Abstract
Why do some countries more effectively respond to crises than others? This paper compares China’s relatively effective response to the 2002–3 SARS outbreak with Taiwan’s relatively ineffective response, focusing on three variables that constitute China’s ‘authoritarian advantage’ - centralized decision making powers; public support; and, relations with the mass media. The paper rejects a fourth explanatory variable specific to the Taiwan case – membership in international organizations. Drawing heavily on the Taiwan example, the paper concludes by suggesting options for overcoming the authoritarian advantage in pandemic response.
Keywords: Taiwan, China, SARS, Pandemic Response, Authoritarian Advantage
Introduction
In the aftermath of the SARS epidemic much was made of China’s effective efforts at disease control and prevention. China’s perceived success in controlling SARS stands in stark contrast with Taiwan’s troubled response to its own SARS outbreak. Why does Taiwan, a geographically small, densely populated country with a democratic government, wealthy and modern knowledge-based economy, fail to effectively respond to SARS whereas big, heavily populated, relatively under-developed and authoritarian China succeeds? Does regime type explain China’s relative success, and to the extent that regime type matters, what can be done to compensate for China’s ‘authoritarian advantage’ in crisis response?
To address these questions I conduct a comparative analysis of pandemic response by Taiwan and China. Due to space limitations, I focus primarily on Taiwan, drawing on previous studies of China to highlight the differences between Chinese and Taiwanese responses. In the final section I draw on this comparison to identify means to compensate for China’s ‘authoritarian advantage’.
Crisis and Response
The crisis literature distinguishes between routine crises and novel crises. In routine crises (frequently recurring crises such as fires and floods), political leaders may defer to operational commanders – people such as fire fighters or police officers - who have dealt with similar crises in the past. These operational commanders have trained for, and perhaps experienced similar crises and are able to respond effectively with only moderate adaptation of existing crisis response procedures [1].
However, this approach cannot be followed in the case of novel crises. Novel crises are crises where there is little past experience to draw on. Such crises include massive events such as hurricane Katrina, the 2011 Japan earthquake and tsunami or the 9/11 attacks on the United States that explode on the scene, or more insidious crises such as the spread of a previously unknown infectious disease that only slowly makes itself evident. Of the two types of novel crises the insidious type is often far more dangerous. The danger lies in the likelihood that the leadership will fail to recognize the insidious crisis as a crisis because it develops only slowly and seems amenable to existing response strategies. As a result, the leadership may become aware of the crisis only after it has become widespread or more threatening [2]. SARS is an example of insidious crises. It at first went unrecognized and only slowly did the leadership come to realize the immensity of the threat it represented.
Both forms of novel crises require flexible leadership and response capabilities. The leadership must quickly identify the challenge, engage relevant bureaucracies, implement a response, communicate the nature of the crisis and response effectively and clearly to the public, and control the message as it is being broadcast by the media to the public. These already extremely challenging tasks must be accomplished in a compressed timeframe under highly stressful conditions. Not surprisingly, governments often fail.
Some authors argue that an already challenging situation for leaders is made even more so if they are functioning in a democratic system. In democracies, major emergencies require involvement by multiple jurisdictions and many levels of representative government. Coordinating among these often overlapping and contentious jurisdictions can be difficult. Politicians must identify and justify priorities and actions to local leaders, the public and the mass media.1
These same authors suggest that the challenges are less significant in authoritarian regimes. Authoritarian leaders enjoy an ‘authoritarian advantage’, being less likely to need to negotiate with bureaucracies over jurisdictional powers or struggle to disentangle overlapping institutions. Furthermore, the media and by extension the message to the public are more easily controlled.
In this paper I conduct a comparative case study of China and Taiwan responses to SARS to explore the authoritarian advantage in pandemic crisis response. Drawing on the crisis literature and previously conducted research on China’s SARS response, three factors appear key to effective response in public health crises. These are centralized decision making powers, public support for government initiatives, and government ability to shape the tone of the crisis in the mass media. Utilizing its authoritarian advantage, China’s regime was able to effectively centralize decision making powers, rally public support and control the message presented by the mass media with the end result an effective pandemic response. Did Taiwan’s lack of an authoritarian regime undermine its engagement with these three factors, contributing to the ineffective Taiwan response?
In conducting this analysis I focus on the contribution of a specific variable (authoritarian advantage) to produce a particular outcome (pandemic response). Thus, I ask, does an authoritarian advantage in particular play a role in effective pandemic response? In so doing I do not suggest that authoritarian advantage is the sole causal variable for successful pandemic response. I acknowledge that other variables may contribute to effective pandemic response. However since it is impossible to identify the causal impact of all potential explanatory variables, I seek to understand the impact of the authoritarian advantage in particular.2
And yet, because the Taiwan government of the time repeatedly and explicitly asserted that Taiwan’s lack of membership in international public health organizations constituted a major obstacle to effective SARS response, I consider this possibility as well.
Section I: Genesis of the Taiwan SARS Epidemic
SARS was first identified in November 2002 in China. The disease crossed the Taiwan Strait in mid-March 2003, with the first Taiwan case diagnosed on 10 March of that year. By the conclusion of what became a global outbreak, Taiwan had earned the dubious distinction of the world’s third largest outbreak location. Indeed, of the 32 countries affected by SARS, Taiwan was the only one to suffer a sustained outbreak after the WHO issued its 12 March Global Alert on atypical pneumonia and its 15 March Emergency Travel Advisory [7].
Taiwan’s SARS epidemic divides into two stages. In the first stage, 10 March to 20 April 2003, 28 probable SARS cases were identified with no fatalities. During this phase, 78 percent of cases were imported from China or Hong Kong, while the remaining cases developed from household or social contact with a SARS patient (16 percent) or through contact in a hospital setting (6 percent). During this first stage, hospitals effectively cared for all SARS patients. In addition, effective contact tracing ensured that of the 28 probable SARS cases reported, only four resulted from secondary transmission rather than imported cases.3 To this stage, Taiwan’s existing mechanisms proved sufficient to effectively respond to the SARS outbreak.
