Abstract
Objectives
To explore the behaviour-related factors influencing influenza vaccination among elderly people using a framework derived from the Health Belief Model (HBM) and the Theory of Reasoned Action (TRA).
Study design
Systematic review.
Methods
Five databases were searched using predetermined strategies in March 2016, and 1927 citations were identified. Articles were selected according to inclusion and exclusion criteria. Key information was extracted from selected studies using a predesigned sheet. Both authors assessed study quality using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) or Critical Appraisal Skills Programme (CASP) checklist.
Results
Thirty-six articles were selected. A new framework was proposed that contributes to shared understanding of factors influencing health behaviour. Possible determinants of influenza vaccination among elderly people were knowledge, health promotion factors, all constructs of the HBM, and some concepts of the TRA. Key factors were threat perception, behavioural beliefs, subjective norms, recommendations, past behaviour and perceived barriers.
Conclusions
This is the first systematic review to analyse the factors influencing influenza vaccination behaviour of elderly people using a framework integrating the HBM and the TRA. The framework identified key factors of influenza vaccination and presented the inter-relation of behaviour-related variables. However, further well-designed studies are required to explore the inter-relationships accurately and comprehensively.
Keywords: Seasonal influenza, Vaccination, Elderly, Health behaviour, Systematic review
Highlights
-
•
Influenza vaccination behaviour in the elderly was associated with demographic factors, health promotion factors and knowledge.
-
•
All constructs of Health Belief Model and some of Theory of Reasoned Action were included in the synthesised framework.
-
•
Keys were threat perception, behavioural beliefs, subjective norms, recommendation, past behaviour and perceived barrier.
-
•
Effective interventions include medical staff's recommendation, peer education, express vaccination clinic, and home visit.
Introduction
Seasonal influenza is an acute infectious disease that may lead to severe illness and death, especially among young children, elderly people and those with chronic illnesses. The annual burden of seasonal influenza is estimated to be 3–5 million cases of severe illness and approximately 250,000–500,000 deaths globally.1 In the United States, elderly people (aged ≥65 years) account for approximately 90% of influenza-associated deaths.2 Vaccination is recommended as the most effective way to prevent seasonal influenza by the World Health Organisation,1 the US Centers for Disease Control and Prevention3 and the European Centre for Disease Control and Prevention.4 These agencies urge elderly people to be vaccinated against influenza each year. Evidence suggests that the influenza vaccine has a moderate preventive effect among elderly people and that it significantly decreases the morbidity of influenza and pneumonia,5 respiratory or cardiovascular complications6 and risk of hospitalisation and death.7, 8, 9, 10 A Cochrane review11 confirmed the safety of the influenza vaccine but found no convincing evidence for its effectiveness. However, the use of inappropriate analytic techniques cast doubt on these findings. Beyer et al.12 reanalysed the same data using a biological and conceptual framework and found meaningful predictions for the effectiveness of the influenza vaccine that supported ongoing efforts to vaccinate elderly people.
The 10th Resolution of the World Health Assembly in 2003 set a vaccination coverage goal of above 50% by 2006 and 75% by 2010 among the elderly population.13 Few countries have achieved this goal despite national campaigns and interventions implemented in local settings.14 In the United States, 66.2% of elderly people received seasonal influenza vaccines during the 2012/2013 influenza season.15 Most European countries maintained a vaccination rate of 50–60% among elderly people during the 2010/2011 influenza season, with 82% in the Netherlands and 75% in the UK.16 The situation is worse in developing countries. In Mainland China, only 4.3% of adults aged ≥60 years reported receiving the influenza vaccine during the 2011/2012 season.17 The vaccination coverage of those aged >65 years was 10% in Romania, 12% in Poland and 14% in South Africa in the 2005/2006 influenza season.18, 19
It is imperative to understand key factors influencing influenza vaccination among elderly people to develop effective strategies to increase vaccination coverage. Previous studies have tried to summarise the reasons for accepting or refusing vaccination20 or to identify predictors of vaccination with more attention on organisational factors.21 Another literature review22 analysed studies conducted in the UK or research findings that could be transferred to the UK setting; it thus failed to acknowledge cross-cultural practices. Few studies used seasonal influenza vaccination as health behaviour or explored behaviour-related factors.
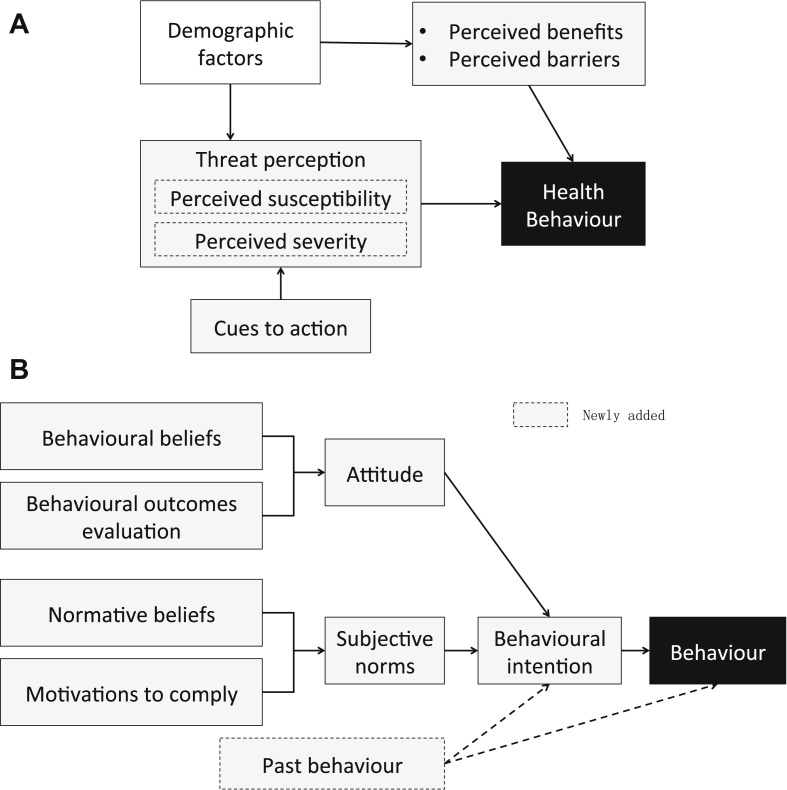
The Health Belief Model (HBM, see Fig. 1 A)23 and the Theory of Reasoned Action (TRA, see Fig. 1B)24 have been used widely in health behaviour studies. Researchers have criticised the HBM for neglecting the influence of social factors (i.e. social norms).25 Subjective norms in the TRA complemented this with individual behavioural perception under various cultural backgrounds. On the other hand, the TRA also has limitations, as it neglects the influence of emotions on behaviours, including threat and fear,26 which could be complemented with threat perception in the HBM. Therefore, the two theories have been integrated into one research framework in many studies.27, 28, 29 This review aimed to determine the factors influencing influenza vaccination behaviour among elderly people using an integrated framework derived from these two theories.
