On March 29, 2003, at approximately 12:23 AM , an 83-year-old woman accompanied by her daughter presented to the ED triage area. The patient's chief complaints were fever, cough, and severe fatigue. She had a history of moderate chronic obstructive pulmonary disease but was otherwise in good health. The patient was normally active, and said that she had just returned from vacation and had started feeling ill 1 day after her return. The triage nurse asked about specific travel history. The patient stated that she and her daughter had been traveling for 2 weeks in China. They stayed at luxury hotels throughout the trip, yet had multiple interactions with the local population as they stopped at various tourist sites.
The patient presented with a productive cough yielding yellow sputum. She had bilateral wheezing, with a pulse oximetry reading 92% on room air. She was warm, flushed, and had an oral temperature of 38.2°C (100.8°F).
The triage nurse asked the patient and the daughter to wear N-95 masks, and then accompanied them to a negative air pressure room. She placed the patient on oxygen at 2 L per nasal cannula and established an intravenous line of 5% dextrose and 0.45% normal saline at 100 mL/h. The patient received 2 Ventolin (Albuterol) aerosol treatments and 400 mg of gatifloxacin (Tequin) intravenously.
The results of the patient's complete blood count and comprehensive metabolic panel were negative. Her white blood cell count (WBC) was 4.2 (normal range: 4.1- 10.6). Results of blood drawn for arterial blood gas analysis were as follows: pH, 7.43; PO 2, 61; PCO 2, 42 on room air. This patient was placed back on oxygen 2 L nasal cannula once the blood gas specimen was obtained. Results from the blood cultures were pending.
Because the triage nurse thought the patient might have severe acute respiratory syndrome (SARS), she notified the infection control on-call nurse. The patient was admitted to ICU with expanded contact and airborne isolation precautions. The isolation precautions extended beyond the normal isolation standards. An N95 mask was used in place of the basic surgical mask. Additionally, gown, gloves, shoe covers, hair cover, and goggles were used. At the time of this case, Centers for Disease Contol and Prevention (CDC) guidelines for a suspected SARS case included personal protection equipment, negative pressure room, and the addition of eye protection. What we now know, from the recommendations of the CDC, is that the employee must also double glove and double gown when caring for suspected cases of SARS.
The hospital infection control specialist alerted public health officials for community follow-up with the daughter. The daughter was monitored for any symptoms of respiratory illness and was placed on house quarantine for 10 days. The admitting pulmonologist performed a bronchoscopy, which showed extensive erythema throughout the airway. Nasopharyngeal and oropharyngeal swabs were collected, sent to the state laboratory, and then were forwarded to the CDC. It turned out that the patient did not have the coronavirus. The CDC makes 2 distinctions in their assessment of cases: “probable” and “suspected.” Our patient was designated “suspected.” Because the patient had continued shortness of breath, she remained in the ICU until March 31, 2003. The remaining 5 days of her hospitalization were spent on the pulmonary unit in strict isolation. On April 5, 2003, she was discharged from the hospital and placed on 10-day isolation at home. Her pulmonologist and other public health practitioners continued frequent contacts with the patient throughout her recovery. After approximately 1 month, her care was transferred to her primary care provider.
With increasing numbers of atypical pneumonia cases, called SARS by the World Health Organization, and several newly reported cases in Canada, the CDC activated its emergency operations center on Friday, March 14, 2003. At that time, there were no reported cases in the United States. The emergency clinical educator and manager at our facility, in collaboration with the hospital infection control specialist, disseminated preliminary information from the CDC and conducted ongoing in-services with the staff. There were posters in the break room and flyers throughout the department that reviewed what experts knew about the disease. Shift charge nurses received a packet of educational materials to use as a review for their staff members.
The differential diagnosis that we considered upon admission of our patient included exacerbation of chronic obstructive pulmonary disease, viral syndrome, reactive airway disease, asthma, pneumonitis, and SARS. In the end, our patient did not have the coronavirus, but had met most of the CDC case definition criteria for SARS. Her temperature was greater than 38°C (100.4°F) orally, she had symptoms of respiratory illness, she had traveled to mainland China, and her pulse oximetry reading was less than 94% on room air. Her initial low WBC count of 4.2 (normal 4.1-10.6) and the low PO 2 were “red flags,” consistent with the diagnosis of SARS. However, throughout her 8-day hospitalization, daily chest radiographs did not show any infiltrates, and the results of her laboratory tests remained unremarkable.
The triage nurse's recall of the SARS information that had been presented during the preceding days led to a quick decision to have the patient and her daughter wear N95 masks. After taking them back to an isolation room, the nurse immediately notified the emergency physician and contacted the on-call infection control nurse. To limit the number of individuals exposed, the triage nurse completed the assessment in the room and collected registration information. The physician and the primary nurse were given report by the triage nurse, and wore masks, plus gowns, gloves, and goggles. Signs placed on the door directed staff and visitors to check with the nurse before entering the room.