Believing SARS to be under control, on 12 April the WHO changed Taiwan’s status from that of an ‘affected area’ to that of an ‘area with limited local transmission’.4 The Taiwan government celebrated its changed status, boasting its ‘three zero’ record: zero deaths; zero community infections and zero exported cases. Partially to celebrate its success in containing SARS, Taiwan hosted an International SARS Symposium on 20–21 April. Perhaps ironically, it was at this time, with the government widely publicizing its success with SARS control that the outbreak entered its second, more dangerous stage of widespread community transmission.
According to Dr. Chen Tsai-Ching, then Director-General of the TCDC (Taiwan Centres for Disease Control), during the second stage of SARS, the majority of community transmissions occurred as a result of one ‘super spreader’.5 The super-spreader, a laundry worker at Taipei Municipal Hoping Hospital, infected over two dozen patients and staff members, initiating an ever widening circle of infection.
On 24 April, 2003, Hoping hospital officials responded to spreading SARS cases by closing down the facility. All patients were expected to either independently or through the health system, transfer to other hospitals for continuing care. This patient dispersal led directly to infectious disease outbreaks in eight additional hospitals in Taipei and Kaohsiung.6
During the second stage, probable SARS incidences increased six-fold in less than one month. Of the new cases, 89 percent were hospital-acquired, two percent were the result of household or social contact with a SARS patient, and nine percent were travel related. When, on 5 July 2003, Taiwan was finally removed from the WHO list of areas with recent local disease transmissions, the island had reported 346 confirmed SARS cases and 37 SARS-related deaths.7 In this second stage of the outbreak, Taiwan clearly failed in its pandemic response. As noted, only Taiwan suffered a sustained outbreak after the 12 March WHO global alert.
Public Health in Taiwan8
In the 1940s-50s, the WHO (World Health Organization) assisted Taiwan’s Nationalist government design a public health system that emphasized diagnosis, treatment and control of infectious diseases, prioritizing preventive care over curative care.9 An outcome of this prevention model was a steep decline in the number and extent of infectious disease outbreaks in Taiwan. Thus, between 1954 and 1970 the annual number of cases of recognized infectious disease outbreaks declined from 6,000 to 300. By the 1980s the preventive care approach adopted by Taiwan’s public health system achieved eradication of numerous infectious diseases, including malaria, infantile paralysis and Japanese encephalitis.
Taiwan’s public health system consists of two levels. At the central level is the DoH (Department of Health) which reports directly to the Executive Yuan. The second, local level consists of health departments in Taiwan’s two special municipalities - Taipei and Kaohsiung - as well as health bureaus based in twenty-three county and city governments. Under the authority of the Executive Yuan, the DoH develops health care policies, declares and cancels epidemic alerts, gives orders for both household and port quarantines, and supervises, commands, guides and assesses local level policy implementation. The local level is responsible for developing implementation plans for DoH policies.10
At the heart of Taiwan’s infectious disease control system is the Communicable Disease Control Act. The Act provides the legal basis for Taiwan’s responses to any infectious disease outbreaks. Article three of the Act designates five categories of communicable diseases and the corresponding severity-based responses. Category 1 includes diseases such as Cholera, Plague, Yellow Fever, and with post-SARS revisions, SARS. Category 2 includes diseases such as Typhus Fever, Diphtheria and Meningococcal Meningitis. Category 3 includes diseases such as Tuberculosis, Leprosy and Rubella. Category 4 includes known communicable diseases and syndromes not appearing in the first three categories, but that the government deems should be controlled. Category 5 is an ad-hoc classification for emerging infectious diseases so that government and health authorities can legally implement control measures as needed until further scientific investigation allows for permanent reclassification.11
Taiwan shifted away from its emphasis on preventive care in the 1980s as government increasingly prioritized rapid economic growth and profitability. Because preventive care proved unprofitable, newly privatized treatment facilities shifted their focus to curative care. Even government infectious disease departments shrank with a decline in DoH budgetary allocations for all that was related to disease prevention, public health services and public health education [9].
In the context of this analysis, the key point is that despite early positive trends and investment in building the infrastructure necessary for effective pandemic response, as a result of shifting priorities, Taiwan’s epidemic response capacity had eroded by the time SARS arrived.
Taiwan’s SARS Response
In accordance with the Communicable Disease Control Act, during an infectious disease outbreak, the DoH (Central Competent Authority) must establish a central epidemic control centre to enable cooperation and resource sharing between private, public, medical, administrative and academic sectors (Art. 17). Local level governments may establish epidemic command centres and mobile disease control teams that are subordinate to the central epidemic control centre (Art. 14-16).
On 17 March 2003, the Executive Yuan ordered the DoH to establish the SARS Coordination Centre and on 28 April, the SARS Prevention and Relief Committee. The TCDC (Taiwan Centres for Disease Control) organized a SARS Advisory Committee, consisting of infectious disease specialists, respiratory specialists and epidemiologists. This committee met daily to review recent SARS cases.
Various regulations and guidelines were developed or revised during spring and summer 2003 to enhance the public health response to SARS. The most important of the new regulations was the Provisional Act Governing the Control and Relief of Severe Acute Respiratory Syndrome (SARS) passed by the Executive Yuan on 2 May 2003 (19 articles). This act contains many of the same regulations as the Communicable Disease Act (amended to include 77 articles), but with specifications to confront the unique challenges posed by SARS.12
The Provisional Act, like the Communicable Disease Control Act, confers immense power on the DoH at the central level; the municipal governments at the municipality level; and the county (city) governments at the county (city) level - described as ‘competent authorities’ (article 2, Communicable Disease Control Act). Under the Communicable Disease Control Act competent authorities may prohibit any group activities such as school attendance, business meetings and banquets, and can restrict transportation and access to specified locations (article 37). Articles five and eight of the Provisional Act confer on competent authorities the power to require suspected SARS patients to undergo prescribed treatment and prevention measures – if necessary, using coercive means. Article 7 of the Provisional Act empowers competent authorities to requisition from the private and public sector land, buildings, medical equipment, waste disposal facilities, vehicles, aircraft and more generally, any materials the DOH deems necessary for epidemic control. The Provisional Act also confers the power to utilize mass media and communications facilities to collect and report information relating to the epidemic and to emergency care initiatives (article 11). Finally, schools, associations, and public and private organizations must grant official leave to anyone placed under mandatory quarantine or isolation (article 8). Additional relevant Taiwanese public health laws arising from the Communicable Disease Control Act include the Law on Control of Communicable Diseases and the Regulations Governing Quarantine. These both strengthen and add specificity to the Communicable Disease Control Act in their respective spheres.
