju B.B. Impact of a pilot acute respiratory infection (ARI) control programme in a rural community of the hill region of Nepal. Ann Trop Paediatr. 1989;9(4):212–220. doi: 10.1080/02724936.1989.11748635. [DOI] [PubMed] [Google Scholar]
- 54.Pandey M.R., Daulaire N.M., Starbuck E.S. Reduction in total under-five mortality in western Nepal through community-based antimicrobial treatment of pneumonia. Lancet. 1991;338(8773):993–997. doi: 10.1016/0140-6736(91)91847-n. [DOI] [PubMed] [Google Scholar]
- 55.WHO . World Health Organization; Geneva, Switzerland: 1991. Programme for the control of acute respiratory infections. Technical basis for the WHO recommendations on the management of pneumonia in children at first level health facilities. [Google Scholar]
- 56.Kielmann A.A., Taylor C.E., DeSweemer C. The Narangwal experiment on interactions of nutrition and infections: II. Morbidity and mortality effects. Indian J Med Res. 1978;68(Suppl):21–41. [PubMed] [Google Scholar]
- 57.Mtango F.D., Neuvians D. Acute respiratory infections in children under five years. Control project in Bagamoyo District, Tanzania. Trans R Soc Trop Med Hyg. 1986;80(6):851–858. doi: 10.1016/0035-9203(86)90241-5. [DOI] [PubMed] [Google Scholar]
- 58.Khan A.J., Khan J.A., Akbar M. Acute respiratory infections in children: a case management intervention in Abbottabad District, Pakistan. Bull World Health Organ. 1990;68(5):577–585. [PMC free article] [PubMed] [Google Scholar]
- 59.World Health Organization . WHO; Geneva: 1998. Case management of acute respiratory infections in children: intervention studies. WHO/ARI/88 2. [Google Scholar]
- 60.Bang A.T., Bang R.A., Tale O. Reduction in pneumonia mortality and total childhood mortality by means of community-based intervention trial in Gadchiroli, India. Lancet. 1990;336(8709):201–206. doi: 10.1016/0140-6736(90)91733-q. [DOI] [PubMed] [Google Scholar]
- 61.Fauveau V., Stewart M.K., Chakraborty J. Impact on mortality of a community-based programme to control acute lower respiratory tract infections. Bull World Health Organ. 1992;70(1):109–116. [PMC free article] [PubMed] [Google Scholar]
- 62.Roesin R., Sutanto A., Sastra K. ARI intervention study in Kediri, Indonesia (a summary of study results) Bull Int Union Tuberc Lung Dis. 1990;65(4):23. [PubMed] [Google Scholar]
- 63.CATCHUP study group Clinical efficacy of co-trimoxazole versus amoxicillin twice daily for treatment of pneumonia: a randomised controlled clinical trial in Pakistan. Arch Dis Child. 2002;86(2):113–118. doi: 10.1136/adc.86.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mulholland E.K., Falade A.G., Corrah P.T. A randomized trial of chloramphenicol vs. trimethoprim-sulfamethoxazole for the treatment of malnourished children with community-acquired pneumonia. Pediatr Infect Dis J. 1995;14(11):959–965. doi: 10.1097/00006454-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 65.Campbell H., Byass P., Forgie I.M. Trial of co-trimoxazole versus procaine penicillin with ampicillin in treatment of community-acquired pneumonia in young Gambian children. Lancet. 1988;2(8621):1182–1184. doi: 10.1016/s0140-6736(88)90244-9. [DOI] [PubMed] [Google Scholar]
- 66.Sidal M., Oguz F., Unuvar A. Trial of co-trimoxazole versus procaine penicillin G and benzathin penicillin + procaine penicillin G in the treatment of childhood pneumonia. J Trop Pediatr. 1994;40(5):301–304. doi: 10.1093/tropej/40.5.301. [DOI] [PubMed] [Google Scholar]
- 67.Hazir T., Fox L.M., Nisar Y.B. Ambulatory short-course high-dose oral amoxicillin for treatment of severe pneumonia in children: a randomised equivalency trial. Lancet. 2008;371(9606):49–56. doi: 10.1016/S0140-6736(08)60071-9. [DOI] [PubMed] [Google Scholar]
- 68.Asghar R., Banajeh S., Egas J. Chloramphenicol versus ampicillin plus gentamicin for community acquired very severe pneumonia among children aged 2–59 months in low resource settings: multicentre randomised controlled trial (SPEAR study) BMJ. 2008;336(7635):80–84. doi: 10.1136/bmj.39421.435949.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hazir T., Qazi S.A., Bin N.Y. Comparison of standard versus double dose of amoxicillin in the treatment of non-severe pneumonia in children aged 2–59 months: a multi-centre, double blind, randomised controlled trial in Pakistan. Arch Dis Child. 2007;92(4):291–297. doi: 10.1136/adc.2005.092494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maher D., Raviglione M. Global epidemiology of tuberculosis. Clin Chest Med. 2005;26(2):167–182. doi: 10.1016/j.ccm.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 71.Atkinson P., Taylor H., Sharland M. Resurgence of paediatric tuberculosis in London. Arch Dis Child. 2002;86(4):264–265. doi: 10.1136/adc.86.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shah N.S., Harrington T., Huber M. Increased reported cases of tuberculosis among children younger than 5 years of age, Maricopa County, Arizona, 2002–2003. Pediatr Infect Dis J. 2006;25(2):151–155. doi: 10.1097/01.inf.0000189987.94158.83. [DOI] [PubMed] [Google Scholar]
- 73.Tuberculosis Coalition for Technical Assistance International standards for tuberculosis care. 2008. 2008. www.istcweb.org/materials.html Available at: Accessed July 2008.
