Emergency departments are often inundated with patients on a daily basis, but disaster events can create a surge of patients that significantly impacts the emergency department’s ability to provide organized, effective care. Recent events such as the 2004 Asian Tsunami, which resulted in more than 700 patients arriving at Patong Hospital in Phuket, Thailand, within 2 hours,1 and the 1995 sarin attack in Tokyo, China, which resulted in 500 patients at St. Luke’s Hospital within 1 hour,2 emphasize the need for ED staff to plan and prepare their response to the particular hazards they are at risk for and the potential patient surge that may be generated. This planning, like direct patient care, needs to be driven by more than educated guesses. Careful utilization of current available evidence will help build a strong foundation to serve as the basis for evidence-based ED disaster planning.
The Center for Evidence-Based Medicine defines evidence-based medicine (EBM) as “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients.”3 EBM relies on research findings to support treatment modalities. Applying EBM to disaster research is challenging because of a lack of standard terminology and data collection methods, incomplete medical records, and research that is retrospective in nature.4
Whereas disaster events may not allow for the collection of controlled, experimental data, there is available evidence that can be applied in ED disaster-planning processes. Using current evidence to support or suggest alterations in ED disaster planning will strengthen overall ED preparedness. This article will review the available evidence and apply it to many pressing issues facing ED staff.
Infectious Disease and Chemical Agent Exposure
Disaster planning involving hazardous materials or emerging diseases typically focuses on how to provide treatment for large numbers of patients who present to the emergency department. However, evidence shows that these events often develop over time and patients will include hospital staff who have become exposed to an agent or disease in the process of patient care.
During the 1995 sarin attack on the Tokyo subways, St Luke’s Hospital saw 606 patients and an additional 110 staff members in whom signs and symptoms of exposure developed. In a makeshift patient care area for ED overflow, 38 of 83 staff workers (45.8%) became exposed to sarin.2
The severe acute respiratory syndrome (SARS) outbreak of 2002-2003 also resulted in significant staff exposures. During the first wave of SARS in Toronto, Ontario, Canada, 51% (n = 73) of the patients who contracted SARS were hospital staff. In the second wave, health care workers comprised 39% of cases (n = 29) in which SARS developed.5 In Taiwan 33% of all SARS cases were health care workers.6
The US Department of Health and Human Services’ Agency for Toxic Substances and Disease Registry collects information from 15 cooperating state health departments related to incidents involving the release of hazardous materials through its Hazardous Substances Emergency Events Surveillance (HSEES) system.7
The HSEES study of US hazardous material events breaks down the events based on whether the incident occurred in a rural setting or “other area” setting. The “other area” category includes more populated residential, industrial, and commercial areas; thus it includes urban populated areas.
A study of 8 years of these HSEES data (1992-2000) related to hospital decontamination found that, in the rural setting, 10 events had occurred that required hospital decontamination, which produced 52 patients; in the urban settings, there were a total of 82 events that required hospital decontamination, which produced 889 patients.8 Of the 52 patients in the rural setting needing hospital decontamination, 29 were first responders and 12 were hospital staff. Of the 889 patients in the urban setting needing decontamination, 170 were first responders and 342 were hospital staff. These events show that a significant portion of the patients who needed treatment are hospital staff who have become exposed during the decontamination process. Of the total number of patients who needed decontamination in these events, hospital staff represented 23% of the total patients in rural settings and 38% in urban settings.8
Whether the hazardous event is large or small, the emergency department will most likely lose staff who become exposed to the agent (Figure 1 ), which impacts ED function with decreased staff numbers and increased patient loads. To protect ED staff, there must be clear procedures for dealing with potentially exposed or contaminated patients. This begins with proper assessment of a patient in need of isolation or decontamination and includes understanding what personal protective equipment (PPE) is appropriate. The ED disaster plan must include rapid relocation of the patient from the waiting room to either an isolation room or a decontamination area.
Figure 1.
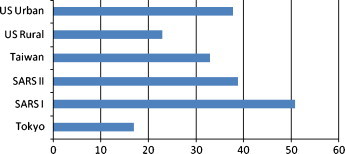
Health care worker exposures as percent of total patients. This figure can be viewed in color and as a full-page document at www.jenonline.org.
ED personnel must also have immediate access to the PPE that they need to limit their risk of exposure. In addition to having a ready supply of N95 masks, chemical suits and respirators should be easily accessible at ED entrances and triage areas. This may require PPE supplies and 2 or 3 respirators for the staff to assist an initially arriving patient; they will not have time to dig deep into far recessed supply rooms to get their PPE supplies for chemical events.