The DoH established two quarantine categories.13 Category A quarantines related to people infected in Taiwan. Category A quarantines took place in the person’s home, unless he/she was a health care worker or hospital patient exposed to a SARS patient. People under category A quarantine were initially required to remain under quarantine for 10–14 days, and could only leave their quarantine site with the permission of health officials. Category B quarantines were for travellers from regions designated by the WHO as SARS affected. People quarantined under category B were confined to their homes, to a designated airport hotel, or to a designated quarantine centre. If they agreed to don a surgical mask, individuals subject to category B quarantine were permitted to exit quarantine for exercise, shopping, meals and other tasks approved by health authorities. In total, 131,132 people were quarantined during Taiwan’s SARS outbreak. All quarantined people were required to check and record their temperatures two to three times a day.
Incentives to comply with quarantine and isolation requirements included a NT$5,000 reward for people adhering to their quarantine requirements for the designated period. In addition, people under quarantine were provided social services such as psychological support and child care through the local governments.
Incentives for those caring for SARS patients included a TCDC-funded NT$10,000/day danger pay bonus for physicians and a NT$3,000/eight hour shift bonus for nurses. Any medical personnel infected with SARS were further compensated. For example, the state committed to providing full tuition through college to any child whose parent died while treating SARS patients. The state also committed to support any family whose livelihood was threatened by the mandatory isolation of its main breadwinner.
From 28 April, the Taiwan government also enacted a two-week ban on visas for travellers from regions designated by the WHO as SARS affected. Following expiry of the two week travel ban, travellers from SARS affected regions were required to don surgical masks prior to departing for Taiwan. Any passenger failing to abide by this regulation was barred entry. Upon arrival in Taiwan, passengers from SARS affected regions were subjected to category B quarantine.14
On 20 May, the DoH specified twelve hospitals that would be dedicated SARS hospitals. Although no regulations were developed regarding admission policies for fever patients, the DoH did establish approximately one hundred fever clinics to screen potential SARS patients and minimize transmission into emergency departments.
Public education became a critical aspect of the government’s efforts to control SARS through voluntary, rather than compulsory prevention and control measures. During the second stage of the epidemic, the DoH held daily press conferences on infection control and prevention and produced a daily SARS prevention TV program to announce government measures and policies aimed at countering the epidemic. The DoH made additional information available through its website and in pamphlets at convenience stores and gas stations. Finally, the DoH developed a temperature monitoring campaign, and advertised on television, in posters, fliers, radio, the internet, magazines and newspapers, to provide the public with access to updated SARS information. These initiatives were supplemented with fever hotlines managed by local medical associations [10].
Comparing Infectious Disease responses in Taiwan and China
Similarities between Taiwan and China make these two political entities useful when comparing causes for their relative success in epidemic prevention and control. Both early on invested heavily in state driven disease prevention policies resulting in unusually healthy populations given their levels of development. In terms of infectious disease control, both China and Taiwan followed a similar path by providing effective health care focused on prevention. The result for both included plummeting mortality rates and rapidly improving quality of life indicators. Their success is illustrated by the fact that both early on underwent the epidemiological transition – with chronic diseases replacing infectious diseases as the main cause of death. Both countries also moved in the 1980s from a health care system focused on preventive care to one focused on curative care. In both systems the state withdrew from health care provision with the private sector expected to pick up the slack.
However, there are also notable differences. In terms of political systems, these two entities differ dramatically. China is a one-party Leninist regime, whereas Taiwan is a vibrant multi-party democracy.15 The WHO is among many health organizations that have praised the Taiwanese National Health Insurance program (established in 1995), describing it as effectively and efficiently providing all Taiwan’s people with health care. A 2008 study by Huang, Wang and Chen found that Taiwan’s health care system compares favourably with OECD country health care systems in terms of health and efficiency indicators [11]. By contrast, by the time of the SARS outbreak, China’s once much vaunted public health system was being described as worse even than those in parts of Africa.16
In addition, Taiwan is an island, and is therefore relatively easily isolated from the outside. By contrast, China has long, often porous land borders. Unlike China’s massive 1.34 billion person population, Taiwan’s population is relatively small (23 million). Taiwan is a developed country with advanced medical facilities and well trained physicians. China too has advanced medical facilities and well trained physicians, however these are heavily concentrated in major cities. Finally, specifically as relates to SARS, Taiwan enjoyed the luxury of time. The epidemic arrived in Taiwan well after appearing in China.
The relative Chinese success in responding to SARS is illustrated by the SARS epidemic curves for Taiwan and China (Figs. 1 and 2 below). Epidemic curves illustrate the progression of an outbreak with the horizontal axis representing time and the vertical axis representing the number of cases. The epidemic curves (the bottom curve in the graphs) illustrate the lifecycle of the epidemic. Excluding the large spikes in late March and early April - which indicate the days that the Chinese government stopped trying to conceal SARS - incidence of the disease in China follow a standard shaped epidemic curve - initial difficulties with prevention and control followed by an eventual effective response. By contrast, Taiwan’s epidemic curve illustrates an ineffective response. The curve displays Taiwan’s initial success with five weeks of control over outbreaks, followed by sharp bumps of SARS incidence in mid to late April, finally coming under control in mid-June.
Fig. 1.
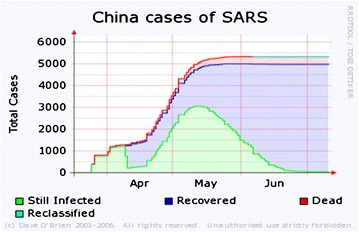
China cases of SARS
Fig. 2.
