Abstract
Dipeptidyl peptidase 4 (DPP4) is a receptor for MERS-CoV. The soluble form of DPP4 (sDPP4) circulates systematically and can competitively inhibit MERS-CoV entry into host cells. Here, we measured the concentration of sDPP4 in the plasma and sputa of 14 MERS-CoV-infected patients of various degrees of disease severity. The concentration of sDPP4 in the plasma of MERS patients (474.76 ± 108.06 ng/ml) was significantly lower than those of healthy controls (703.42 ± 169.96 ng/ml), but there were no significant differences among the patient groups. Interestingly, plasma levels of IL-10 and EGF were negatively and positively correlated with sDPP4 concentrations, respectively. The sDPP4 levels in sputa were less than 300 ng/ml. Viral infection was inhibited by 50% in the presence of more than 8000 ng/ml of sDPP4. Therefore, sDPP4 levels in the plasma of MERS patients are significantly reduced below the threshold needed to exert an antiviral effect against MERS-CoV infection.
Keywords: Middle East respiratory syndrome coronavirus (MERS-CoV), Dipeptidyl peptidase 4 (DPP4), Soluble DPP4, Antiviral therapy
Highlights
-
•
sDPP4, a soluble form of MERS-CoV receptor, in plasma is reduced in MERS patients.
-
•
IL-10 and EGF in plasma are negatively and positively correlated with sDPP4.
-
•
sDPP4 levels of MERS patients are not sufficient to exert an antiviral effect.
1. Introduction
Middle East respiratory syndrome coronavirus (MERS-CoV), an emerging zoonotic pathogen, causes severe respiratory disease with a mortality rate of approximately 35%. Since its first isolation in 2012, a total of 2080 MERS cases were confirmed and 722 related deaths were reported by September 2017 in 27 countries (de Wit et al., 2016, Organization, 2017). The largest outbreak of MERS outside of the Arabian Peninsula occurred in the Republic of Korea in 2015, resulting in 186 confirmed cases with 39 deaths (Kim et al., 2017). Despite of the high mortality, proper antiviral therapy has not been established yet (Min et al., 2016).
Dipeptidyl peptidase 4 (DPP4) was identified as a functional receptor for MERS-CoV through its interaction with the spike protein (Raj et al., 2013). Notably, DPP4 is cleaved from the membrane and released into circulation as a soluble form (sDPP4), although the physiological roles of sDPP4 are poorly understood. The sDPP4 level in plasma varies depending on pathophysiological conditions such as the presence of metabolic disease or inflammation (Lambeir et al., 2003, Rohrborn et al., 2015). sDPP4 level and enzyme activity are also affected by viral infections including hepatitis C virus and Epstein-Barr virus (Andrieu et al., 2003). Since sDPP4 is capable of interfering with MERS-CoV infection by competitively interacting with the viral spike protein (Raj et al., 2013), we sought to evaluate sDPP4 levels in the body fluids of MERS patients.
2. Materials and methods
2.1. Clinical specimens and ethics statement
Clinical specimens of 14 MERS patients were collected during hospitalization in Chungnam National University Hospital as described in a previous study (Min et al., 2016). This study was performed following the approval of the Institutional Review Boards in Chungnam National University Hospital and Seoul National University Hospital (IRB number: CNUH 2015-07-021 and C-1509-103-705). All surviving patients and healthy volunteers provided written, informed consent to participate. In fatal cases, we obtained an exemption of patients’ consent from the institutional review boards for the retrospective analysis of clinical samples. The information of the clinical and immunological responses of the MERS patients as denoted by the same identifiers are available in our previous report (Min et al., 2016). Basic information on the patients and their clinical specimens are also summarized in Supplementary Table 1.
2.2. ELISA
Expectorated sputa samples were processed to analyze sDPP4 levels as previously described (Willis et al., 2013). In brief, sputum was diluted with phosphate-buffered saline (PBS), and mechanically disrupted using 18-gauge needle and centrifuged to separate the cellular materials. Plasma and sputum samples were diluted in PBS and sDPP4 was measured using the human DPP4/CD26 Quantikine ELISA kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer's instructions.