Fig. 1.
(A) Health Belief Model and (B) Theory of Reasoned Action.
Methods
Search strategy
A literature search was conducted in March 2016. The following databases were searched electronically: PubMed (1874–2016), Embase (1945–2016), Science Collection Index Expanded (2007–2016), CINAHL (1939–2016) and Elsevier. The search process is shown in Table A (see online supplementary material). There were four groups of keywords when conducted literature search, such as influenza, vaccination, elderly people, and knowledge/attitude/acceptance/perception/intention, and their synonyms or alternative spelling, see Table A. In consideration of search sensitivity and comprehensiveness, the former three groups of keywords were refined to ‘title or abstract’ in some databases, while no restriction was set on the fourth group.
Literature selection
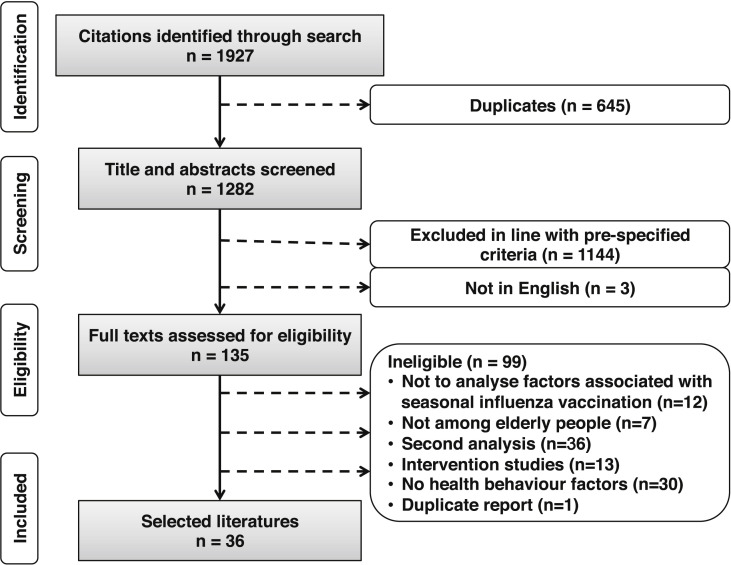
The initial electronic search produced 1927 citations. No other method was used for the primary search. Attempts were made to contact study authors in order to obtain inaccessible full texts. No efforts were spared to obtain unpublished data or informally published literature. Titles and abstracts were screened manually by one author according to the inclusion and exclusion criteria (see Box 1 ). The other author examined the entire screening process. Thirty-six full texts30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65 were included for further analysis through the selection process presented in Fig. 2 . Two articles reported data from the same study,50, 66 so only one article50 was included.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria:
-
•
Studies that analysed factors associated with seasonal influenza vaccination
-
•
Age ≥60 years
-
•
Cross-sectional, longitudinal and qualitative studies
-
•
English language
-
•
No restriction on publication year, research country or setting
Exclusion criteria:
-
•
Vaccination against pandemic influenza or pneumonia
-
•
Articles that explored determinants not including health behaviour factors
-
•
Intervention studies or second analysis studies based on national surveys or other data sources
-
•
Duplicate reports of the same research
Fig. 2.
Flow chart of literature selection process.
Information extraction and quality assessment
The following key information was extracted from the studies by one author: study country/countries, study design and sample, survey instruments and data collection and main findings (Table B, see online supplementary material). The other author checked the information to ensure reliability. The quality of selected studies was assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)67 or Critical Appraisal Skills Programme (CASP) checklist.68 As different quality appraisal approaches lack consistency in the inclusion criteria,21, 69 no studies were excluded; instead, quality levels were provided. Tables C and D (see online supplementary material) show the assessment process. Table 1 presents the final quality rating.
Table 1.
Involved factors and quality rating of included studies.
| First author, date and country | Demographic factors | Knowledge/information | Health promotion factors | Health behavioural factors |
Quality rating | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Threat perception |
Perceived barriers | Cues to action |
Behavioural beliefs |
Subjective norms |
Behavioural expe-rience | Behav-ioural intention | |||||||||
| Perceived susceptibility | Perceived severity | Recommendation | Disease experience | Perceived-efficacy | Perceived safety | Norm-ative beliefs | Motiv-ations to reply | ||||||||
| Frank, 1985, Canada30 | √ | √ | √ | √ | Low | ||||||||||
| Pearson, 1994, USA31 | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | |||||
| Honkanen, 1996, Finland32 | √ | √ | √ | √ | √ | √ | Moderate | ||||||||
| Van Essen, 1997, Netherlands33 | √ | √ | √ | √ | √ | √ | Moderate | ||||||||
| Nexøe, 1999, Denmark34 | √ | √ | √ | √ | √ | √ | √ | High | |||||||
| Pregliasco, 1999, Italy35 | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||||
| Abramson, 2000, Israel36 | √ | √ | √ | √ | √ | Moderate | |||||||||
| Armstrong, 2001, USA37 | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||||
| Santibanez, 2002, USA38 | √ | √ | √ | √ | √ | √ | High | ||||||||
| Evans, 2003, UK39 | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | |||||
| Madhavan, 2004, USA40 | √ | √ | √ | √ | √ | High | |||||||||
| Chi, 2004, USA41 | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||
| Zimmerman, 2004, USA42 | √ | √ | √ | √ | High | ||||||||||
| Bardenheier, 2006, USA43 | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | |||||
| Gallagher, 2006, UK44 | √ | √ | √ | √ | Moderate | ||||||||||
| Mangtani, 2006, UK45 | √ | √ | √ | √ | √ | √ | Moderate | ||||||||
| Winston, 2006, USA46 | √ | √ | √ | √ | Moderate | ||||||||||
| Lau, 2007, Hong Kong47 | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | High | |||
| Kwong, 2009, Hong Kong48 | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||||
| Kwong, 2008, Hong Kong49 | √ | √ | √ | √ | √ | √ | √ | Low | |||||||
| Lau, 2008, Hong Kong50 | √ | √ | √ | √ | √ | √ | √ | √ | √ | High | |||||
| Lau, 2009, Hong Kong51 | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||
| Avelino-Silva, 2011, Brazil52 | √ | √ | √ | √ | √ | √ | √ | Low | |||||||
| Matsui, 2011, Japan53 | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | |||||
| Yu, 2014, Hong Kong54 | √ | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | |||||
| Boggavarapu, 2014, USA55 | √ | √ | √ | √ | √ | Moderate | |||||||||
| Bödeker, 2015, Germany56 | √ | √ | √ | √ | √ | √ | √ | √ | Moderate | ||||||
| Mo, 2015, Hong Kong57 | √ | √ | √ | √ | √ | √ | √ | √ | High | ||||||
| Klett-Tammen, 2016, Germany58 | √ | √ | √ | √ | √ | √ | √ | √ | High | ||||||
| Cornford, 1999, UK59 | √ | √ | √ | √ | Moderate | ||||||||||
| Telford, 2003, UK60 | √ | √ | √ | √ | √ | Moderate | |||||||||
| Evans, 2007, UK61 | √ | √ | √ | √ | √ | √ | High | ||||||||
| Cameron, 2009, USA62 | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | High | ||||
| Payaprom, 2010, Thailand63 | √ | √ | √ | √ | √ | ||||||||||
| Kwong, 2010, nine countries64 | √ | √ | √ | √ | √ | Moderate | |||||||||
| Dixon-Woods, 2004, UK65 | √ | √ | √ | √ | √ | √ | Moderate | ||||||||
Framework synthesis
All the constructs of the HBM and the TRA were included initially. One author classified the influencing factors surveyed in each study into a specific construct according to the meaning of the construct defined by the theories. Constructs with the same meaning were taken as one construct, and constructs were excluded if not explored by any study. The other author checked the classification and proposed disagreement, if any. Agreement was achieved through discussion. The construct analysed in the included studies is shown in Table 1. The inter-relationship of the constructs was developed based on the two theories and the evidence in the included studies.