- 74.Smuts N.A., Beyers N., Gie R.P. Value of the lateral chest radiograph in tuberculosis in children. Pediatr Radiol. 1994;24(7):478–480. doi: 10.1007/BF02015003. [DOI] [PubMed] [Google Scholar]
- 75.Swingler G.H., du T.G., Andronikou S. Diagnostic accuracy of chest radiography in detecting mediastinal lymphadenopathy in suspected pulmonary tuberculosis. Arch Dis Child. 2005;90(11):1153–1156. doi: 10.1136/adc.2004.062315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abadco D.L., Steiner P. Gastric lavage is better than bronchoalveolar lavage for isolation of Mycobacterium tuberculosis in childhood pulmonary tuberculosis. Pediatr Infect Dis J. 1992;11(9):735–738. doi: 10.1097/00006454-199209000-00013. [DOI] [PubMed] [Google Scholar]
- 77.Ranganathan S., Connell T., Curtis N. Interferon-gamma release assays in children—no better than tuberculin skin testing? J Infect. 2007;54(4):412–413. doi: 10.1016/j.jinf.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 78.Connell T.G., Curtis N., Ranganathan S.C. Performance of a whole blood interferon gamma assay for detecting latent infection with Mycobacterium tuberculosis in children. Thorax. 2006;61(7):616–620. doi: 10.1136/thx.2005.048033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schaaf H.S., Parkin D.P., Seifart H.I. Isoniazid pharmacokinetics in children treated for respiratory tuberculosis. Arch Dis Child. 2005;90(6):614–618. doi: 10.1136/adc.2004.052175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Simoes E.A., Cherian T., Chow J. Acute respiratory infections in children. In: Jamieson D.T., Breman J.G., Measham A.R., editors. Disease control priorities in developing countries. Oxford University Press; New York: 2006. pp. 483–498. [Google Scholar]
- 81.Management of children with pneumonia and HIV in low-resource settings. Report of a consultative meeting. Harare, Zimbabwe, 2003. Geneva: World Health Organization; 2004.
- 82.McNally L.M., Jeena P.M., Gajee K. Effect of age, polymicrobial disease, and maternal HIV status on treatment response and cause of severe pneumonia in South African children: a prospective descriptive study. Lancet. 2007;369(9571):1440–1451. doi: 10.1016/S0140-6736(07)60670-9. [DOI] [PubMed] [Google Scholar]
- 83.Qian Z.X. Thoracic hydatid cysts: a report of 842 cases treated over a thirty-year period. Ann Thorac Surg. 1988;46(3):342–346. doi: 10.1016/s0003-4975(10)65941-3. [DOI] [PubMed] [Google Scholar]
- 84.Kilani T., El H.S. Pulmonary hydatid and other lung parasitic infections. Curr Opin Pulm Med. 2002;8(3):218–223. doi: 10.1097/00063198-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 85.Cohen H.G., Reynolds T.B. Comparison of metronidazole and chloroquine for the treatment of amoebic liver abscess. A controlled trial. Gastroenterology. 1975;69(1):35–41. [PubMed] [Google Scholar]
- 86.Cameron E.W. The treatment of pleuropulmonary amebiasis with metronidazole. Chest. 1978;73(5):647–650. doi: 10.1378/chest.73.5.647. [DOI] [PubMed] [Google Scholar]
- 87.Ibarra-Perez C., Selman-Lama M. Diagnosis and treatment of amebic “empyema”: report of eighty-eight cases. Am J Surg. 1977;134(2):283–287. doi: 10.1016/0002-9610(77)90364-6. [DOI] [PubMed] [Google Scholar]
- 88.Ibarra-Perez C. Thoracic complications of amebic abscess of the liver: report of 501 cases. Chest. 1981;79(6):672–677. doi: 10.1378/chest.79.6.672. [DOI] [PubMed] [Google Scholar]