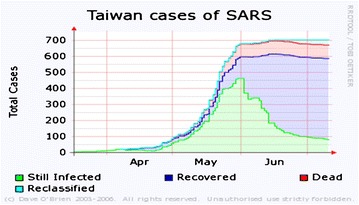
Taiwan cases of SARS
A comparison of the number of cases and fatalities in China and Taiwan is also informative. During the SARS outbreak China suffered a total of 5327 cases and 349 deaths. By contrast, Taiwan suffered 346 cases and 37 deaths. On a per capita basis, Taiwan clearly suffered more cases and more fatalities. This is illustrated by the Case Fatality Ratios. The WHO defines Case Fatality Ratio as “the ratio of deaths within a designated population of people with a particular condition, over a certain period of time”.17 China’s Case Fatality Ratio of 7 was superior to the global Ratio of 9.6, whereas Taiwan’s Ratio of 11 was inferior. These data suggest that, despite the advantages enjoyed by Taiwan, as Taiwanese officials admit, Taiwan’s response to SARS was problematic.18
I turn now to an analysis of how centralized decision making powers, public support for government initiatives, and government ability to shape the tone of the crisis in the mass media were impacted by the existence or lack of an authoritarian advantage.
Centralized Decision Making Powers
Since initiating economic reforms in China in the late 1970s, the Chinese system has undergone increased decentralisation. However, despite this trend towards greater local decision making and implementation autonomy, the central leadership retains significant powers. Thus, when the leadership identifies an issue as a high priority, it is able to re-centralise power to itself. After initial hesitation, the Chinese leadership concluded that the SARS outbreak represented a significant threat to China. The leadership therefore recentralised power, establishing clear lines of control from the central level to the township level. While local governments occasionally disregarded central government decisions, by and large, the centre was able to control policy implementation. Thus, local health officials were required to provide daily reports up a clear chain of command to the centre. These reports were made available online. When the newly established (2001) Chinese CDC proved insufficiently effective in responding to SARS, the central government transferred responsibility for SARS to the MoH. In an unusual step for the PRC, the minister of health was replaced with a vice-premier (Wu Yi). Wu Yi’s high rank and status in the Party/state lent tremendous prestige and power to the MoH, signalling the seriousness with which the centre took the outbreak.
By contrast, Taiwan’s Provisional Act did not include explicit delineations of power and responsibilities. As the incidences of SARS rapidly increased, Taiwan’s SARS Prevention and Relief Committee could no longer review all potential SARS cases in a timely fashion with official SARS classifications taking over twelve days (during which patients were often placed in general hospital rooms). Recognizing that this was too slow, the TCDC began cooperating with the Bureau of National Health Insurance regional offices in north, south and central Taiwan. These regional offices took over case review responsibilities and established a far more efficient set of local SARS expert committees. However, these multiple SARS committees lacked clear bureaucratic lines of control. As a result, communication between central and local SARS epidemic control centres was poor, with the failure to establish a central coordination and control mechanism contributing to the confusion. Essentially working independently, local governments improvised responses to the increasing number of SARS patients.
Taiwan CDC authorities did not begin advising local healthcare workers about SARS transmission or infection control until the second stage of the Taiwan outbreak – with the chain of April-May 2003 nosocomial (hospital related) infections catapulting Taiwan from a WHO classification of limited transmission to the 3rd largest SARS outbreak in the world in absolute terms (Following China and Hong Kong). Nonsocomial infection control mechanisms and a requirement for all healthcare workers to wear masks were not implemented until 26 April. The DoH requested that health officials strengthen infection control auditing in hospitals on 14 May as no guidelines for hospital infection control existed. Only on 23 May did the central SARS Contingency Committee finally pass a resolution to implement guidelines on SARS patient assessment.
An additional constraint on cooperation and coordination among authorities in Taiwan was the large number of units involved in all decisions, and political manoeuvring within and among levels of government. At the central level, coordination was required among departments and sub-departments of the Executive Yuan, the Labour Affairs Council, the Mainland Affairs Council, the Civil Aeronautics Administration, the Ministry of Transportation, the Ministry of Communications and the Government Information office. This required strong guidance from the central government, something that was not possible. Indeed different spokespersons represented different branches of government, and as a result failed to provide a unified message.
Exemplifying the challenge of unifying control was the failure to effectively coordinate between the Taipei government and the central government. Taipei was the main outbreak locale in the country, and was governed by the KMT party, whereas the central government was controlled by the rival DPP. These governments struggled to work together because of their adversarial political relationship. In addition, since during the SARS outbreak, Public Health Bureaus (at the city level) and public health centres (at the local level) were bureaucratically subordinate to the local government rather than to the TCDC or DoH, local governments were able to ignore central government agency directives.19
As a component of its SARS response, China developed detailed hospitalization procedures that were widely implemented. These required that any person arriving at a hospital be checked for fever prior to entering the hospital grounds. If the person was found to have fever or other SARS-like symptoms, she was placed in a ward isolated from the hospital itself.20
In Taiwan, hospitals lacked standard procedures for admitting fever patients. Panicked patients with minor illnesses swamped many hospitals. Overall, hospital facilities proved insufficient to absorb the flood of patients potentially ill with SARS. Consequently, while awaiting proper treatment and isolation, undiagnosed SARS patients often remained in crowded wards or emergency departments for days, exposing hundreds of people to SARS.
In response to the failure of Taiwan hospitals to control the in-hospital spread of SARS, in Spring 2003 nine major hospital centres were fully or partially closed. Taiwan University Hospital superintendent, Dr. Chen Ming-Feng blamed the Taiwan CDC and DoH for his hospital’s poor response. Among the leading hospital centres in Taiwan, Taiwan University hospital was so overcrowded it was forced to turn away new patients or transfer existing patients to other hospitals. However, reflecting the chaos in the health system, these other hospitals often refused to accept the transferred patients.
In addition, Taiwan hospitals receive funding from the state based on the number of patients seen. In order to minimize financial loses that would result from a rush to depart the hospital by patients fearing SARS, many hospitals sought to avoid reporting probable SARS patients within their facilities.