Results
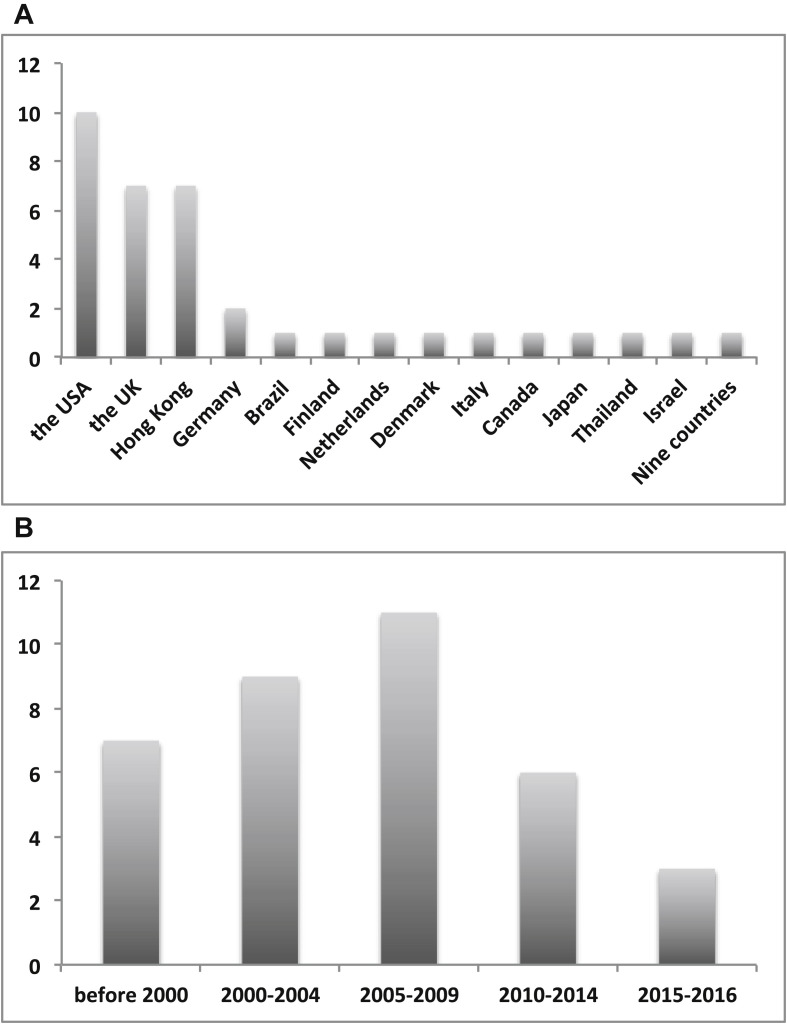
The distribution of country and year of publication of the 36 studies is presented in Fig. 3 . Thirty-three studies were conducted in developed countries or regions, and two studies52, 63 were conducted in developing countries. One study conducted by Hong Kong researchers recruited samples from nine countries, including China (Mainland China and Hong Kong), Indonesia, Turkey, South Korea, Greece, Canada, the UK, Brazil and Nigeria.64 All studies had been published since 1985, and most studies were published in the decade from 2000 to 2009 (n = 20). Table B (see online supplementary material) summarises the design features and main findings. Ten studies were rated as high quality using the STROBE or CASP checklist, most studies were of moderate quality, and three were rated as low quality.
Fig. 3.
Distribution of (A) country and (B) year of publication of included studies.
Twenty-seven studies evaluated seasonal influenza vaccination coverage among elderly people, which ranged from 26%35 to 84%.33 Only seven studies reported vaccine uptake rates ≥75%, and 10 studies reported rates ≤50%.
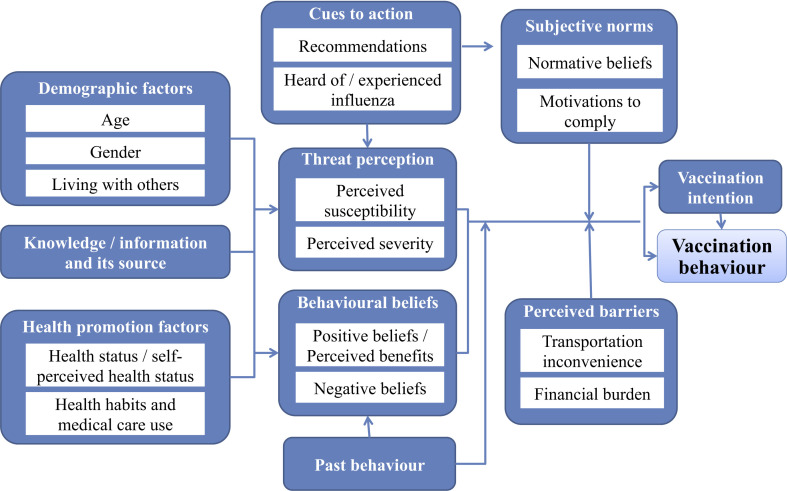
A new framework was synthesised based on all 36 studies (see Fig. 4 ). In the context of influenza vaccination behaviour among elderly people, the meaning of perceived benefits from the HBM was as same as that of positive behavioural beliefs from the TRA. Therefore, the two constructs were taken as one in the analysis. No study surveyed behavioural outcomes evaluation of the TRA, so this construct was excluded from the research framework. Attitude was also excluded as it was measured by multiplying the score of behavioural outcomes evaluation and behavioural beliefs.
