Abstract
Background: Acute community-acquired sinusitis is considered a bacterial complication of the common cold. Radiologic abnormalities in sinuses occur, however, in most patients with upper respiratory virus infections.
Objective: Assessment of the occurrence, clinical profile, laboratory findings, and outcome of radiologically confirmed sinusitis was carried out as part of a common cold study in young adults.
Methods: Clinical examinations and radiography of the paranasal sinuses were carried out on days 1, 7, and 21 in 197 patients with the common cold. The symptoms were recorded on diary cards on days 1 to 20. Ten viruses and 5 bacteria were studied as etiologic agents of common cold as reported earlier. Serum C reactive protein concentrations, erythrocyte sedimentation rates, and total white blood cell counts with differentials were determined in 40 randomized subjects on day 7. The effect of 6 days of intranasal fluticasone propionate treatment of the common cold in the prevention of sinusitis was analyzed.
Results: On day 7, 39% of patients with the common cold in the placebo group (n = 98) had sinusitis, which we would prefer to call viral sinusitis. The symptoms of patients with sinusitis and those without it were not clinically distinguishable. Viral infection was detected in 81.6% of patients with sinusitis. No significantly increased levels of antibodies to bacteria were detected. Serum C reactive protein concentrations, erythrocyte sedimentation rates, and white blood cell counts were low in patients with sinusitis. All patients made a clinical recovery within 21 days without antibiotic treatment. Fluticasone propionate treatment tended to prevent paranasal sinusitis, especially in rhinovirus-positive subjects.
Conclusion: Viral sinusitis frequently occurs in the early days of the common cold, but it is a self-limited illness. The sinuses should not be imaged in patients with the common cold if the signs and symptoms of illness gradually become less severe and no specific signs suggestive of bacterial sinusitis occur. (J Allergy Clin Immunol 1998;102:403-8.)
Keywords: Sinusitis, paranasal sinusitis, viral sinusitis, common cold, cold, rhinovirus, viral respiratory infection, fluticasone propionate
Abbreviations: CRP:, Serum C reactive protein; ESR:, Erythrocyte sedimentation rate; FP:, Fluticasone propionate; NPA:, Nasopharyngeal aspirate; WBC:, White blood cell count
Acute bacterial sinusitis develops in 0.5% to 2.5% of adult patients after viral upper respiratory tract infection.1 If untreated, acute bacterial sinusitis may become chronic or lead to severe complications. Therefore antibiotics are generally considered necessary for its medical management.2 Bacterial sinusitis is difficult to differentiate from radiologic sinusitis, which is common in many patients during the early stage of the common cold.3 If the signs and symptoms of the common cold last longer than for 7 to 10 days after onset of illness, the diagnosis of bacterial sinusitis should be considered.4
In a study of intranasal fluticasone propionate (FP) in the treatment of the common cold,5 we took paranasal sinus radiographs in 197 young adults on days 1, 7, and 21 of common cold, and the patients were followed daily for 21 days after onset of illness. The occurrence, clinical profile, laboratory findings, and outcome of radiologically confirmed sinusitis were assessed. Furthermore, it was investigated whether FP treatment prevented the development of sinusitis.
METHODS
Study subjects
Two hundred young adults were enrolled in the study. The study period was November 1994 to November 1995, excluding the summer months (June, July, and August of 1995). The subjects were recruited through advertisements in local newspapers, through posters in student canteens, and through contact persons. All subjects were white. The mean age (± SD) of the male subjects (n = 59) was 24.0 years (± 2.7 years), and that of the female subjects (n = 141) was 24.1 years (± 3.6 years). Patients contacted the study office within 24 to 48 hours after onset of symptoms they considered as the common cold on the basis of their earlier experiences. The day of recruitment to the study was day 1. The entry criterion was that the subject had to be healthy and without antibiotics for 4 weeks before study entry. The exclusion criteria were a history of allergic rhinitis, a history of chronic or recurrent sinusitis and lower respiratory tract disease, major nasal septal deviation, nasal polyposis, pregnancy, or lactation. All subjects signed a written consent form, and the study was approved by the Ethics Committee of the Turku University Hospital, Turku, Finland.