After the Tokyo sarin event, the Japanese government budgeted for only 4 chemical suits per hospital.9 In Toronto there was a general lack of N95 mask use compliance by hospital staff before and during the initial aspects of the SARS epidemic.6 ED staff must have adequate PPE supplies readily available, and the hospital must require compliance with wearing the correct PPE during a potential exposure.
Not only should suits and PPE be rapidly available, but the equipment should be readily accessible. Large-scale decontamination systems have the capability of handling large numbers of patients but often lack the capability of being immediately operational. Patients arrive rapidly to the emergency department after exposure events. In the Tokyo sarin event, patients arrived at St. Luke’s Emergency Department within 12 minutes of the first hospital notification that there had been an event.2 Large decontamination systems may not be needed because evidence suggests that small numbers of patients (between 5 and 15) usually require hospital decontamination.8 For ED planning, this means that a scalable decontamination process, one that can start small and then immediately ramp up over time, is needed. Emergency departments should use multiple showerheads in their decontamination rooms in addition to outside systems that may range from garden hoses with nozzles to fixed shower systems concreted in place. Decontamination procedures can start immediately with the first arrival of patients, and if the event escalates, the decontamination process continues at the initial sites until the large showers are assembled and ready to go.
A lesson learned from the sarin attack in the Tokyo subways is that staff will have difficulty identifying the chemical agent involved in the exposure. At 8:28 am, the first patients arrived at Tokyo’s St. Luke’s Emergency Department. At 9:00 am, the emergency department received initial notification that the Tokyo Fire Department had identified the chemical (incorrectly) as acetonitrile. At 9:40 am, a medical doctor with experience from the previous sarin attack in Matsumoto, Japan, called to advise medical staff to suspect sarin, and the hospital began treating patients with the appropriate MARK 1 sarin antidote kits at that time. It was not until 11:00 am that the hospital was notified that police analysis had identified the chemical as sarin and the ED staff received that information while watching the television news.9
Because scene reports may be delayed or inaccurate and laboratory confirmation takes time, ED staff must be knowledgeable about the presenting signs and symptoms of the various types of agents and infectious diseases. Information from patients about the event and their signs and symptoms will be the primary sources of data that ED personnel receive to determine what agent the patients may have been exposed to. Staff must have the ability to start decontamination or isolation procedures as soon as they are suspicious that an exposure occurred, and this clinical suspicion needs to be based in appropriate training. Training needs to include not only basic classes reviewing agent characteristics but also the application of that knowledge into practical considerations, such as how and when to implement ED response procedures. This can be accomplished through interactive classes, role playing, and regular drilling. It is crucial that the ED charge nurses have regular practice with the decision-making steps that they will need to perform when they believe a patient has been exposed to a chemical or infectious agent. Staff should not experience repercussions for “jumping the gun” if their suspicions of contamination turn out to be erroneous.
In Toronto, ED staff were unaware of the SARS events taking place in Hong Kong and China, because of a lack of international health alerts about SARS.5 As a result, ED personnel did not know what pertinent questions were needed in the triage assessment (e.g., travel history). Hospitals must ensure that their personnel has up-to-date information to correctly identify and isolate contaminated patients. This consists of maintaining access to health alerts through systems such as the Centers for Disease Control and Prevention’s Health Alert Network. These alerts should be monitored daily to ensure dissemination to the ED staff.
Surge
Disasters are the result of a variety of events, and the impact on hospitals is in 2 forms. Events such as explosions or chemical releases cause an immediate impact on the hospital. Events involving infectious disease outbreaks or biologic agent exposures cause a slower but more long-term impact on the hospital. Both types of events can produce a surge, that is, an increase in normal patient census that can strain an emergency department’s ability to provide efficient and effective care to patients.
Immediate Impact
The time of the first patient arrival to the emergency department after a disaster event occurs varies, typically from 5 to 30 minutes.2, 10, 11, 12, 13 However, given the time involved in scene evaluation, the emergency department may not have notification that an event has occurred before receiving patients. For instance, during the 2005 bombings in London, England, the London hospitals received notification 17 minutes after the first of the bombings occurred, and it was only notification of a “suspicious event”: it was another 19 minutes before authorities declared a “major incident.”14
Between 66% and 93% of patients arriving to the emergency department from the scene of a disaster do so by means other than EMS transport.9, 10, 11, 12, 13 These self-directed patients are usually the “walking wounded” (i.e., those with minor injuries) and are the first to arrive because they have left the scene before EMS arrival. Because critical patients cannot typically leave the scene without EMS transport, they tend to arrive later as a result of the inherent scene delays as EMS works to establish incident command and triage with few initial ambulances on the scene.