In China, designated SARS physicians and nurses were on 24 hour duty and were not permitted to leave their places of work for up to three months. All their needs were provided at the hospital itself, with the result that they were cut off from family and friends for the entire period. Very few health care providers refused to serve. Those who did refuse were fired from their positions. Strengthening health care worker resolve were official, televised ceremonies describing the heroic efforts they were making and thanking them for their work.
Contrasting this situation was the chaos that defined Taiwan hospitals as the second stage of the SARS epidemic developed. Hoping Hospital where the second SARS phase originated, was closed on 23 April 2003. Anyone in the hospital when it was closed, including patients, visitors, doctors and other staff members, was quarantined within the hospital for two weeks. Police were sent in to enforce this quarantine, however, after only one day, several health care workers and staff members broke quarantine, escaping by jumping out windows and climbing fences. Lacking faith in the government, scores of doctors and nurses resigned during the epidemic, including 160 in a single week. Despite efforts by Taiwan authorities to contain SARS through strong measures, the government encountered numerous incidents of disobedience and resistance.21
With over 130,000 Taiwanese under home quarantine during the SARS epidemic, quarantine enforcement proved problematic. For example, after two people suspected of being infected with SARS were found in the Huachang Public Housing Complex, all of the project residents were placed under home quarantine. However, over 200 residents ‘disappeared’ and had to be asked to return home. During the epidemic, hundreds of people violated quarantine orders. In theory, they faced home video surveillance, fines of NT$60,000 – NT$300,000, or up to two years imprisonment. However, of the many violators, only 286 (0.2 percent) were punished.22
Public Support for Government Initiatives
Comparative data on public confidence in government and political parties in Taiwan and China exhibit major differences. According to World Values Survey data, 96.7 percent of Chinese express either a great deal or quite a lot of confidence in government. In Taiwan the equivalent level of confidence is expressed by only 69.7 percent. Eighty six point five percent of Chinese express a great deal or quite a lot of confidence in political parties (CCP), whereas in Taiwan only 35.6 percent express such confidence. These significant differences reflect the greater legitimacy enjoyed by China’s central government leadership and the government’s greater ability to mobilize the population in response to a crisis.23
Due to the relative lack of public confidence in the leadership in Taiwan, government leaders hesitated to act strongly against the SARS outbreak for fear of alienating the voting population. Officials feared that unpopular restrictions on personal movement and economic activity might turn the public against the ruling party. The public, influenced by often sensationalist reports in the mass media, were openly sceptical of government statements and acted to block or simply ignore central government initiatives. For example, despite ongoing central government assurances, when the public in Hsinchu county learned of plans to move SARS patients to their local hospital from hospitals in Taipei, numerous people, led by local government officials, rallied to block the transfer. Similar incidents across the island left Taiwan ‘divided into many small fortresses…’. Notably, though recognizing the benefits to activating civil society organizations to respond to outbreaks, this was not done during SARS.24
Enjoying high public confidence, China’s leadership could mobilize the public. While its ability to recentralize decision making power, rapidly enact rules and regulations including clearly coercive and civil liberties-limiting policies, were central to China’s SARS response, these actions were accompanied by reliance on a traditional communist tool that proved highly effective - the mobilization campaign. The government mobilized the public in general but also a variety of traditional and non-traditional civil society groups.
Traditional civil society organizations played only a limited role in the Chinese SARS response, the key to effective mobilization in China was the Shequ (which replaced the residence committee in 1999) [13]. These are defined as grassroots, self-governing mass organizations in article 11 of China’s constitution. Shequ are appendages of sub-district offices, which in turn are subordinate to district and then municipal governments. Described as non-conventional social service organizations, Shequ both assist in implementing government policies (such as the one child policy) but also intercede on behalf of the public (for example coordinating collective responses to local problems). Paralleling the Shequ are the village committees. These are perhaps best described as a form of quasi-independent organization under the close supervision of the state [14]. Read describes these as “straddler groups” – groups that bridge the divide between state and society. They cannot be viewed as autonomous social organizations in the conventional Western sense, nor should they be dismissed as purely instruments of the state [15]. During the SARS outbreak, they served under the guidance and with the training of local CDCs and hospitals. They took responsibility for monitoring their communities for potential SARS cases and notifying hospitals. Because the committees are constituted of community members, the committees knew most of the people in their locations and were able to keep close tabs on comings and goings. If a person had recently returned from a SARS affected region of the country, this information would soon be obtained by the committee members and passed on to relevant officials [16].
Government Ability to Shape the Tone of the Crisis in the Mass Media
Since the late 1980s Taiwan’s media have become increasingly independent and active. In 2002, during the lead-up to the SARS outbreak in Taiwan, Taiwan ranked 31st in the world in terms of press freedoms among 139 countries included in the Press Freedom Index. By contrast, in mainland China the mass media were tightly controlled by the state. China’s 2002 Press Freedom Index ranking was 138th of 139 countries included. And yet despite these clear disparities, data from the World Values Survey reveals that 62 percent of Chinese express either a great deal or quite a lot of confidence in the press, whereas only 40.9 percent of Taiwanese express similar confidence levels.25
Because the mass media market in Taiwan is extremely competitive, many media outlets depend on sensationalist journalism to capture market share. Drawing on this point, Ku and Wang argue that Taiwan’s media were crucial to creating an atmosphere of mass hysteria about SARS. Rumours and hearsay were repeated throughout the day during the early part of the second stage of the Taiwan outbreak. Panicking frontline health workers demanding to be released from treating SARS patients were given prominent media attention, thereby increasing public panic and demoralization, as well as distrust of state initiatives and reassurances [17].