Study design
The study office was located at the Department of Pediatrics, Turku University Hospital. The subjects had to have at least nasal drainage and 1 of the following symptoms: cough, headache, sore throat, hoarseness, myalgia, or oral temperature higher than 37°C. Subjects with only a sore throat were excluded, because they were considered to have pharyngitis or tonsillitis. Clinical examinations were carried out on day 1 (visit 1), day 7 (visit 2), and day 21 (visit 3) by the study physician. In subjects with fever or pain, acetaminophen therapy was permitted. Drugs affecting nasal or lung function (ie, sympathomimetics, anticholinergics, steroids, or nonsteroidal antiinflammatory drugs), including over-the-counter medication, were not allowed during the study. If a subject had an unexpected exacerbation of symptoms of the common cold, an additional visit was arranged.
Radiography of paranasal sinuses
Plain radiography of the paranasal sinuses (occipitomental view) was carried out on days 1, 7, and 21 of the common cold. Of the 200 subjects included in the study, 1 was rejected because of poor compliance, and the radiographs of 2 patients were lost before interpretation. The 591 radiographs obtained were interpreted after the study period independently by 3 radiologists who were unaware of clinical patient data. The 3 radiologists agreed on the interpretation of radiographs in 60.9% of the 1182 maxillary sinuses imaged. In 35.5% of the cases, 2 of the 3 radiologists agreed, and this was chosen for the final diagnosis. In 3.6% of the cases, there was a disagreement between all 3 radiologists, and the final diagnosis was established through discussion. The findings of the maxillary sinuses were categorized as normal (1), mucosal thickening of 5 mm or less (2), mucosal thickening of more than 5 mm (3), total opacity (4), air-fluid level (5), and cyst or polyp (6). Subjects with maxillary sinus radiographs showing mucosal thickening of more than 5 mm, total opacity, or air-fluid level were classified as having sinusitis.6 Because a single occipitomental view images poorly areas other than the maxillary sinuses, the results for the frontal, ethmoid, and sphenoid sinuses were combined and designated as either normal or showing an infection of the frontal, ethmoid, or sphenoid sinus.
Assessment of illness
The subjects recorded their symptoms on a diary card for 20 days. The severity of symptoms was assessed on a 4-point scale (0 = absent, 1 = mild, 2 = moderate, and 3 = severe). The symptoms recorded were watery rhinitis, purulent rhinitis, nasal congestion, nasal irritation, headache, cough, sputum, sore throat, and fever. The subjects were also asked to record any other possible symptoms, such as pain in the upper teeth or in the maxillo-facial area.3, 7, 8 On days 1 to 6, symptoms were recorded both in the morning and in the evening, and on days 7 to 20 they were recorded in the evening only.
Microbiologic studies
The details of the microbiologic methods and results have been published separately.9 The etiologic role of 10 viruses (rhinovirus; adenovirus; coronavirus; enterovirus; influenza A and B viruses; parainfluenza virus types 1, 2 and 3; and respiratory syncytial virus) was investigated by virus culture, antigen detection, serology, and rhinovirus PCR. Antibodies to 5 bacteria (Chlamydia pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Mycoplasma pneumoniae, and Streptococcus pneumoniae) were studied. Nasopharyngeal aspirate (NPA) was taken with a disposable mucus extractor (Vygon, Ecouen, France). The catheter was advanced to a depth of 6 to 10 cm in the nasopharynx through the nostril and withdrawn while applying gentle suction with a suction device. This procedure was carried out through both nostrils and repeated 2 to 3 times. NPA was inoculated on blood and chocolate agar plates according to routine procedures for detection of bacteria present in the nasopharynx on days 1 and 7.
Study medication
The effect of high-dose intranasal FP in the prevention of sinusitis was studied. The subjects were randomly assigned to receive either FP or placebo for 6 days beginning on day 1. The daily dose was 800 μg (2 puffs per nostril 4 times daily at equal intervals during waking hours). We wanted to maximize the effect of FP by using a 4-fold dose compared with the recommended dosage in allergic rhinitis (200 μg/day). The medication was administered with a metered-pump bottle designed to deliver a total dose of 50 μg. The placebo was identical to the study drug without FP, containing benzalkonium chloride, phenylethyl alcohol, dextrose, microcrystalline cellulose and carboxymethyl cellulose sodium, polysorbate 80, and purified water. Both the study drug and the placebo were supplied by Glaxo Research and Development Limited (Uxbridge, Middlesex, UK). After the treatment, the medication sprayers were collected, and the use of medication was determined by measuring any remaining medication.