Fig. 4.
Synthesis framework based on findings of included studies.
Demographic factors
Age
One study found that elderly people aged >75 years were more compliant regarding influenza vaccination than younger people.33 Three studies39, 47, 56 obtained similar findings, with a higher vaccination rate found among people aged 70–79 years compared with younger age groups. However, another study found that people aged >85 years were less likely to have been vaccinated than younger age groups.51 Elderly people aged 70–84 years seemed to have a higher vaccination rate than other age groups, but further evidence is needed.
Sex
Three studies47, 56, 57 suggested that elderly females were more likely to have a vaccination history and to have been vaccinated in the last 6 months than elderly males. Among these three studies, one was high quality47 and two were moderate quality.56, 57 However, another study45 reported that vaccination coverage was higher among elderly males than elderly females. This study was of moderate quality.
Living with others
Living with another person predicted vaccination uptake in a study in Denmark.34 A study in Hong Kong also reported that elderly people who lived with family members were more likely to have been vaccinated in the last 6 months.47
Health promotion factors
Health status and self-perceived health status
Influenza vaccination coverage was higher among elderly people with one or more chronic diseases than among healthier elderly people.32, 39, 56, 57 Lau et al.51 found that elderly people with fewer chronic diseases were more likely to have been vaccinated than those with three or more diseases. However, this study also found that those with better physical function were more likely to have been vaccinated. The majority of the participants in this study had good physical status, which might be the reason for the contradiction. The five studies were all of moderate quality. Several studies33, 39, 49, 51, 58 indicated that self-perceived poor health status encouraged vaccination behaviour, while self-perceived good health was the most common reason for vaccination refusal.
Health habits and medical service use
Bad health habits (e.g. smoking) were associated with vaccination refusal.42, 53 Medical service use was another influencing factor; elderly people who had visited a clinic in the last 3 months36 or had hospitalisation follow-ups in the previous year51 were more likely to have been vaccinated. Furthermore, some medical services (i.e. colon cancer screening) were associated with influenza vaccination.42
Knowledge/information and its sources
Elderly adults who scored more highly on knowledge questions were more likely to have been vaccinated40, 51, 57, 58 while unvaccinated subjects knew little about influenza symptoms38 and the side-effects of the vaccine.39 Elderly people would have more positive beliefs towards vaccination and be more likely to accept vaccination if they received knowledge/information from healthcare professionals.32, 53 Knowledge/information had a negative effect on vaccination uptake when elderly people used mass media as knowledge/information sources.53 However, mass media remained among the most widely cited sources.32, 53
Health behaviour factors
Threat perception
Perceived susceptibility
Vaccinated elderly people tended to believe that they were vulnerable and could contract influenza easily,42, 48, 51, 53 whereas unvaccinated elderly people perceived that they had low susceptibility to influenza.33, 36, 38, 40, 49, 52 Perception of a greater likelihood of contracting influenza also facilitated the first influenza vaccine.30 A qualitative study in the United States with African-American elderly people revealed that perception of susceptibility was influenced by perceived health status, age and prevalence of influenza.62
Perceived severity
Perceived severity was weakly correlated with vaccination acceptance.34, 41, 56 Vaccinated elderly people agreed more strongly that influenza would cause serious complications and change daily activities48 while unvaccinated elderly people did not think that influenza or its complications were serious.49 This result was supported by a qualitative study.59 Of 50 interviewees aged >75 years in the UK, 40 felt that influenza was fatal for very old people and those with low resistance or severe diseases. However, they did not think that influenza was a risk to their own health. Interviewees who had experienced severe symptoms previously perceived that influenza was fatal or exacerbated comorbidities.62
Some studies examined perceived susceptibility and severity together as perceived risk. In a qualitative study in Thailand, vaccinated participants reported a risk perception of contracting influenza, whereas others stated that they might be vaccinated only when an outbreak occurred.63 Two qualitative studies found that self-perceived low health status, and experiencing or observing influenza and its complications, increased threat perception, which made those who initially refused vaccination decide to receive the vaccine in the subsequent season.60, 64
Perceived barriers
Perceived barriers predicted vaccine refusal by elderly people, including perceived transportation inconvenience and financial burden. Some studies suggested that perceived transportation inconvenience and perceived long travelling time to obtain the influenza vaccination were associated with less willingness to be vaccinated.37, 48, 49, 50, 53, 58 Perceived financial difficulties were a hindering factor for previous vaccination history and vaccination in the last 6 months.47 Another study suggested that elderly people would consider vaccination if it was free.63
Cues to action
Recommendations
Elderly people cited recommendation from medical staff as a reason for accepting vaccination.33, 45, 52 A qualitative study reported that an individual prompt from a general physician was the most significant motivator.61 In addition, 14 studies indicated that advice or a reminder letter from a health provider was strongly associated with vaccination uptake.30, 31, 34, 37, 39, 41, 46, 47, 48, 51, 55, 56, 57, 58 A study found that provider recommendations could overcome negative beliefs about vaccination.41 Some studies showed that the health professional's identity influenced the adoption of the advice. Medical talks presented by physicians promoted vaccination compliance, while talks presented by nurses or other providers did not.31 Recommendations from a family physician were more effective than those from a general physician.36
Recommendations from families/friends also had an influence. Elderly people in Hong Kong who received advice from family members/friends were more likely to have been vaccinated.51 Other studies showed that visiting elderly social/community centres was associated with ever being vaccinated,47 and this was the only longitudinal predictor for first-time vaccination.42 Kwong et al.48 also demonstrated that family encouragement was a positive factor but recommendation from a friend was not. Another study found that advice from friends hindered vaccination behaviour among elderly people.39
Heard of or experienced influenza/respiratory diseases
A study in the United States suggested that knowing someone with influenza was a key predictor for vaccination among elderly people.40 Elderly people were more likely to have been vaccinated if they often suffered from a upper respiratory tract infection.53 A qualitative study showed that elderly interviewees or their friends/relatives contracting influenza led to a sudden increase in threat perception, which was a key factor in subsequent vaccination acceptance.60
Behavioural beliefs
Positive beliefs about influenza vaccination/perceived benefits
Beliefs regarding vaccine efficacy were strongly associated with vaccination uptake30, 32, 41, 48, 53, 56 and ever having been vaccinated.33, 34, 40, 47, 50, 57 Other studies showed that doubts about vaccine efficacy were widely cited as a reason for refusal.39, 61 Abramson and Cohen-Noar36 found that participants who wrongly believed that the vaccine provided complete protection were more likely to accept vaccination, but those who wrongly believed that it would cause influenza tended to refuse vaccination. Dixon-Woods et al.65 classified elderly people into groups and reported that ‘sceptics’ viewed vaccines as ineffective or irrelevant because they were invulnerable to influenza. A qualitative study61 similarly reported that ‘refusers’ and ‘defaulters’ were more likely to express scepticism about vaccine effectiveness.