2.3. Viral infection assay
Spike-pseudotyped lentivirus were prepared as described in a previous study (Kim et al., 2016). Pseudoviruses were pre-incubated with serially diluted sDPP4 (R&D Systems, Minneapolis, MN, USA) at 4 °C for 1 h. Subsequently, 293T (ATCC, Manassas, VA, USA) cells expressing human CD26 (293T-CD26) were infected and further incubated for 48 h as previously described (Kim et al., 2016). Virus entry was quantified by a luciferase assay using the Luciferase assay kit (Promega, Madison, WI, USA) according to the manufacturer's instructions. For the plaque-forming assays, MERS-CoV (0.004 m.o.i. in 24 well), provided by the Korean Centers for Disease Control (Yang et al., 2015), was pre-incubated with sDPP4 and then added to Vero cell culture. After 1 h of incubation, cells were overlaid with a medium containing 1% Seaplaque agarose (Lonza, Basel, Switzerland). At 48 h after MERS-CoV infection, cells were fixed and stained with anti-MERS CoV N protein antibody (Sino Biological Inc., Beijing, China) to count the viral plaques.
3. Results
During the 2015 Korean outbreak, we collected blood and respiratory secretion samples from 14 MERS patients with a wide range of clinical severity, from mild febrile illness to fatal pneumonia (Min et al., 2016). The patients were classified into four groups based on disease severity as previously described (Min et al., 2016). Briefly, Group I (n = 2) included patients with mild febrile illness who recovered without any treatment. Group II (n = 3) comprised of patients who developed mild pneumonia without hypoxemia. Group III (n = 4) and Group IV (n = 5) included infectious cases that resulted in severe pneumonia or were fatal, respectively. Detailed clinical characteristics and immunological responses were previously described (Min et al., 2016).
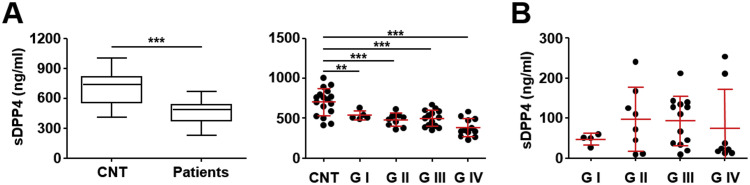
We measured the concentration of sDPP4 proteins in plasma and sputa from the patients and healthy controls by ELISA. The sDPP4 level in the plasma of MERS patients (474.76 ± 108.06 ng/ml) was significantly lower than those of healthy controls (703.42 ± 169.96 ng/ml) ( Fig. 1A, left panel). The levels of sDPP4 were relatively variable and not significantly associated with age or gender in normal controls (Supplementary Table 1). To our knowledge, this is the first report demonstrating a decrease in the sDPP4 protein level in patients experiencing acute viral infection. All the MERS patient groups displayed a statistically significant decrease of plasma sDPP4 levels compared with healthy controls (Fig. 1A, right panel). Although samples from Group IV fatal cases showed the lowest value (360.50 ± 111.93 ng/ml), there was no statistically significant difference among the patient groups. sDPP4 levels in sputa samples (83.53 ± 72.57 ng/ml) were much lower compared with plasma samples, and there was no significant difference among the patient groups (Fig. 1B). The kinetic changes of sDPP4 levels in plasma and sputa showed personal variation without notable trends during the acute phase of infection (Supplementary Table 1). We could not found any correlation between sDPP4 level and disease severity.
Fig. 1.
Quantitation of soluble dipeptidyl peptidase (sDPP4) in clinical samples from 14 Middle East respiratory syndrome (MERS) patients. The concentration of sDPP4 was measured in the plasma (A, total n = 43) and sputa (B, total n = 33) collected at multiple time points from MERS patients in groups (G I–G IV) classified according to disease severity and mortality. Plasma samples from 17 healthy donors (CNT) served as a control for the comparison. The number and collection time of plasma and sputa samples from each group of patients are summarized in Supplementary Table 1. Every experiment was performed in duplicate and p values were calculated by student t-test or one-way analysis of variance. **p < 0.01, ***p < 0.001.