Hematology
Venous blood was obtained from 40 randomized subjects in the placebo group on day 7 for determining the concentration of serum C reactive protein (CRP, nephelometric method), erythrocyte sedimentation rate (ESR), and total white blood cell count (WBC) with differential.
Data analysis
Data for these analyses were obtained from the placebo group only, with the exception of the results of sinusitis prevention with intranasal FP. The mean severity scores of symptoms were calculated for days 1 to 6 separately. The mean severity scores during days 1 to 6 were obtained by summing the severity scores and dividing the sum by the number of days. Student’s t test was used to compare the mean severity scores, mean duration of symptoms, and mean hematologic values between the 2 groups. If the distribution of means was not normal, the Wilcoxon test was used instead. The frequency of categorical variables between the groups on a single day was compared by using the Pearson chi-square test or Fisher’s exact test, if the number of expected observations was 5 or less in at least 1 cell.
RESULTS
Development of sinusitis
In the placebo group 294 radiographs of 98 subjects were interpreted. The radiographs of 14.2% of the subjects showed sinusitis on day 1, 38.8% showed sinusitis on day 7, and 11.3% showed sinusitis on day 21 (Table I).In the 50 rhinovirus-positive subjects the corresponding rates were 14.0%, 42.0%, and 8.0%. Among the 38 subjects with sinusitis on day 7, 71.1% had mucosal thickening of more than 5 mm, 23.7% had air-fluid level, and 5.3% had total opacity (Table I). In the rhinovirus-positive subjects these frequencies were similar (data not shown). On day 1, 14 patients had sinusitis, 12 had it on day 7, and 5 had it on day 21. Of the 84 patients who did not have sinusitis initially, 26 had it on day 7 (P = .0001) and 6 on day 21 (P = .002). Altogether 57% of the patients had sinus abnormalities (mucosal thickening, total opacity, air-fluid level, or cyst or polyp) during the 21 days of the common cold.
Table I.
Radiographic findings (occipitomental view) of paranasal sinuses of patients during common cold(n = 98)
| Days of common cold | |||
|---|---|---|---|
| Day 1 | Day 7 | Day 21 | |
| Paranasal sinusitis (%) | 14.2 | 38.8 | 11.3 |
| Maxillary sinusitis (%) | 14.2 | 38.8 | 11.3 |
| Mucosal thickening over 5 mm (%) | 50.0 | 71.1 | 72.7 |
| Air-fluid level (%) | 35.7 | 23.7 | 27.3 |
| Total opacity (%) | 14.3 | 5.3 | 0 |
| Ethmoid, frontal or sphenoid sinusitis (%) | 3.1 | 1.0 | 1.0 |
| Mucosal thickening (≤5 mm) (%) | 20.4 | 11.2 | 4.1 |
| Cyst or polyp (%) | 5.1 | 3.1 | 7.1 |
| Normal (%) | 60.2 | 46.9 | 77.6 |
Symptoms
Purulent rhinitis was more common during days 1 to 6 in subjects with sinusitis on day 7 compared with subjects without sinusitis (94.7% vs 76.7%, P = .02) (Table II).A similar tendency was found in rhinovirus-positive subjects (100.0% vs 72.4%, respectively, P = .02). In the rhinovirus-positive group headache also tended to be more common in subjects with sinusitis on day 7 (85.7% vs 65.5%, P = .11). No other differences occurred in the frequency of symptoms during days 1 to 6 between patients with sinusitis and those without sinusitis. No subjects recorded unilateral pain in the maxillo-facial area or pain in the upper teeth, which are considered as specific symptoms of bacterial sinusitis.3, 7, 8
During days 1 to 6, the mean severity score of purulent rhinitis was higher in subjects with sinusitis than in those without sinusitis (1.1 vs 0.8, P = .05) (Table III).
Table III.