Negative beliefs about vaccination
One of the most common reasons for refusal of vaccination by elderly people was fear of potential side-effects, concern about the undisclosed content of the vaccine, or belief that the vaccine would cause influenza or influenza-like illness.35, 38, 45, 52 Vaccine acceptance was negatively influenced by fear of adverse events31, 32, 33, 40, 47, 50, 53, 55, 56, 57 and the belief that vaccination is painful.37, 48 Vaccination coverage was lower among those who had heard predominantly negative comments about influenza vaccines.30 Telford and Rogers reported that the experiences of relatives had a greater impact on vaccination than medical talks.60
Subjective norms
Normative beliefs
Elderly people were more likely to have been vaccinated if they believed that their doctor wanted them to receive the influenza vaccine, regardless of whether they were chronically sick or healthy.31 Madhavan et al.40 found that elderly people who believed that ‘people who are important to me think that it is important to get immunised’ scored higher on perceived benefits and were more likely to have been vaccinated. Kwong et al.64 revealed that vaccination coverage was higher in countries where normative beliefs were in favour of vaccination (i.e. South Korea, the UK and Greece). Furthermore, they found that the formation of normative beliefs depended greatly on the elderly person's own or observed positive vaccination experiences.
Motivations to comply
Vaccinated elderly people stated that they would receive the vaccine if it was recommended by a doctor or nurse.41 Elderly people whose medical decisions were influenced by family members were more likely to have a vaccination history.47
Past behaviour
Previous vaccination history was positively associated with current vaccination status.31, 32, 34, 35, 52 Likewise, prior vaccination refusal was associated with future non-vaccination behaviour.37 Elderly people with an adverse reaction history after vaccination were less likely to be vaccinated again.37, 41 Moreover, unvaccinated elderly people listed the experience of side-effects as a common reason for refusal.38 Cornford and Morgan59 found that vaccinated and unvaccinated elderly people who had experienced adverse effects had different interpretations. Prior vaccination of relatives/co-residents also influenced the vaccination decisions of elderly people.53
Behavioural intention
Three studies50, 51, 58 that used vaccination intention as an independent variable and explored its impact on vaccination behaviour suggested that those who intended to be vaccinated were more likely to have ever undergone vaccination. Five studies39, 46, 47, 50, 57 employed vaccination intention and vaccination behaviour as dependent variables, and two studies44, 54 adopted vaccination intention as the only outcome variable. Vaccination intention was positively associated with living with family members, poor health status, knowledge about influenza and influenza vaccines, perceived susceptibility of contracting influenza or severe acute respiratory syndrome, perceived severity of influenza, receiving financial allowance, perceived efficacy of vaccines, subjective norms and past vaccination behaviour and was negatively influenced by concern about side-effects and prior vaccination discomfort.
Discussion
The 36 studies in this review suggest that elderly people have suboptimal seasonal influenza vaccination coverage. Fewer studies were conducted in developing countries than developed countries. Effective promotion strategies in developed countries might not work in developing countries due to different social and cultural backgrounds. Therefore, researchers need to identify factors influencing vaccination behaviour in specific cultural backgrounds. For example, Kwong et al.64 found that elderly people cited family protection as a benefit of vaccination, which is a factor of Confucian cultural heritage. This finding indicated that vaccination campaigns that stress family protection might encourage vaccination behaviour among elderly people in such a cultural background.
The synthesis framework employed the HBM's and TRA's core constructs and complemented the limitations of the original theories. This framework identified possible factors influencing seasonal influenza vaccination among elderly people, including demographic factors, knowledge/information and its sources, health promotion factors and behaviour-related factors. As Fig. 4 shows, not all variables influenced vaccination behaviour directly. Some key factors might be mediating variables, such as threat perception and behavioural beliefs (i.e. perceived efficacy and concerns about side-effects). Other key factors included recommendations from health professionals, past behaviour and perceived barriers.
These findings contribute to future intervention strategies to increase vaccination coverage among elderly people. Elderly people tend to regard medical staff as authorities, so vaccination coverage could be increased if health providers integrated vaccination promotion into their practices. When they have a medical talk with elderly people, accurate and evidence-based information about influenza vaccination should be provided, including topics about elderly susceptibility to influenza, symptoms and severe complications of influenza, efficacy of vaccination and possible adverse events. Peer education may be another effective method, since prior vaccination was a key predictor of current vaccination decision, and visiting social centres was reported as the only significant variable of first-time vaccination.42 Vaccination promotion activities could be organised in elderly centres by inviting vaccinated elderly people to share their positive experiences of vaccination.
Transportation inconvenience and financial burden were the main perceived barriers of elderly people. The qualitative study conducted in nine countries found that different government promotion policies produced different concerns among elderly people.64 Affordability was the top concern in Turkey and China, where people have to pay for vaccination themselves, whereas in Brazil, where vaccination is covered by the national healthcare system, accessibility was the main concern. This finding demonstrates that government and healthcare institutions play a crucial role in eliminating these barriers. Methods to improve transportation convenience include establishing express vaccination clinics42 and providing home visits18 for elderly people with accessibility problems. Recently, some researchers refitted an ambulance into a mobile ‘flu stop’ and attracted many people to receive the vaccine.70
Other factors should also be taken into consideration. Sociodemographic variables (i.e. age and sex) can be used to identify target groups whose decisions can be influenced more easily by health providers. The impact of health status could also be designed as an intervention. A study showed that coverage was increased by assessing elderly people's health problems using a health risk appraisal and giving recommendations accordingly.71 Family encouragement and subjective norms influenced the vaccination behaviours of elderly people, which suggests that family members should also be included in interventions.