These “walking wounded” patients can consume valuable ED resources before the arrival of the more seriously injured patients. Disaster triage in the emergency department should be aimed at rapidly identifying the patients with minor injuries and relocating them to a minor treatment area (MTA) outside the main emergency department to keep valuable ED rooms available for potential critical patients, who have yet to arrive. The MTA needs to be large enough to accommodate large volumes of patients, because up to 80% of presenting patients1, 2, 9, 10, 11, 14, 15, 16, 17 will be low-acuity patients and should be triaged to this area. Additional resources, such as counseling, assistance with contacting families, and basic comfort measures, will be needed in the MTA area.
As incoming patients surge in volume, ED staff should be surged to additional triage stations to rapidly process the incoming walking wounded. The number of arriving patients often peaks within 60 to 90 minutes, and within 2 to 4 hours, most of the patients have arrived (Figure 2 ).1, 2, 10, 11, 12, 13, 14, 15, 16 As the arrival of the patients with minor injuries diminishes and more critical patients begin arriving, triage stations can be shut down, and these nurses are then available to staff the treatment areas.
Figure 2.
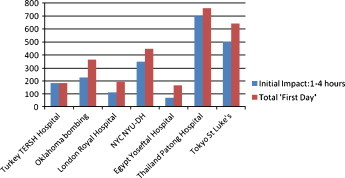
Surge from immediate impact events. This figure can be viewed in color and as a full-page document at www.jenonline.org. NYCNYU-DH, New York City New York University Downtown Hospital
Resources will need to be prioritized for incoming critical ICU or operating room patients during the peak period 2 to 4 hours into the event. Because many emergency departments are routinely at or near capacity with a combination of admitted patients awaiting inpatient rooms and other patients awaiting laboratory or radiographic results, a mechanism needs to be in place to relocate these patients to free up ED beds for acute or critical patients. This will involve expediting discharges or bed assignments for admitted patients and will require coordinated hospital-wide cooperation. The incoming volume may still exceed ED capacity, given that a typical sudden-onset surge event will generate 5 to 30 patients needing critical care, or 5% to 37% of the total hospital admissions (Figure 3 ).9, 11, 14, 17, 18, 19 A temporary surge admission/holding area will be needed to prevent patient bottleneck in the emergency department. Patients would be held in this temporary surge area and monitored by nurses from areas other than the emergency department who responded to the disaster call-down process, which will allow critical patients immediate access to ED beds and staff capable of providing emergency resuscitation and stabilization.
Figure 3.
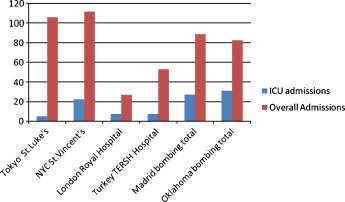
ICU admissions compared with overall admissions. This figure can be viewed in color and as a full-page document at www.jenonline.org. ICU, Intensive Care Unit; NYC, New York City
Sudden surge from blast events will include patients who will require advanced airway procedures. Enclosed bombings, such as bus bombings, tend to cause a greater number of fatalities and a greater number of patients with life-threatening injuries because of the amplification of the blast. One study shows a 42% intubation rate for bus bombings compared with a 7% intubation rate for open-air bombings.20 As Figure 4 shows, this typically translates to 7 to 20 patients who will require intubation from a blast event. Surge planning should, therefore, incorporate airway considerations and include the involvement of hospital respiratory therapists. Airway supplies should be rapidly available and include either immediate access to traditional ventilators or disposable ventilators for temporary use.
Figure 4.
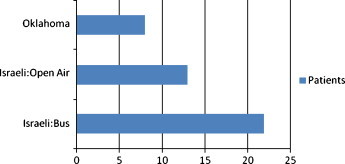
Blast injury patients requiring intubation. This figure can be viewed in color and as a full-page document at www.jenonline.org.