Mean severity scores of symptoms in patients with sinusitis and those without sinusitis on day 7 of common cold*
| Mean severity scores during days 1-6 | |||
|---|---|---|---|
| Sinusitis (n= 38) | No sinusitis (n= 60) | Pvalue | |
| Watery rhinitis | 1.1 | 1.0 | .20 |
| Purulent rhinitis | 1.1 | 0.8 | .05 |
| Nasal congestion | 1.5 | 1.3 | .09 |
| Cough | 1.0 | 1.0 | .77 |
| Sore throat | 0.6 | 0.5 | .42 |
| Headache | 0.4 | 0.4 | .94 |
| Fever | 0.2 | 0.2 | .36 |
| *The mean severity scores during days 1 to 6 were obtained by summing the severity scores and dividing the sum by the number of days. Radiologically established sinusitis was defined as mucosal thickening over 5 mm, total opacity, or air-fluid level. | |||
A similar tendency was seen in rhinovirus-positive subjects (1.3 vs 0.8, respectively, P = .04). The severity of nasal congestion was also higher in subjects with sinusitis in the rhinovirus-positive group (1.6 vs 1.3, P = .04) during days 1 to 6. On day 7, the mean severity scores of symptoms were on the whole the same between subjects with sinusitis and those without sinusitis (data not shown).
The mean duration of all symptoms was similar in subjects with sinusitis and those without sinusitis on day 7 (Table II). Cough lasted for 9.0 (SD = 6.9) days and purulent rhinitis for 8.4 (SD = 5.6) days in subjects with sinusitis on day 7. In subjects without sinusitis, the numbers were 8.3 (SD = 6.8) and 7.3 (SD = 6.2) days, respectively. In the rhinovirus-positive group cough lasted for 11.2 (SD = 6.3) days, and purulent rhinitis lasted for 9.8 (SD = 5.6) days in subjects with sinusitis.
Table II.
Frequency and mean duration of symptoms in patients with sinusitis and those without sinusitis on day 7 of common cold*
| Frequency of symptoms during days 1-6 (%) | Mean duration (days [SD]) | |||||
|---|---|---|---|---|---|---|
| Sinusitis (n= 38) | No sinusitis (n= 60) | Pvalue | Sinusitisn= 38) | No sinusitis (n= 60) | Pvalue | |
| Watery rhinitis | 100.0 | 98.3 | 1.00 | 9.7 (6.0) | 8.6 (5.3) | .33 |
| Nasal congestion | 100.0 | 98.3 | 1.00 | 11.2 (4.7) | 10.2 (5.0) | .34 |
| Purulent rhinitis | 94.7 | 76.7 | .02 | 8.4 (5.6) | 7.3 (6.2) | .37 |
| Cough | 89.5 | 88.3 | 1.00 | 9.0 (6.9) | 8.3 (6.8) | .62 |
| Sore throat | 81.6 | 90.0 | .23 | 3.6 (3.1) | 3.7 (3.6) | .85 |
| Headache | 76.3 | 71.7 | .61 | 3.7 (3.5) | 3.9 (4.3) | .79 |
| Fever | 55.3 | 55.0 | .98 | 1.3 (1.8) | 1.7 (2.4) | .39 |
| *Radiologically established sinusitis was defined as mucosal thickening over 5 mm, total opacity, or air-fluid level. | ||||||
Microbiologic findings
The etiology of the common cold was determined in 69.5% of subjects. Viral infection was detected in 81.6% of patients with sinusitis (n = 38) and in 63.3% of patients without sinusitis (n = 60) (P = .05). Rhinovirus was the most frequent cause of infection, detected in 55.3% and in 48.3% of subjects, respectively. No significantly increased levels of antibodies to bacteria were detected in the sinusitis group. One patient without sinusitis had antibody conversion to C. pneumoniae. In 23.7% of subjects with sinusitis and in 28.3% of those without sinusitis, a pathogenic bacteria (S. pneumoniae, H. influenzae, or M. catarrhalis) was cultured in NPA on day 1 or on day 7. No differences in the frequency of bacteria between day 1 and day 7 were seen in these groups (data not shown).