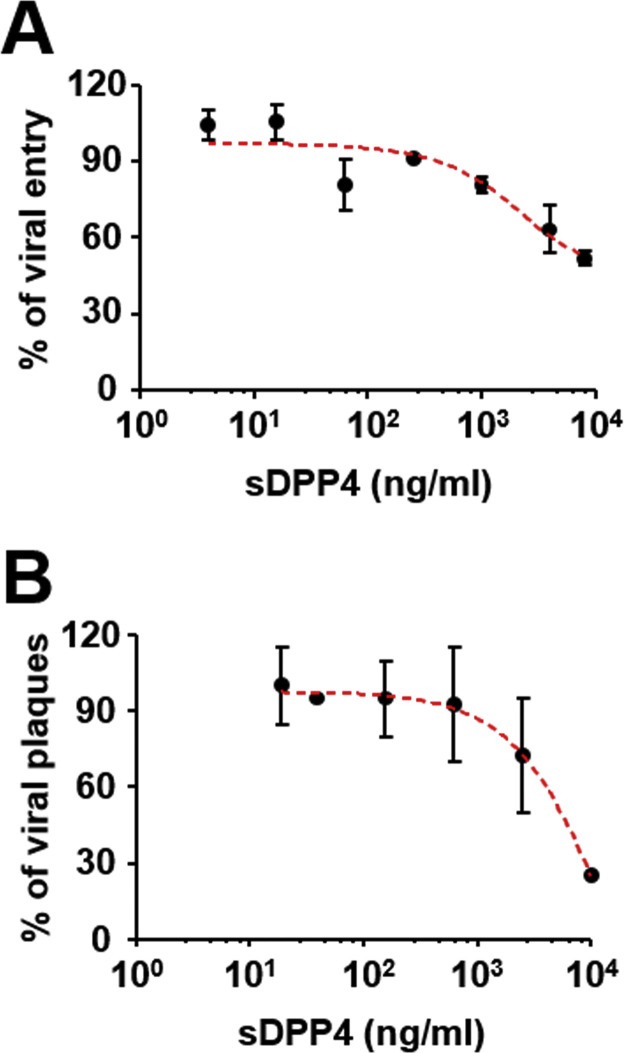
Given that sDPP4 is capable of suppressing MERS-CoV infection by acting as a decoy receptor, we assessed the ability of sDPP4 to suppress the entry of MERS-CoV. The percent inhibition of viral entry by 250 and 1000 ng/ml of sDPP4 was approximately 14% and 24%, respectively ( Fig. 2A). A concentration higher than 8000 ng/ml of sDPP4 is required to achieve 50% inhibition of pseudotyped lentivirus infection, indicating that physiological levels of plasma sDPP4 observed in MERS patients may not be sufficient to resist MERS-CoV entry. Consistently, sDPP4 within the physiological range failed to induce a significant reduction of viral plaques in a plaque-forming assay using MERS-CoV (Fig. 2B).
Fig. 2.
Effects of soluble dipeptidyl peptidase (sDPP4) on Middle East respiratory syndrome (MERS-CoV) infection. (A) The effect of sDPP4 on MERS-CoV entry was determined using a pseudotyped-lentivirus containing MERS-CoV Spike protein and a luciferase reporter system. (B) The effect of sDPP4 on plaque formation by MERS-CoV was determined using a plaque-forming assay. Relative values compared with untreated samples are presented. Error bars represent standard deviations.
4. Discussion
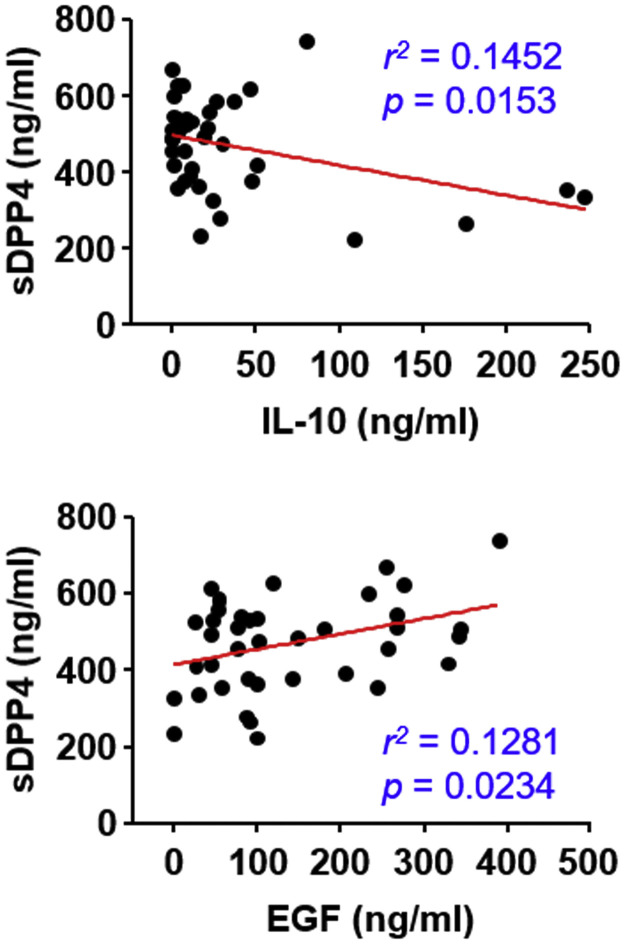
Previous studies suggested that inflammation tends to increase sDPP4 levels (Wronkowitz et al., 2014) and altered DPP4 activities or concentrations in serum have been associated with various pathologic conditions (Klemann et al., 2016). Chronic infection of hepatitis C and E viruses significantly increase sDPP4 activity and protein levels in patients’ sera (Andrieu et al., 2003, Rafiei et al., 2016). sDPP4 is also elevated in bronchoalveolar lavage fluids from patients with pulmonary pathologic conditions, but these levels are regulated independent of serum levels (Juillerat-Jeanneret et al., 1997). Recently, it has been shown that DPP4 expression in pulmonary tissues of smokers and patients with chronic respiratory diseases is upregulated, which could partially explain why these individuals are more susceptible to MERS-CoV infection (Meyerholz et al., 2016, Seys et al., 2018). We observed that sDPP4 is released into respiratory secretions of MERS patients to varying degrees. Although we did not show whether the levels of sDPP4 in respiratory secretions are upregulated, we can suppose that lung inflammation induced by MERS-CoV infection may upregulate sDPP4 secretion as reported in other pulmonary diseases (Juillerat-Jeanneret et al., 1997). However, it is interesting to note that the levels of sDPP4 in the plasma of MERS patients were significantly lower