While in China there was room for some criticism of the state in normal times, during the SARS crisis the state controlled information releases and ensured a unified and reassuring message. At the outset of SARS, the central government clamped down on any reporting, denying the public access to information on developments. This initial approach fomented rumour and panic. However, as the epidemic spread, this approach was replaced by mass media saturation with information about SARS and how to identify symptoms of the disease. Discussion of the SARS epidemic in the media began with public statements by Premier Wen Jiabao calling the situation grave. And in an effort to illustrate their engagement with, and commitment to society’s welfare, Wen Jiabao was joined by President Hu Jintao on a travel and media blitz to rally the country in the fight against SARS, describing the disease as requiring ‘prompt and resolute’ measures. China’s media outlets provided daily statistics on the disease as well as descriptions of government and grassroots containment efforts. While focusing on keeping the public informed about the disease and its prevention, the media also sought to convey the message that the disease was surmountable.26
To this point, China exhibits a clear advantage in pandemic response arising from the authoritarian advantage: it is able to effectively centralize decision making power, and engage and mobilize the public and the media. But as noted, an alternative explanation frequently raised in Taiwan is that Taiwan’s international isolation played a major role in its underperformance with regards to SARS. I turn here to consideration of this argument.
Participation in Inter-governmental Organizations
Then-Taiwan president Chen Shui-bian blamed difficulties in handling SARS on Taiwan’s isolation from the international public health community. In 1972, the People’s Republic of China replaced the Republic of China (on Taiwan) at the WHO. Thereafter, WHO officials ceased all direct interaction with Taiwan. Now described as a province of the PRC, Taiwan was expected to access the WHO only through the PRC government. Since the change in status, Taiwan’s health officials and medical professionals have been excluded from the WHO, its forums and workshops on important issues ranging from diagnosis, monitoring and controlling newly emerging infectious diseases. Thus, Taiwan no longer has access to pandemic surveillance, risk assessment and early warning information that is provided by the Pandemic Influenza Program Intergovernmental Meeting – a WHO service available only to member states. Furthermore, it cannot access WHO virus samples and equipment stockpiles.27
Taiwan officials note that during the SARS outbreak, China blocked cooperation and information sharing between the WHO and Taiwan. Taiwan health professionals seeking information from the WHO were told by the WHO to request it from Beijing, a politically difficult option (Brown 2003; Taiwan MoH). Another option was to obtain data from the WHO website. However, according to Chen Yuan-Tsong – 2003 director of the institute of Bio-Medical Sciences at Academia Sinica – ‘by the time the information is in the public domain, it is probably out of date’ [18].
However, acknowledging the challenges faced by Taiwan, the WHO did organize a visit by USCDC officials who liaised with the island’s government health officials. The USCDC team provided guidance and information on disease control protocols. Thus, information on disease control was transmitted to Taiwan via US intermediaries. Also, eventually the PRC permitted two WHO investigators to visit Taiwan, though they were forbidden to interact with Taiwan government officials. However, despite these visits and the resultant access to information, the challenge lay in how the information, once received, was handled. Unclear lines of control and confusion in the bureaucracy resulted in the Taiwan government failing to effectively convey information down the bureaucratic lines of control. As a result, doctors and hospital administrators claimed that the majority of SARS-related information they received derived not from the USCDC or WHO as conveyed via the Taiwan government, but rather directly from the WHO website.
Thus, while direct WHO-Taiwan government interaction would have been beneficial, the necessary prevention and control information was available to the Taiwan government either directly from the WHO or indirectly through the USCDC. The failure lay in the government’s inability to effectively convey the information received to those most needing it.
Contrasting the Taiwan situation, the WHO has extensive permanent representation in China. During the initial phase of the outbreak Chinese officials were reluctant to cooperate with the WHO. However as the SARS outbreak spread and Chinese leaders concluded that China could not alone resolve the crisis, China began collaborating with WHO officials. Collaboration included WHO experts working closely with MoH and CDC officials. For example, joint WHO-MoH teams visited hospitals where SARS cases were treated. WHO experts also travelled to regions of China where SARS cases appeared and reviewed control measures taken by the Chinese in response to the outbreak.
Discussion
A comparison of public health conditions in China and Taiwan at the outset of SARS illustrates that Taiwan was in a stronger initial position in terms of potential to successfully control SARS. In comparison with China, Taiwan was a wealthy country with a highly educated and healthy population, easily managed borders, and government legitimacy arising from the democratic nature of the political system. In addition, since SARS began in China, Taiwan had time to prepare for its potential spread. China enjoyed none of these advantages. Nonetheless, China ultimately responded more effectively to the SARS outbreak than did Taiwan.
As noted, in evaluating its response to SARS, the Taiwan government attributed its failure to effectively overcome SARS at least in part to exclusion from inter-governmental organizations, specifically the WHO. It is correct that after been expelled Taiwan lost the direct support of the WHO. However, this is an insufficient explanation of relative failure. As seen, Taiwan public health officials conceded that despite some delays in obtaining information on SARS, they ultimately obtained the information required from the USCDC and WHO officials. Furthermore, the WHO website offered a wealth of information, thereby providing Taiwan officials an additional resource. In short, lack of WHO membership does not offer a convincing explanation of Taiwan’s relative failure to control SARS.
The authoritarian advantage argument carries more weight. With the disease spreading across China, the Chinese leadership was able to recentralize decision making power, enforce strict top-down regulations on SARS treatment, control and reporting; mobilize state and non-state actors and the public as a whole; and, control the message deriving from the mass media.
In Taiwan, political considerations constrained similar government actions. Inter-party rivalries limited communication and cooperation among jurisdictions. And even though recognized by epidemiologists as important and effective, fear of inducing a popular backlash at the polls caused the government to hesitate when considering implementation of coercive and unpopular disease control initiatives. The state was unable to control the flow of information to the public, and in important cases the public refused to believe state pronouncements or cooperate with state initiatives.
This analysis points to the benefits of the authoritarian advantage enjoyed by China in pandemic response. The conclusion to draw might therefore be that, in our search for effective pandemic response, we should encourage authoritarianism. However, this is clearly both impractical and unpalatable. Therefore the goal must be to find means to compensate for the authoritarian advantage in democratic systems such as Taiwan’s.
Centralized Decision Making
In China’s experiences of the SARS pandemic, the response was controlled, top-down, and fairly uniform, with the more or less full cooperation of the state bureaucracy and public. In Taiwan on the other hand, there was an unwillingness of local government to subsume power to the federal government, even in emergency situations.
In order to overcome this challenge, Taiwan must focus as much as possible on preparedness and advance planning to avoid power struggles between central and local actors. Government officials, faced with resistance to a hierarchical system, must compensate by emphasizing the need for strong and responsible leadership, particularly at the local level.