Hematologic findings
Subjects with sinusitis on day 7 (n = 16) had a significantly higher mean ESR and mean differential count of neutrophilic granulocytes than subjects without sinusitis (n = 24): ESR, 14.2 mm/h (range, 2 to 26 mm/h) versus 7.4 mm/h (range, 1 to 20 mm/h) (P = .004), respectively; the mean differential count of neutrophilic granulocytes, 64.0% (range, 43% to 76%) versus 55.0% (40% to 76%) (P = .01), respectively. In the sinusitis group the mean WBC was 7.1 × 109/L (range, 5.3 to 10.1 × 109/L), and in subjects without sinusitis it was 6.1 × 109/L (range, 3.2 to 11.6 × 109/L) (P = .06). The median CRP concentration was less than 10 mg/L in both of these groups (range, <10 to 36 mg/L and <10 to 17 mg/L, respectively).
Outcome
All patients with common cold made a clinical recovery within 21 days (Fig 1).
Fig. 1.
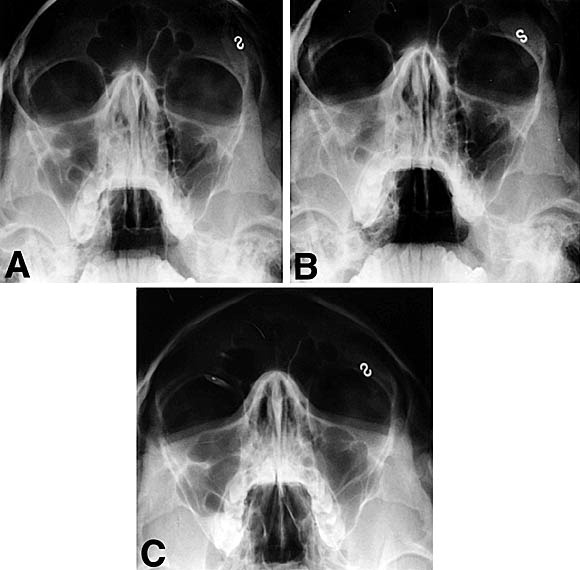
A 23-year-old woman with rhinovirus-induced common cold and normal sinus radiograph on day 1 (A). On day 7 (B), the radiograph shows maxillary sinusitis (mucosal thickening over 5 mm in the right sinus), CRP less than 10 mg/L, ESR of 13 mm/hour, and WBC of 5.3 × 109/L. Symptoms disappeared within 14 days after onset of illness. On day 21 (C), mucosal thickening has resolved, but minor air-fluid level is seen in right maxillary sinus.
No subjects with radiologically established sinusitis were treated with antibiotics during their common cold illness, with the exception of 1 patient with acute otitis media on day 12. Three subjects had an exacerbation of symptoms of common cold during the study, and an additional visit was arranged. Additional radiographs of sinuses of 2 of these subjects were taken and found to be normal. The radiograph of 1 asymptomatic female subject showed frontal sinusitis on day 21 (Fig 2).
Fig. 2.

A 25-year-old woman with common cold. No virus was detected. Symptoms disappeared within 14 days after onset of illness. Air-fluid level was found in right frontal sinus on day 21. Follow-up radiograph was taken after 2 weeks and found to be normal. Subject was asymptomatic, and no treatment was given.
After 2 weeks, a follow-up radiograph was taken, and the frontal sinusitis was found to have resolved. No treatment was given.
Intranasal FP in the prevention of sinusitis
The study was completed by 199 subjects (99.5%) according to the protocol.5 One subject (from the placebo group) was excluded on day 7 because of improper use of study medication. The effects of FP treatment in the prevention of paranasal sinusitis are shown in Table IV.
Table IV.