Limitations
This systematic review has some limitations. First, non-English language articles were not included, which may have led to exclusion of important evidence from specific cultural backgrounds. Second, a conclusion about the causal relationship cannot be drawn, as most selected studies were cross-sectional or qualitative. Third, researchers should be cautious about referring to the findings of poor-quality studies. Fourth, due to the limited resources, some inaccessible full texts were excluded without eligibility assessment.
Conclusion
To the authors' knowledge, this is the first systematic review to analyse factors influencing influenza vaccination among elderly people using a framework integrating the HBM and the TRA. Using a conceptual framework contributes to shared understanding of factors influencing health behaviour.72, 73 The framework identified key factors of influenza vaccination and presented the inter-relation of behaviour-related variables. However, further well-designed studies are required to explore inter-relationships accurately and comprehensively. Researchers or health providers could also apply the synthesis framework to practice. A good understanding of the influencing variables is needed to inform vaccination campaigns if they are to be effective.
Author statements
Acknowledgements
The authors thank the team at Editage for language polishing.
Ethical approval
None sought.
Funding
None declared.
Competing interests
None declared.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.puhe.2017.12.007.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.World Health Organization. Influenza (seasonal). Geneva: WHO. 2017. Available at: http://www.who.int/mediacentre/factsheets/fs211/en/ [Accessed 9 January 2018].
- 2.Centers for Disease Control and Prevention Estimates of deaths associated with seasonal influenza – United States, 1976–2007. MMWR Morb Mortal Wkly Rep. 2010;59:1057. [PubMed] [Google Scholar]
- 3.Grohskopf L.A., Sokolow L.Z., Olsen S.J., Bresee J.S., Broder K.R., Karron R.A. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices, United States, 2015–16 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64:818–825. doi: 10.15585/mmwr.mm6430a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centers for Disease Control and Prevention. Solna: ECDC. Fact sheet for health professionals. 2016. Available at: http://ecdc.europa.eu/en/healthtopics/seasonal_influenza/basic_facts/Pages/factsheet_professionals_seasonal_influenza.aspx [Accessed 9 January 2018].
- 5.Gefenaite G., Rahamat-Langendoen J., Ambrozaitis A., Mickiene A., Jancoriene L., Kuliese M. Seasonal influenza vaccine effectiveness against influenza in 2012–2013: a hospital-based case–control study in Lithuania. Vaccine. 2014;32:857–863. doi: 10.1016/j.vaccine.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 6.Udell J.A., Zawi R., Bhatt D.L., Keshtkar-Jahromi M., Gaughran F., Phrommintikul A. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA. 2013;310:1711–1720. doi: 10.1001/jama.2013.279206. [DOI] [PubMed] [Google Scholar]
- 7.Jefferson T., Rivetti D., Rivetti A., Rudin M., Pietrantonj C.D., Demicheli V. Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet. 2005;366:1165–1174. doi: 10.1016/S0140-6736(05)67339-4. [DOI] [PubMed] [Google Scholar]
- 8.Nichol K.L., Nordin J.D., Nelson D.B., Mullooly J.P., Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med. 2007;357:1373–1381. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]
- 9.Ridenhour B.J., Campitelli M.A., Kwong J.C., Rosella L.C., Armstrong B.G., Mangtani P. Effectiveness of inactivated influenza vaccines in preventing influenza-associated deaths and hospitalizations among Ontario residents aged ≥65 years: estimates with generalized linear models accounting for healthy vaccine effects. PloS One. 2013;8:e76318. doi: 10.1371/journal.pone.0076318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talbot H.K., Griffin M.R., Chen Q., Zhu Y.W., Williams J.V., Edwards K.M. Effectiveness of seasonal vaccine in preventing confirmed influenza-associated hospitalizations in community dwelling older adults. J Infect Dis. 2011;203:500–508. doi: 10.1093/infdis/jiq076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jefferson T., Di Pietrantonj C., Al-Ansary L.A., Ferroni E., Thorning S., Thomas R.E. Vaccines for preventing influenza in the elderly (Review) Cochrane Database Syst Rev. 2010;2 doi: 10.1002/14651858.CD004876.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Beyer W.E.P., McElhaney J., Smith D.J., Monto A.S., Nguyen-Van-Tam J.S., Osterhaus A.D. Cochrane re-arranged: support for policies to vaccinate elderly people against influenza. Vaccine. 2013;31:6030–6033. doi: 10.1016/j.vaccine.2013.09.063. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . WHO; Geneva: 2003. Prevention and control of influenza pandemics and annual epidemics. WHA 10th Plenary Meeting 2003.apps.who.int/gb/archive/pdf_files/WHA56/ea56r19.pdf Available at: [Google Scholar]
- 14.Thomas R.E., Russell M.L., Lorenzetti D.L. Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine. 2010;28:1684–1701. doi: 10.1016/j.vaccine.2009.11.067. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Flu vaccination coverage, United States, 2014–15 influenza season. Atlanta, GA: CDC. 2015. Available at: http://www.cdc.gov/flu/pdf/fluvaxview/nfid-coverage-2014-15-final.pdf [Accessed 9 January 2018].