Other hospital services, such as radiography, computed tomography scan, and dialysis, will be impacted by the disaster event. During the bombings in Oklahoma City, Okla, Manchester, England, and Bologna, Italy, 40% to 50% of arriving patients needed radiology procedures.20 Nineteen percent of the patients from the Oklahoma City bombing required computed tomography scan.10 During Taiwan’s Chi-Chi Earthquake, 30% of the 95 patients with crush syndrome needed hemodialysis.21 Plans for obtaining portable x-ray machines and portable dialysis units need to be considered, and the ED staff should plan for a system to prioritize these services before an event occurs.
Many disaster events result in the deployment of a field medical team from the hospital to the scene. At the Tokyo sarin attack, St. Luke’s Hospital (the most heavily impacted hospital) sent 8 physicians and 3 nurses to the scene; however, no emergency procedures were performed.2 At the London bombing, the only Grade 1 Trauma Center, designated as the primary receiving center for bombing victims, sent physician teams to the field scenes.14 In New York City, NY, on September 11, 2001, Chelsea Piers was set up as a triage area and staffed with physicians from New York University’s Downtown Hospital, close to the World Trade Center site, but they saw no critical patients; Bellevue Hospital also sent physician teams to the World Trade Center site who cared for patients with minor cuts and bruises but no critical patients.16 Sending physician/nurse field teams to disaster sites has limited value. The teams often arrive late and leave their hospitals with less coverage. EMS usually has well-established and well-drilled mass casualty plans that do not include the use of an ad hoc team; the arrival of uncoordinated volunteers on the scene detracts from scene coordination rather than enhancing it. The hospital teams might be better utilized by staying at their hospital or moving to more heavily impacted hospitals unless specifically requested by EMS. EMS should then have a clear plan in place to maximize the use of the teams by directing them to patients needing critical medical interventions.
Gradual Impact
The patient surge from disaster events caused by infectious diseases or biologic diseases causes a more gradual and longer-term impact on the hospital than a blast or chemical event. The surge from the SARS epidemic had a gradual impact on hospitals in Hong Kong, Taiwan, and Toronto. There were 668 total SARS admissions during the Taiwan outbreak (March-July 2003) and 375 total cases in Toronto (March-June 2003).5, 22 However, there were also decreases in ED visits and overall bed occupancy during these time periods, attributed in part to people avoiding the risk of becoming infected during a hospital visit. Comparing pre-SARS data and data collected during the SARS event, National Taiwan University Hospital noted a 63% decrease in ED visits, and overall bed occupancy decreased from 86% to 38%.23 Similarly, China Medical University Hospital noted a 33.4% decrease in ED visits, and among 15 hospitals, there was an overall decrease of 19.9% in bed occupancy.24, 25 Canada’s Hospital for Sick Children found a mean decrease of 27% in patient volume in their emergency department during the SARS epidemic.26
SARS resulted in staff shortages, primarily in the emergency department and ICU, because of potential exposures, quarantine, and staff choosing not to report to work. However, the documented decrease in ED visits and hospital admissions, noted previously, can help alleviate this shortage. Disaster plans should incorporate closure of a portion of the hospital’s general non-isolation beds; staff and supplies from these areas should be used to support the new surge isolation units and the emergency department, which will need to cover staff shortages and will require additional personnel to staff an outside screening center.
Although studies show that overall ED visits decrease, that decrease is largely a result of redirecting patients to screening centers or fever clinics. These centers are established to provide an assessment area before entry into the emergency department and to limit ED admissions to those patients with significant signs and symptoms of infection. These centers can be constructed as stand-alone structures or retrofitted onto an existing entryway. Over a period of 3 weeks, National Taiwan University Hospital screened 754 patients and admitted 63 at its screening unit, and over a period of 1 month, a Toronto teaching hospital screened over 1,000 patients and admitted 70.26, 27 The screening centers should have patients spaced sufficiently apart and proper PPE in place to limit the potential spread of the agent in overcrowded conditions. On the basis of established local public health criteria, patients testing positive will be sent to home quarantine or admitted. (In Ontario, with a population of 11 million, 10,000-20,000 people were home quarantined.)28
Communication
Contending with communication difficulties is a major challenge in disaster events even if telecommunication infrastructure remains intact. During September 11, St. Vincent’s Hospital had neither cell phone nor public telephone availability, because all systems were overwhelmed.18 In the Tokyo subway event, St. Luke’s Hospital found its internal communications jammed, and personnel were forced to yell down the hall to relay information.2 Bombings in Istanbul, Turkey, resulted in complete city phone and cell phone system failure.11 In New Orleans, La, Tulane Hospital’s post–Hurricane Katrina communication failure caused the inability to activate its disaster plan.29
Hospitals have an over-reliance on communication systems and (electrically powered) computer-based systems. Large-scale events are going to disrupt the infrastructure that supports both civilian and medically used communication systems. Surviving hospital communication systems will be overwhelmed with incoming calls from the community. Even relatively small events (e.g., bombings) will cause a failure in the local communication system.
