Abstract
The fusogenic potential of Class I viral envelope glycoproteins is activated by proteloytic cleavage of the precursor glycoprotein to generate the mature receptor-binding and transmembrane fusion subunits. Although the coronavirus (CoV) S glycoproteins share membership in this class of envelope glycoproteins, cleavage to generate the respective S1 and S2 subunits appears absent in a subset of CoV species, including that responsible for the severe acute respiratory syndrome (SARS). To determine whether proteolytic cleavage of the S glycoprotein might be important for the newly emerged SARS-CoV, we introduced a furin recognition site at single basic residues within the putative S1–S2 junctional region. We show that furin cleavage at the modified R667 position generates discrete S1 and S2 subunits and potentiates membrane fusion activity. This effect on the cell–cell fusion activity by the S glycoprotein is not, however, reflected in the infectivity of pseudotyped lentiviruses bearing the cleaved glycoprotein. The lack of effect of furin cleavage on virion infectivity mirrors that observed in the normally cleaved S glycoprotein of the murine coronavirus and highlights an additional level of complexity in coronavirus entry.
Keywords: Coronavirus, Envelope (spike) glycoprotein, Membrane fusion, Furin protease, SARS, Pseudotyped virion, Mutagenesis
Introduction
The coronaviruses (CoVs) are a diverse family of enveloped, positive-sense RNA viruses that are distributed widely among animal species. The recent emergence of a novel human CoV responsible for severe acute respiratory syndrome (SARS) (Drosten et al., 2003, Ksiazek et al., 2003, Kuiken et al., 2003, Peiris et al., 2003) highlights the public health risks associated with the continual evolution and zoonotic spread of new CoVs. The human SARS-CoV of 2002–2003 was likely derived from a CoV of the civet cat, an animal common to live-animal food markets in China (Guan et al., 2003). Cross-species transmission events have also been implicated in the emergence and establishment of other novel CoVs, such as the transmissible gastroenteritis virus (TGEV) of pigs (Sanchez et al., 1992) and the human respiratory CoV OC43 (Vijgen et al., 2005).
The spike (S) glycoprotein of the CoV is an important determinant of virus host range and pathogenicity (Lai and Holmes, 2001). This glycoprotein mediates the initial attachment of the virus to host-cell receptors and the subsequent fusion of the viral and cellular membranes to allow entry of the virion core. The S glycoproteins within the CoV family differ among themselves in several features that are reflective of their serologic and phylogenetic groupings (Gonzalez et al., 2003, Lai and Holmes, 2001). Of particular interest is the dimorphism seen with respect to proteolytic maturation of the S glycoprotein precursor. In the group 2 viruses, such as the prototype murine hepatitis virus (MHV), and in the avian group 3 viruses, the S glycoprotein precursor is cleaved, likely by furin-like cellular proteases (de Haan et al., 2004), to yield the canonical receptor-binding (S1) and transmembrane fusion (S2) subunits. By contrast, the S glycoproteins of the group 1 viruses are not subjected to proteolytic cleavage during biogenesis. Interestingly, the newly emerged SARS-CoV displays characteristics of both groups: although the SARS-CoV is phylogenetically related to the group 2 viruses (Gibbs et al., 2004, Snijder et al., 2003), the S glycoprotein does not show evidence of proteolytic maturation (Moore et al., 2004, Simmons et al., 2004, Song et al., 2004, Xiao et al., 2003).
The absence of proteolytic cleavage in certain S glycoproteins stands in contradistinction to the special role for proteolytic maturation in the structure and function of other Class I viral envelope glycoproteins. Cleavage by cellular proteases is universally required to enable the fusion potential of the envelope glycoproteins of retroviruses, orthomyxoviruses, paramyxoviruses, filoviruses and arenaviruses. Upon subsequent activation of the matured Class I envelope glycoprotein, by receptor binding and/or low endosomal pH, these complexes undergo profound structural reorganization to ultimately form highly stable trimer-of-hairpins structures that contribute to fusion of the viral and cellular membranes ((Eckert and Kim, 2001, Hughson, 1997, Skehel and Wiley, 2000, Weissenhorn et al., 1999) and references therein). Although the SARS-CoV S glycoprotein is a bona fide member of the Class I fusion proteins (Bosch et al., 2003, Duquerroy et al., 2005, Follis et al., 2005, Supekar et al., 2004, Xu et al., 2004), it paradoxically appears able to initiate membrane fusion without proteolytic activation and to complete the conformational changes without proteolytic separation of the S1 and S2 subunits.
The requirement for proteolytic maturation among the normally cleaved S glycoproteins of the group 2 CoV species is likewise ambiguous. In the MHV glycoprotein, mutations that alter the furin protease recognition sequence (R-X-R/K-R↓; (Molloy et al., 1999, Rockwell et al., 2002) and references therein) and prevent cleavage generally diminish cell–cell fusion activity (Bos et al., 1995, de Haan et al., 2004, Sturman et al., 1985, Taguchi, 1993, Yamada et al., 1998), yet do not markedly affect viral infectivity or pathogenesis (Bos et al., 1997, de Haan et al., 2004, Hingley et al., 2002). By contrast, MHV infectivity can be enhanced by exogenous treatment with trypsin (Sturman et al., 1985), raising the possibility that proteases that recognize single basic residues may be important. Thus, the role of proteolytic maturation in CoV entry, and the identity of the putative cellular protease, remains unclear.
In this report, we examined the effect of proteolytic cleavage on the ability of the SARS-CoV S glycoprotein to mediate cell–cell fusion and viral infectivity. We show that the introduction of a prototypic furin recognition motif at R667 allows for efficient cleavage of the mutant glycoprotein and increased cell–cell fusion activity. Nonetheless, the cleaved S glycoprotein was not able to enhance the infectivity of pseudotyped virions. These findings reinforce, in the converse, the observations reported in the naturally cleaved group 2 CoVs (Bos et al., 1997, de Haan et al., 2004, Hingley et al., 2002) and call attention to the distinct, albeit unclear, requirements for virion entry in the CoVs.
Results
Sequence analysis of CoV S glycoproteins
The amino acid sequence of the SARS-CoV S glycoprotein was compared with that of representative CoVs of group 1 (HuCoV-229E, HuCoV-NL63, TGEV and FIPV) and group 2 (HuCoV OC43, MHV and BCoV) using the MAXHOM algorithm (Sander and Schneider, 1991). Alignment within the S1 receptor-binding domain was minimal, and meaningful similarity was observed only in the S2 fusion domain. These similarities include the N- and C-terminal heptad-repeat regions that together comprise the α-helical core of the fusion-active trimer-of-hairpins structure and the intervening ‘loop’ region. Extending towards the N-terminus, the alignment could readily be followed through to a well-conserved nonamer (IPTNFSISI) at SARS-CoV positions 696–704 (Fig. 1A). In the group 2 viruses that are proteolytically cleaved (e.g., MHV and BCoV), the furin protease recognition site lies 33 amino acids upstream of this nonamer (RRAHR and RRSRR, respectively). The HuCoV OC43 contains a variant site (RRSRG) at which cleavage may also occur (Kunkel and Herrler, 1996). Further upstream of the furin-like recognition site in the group 2 glycoproteins, we identified a GxCx motif that could also be made to align with the group 1 and SARS-CoV glycoproteins (Fig. 1A). We speculate that the conserved GxCx and nonamer motifs delineate the junction between the S1 and S2 domains in the SARS-CoV S glycoprotein.
Fig. 1.
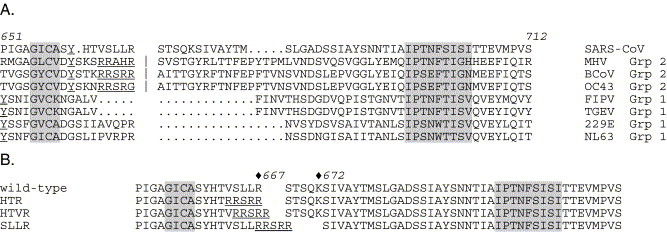
Sequence alignment to define the putative S1–S2 junctional region of SARS-CoV S glycoprotein. (A) The MAXHOM algorithm (Sander and Schneider, 1991) as accessed in the PredictProtein suite (http://cubic.bioc.columbia.edu/predictprotein) was used for the initial alignment of the full-length amino acid sequences of the following CoV S glycoproteins: SARS-CoV (Urbani; AAP1344), murine hepatitis virus (MHV; AAA87062), bovine CoV (BCoV; AAF25499), human respiratory CoV OC43 (AAT84362), feline infectious peritonitis virus (FIPV; VGIH79), porcine transmissible gastroenteritis virus (TGEV; AAT00645) and the human respiratory CoVs 229E (AAK32191) and NL63 (AAS58177). The regions containing the furin cleavage site (in group 2 viruses; underlined) and the S1 GxCx motif and conserved S2 nonamer (gray) were manually adjusted to yield the alignment shown. A tyrosine (Y) present in all S1 domains is also underlined. Deletions in SARS-CoV and the group 1 viruses (.) are arbitrarily displayed. (B) The two basic residues in the junctional region of the wild-type SARS-CoV S glycoprotein (R667 and K672) are indicated by diamonds. The furin protease recognition sites engineered at these sites are underlined in the HTR, HTVR and SLLR mutants.