This patient received preliminary antibiotics for her acute respiratory infection, pending the confirmation of SARS. The CDC guidelines at the time of this case recommended that patients with symptoms of SARS receive the same treatment that would be used for any patient with a serious community-acquired atypical pneumonia of unknown cause. Although we gave this patient an antibiotic before a diagnosis was confirmed, antibiotics have since been demonstrated to be ineffective against SARS; there is no specific treatment for this viral condition.
Our patient also received an aerosol treatment in the emergency department. At the time she was seen, CDC guidelines were not yet widely implemented. Now we would not administer any aerosol treatment to a potential SARS patient, in light of the danger of transmission.
After this patient left our emergency department, the triage nurse, the only one exposed to the patient and her daughter, was placed on 10-day at-home quarantine, and was required to contact employee health daily by telephone, reporting her temperature and general state of health. She lives alone, so there were no other family members to be exposed. She did not contract any illness from her exposure. Because the triage nurse remembered the in-service on SARS, she had quickly put a mask on the patient and brought that patient to an isolation room. In the end, we lost 1 nurse for 10 days. If she had not acted quickly, there is no telling how many staff we might have had to quarantine.
In response to this patient and increasing numbers of SARS cases throughout the world, the emergency department initiated the use of a SARS screening tool. The hospital infection control specialist developed this tool to screen all patients presenting to the emergency department (Figure 1).
Fig. 1.
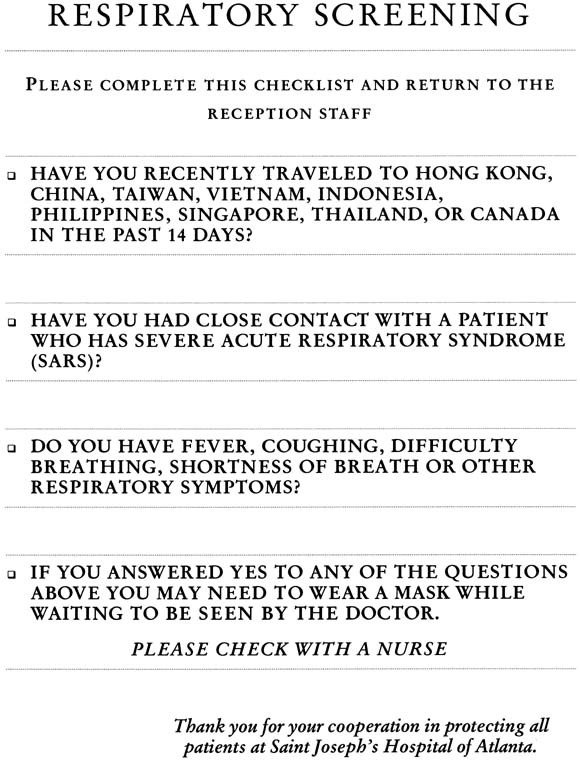
Volunteers attach this bright red screening tool to the top of the patient's chart packet before the patient is triaged. Originally, it was going to be handed to patients while they were waiting to be triaged in, but it was yet another task for triage nurses who were too busy to do it in addition to their other responsibilities. It was intended for all ambulatory patients, but it soon became apparent that patients arriving by ambulance also needed to be screened, and so they have been distributed to the local EMS who we encourage to screen, in the field. Hospital administration has adopted this tool in other areas of the hospital, to capture other patients not coming in through the emergency department.
Basic questions include recent travel history, contact with any person suspected of having SARS, and any fever or respiratory symptoms. Local EMS units were encouraged to perform similar prehospital screenings, place surgical masks on patients before they arrive at the emergency department, and provide SARS screening information during their radio reports. With this information, the charge nurse can then arrange for the patient to be placed directly into an ED isolation room. Educational notices were placed in the EMS reception area, which provided instruction on the initial care and isolation of suspected SARS patients. We provided surgical and N95 masks at points of entry to the emergency department. The ED screening form has been adapted for use with direct admit patients in other parts of the hospital.
Two rooms in our emergency department are negative pressure rooms.
Our facility recently built a new emergency department that opened on January 13, 2003. There was extensive planning that involved design input from the emergency preparedness coordinator, epidemiology department, and the infection control specialist. The structural design included physical requirements for the treatment and isolation of possible victims of bio-terrorism attacks and serious airborne illnesses. As part of that design, 2 rooms in our emergency department are negative pressure rooms.
Our experience with this patient, the first such case in Georgia, has heightened all of our awareness. Although she was not a confirmed case of SARS, our experience provided us with the opportunity to critically assess our process and improve our future practice.
For additional information:
Preliminary Clinical Description of Severe Acute Respiratory Syndrome. 2003 March 27. Available from: www.cdc.gov/mmwr/preview/mmwrhtml/mm5212a5.htm
CDC Advisory/atypical pneumonia. 2003 March 15. Available from: www.cdc.gov/ncidod/hip.
Footnotes
For reprints, write: Cyndi Kalafut, RN, MBA, St Joseph Hospital, 5665 Peachtree Dunwoody Road NE, Atlanta, GA 30342; E-mail: CKalafut@sjha.org.
J Emerg Nurs 2003;29:326-9.