Intranasal FP in the prevention of paranasal sinusitis associated with common cold*
| FP | Placebo | Pvalue | |
|---|---|---|---|
| Frequency (%) of sinusitis on day 7 | |||
| All subjects (n = 169) | 24.7 | 31.0 | .37 |
| Rhinovirus-positive subjects(n = 92) | 18.4 | 34.9 | .07 |
| Frequency (%) of sinusitis on day 21 | |||
| All subjects (n = 169) | 8.2 | 7.1 | .79 |
| Rhinovirus-positive subjects(n = 92) | 4.1 | 2.3 | 1.00 |
| *Subjects whose radiographs showed sinusitis on day 1 are excluded. Radiologically established sinusitis was defined as mucosal thickening over 5 mm, total opacity, or air-fluid level. | |||
In 104 rhinovirus-positive subjects, FP treatment tended to prevent paranasal sinusitis. The frequency of sinusitis on day 7 was 18.4% in the FP group compared with 34.9% in the placebo group (P = .07). Of the subjects in the FP group with radiographs showing sinusitis on day 7, 55.6% had mucosal thickening of more than 5 mm, 33.3% had air-fluid level, and 11.1% had total opacity. In the placebo group the corresponding rates were 73.3%, 26.7%, and 0%. The differences were not statistically significant.
DISCUSSION
The primary finding of our study was that sinusitis occurs frequently during the early days of the common cold, but it is a self-limited illness. Within 48 hours after the onset of symptoms, 14% of our patients had radiologically diagnosed sinusitis. Whether all these radiologic abnormalities were caused by the current respiratory virus infection is uncertain. On day 7, 39% of the subjects had sinusitis. In the study by Kaiser et al,10 19% of patients with the common cold had radiologically diagnosed sinusitis. In their study patients were excluded if they had symptoms predicting sinusitis (facial pain, maxillary toothache, or tenderness of the maxillary or frontal sinuses). Gwaltney et al11 used computed tomography to find abnormalities in the maxillary sinuses in 87% of their 31 patients during common cold episodes. In our study 57% of patients had sinus abnormalities during 21 days of the common cold, according to the 3 radiographs (Table I). Our patients received intranasal spray treatment (placebo) during the first 6 days of infection, which may have influenced the development of sinus abnormalities.
We suggest that sinusitis during the common cold should be called viral sinusitis for the following reasons. First, a virus infection was detected in 81.6% of the patients with sinusitis. A recent study by Pitkäranta et al12 showed that when a virus is detected in a nasal swab from a patient with acute community-acquired sinusitis, it can also be found in the maxillary sinus sample of 78% of these patients. Second, no patients had significantly increased levels of antibodies to S. pneumoniae, H. influenzae, or M. catarrhalis, which are the most common bacteria causing bacterial sinusitis. Third, our patients with viral sinusitis had low CRP concentrations, ESRs, and WBCs, which are compatible with viral illness. In 2 previous studies, elevated CRP concentrations and ESRs have been shown in acute bacterial sinusitis.3, 13 Fourth, the symptoms of our patients were clearly reduced within 7 to 10 days after onset of the common cold and were not markedly distinguishable from those of the common cold without sinusitis (Table II). Although the mean duration of symptoms of illness was 10 days in our study, with the exception of 3 patients, the symptoms of our patients abated gradually, and none had specific symptoms suggestive of bacterial sinusitis, such as pain in the upper teeth or in the maxillo-facial area.3, 7, 8 Fifth and most importantly, all our 71 (of 197) patients with sinusitis made a clinical recovery within 21 days without antibiotic treatment, in agreement with the results of Gwaltney et al.11 For definite diagnosis of viral sinusitis, maxillary puncture should have been performed to discover the presence of secretion and viruses and the absence of bacteria in the sinus cavity. However, the ethics of maxillary puncture in patients without signs and symptoms of bacterial sinusitis can be questioned.
In general practice it is difficult to differentiate between the common cold, viral sinusitis, and bacterial sinusitis only on the basis of case history and clinical examination. In our study not much difference was seen between patients with the common cold and patients with viral sinusitis. Patients with sinusitis had more purulent rhinitis and nasal congestion, but clinically assessed, the differences in symptoms were small. Interestingly, patients with viral sinusitis had marginally higher ESRs and more neutrophilic granulocytes. Some of our patients may have had bacterial sinusitis, but they recovered without antibiotic treatment, which is in agreement with the results of van Buchem et al.14 Even the symptoms of bacterial sinusitis are often nonspecific and difficult to distinguish from the symptoms of the common cold.3 Our study was limited, because we followed patients with the common cold only for 21 days, and no cases of bacterial sinusitis were found for comparison. Three weeks after onset of symptoms, all our patients were clinically cured, but 11% still had radiologic sinusitis. It is unknown whether some of them subsequently developed bacterial or chronic sinusitis.