We find considerable sequence variation and deletion between the GxCx motif and the conserved S2 nonamer in the uncleaved group 1 CoV S glycoproteins. In FIPV and TGEV, the deletions remove all basic amino acids that might be used in furin- or trypsin-mediated cleavage. By contrast, one or more basic residues remain in the glycoproteins of SARS-CoV and the human CoVs 229E and NL63. The alignment for these human viruses in Fig. 1B highlights the single arginine at position 667 of the SARS-CoV S glycoprotein, which may signal a protease-sensitive site. Another basic residue in this region of the SARS-CoV glycoprotein (lysine 672) may likewise be relevant to protease recognition.
Mutation at R667, but not K672, affects S-glycoprotein-mediated cell–cell fusion
Although biochemical evidence for proteolytic cleavage in the wild-type SARS-CoV glycoprotein is largely negative (Moore et al., 2004, Simmons et al., 2004, Song et al., 2004, Xiao et al., 2003), we cannot exclude the possibility that trace levels of cleavage by proteases that recognize single (trypsin-like) or multiple (furin-like) basic residues may in fact be responsible for S-glycoprotein-mediated membrane fusion. To test this hypothesis, we mutated the two basic amino acids in the presumptive S1–S2 junction region to serine. As shown in Fig. 2A (top), the wild-type, R667S and K672S glycoproteins were comparably expressed to yield the intact S glycoprotein, which migrated as two precursor bands: the mature, terminally glycosylated form of 220 kDa molecular weight (S r) and an Endo H-sensitive (S s) form of 200 kDa ((Song et al., 2004) and K.E.F. and J.H.N, unpublished). These collapse upon deglycosylation with PNGase F to yield the 140 kDa S polypeptide (Fig. 2A, bottom). The R667S and K672S mutations did not appear to alter the expression or glycosylation of the glycoproteins, and we too find no evidence of proteolytic cleavage to form S1 and S2 subunits. Interestingly, however, the ability of the R667S mutant to promote cell–cell fusion was consistently reduced to 60% of wild-type levels (Fig. 2B). Fusion by the K672S mutant was largely unaffected. These results point to R667 as an important amino acid in the S glycoprotein and perhaps as a site susceptible to proteolytic cleavage.
Fig. 2.
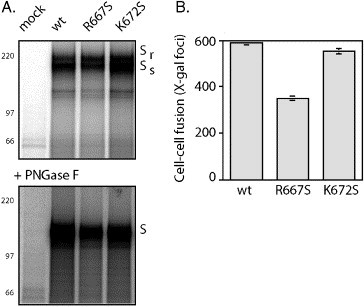
Serine mutation at R667, but not K672, reduces the ability of the S glycoprotein to mediate cell–cell fusion. (A) Wild-type SARS-CoV S glycoprotein and the R667S and K672S mutants were metabolically labeled in COS-7 cells and isolated using the C-terminal S-peptide (Spep) affinity tag (Kim and Raines, 1993). The mock lane represents cells transfected without vTF7-3 infection. Proteins were resolved by SDS polyacrylamide gel electrophoresis in NuPAGE 3–8% Tris–acetate gels (Invitrogen) either as the isolated glycoproteins (above) or following deglycosylation using PNGase F (below). The Endo-H-resistant (Sr) and Endo-H-sensitive (Ss) forms of the S glycoprotein are indicated, as is the fully deglycosylated S polypeptide (S). [14C]-methylated Rainbow molecular weight markers are indicated. The images are printed dark to highlight the absence of proteolytic cleavage. (B) The ability of the S glycoproteins to promote ACE2-dependent cell–cell fusion was detected using the recombinant vaccinia virus-based β-galactosidase reporter assay (Nussbaum et al., 1994, York et al., 2004). COS-7 cells expressing the wild-type and mutant glycoproteins were co-cultured with COS-7 cells transiently expressing the SARS-CoV cellular receptor ACE2 and infected with the fusion reporter recombinant vaccinia virus vCB21R-lacZ (Nussbaum et al., 1994, York et al., 2004). X-gal was used to detect β-galactosidase activity arising from cell–cell fusion. The number of blue syncytia is shown from two experiments, and error bars represent one standard deviation. Transfection efficiencies were comparable in all cases.
Insertion of furin recognition sites in the SARS-CoV S glycoprotein
To investigate whether proteolytic cleavage at the basic amino acid residues, were it to occur, might facilitate cell–cell fusion activity, we mutated the wild-type SARS-CoV glycoprotein to construct a prototypic furin recognition site (RRSRR) at either position. Based on our alignment, we engineered three variants (Fig. 1B): one at position R667 to replace the resident sequence with YHTRRSRR (referred to as HTR) and another at the same position designed to accommodate the deletion indicated in the alignment, YHTVRRSRR (HTVR). The sequence at K672 (RSTSQK) was shortened to RRSRR in order to include the two naturally occurring basic residues (the SLLR variant). These furin-site-containing glycoproteins were expressed in COS-7 cells and isolated using the C-terminal affinity tag (Fig. 3). Proteolytic cleavage to yield novel subunits of 110 kDa and 90 kDa was apparent in the HTVR glycoprotein and less so in HTR (top left). Little cleavage was seen in the SLLR glycoprotein. The proteolytically cleaved products appear to be derived from the mature, terminally glycosylated S r form of the S glycoprotein as the 220 kDa form in HTVR was consistently reduced relative to the S s form. This result is in keeping with the subcellular localization of the furin protease in the trans-Golgi network (Molloy et al., 1999, Rockwell et al., 2002). Upon deglycosylation with PNGase F, the two novel subunits in HTVR and HTR migrated as 72 and 64 kDa peptides (bottom, left), consistent with the anticipated molecular weights of the predicted S1 and S2 polypeptides, respectively. The S2 polypeptide was typically accompanied by lower molecular forms, which suggest additional N-terminal cleavage events. As in the naturally cleaved S glycoprotein of MHV (Krueger et al., 2001), the S1 and S2 subunits derived from the furin-site-containing glycoproteins remain associated upon cell lysis in nonionic detergent.
Fig. 3.
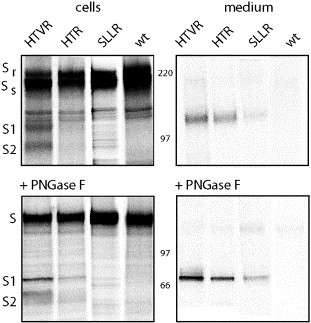
Proteolytic cleavage of the S glycoprotein at introduced furin sites. Wild-type S glycoprotein and the furin-site-containing mutants HTVR, HTR and SSLR were metabolically labeled in COS-7 cells. The S glycoprotein in cell lysates was affinity isolated (cells; left panels), whereas the S1 subunit in the cell culture supernatant (medium; right panels) was immunoprecipitated using MAb F26G18 (Berry et al., 2004). Polypeptides obtained upon deglycosylation with PNGase F are shown in bottom panels. Molecular weight markers and S glycoforms are as described in Fig. 2A. Both S1 and S2 polypeptide molecular weights are consistent with cleavage in the junctional region.
The virus-neutralizing S-glycoprotein-specific monoclonal antibody (MAb) F26G18 (Berry et al., 2004) recognizes a predominantly linear epitope in the S1 subunit of the SARS-CoV S glycoprotein (unpublished). This enabled us to determine whether the S1 subunit was shed from the proteolytically cleaved complex, as has been reported for the naturally cleaved MHV S glycoprotein (Krueger et al., 2001). Upon immunoprecipitation from the medium (Fig. 3 ; right), the S1 subunit was readily isolated in cultures expressing HTVR and HTR. A small amount of S1 was also shed from the SLLR mutant. No S1 subunit was found in the culture medium from cells expressing the wild-type SARS-CoV S glycoprotein, consistent with the lack of proteolytic cleavage. Taken together, these studies indicate that proteolytic cleavage of the SARS-CoV S glycoprotein can be achieved by the introduction of a furin recognition motif, especially at R667. The differences in the degree of cleavage between the two R667 mutants, and in SLLR, suggest specificity in the recognition of the engineered furin sites.
HTVR is transported to the cell surface as the wild-type glycoprotein
Based on our observation that the S1 subunit is shed from cells expressing the furin-site-containing glycoproteins, we investigated the expression and receptor-binding capability of the complex on the cell surface. COS-7 cells transiently expressing the wild-type and HTVR glycoproteins were stained to detect the S1 domain using MAb F26G18 (Berry et al., 2004). Upon flow cytometric analysis (Fig. 4 ), the population of positively staining cells was comparable in number and fluorescence intensity in both the wild-type and HTVR mutant, suggesting comparable transport and cell-surface expression of the two glycoproteins. Studies using recombinant soluble ACE2 (Fig. 4) failed to demonstrate significant differences in the capacity of the cell-surface glycoproteins to bind receptor.