than those of normal volunteers. Downregulation of circulating sDDP4 in sera has also been reported in various inflammatory diseases such as rheumatoid arthritis, sepsis, and several cancers (Klemann et al., 2016). Even though the control and source of systemic DPP4 shedding is poorly understood, several organs including the spleen, lung, liver, kidney, and some immune cells with high DPP4 activity might be putative targets for regulating systemic sDPP4 levels in plasma (Mulvihill and Drucker, 2014). Since a large number of studies clearly demonstrate that DPP4 also plays an integral role in the immune system (Klemann et al., 2016), it would be interesting to determine how MERS-CoV infection regulates the expression and secretion of sDPP4, and the specific role of reduced sDPP4 in anti-viral immunity or viral pathogenesis. Interestingly, when we assessed various cytokines levels in the same plasma samples in a previous study (Min et al., 2016), only the levels of IL-10 and EGF are significantly negatively and positively correlated with plasma sDPP4 concentration, respectively ( Fig. 3). The functional correlation of sDPP4 with the immune-suppressive cytokine, IL-10, or protective growth factor, EGF, on mucosal epithelium and disease severity needs to be carefully assessed in a future study with a larger sample size. Nevertheless, physiological concentrations of sDPP4 are not sufficient to significantly reduce MERS-CoV infection, suggesting that exogenous sDPP4 may have therapeutic potential in MERS patients. In addition, sDPP4 levels before infection with MERS-CoV might be associated with susceptibility or disease severity since its concentrations are relatively variable among normal individuals (Fig. 1). The physiological roles of sDPP4 on MERS-CoV pathogenesis and viral life cycle also remain to be elucidated.
Fig. 3.
Correlation of IL-10, EGF, and sDPP4 levels in patients’ plasma. The plasma levels of sDPP4 were negatively and positively correlated with IL-10 and EGF levels, respectively. The concentrations of IL-10 and EGF in the same plasma samples (n = 40) were determined in a previous report (Min et al., 2016). Correlations between the levels of cytokines and sDPP4 were assessed by linear regression analysis (red lines), and the r2 and p values are shown.
Acknowledgements
This study was supported by grants of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI15C3034 and HI15C3227).
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.virol.2018.03.015.
Appendix A. Supplementary material
Supplementary material. Supplementary Table 1. Information on the patients and their clinical specimens.