ED communication planning must have backup plans in place that do not rely on public phone or cell phone systems. Simple 2-way handheld radios (walkie-talkies) should be in place to use during communication failure; these types of radios need no outside source (e.g., a cell phone tower) to operate. Runners are still an effective way to communicate during a system failure, but runners must be assigned to that role and there should be at least 1 assigned to each independent area.
Summary
Using the best currently available evidence creates a strong, justifiable foundation of lessons learned, expert opinions, study results, and survey measurements to form the basis of ED disaster planning. This evidence helps identify deficiencies in current planning (e.g., training, supplies, or procedures) and helps to prioritize the shortcomings that need to be addressed. ED staff charged with preparing for a disaster, or staff members who understand the need for preparedness and step forward to fill the void, should conscientiously seek out the evidence and apply it to ED disaster preparedness.
Biography
Robert Powers, Member, Heart of Carolina Chapter, is Consultant, Emergency Services Disaster Consulting and Research, Raleigh, NC.
Footnotes
Earn Up to 8 CE Hours. See page 272.
There are no conflicts of interest.
References
- 1.Leiba A, Ashkenasi I, Nakash G, Pelts R, Schwartz D, Goldberg A. Response of Thai hospitals to the Tsunami disaster. Prehosp Disaster Med. 2006;21:s32–s37. [PubMed] [Google Scholar]
- 2.Okumura T, Suzuki K, Fukuda A, Kohama A, Takasu N, Ishimatsu S, Hinohara S. The Tokyo subway sarin attack: disaster management, part 1: community emergency response. Acad Emerg Med. 1998;5:613–628. doi: 10.1111/j.1553-2712.1998.tb02470.x. [DOI] [PubMed] [Google Scholar]
- 3.Center for Evidence-Based Medicine. Available at: http://www.cebm.net/glossary.asp. Accessed February 10, 2007.
- 4.World Association of Disaster and Emergency Medicine Hospital disaster management: guidelines for evaluation and research in the Utstein style. Volume I. Conceptual framework. 2003. http://pdm.medicine.wisc.edu/Guidelines/TOCVol1.htm Available at: Accessed February 20, 2007. [PubMed]
- 5.The SARS Commission Spring of fear. http://www.sars.ca Available at: Accessed February 20, 2007.
- 6.Centers for Disease Control and Prevention Severe acute respiratory syndrome—Taiwan 2003. MMWR Weekly. 2003;52:461–466. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5220a1.htm Available at: Accessed February 25, 2007. [PubMed] [Google Scholar]
- 7.Agency for Toxic Substance and Disease Registry. Available at: http://www.atsdr.cdc.gov/HS/HSEES/hsees.html. Accessed July 30, 2007.
- 8.Berkowitz Z, Horton DK, Kaye WE. Hazardous substances releases causing fatalities and/or people transported to hospitals: rural/agricultural vs. other areas. Prehosp Disaster Med. 2004;19:213–220. doi: 10.1017/s1049023x00001801. [DOI] [PubMed] [Google Scholar]
- 9.Pangi R. Consequence management in the 1995 sarin attacks on the Japanese subway system. BCSIA Discussion Paper 2002-4, ESDP Discussion Paper ESDP-2002-01. John F. Kennedy School of Government, Harvard University; Cambridge (MA): 2002. [Google Scholar]
- 10.Hogan D, Waeckerie J, Dire D, Lillibridge S. Emergency department impact of the Oklahoma City terrorist bombing. Ann Emerg Med. 1999;34:160–167. doi: 10.1016/s0196-0644(99)70224-6. [DOI] [PubMed] [Google Scholar]
- 11.Rodoplu U, Arnold JL, Tokyay R, Ersoy G, Cetinar S, Yücal T. Mass-casualty terrorist bombings in Istanbul, Turkey, November 2003: report of the events and the prehospital emergency response. Prehosp Disaster Med. 2004;19:133–145. doi: 10.1017/s1049023x00001643. [DOI] [PubMed] [Google Scholar]
- 12.Leiba A, Blumenfeld A, Hourvitz A, Weiss G, Peres M, Laor D. Lessons learned from cross border medical response to the terrorist bombings in Tabba and Ras-el-Satan, Egypt on 07 October 2004. Prehosp Disaster Med. 2005;20:253–257. doi: 10.1017/s1049023x00002624. [DOI] [PubMed] [Google Scholar]