Fig. 4.
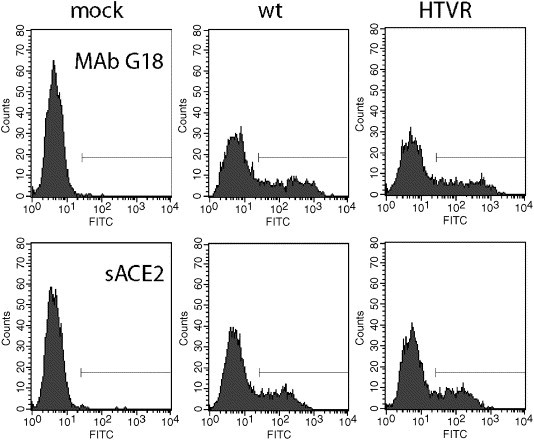
Flow cytometric analysis of cell surface S glycoprotein. COS-7 cells transiently expressing the wild-type and HTVR mutant S glycoproteins were stained using either (top) MAb F26G18 (Berry et al., 2004) and a secondary fluorescein isothiocyanate (FITC)-conjugated anti-mouse antibody or (bottom) a recombinant soluble ACE2 receptor, biotinylated goat anti-ACE2 antibody and FITC-conjugated streptavidin. Cells were analyzed using a FACSCalibur flow cytometer (BD Biosciences), and propidium-iodide-staining (dead) cells were excluded. Background staining of mock-transfected cells is shown in the left panel; non-expressing cells are also evident in the transfected cell populations. Expressing cells were defined using a gate of ≥30 (<0.1% of the mock-transfected population).
Membrane fusion activity of the furin-site-containing mutant glycoproteins
We then investigated the consequences of proteolytic cleavage on the ability of the SARS-CoV S glycoprotein to mediate membrane fusion. As shown in Fig. 5 , COS-7 cells expressing the HTVR glycoprotein were markedly enhanced in their ability to fuse with cells expressing the ACE2 receptor. In multiple experiments, this mutant generated 3- to 8-fold more syncytia than did the wild-type S glycoprotein. The HTR glycoprotein was also more fusogenic than the wild-type (1.8 fold), whereas the insertion in SLLR appeared to inhibit fusion. Discounting potential detrimental effects of the amino acid substitutions per se, the fusogenicity of the mutant glycoproteins generally correlated with the extent of proteolytic cleavage (Fig. 3). Recombinant expression of ACE2 receptor was required in all cases for fusion. The marked increase in fusogenicity in concert with proteolytic cleavage suggests strongly that proteolytic maturation of the CoV S glycoprotein impacts the ability of the glycoprotein to mediate membrane fusion.
Fig. 5.
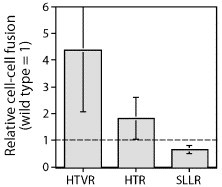
Cell–cell fusion is enhanced by proteolytic cleavage. Wild-type S glycoprotein and the furin-site-containing mutants HTVR, HTR and SSLR were expressed in COS-7 cells, and fusogenicity was determined as described in Fig. 2B (Nussbaum et al., 1994, York et al., 2004). The number of blue syncytia relative to that in the wild-type S glycoprotein control is shown from four independent experiments, and error bars represent one standard deviation. Transfection efficiencies within each experiment were comparable.
Proteolytic cleavage of the mutant glycoproteins is mediated by furin protease
We further investigated our assumption that proteolytic cleavage in the furin-site-containing mutants is mediated by the furin protease, and not by adventitious cellular enzymes that may also cleave at the highly hydrophilic furin recognition site. A Chinese hamster ovary (CHO) cell line deficient in furin protease (FD11; (Gordon et al., 1995)) was obtained from S. Leppla (NIH) and used to express the S glycoproteins. The FD11 cell line was derived following chemical mutagenesis and selection for resistance to anthrax toxin protective antigen (PA), which is activated intracellularly by furin cleavage (Gordon et al., 1995). As shown in Fig. 6 , proteolytic processing of the HTVR, HTR and SLLR glycoproteins was abrogated in the furin-deficient FD11 cell line. The S1 and S2 subunits were absent in FD11 cells, and S1 was not detected in the cell culture medium. These findings provide evidence that proteolytic cleavage in the furin-site-containing mutants is indeed mediated by the furin protease.
Fig. 6.
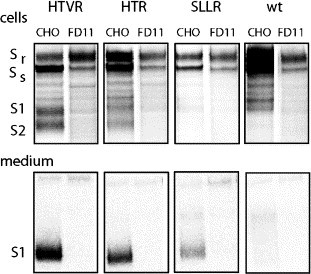
Proteolytic processing in furin-deficient FD11 and wild-type CHO cells. Wild-type S glycoprotein and the furin-site-containing mutants HTVR, HTR and SSLR were metabolically labeled in furin-deficient cells and parental CHO cells (Gordon et al., 1995). The S glycoprotein in cell lysates was affinity isolated (top panels), and the S1 subunit in the cell culture medium (bottom panels) was immunoprecipitated using MAb F26G18 (Berry et al., 2004).
Efforts to determine the relative fusogenicity of the cleaved and uncleaved glycoproteins in the CHO and FD11 cells were confounded, however, by differences in the levels of S glycoprotein expression. Although cell–cell fusion by both the wild-type and HTVR glycoproteins was dramatically reduced in furin-deficient FD11 cells (Fig. 7B), the relative transfection efficiencies in the two cell lines also differed markedly (4% vs. 20% in the parental CHO cells). The basis for this difference is unclear and was not mitigated in a furin-expressing cell line derived from FD11 (Gordon et al., 1995). Direct comparison of fusion activity in the two cell lines was therefore difficult.
Fig. 7.
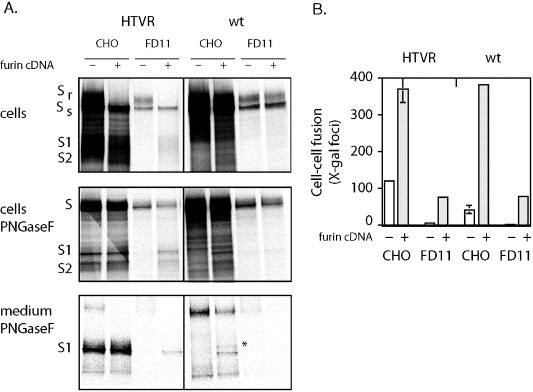
Co-expression of furin cDNA enhances proteolytic cleavage and cell–cell fusion. (A) Wild-type or HTVR S glycoprotein plasmid was co-transfected with a furin-expressing plasmid (+furin cDNA), or a pcDNA3.1− control (−furin cDNA), into furin-deficient FD11 or wild-type CHO cells (Gordon et al., 1995). The S glycoproteins were expressed and metabolically labeled as described in Fig. 3. Isolated glycoproteins from cell lysates (top panel) were also examined following deglycosylation with PNGase F (middle panel); shed S1 subunit was immunoprecipitated from the cell culture medium and examined following deglycosylation (bottom panel). Molecular weight markers and forms of the S glycoprotein are as described in Fig. 3. A 69 kDa molecular weight form of S1 was also detected in the culture medium upon PNGase F-treatment (indicated by *), as was a 140 kDa polypeptide which is consistent with blebbing of the intact S glycoprotein. (B) Cell–cell fusion was assessed using the indicated S-glycoprotein-expressing cells and COS-7 target cells expressing exogenous ACE2 receptor. The number of blue syncytia is shown from two experiments, and error bars represent one standard deviation. Small error bars are not shown.
To circumvent this problem, we co-expressed the S glycoprotein with furin cDNA in FD11 cells. As anticipated, recombinant furin expression was required for proteolytic cleavage of the HTVR glycoprotein in FD11 cells (Fig. 7A). Despite the reduced levels of S glycoprotein expression in the FD11 cells, S1 and S2 subunits were generated and S1 glycoprotein was shed into the culture medium with good efficiency. Cell–cell fusion by the HTVR glycoprotein was also enhanced by co-expression of furin in FD11 cells (Fig. 7B). Interestingly, the wild-type S glycoprotein was also cleaved in CHO cells co-expressing the furin cDNA to yield S1 and S2 subunits that co-migrated with those in the HTVR glycoprotein (Fig. 7A). This may represent exuberant cleavage at the suboptimal SLLR667 site in the wild-type glycoprotein. Concomitant with this cleavage event, cell–cell fusion by the wild-type S glycoprotein was enhanced by co-expression of furin (Fig. 7B). In addition to the nominal S1 subunit, these cells also shed a larger glycoprotein (indicated by the asterisk in Fig. 7A) whose molecular weight is consistent with cleavage at a previously suggested furin recognition motif at position 758–761 (RNTR (Xiao et al., 2003)), a site we place by sequence alignment in the S2 subunit (Fig. 1A).