- 16.Mereckiene J., Cotter S., Nicoll A., Lopalco P., Noori T., Weber J. Seasonal influenza immunisation in Europe. Overview of recommendations and vaccination coverage for three seasons: pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11) Euro Surveill. 2014;19:20780–20790. doi: 10.2807/1560-7917.es2014.19.16.20780. [DOI] [PubMed] [Google Scholar]
- 17.Zhou L., Su Q., Xu Z., Feng A., Jin H., Wang S. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12) PloS One. 2013;8:e73724. doi: 10.1371/journal.pone.0073724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas R.E., Lorenzetti D.L. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Library. 2014;2014:189–190. doi: 10.1002/14651858.CD005188.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Lataillade C., Auvergne S., Delannoy I. 2005 and 2006 seasonal influenza vaccination coverage rates in 10 countries in Africa, Asia Pacific, Europe, Latin America and the Middle East. J Publ Health Pol. 2009;30:83–101. doi: 10.1057/jphp.2008.40. [DOI] [PubMed] [Google Scholar]
- 20.Kohlhammer Y., Schnoor M., Schwartz M., Raspe H., Schäfer T. Determinants of influenza and pneumococcal vaccination in elderly people: a systematic review. Public Health. 2007;121:742–751. doi: 10.1016/j.puhe.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Nagata J.M., Isabel H.R., Kurup A.S., Albrecht D., Vivas-Torrealba C., Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults ≥65 years: a systematic review of qualitative and quantitative data. BMC Public Health. 2013;13:388–412. doi: 10.1186/1471-2458-13-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ward L., Draper J. A review of the factors involved in older people's decision making with regard to influenza vaccination: a literature review. J Clin Nurs. 2008;17:5–16. doi: 10.1111/j.1365-2702.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosenstock I.M. What research in motivation suggests for public health. Am J Public Health Nations Health. 1960;50:295–302. doi: 10.2105/ajph.50.3_pt_1.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fishbein M. University of Nebraska Press; Lincoln: 1980. A theory of reasoned action: some applications and implications; pp. 65–116. [PubMed] [Google Scholar]
- 25.van Landingham M.J., Suprasert S., Grandjean N., Sittitrai W. Two views of risky sexual practices among Northern Thai males: the health belief model and the theory of reasoned action. J Health Soc Behav. 1995;36:195–212. [PubMed] [Google Scholar]
- 26.Dutta-Bergrnan M.J. Theory and practice in health communication campaigns: a critical interrogation. J Health Commun. 2005;18:103–122. doi: 10.1207/s15327027hc1802_1. [DOI] [PubMed] [Google Scholar]
- 27.Doukas D.J., Localio A.R., Li Y. Attitudes and beliefs concerning prostate cancer genetic screening. Clin Genet. 2004;66:445–451. doi: 10.1111/j.1399-0004.2004.00305.x. [DOI] [PubMed] [Google Scholar]
- 28.Sun X., Guo Y., Wang S., Sun J. Predicting iron-fortified soy sauce consumption intention: application of the theory of planned behavior and health belief model. J Nutr Educ Behav. 2006;38:276–285. doi: 10.1016/j.jneb.2006.04.144. [DOI] [PubMed] [Google Scholar]
- 29.Yang Z.J. Predicting young adults' intentions to get the H1N1 vaccine: an integrated model. J Health Commun. 2015;20:69–79. doi: 10.1080/10810730.2014.904023. [DOI] [PubMed] [Google Scholar]
- 30.Frank J.W., Henderson M., McMurray L. Influenza vaccination in the elderly: 1. Determinants of acceptance. CMAJ. 1985;132:371–375. [PMC free article] [PubMed] [Google Scholar]
- 31.Pearson D.C., Thompson R.S. Evaluation of group health cooperative of Puget Sound's senior influenza immunization program. Public Health Rep. 1994;109:571–578. [PMC free article] [PubMed] [Google Scholar]
- 32.Honkanen P.O., Keistinen T., Kivela S.L. Factors associated with influenza vaccination coverage among the elderly: role of health care personnel. Public Health. 1996;110:163–168. doi: 10.1016/s0033-3506(96)80070-9. [DOI] [PubMed] [Google Scholar]
- 33.van Essen G.A., Kuyvenhoven M.M., de Melker R.A. Why do healthy elderly people fail to comply with influenza vaccination? Age Ageing. 1997;26:275–279. doi: 10.1093/ageing/26.4.275. [DOI] [PubMed] [Google Scholar]
- 34.Nexøe J., Kragstrup J., Søgaard J. Decision on influenza vaccination among the elderly: a questionnaire study based on the health belief model and the multidimensional locus of control theory. Scand J Prim Health Care. 1999;17:105–110. doi: 10.1080/028134399750002737. [DOI] [PubMed] [Google Scholar]
- 35.Pregliasco F., Sodano L., Mensi C., Selvaggi M.T., Adamo B., D'Argenio P. Influenza vaccination among the elderly in Italy. Bull World Health Organ. 1999;77:127–131. [PMC free article] [PubMed] [Google Scholar]
- 36.Abramson Z.H., Cohen-Naor V. Factors associated with performance of influenza immunization among the elderly. IMAJ. 2000;2:902–907. [PubMed] [Google Scholar]
- 37.Armstrong K., Berlin M., Schwartz J.S., Propert K., Ubel P.A. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20:21–25. doi: 10.1016/s0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 38.Santibanez T.A., Nowalk M.P., Zimmerman R.K., Jewell I.K., Bardella I.J., Wilson S.A. Knowledge and beliefs about influenza, pneumococcal disease, and immunizations among older people. J Am Geriatr Soc. 2002;50:1711–1716. doi: 10.1046/j.1532-5415.2002.50466.x. [DOI] [PubMed] [Google Scholar]
- 39.Evans M.R., Watson P.A. Why do older people not get immunised against influenza? A community survey. Vaccine. 2003;21:2421–2427. doi: 10.1016/s0264-410x(03)00059-8. [DOI] [PubMed] [Google Scholar]
- 40.Madhavan S.S., Borker R.D., Fernandes A.W., Amonkar M.M., Rosenbluth S.A. Assessing predictors of influenza and pneumonia vaccination in rural senior adults. J Health Soc Pol. 2004;18:71–93. doi: 10.1300/j045v18n02_05. [DOI] [PubMed] [Google Scholar]
- 41.Chi R.C., Neuzil K.M. The association of sociodemographic factors and patient attitudes on influenza vaccination rates in older persons. Am J Med Sci. 2004;327:113–117. doi: 10.1097/00000441-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Zimmerman R.K., Nowalk M.P., Bardella I.J., Fine M.J., Janosky J.E., Santibanez T.A. Physician and practice factors related to influenza vaccination among the elderly. Am J Prev Med. 2004;26:1–10. doi: 10.1016/j.amepre.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 43.Bardenheier B.H., Wortley P.M., Winston C.A., Lindley M.C., Sapsis K. Do patterns of knowledge and attitudes exist among unvaccinated seniors? Am J Health Behav. 2006;30:675–683. doi: 10.5555/ajhb.2006.30.6.675. [DOI] [PubMed] [Google Scholar]
- 44.Gallagher S., Povey R. Determinants of older adults' intentions to vaccinate against influenza: a theoretical application. J Public Health. 2006;28:139–144. doi: 10.1093/pubmed/fdl008. [DOI] [PubMed] [Google Scholar]