The prevention of sinusitis is important, but there are no proven methods of prevention.2 Although not a statistically significant finding, intranasal FP tended to prevent the development of viral sinusitis in rhinovirus-positive patients when administered from the beginning of common cold. Rhinovirus is the most common etiologic agent of the common cold, causing up to 90% of cold episodes during spring and fall epidemics.9, 15 Because the maximum benefit of FP may take days to appear,16 the effect might have been more beneficial if the treatment period had been longer than 6 days. In addition, if we had included allergic patients and patients prone to sinusitis, the effect could have been more favorable. In these patients topical steroids may effectively prevent viral sinusitis and consequent development of bacterial sinusitis. Five trials have assessed the effect of glucocorticosteroids as an adjunct to antibiotics in the treatment of sinusitis.17, 18, 19, 20, 21 In 4 of these studies, the subjects had chronic sinusitis,18, 19, 20, 21 and the overall effect of glucocorticosteroids was controversial. In our subjects intranasal FP treatment had no clinically recognizable effects on the symptoms of common cold.5
The clinically important yield of our study is that sinuses should not be imaged in patients with the common cold if the signs and symptoms of illness are gradually reducing and there are no signs of bacterial sinusitis. In addition to irradiation and the cost, unnecessary imaging of viral sinusitis may lead to unnecessary treatment.
Footnotes
From the Departments of aPediatrics, bPulmonary Diseases and Clinical Allergology, cDiagnostic Radiology, and dOtorhinolaryngology, Turku University Hospital, Turku; ethe Department of Virology, Turku University, Turku; fNational Public Health Institute, Oulu; and gGlaxoWellcome Ltd, Espoo, Finland.
Supported by the Academy of Finland (Finland), Turku University Foundation (Finland), and GlaxoWellcome Ltd (UK).
Reprint requests: Tuomo Puhakka, MD, Research Unit, Department of Pediatrics, Vähä Hämeenkatu 1 A 3, 20500 Turku, Finland.
0091-6749/98 $5.00 + 0 1/1/92238
References
- 1.Kaliner MA, Osguthorpe JD, Fireman P, Anon J, Georgitis J, Davis ML. Sinusitis: bench to bedside. Current findings, future directions. J Allergy Clin Immunol. 1997;99:S829–S847. [PubMed] [Google Scholar]
- 2.Gwaltney JM., Jr. Sinusitis. In: Mandell GL, Douglas RG, Bennett JE, editors. 4th ed. Churchill Livingstone; New York: 1995. pp. 585–590. (Principles and practise of infectious diseases.). [Google Scholar]
- 3.Hansen JG, Schmidt H, Rosborg J, Lund E. Predicting acute maxillary sinusitis in a general practice population. Br Med J. 1995;311:233–236. doi: 10.1136/bmj.311.6999.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro GG, Rachelefsky GS. Introduction and definition of sinusitis. J Allergy Clin Immunol. 1992;90:417–418. doi: 10.1016/0091-6749(92)90160-4. [DOI] [PubMed] [Google Scholar]
- 5.Puhakka T, Mäkelä MJ, Malmström K, Uhari M, Savolainen J, Terho EO, et al. Common cold: effects of intranasal fluticasone propionate treatment. J Allergy Clin Immunol In press. [DOI] [PubMed]
- 6.Axelsson A, Grebelius N, Chidekel N, Jensen C. The correlation between the radiological examination and the irrigation findings in maxillary sinusitis. Acta Otolaryngol (Stockh) 1970;69:302–306. doi: 10.3109/00016487009123368. [DOI] [PubMed] [Google Scholar]
- 7.Willett LR, Carson JL, Williams JW., Jr. Current diagnosis and management of sinusitis. J Gen Intern Med. 1994;9:38–45. doi: 10.1007/BF02599141. [DOI] [PubMed] [Google Scholar]