The dramatic effects observed upon co-expression of furin in an experimental setting raise the possibility of cryptic cleavage events in the wild-type S glycoprotein under natural conditions. The ability of the co-expressed furin to cleave the wild-type glycoprotein to produce S1 and S2 subunits that co-migrate with those generated in the HTVR mutant lends credence to the suggestion that the S1–S2 junctional region defined by sequence alignment (Fig. 1) may contain vestigial or inefficiently utilized furin recognition sites.
R667 is important for furin-mediated cleavage in the wild-type S glycoprotein
To specifically determine which of the basic residues within the junctional region is utilized for cleavage of the wild-type S glycoprotein, we re-examined the expression of the R667S and K672S mutant glycoproteins in CHO cells co-transfected to over-express the furin cDNA. S1 and S2 subunits were generated in cell lysates of both the wild-type and K672S glycoproteins, but not in the R667S mutant. Consistent with this finding, only cells expressing the wild-type and K672S glycoproteins were able to shed S1 glycoprotein to the cell culture medium (Fig. 8A). These findings suggest that the furin-mediated cleavage event at R667 is disrupted by the substitution of serine and, importantly, is responsible for the generation of the S1 subunit in the wild-type and HTVR glycoproteins. By contrast, the larger S1-like fragment thought to represent cleavage at the RNTR site at position 758–761 (indicated by the asterisk in Fig. 8A) was produced and shed by both the R667S and K672S mutants and by the wild-type glycoprotein.
Fig. 8.
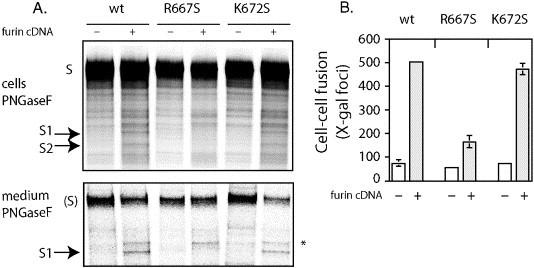
Co-expression of furin cDNA results in cleavage and enhanced fusogenicity of the wild-type and K672S glycoproteins. (A) Wild-type or mutant S glycoprotein plasmid (R667S or K672S) was co-transfected into wild-type CHO cells with a furin-expressing plasmid (+furin cDNA) or a pcDNA3.1− control (−furin cDNA). Isolated glycoproteins from cell lysates (cells; top panel) and immunoprecipitated S1 subunit from culture medium (bottom panel) were deglycosylation with PNGase F. Molecular weight markers and forms of the S polypeptide, including the larger S1 fragment (*), are as described in Fig. 7. The intact S polypeptide present in the medium (bottom panel) is shown for internal size reference. (B) Cell–cell fusion was assessed using the S-glycoprotein-expressing CHO cells and COS-7 target cells expressing exogenous ACE2 receptor. The number of blue syncytia is shown from two experiments, and error bars represent one standard deviation. Smaller error bars are not shown.
We had shown that the membrane fusion activity of the R667S glycoprotein was reduced in COS-7 cells relative to the wild-type glycoprotein (Fig. 2B), and a similar result was obtained in CHO cells (Fig. 8B). Co-expression of furin cDNA in the CHO cells resulted in a 5-fold increase in fusion activity by the wild-type and the K672S glycoproteins (Fig. 8B). The increase was considerably blunted in the R667S mutant, consistent with the reduction in furin-mediated cleavage at the mutated SLLS667 site. Thus, maximal cell–cell fusion activity correlates with the presence of the S1 subunit generated by cleavage at R667. The larger S1-like product, generated in all the glycoproteins and thought to reflect cleavage at position 761, is likely not a key contributor to fusion competence.
Enhanced cell–cell fusion activity does not translate to increased virion infectivity
Studies of the normally cleaved S glycoprotein of group 2 MHVs have highlighted a clear and puzzling distinction between the roles of proteolytic cleavage in cell–cell fusion and in virion infectivity and pathogenicity (Bos et al., 1997, de Haan et al., 2004, Hingley et al., 2002). To determine whether proteolytic cleavage of the normally uncleaved SARS-CoV S glycoprotein affects virion infectivity, we generated pseudotyped retroviral virions bearing the wild-type and HTVR SARS-CoV glycoproteins (Moore et al., 2004, Simmons et al., 2004, Yang et al., 2004, Yuan et al., 2004). For these studies, we utilized the HIV-1 provirus-based vector pNL4-3.Luc.R−E−, which has been engineered to disrupt HIV envelope glycoprotein expression and to encode a luciferase reporter protein (Connor et al., 1995). A codon-optimized S glycoprotein gene (Moore et al., 2004) was provided by M. Farzan (Harvard Medical School, Boston) to obviate the need for vTF7-3 in these studies. The codon-optimized gene was further modified to delete the C-terminal 19 amino acids (co-S Δ19) that interfere with pseudotyping efficiency (Fukushi et al., 2005, Giroglou et al., 2004, Moore et al., 2004). Purified pseudotyped virions bearing the wild-type co-S Δ19 glycoprotein or the HTVR-derivative were initially examined by immunoprecipitation to characterize pseudotype formation (Fig. 9A). Comparable levels of HIV Gag proteins p24 and p17 were found in pseudotyped particles bearing either co-S Δ19 or co-HTVR Δ19 glycoproteins. Importantly, comparable amounts of the two S glycoproteins were incorporated into the retroviral particles. Pseudotyped virions containing the HTVR glycoprotein were highly enriched in the cleaved subunits (S1 and S2) relative to the expressing cells (e.g., Fig. 3), although the uncleaved form was also present. This enrichment is likely due to the exclusion of immature intracellular forms of the glycoprotein from the pseudotyped virion sample. As anticipated, no cleaved S glycoprotein products were observed in virions bearing the wild-type co-S Δ19 glycoprotein. Thus, the respective S glycoproteins are comparably and faithfully incorporated into pseudotyped virions.
Fig. 9.
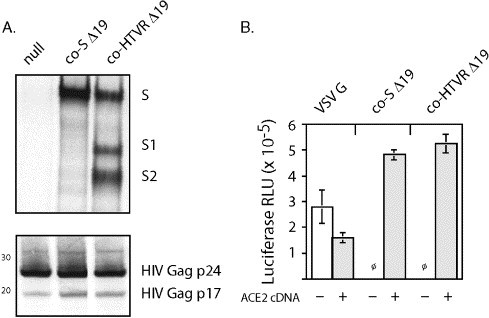
Pseudotyped virions bearing HTVR S glycoprotein are not enhanced in their infectivity. (A) Metabolically labeled pseudotyped virions bearing the co-S Δ19 or co-HTVR Δ19 glycoprotein were pelleted through 20% sucrose and solubilized in 1% Triton X-100 lysis buffer prior to immunoprecipitation. HIV proteins were isolated using anti-HIV immunoglobulin from infected individuals (HIVIG; Prince et al., 1991), and SARS-CoV S glycoproteins were immunoprecipitated using MAb F26G18 (Berry et al., 2004). Particles lacking any envelope glycoprotein (null) served as controls. S-glycoprotein-containing samples were heated to 100 °C prior to SDS-PAGE electrophoresis to disrupt S2 oligomers. Molecular weight markers, HIV proteins (Gag p24 and p17) and forms of the S glycoprotein are indicated. (B) Pseudotyped virions bearing the co-S Δ19 or co-HTVR Δ19 glycoprotein, or the VSV G glycoprotein control, were used to infect 293T cells transiently expressing ACE2 (+) or native 293T cells (−). Fresh pseudotyped virion stocks were applied neat to 293T cell microcultures, and infection was determined 2 days later by chemiluminescence of the luciferase reporter (reported in relative light units (RLUs)). No infection by S-glycoprotein-containing virions was detected (ϕ) in the absence of ACE2 expression. Error bars represent one standard deviation.
To determine the infectivity of the respective pseudotyped virions, cell culture supernatants were incubated with human 293T cells expressing the ACE2 receptor, and viral entry was assessed 2 days later by expression of the luciferase gene reporter. Despite the dramatic differences observed in assays of cell–cell fusion, pseudotyped virions bearing the co-S Δ19 or co-HTVR Δ19 glycoprotein were equally infectious (Fig. 9B). Expression of the ACE2 receptor remained essential for entry. Thus, the enhanced facility of the furin-cleaved HTVR glycoprotein to mediate membrane fusion is apparently not reflected in the overall process of virion entry. The disconnect between the membrane fusion activity of the S glycoprotein and its ability to mediate viral entry, demonstrated here in the normally uncleaved SARS-CoV S glycoprotein and previously in the normally cleaved glycoprotein of MHV (Bos et al., 1997, de Haan et al., 2004, Hingley et al., 2002), highlights unresolved complexities in the pathway used by CoVs to infect target cells.