References
- Andrieu T., Thibault V., Malet I., Laporte J., Bauvois B., Agut H., Cahour A. Similar increased serum dipeptidyl peptidase IV activity in chronic hepatitis C and other viral infections. J. Clin. Virol. 2003;27:59–68. doi: 10.1016/s1386-6532(02)00128-2. [DOI] [PubMed] [Google Scholar]
- de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juillerat-Jeanneret L., Aubert J.D., Leuenberger P. Peptidases in human bronchoalveolar lining fluid, macrophages, and epithelial cells: dipeptidyl (amino)peptidase IV, aminopeptidase N, and dipeptidyl (carboxy)peptidase (angiotensin-converting enzyme) J. Lab. Clin. Med. 1997;130:603–614. doi: 10.1016/S0022-2143(97)90110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K.H., Tandi T.E., Choi J.W., Moon J.M., Kim M.S. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. J. Hosp. Infect. 2017;95:207–213. doi: 10.1016/j.jhin.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Cheon S., Min C.K., Sohn K.M., Kang Y.J., Cha Y.J., Kang J.I., Han S.K., Ha N.Y., Kim G., Aigerim A., Shin H.M., Choi M.S., Kim S., Cho H.S., Kim Y.S., Cho N.H. Spread of mutant middle east respiratory syndrome coronavirus with reduced affinity to human CD26 during the South Korean Outbreak. MBio. 2016;7:e00019. doi: 10.1128/mBio.00019-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemann C., Wagner L., Stephan M., von Horsten S. Cut to the chase: a review of CD26/dipeptidyl peptidase-4's (DPP4) entanglement in the immune system. Clin. Exp. Immunol. 2016;185:1–21. doi: 10.1111/cei.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambeir A.M., Durinx C., Scharpe S., De Meester I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit. Rev. Clin. Lab. Sci. 2003;40:209–294. doi: 10.1080/713609354. [DOI] [PubMed] [Google Scholar]
- Meyerholz D.K., Lambertz A.M., McCray P.B., Jr. Dipeptidyl peptidase 4 distribution in the human respiratory tract: implications for the middle east respiratory syndrome. Am. J. Pathol. 2016;186:78–86. doi: 10.1016/j.ajpath.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min C.K., Cheon S., Ha N.Y., Sohn K.M., Kim Y., Aigerim A., Shin H.M., Choi J.Y., Inn K.S., Kim J.H., Moon J.Y., Choi M.S., Cho N.H., Kim Y.S. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci. Rep. 2016;6:25359. doi: 10.1038/srep25359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvihill E.E., Drucker D.J. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr. Rev. 2014;35:992–1019. doi: 10.1210/er.2014-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W.H., 2017. World Health Organization.
- Rafiei A., Ajami A., Mohammad Mirabi A., Saffar M.J., Amjadi O., Haghshenas M.R., Abedian F., Khaje-Enayati P. Serum levels of soluble CD26, a novel prognostic marker for hepatitis E infection. Jundishapur J. Microbiol. 2016;9:e31110. doi: 10.5812/jjm.31110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj V.S., Mou H., Smits S.L., Dekkers D.H.W., Müller M.A., Dijkman R., Muth D., Demmers J.A.A., Zaki A., Fouchier R.A.M., Thiel V., Drosten C., Rottier P.J.M., Osterhaus A.D.M.E., Bosch B.J., Haagmans B.L. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrborn D., Wronkowitz N., Eckel J. DPP4 in diabetes. Front. Immunol. 2015;6:386. doi: 10.3389/fimmu.2015.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seys L.J.M., Widagdo W., Verhamme F.M., Kleinjan A., Janssens W., Joos G.F., Bracke K.R., Haagmans B.L., Brusselle G.G. DPP4, the middle east respiratory syndrome coronavirus receptor, is upregulated in lungs of smokers and chronic obstructive pulmonary disease patients. Clin. Infect. Dis. 2018;66:45–53. doi: 10.1093/cid/cix741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis V.C., Demoruelle M.K., Derber L.A., Chartier-Logan C.J., Parish M.C., Pedraza I.F., Weisman M.H., Norris J.M., Holers V.M., Deane K.D. Sputum autoantibodies in patients With established rheumatoid arthritis and subjects at risk of future clinically apparent disease. Arthritis Rheumatol. 2013;65:2545–2554. doi: 10.1002/art.38066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wronkowitz N., Gorgens S.W., Romacho T., Villalobos L.A., Sanchez-Ferrer C.F., Peiro C., Sell H., Eckel J. Soluble DPP4 induces inflammation and proliferation of human smooth muscle cells via protease-activated receptor 2. Biochim. Biophys. Acta. 2014;1842:1613–1621. doi: 10.1016/j.bbadis.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Yang J.S., Park S., Kim Y.J., Kang H.J., Kim H., Han Y.W., Lee H.S., Kim D.W., Kim A.R., Heo D.R., Kim J.A., Kim S.J., Nam J.G., Jung H.D., Cheong H.M., Kim K., Lee J.S., Kim S.S. Middle east respiratory syndrome in 3 persons, South Korea, 2015. Emerg. Infect. Dis. 2015;21:2084–2087. doi: 10.3201/eid2111.151016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material. Supplementary Table 1. Information on the patients and their clinical specimens.