- 8.van Duijn NP, Brouwer HJ, Lamberts H. Use of symptoms and signs to diagnose maxillary sinusitis in general practice: comparison with ultrasonography. Br Med J. 1992;305:684–687. doi: 10.1136/bmj.305.6855.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mäkelä MJ, Puhakka T, Ruuskanen O, Leinonen M, Saikku P, Kimpimäki M. Viruses and bacteria in the etiology of the common cold. J Clin Microbiol. 1998;36:539–542. doi: 10.1128/jcm.36.2.539-542.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaiser L, Lew D, Hirschel B, Auckenthaler R, Morabia A, Heald A. Effects of antibiotic treatment in the subset of common-cold patients who have bacteria in nasopharyngeal secretions. Lancet. 1996;347:1507–1510. doi: 10.1016/s0140-6736(96)90670-4. [DOI] [PubMed] [Google Scholar]
- 11.Gwaltney JM, Jr, Phillips CD, Miller RD, Riker DK. Computed tomographic study of the common cold. N Engl J Med. 1994;330:25–30. doi: 10.1056/NEJM199401063300105. [DOI] [PubMed] [Google Scholar]
- 12.Pitkäranta A, Arruda E, Malmberg H, Hayden FG. Detection of rhinovirus in sinus brushings of patients with acute community-acquired sinusitis by reverse transcription-PCR. J Clin Microbiol. 1997;35:1791–1793. doi: 10.1128/jcm.35.7.1791-1793.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savolainen S, Jousimies-Somer H, Karjalainen J, Ylikoski J. Do simple laboratory tests help in etiologic diagnosis in acute maxillary sinusitis? Acta Otolaryngol (Stockh) 1997;29(suppl 5):144–147. doi: 10.3109/00016489709124107. [DOI] [PubMed] [Google Scholar]
- 14.van Buchem FL, Knottnerus JA, Schrijnemaekers VJJ, Peeters MF. Primary-care-based randomised placebo-controlled trial of antibiotic treatment in acute maxillary sinusitis. Lancet. 1997;349:683–687. doi: 10.1016/s0140-6736(96)07585-x. [DOI] [PubMed] [Google Scholar]
- 15.Arruda E, Pitkäranta A, Witek TJ, Jr, Doyle CA, Hayden FG. Frequency and natural history of rhinovirus infections in adults during autumn. J Clin Microbiol. 1997;35:2864–2868. doi: 10.1128/jcm.35.11.2864-2868.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiseman LR, Benfield P. Intranasal fluticasone propionate. A reappraisal of its pharmacology and clinical efficacy in the treatment of rhinitis. Drugs. 1997;53:885–907. doi: 10.2165/00003495-199753050-00014. [DOI] [PubMed] [Google Scholar]
- 17.Barlan IB, Erkan E, Bakir M, Berrak S, Basaran MM. Intranasal budesonide spray as an adjunct to oral antibiotic therapy for acute sinusitis in children. Ann Allergy Asthma Immunol. 1997;78:598–601. doi: 10.1016/S1081-1206(10)63223-1. [DOI] [PubMed] [Google Scholar]
- 18.Meltzer EO, Orgel HA, Backhaus JW, Busse WW, Druce HM, Metzger WJ. Intranasal flunisolide spray as an adjunct to oral antibiotic therapy for sinusitis. J Allergy Clin Immunol. 1993;92:812–823. doi: 10.1016/0091-6749(93)90058-n. [DOI] [PubMed] [Google Scholar]
- 19.Qvarnberg Y, Kantola O, Salo J, Toivanen M, Valtonen H, Vuori E. Influence of topical steroid treatment on maxillary sinusitis. Rhinology. 1992;30:103–112. [PubMed] [Google Scholar]
- 20.Sykes DA, Wilson R, Chan KL, Mackay IS, Cole PJ. Relative importance of antibiotic and improved clearance in topical treatment of chronic mucopurulent rhinosinusitis. A controlled study. Lancet. 1986;2:359–360. doi: 10.1016/s0140-6736(86)90051-6. [DOI] [PubMed] [Google Scholar]
- 21.Cuenant G, Stipon JP, Plante Longchamp G, Baudoin C, Guerrier Y. Efficacy of endonasal neomycin-tixocortol pivalate irrigation in the treatment of chronic allergic and bacterial sinusitis. ORL J Otorhinolaryngol Relat Spec. 1986;48:226–232. doi: 10.1159/000275873. [DOI] [PubMed] [Google Scholar]