Discussion
The paradigm developed from the study of other Class I viral fusion proteins – that proteolytic maturation of a precursor glycoprotein is absolutely required to activate the fusogenic potential of the envelope glycoprotein complex – is not neatly applied to the CoV S glycoprotein. Some naturally occurring CoV S glycoproteins undergo proteolytic cleavage (those of the group 2 and 3 CoVs) and others do not (those of the group 1 viruses). Judging that it is unlikely that a proteolytically intact S glycoprotein is capable of mediating membrane fusion, one is left to consider the alternative that the fusion activity of the group 1 viruses, and the newly emerged SARS-CoV, may derive from proteolytic cleavage that has heretofore gone undetected. In this report, we have examined the role of furin cleavage on the fusogenicity of the normally uncleaved SARS-CoV S glycoprotein. We found that introduction of a synthetic furin recognition sequence at R667 in the putative S1–S2 junctional region enabled efficient cleavage of the S glycoprotein to generate discrete S1 and S2 subunits and markedly increased the ability of the spike complex to mediate cell–cell fusion. In the wild-type S glycoprotein, over-expression of furin cDNA made manifest a cleavage event that has not been otherwise observed (see also Bergeron et al., 2005), most likely at the naturally occurring sequence SLLR667. This exuberant cleavage likewise resulted in an increase in fusogenicity. Direct physical confirmation of cleavage at R667 is however lacking. Although a synthetic peptide bearing the SLLR site was insensitive to furin cleavage in vitro (Bergeron et al., 2005), it is possible that this sequence may be recognized under some natural conditions. For instance, cleavage might take place on the extracellular virion, perhaps in specialized tissue environments (Klenk and Garten, 1994) or upon endocytosis (Nash and Buchmeier, 1997, Simmons et al., 2004, Yang et al., 2004).
In our studies, we show a consistent correlation between furin cleavage at SLLR667 and an increased ability of the glycoprotein to mediate cell–cell fusion. By contrast, furin-mediated cleavage of the S glycoprotein at a more C-terminal recognition motif, RNTR761, does not appear to affect fusogenicity. Although cleavage at these sites has previously been reported (Bergeron et al., 2005), our studies demonstrate the importance of the SLLR667 cleavage in fusion competence of the S glycoprotein. This finding is in agreement with the evolutionary homology in this S1–S2 junctional region among CoV species (Fig. 1).
Based on the widespread conservation of furin recognition sites in the group 2 and 3 CoVs, we have focused on this protease. Interestingly, inhibition of furin activity by a peptidic furin inhibitor has recently been reported to prevent the cytopathic effect of SARS-CoV infection in cell culture (Bergeron et al., 2005). Nonetheless, other proteolytic enzymes have also been implicated in CoV entry (Matsuyama et al., 2005, Simmons et al., 2004, Storz et al., 1981, Sturman et al., 1985). The recent finding that SARS-CoV entry can be blocked by a specific inhibitor of cathepsin L (Huang et al., 2006, Simmons et al., 2005) highlights the possible role of endosomal proteases. The multiple opportunities for proteolytic activation of the S glycoprotein in natural infection remain to be examined.
The specific facilitation of cell–cell fusion activity by furin cleavage of the SARS-CoV S glycoprotein reported here extends previous findings from studies of the naturally cleaved group 2 CoVs, in which reductions in S glycoprotein cleavage have been associated with deficiencies in cell–cell fusion activity (Bos et al., 1995, de Haan et al., 2004, Sturman et al., 1985, Taguchi, 1993, Yamada et al., 1998). Despite a reasonable correlation between proteolytic cleavage and membrane fusion activity in both the naturally cleaved and uncleaved S glycoproteins, the presence or absence of furin cleavage appears to have surprisingly little impact on the infectivity of the virion particle. MHV virions that contain significant mutations in the furin-recognition site are not proteolytically cleaved yet remain infectious and pathogenic (Bos et al., 1997, de Haan et al., 2004, Hingley et al., 2002). Here, we demonstrate the converse—that pseudotyped virions bearing the cleaved HTVR glycoprotein are no more capable of mediating virion entry than those bearing the uncleaved wild-type S glycoprotein.
The discordant effects of proteolytic cleavage highlight the potential for differences in the requirements and pathways for S-glycoprotein-mediated cell–cell fusion and viral entry. This dichotomy is further reflected in the ability of exogenous trypsin to enhance SARS-CoV S-glycoprotein-mediated cell–cell fusion, but not infectivity by pseudotyped virion (Simmons et al., 2004). Reciprocally, cell–cell fusion by the MHV S glycoprotein is prevented by a peptidic furin inhibitor, whereas MHV infection is not (de Haan et al., 2004).
The recent finding that SARS-CoV entry is blocked by a specific inhibitor of the endosomal protease cathepsin L provides one plausible resolution to this conundrum (Huang et al., 2006, Simmons et al., 2005): the cleavage critical for viral entry may take place unobserved upon endocytosis or during vesicular trafficking. Other cleavage events mediated by furin, while evolutionarily conserved and no doubt important, may serve supportive or even distinct functions. A similar paradigm has been proposed for entry by the Ebola filovirus (Chandran et al., 2005). As in MHV, furin cleavage of the Ebola virus envelope glycoprotein precursor occurs in nature yet appears unnecessary for viral entry (Neumann et al., 2002, Wool-Lewis and Bates, 1999).
Although further investigation of the role of endosomal proteases in viral entry will no doubt reveal additional detail to this novel mechanism for envelope glycoprotein activation, the function of the highly conserved furin cleavage site in the CoV life cycle remains unclear. In this regard, it is worthwhile to note another trait of the CoV S glycoproteins that is phylogenetically linked to the presence or absence of the furin cleavage site. In the ectodomain of S glycoproteins that remain uncleaved (group 1 CoVs), the N- and C-terminal heptad-repeat regions are extended by two additional in-register units (14 amino acids) relative to those of S glycoproteins that normally undergo furin cleavage (groups 2 and 3 CoVs). These heptad-repeat regions in Class I viral fusion proteins form the six α-helical core of the trimer-of-hairpins structure upon envelope glycoprotein activation and, in doing so, contribute energetically toward the initiation of membrane fusion ((Eckert and Kim, 2001, Hughson, 1997, Skehel and Wiley, 2000, Weissenhorn et al., 1999) and references therein). By this model, the extended heptad repeats in the group 1 viruses may facilitate formation of the six-helix bundle and membrane fusion, perhaps in compensation for the lack of furin cleavage. Biophysical and structural evidence for this suggestion is however lacking.
It is of interest, then, that the S glycoproteins of the SARS-CoV and its related CoVs (Guan et al., 2003, Lau et al., 2005, Li et al., 2005) represent an exception to this rule in the other CoVs. Despite the lack of furin cleavage, these glycoproteins contain only the shorter heptad-repeat regions. The consequences of this exception for viral replication, pathogenesis and CoV ecology are unknown. Further studies of CoV entry and the role of proteolytic cleavage events in this process are likely to impact our understanding of CoV pathogenesis and our ability to respond to newly emerging CoVs.
Materials and methods
Molecular reagents and monoclonal antibodies
The S glycoprotein gene of the Urbani isolate of SARS-CoV (Ksiazek et al., 2003) was obtained from P. Rota (Centers for Disease Control and Prevention, Atlanta) and adapted for expression in pcDNA3.1− (Invitrogen). We further modified this plasmid to introduce an S-peptide (Spep) affinity tag (Kim and Raines, 1993) at the cytoplasmic C-terminus of the S glycoprotein to facilitate manipulations. The Spep addition is innocuous with regard to S-glycoprotein-mediated membrane fusion (Follis et al., 2005), in keeping with reports of other C-terminal tags (Bisht et al., 2004, Bosch et al., 2004, Moore et al., 2004). Mutations were introduced by using QuikChange mutagenesis (Stratagene) and confirmed by DNA sequencing. A plasmid encoding the cell surface receptor of the SARS-CoV, angiotensin-converting enzyme 2 (ACE2) was provided by M. Farzan (Harvard Medical School, Boston) (Li et al., 2003). Mouse monoclonal antibodies (MAbs) directed to the S glycoprotein were provided by J. Berry (National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg) (Berry et al., 2004, Gubbins et al., 2005). The human furin precursor cDNA (Bresnahan et al., 1990) was from G. Thomas (Oregon Health Sciences University, Portland) and was transferred to pcDNA3.1− for expression. Wild-type Chinese hamster ovary (CHO) cells and the furin-deficient derivative FD11 (Gordon et al., 1995) were provided by S. Leppla (National Institutes of Health, Bethesda).