- 89.Parab P.B., Samuel A.M., Udwadia F.E. Hypersensitivity reaction in tropical eosinophilia. Indian J Med Res. 1979;69:122–127. [PubMed] [Google Scholar]
- 90.Ottesen E.A., Nutman T.B. Tropical pulmonary eosinophilia. Annu Rev Med. 1992;43:417–424. doi: 10.1146/annurev.me.43.020192.002221. [DOI] [PubMed] [Google Scholar]
- 91.Ganatra R.D., Sheth U.K., Lewis R.A. Diethylcarbamazine (Hetrazan) in tropical eosinophilia. Indian J Med Res. 1958;46(2):205–222. [PubMed] [Google Scholar]
- 92.Pinkston P., Vijayan V.K., Nutman T.B. Acute tropical pulmonary eosinophilia. Characterization of the lower respiratory tract inflammation and its response to therapy. J Clin Invest. 1987;80(1):216–225. doi: 10.1172/JCI113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thomson A.H., Hull J., Kumar M.R. Randomised trial of intrapleural urokinase in the treatment of childhood empyema. Thorax. 2002;57(4):343–347. doi: 10.1136/thorax.57.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sonnappa S., Cohen G., Owens C.M. Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Am J Respir Crit Care Med. 2006;174(2):221–227. doi: 10.1164/rccm.200601-027OC. [DOI] [PubMed] [Google Scholar]
- 95.Kurt B.A., Winterhalter K.M., Connors R.H. Therapy of parapneumonic effusions in children: video-assisted thoracoscopic surgery versus conventional thoracostomy drainage. Pediatrics. 2006;118(3):e547–e553. doi: 10.1542/peds.2005-2719. [Epub 2006 Aug 14] [DOI] [PubMed] [Google Scholar]
- 96.Avansino J.R., Goldman B., Sawin R.S. Primary operative versus nonoperative therapy for pediatric empyema: a meta-analysis. Pediatrics. 2005;115(6):1652–1659. doi: 10.1542/peds.2004-1405. [DOI] [PubMed] [Google Scholar]
- 97.Victoria M.S., Steiner P., Rao M. Persistent postpneumonic pneumatoceles in children. Chest. 1981;79(3):359–361. doi: 10.1378/chest.79.3.359. [DOI] [PubMed] [Google Scholar]
- 98.Imamoglu M., Cay A., Kosucu P. Pneumatoceles in postpneumonic empyema: an algorithmic approach. J Pediatr Surg. 2005;40(7):1111–1117. doi: 10.1016/j.jpedsurg.2005.03.048. [DOI] [PubMed] [Google Scholar]
- 99.Asher M.I., Spier S., Beland M. Primary lung abscess in childhood: the long-term outcome of conservative management. Am J Dis Child. 1982;136(6):491–494. doi: 10.1001/archpedi.1982.03970420015002. [DOI] [PubMed] [Google Scholar]
- 100.van Sonnenberg E., D'Agostino H.B., Casola G. Lung abscess: CT-guided drainage. Radiology. 1991;178(2):347–351. doi: 10.1148/radiology.178.2.1987590. [DOI] [PubMed] [Google Scholar]
- 101.Yen C.C., Tang R.B., Chen S.J. Pediatric lung abscess: a retrospective review of 23 cases. J Microbiol Immunol Infect. 2004;37(1):45–49. [PubMed] [Google Scholar]
- 102.Chan P.C., Huang L.M., Wu P.S. Clinical management and outcome of childhood lung abscess: a 16-year experience. J Microbiol Immunol Infect. 2005;38(3):183–188. [PubMed] [Google Scholar]
- 103.Balfour-Lynn I.M., Abrahamson E., Cohen G. BTS guidelines for the management of pleural infection in children. Thorax. 2005;60(Suppl 1):i1–i21. doi: 10.1136/thx.2004.030676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Puskas J.D., Mathisen D.J., Grillo H.C. Treatment strategies for bronchopleural fistula. J Thorac Cardiovasc Surg. 1995;109(5):989–995. doi: 10.1016/S0022-5223(95)70325-X. [DOI] [PubMed] [Google Scholar]
- 105.Hallows M.R., Parikh D.H. Surgical management of children with pyopneumothorax: serratus anterior digitation flap. J Pediatr Surg. 2004;39(7):1122–1124. doi: 10.1016/j.jpedsurg.2004.03.074. [DOI] [PubMed] [Google Scholar]