- 13.Aud der Heide E. The importance of evidence-based disaster planning. Ann Emerg Med. 2006;47:34–49. doi: 10.1016/j.annemergmed.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Mohammed AB, Mann HA, Nawabi DH, Goodier DW, Ang SC. Impact of London’s terrorist attacks on a major trauma center in London. Prehosp Disaster Med. 2006;21:340–344. doi: 10.1017/s1049023x00003988. [DOI] [PubMed] [Google Scholar]
- 15.Aylwin CJ, Konig TC, Brennan NW, Shirley PJ, Davies G, Walsh MS, Brohi K. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2006;368:2219–2225. doi: 10.1016/S0140-6736(06)69896-6. [DOI] [PubMed] [Google Scholar]
- 16.Cushman J, Pachter H, Beaton H. Two New York City hospitals’ surgical response to the September 11, 2001, terrorist attack in New York City. J Trauma. 2003;54:147–155. doi: 10.1097/00005373-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 17.de Ceballos JP, Turegano-Fuentes F, Perez-Diaz D, Sanz-Sanchez M, Martin-Llorente C, Guerrero-Sanz JE. 11 March 2004: the terrorist bomb explosions in Madrid, Spain—an analysis of the logistics, injuries sustained and clinical management of casualties treated at the closest hospital. Crit Care. 2005;9:104–111. doi: 10.1186/cc2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirschenbaum L, Keene A, O’Neill P, Westfal R, Astiz M. The experience at St. Vincent’s Hospital, Manhattan, on September 11, 2001: preparedness, response, and lessons learned. Crit Care Med. 2005;33(Suppl):S48–S52. doi: 10.1097/01.ccm.0000151067.76074.21. [DOI] [PubMed] [Google Scholar]
- 19.Teague DC. Mass casualties in the Oklahoma City bombing. Clin Orthop Relat Res. 2004:77–81. doi: 10.1097/01.blo.0000131201.20418.82. [DOI] [PubMed] [Google Scholar]
- 20.Halpern P, Tsai MC, Arnold JL, Stok E, Ersoy G. Mass-casualty, terrorist bombings: implications for emergency department and hospital emergency response (part II) Prehosp Disaster Med. 2003;18:235–241. doi: 10.1017/s1049023x00001102. [DOI] [PubMed] [Google Scholar]
- 21.Chan YF, Alagappan K, Gandhi A, Donovan C, Tewari M, Zaets SB. Disaster management following the Chi-Chi Earthquake in Taiwan. Prehosp Disaster Med. 2006;21:196–202. doi: 10.1017/s1049023x00003678. [DOI] [PubMed] [Google Scholar]
- 22.McDonald LC, Simor AE, Su SJ, Maloney S, Ofner M, Chen KT. SARS in healthcare facilities, Toronto and Taiwan. Emerg Infect Dis. 2004;10:777–781. doi: 10.3201/eid1005.030791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen YC, Chen MF, Liu SZ, Romeis JC, Lee YT. SARS in teaching hospital, Taiwan. Emerg Infect Dis. 2004;10:1886–1887. doi: 10.3201/eid1010.040356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen W, Cheng Y, Chung Y, Lin C. The impact of the SARS outbreak on an urban emergency department in Taiwan. Med Care. 2005;43:168–172. doi: 10.1097/00005650-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Chen TJ, Lin MH, Chou LF, Hwang SJ. Hospice utilization during the SARS outbreak in Taiwan. BMC Health Serv Res. 2006;6:94. doi: 10.1186/1472-6963-6-94. http://www.biomedcentral.com/1472-6963/6/94 Available at: Accessed March 12, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boutis K, Stephens D, Lam K, Ungar W, Schuh S. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. 2004;171:1353–1358. doi: 10.1503/cmaj.1031257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen YC, Huang LM, Chan CC, Su CP, Chang SC, Chang YY. SARS in hospital emergency room. Emerg Infect Dis. 2004;10:782–788. doi: 10.3201/eid1005.030579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 29.Gray B, Hebert K. Hospitals in Hurricane Katrina: challenges facing custodial institutions in a disaster. The Urban Institute. 2006. http://www.urban.org/publications/411348.html Available at: Accessed February 20, 2007. [DOI] [PubMed]