Expression of the S glycoprotein
The full-length S glycoprotein was transiently expressed using the pcDNA3.1− T7 promoter and the recombinant vaccinia virus vTF7-3 encoding T7 polymerase (Follis et al., 2005, Fuerst et al., 1986). vTF7-3 was obtained from T. Fuerst and B. Moss (National Institutes of Health) through the NIH AIDS Research and Reference Reagent Program. COS-7 cells were infected with the recombinant vaccinia virus at a multiplicity of eight in Dulbecco's Minimal Essential Medium (DMEM) containing 2% fetal bovine serum (FBS). Cytosine arabinoside (araC) was added to the medium at 10 μM to limit vaccinia virus expression (Hruby et al., 1980). CHO cells were infected at a multiplicity of eight in F12 medium containing 2% FBS. After 30 min, infected cells were washed and transfected with the S glycoprotein expression plasmid using FuGene-6 reagent (Roche Biochemicals). Metabolic labeling using 80 μCi/ml of [35S]-ProMix (Amersham Pharmacia Biotech) was initiated 6 h post-transfection in methionine- and cysteine-free DMEM containing 10% dialyzed FBS and 10 μM araC and was continued for 12–16 h. Cell culture supernatants were collected, cleared and filtered (0.2 μm) and were made to 1% Triton X-100 and 1 μg/ml each of protease inhibitors (aprotinin, leupeptin and pepstatin) prior to immunoprecipitation using the S1 domain-directed MAb F26G18 (Berry et al., 2004) and Protein A–Sepharose (Sigma). Cells were washed in physiological buffered saline (PBS) and lysed using cold Tris–saline buffer (50 mM Tris–HCl and 150 mM NaCl at pH 7.5) containing 1% Triton X-100 nonionic detergent and protease inhibitors. A soluble fraction was prepared by centrifugation at 15,000 × g for 15 min at 4 °C. The S glycoproteins in cell lysates were isolated using the Spep affinity tag and S-protein agarose (Novagen). Comparable results were obtained by immunoprecipitation from cell lysates (not shown). In some studies, the glycoproteins were deglycosylated using peptide N-glycosidase (PNGase F; New England Biolabs). The isolated glycoproteins and deglycosylated polypeptides were resolved using NuPAGE 3–8% Tris–acetate gels (Invitrogen) and the recommended sample buffer containing lithium dodecyl sulfate and reducing agent. Molecular size markers are [14C]-methylated Rainbow proteins (Amersham Pharmacia Biotech). Radiolabeled proteins were imaged using a Fuji FLA-3000G imager and analyzed using ImageGauge software (Fuji).
Flow cytometry
COS-7 cells transiently expressing the SARS-CoV S glycoprotein were labeled using either the S1-directed MAb F26G18 (Berry et al., 2004) and a secondary fluorescein-isothiocyanate (FITC)-conjugated goat anti-mouse antibody (Jackson ImmunoResearch) or with recombinant soluble ACE2 receptor (R&D Systems; 0.5 μg in 100 μl), biotinylated goat anti-ACE2 antibody (R&D Systems) and FITC-conjugated streptavidin (BD Biosciences). Cells were subsequently stained using propidium iodide (1 μg/ml) and then fixed in 2% formaldehyde. Populations were analyzed using a FACSCalibur flow cytometer and CellQuest software (BD Biosciences).
S-glycoprotein-mediated cell–cell fusion
The β-galactosidase fusion reporter assay (Nussbaum et al., 1994) was used to assess the ability of the S glycoproteins to mediate receptor-dependent cell–cell fusion (Follis et al., 2005). The recombinant vaccinia virus vCB21R-lacZ expressing β-galactosidase under the control of the T7 promoter (Alkhatib et al., 1996) was obtained from C. Broder, P. Kennedy and E. Berger (NIH) through the NIH AIDS Research and Reference Reagent Program. In these studies, cells infected with vTF7-3 and expressing the S glycoprotein were co-cultured with target COS-7 cells transfected to express the SARS-CoV cellular receptor ACE2 (Li et al., 2003) and infected with vCB21R-lacZ. Upon fusion of the effector and target cells, β-galactosidase expression was induced. To generate the target cell population, COS-7 cells that had been transfected 1 day previously with the ACE2 expression plasmid (Li et al., 2003) were incubated with vCB21R-lacZ at a multiplicity of 10 and the infection was allowed to proceed overnight in the presence of 100 μg/ml of the vaccinia virus assembly inhibitor rifampicin. The following day, S-glycoprotein-expressing cells and ACE2-expressing target cells were co-cultured for 10 h in medium containing both araC and rifampicin (Hruby et al., 1980, York et al., 2004). Cultures were then fixed for 5 min at 4 °C in cold PBS containing 2% formaldehyde and 0.2% glutaraldehyde, and β-galactosidase activity was detected using the chromogenic X-gal substrate (Nussbaum et al., 1994). The numbers of blue syncytia per 24-well microculture dish were determined microscopically.
Pseudotyped virions
Lentiviral virions bearing the SARS-CoV S glycoprotein were generated using the HIV-1 proviral vector pNL4-3.Luc.R−E− (Connor et al., 1995) obtained through the NIH AIDS Research and Reference Reagent program from N. Landau (Salk Institute, La Jolla, CA). To eliminate the requirement for recombinant vaccinia virus vTF7-3 in these studies, a codon-optimized S glycoprotein gene (Urbani strain; co-S-C9; Moore et al., 2004) was obtained from M. Farzan (Harvard Medical School, Boston). The S glycoprotein reading frame was subsequently modified to remove the C-terminal tag, to generate the HTVR mutation and to delete the C-terminal 19 amino acids. This latter Δ19 truncation increased the efficiency of pseudotyping (Fukushi et al., 2005, Giroglou et al., 2004, Moore et al., 2004). A plasmid expressing the vesicular stomatitis virus (VSV) G glycoprotein was provided by J. Rose (Yale University) and served as a control in our studies.
Pseudotyped virions were generated by co-transfection of the pNL4-3.Luc.R−E− and pcDNA3.1-based envelope glycoprotein-expressing plasmids at a 4:1 ratio in COS-7 cells. Supernatants were harvested after 2 days and filtered (0.45 μm produce pseudotyped virion stocks. In these experiments, transfection efficiencies in the cultures were gauged by expression of the pNL4-3.Luc.R−E−-encoded luciferase gene. Chemiluminescence was assayed using Luc-Screen System reagents (Applied Biosystems) and a Tropix TR717 microplate luminometer. Luciferase expression was comparable in transfected cultures expressing either the wild-type or HTVR co-S glycoprotein. Pseudotyped virion stocks were used fresh to infect human 293T cells that had previously been transfected to transiently express human ACE2. Infection was determined 2 days later by expression of the luciferase reporter.
Metabolically labeled pseudotyped virions were examined to characterize the relative efficiency of S glycoprotein incorporation. Transfected cultures were labeled for 24 h prior to harvest using 80 μCi/ml of [35S]-ProMix (Amersham Pharmacia Biotech), and supernatant virions were purified by ultracentrifugation through 20% sucrose. Pelleted particles were lysed and immunoprecipitated using MAb F26G18 as described above. HIV proteins were separately precipitated using anti-HIV immunoglobulin from infected individuals (HIVIG; Prince et al., 1991).
Acknowledgments
We are most grateful to Drs. Paul Rota (Centers for Disease Control and Prevention, Atlanta), Jody Berry (National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg), Michael Farzan (Harvard Medical School, Boston), Stephen Leppla (National Institutes of Health, Bethesda), Gary Thomas (Oregon Health Sciences University), Jack Rose (Yale University, New Haven) and the NIH AIDS Research and Reference Reagent program for providing important reagents for this work. We thank Drs. Min Lu (Weill Medical College of Cornell University, New York) and Meg Trahey (The University of Montana) for helpful discussions in preparation of the manuscript.