Local leaders must clearly understand their roles and responsibilities during a pandemic event. Since most responses will, at least initially, be local, these leaders must develop cooperative relations with local responders well in advance of any outbreak, and determine what will trigger requests for involvement from the central government and the nature of that involvement when it occurs. In order to mount a successful response to any disaster, public health officials will have to cooperate with and support elected leaders, and those leaders will have to support efforts of public health officials.
Public Support
A key to successful pandemic response in China was the ability of the state to effectively mobilize a variety of actors. In contrast, low levels of trust among the Taiwan public for the government make a similar government mobilization much more challenging.
While confidence in government organisations may be low in Taiwan, there is relatively high confidence in social organisations. Faith-based community and national organisations such as Tzu Chi Buddhist foundation, the Church and other places of worship often count disaster response as part of their missions. In fact, as of 2005, Taiwan had approximately 120 health related civil society organisations. These groups should be engaged by the state, trained and prepared to become involved in service provision and support during any future pandemic.
The Mass Media
In China, a unified message, clearly sent via all media outlets, proved a powerful tool in counteracting potential chaos and managing the pandemic response. This important tool cannot be similarly controlled by the Taiwan government, nor is this likely to change. An alternative approach to disseminating necessary emergency information might be creation of a dedicated media outlet devoted solely to reporting during emergencies. The emergency outlet could communicate through television, radio and other web-based mediums. It would be activated solely when a predetermined disaster threshold has been reached (such as a declared level 4 pandemic). In order to ensure a focused message, information might draw on WHO reports which could be regularly updated.
An important element in building trust and confidence in the emergency outlet is appointing a trusted apolitical spokesperson who would serve as the point person for all messaging. This spokesperson would avoid speculative statements, relying instead on the best evidence-based information available, and would emphasize that responding to disasters is an ongoing process requiring flexibility. The spokesperson would also have to make clear that contradictions or changes in recommendations are part of the process of an ongoing pandemic response and do not indicate unreliable information. At the same time, the outlet would make this spokesperson available for interviews and discussion in the standard media. These might be accompanied by the requirement that any editing of actual recommendations or pandemic specific information be cleared with the outlet to insure that information was not taken out of context.
In order for such an outlet to be successful, it will have to be proactive in its reporting, rather than reactive. The focus should be on creating the headlines in the form of statements based on verifiable facts and scientific evidence, rather than on responding to sensationalism reported in other media outlets, or serving as a simple government mouthpiece.
Conclusion
The seemingly obvious conclusion to draw from this analysis is that effective pandemic response depends on coercive government actions that would be deeply unpopular and distasteful and therefore difficult to implement in a democratic society. However, the problems associated with taking strong, centralized and coercive actions does not necessarily doom democratic regimes to failure in the face of infectious disease outbreaks (or other crisis situations). Rather the priority must be to ensure that the state, when faced with a potential crisis situation, has developed options that compensate for the authoritarian advantage.
The state must educate the public about the advantages in crisis situations of a centralized decision making process with clear bureaucratic lines of control that facilitate smooth and rapid decision making, coupled with public cooperation. As part of this education, the state must enhance public trust by developing mechanisms to increase government transparency and interaction with the public. Much of the information sharing and nurturing of public trust can be achieved through providing the media with greater access to the leadership, coupled with a concerted effort by the state to reach out to the public.
While this approach may seem cumbersome, requiring tremendous long term investment by the state, given the importance of effectively delineating power, engaging the public and working with the mass media, it is essential that governments early on engage their populations in a dialogue over how to achieve these goals within a democratic system. As the likelihood of a future global pandemic increases, so too does the importance of engaging in this dialogue.
Acknowledgments
I would like to thank the EAI Fellows Program on Peace, Governance and Development in East Asia supported by the Henry Luce Foundation of New York, the East Asia Foundation of Seoul, and the Chiang Ching-Kuo Foundation for International Scholarly Exchange of Taipei for their generous support in providing resources for travel and research.
Jonathan Schwartz
Associate Professor of Political Science at the State University of New York at New Paltz, writes on policy enforcement in China. Recent publications include, with Rachel Schwartz, “Confronting Global Pandemics: Lessons from China and the United States,” Global Health Governance (2010), and “Pandemic Responses in the Asia-Pacific: Risk and Opportunity in PRC’s International Relations,” in Guoguang Wu (ed.) China’s Challenges to Human Security: Foreign Relations and Global Implications (London: Routledge, forthcoming 2012). His most recently edited volume with Shawn Shieh is State and Society Responses to Social Welfare Needs in China: Serving the People (Routledge, paperback 2010).
Footnotes
This methodological approach is discussed in greater detail in Homer-Dixon [4], Dessler [5]. Also, Mill [6].
‘Consensus document on the epidemiology of SARS’, WHO: Department of Communicable Disease Surveillance and Response (16–17 May 2003); “Severe Acute Respiratory Syndrome – Taiwan, 2003,” Morbidity and Mortality Weekly Report,52(20) 23 May, 2003.
Limited local transmission meaning there was no evidence of international spread from the area since 15 March 2003 and no transmission other than close person-to-person contact.
Community transmission as opposed to secondary transmission to family or health care worker contacts. “Super spreader” is defined as a highly infectious person who spreads the agent of an infectious disease to many other people. In Taiwan there were a total of four super spreaders identified. http://www.medterms.com/script/main/art.asp?articlekey=22951 <accessed 9 February 2007 > .
MMWR 2003.
WHO 2003.
For an equivalent study of the Chinese public health system see Schwartz et al. [8].