- 45.Mangtani P., Breeze E., Stirling S., Hanciles S., Kovats S., Fletcher A. Cross-sectional survey of older peoples' views related to influenza vaccine uptake. BMC Public Health. 2006;6:249–255. doi: 10.1186/1471-2458-6-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Winston C.A., Wortley P.M., Lees K.A. Factors associated with vaccination of Medicare beneficiaries in five US communities: results from the racial and ethnic adult disparities in immunization initiative survey, 2003. J Am Geriatr Soc. 2006;54:303–310. doi: 10.1111/j.1532-5415.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- 47.Lau J.T.F., Kim J.H., Choi K.C., Tsui H.Y., Yang X. Changes in prevalence of influenza vaccination and strength of association of factors predicting influenza vaccination over time –results of two population-based surveys. Vaccine. 2007;25:8279–8289. doi: 10.1016/j.vaccine.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 48.Kwong E.W., Lam I.O., Chan T.M.F. What factors affect influenza vaccine uptake among community-dwelling older Chinese people in Hong Kong general outpatient clinics? J Clin Nurs. 2009;18:960–971. doi: 10.1111/j.1365-2702.2008.02548.x. [DOI] [PubMed] [Google Scholar]
- 49.Kwong E.W., Lam I.O. Chinese older people in Hong Kong: health beliefs about influenza vaccination. Nurs Older People. 2008;20:29–33. doi: 10.7748/nop2008.09.20.7.29.c6696. [DOI] [PubMed] [Google Scholar]
- 50.Lau J.T.F., Kim J.H., Yang X., Tsui H.Y. Cross-sectional and longitudinal factors predicting influenza vaccination in Hong Kong Chinese elderly aged 65 and above. J Infect. 2008;56:460–468. doi: 10.1016/j.jinf.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 51.Lau L., Lau Y., Lau Y.H. Prevalence and correlates of influenza vaccination among non-institutionalized elderly people: an exploratory cross-sectional survey. Int J Nurs Stud. 2009;46:768–777. doi: 10.1016/j.ijnurstu.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Avelino-Silva V.I., Avelino-Silva T.J., Miraglia J.L., Miyaji K.T., Jacob-Filho W., Lopes M.H. Campaign, counseling and compliance with influenza vaccine among older persons. Clinics. 2011;66:2031–2035. doi: 10.1590/S1807-59322011001200006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Matsui D., Shigeta M., Ozasa K., Kuriyama N., Watanabe I., Watanabe Y. Factors associated with influenza vaccination status of residents of a rural community in Japan. BMC Public Health. 2011;11:149–157. doi: 10.1186/1471-2458-11-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu D.S., Low L.P., Lee I.F., Lee D.T., Ng W.M. Predicting influenza vaccination intent among at-risk Chinese older adults in Hong Kong. Nurs Res. 2014;63:270–277. doi: 10.1097/NNR.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 55.Boggavarapu S., Sullivan K.M., Schamel J.T., Frew P.M. Factors associated with seasonal influenza immunization among church-going older African Americans. Vaccine. 2014;32:7085–7090. doi: 10.1016/j.vaccine.2014.10.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bödeker B., Remschmidt C., Schmich P., Wichmann O. Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu? A population-based study. BMC Public Health. 2015;15:618–627. doi: 10.1186/s12889-015-1970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mo P.K., Lau J.T. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: the application of the Health Belief Model. Health Educ Res. 2015;30:706–718. doi: 10.1093/her/cyv038. [DOI] [PubMed] [Google Scholar]
- 58.Klett-Tammen C.J., Krause G., Seefeld L., Ott J.J. Determinants of tetanus, pneumococcal and influenza vaccination in the elderly: a representative cross-sectional study on knowledge, attitude and practice (KAP) BMC Public Health. 2016;16:121–129. doi: 10.1186/s12889-016-2784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cornford C.S., Morgan M. Elderly people's beliefs about influenza vaccination. Br J Gen Pract. 1999;49:281–284. [PMC free article] [PubMed] [Google Scholar]
- 60.Telford R., Rogers A. What influences elderly peoples' decisions about whether to accept the influenza vaccination? A qualitative study. Health Educ Res. 2003;18:743–753. doi: 10.1093/her/cyf059. [DOI] [PubMed] [Google Scholar]
- 61.Evans M.R., Prout H., Prior L., Tapper-Jones L.M., Butler C.C. A qualitative study of lay beliefs about influenza immunisation in older people. Br J Gen Pract. 2007;57:352–358. [PMC free article] [PubMed] [Google Scholar]
- 62.Cameron K.A., Rintamaki L.S., Kamanda-Kosseh M., Noskin G.A., Baker D.W., Makoul G. Using theoretical constructs to identify key issues for targeted message design: African American seniors' perceptions about influenza and influenza vaccination. J Health Commun. 2009;24:316–326. doi: 10.1080/10410230902889258. [DOI] [PubMed] [Google Scholar]
- 63.Payaprom Y., Bennett P., Burnard P., Alabaster E., Tantipong H. Understandings of influenza and influenza vaccination among high-risk urban dwelling Thai adults: a qualitative study. J Public Health. 2010;32:26–31. doi: 10.1093/pubmed/fdp086. [DOI] [PubMed] [Google Scholar]
- 64.Kwong E.W., Pang S.M., Choi P., Wong T.K. Influenza vaccine preference and uptake among older people in nine countries. J Adv Nurs. 2010;66:2297–2308. doi: 10.1111/j.1365-2648.2010.05397.x. [DOI] [PubMed] [Google Scholar]
- 65.Dixon-Woods M., Brown H., Arthur A., Matthews R., Jagger C. Organising services for influenza vaccination for older people. J Health Serv Res Pol. 2004;9:85–90. doi: 10.1258/135581904322987490. [DOI] [PubMed] [Google Scholar]
- 66.Lau J.T.F., Yang X., Tsui H.Y., Kim J.H. Prevalence of influenza vaccination and associated factors among community-dwelling Hong Kong residents of age 65 or above. Vaccine. 2006;24:5526–5534. doi: 10.1016/j.vaccine.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 67.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 68.Critical Appraisal Skills Programme . 2017. CASP Qualitative Study Checklist.http://www.casp-uk.net/checklists Available at: [Accessed 8 January 2018] [Google Scholar]
- 69.Dixon-Woods M., Sutton A., Shaw R., Miller T., Smith J., Young B. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Pol. 2007;12:42–47. doi: 10.1258/135581907779497486. [DOI] [PubMed] [Google Scholar]
- 70.von Gierke L., Wicker S. Flu vaccination goes mobile. Vaccine. 2014;32:205–206. doi: 10.1016/j.vaccine.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 71.Dapp U., Anders J.A.M., Rentelnkruse W.V., Minder C.E., Meier-Baumgartner H.P., Swift C.G. A randomized trial of effects of health risk appraisal combined with group sessions or home visits on preventive behaviors in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:591–598. doi: 10.1093/gerona/glr021. [DOI] [PubMed] [Google Scholar]
- 72.Bhattacharyya O., Reeves S., Garfinkel S., Zwarenstein M. Designing theoretically-informed implementation interventions: fine in theory, but evidence of effectiveness in practice is needed. Implement Sci. 2006;1:5. doi: 10.1186/1748-5908-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Smiddy M.P., Connell R.O., Creedon S.A. Systematic qualitative literature review of health care workers' compliance with hand hygiene guidelines. Am J Infect Contr. 2015;43:269–274. doi: 10.1016/j.ajic.2014.11.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.