References
- Alkhatib G., Broder C.C., Berger E.A. Cell type-specific fusion accessory factors determine human immunodeficiency type-1 tropism for T-cell lines vs primary macrophages. J. Virol. 1996;70:6487–6494. doi: 10.1128/jvi.70.8.5487-5494.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron E., Vincent M.J., Wickham L., Hamelin J., Basak A., Nichol S.T., Chretien M., Seidah N.G. Implication of proprotein convertases in the processing and spread of severe acute respiratory syndrome coronavirus. Biochem. Biophys. Res. Commun. 2005;326:554–563. doi: 10.1016/j.bbrc.2004.11.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry J.D., Jones S., Drebot M.A., Andonov A., Sabara M., Yuan X.Y., Weingartl H., Fernando L., Marszal P., Gren J., Nicolas B., Andonova M., Ranada F., Gubbins M.J., Ball T.B., Kitching P., Li Y., Kabani A., Plummer F. Development and characterisation of neutralising monoclonal antibody to the SARS-coronavirus. J. Virol. Methods. 2004;120:87–96. doi: 10.1016/j.jviromet.2004.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisht H., Roberts A., Vogel L., Bukreyev A., Collins P.L., Murphy B.R., Subbarao K., Moss B. Severe acute respiratory syndrome coronavirus spike protein expressed by attenuated vaccinia virus protectively immunizes mice. Proc. Natl. Acad. Sci. U.S.A. 2004;101:6641–6646. doi: 10.1073/pnas.0401939101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos E.C., Heijnen L., Luytjes W., Spaan W.J. Mutational analysis of the murine coronavirus spike protein: effect on cell-to-cell fusion. Virology. 1995;214:453–463. doi: 10.1006/viro.1995.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos E.C., Luytjes W., Spaan W.J. The function of the spike protein of mouse hepatitis virus strain A59 can be studied on virus-like particles: cleavage is not required for infectivity. J. Virol. 1997;71:9427–9433. doi: 10.1128/jvi.71.12.9427-9433.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch B.J., van der Zee R., de Haan C.A., Rottier P.J. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J. Virol. 2003;77:8801–8811. doi: 10.1128/JVI.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch B.J., de Haan C.A., Rottier P.J. Coronavirus spike glycoprotein, extended at the carboxy terminus with green fluorescent protein, is assembly competent. J. Virol. 2004;78:7369–7378. doi: 10.1128/JVI.78.14.7369-7378.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresnahan P.A., Leduc R., Thomas L., Thorner J., Gibson H.L., Brake A.J., Barr P.J., Thomas G. Human fur gene encodes a yeast KEX2-like endoprotease that cleaves pro-beta-NGF in vivo. J. Cell Biol. 1990;111:2851–2859. doi: 10.1083/jcb.111.6.2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandran K., Sullivan N.J., Felbor U., Whelan S.P., Cunningham J.M. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor R.I., Chen B.K., Choe S., Landau N.R. Vpr is required for efficient replication of human immunodeficiency virus type-1 in mononuclear phagocytes. Virology. 1995;206:935–944. doi: 10.1006/viro.1995.1016. [DOI] [PubMed] [Google Scholar]
- de Haan C.A., Stadler K., Godeke G.J., Bosch B.J., Rottier P.J. Cleavage inhibition of the murine coronavirus spike protein by a furin-like enzyme affects cell–cell but not virus–cell fusion. J. Virol. 2004;78:6048–6054. doi: 10.1128/JVI.78.11.6048-6054.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drosten C., Gunther S., Preiser W., van der Werf S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A., Berger A., Burguiere A.M., Cinatl J., Eickmann M., Escriou N., Grywna K., Kramme S., Manuguerra J.C., Muller S., Rickerts V., Sturmer M., Vieth S., Klenk H.D., Osterhaus A.D., Schmitz H., Doerr H.W. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Duquerroy S., Vigouroux A., Rottier P.J., Rey F.A., Bosch J.B. Central ions and lateral asparagine/glutamine zippers stabilize the post-fusion hairpin conformation of the SARS coronavirus spike glycoprotein. Virology. 2005;335:276–285. doi: 10.1016/j.virol.2005.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckert D.M., Kim P.S. Mechanisms of viral membrane fusion and its inhibition. Annu. Rev. Biochem. 2001;70:777–810. doi: 10.1146/annurev.biochem.70.1.777. [DOI] [PubMed] [Google Scholar]
- Follis K.E., York J., Nunberg J.H. Serine-scanning mutagenesis studies of the C-terminal heptad repeats in the SARS coronavirus S glycoprotein highlight the important role of the short helical region. Virology. 2005;341:122–129. doi: 10.1016/j.virol.2005.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuerst T.R., Niles E.G., Studier F.W., Moss B. Eukaryotic transient-expression system based on recombinant vaccinia virus that synthesizes bacteriophage T7 RNA polymerase. Proc. Natl. Acad. Sci. U.S.A. 1986;83:8122–8126. doi: 10.1073/pnas.83.21.8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukushi S., Mizutani T., Saijo M., Matsuyama S., Miyajima N., Taguchi F., Itamura S., Kurane I., Morikawa S. Vesicular stomatitis virus pseudotyped with severe acute respiratory syndrome coronavirus spike protein. J. Gen. Virol. 2005;86:2269–2274. doi: 10.1099/vir.0.80955-0. [DOI] [PubMed] [Google Scholar]
- Gibbs A.J., Gibbs M.J., Armstrong J.S. The phylogeny of SARS coronavirus. Arch. Virol. 2004;149:621–624. doi: 10.1007/s00705-003-0244-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giroglou T., Cinatl Jr J., Rabenau H., Drosten C., Schwalbe H., Doerr H.W., von Laer D. Retroviral vectors pseudotyped with severe acute respiratory syndrome coronavirus S protein. J. Virol. 2004;78:9007–9015. doi: 10.1128/JVI.78.17.9007-9015.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez J.M., Gomez-Puertas P., Cavanagh D., Gorbalenya A.E., Enjuanes L. A comparative sequence analysis to revise the current taxonomy of the family Coronaviridae. Arch. Virol. 2003;148:2207–2235. doi: 10.1007/s00705-003-0162-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon V.M., Klimpel K.R., Arora N., Henderson M.A., Leppla S.H. Proteolytic activation of bacterial toxins by eukaryotic cells is performed by furin and by additional cellular proteases. Infect. Immun. 1995;63:82–87. doi: 10.1128/iai.63.1.82-87.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y., Zheng B.J., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L., Luo S.W., Li P.H., Zhang L.J., Guan Y.J., Butt K.M., Wong K.L., Chan K.W., Lim W., Shortridge K.F., Yuen K.Y., Peiris J.S., Poon L.L. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- Gubbins M.J., Plummer F.A., Yuan X.Y., Johnstone D., Drebot M., Andonova M., Andonov A., Berry J.D. Molecular characterization of a panel of murine monoclonal antibodies specific for the SARS-coronavirus. Mol. Immunol. 2005;42:125–136. doi: 10.1016/j.molimm.2004.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingley S.T., Leparc-Goffart I., Seo S.H., Tsai J.C., Weiss S.R. The virulence of mouse hepatitis virus strain A59 is not dependent on efficient spike protein cleavage and cell-to-cell fusion. J. NeuroVirol. 2002;8:400–410. doi: 10.1080/13550280260422703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruby D.E., Lynn D.L., Kates J.R. Identification of a virus-specified protein in the nucleus of vaccinia virus-infected cells. J. Gen. Virol. 1980;47:293–299. doi: 10.1099/0022-1317-47-2-293. [DOI] [PubMed] [Google Scholar]
- Huang I.C., Bosch B.J., Li F., Li W., Lee K.H., Ghiran S., Vasilieva N., Dermody T.S., Harrison S.C., Dormitzer P.R., Farzan M., Rottier P.J., Choe H. SARS coronavirus, but not human coronavirus NL63, utilizes cathepsin L to infect ACE2-expressing cells. J. Biol. Chem. 2006;281:3198–3203. doi: 10.1074/jbc.M508381200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughson F.M. Enveloped viruses: a common mode of membrane fusion? Curr. Biol. 1997;7:R565–R569. doi: 10.1016/s0960-9822(06)00283-1. [DOI] [PubMed] [Google Scholar]
- Kim J.-S., Raines R.T. Ribonuclease S-peptide as a carrier in fusion proteins. Protein Sci. 1993;2:348–356. doi: 10.1002/pro.5560020307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klenk H.D., Garten W. Host cell proteases controlling virus pathogenicity. Trends Microbiol. 1994;2:39–43. doi: 10.1016/0966-842x(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Krueger D.K., Kelly S.M., Lewicki D.N., Ruffolo R., Gallagher T.M. Variations in disparate regions of the murine coronavirus spike protein impact the initiation of membrane fusion. J. Virol. 2001;75:2792–2802. doi: 10.1128/JVI.75.6.2792-2802.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., Tong S., Urbani C., Comer J.A., Lim W., Rollin P.E., Dowell S.F., Ling A.E., Humphrey C.D., Shieh W.J., Guarner J., Paddock C.D., Rota P., Fields B., DeRisi J., Yang J.Y., Cox N., Hughes J.M., LeDuc J.W., Bellini W.J., Anderson L.J., and SARS Working Group A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- Kuiken T., Fouchier R.A., Schutten M., Rimmelzwaan G.F., van Amerongen G., van Riel D., Laman J.D., de Jong T., van Doornum G., Lim W., Ling A.E., Chan P.K., Tam J.S., Zambon M.C., Gopal R., Drosten C., van der Werf S., Escriou N., Manuguerra J.C., Stohr K., Peiris J.S., Osterhaus A.D. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet. 2003;362:263–270. doi: 10.1016/S0140-6736(03)13967-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunkel F., Herrler G. Structural and functional analysis of the S proteins of two human coronavirus OC43 strains adapted to growth in different cells. Arch. Virol. 1996;141:1123. doi: 10.1007/BF01718615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai M.M.C., Holmes K.V. Coronaviridae: the viruses and their replication. In: Knipe D., Howley P.M., editors. Fields' Virology. 4th ed. Lippincott Williams and Wilkins; Philadelphia: 2001. pp. 1163–1185. [Google Scholar]