According to Rothstein et al., 5.4 percent of Taiwan’s GDP was invested in health care. Taiwan enjoyed among the highest life expectancies in Asia. Quarantine and Isolation: Lessons Learned from SARS. http://www.louisville.edu/bioethics/pulic-health/sars.pdf <accessed 27 June 2007>
As of 2004, there are 23 health bureaus managing 369 health stations and 497 health rooms. Health stations manage the grassroots level of public health and are found in rural and urban townships. Health rooms provide basic medical care and public health services in remote areas. In 1989 the DoH established the National Quarantine Service, a consolidation of seven quarantine stations and two substations. http://www.doh.gov.tw/ufile/doc/taiwan%20public%20health%20report%202004.pdf <accessed 5 August 2007>
Quarantine and Isolation: Lessons Learned from SARS, November 2003. http://www.cdc.gov.tw/ct.asp?xItem=21974&ctNode=2007&mp=5 <accessed 27 March 2009>
These included: ‘Communicable Disease Control Rewarding Guidelines’, ‘Communicable Disease Isolation Hospital Regulations’, ‘Implementation Regulations of the Surveillance and Early Warning System for Communicable Diseases’, ‘The Detailed Implementation of the Law on the Control of Communicable Diseases’, ‘Regulations Governing Quarantine’, and, ‘Provisional Regulations Governing the Prevention and Relief of SARS’. All temporary regulations established during the SARS outbreak expired 31 December 2003 unless permanently amended into law.
MMWR 52 (2003); Rothstein et al., 2003.
Taiwan CDC (2003).
Freedom House, Map of Freedom: 2002, http://www.freedomhouse.org/template.cfm?page=363&year=2002 <accessed 29 March 29, 2011>
Interview, H. Bekedam, WHO Country Representative for China (31 May 2005).
WHO, “Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003,” Global Alert and Response (26 September, 2003). http://www.who.int/csr/sars/country/table2003_09_23/en (accessed 30 August, 2011).
Interview, C. J. Chen, Academia Sinica, former Taiwan Minister of Health (29 May 2009).
Interview, C. J. Chen.
Interview, staff surgeon, Shaanxi Provincial People’s Hospital (Anonymous, 2 June 2005).
D. G. McNeil, ‘SARS Fears Shake Taiwan Medical Staff’, The New York Times, 21 May 2003. Ku and Wang [12].
Interview, C. J. Chen (29 May 2009).
World Values Survey. http://www.wvsevsdb.com (accessed 31 August 2011).
Ku and Wang (2004); Interview, S. Hsu, Academia Sinica (1 June 2009).
Reporters without Borders, Press Freedom Index: 2002. http://en.rsf.org/spip.php?page=classement&id_rubrique=297 (accessed 29 March 2011).
Y. Ruan, ‘Can China’s Public Health System Cope with SARS?’, Zhong Guo Xinwen She, 8 June 2003.
Interviews, Hsu; S. Lin, executive director of the Foundation of Medical Professionals Alliance (27 May 2009); C. Shih, Deputy Director, 1st division, Taiwan CDC (1 June 2009).
References
- 1.Leonard, H., and A. Howitt. 2007. Against desperate peril: High performance in emergency preparation and response. In Communicable crises: Prevention, management and resolution in an era of globalization, ed. D. E. Gibbons, 1–26. Information Age.
- 2.E. Lagadec. 2007. A survey of unconventional crises. In Unconventional crises, unconventional responses, ed. E. Lagadec, 5–20. Centre for Transatlantic Relations.
- 3.Boin, A. et al. 2007. The politics of crisis management: Public leadership under pressure. Cambridge.
- 4.Homer-Dixon T. Strategies for studying causation in complex ecological-political systems. The Journal of Environment & Development. 1996;5:132–148. doi: 10.1177/107049659600500202. [DOI] [Google Scholar]
- 5.Dessler, David. 1992. “The Architecture of Causal Analysis,” unpublished manuscript prepared for the Seminar for Philosophy and Methodology of the Social Sciences, Centre for International Affairs, Harvard University, April 1992, p. 8.
- 6.Mill JS. A system of logic. London: Longmans, Green and Co; 1930. p. 360. [Google Scholar]
- 7.Bradsher, K. 2003. ‘As SARS ebbs, WHO lifts its advisory on Taiwan’, The New York Times (18 June 2003).
- 8.Schwartz J, Evans RG, Greenberg S. Evolution of health provision in Pre-SARS China: The changing nature of disease prevention. The China Review. 2007;7(1):81–104. [Google Scholar]
- 9.Teng, S. 2003. ‘Rebuilding the Missing Link – Toward the Rebirth of Taiwan’s Public Health System’, Sinorama, August 2003, pp. 72–79. http://www.sinorama.com.tw/en.
- 10.Kaydos-Daniels SC, et al. Body temperature monitoring and SARS fever hotline, Taiwan. Emerging Infectious Diseases. 2004;10(2):373. doi: 10.3201/eid1002.030748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang, Hung-chi, Cheng-hua Wang, and Pi-ching Chen. “Health care efficiency in Taiwan – compare with OECD countries,” paper presented at the 6th AIMS International Conference on Management (28–30 December, 2008). (accessed 17 March 2009).
- 12.Ku AS, Wang H. The making and unmaking of civic solidarity: Comparing coping responses of civil societies in Hong Kong and Taiwan during the SARS crisis. Asian Perspective. 2004;28(1):124. [Google Scholar]
- 13.Derleth J, Koldyk D. The Shequ experiment: Grassroots political reform in urban China. Journal of Contemporary China. 2004;13:747–777. doi: 10.1080/1067056042000281473. [DOI] [Google Scholar]
- 14.O’Brien KJ. Villagers, elections and citizenship in contemporary China. Modern China. 2001;27:416. [Google Scholar]
- 15.Read BL, Pekkanen R, editors. Local organizations and urban governance in East and Southeast Asia: Straddling state and society. Abingdon: Routledge; 2009. [Google Scholar]
- 16.Schwartz, J., and R. G. Evans. 2007. Causes of effective policy implementation: China’s Public Health Response to SARS. Journal of Contemporary China 16(51).
- 17.Ku AS, Wang H- The making and unmaking of civic solidarity: Comparing the coping responses of civil societies in Hong Kong and Taiwan during the SARS crisis. Asian Perspective. 2004;28(1):135. [Google Scholar]
- 18.Cyranoski, D. 2003. ‘Taiwan Left Isolated in Fight Against SARS’. Nature 422(6933). [DOI] [PMC free article] [PubMed]