- Lau S.K., Woo P.C., Li K.S., Huang Y., Tsoi H.W., Wong B.H., Wong S.S., Leung S.Y., Chan K.H., Yuen K.Y. Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proc. Natl. Acad. Sci. U.S.A. 2005;102:14040–14045. doi: 10.1073/pnas.0506735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., Choe H., Farzan M. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Shi Z., Yu M., Ren W., Smith C., Epstein J.H., Wang H., Crameri G., Hu Z., Zhang H., Zhang J., McEachern J., Field H., Daszak P., Eaton B.T., Zhang S., Wang L.F. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310:676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- Matsuyama S., Ujike M., Morikawa S., Tashiro M., Taguchi F. Protease-mediated enhancement of severe acute respiratory syndrome coronavirus infection. Proc. Natl. Acad. Sci. U.S.A. 2005;102:12543–12547. doi: 10.1073/pnas.0503203102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molloy S.S., Anderson E.D., Jean F., Thomas G. Bi-cycling the furin pathway: from TGN localization to pathogen activation and embryogenesis. Trends Cell Biol. 1999;9:28–35. doi: 10.1016/s0962-8924(98)01382-8. [DOI] [PubMed] [Google Scholar]
- Moore M.J., Dorfman T., Li W., Wong S.K., Li Y., Kuhn J.H., Coderre J., Vasilieva N., Han Z., Greenough T.C., Farzan M., Choe H. Retroviruses pseudotyped with the severe acute respiratory syndrome coronavirus spike protein efficiently infect cells expressing angiotensin-converting enzyme 2. J. Virol. 2004;78:10628–10635. doi: 10.1128/JVI.78.19.10628-10635.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash T.C., Buchmeier M.J. Entry of mouse hepatitis virus into cells by endosomal and nonendosomal pathways. Virology. 1997;233:1–8. doi: 10.1006/viro.1997.8609. [DOI] [PubMed] [Google Scholar]
- Neumann G., Feldmann H., Watanabe S., Lukashevich I., Kawaoka Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 2002;76:406–410. doi: 10.1128/JVI.76.1.406-410.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum O., Broder C.C., Berger E.A. Fusogenic mechanisms of enveloped-virus glycoproteins analyzed by a novel recombinant vaccinia virus-based assay quantitating cell fusion-dependent reporter gene activation. J. Virol. 1994;68:5411–5422. doi: 10.1128/jvi.68.9.5411-5422.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris J.S., Lai S.T., Poon L.L., Guan Y., Yam L.Y., Lim W., Nicholls J., Yee W.K., Yan W.W., Cheung M.T., Cheng V.C., Chan K.H., Tsang D.N., Yung R.W., Ng T.K., Yuen K.Y., SARS study group Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince A.M., Reesink H., Pascual D., Horowitz B., Hewlett I., Murthy K.K., Cobb K.E., Eichberg J.W. Prevention of HIV infection by passive immunization with HIV immunoglobulin. AIDS Res. Hum. Retroviruses. 1991;7:971–973. doi: 10.1089/aid.1991.7.971. [DOI] [PubMed] [Google Scholar]
- Rockwell N.C., Krysan D.J., Komiyama T., Fuller R.S. Precursor processing by kex2/furin proteases. Chem. Rev. 2002;102:4525–4548. doi: 10.1021/cr010168i. [DOI] [PubMed] [Google Scholar]
- Sanchez C.M., Gebauer F., Sune C., Mendez A., Dopazo J., Enjuanes L. Genetic evolution and tropism of transmissible gastroenteritis coronaviruses. Virology. 1992;190:92–105. doi: 10.1016/0042-6822(92)91195-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander C., Schneider R. Database of homology-derived structures and the structural meaning of sequence alignment. Proteins. 1991;9:56–68. doi: 10.1002/prot.340090107. [DOI] [PubMed] [Google Scholar]
- Simmons G., Reeves J.D., Rennekamp A.J., Amberg S.M., Piefer A.J., Bates P. Characterization of severe acute respiratory syndrome-associated coronavirus (SARS-CoV) spike glycoprotein-mediated viral entry. Proc. Natl. Acad. Sci. U.S.A. 2004;101:4240–4245. doi: 10.1073/pnas.0306446101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons G., Gosalia D.N., Rennekamp A.J., Reeves J.D., Diamond S.L., Bates P. Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proc. Natl. Acad. Sci. U.S.A. 2005;102:11876–11881. doi: 10.1073/pnas.0505577102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skehel J.J., Wiley D.C. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 2000;69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- Snijder E.J., Bredenbeek P.J., Dobbe J.C., Thiel V., Ziebuhr J., Poon L.L., Guan Y., Rozanov M., Spaan W.J., Gorbalenya A.E. Unique and conserved features of genome and proteome of SARS-coronavirus, an early split-off from the coronavirus group 2 lineage. J. Mol. Biol. 2003;331:991–1004. doi: 10.1016/S0022-2836(03)00865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H.C., Seo M.Y., Stadler K., Yoo B.J., Choo Q.L., Coates S.R., Uematsu Y., Harada T., Greer C.E., Polo J.M., Pileri P., Eickmann M., Rappuoli R., Abrignani S., Houghton M., Han J.H. Synthesis and characterization of a native, oligomeric form of recombinant severe acute respiratory syndrome coronavirus spike glycoprotein. J. Virol. 2004;78:10328–10335. doi: 10.1128/JVI.78.19.10328-10335.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storz J., Rott R., Kaluza G. Enhancement of plaque formation and cell fusion of an enteropathogenic coronavirus by trypsin treatment. Infect. Immun. 1981;31:1214–1222. doi: 10.1128/iai.31.3.1214-1222.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturman L.S., Ricard C.S., Holmes K.V. Proteolytic cleavage of the E2 glycoprotein of murine coronavirus: activation of cell-fusing activity of virions by trypsin and separation of two different 90K cleavage fragments. J. Virol. 1985;56:904–911. doi: 10.1128/jvi.56.3.904-911.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Supekar V.M., Bruckmann C., Ingallinella P., Bianchi E., Pessi A., Carfi A. Structure of a proteolytically resistant core from the severe acute respiratory syndrome coronavirus S2 fusion protein. Proc. Natl. Acad. Sci. U.S.A. 2004;101:17958–17963. doi: 10.1073/pnas.0406128102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taguchi F. Fusion formation by the uncleaved spike protein of murine coronavirus JHMV variant cl-2. J. Virol. 1993;67:1195–1202. doi: 10.1128/jvi.67.3.1195-1202.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijgen L., Keyaerts E., Moes E., Thoelen I., Wollants E., Lemey P., Vandamme A.M., Van Ranst M. Complete genomic sequence of human coronavirus OC43: molecular clock analysis suggests a relatively recent zoonotic coronavirus transmission event. J. Virol. 2005;79:1595–1604. doi: 10.1128/JVI.79.3.1595-1604.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissenhorn W., Dessen A., Calder L.J., Harrison S.C., Skehel J.J., Wiley D.C. Structural basis for membrane fusion by enveloped viruses. Mol. Membr. Biol. 1999;16:3–9. doi: 10.1080/096876899294706. [DOI] [PubMed] [Google Scholar]
- Wool-Lewis R.J., Bates P. Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J. Virol. 1999;73:1419–1426. doi: 10.1128/jvi.73.2.1419-1426.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao X., Chakraborti S., Dimitrov A.S., Gramatikoff K., Dimitrov D.S. The SARS-CoV S glycoprotein: expression and functional characterization. Biochem. Biophys. Res. Commun. 2003;312:1159–1164. doi: 10.1016/j.bbrc.2003.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Lou Z., Liu Y., Pang H., Tien P., Gao G.F., Rao Z. Crystal structure of severe acute respiratory syndrome coronavirus spike protein fusion core. J. Biol. Chem. 2004;279:49414–49419. doi: 10.1074/jbc.M408782200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada Y.K., Takimoto K., Yabe M., Taguchi F. Requirement of proteolytic cleavage of the murine coronavirus MHV-2 spike protein for fusion activity. Adv. Exp. Med. Biol. 1998;440:89–93. doi: 10.1007/978-1-4615-5331-1_12. [DOI] [PubMed] [Google Scholar]
- Yang Z.Y., Huang Y., Ganesh L., Leung K., Kong W.P., Schwartz O., Subbarao K., Nabel G.J. pH-dependent entry of severe acute respiratory syndrome coronavirus is mediated by the spike glycoprotein and enhanced by dendritic cell transfer through DC-SIGN. J. Virol. 2004;78:5642–5650. doi: 10.1128/JVI.78.11.5642-5650.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York J., Romanowski V., Lu M., Nunberg J.H. The signal peptide of the Junín arenavirus envelope glycoprotein is myristoylated and forms an essential subunit of the mature G1–G2 complex. J. Virol. 2004;78:10783–10792. doi: 10.1128/JVI.78.19.10783-10792.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K., Yi L., Chen J., Qu X., Qing T., Rao X., Jiang P., Hu J., Xiong Z., Nie Y., Shi X., Wang W., Ling C., Yin X., Fan K., Lai L., Ding M., Deng H. Suppression of SARS-CoV entry by peptides corresponding to heptad regions on spike glycoprotein. Biochem. Biophys. Res. Commun. 2004;319:746–752. doi: 10.1016/j.bbrc.2004.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]


